CHAPTER 14 Supracondylar Fractures of the Elbow in Children
INTRODUCTION
Supracondylar humerus fractures are the most common fracture about the elbow in children and have the highest complication rate for elbow fractures in this age group.8,16,39 These compelling facts continue to pique the interest and hold the attention of orthopedists who treat pediatric patients. Since the last edition of this text, issues that have generated the most discussion regarding supracondylar fracture treatment concern timing of reduction and treatment as well as pin configuration used for fracture stabilization. Both issues are addressed in the body of this chapter.
INCIDENCE AND ETIOLOGY
Supracondylar humerus fractures almost exclusively affect the immature skeleton.41,50 Eliason25 reported that 84% of supracondylar fractures occurred in patients younger than 10 years. The peak age for supracondylar humerus fracture has been reported to be between ages 6 and 7 years, and the left arm is injured more frequently than the right.* Previous reports have suggested that supracondylar fractures are common in boys, but more recent studies have documented an equal sex distribution.†
Traditional teaching has held that the peak incidence for extension-type supracondylar humerus fractures occurs at approximately age 7 because that is the age of maximum elbow flexibility and hyperextension. This mechanism has been confirmed by research suggesting that a fall on a hyperextended elbow produces a supracondylar humerus fracture, whereas a fall on an outstretched arm without elbow hyperextension is more likely to cause a distal radius fracture.60 Hyperextension converts what would be an axial loading force to the elbow into a bending moment. The tip of the olecranon acts as a fulcrum, causing the fracture to occur through the relatively thin bone of the olecranon fossa (Fig. 14-1). The distinctive shape of the humeral metaphysis with the medial and lateral condyles and columns, and the narrow midpoint of the olecranon fossa, adds to the instability of the fracture, particularly when there is rotation and tilting of the distal fragment.62,63
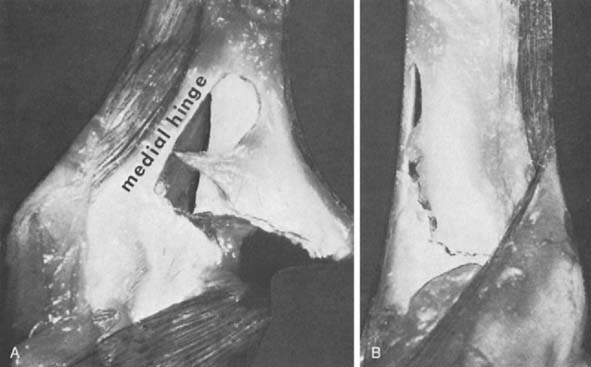
Knowledge of elbow anatomy is important to understanding the cause of the injury, and to understanding effective treatment principles (see Chapters 2 and 3). The stability of the elbow derives from bony and soft tissue structures.33,61,66 Soft tissue stability on the lateral aspect of the elbow is provided by an expansion of the triceps, anconeus, brachioradialis, and extensor carpi radialis longus. The thickened periosteum of a young child, both medially and laterally, is an important additional stabilizer of the fracture fragment and provides a medial or lateral hinge during attempted reduction (Fig. 14-2). Research by Khare et al45 has confirmed the importance of the triceps tendon’s acting as a tension band to achieve fracture stability in the flexed elbow.
Because angular deformity is a common complication of these fractures, the normal variations in pediatric anatomy should be understood. The carrying angle of the elbow joint is the angle formed by the intersection of the longitudinal axis of the arm and the forearm (Fig. 14-3). The normal elbow is usually in slight valgus alignment, but this feature varies among children.1,17,77 Smith77 noted that, of 150 children aged 3 to 11, the carrying angle in boys averaged 5.4 degrees and ranged from 0 to 11 degrees, whereas in girls, it averaged 6 degrees and ranged from 0 to 12 degrees. Aebi1 observed that the measurements were not constant and changed as the child matured, tending to decrease in magnitude and in variation between children.
Although not commonly associated with abuse in the past, a recent report found that 36% of patients younger than age 15 months at the time of their supracondylar fracture sustained the fracture as a result of abuse.79 Clinicians must exclude “nonaccidental trauma” as a potential cause of injury whenever an infant presents with a supracondylar humerus fracture.
CLASSIFICATION
A classification system should guide treatment, provide information on prognosis, and facilitate research by ensuring that similar injuries are compared in the literature. The vast majority of supracondylar humerus fractures can be classified as either flexion or extension injuries, a distinction based on the radiographic appearance and the mechanism of injury. The distinction is important for treatment because the reduction maneuvers are essentially opposite for the two fracture types and flexion-type fractures are significantly more difficult to reduce by closed means. A small minority of fractures exhibit multidirectional instability and do not fit into either flexion or extension types.49 Recognition of multidirectional instability is helpful in formulating an effective treatment strategy.
FLEXION-TYPE FRACTURES
Flexion-type fractures are the result of a direct fall onto a flexed elbow in which a powerful flexion force is applied to the distal humerus, usually through the olecranon. The distal humeral fragment is displaced anteriorly, and the fracture line crosses the humerus from the distal posterior to the proximal anterior aspect (Fig. 14-4). Flexion-type fractures are frequently completely displaced and are difficult to reduce by closed means. The reduction maneuver for flexion-type fractures involves elbow extension or involves using the forearm to apply a posterior-directed force to the anteriorly displaced distal fracture fragment.
EXTENSION-TYPE FRACTURES
Extension-type fractures typically occur as the result of a fall onto an outstretched arm with a hyperextended elbow. The fracture line traverses the distal humerus from the proximal posterior to the distal anterior aspect. Displacement varies from none to marked displacement with fracture fragments separated by interposed soft tissue. Numerous classifications systems have been devised for extension-type supracondylar humerus fractures,10,24,40,41,68 but the classification system attributed to Gartland31 is the most commonly accepted system in use today. As described by Gartland, the classification system is simple, reproducible, helpful in guiding treatment, and provides information on prognosis and potential complications. A very similar fracture classification system was published in the German literature of the early 20th century by Felsenreich.26
TYPE I
Type I fractures are nondisplaced (Fig. 14-5). In many patients, the fracture line may not be visible on injury radiographs, but the posterior fat pad sign, palpable tenderness in the supracondylar region, and an appropriate mechanism of injury allows the physician to establish a correct diagnosis. The diagnosis is often confirmed when periosteal callus is seen on radiographs taken 3 weeks after the injury. If recognized and treated appropriately, type I fractures should never be associated with neurovascular injury or malunion.
TYPE II
In type II fractures, there is displacement or angulation at the fracture site, but a hinge of bone crossing the fracture keeps the fragments in continuity. The distal fragment is most often displaced posteriorly, and apex anterior angulation at the fracture site results in a hyperextension deformity (Fig. 14-6). Variations of type II fractures have also been described that involve medial impaction or rotation, which can result in cubitus varus if unrecognized (Fig. 14-7). Although there are reports of neurovascular injury associated with type II fractures, such injuries are rare.69
TYPE III
Type III fractures are completely displaced fractures in which there is no continuity between fracture fragments (Fig. 14-8). The distal fragment is displaced posteriorly and may be displaced medially or laterally as well. There is a much higher incidence of neurovascular complications with type III fractures, and soft tissue is usually interposed between fracture fragments. The brachialis muscle is most often interposed, but the median nerve, radial nerve, or brachial artery may also be entrapped.
DIAGNOSIS AND RADIOGRAPHIC EVALUATION
We define a supracondylar humerus fracture to be a transverse fracture crossing the entire width of the distal humeral metaphysis without involving the distal humeral physis. The primary challenge in establishing this diagnosis is to rule out other fractures of the distal humerus that do not meet these criteria. Fractures that can sometimes be confused with supracondylar humerus fractures include lateral condyle fractures, medial condyle fractures, and transphyseal fractures. Establishing the correct diagnosis is most difficult in patients younger than 4 years, whose ossific nuclei of the distal humerus are yet unossified.
The anterior and posterior fat pad signs are often helpful in diagnosing intra-articular elbow fractures such as supracondylar humerus fractures (see Chapter 15). Although it is very sensitive, the anterior fat pad sign is not very specific for intra-articular elbow fractures because the coronoid fossa of the humerus (occupied by the anterior fat pad) is much more shallow than the olecranon fossa (occupied by the posterior fat pad). Any insult that causes a joint effusion may cause the anterior fat pad to become visible on the lateral radiograph. A larger intra-articular fluid collection such as fracture hemarthrosis is necessary to displace the posterior fat pad enough for it to become visible on lateral radiographs; therefore, the posterior fat pad sign is much more reliable.
Additional radiographic measurements have been described to assess fracture alignment before and after reduction. The most commonly used measurement is Baumann’s angle, the intersection of a line drawn along the longitudinal axis of the humerus and a line drawn along the physis between capitellum and distal lateral humeral metaphysis. The normal angle varies in magnitude but averages approximately 72 degrees, and it should always be compared with the uninjured contralateral elbow (Fig. 14-9).88 A second useful radiographic reference line is the anterior humeral line (Fig. 14-10). If the capitellar ossific nucleus is displaced posterior to the anterior humeral line, fracture reduction should be considered. Fracture reduction should restore Baumann’s angle to a measurement similar to that of the opposite elbow on the anteroposterior view, and on the lateral view, it should restore the capitellum to a position in which the central third is bisected by the anterior humeral line.
For all patients with supracondylar humerus fractures, the entire extremity should be examined and radiographs obtained of all areas where associated injuries might be present. Approximately 15% of patients with supracondylar fractures have an associated fracture in the ipsilateral extremity.86 Supracondylar fracture associated with a Montaggia lesion has also been reported.3,65
TREATMENT
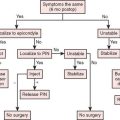
TYPE II FRACTURES
Despite an intact osseous hinge, type II fractures can vary significantly in displacement and injury severity, which determines treatment choice. For fractures in which the anterior humeral line does intersect the capitellum, reduction may not be necessary and immediate cast immobilization in 90 degrees of flexion is appropriate. Closed reduction should be seriously considered for moderately displaced fractures when the anterior humeral line passes anterior to the capitellum. In a cooperative reliable patient with minimal elbow swelling, gentle closed reduction may be performed under regional anesthesia or conscious sedation in the emergency department, and the fracture should be immobilized in an above-elbow cast with enough flexion to maintain fracture reduction (see Fig. 14-6). If any swelling is present, close attention to the neurovascular examination is critical when immobilizing the elbow in more than 100 degrees of flexion. Fluoroscopic obser-vation can be helpful in determining the minimum degree of flexion required to safely maintain fracture reduction.
Displaced or angulated type II fractures may be associated with neurovascular injury. Neurologic and vascular examinations, performed and documented meticulously, are essential. Swelling may make it impossible or unsafe to flex the elbow enough so that the fracture reduction can be maintained. In such situations, closed reduction and percutaneous pinning is indicated to maintain fracture reduction without compromising the neurovascular integrity of the limb. Moderately or severely angulated type II fractures may also be associated with medial column impaction, lateral column impaction, or rotation. If unrecognized, any of these three variations of a type II fracture can lead to malunion and angular deformity. Medial impaction, lateral impaction, and rotation all necessitate closed reduction, which is most dependably maintained with percutaneous pinning.19 After percutaneous pinning, a splint or bivalved cast is applied, and 5 to 10 days later, the bivalved cast is overwrapped or the splint removed and an above-elbow cast applied.
TYPE III FRACTURES
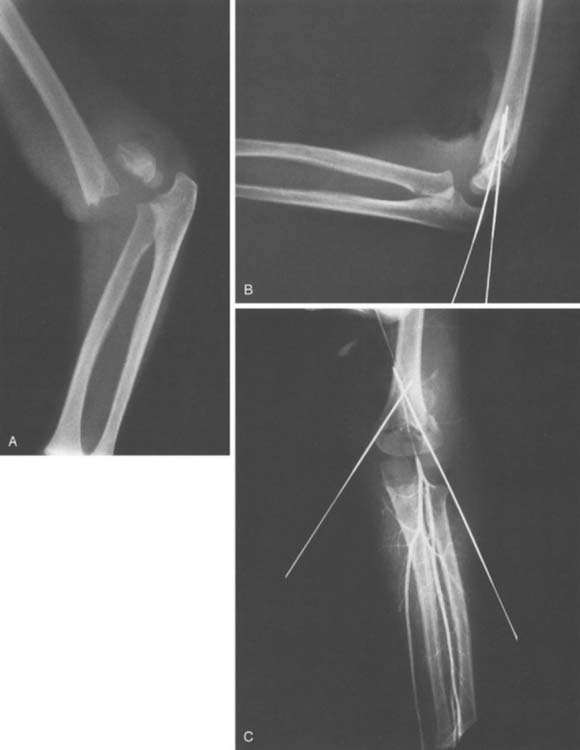
Completely displaced supracondylar humerus fractures are intrinsically unstable, typically cause severe swelling, and are frequently associated with neurovascular injury (Fig. 14-11). These factors make management of type III fractures challenging and anxiety provoking.
CLOSED REDUCTION
Type III extension-type fractures have an intact posterior periosteal hinge, which, in addition to the triceps tendon, provides some stability to the fracture when it is immobilized in flexion. Paradoxically, the completely displaced supracondylar fracture is just the fracture that requires elbow flexion greater than 100 degrees to maintain adequate fracture reduction, but it is also the fracture least able to tolerate flexion beyond 100 degrees because of swelling and risk of neurovascular compromise (Fig. 14-12).53 Because of the relatively high incidence of malunion and neurovascular compromise, immobilization in flexion has been replaced by closed or open reduction and pinning.47,59,64,87,89
PERCUTANEOUS PINNING
In 1988, Pirone et al64 published a series of 230 displaced supracondylar humerus fractures and analyzed the results of (1) closed reduction and percutaneous pinning, (2) open reduction, (3) skeletal traction, and (4) closed reduction with casting. Pirone and colleagues reported significantly better results in the group treated with closed reduction and percutaneous pinning as compared with the other three groups. Subsequent studies have confirmed these results, and closed reduction with percutaneous pinning has become the most used and most accepted treatment.12,27,35,36,87
In the emergency department, a meticulous neurovascular examination should be performed and properly documented including median, radial, ulnar, and anterior interosseous nerve function. Because it has only motor function, anterior interosseous nerve injury has been underdiagnosed in the past, but separate investigators have provided substantial evidence to suggest that the anterior interosseous nerve is the nerve most frequently injured in association with supracondylar fractures.17,18,21 Because of the severe nature of the injury, the amount of manipulation required for reduction, and the possible need to perform an open reduction, an attempt at closed reduction should not be made in the emergency department. However, severe displacement and deformity may result in a pulseless or dysvascular extremity. In this situation, under adequate analgesia in the emergency department, gently correcting the severe deformity followed by splinting in a relaxed position—usually approximately 30 degrees of elbow flexion—often restores the radial pulse and minimizes further tissue damage caused by severe fracture displacement. If the limb remains dysvascular, emergent transport to the operating room is indicated, where closed reduction restores perfusion to the upper extremity in the vast majority of patients.
A question that has generated considerable discussion in recent medical literature concerns whether a neurovascularly intact, displaced, type III fracture should be treated emergently in the middle of the night, or whether such a fracture can be effectively and safely treated the following morning? In a review of 198 patients with a displaced type III fracture and perfused limb, Mehlman et al55 compared urgent treatment with treatment provided the day following injury and reported no statistical difference between groups with regard to perioperative complications or the need to convert to open fracture reduction. Additional authors have published similar results, suggesting that compared with emergent treatment, delay until the following day does not increase the risk of perioperative complication or the need for open reduction, and does not compromise final outcome.37,43 One article did note an increased need to convert to open reduction when treatment was delayed.85 Our opinion is that the fracture is never easier to reduce than the moment after the fracture occurs; each subsequent hour adds to the swelling and difficulty of reduction. However, there does not seem to be any significant difference in clinical outcome between a neurovascularly intact extremity with a fracture that is reduced and pinned at 2:00 am compared with a fracture in which treatment is delayed until later that same morning.
Closed reduction and percutaneous pinning can be performed successfully using a variety of techniques with the patient positioned supine, lateral, or prone.28 We prefer to perform the reduction with the patient positioned supine using the following series of steps. After general anesthesia has been administered, the patient is positioned toward the edge of the operating table with the affected extremity carefully supported over the side. C-arm fluoroscopy is brought in from the foot of the table, parallel to the table, so the patient’s arm can rest on the C-arm.
Before prepping, with the arm less constrained by drapes, closed reduction is attempted. If the metaphyseal spike from the proximal fragment is tenting the skin and subcutaneous tissue, the brachialis is gently “milked” off of the fragment.5 With the arm in a relaxed position at approximately 20 to 30 degrees of elbow flexion, the medial-lateral displacement is corrected. When available, an assistant supports the forearm, and the operating surgeon places a thumb on posterior aspect of the medial and lateral columns of the distal humeral fragment. The final reduction maneuver involves the assistant’s applying gentle longitudinal traction while the operating surgeon uses each thumb to manipulate the distal fragment distally and anteriorly. Simultaneously, the assistant flexes the elbow to maintain the reduction (Fig. 14-13).58 When working alone, the operating surgeon can apply traction to the forearm and flexion to the elbow with one hand while applying distal and anterior pressure to the patient’s olecranon with the other hand (Fig. 14-14). If the initial displacement is posterior and medial, suggesting an intact medial periosteal hinge, the forearm is pronated. If the initial displacement is posterior and lateral, the forearm is supinated. Occasionally, pronation can cause displacement when in theory it should improve the reduction and vice versa with supination. The key is remaining flexible and gently trying several methods until the best and most stable reduction is obtained.
Controversy persists about the optimal pin configuration that maintains adequate fracture reduction and minimizes potential complications.32,34,48,74 Crossed pins provide the greatest biomechanical stability but have the potential to cause ulnar nerve injury90 (Fig. 14-15). Published reports suggest that the biomechanical stability sacrificed by using two or three lateral pins is not clinically significant and avoids iatrogenic ulnar nerve injury.15,82 If two lateral pins are used, great care must be taken to ensure that both pins cross through both fracture fragments with adequate spacing between the pins; otherwise, fracture reduction may be lost. To pin the medial column first, the elbow is externally rotated; to pin the lateral column, internal rotation is used. Sometimes the fracture is more stable in internal or in external rotation, and this determines which column is pinned first. Because internal rotation of the elbow can result in posterior displacement of the medial distal fragment causing varus angulation, when possible, we typically externally rotate the elbow and pin the medial column first.63
The operating surgeon palpates the medial epicondyle and uses a thumb to retract and protect the ulnar nerve posteriorly (see Fig. 14-13). A 0.062 Kirschner wire is then placed just anterior to the thumb on the medial epicondyle. The Kirschner wire is angled cephalad to travel within the medial column of bone and advanced until it just penetrates the opposite cortex. Using fluoroscopy, the position of the Kirschner wire is checked in anteroposterior and lateral planes. This first pin often substantially improves fracture stability, allowing extension past 90 degrees to image the elbow and facilitate placement of the second pin. The second pin is placed within the lateral column of bone, crossing the first pin well above the fracture site (see Fig. 14-15). The pins are left protruding through the skin, bent at a 90-degree angle, cut long, and a foam or gauze dressing placed beneath the ends to ensure that the pins will not become buried beneath the skin while in the postoperative dressing. Literature describing the use of bioabsorbable pins has reported an unacceptable level of implant failure and loss of reduction.11
Occasionally, the elbow is too swollen or the child too young to allow accurate palpation of the medial epicondyle. In such instances there are several options. A 1-cm incision may be made directly over the medial epicondyle. Soft tissues are spread with a small clamp down to the medial condyle, and a small retractor is used to hold the ulnar nerve and all soft tissues posterior to the pin. With the ulnar nerve retracted, the medial column pin can be placed safely. Alternatively, two or three lateral pins may be used. Zionts’ cadaver study90 demonstrated that, after crossed pins, the next strongest configuration used three lateral pins; two pins placed obliquely across the fracture from the distal lateral to the proximal medial aspect and a third through the capitellum directed up the humeral shaft.
OPEN REDUCTION
Inability to achieve closed reduction is usually due to soft tissue interposition. Most frequently, the brachialis muscle is interposed and can be “milked” off the distal metaphyseal spike by closed means. Occasionally, the brachial artery, median nerve, or radial nerve can become interposed between the fracture fragments. Inability to achieve an adequate closed reduction warrants open reduction. Fractures displaced posterolaterally are most likely to cause interposition of the median nerve or brachial artery and are approached anteromedially. Conversely, fractures displaced posteromedially are more likely to have interposition of the radial nerve and are approached anterolaterally. Several recent papers have reported excellent success using a small transverse incision in the elbow flexion crease.7,46,80 Through this limited approach, the offending interposed tissue can usually be easily extracted from the fracture site and anatomic reduction confirmed before percutaneous pinning proceeds. Past reluctance to perform open reduction of supracondylar fractures for fear of causing elbow stiffness has been shown to be unfounded: Several studies have demonstrated that open reduction is safe and effective and does not increase the risk of elbow stiffness.4,6,14,30,73
The majority of severely displaced supracondylar fractures without a radial pulse regain the pulse after fracture reduction. If after closed reduction, the radial pulse does not return and the limb is not perfused, immediate exploration of the brachial artery and open reduction is indicated. A more controversial situation is encountered when an adequate reduction is obtained, the limb remains pulseless, and the state of limb perfusion is unclear. In separate reports, Schoenecker and Shaw and their respective associates have formulated similar algorithms that are useful in this situation.71,72 After reduction and pinning, the vascular status of the limb is assessed. If the radial pulse is detectable by Doppler ultrasound and the hand is pink with brisk capillary refill, the elbow is immobilized, the case is completed, and the patient is carefully monitored overnight. If the radial pulse is not detectable by ultrasound, the brachial artery is explored at the fracture site. Using this algorithm, combining numbers from both studies, 10 patients did not have a detectable radial pulse by Doppler ultrasound and were explored immediately. All 10 arteries were found to be obstructed or transected, and in all extremities, blood flow was re-established by freeing the trapped or kinked vessel (five extremities) or by repairing the lesion with vein graft (five extremities). Using Doppler ultrasound to detect a radial pulse appears to be effective at detecting almost all clinically significant vascular injuries without arteriography and with minimal risk of exposing patients to unnecessary vascular exploration.
POSTOPERATIVE CARE
After the fracture is reduced and pinned and adequate perfusion of the limb confirmed, the upper extremity is immobilized. Pin stabilization permits immobilization in a position that optimizes perfusion and minimizes swelling. A simple posterior splint or bivalved cast may be used to immobilize the elbow in approximately 80 degrees of flexion. A fluffed 4-by-4-inch gauze may be placed in the antecubital fossa as great care is taken to prevent constriction from the dressing. A neurologic examination is performed immediately after the patient awakens from anesthesia, and median, radial, and ulnar nerve function is assessed.
Patients are admitted overnight for neurovascular monitoring. The elbow is elevated, and ice is applied through the dressing. Most patients are discharged from the hospital on the day after surgery and are seen back in follow-up 5 to 10 days after surgery. At that time, radiographs are taken and the limb is examined. If adequate reduction has been maintained and swelling has decreased, bivalved casts are overwrapped with fiberglass casting material or the posterior splint may be removed and a cast applied. Three weeks after the injury, the cast is removed and radiographs are repeated. If periosteal bone formation across the fracture is present, the pins are removed, immobilization is discontinued, and gentle active range-of-motion exercise is begun. Immobilization longer than 4 weeks increases the risk of permanent elbow stiffness. Vuckov84 reported immobilizing patients for as short as 2 weeks following supracondylar fractures with no untoward consequences.
TRACTION
Historically, traction has been used with acceptable results to obtain and maintain supracondylar fracture reduction until healing has progressed enough to permit cast immobilization.* More recently, improved results, decreased cost, and decreased time in the hospital after closed reduction and percutaneous pinning have resulted in complete abandonment of traction for supracondylar fracture treatment.29,64,67,81 Rarely, however, traction may be an appropriate treatment for type III supracondylar fractures. The most common indication for traction would be a displaced fracture that presents for treatment longer than 24 hours after injury and with severe swelling that precludes open or closed reduction (Fig. 14-16). Additional indications for traction include patients with a contraindication to general anesthesia or lack of access to adequate imaging or other equipment necessary for pinning.
Gross displacement is corrected at this time. The arm is suspended from an overhead frame with a sling under the forearm to control its position. Three to five pounds of traction is usually sufficient to reduce and stabilize the fracture. Too much weight elevates the shoulder and twists the thorax causing the child to shift position resulting in loss of control of the fracture fragment. Suspension of the forearm in this position permits rapid reduction of edema and good control of elbow flexion. Rotational deformity can be controlled by placing the arm in either a cephalad or a caudad position. If necessary, a lateral sling around the upper arm also may provide lateral traction to correct anterior displacement of the proximal fragment (Fig. 14-17). Serial radiographs must be taken, and producing adequate films may require some ingenuity on the part of the technician and direction on the part of the physician. The lateral projection usually is obtained without difficulty, but the axial view requires overcoming the obstruction of the overhead frame by some means. Fracture stability is assessed clinically and radiographically. When the fracture is minimally tender to palpation, swelling has subsided and early callus has developed, a well-molded above-elbow cast is applied.
COMPLICATIONS
Complications are discussed in detail in Chapter 15. The two broad categories of complications most often associated with supracondylar humerus fractures are malunion and neurovascular injury. Even the most skilled surgeons occasionally encounter complications, but adherence to the principles outlined here will help to minimize these unfortunate events.
1 Aebi H. Der Ellbogenwinkel, seine Beziehungen zu Geschlecht Körperbau und Hüfthreite. Acta Anat.. 1947;3:228.
2 Alburger P.D., Weidner P.L., Betz R.R. Supracondylar fractures of the humerus in children. J. Pediatr. Orthop.. 1992;12:16.
3 Arazi M., Oun T.C., Kapiciolum M.I. The Monteggia lesion and ipsilateral supracondylar humerus and distal radius fractures. J. Orthop. Trauma. 1999;13:60.
4 Archibald D.A., Roberts J.A., Smith M.G. Transarticular fixation for severely displaced supracondylar fractures in children. J. Bone Joint Surg.. 1991;73B:147.
5 Archibeck M.J., Scott S.M., Peters C.L. Brachialis muscle entrapment in displaced supracondylar humerus fractures: a technique of closed reduction and report of initial results. J. Pediatr. Orthop.. 1997;17:298.
6 Aronson D.C., van Vollenhoven E., Meeuwis J.D. K-wire fixation of supracondylar humeral fractures in children: results of open reduction via a ventral approach in comparison with closed treatment. Injury. 1993;24:179.
7 Ay S., Akinci M., Ercetin O. The anterior cubital approach for displaced pediatric supracondylar humeral fractures. Tech. Hand Up. Extrem. Surg.. 2006;10:235.
8 Beekman F., Sullivan J.E. Some observations on fractures of long bones in children. Am. J. Surg.. 1941;51:722-738.
9 Bender J., Busch C.A. Results of treatment of supracondylar fractures of the humerus in children with special reference to the cause and prevention of cubitus varus. Arch. Chir. Neerland.. 1978;30:29.
10 Bergenfeldt E. Uber Schaden an der Epiphysenfuge bei operativer Behandlung von Frakturen am unteren Humerusende. Acta Chir. Scand.. 1932;71:103.
11 Bostman O., Makela E.A., Sodergard J., Hirvensalo E., Tormala P., Rokkanen P. Absorbable polyglycolide pins in internal fixation of fractures in children. J. Pediatr. Orthop.. 1993;13:242-245.
12 Boyd D.W., Aronson D.D. Supracondylar fractures of the humerus: a prospective study of percutaneous pinning. J. Pediatr. Orthop.. 1992;12:789-794.
13 Buhl O., Hellberg S. Displaced supracondylar fractures of the humerus in children. Acta Orthop. Scand.. 1982;53:67.
14 Celiker O., Pestilci F.I., Tuzuner M. Supracondylar fractures of the humerus in children: analysis of the results in 142 patients. J. Orthop. Trauma. 1990;4:265-269.
15 Cheng J.C., Lam T.P., Shen W.Y. Closed reduction and percutaneous pinning for type III displaced supracondylar fractures of the humerus in children. J. Orthop. Trauma. 1995;9:511.
16 Cheng J.C., Shen W.Y. Limb fracture pattern in different pediatric age groups: a study of 3,350 children. J. Orthop. Trauma. 1993;7:15.
17 Churst A.P.C. An Anatomical and Surgical Study of Fractures of the Lower End of the Humerus. Philadelphia: Lea & Febiger, 1910.
18 Cramer K.E., Green N.E., Devito D.P. Incidence of anterior interosseous nerve palsy in supracondylar humerus fractures in children. J. Pediatr. Orthop.. 1993;13:502.
19 De Boeck H., De Smet P., Penders W., De Rydt D. Supracondylar elbow fractures with impaction of the medial condyle in children. J. Pediatr. Orthop.. 1995;15:444.
20 Dodge H.S. Displaced supracondylar fractures of the humerus in children—treatment by Dunlop’s traction. J. Bone Joint Surg.. 1972;54A:1408.
21 Dormans J.P., Squillante R., Sharf H. Acute neurovascular complications with supracondylar humerus fractures in children. J. Hand Surg.. 1995;20:1.
22 Dunlop J. Transcondylar fractures of the humerus in childhood. J. Bone Joint Surg.. 1939;21:59.
23 Edman P., Lohr G. Supracondylar fractures of the humerus treated with olecranon traction. Acta Chir. Scand.. 1963;126:505.
24 El-Ahwany M.D. Supracondylar fractures of the humerus in children with a note on the surgical correction of late cubitus varus. Injury. 1974;6:45.
25 Eliason E.L. Dressing for supracondylar fractures of the humerus. J. A. M. A.. 1924;82:1934.
26 Felsenreich F. Kindlich supracondylaire Fracturen und posttraumatisch Deformitäten des Ellenbogengelenkes. Arch. Orthop. Unfall-Chir.. 1931;29:555.
27 Flynn J.C., Zink W.P. Fractures and dislocations of the elbow. In: MacEwen G.D., Kasser J.R., Heinrich S.D., editors. Pediatric Fractures, A Practical Approach to Assessment and Treatment. Baltimore: Williams & Wilkins; 1993:87.
28 Fowler T.P., Marsh J.L. Reduction and pinning of pediatric supracondylar humerus fractures in the prone position. J. Orthop. Trauma.. 2006;20:277.
29 France J., Strong M. Deformity and function in supracondylar fractures of the humerus in children variously treated by closed reduction and splinting, traction, and percutaneous pinning. J. Pediatr. Orthop.. 1992;12:494.
30 Furrer M., Mark G., Ruedi T. Management of displaced supracondylar fractures of the humerus in children. Injury. 1991;22:259.
31 Gartland J.J. Management of supracondylar fractures of the humerus in children. Surg. Gynecol. Obstet.. 1959;109:145.
32 Gordon J.E., Patton C.M., Luhmann S.J., Bassett G.S., Schoenecker P.L. Fracture stability after pinning of displaced supracondylar distal humerus fractures in children. J. Pediatr. Orthop.. 2001;21:313.
33 Graham H.A. Supracondylar fractures of the elbow of children. Part II. Clin. Orthop.. 1967;54:93.
34 Green D.W., Widmann R.F., Frank J.S., Gardner M.J. Low incidence of ulnar nerve injury with crossed pin placement for pediatric supracondylar humerus fractures using a mini-open technique. J. Orthop. Trauma. 2005;19:158.
35 Green N.E. Fractures and dislocations about the elbow. In: Green N.E., Swiontkowski M.F., editors. Skeletal Trauma in Children. Philadelphia: W. B. Saunders Co.; 1994:223.
36 Grimard, G., Labelle, H., and Girard, P.: Treatment of displaced supracondylar fractures of the distal humerus in children: a prospective and controlled study. Poster Exhibit, American Orthop Assoc, Annual Meeting, 1992.
37 Gupta N., Kay R.M., Leitch K., Femino J.D., Tolo V.T., Skaggs D.L. Effect of surgical delay on perioperative complications and the need for open reduction in supracondylar humerus fractures in children. J. Pediatr. Orthop.. 2004;24:245.
38 Hagen R. Skin traction treatment of supracondylar fractures of the humerus in children. Acta Orthop. Scand.. 1964;35:138.
39 Hanlon C.R., Estes W.L. Fractures in childhood: a statistical analysis. Am. J. Surg.. 1954;87:312.
40 Henrikson B. Supracondylar fractures of the humerus in children. Acta Chir. Scand.. 1966;369(suppl.):1.
41 Holmberg L. Fractures in the distal end of the humerus in children. Acta Orthop. Scand.. 1945;92(suppl.):103.
42 Hoyer A. Treatment of supracondylar fractures of the humerus by skeletal traction in an abduction splint. J. Bone Joint Surg.. 1952;34A:623.
43 Iyengar S.R., Hoffinger S.A., Townsend D.R. Early versus delayed reduction and pinning of type III displaced supracondylar fractures of the humerus in children: a comparative study. J. Orthop. Trauma. 1999;13:51.
44 Jefferiss C.D. “Straight lateral traction” in selected supracondylar fractures of the humerus in children. Injury. 1977;8:213.
45 Khare G.N., Gautam V.K., Kochlar V.L., Anand C. Prevention of cubitus varus deformity in supracondylar fractures of the humerus. Injury. 1991;22:202.
46 Koudstaal M.J., De Ridder V.A., De Lange S., Ulrich C. Pediatric supracondylar humerus fractures: the anterior approach. J. Orthop. Trauma. 2002;16:409.
47 Kurer M.H.J., Regan M.W. Completely displaced supracondylar fracture of the humerus in children. A review of 1708 comparable cases. Clin. Orthop.. 1990;256:205.
48 Lee S.S., Mahar A.T., Miesen D., Newton P.O. Displaced pediatric supracondylar humerus fractures: biomechanical analysis of percutaneous pinning techniques. J. Pediatr. Orthop.. 2002;22:440.
49 Leitch K.K., Kay R.M., Femino J.D., Tolo V.T., Storer S.K., Skaggs D.L. Treatment of multidirectionally unstable supracondylar humeral fractures in children. A modified Gartland type—IV fracture. J. Bone Joint Surg.. 2006;88A:980.
50 Lipscomb P. Vascular and neural complications in supracondylar fractures of the humerus in children. J. Bone Joint Surg.. 1955;37A:487.
51 Lund-Kristensen J., Vibild O. Supracondylar fractures of the humerus in children. Acta Orthop. Scand.. 1976;47:375.
52 MacLemman A. Common fractures about the elbow in children. Surg. Gynecol. Obstet.. 1947;64:447.
53 Mapes R.C., Hennrikus W.L. The effect of elbow position on the radial pulse measured by Doppler ultrasonography after surgical treatment of supracondylar elbow fractures in children. J. Pediatr. Orthop.. 1998;18:441.
54 Maylahn D.J., Fahey J.J. Fractures of the elbow in children. Review of three hundred consecutive cases. J. A. M. A.. 1958;166:220.
55 Mehlman C.T., Strub W.M., Roy D.R., Wall E.J., Crawford A.H. The effect of surgical timing on the perioperative complications of supracondylar humeral fractures in children. J. Bone Joint Surg.. 2001;83A:323.
56 Micheli L.J., Santore R., Stanitski C.L. Epiphyseal fractures of the elbow in children. Am. Family Physician. 1980;22:107.
57 Micheli L.J., Skolnick D., Hall J.E. Supracondylar fractures in the humerus in children. Am. Family Physician. 1979;19:100.
58 Minkowitz B., Busch M.T. Supracondylar humerus fractures. Current trends and controversies. Orthop. Clin. North Am.. 1994;25:581-594.
59 Mohammed S., Rymaszewski L.A. Supracondylar fractures of the distal humerus in children. Injury. 1995;26:487.
60 Nassar, A.: Correction of varus deformity following supracondylar fracture of the humerus. Poster Presentation, American Orthopedic Assoc., Annual Meeting, 1992.
61 Ogden J. Skeletal Injury in the Child. Philadelphia: Lea & Febiger, 1982;240.
62 Ottolenghi C.E. Prophylactic due Syndrome de Volkmann dans des Humerus Supracondyliennes du Coude chez l’enfant. Rev. Chir. Orthop.. 1971;57:517.
63 Paradis G., Lavallee P., Gagnon N., Lemire L. Supracondylar fractures of the humerus in children. Technique and results of crossed percutaneous K-wire fixation. Clin. Orthop.. 1993;297:231-237.
64 Pirone A.M., Graham H.K., Krajbich J.I. Management of displaced extension-type supracondylar fractures of the humerus in children. J. Bone Joint Surg.. 1988;70A:641.
65 Powell R.S., Bowe J.A. Ipsilateral supracondylar humerus fracture and Monteggia lesion: a case report. J. Orthop. Trauma.. 2002;16:737.
66 Rang M. Children’s Fractures, 2nd ed. Philadelphia: J. B. Lippincott, 1983.
67 Rodriguez Merchan E.C. Supracondylar fractures of the humerus in children: treatment by overhead skeletal traction. Orthop. Rev.. 1992;21:475.
68 Rogers L.F., Malave S.Jr., White H., Tachdjian M.O. Plastic bowing, torus and greenstick supracondylar fractures of the humerus: radiographic clues to obscure fractures of the elbow in children. Radiology. 1978;128:145.
69 Sairyo K., Henmi T., Kanematsu Y., Nakano S., Kajikawa T. Radial nerve palsy associated with slightly angulated pediatric supracondylar humerus fracture. J. Orthop. Trauma. 1997;11:227-229.
70 Schickendanz H., Schramm H., Herrmann K., Jager S. Fractures and dislocations in the elbow in childhood. Am. Family Physician. 1973;13:311.
71 Schoenecker P.L., Delgado E., Rotman M., Sicard G.A., Capelli A.M. Pulseless arm in association with totally displaced supracondylar fracture. J. Orthop. Trauma. 1996;10:410.
72 Shaw B.A., Kasser J.R., Emans J.B., Rand F.F. Management of vascular injuries in displaced supracondylar humerus fractures without arteriography. J. Orthop. Trauma. 1990;4:25.
73 Sibly T.F., Briggs P.J., Gibson M.J. Supracondylar fractures of the humerus in childhood: range of movement following the posterior approach to open reduction. Injury. 1991;22:456.
74 Skaggs D.L., Hale J.M., Bassett J., Kaminsky C., Kay R.M., Tolo V.T. Operative treatment of supracondylar fractures of the humerus in children. The consequences of pin placement. J. Bone Joint Surg. 2001;83A:735.
75 Smith F.M. Children’s elbow injuries. Fractures and dislocations. Clin. Orthop. 1967;50:7.
76 Siris J.E. Supracondylar fractures of the humerus analyzed: 330 cases. Surg. Gynecol. Obstet. 1939;68:201.
77 Smith L. Deformity following supracondylar fractures. J. Bone Joint Surg. 1960;42A:235.
78 Staples O.S. Complication of traction treatment of supracondylar fractures of the humerus in children. J. Bone Joint Surg. 1959;41A:369.
79 Strait R.T., Siegel R.M., Shapiro R.A. Humeral fractures without obvious etiologies in children less than 3 years of age: when is it abuse? Pediatrics. 1995;96(4 pt 1):667-671.
80 Suh S.W., Oh C.W., Shingade V.U., Swapnil M.K., Park B.C., Lee S.H., Song H.R. Minimally invasive surgical techniques for irreducible supracondylar fractures of the humerus in children. Acta Orthop. 2005;76:862.
81 Sutton W.R., Green W.B., Georgopoulos G., Dameron T.B.Jr. Displaced supracondylar humeral fractures in children. A comparison of results and costs in patients treated by skeletal traction versus percutaneous pinning. Clin. Orthop. 1992;278:81.
82 Topping R.E., Blanco J.S., Davis T.J. Clinical evaluation of crossed-pin versus lateral-pin fixation in displaced supracondylar humerus fractures. J. Pediatr. Orthop. 1995;15:435.
83 Vahvanen V., Aalto K. Supracondylar fractures of the humerus in children. A long-term follow-up study of 107 cases. Acta Orthop. Scand. 1978;49:225.
84 Vuckov S., Kvesi A., Rebac Z., Cuculi D., Lovasi F., Bukvi N. Treatment of supracondylar humerus fractures in children: minimal possible duration of immobilization. Coll. Antropol. 2001;25:255.
85 Walmsley P.J., Kelly M.B., Robb J.E., Annan I.H., Porter D.E. Delay increases the need for open reduction of type-III supracondylar fractures of the humerus. J. Bone Joint Surg. 2006;88B:528.
86 Wilkins K.E. Residuals of elbow trauma in children. Orthop. Clin. North Am. 1990;21:291.
87 Wilkins K.E. Supracondylar fractures: what’s new? J. Pediatr. Orthop. 1997;6:110.
88 Williamson D.M., Coates C.J., Miller R.K., Cole W.G. Normal characteristics of the Baumann (humerocapitellar) angle: an aid in assessment of supracondylar fractures. J. Pediatr. Orthop. 1992;12:636.
89 Williamson D.M., Cole W.G. Treatment of selected extension supracondylar fractures of the humerus by manipulation and strapping in flexion. Injury. 1993;24:249.
90 Zionts L.E., McKellop H.A., Hathaway R. Torsional strength of pin configurations used to fix supracondylar fractures of the humerus in children. J. Bone Joint Surg. 1994;76A:253-256.