FIG. 7.8 Internal female reproductive organs. Posterior view. Diagram shows left side of uterus and upper portion of the vagina and the left uterine tube and ovary in a frontal section. The broad ligament has been removed from the posterior surface of the uterus and adjacent structures. (From Patton KT, Thibodeau GA: The human body in health & disease, ed 6, St Louis, 2014, Mosby.)
Obstetric Surgeries
Procedures
• Cesarean section
• Cervical cerclage
• Vaginal delivery
Basic Anatomy Involved
• Uterus
• Bladder
• Round ligament
• Broad ligament
• Cardinal ligament
• Uterosacral ligament
Additional Facts to Remember
• In most OB/GYN procedures, a Foley or straight catheter will be inserted beforehand to decompress the bladder and help prevent injury.
C-section or Vaginal Delivery
• Remember that failure to progress is the primary indicator for C-section.
• In a C-section, four surgical counts are taken:
• Before skin incision
• Before closure of the uterus
• Before closure of the peritoneum (abdominal cavity)
• Before closure of the skin
• The bladder is freed from the uterus before an incision is made into the uterus.
• The umbilical cord is cut either with Lister bandage scissors or curved Mayo scissors.
• Umbilical cord blood may be collected for cord blood gas determination. Why? Umbilical cord pH and blood gas values provide valuable information regarding an infant’s metabolic condition at birth; base excess determination quantifies the magnitude of perinatal hypoxia/asphyxia and metabolic acidosis, the putative risk factor for central neurological injury
• A De Lee suction catheter is used to suction meconium-stained amniotic fluid. Before or during labor, the fetus sometimes passes meconium (fetal stool) into the amniotic sac. The reason is not clearly understood, but this phenomenon is thought to be related to fetal distress in some babies. The thick meconium mixes with the amniotic fluid and then swallowed and breathed into the airway by the fetus. As the neonate takes the first breaths after delivery, meconium particles may enter the airway and be aspirated deep into the lungs.
• The placenta is placed in a large basin and passed off to the circulating nurse, who will check for evidence of abnormality, such as infection or chronic blood deprivation, and determine whether the placenta is whole or shows any meconium discoloration.
Cervical Cerclage (Shirodkar and McDonald Procedures)
• Shirodkar: In this procedure, a suture is used to close the internal os in a pregnant woman whose cervix has failed to retain previous pregnancies. The sutures are passed through the walls of the cervix so they’re not exposed. In most cases, a cesarean section will eventually be performed.
• McDonald: The internal os is sutured after the lower part has already started to efface (Fig. 7.9). Sutures are usually placed between 16 and 18 weeks of pregnancy and removed around the 37th week.
• These procedures are performed during the second or third trimester because the cervix tends to dilate spontaneously at this time, possibly resulting in spontaneous abortion.
• The procedure may be performed one of two ways:
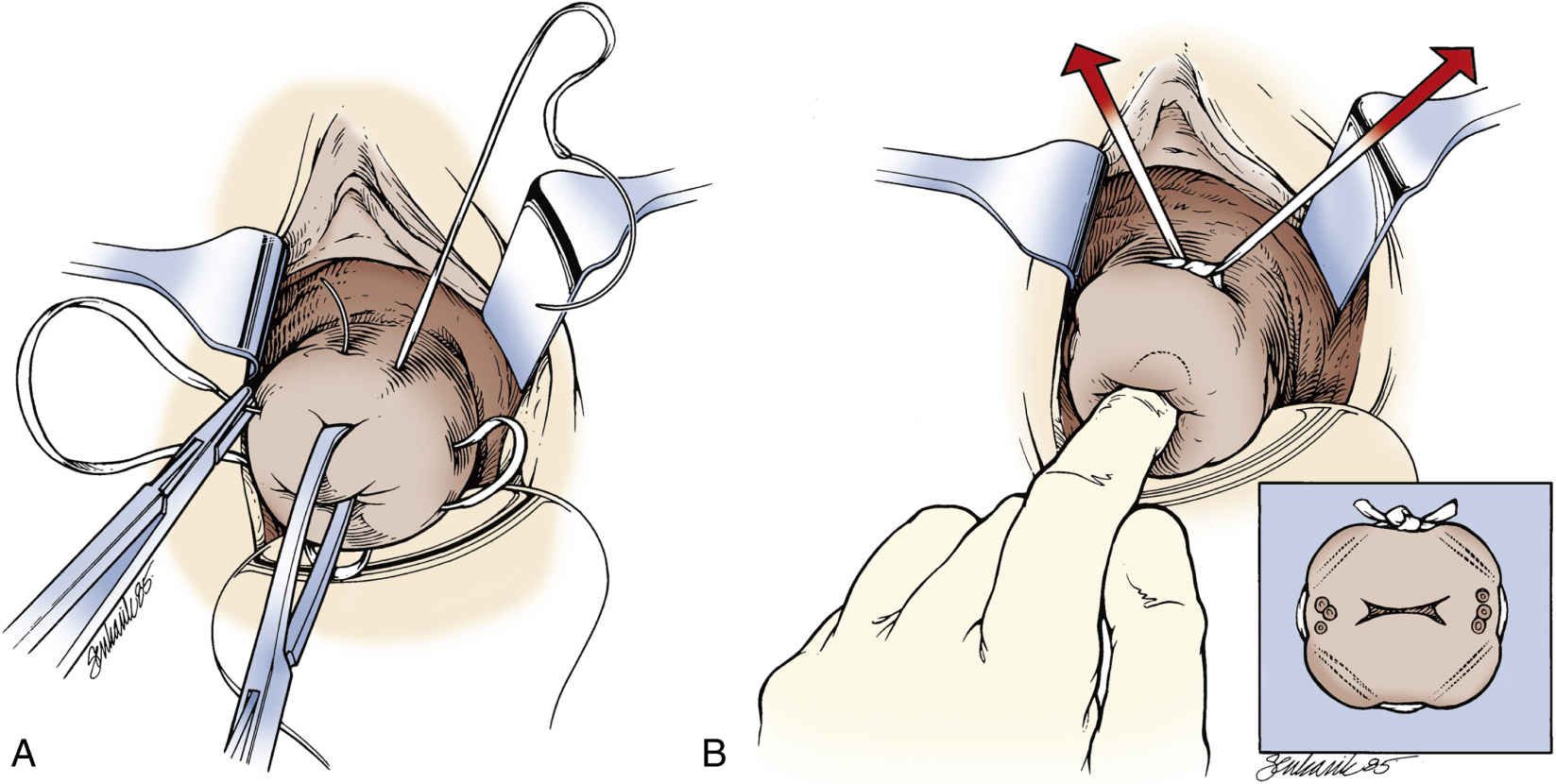
FIG. 7.9 Placement of sutures for McDonald cerclage. A, Double-headed Mersilene band with four bites in the cervix, avoiding the vessels. B, The suture is placed high up in the cervix, close to the cervicovaginal junction, approximately at the level of the internal os. (From Gabbe SG, et al: Obstetrics: normal and problem pregnancies, ed 7, Philadelphia, 2017, Elsevier.)
• In transabdominal cerclage (TAC), Mersilene tape (suture) is placed at the internal os after a short suprapubic incision is made. C-section is required for delivery.
Mapping
Here you can see how two commonly performed procedures, the cesarean section and cervical cerclage, look when they’re mapped:
Ready to map the remaining OB/GYN procedure? Use the template available on the Evolve Resources site.
• Vaginal delivery
Gynecologic Abdominal Contents Procedures
These procedures involve the uterus, fallopian tube, ovary, or some combination thereof. They may be performed as open surgeries or laparoscopically, depending on the procedure.
Laparoscopic Surgeries
Procedures
Equipment
• Light cord
• Camera
• Insufflation tubing
• Trocars
• Laparoscopic instruments
• Minor soft instruments
Additional Facts to Remember
• In all GYN laparoscopic procedures, it is important to have a GYN major tray available along with other accessory supplies in case the surgeon decides to perform an open surgery.
Open Surgeries
Procedures
• TAH (total abdominal hysterectomy)
Radical hysterectomy (Fig. 7.10) is the removal of the ovaries, fallopian tubes, uterus, upper third of the vagina, and associated lymph nodes.
• Vaginal hysterectomy is removal of the uterus by way of a vaginal approach. It’s ideal for the patient with a prolapsed uterus.
• Pelvic exenteration
Equipment
• GYN major instruments
Additional Facts to Remember
• In TAH and LAVH, a Foley or straight catheter will be inserted before the procedure to decompress the bladder and help prevent injury.
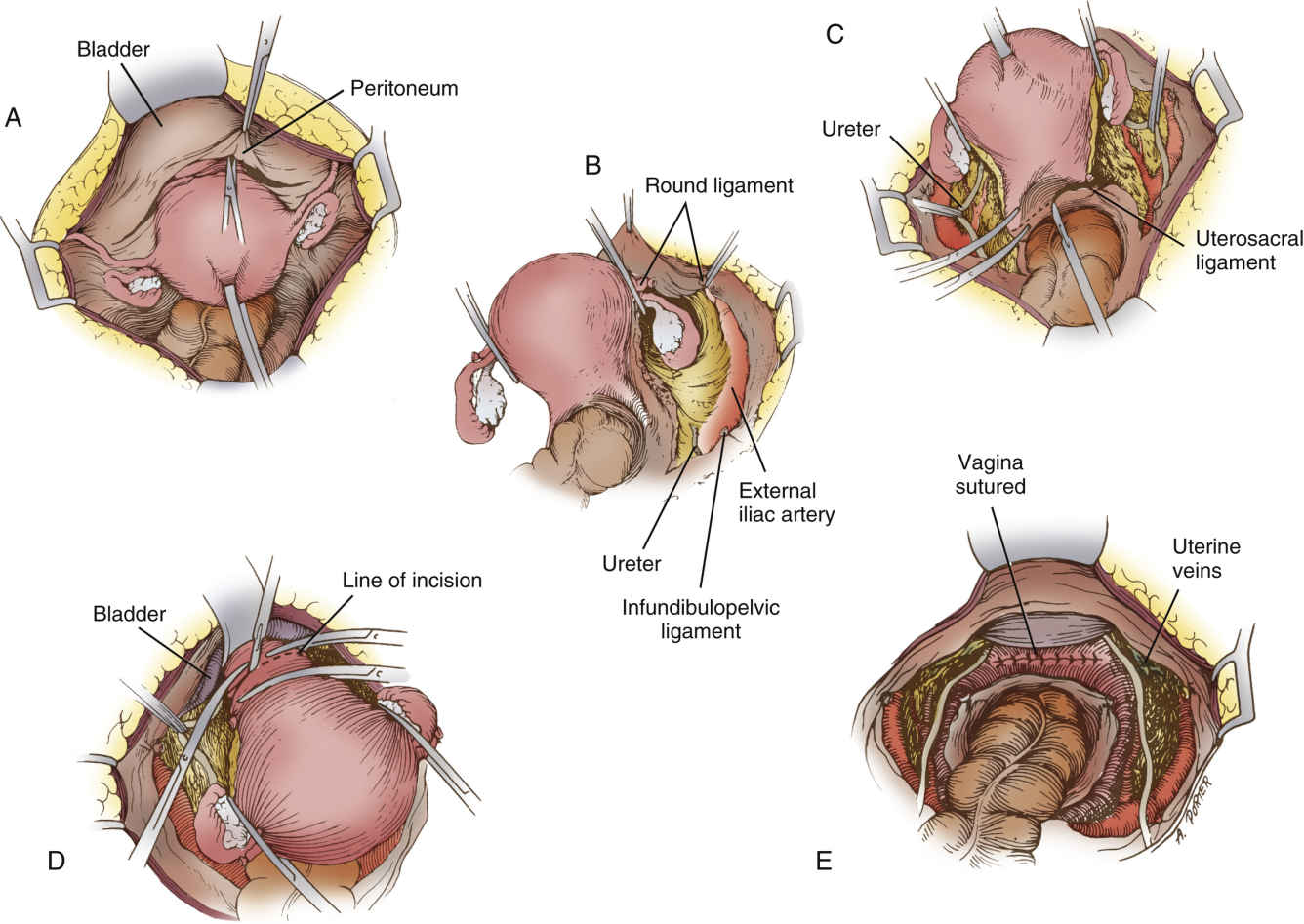
FIG. 7.10 Wertheim radical hysterectomy. A, With upward traction applied on uterus, peritoneum is incised from round ligament to round ligament. B, Right round and infundibulopelvic ligaments are ligated and cut, thus exposing right external iliac artery. C, Uterus is held upward and forward, exposing cul-de-sac, which is incised as shown by dotted line. D, After dissection is completed, vagina is doubly clamped preparatory to transection, after which entire specimen is lifted out en bloc. E, Vagina is closed. Peritoneum remains to be reperitonealized. (From Rothrock JC, Alexander SM: Alexander’s surgical procedures, ed 1, St. Louis, 2012, Mosby.)
Mapping
Here’s how total abdominal hysterectomy looks when mapped:
Go ahead and try to map the remaining procedures, using the template on the Evolve Resources site:
• Tuboplasty
• Tubal sterilization
• GYN laparoscopy
• Resection of ectopic pregnancy
• Myomectomy
• Pelvic exenteration
• Salpingectomy
• Oophorectomy
Vaginal Procedures
Procedures
• Marsupialization of abscessed Bartholin gland (Fig. 7.11)
• Hysteroscopy
• Anterior (cystocele) and posterior (rectocele) colporrhaphy
• Dilation & curettage (D&C)
• Suction D&C
• Labiaplasty
• Vulvectomy
Basic Hysteroscopy Equipment Required
• Light cord
• Camera
• Irrigation tubing
• Trocars
• Hysteroscopic instruments
• D&C instruments
• Fluid (medium for distention)
• Allen or candy cane stirrups for lithotomy position
Additional Facts to Remember
• Marsupialization of a Bartholin gland consists of incison, opening (like a kangaroo’s pouch), and drainage of the gland, followed by suturing to keep the incision open and permit healing by granulation from the base of the pouch.
• Two types of specimens may be obtained during D&C: endometrial and endocervical.
• A red rubber Robinson straight catheter is used to decompress the bladder and help prevent injury.
• A pudendal block—injection of anesthetic into the pudendal canal, where the pudendal nerve is located—provides quick pain relief and blockage of sensation in the perineum, vulva, and vagina.
• Menorrhagia is the medical term for menstrual periods involving abnormally heavy or prolonged bleeding. It is a common concern among premenopausal women.
• Metrorrhagia is uterine bleeding at irregular intervals, particularly between the expected menstrual periods.
• Dysmenorrhea is painful menstruation, typically involving abdominal cramps.
• In marsupialization of a Bartholin gland, the wound is allowed to heal through granulation.
• Endometrial and endocervical specimens should be sent separately.
• In all vaginal procedures, the patient’s legs are placed in and removed from stirrups simultaneously.
Mapping
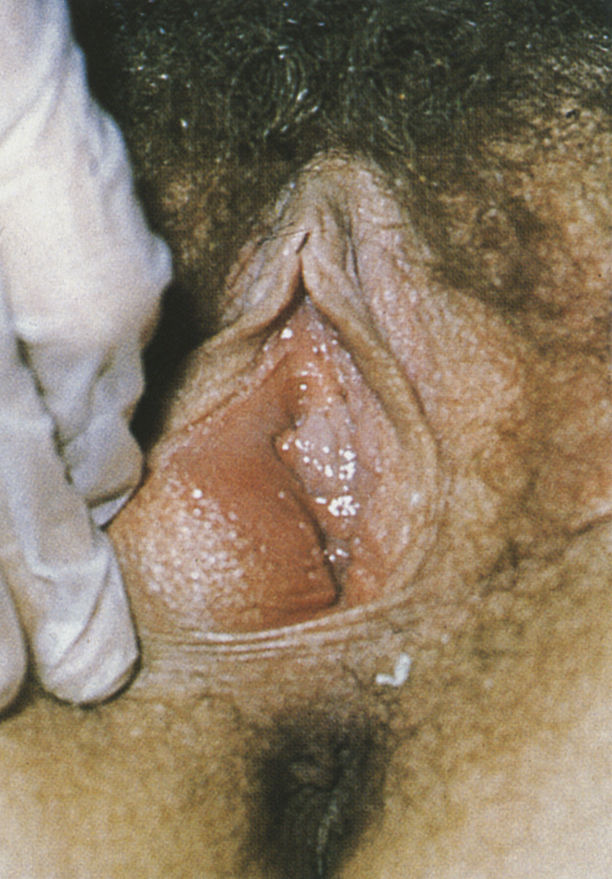
FIG. 7.11 Bartholin abscess. (From Emond RT: Colour atlas of infectious diseases, ed 4, St Louis, 2003, Mosby.)
Use the template available on the Evolve Resources site to map the remaining procedures:
• Hysteroscopy
• Anterior (cystocele) and posterior (rectocele) colporrhaphy
• Labiaplasty
• Vulvectomy