CHAPTER 9 Supine Approach to Hip Arthroscopy
Surgical technique
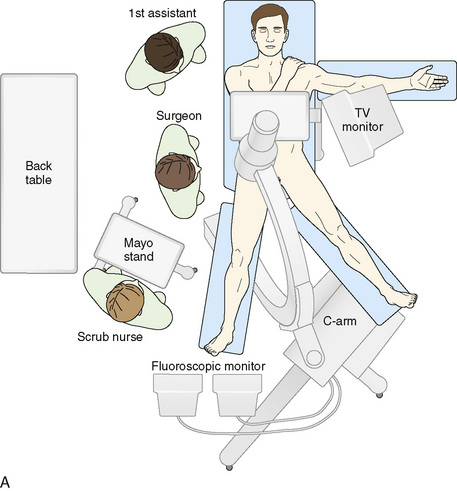
For the supine position technique, the patient is given a general anesthetic that provides muscle relaxation. Paralysis is recommended, because this allows less force to be used to distract the hip, with the purpose of reducing the risk of pudendal nerve injury from pressure between the pelvis and the perineal post of the traction table. The patient is placed supine on the fracture table with both feet secured to traction boots or mobile spars, depending on the specific table used. A well-padded perineal post is placed, and the patient is brought into position so that the post is firmly situated against the perineum and lateralized toward the operative hip, with care taken to protect the genitalia. The operative leg is positioned in 10 degrees of abduction, neutral flexion–extension, and neutral rotation. The nonoperative extremity is positioned in 45 degrees to 60 degrees of abduction, neutral flexion–extension, and neutral rotation to serve as countertraction for lateralization. Gentle traction is applied to the abducted nonoperative leg, which lateralizes the patient’s pelvis and results in the perineal post resting on the inner upper thigh of the operative extremity (Figure 9-1). This allows for the pressure of the perineal post to be diverted away from the perineum itself to minimize the risk of neuropraxia to the pudendal nerve as traction is applied to the operative leg. In addition—and quite important—this also helps to generate the appropriate vector of force for a uniform distraction both laterally and distally (Figure 9-2). Traction to the operative leg straight distally would be met with unnecessary resistance to overcome the inferior transverse acetabular ligament. Lateralization of the hip with the use of the post helps to pull the femoral head laterally and distally from the socket without having to overcome the ligament as a barrier to distal translation.
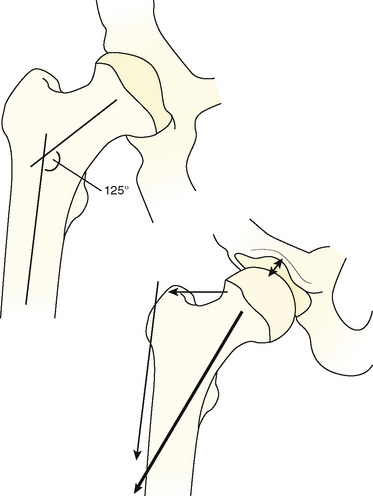
From Byrd JWT. The supine position. In: Byrd JWT ed. Operative hip arthroscopy. New York; Thieme Publishers; 1998: Figure 9.2, page 125.
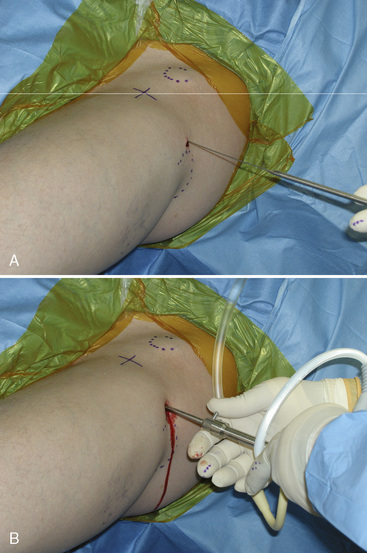
After the patient has been positioned appropriately and slight traction has been applied to the nonoperative extremity, traction on the operative limb can be applied. This should be incremental, and it can be monitored with serial images from an image intensifier (i.e., C-arm). A tensiometer can also be used; however, the senior author has not found this to be useful. Jim Glick has shown that the risk of nerve injury as assessed by somatosensory evoked potentials is associated with the duration of traction rather than the amount of traction (Glick, personal communication). Thus, the absolute amount of traction is apparently not important. Some surgeons use the tensiometer to evaluate any changes in tension. We use the fluoroscopic image intensifier routinely; we bring the base of the machine in from the foot of the table in between the patient’s abducted legs, and we center the column over the operative hip (see Figure 9-1). Incremental traction is then applied until approximately 8 mm to 10 mm of femoroacetabular joint distraction is generated. The area of the proposed anterolateral portal is identified and marked; the area around this proposed portal site is prepared with Betadine solution; and a spinal needle is then used to enter the hip joint to verify the correct path of the anterolateral portal, to ease joint access, and to perform an air arthrogram to release negative intra-articular pressure. In a cadaver study, Dienst and colleagues demonstrated that positioning the hip in 20 degrees of flexion and performing an air arthrogram (i.e., disrupting the vacuum seal and distending the hip joint) reduced the amount of traction required to distract the joint for safe entry, thereby further reducing the risk of neuropraxia. The needle is placed from the intended anterolateral portal with the guidance of the fluoroscopic image intensifier (Figure 9-3). The needle needs to enter the central compartment to effectively reduce the intra-articular pressure. We have shown that placing the needle onto the femoral neck does not release the negative intra-articular pressure within the joint. Care is taken to keep the spinal needle close to the femoral head (to reduce the risk of injury to the labrum) and to keep the longer part of the tip away from the femoral head. When the suction seal is broken, the joint will open more widely. The needle position relative to the femoral head is evaluated before and after the seal is broken. If the needle moves proximally when the negative pressure is released, the labrum may have been violated by the needle. If the needle moves with the femoral head, the labrum has likely not been injured.
Central compartment
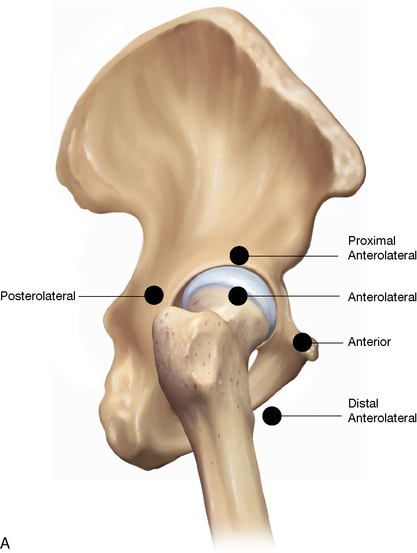
The anterolateral portal (Figure 9-4) is started approximately 1 cm anterior to the superior aspect of the anterior border of the greater trochanter. The needle is placed nearly parallel to the floor and angled toward the sourcil of the acetabulum, between the labrum and the distracted femoral head (see Figure 9-3, B). Avoiding the labrum is the key aspect of this part of the procedure. This can be optimized by careful visualization with the C-arm and by trying to keep the needle closer to the femoral head. The apex of the needle is kept away from the femoral head to help avoid injury to the femoral head articular cartilage. If the needle is near the acetabulum and does not pass easily after the puncture of the capsule, then it is likely within the substance of the labrum; it must be withdrawn and carefully redirected. After the needle is placed appropriately, the obturator of the spinal needle may be removed to allow for the inflow of air. This air arthrogram will verify appropriate placement, reduce the amount of traction required, and further increase the joint space produced by the traction with the same amount of force (see Figure 9-3, B and C). When this procedure is completed, the spinal needle is removed, the traction is released, and the patient’s hip can then be prepped and draped from the pelvis to the knee.
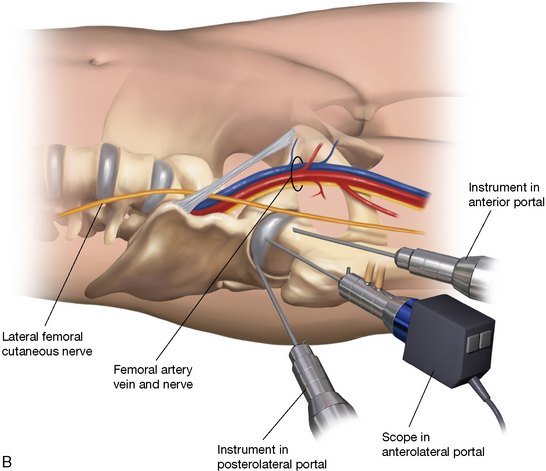
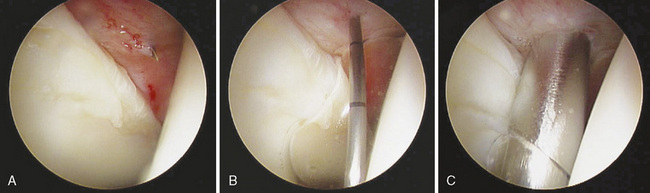
When the patient has been draped, the traction can be reapplied and verified with the C-arm, and then the anterolateral portal is created. Once again, place the spinal needle into the hip joint by following the same format and path. After the needle has been verified with the arthroscope to be intra-articular within the capsule and not damaging the labrum or articular cartilage, a guidewire is placed through the spinal needle. The spinal needle is then removed, leaving the guidewire in the place. A scalpel with a No. 11 blade is used to make a 5-mm incision over the guidewire. The cannulated trocar system is then used to place the arthroscope. Slowly and with controlled pressure and twisting to pierce the hip capsule, the blunt cannulated trocar is then introduced over the guidewire; this will provide moderate resistance (Figure 9-5). Care must be taken to not advance the guidewire too far or to bend the guidewire when inserting the cannula, because this may fracture the guidewire. Sharp trochars are discouraged, because this may cause iatrogenic injury to the joint. Trochar and sheath entry into the joint can be visualized with the C-arm. After getting inside of the joint, the blunt obturator and guidewire are removed, and an arthroscope with a 70-degree lens is introduced. When a clear picture is obtained, a cursory visualization of the hip joint may be conducted. The anterior portal is usually made right after the anterolateral portal is achieved. The anterior portal is made with the guidance of arthroscopic visualization to reduce the risk of iatrogenic injury to the acetabular or labral cartilage. Some surgeons insufflate fluid into the joint after the spinal needle for the anterolateral portal is introduced to allow for joint distention. The senior author does not do this and in fact does not run fluid into the joint until the spinal needle for the second portal has been established. There is often blood in the joint after distraction and capsular injury from the entry into the joint. With no outflow of fluid, insufflation of the joint will result in cloudy visualization or obstructed visualization through the bloody fluid. Thus, the second portal is created while the joint is dry.
Next, the second portal is created; this is an anterior working and visualization portal. There are several described locations for the introduction of the anterior portal. One of the more common places for the anterior portal is at the intersection of a line drawn caudally from the anterior superior iliac spine and a perpendicular line drawn from the tip of the greater trochanter (see Figures 9-4 and 9-5). This portal carries the risk of injury to the lateral femoral cutaneous nerve (because of this superficial nerve’s intimate proximity to the portal) and to the rectus femoris. Our current preferred location for the anterior portal was described by Philippon (personal communication, 2007) and can be considered a mid-anterior portal. This portal is located 6 cm to 8 cm distal and anteromedial to the anterolateral portal at a 45-degree angle (Figure 9-6). This portal minimizes the risk of injury to the lateral femoral cutaneous nerve and the rectus femoris. In general, the different anterior portals are very near the arborization of the lateral femoral cutaneous nerve. Therefore, care must be taken when making this portal so that the skin incision remains superficial, with the No. 11 scalpel blade being used to reduce the risk of injury to the lateral femoral cutaneous nerve. The method for creating this portal is identical to that of creating the anterolateral; however, now the spinal needle may be visualized with the arthroscope in the anterolateral portal when the needle enters the joint, and care must be taken to pierce the capsule while avoiding injury to the labrum and the chondral surface (Figure 9-7). The spinal needle, the guidewire, and the subsequent trochar with cannula sheath all can be visualized with the arthroscope during entry to help avoid injury to the labrum and the articular cartilage. With this portal established, the arthroscope may be exchanged in this anterior portal to visualize the anterolateral portal placement to verify that no iatrogenic damage has occurred to the labrum. If the anterolateral portal is disrupting the labrum, it can now be redirected with the help of visualization from the anterior portal.
Byrd J.W.T. Hip arthroscopy utilizing the supine position. Arthroscopy. 1994;10:275-280.
Byrd J.W.T. The supine position. In: Byrd J.W.T., editor. Operative hip arthroscopy. New York: Thieme Publishers; 1998:123-138.
Byrd J.W.T., Pappas J.N., Pedley M.J. Hip arthroscopy: an anatomic study of portal placement and relationship to extra-articular structures. Arthroscopy. 1995;11:418-423.
Dienst M., Seil R., Gödde S., Brang M., Becker K., Georg T., Kohn D. Effects of traction, distention, and joint position on distraction of the hip joint: an experimental study in cadavers. Arthroscopy. 2002;18(8):865-871.