Chapter 64 Subaxial Cervical Spine Injuries
Cervical fractures are found in approximately 3% of all trauma patients.1 The subaxial spine accounts for the majority of cervical injuries, making up approximately 65% of fractures and more than 75% of all dislocations.2 Approximately 150,000 cervical spine injuries occur annually in North America. In the same region, there are 11,000 new spinal cord injuries (1 per 25,000 people) annually.3 Trauma in the subaxial cervical spine accounts for almost half of all cervical spine injuries and the largest proportion of new traumatic spinal cord injuries.
Anatomy
Various authors have modeled the cervical spine as either a two-column4,5 or three-column system.6,7 Although both systems have merits, the two-column system probably provides the best understanding of the common injury patterns seen in the lower cervical region. The two-column spine consists of an anterior column and a posterior column. The anterior column contains the anterior longitudinal ligament, intervertebral disc, vertebral body, and posterior longitudinal ligament. The posterior column consists of the posterior bony elements, facet capsules, interspinous and supraspinous ligaments, and ligamentum flavum. The most important stabilizer of the anterior column is the anulus fibrosus, whereas the facet joints are the most important stabilizers of the posterior column.5
The ligamentous structures provide a check to hypermobility during normal motion. For example, the anterior longitudinal ligament and ventral anulus become taut during extension, whereas the posterior column ligamentous structures act as a tension band during flexion. Compressive loads are resisted by the vertebral bodies, intervertebral discs, and facet joints. Pure tensile loads are resisted by the anulus, interspinous ligament, ligamentum flavum, and facet capsules. Flexion is resisted by the interspinous ligaments, facet capsules and facet joints, anterior longitudinal ligament, and posterior anulus. Extension is also resisted by the bony block of the facet joints. Maximal sagittal plane translation occurring under physiologic loads is 2 to 2.7 mm.5 Lower cervical spine injuries can be understood as a failure of the structures designed to resist the forces and moments occurring at the time of the injury. By observing the pattern of bony and ligamentous disruption on imaging studies, the treating physician may generally deduce the force vectors that acted to create the injury pattern and also begin to gain an understanding of the “personality” of the injury, and thus the tendency for displacement under physiologic loads.
Injury Classification
The simplest method of discussing injuries to the cervical spine is to use radiographic descriptions of the injury. Hence, terms such as compression fracture, burst fracture, teardrop fracture, or facet dislocation remain in common usage, although these descriptive terms provide only a broad overview of the injury and do not provide information on injury severity, neurologic status, or treatment options. Mechanistic classifications are useful in promoting an understanding of injury pathomechanics and also assist the surgeon in designing a rational treatment approach, although biomechanical validation of the presumed injury mechanisms is generally lacking. Despite this limitation, these classification schemes are useful in clinical practice and remain the preferred scheme at most trauma centers managing large volumes of cervical trauma.
Although many classification schemes have been proposed, this chapter reviews several schemes that have strong historical significance or practical utility, or are recent additions to the literature, including those proposed by Whitley and Forsyth (1960),8 Allen et al. (1982),9 Harris et al. (1986),10 Anderson et al. (2007),11 and, finally, Vaccaro et al. (2007).3
Whitley and Forsyth8 described a mechanistic classification of cervical spine injuries in 1960 based on a review of 159 patients with cervical fractures. In their scheme, fractures were divided into flexion injuries, extension injuries, combined flexion-extension injuries, burst-type injuries, and direct trauma. The authors further divided flexion and extension injuries into those occurring with and without compression. This classification system retains historical importance for promoting a mechanistic thinking about cervical spine injuries.
White and Panjabi5 devised an early checklist for instability after cervical trauma. They hypothesized that a similar injury mechanism might produce different injury patterns because of the complex multidirectional forces, moments, and positions of the affected joints at the time of trauma. They devised a point-based system for assessing stability in lower cervical spine injury, summarized in Table 64-1. To use their system, radiographic criteria, physical examination, and a stretch test are required. A score of 5 or more points in this system is said to predict spinal instability.12
TABLE 64-1 Diagnosis of Clinical Instability in the Middle and Lower Cervical Spine
| Element | Point |
|---|---|
| Anterior elements destroyed or unable to function | 2 |
| Posterior elements destroyed or unable to function | 2 |
| Positive stretch test | 2 |
| Radiographic criteria | |
| Flexion-extension radiographs | |
| Sagittal plane translation > 3.5 mm | 2 |
| Sagittal plane rotation > 20° | 2 |
| Resting radiographs | |
| Sagittal plane displacement > 3.5 mm | 2 |
| Relative sagittal plane angulation > 11° | 2 |
| Developmentally narrow spinal canal | 1 |
| Abnormal disc narrowing | 1 |
| Spinal cord damage | 2 |
| Nerve root damage | 1 |
| Dangerous loading anticipated | 1 |
A total of five or more points indicates clinical instability.
The stretch test described by White and Panjabi is performed by securing the patient’s head in halter or tong traction with a roller beneath the head to reduce friction. Initial lateral radiographs of the cervical spine with 10 pounds of traction are carefully analyzed to rule out a disruption of the occipitocervical junction. Serial weight is sequentially added in 10-pound increments, performing neurologic testing with each addition of weight. The end point of the test is reached when “instability” is noted on radiographs or when there is a change in neurologic examination, or when the weight limit (65 pounds or one-third body weight) is reached. Instability on the stretch test is defined as distraction of a vertebral interspace by 1.7 mm or greater or a change in segmental alignment of 7.5 degrees or greater compared with the baseline radiographs.12 Although advocated by several authors, this type of test has not become a standard method for analyzing stability in most trauma centers because of its cumbersome nature and concerns regarding iatrogenic neurologic injury.
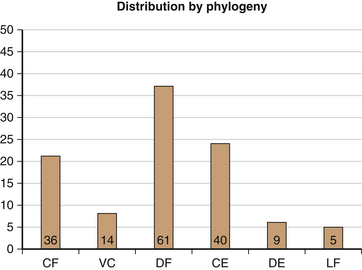
In 1982, Allen et al.9 published a mechanistic classification system that has been widely used in recent years. They based their scheme on the clinical review of 165 patients with indirect lower cervical spine trauma. In this system, subaxial cervical injuries were divided into “phylogenies” based on a common proposed injury mechanism, with an orderly progression of severity ranging from mild to severe. They included six injury phylogenies—compressive flexion, vertical compression, distractive flexion, compressive extension, distractive extension, and lateral flexion (Fig. 64-1). The terms used for each category describe the attitude of the cervical spine at the time of injury and the dominant force vector. The authors acknowledged the presence of minor force vectors that may cause separate or combined injuries. “Rotation” in this system was described as localizing an injury asymmetrically to one side rather than acting as an independent force vector. In general, the risk and severity of neurologic injury were noted to increase with increasing severity stages (Box 64-1).
BOX 64-1 Lower Cervical Spine Trauma Phylogeny Classification System*
1 Compressive Flexion (CF)
CFS1: rounded shape to the anterior superior vertebral body without any posterior ligamentous disruption
CFS2: “beaked” appearance of the anterior vertebral body with loss of anterior height due to compression failure
CFS3: an oblique fracture line traversing from the anterosuperior vertebral body to the inferior end plate
CFS4: up to 3 mm of posterior translation of the posterior vertebral body into the neural canal
CFS5: >3 mm displacement of the posterior aspect of the vertebral body into the neural canal
3 Distractive Flexion (DF)
DFS1: forward subluxation of the upper facet in the motion segment with widening of the space between the spinous processes
DFS2: unilateral facet dislocation demonstrating up to 25% forward subluxation of the vertebral body in the motion segment
DFS3: bilateral facet dislocation with approximately 50% anterior subluxation of the upper vertebra in the motion segment
DFS4: gross anterior displacement of the upper vertebra on the lower vertebra in the motion segment, creating the “floating vertebra”
4 Compressive Extension (CE)
CES1: unilateral vertebral arch fracture (pedicle, facet, and/or lamina) with or without rotational displacement of the vertebral body
CES2: bilateral laminar fractures, often at multiple contiguous levels but without evidence of other soft tissue failure
CES3: bilateral disruption of the articular pillars (pedicle, facet, and/or lamina) without displacement
CES4: partial forward subluxation of the fractured vertebra on the vertebra below
Adapted from Allen BL, Ferguson RL, Lehmann TR, et al: A mechanistic classification of closed indirect fractures and dislocations of the lower cervical spine. Spine (Phila Pa 1976) 7:1–27, 1982.
In 1986, Harris et al.10 proposed a similar classification system that placed injuries into groups related to a predominant causative force vector or combination of force vectors (Box 64-2). Unlike the Allen scheme, Harris et al. included the rotational vectors combined with flexion or extension but did not emphasize the role of distractive forces.
BOX 64-2 Mechanism of Cervical Spine Injuries
From Harris J, Edeiken-Monroe B, Kopaniky D: A practical classification of acute cervical spine injuries. Orthop Clin North Am 17:15–30, 1986.
In 2007, Anderson et al.11 presented the Cervical Spine Injury Severity Score (CSISS), a scheme allowing the observer to grade the degree of osteoligamentous disruption of the injury based on a four-column concept of the cervical spine modified from the work of Louis. The concept is to correlate increasing amounts of osseous separation or ligamentous disruption with a higher degree of instability using an analogue scale, with the goal of identifying patients who would benefit from surgical stabilization. The authors found excellent intraobserver and interobserver reliability when applying their scheme to a cervical trauma population, perhaps owing to the critical analysis of each of the four columns of the cervical spine. When analyzed, the CSISS was noted to perform well for all fracture types and for a spectrum of injuries from relatively minor to grossly unstable.11 Patients with scores greater than 7 points were generally subjected to surgical stabilization, suggesting the system produced consensus regarding the need for operative stabilization.
Vaccaro et al.3 presented a point-based scheme for evaluating subaxial cervical injuries in 2007. The authors reviewed the positive elements of prior classification systems and used the expertise of an experienced group of clinicians in the Spine Trauma Study Group (STSG) to devise a working system known as the Subaxial Injury Classification (SLIC; Table 64-2). The SLIC system applies a severity ranking in three specific areas: (1) a morphologic description of the bony fracture pattern, (2) a rating of the discoligamentous complex, and (3) a rating of the patient’s neurologic status.3 By applying points in each area, the authors were able to produce a severity score that was used to separate treatment into surgical and nonsurgical categories.
TABLE 64-2 Subaxial Cervical Spine Injury Classification System
| Characteristic | Points |
|---|---|
| Morphology | |
| No abnormality | 0 |
| Compression | 1 |
| Burst | 1–2 |
| Distraction (e.g., facet perch, hyperextension) | 3 |
| Rotation/translation (e.g., facet dislocation, unstable teardrop or advanced-stage flexion compression injury) | 4 |
| Discoligamentous Complex | |
| Intact | 0 |
| Indeterminate (e.g., isolated interspinous widening, MRI signal change only) | 1 |
| Disrupted (e.g., widening of disc space, facet perch or dislocation) | 2 |
| Neurologic Status | |
| Intact | 0 |
| Root injury | 1 |
| Complete cord injury | 2 |
| Incomplete cord injury | 3 |
| Continuous cord compression in setting of neurodeficit (neuromodifier) | 1 |
Adapted from Vaccaro A, Hulbert J, Patel P, et al: The subaxial cervical spine injury classification system: a novel approach to recognize the importance of morphology, neurology, and integrity of the disco-ligamentous complex. Spine (Phila Pa 1976) 32:2365–2374, 2007.
Spinal Stability
Spinal stability is one of the most fundamental issues affecting treatment decisions for cervical trauma, yet an absolute method to define stability remains elusive. Many attempts have been made to define instability by various researchers. Spinal stability was defined by White and Panjabi13 as “the ability of the spine under physiologic loads to limit patterns of displacement so as not to damage or irritate the spinal cord or nerve roots and, in addition, to prevent incapacitating deformity or pain due to structural changes.” Although this definition is logical, it is notoriously difficult to apply in clinical practice.13 In contrast, Anderson et al.11 used a continuous scale for grading stability of the bony and ligamentous structures in the CSISS. This approach seems to have good reliability, but the exact point at which an injury becomes unstable still remains imprecise. Allen et al.9 defined instability as “greater than normal range of motion within a motion segment” and viewed each injury pattern as a spectrum. However, clinical judgment and experience on the part of the treating physician remain critical in defining stability.9
Holdsworth4 and others14,15 have emphasized the importance of the posterior ligamentous complex in conferring stability to the spine. In their description, the disruption of the posterior ligamentous complex is the primary determinant of instability. Instability comprises a spectrum, with rare cases of clinically significant instability not being recognizable on initial imaging. Herkowitz and Rothman16 coined the term subacute instability to describe patients with negative initial radiographs and neurologic examinations who were subsequently noted to have unstable cervical injuries on follow-up radiographs. This situation was thought to be due to initial muscle spasm masking the instability. Because of the risk of a missed injury, early removal of cervical immobilization was discouraged. Instead, it was recommended that a patient with a suggestive trauma mechanism and neck pain remain in a secure cervical collar immobilization until the muscle spasm has resolved, at which time clinical and flexion and extension radiographs can be obtained.
Neurologic Classification
Neurologic classification is critical for the spinal cord-injured population. The neurologic examination should be repeated frequently in the early course after a spinal cord injury because the examination can change and affect the management of the patient. Accurate neurologic classification is crucial when performing research in the spinal cord-injured population and should be done in a careful and reproducible manner.17 Many authors have noted a poor correlation between the severity of the spinal column injury and the severity of the neurologic injury. Total quadriplegia may occur without an apparent spinal column disruption; conversely, a widely displaced cervical dislocation may sometimes occur in a neurologically intact patient.
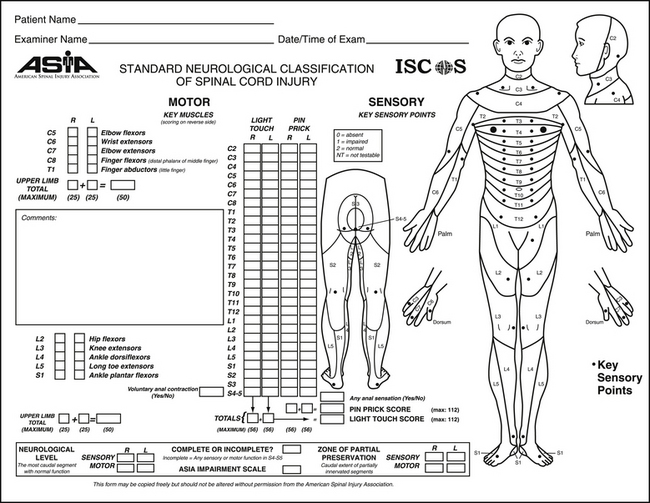
The first edition of the International Standards for Neurological and Functional Classification of Spinal Cord Injury was published in 1982 by the American Spinal Injury Association (ASIA). Since then there have been three revisions, the most recent in 1996.18 The ASIA clinical format for recording a neurologic examination is shown in Figure 64-2. Sensory and motor testing are performed separately for each side of the body over 28 standardized dermatomes and 10 standardized myotomes. Sensation is tested for pinprick and light touch modalities. The neurologic level is recorded as the most distal level with normal function. In cases where there is a discrepancy between sides of the body or between sensory and motor testing, each neurologic category should be individually recorded. Because many key muscles have neurologic input from more than one nerve root level, mild weakness may be present when a portion of the normal nerve supply is absent because of a neurologic injury. The motor level is defined as the most distal muscle group with a power score of 3 out of 5 or greater strength given normal motor testing above. It is important to test the most distal sacral levels (S4 and S5) for sensation as well as for anal sphincter motor function to define injury prognosis. Functional impairment can be categorized using the ASIA Impairment Scale (Box 64-3), which is a modification of the original Frankel grading system.
BOX 64-3 American Spinal Injury Association Impairment Scale
A. Complete. No sensory or motor function is preserved in the sacral segments S4-5.
B. Incomplete. Sensory but not motor function is preserved below the neurologic level and extends through the sacral segments S4-5.
C. Incomplete. Motor function is preserved below the neurologic level, and more than half of key muscles below the neurologic level have a muscle grade of less than 3.
D. Incomplete. Motor function is preserved below the neurologic level, and at least half of the key muscles below the neurologic level have a muscle grade of greater than or equal to 3.
Diagnosis
The spinal literature supports not obtaining radiographs in asymptomatic patients who are awake, alert, nonintoxicated, and without distracting injuries who exhibit no neck tenderness or pain with range of motion after trauma.19 All other patients sustaining significant neck trauma should be evaluated with plain radiographs at a minimum. Although plain radiographs continue to be the most common modality for initial imaging of the cervical spine after trauma, Woodring et al. and others have reported the limitations of plain radiography in detecting certain types of cervical fractures, particularly fractures of the posterior elements.20–22 In one study, plain radiographs missed 23% of cervical fractures, including some that created the potential for instability. CT scanning has become a common initial imaging modality for patients after high-energy trauma in many trauma centers and is particularly indicated in cases of neurologic deficits or altered mental status.23 In addition to a high sensitivity for fracture detection, CT with reformatted images provides an excellent assessment of sagittal and rotational alignment of the spine and has proved to be a beneficial tool for preoperative planning of surgical cases.24
MRI has been used increasingly in the setting of cervical trauma, particularly in patients with a neurologic deficit. MRI can localize and quantify cord compression, hemorrhage, or signal change within the cord and can detect the presence of nonbony lesions such as epidural hematoma or disc herniation. MRI may also demonstrate disruptions of the cervical ligaments, which are not detectable by plain radiographs or CT.25 MR angiography can be used to define patency or injury to the vertebral arteries in the setting of high-energy trauma.26,27
Lateral flexion-extension radiographs are rarely indicated in the acute trauma setting because pain and muscle spasm may prevent an accurate identification of injuries.16 Dynamic films, however, are useful when performed in a delayed fashion (10 to 14 days after the injury) to rule out subtle instability before the discontinuation of immobilization. Patients subjected to this technique should have voluntary motion of the neck and an absence of significant muscle spasm for accurate detection of a subtle injury.
Treatment
Simple Compression Fractures
Simple compression fractures (Fig. 64-3) may involve the upper or lower vertebral end plates (or both) and are caused by forceful flexion or axial loading of the neck. This type of injury is common in patients with osteopenia but may also be seen after higher-energy trauma in patients with normal bone. By definition, these injuries have no significant ligament disruption, facet diastasis, or subluxation. Our preferred treatment involves immobilization in a semirigid cervical orthosis for 6 to 8 weeks followed by flexion-extension lateral radiographs to rule out a more serious instability pattern. If no abnormal motion is seen on flexion-extension lateral radiographs, the patient can be weaned from the collar and begin a postinjury rehabilitation program.28
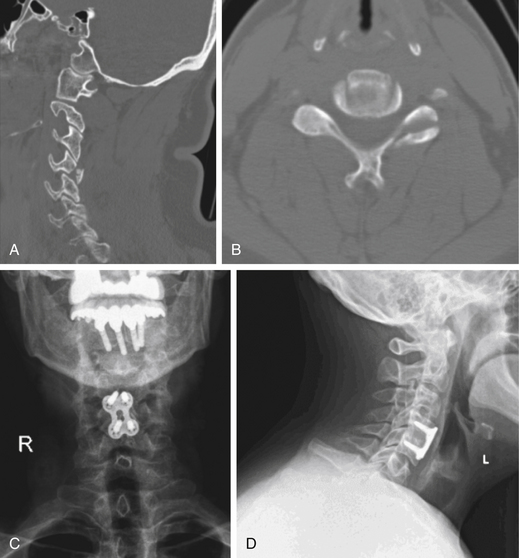
Severe Compression/Burst Fractures/Axial Compression Injuries
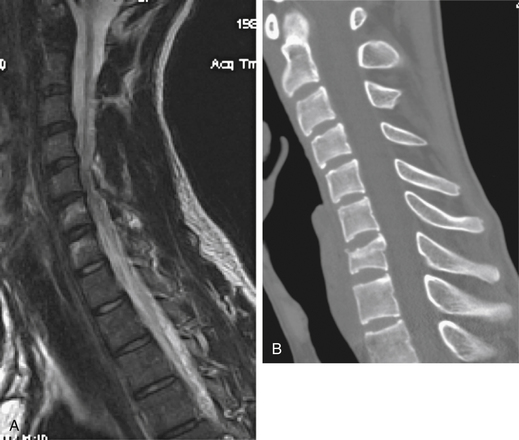
These injuries are usually seen with high-energy trauma when the cervical spine is subjected to axial loading with various amounts of flexion. The energy of these injuries is sufficient to produce a substantial crush injury to the discoligamentous complex and may, in the case of burst fractures, lead to retropulsion of material into the spinal canal. Unlike the teardrop/compressive flexion injury pattern (see later), the posterior osteoligamentous complex remains competent. Therefore, diastasis of the facets or widening between the spinous processes generally is not present (Fig. 64-4).
In cases where there is substantial compression of the spinal cord with an incomplete neurologic deficit, operative intervention is generally recommended. The most common operative approach is anterior, performing a corpectomy of the fractured vertebral body with decompression of the spinal cord and reconstruction using a structural graft and ventral cervical plate.29 Treatment for patients with complete neurologic deficits or significant kyphosis without a neurologic deficit is more controversial. Many authors have recommended surgery to facilitate early rehabilitation of patients with complete spinal cord injuries or to promote root recovery at levels below the injury. Anderson and Bohlman found an average recovery of one to two root levels below the level of a complete cord injury even with delayed decompression.30 Substantial posttraumatic cervical kyphosis may lead to problems with chronic neck pain or even delayed neurologic symptoms, and, therefore, such patients are candidates for anatomic reconstruction of the fractured level.
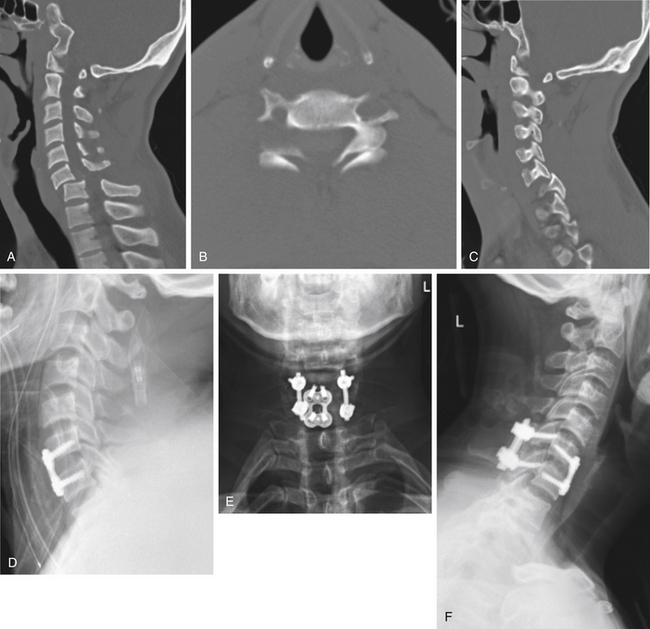
Cervical Facet Dislocations/Distractive Flexion Injuries
Cervical facet dislocations result from hyperflexion and posterior distraction of the cervical spine, with or without rotational forces. These injuries are most commonly seen after high-energy trauma such as motor vehicle collisions, diving accidents, or severe falls.31 Unilateral facet dislocations generally exhibit up to 25% anterior subluxation of the cranial vertebral body over the caudal level. In contrast, bilateral facet dislocations generally demonstrate 50% or more ventral displacement of the upper vertebral body over the lower (Fig. 64-5). Fracture of the inferior or superior articular processes or comminution of the lateral mass region is commonly seen with facet dislocations, producing a continuum of injury. MRI and surgical exploration commonly reveal massive disruption of the posterior musculature, interspinous ligament, supraspinous ligament, facet capsule, and ligamentum flavum, making this injury pattern intrinsically unstable. Neurologic injuries are commonly seen in patients sustaining bilateral facet dislocations, but are much less common after unilateral facet dislocations. Patients with unilateral facet dislocations may demonstrate evidence of an isolated nerve root injury.
The initial assessment and management of cervical facet dislocations has raised controversy in the literature. Some authors have recommended rapid realignment of the spine through closed traction, followed by surgical stabilization. Proponents of this approach argue that in the awake, alert, and examinable patient, the application of progressive traction to achieve a rapid reduction of the dislocation will achieve the quickest decompression of the cord and thus the highest chance of neurologic recovery.32 With this approach it is crucial to perform careful serial neurologic examinations and serial radiographs with each application of weight.
An alternative approach for managing a cervical facet dislocation injury has been advocated by Eismont et al.33 These authors believe that before any significant traction or attempt to reduce a cervical facet dislocation, an MRI should be obtained to rule out the presence of a traumatic disc herniation. Proponents of this approach point to rare case examples of neurologic deterioration that have occurred after closed reduction, particularly if done under general anesthesia where serial neurologic examination is not possible. With the approach of Eismont et al., after obtaining an MRI, the treating surgeon would perform an anterior decompression for those patients with a traumatic disc herniation, followed by reconstruction. Those without a traumatic disc herniation may be reduced either by closed or open reduction, followed by surgical stabilization.33 The safety and efficacy of each approach for traumatic facet dislocation continue to generate debate.34
In comparisons of surgical reconstruction techniques, posterior reconstruction has been shown to be more biomechanically sound than anterior reconstruction.28 Posterior reconstruction allows the disrupted posterior tension band to be reestablished. Despite this, Elgafy et al. and others (as cited in Jenkins et al.28) have reported the development of segmental kyphosis in some cases of bilateral facet dislocation treated with posterior-only instrumentation, particularly if nonrigid forms of instrumentation (i.e., wiring) are used. The most stable reconstruction technique of all is a circumferential approach with both anterior and posterior instrumentation. However, this approach produces increased surgical morbidity and requires additional time under anesthesia.35
In the case of a unilateral facet dislocation in the neurologically intact patient, some authors have advocated the use of a halo-vest orthosis or even cervical collar for immobilization without performing a reduction of the displaced joint. However, failure rates with immobilization because of either recurrent instability or chronic pain have ranged as high as 50%, suggesting reconsideration of this strategy.36 In the cases of an unreduced, unilateral dislocation, there is a significant risk of radiculopathic symptoms from compression of the exiting nerve root.37 Reduction can be achieved in either a closed fashion (with traction) or in an open surgical procedure, usually from a posterior approach. If the dislocation is reduced with traction, the surgeon has the option of performing either an anterior or posterior approach for stabilization. If open reduction is chosen, a posterior instrumented fusion would normally be performed.37 Shapiro et al. evaluated reconstructive options (interspinous braided cable/lateral mass plating with spinous process/facet wiring) with a posterior approach in patients with unilateral facet dislocations.38 Although all of the techniques proved to be effective, the more rigid lateral mass plating techniques were preferred. Henriques et al. reported a small series of patients with unilateral facet dislocations treated with anterior fusion.39 Successful fusion was achieved in most cases, but reoperation was required in 5.9% of the patients.
There is almost universal agreement regarding the need for surgical stabilization in cases of bilateral facet dislocation. These injuries are highly unstable and may redislocate after reduction, even when immobilized in a halo-vest orthosis.35 In the absence of an anterior disc herniation, reduction can be achieved by either closed or open means followed by posterior stabilization of the injury, preferably with rigid instrumentation.35 However, treatment of a bilateral facet dislocation in the presence of a large anterior traumatic disc herniation involves a more complex series of steps. First, a ventral approach is used to remove the disc herniation and decompress the spinal cord. Next, the surgeon can reduce the dislocation using either traction or anterior manipulation, or can proceed to a posterior open reduction. The advantage of achieving the reduction during the ventral portion of the procedure is that it allows the anterior column defect to be grafted. If a posterior approach is required to obtain the reduction, the posterior column of the spine can be stabilized with internal fixation; however, the anterior column must again be approached to graft the defect at the level of the disc space. Great care should be taken to avoid overdistraction of the disc space, which may occur in these grossly unstable injuries.
Although some have described successful treatment of bilateral facet dislocations with ventral stabilization alone, others have found an unacceptable rate of redislocation after this technique.40 Therefore, many authors recommend dorsal supplemental instrumentation even if the reduction and stabilization are achieved through an anterior approach. If the reduction cannot be achieved from the anterior approach or is not attempted owing to neurologic concerns, the surgeon should close the ventral wound and proceed to the dorsal spine to perform the reduction and stabilization of the segment, followed by a final return to the anterior column to graft the defect. One unique solution to handle a case with bilateral facet dislocation and a ventral disc herniation was described by Allred and Sledge,41 who placed a small ventral graft after ventral decompression, followed by placement of a ventral cervical plate attached only to the rostral vertebral body to retain the graft. With this technique, they were able to coax the graft back into position (using fluoroscopic guidance) during the dorsal reduction maneuver, thus avoiding the need to return to the ventral spine to graft the defect.41
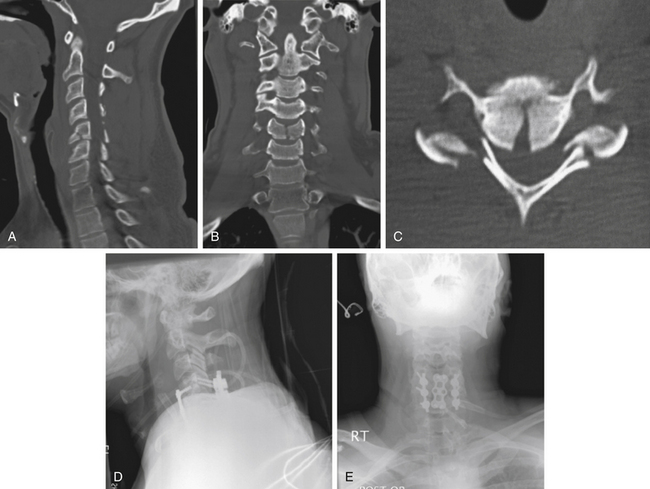
Teardrop Fractures/Severe Compressive Flexion Injuries
The teardrop fracture pattern is thought to result from severe flexion and compression of the cervical spine.9 This injury pattern demonstrates disruption to both the anterior and posterior columns of the cervical spine and has a high rate of neurologic injury. The injury pattern can be recognized on lateral radiographs by the fracture of the anteroinferior corner of the vertebral body and the commonly associated retrolisthesis of the upper vertebral body on the lower (Fig. 64-6). In addition, the posterior elements usually exhibit diastasis and the segment demonstrates kyphosis. A closely related variant, termed the quadrangular fracture, has a larger fracture fragment ventrally, seen on the lateral view, that courses vertically through the vertebral body from end plate to end plate.28 CT usually demonstrates dorsal fractures of the lamina or lateral mass, diastasis of the facet joints, and a sagittally oriented split through the vertebral body. MRI scanning commonly demonstrates spinal cord compression, cord signal change, and traumatic hemorrhage within the spinal canal, along with disruption of the dorsal ligamentous structures.
Neurologic injuries are exceedingly common in patients with the teardrop fracture pattern. The classic picture is a dense ventral spinal cord injury, although any pattern of injury may be encountered.28 Treatment for severe teardrop fractures is generally surgical, with the goals of decompressing the spinal canal, correcting the traumatic deformity, and providing stability to allow fusion across the fractured segment.
Some authors, including Toh et al. (as cited in Jenkins et al.28), have advocated a ventral approach with corpectomy, strut grafting, and the application of an ventral cervical plate. Although this approach may provide early reconstruction of the spinal injury, concerns regarding the lack of stability of the disrupted posterior column remain. For this reason, many authors have recommended a combined ventral and dorsal fixation strategy to address the more severe versions of this injury pattern. Cybulski et al.28 identified vertebral body retrolisthesis, facet diastasis, and shearing through the disc as indications for a circumferential fusion. De Iure et al.28 recommended circumferential surgery for any teardrop fracture in which an anatomic reduction could not be obtained or there was a traumatic listhesis of the segment. With the circumferential approach, the ventral decompression is usually performed first, achieving decompression of the spinal cord and reconstruction of the anterior column by placement of a structural strut graft, followed by posterior stabilization with segmental instrumentation. Dorsal stabilization can be achieved using a variety of techniques, although lateral mass fixation has become popular in recent years.
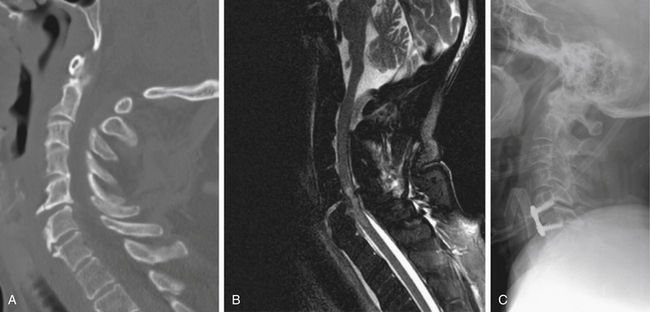
Hyperextension/Distractive Extension Injuries
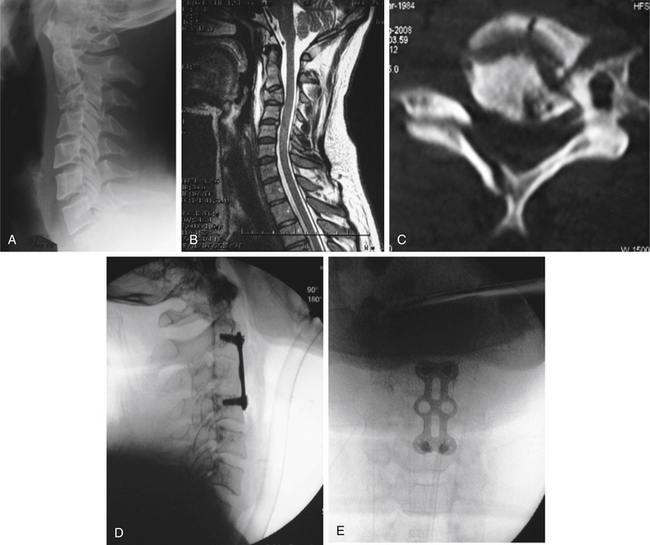
Severe extension injuries are most commonly seen in elderly patients or those with a stiff or ankylosed cervical spine, particularly those with diffuse idiopathic skeletal hyperostosis or ankylosing spondylitis. The most common injury mechanism is a ground-level fall or other low-energy trauma causing forced hyperextension of the neck with disruption of the anterior longitudinal ligament and disc. The stiff or ankylosed spinal segments are thought to create a long lever arm that concentrates the traumatic forces to the injury site, which is most commonly the disc space.28 The more severe forms of this injury pattern also exhibit disruption of the dorsal ligaments, which can be recognized by retrolisthesis of the rostral vertebral body on the caudal body. The treating physician must have a high index of suspicion when evaluating an elderly patient or a patient with a stiff spine after a suggestive trauma mechanism. Plain radiographs or even CT scans may fail to demonstrate displacement at the site of the disc space disruption, making it difficult to identify the injury. In such cases, an MRI often proves useful because it may demonstrate signal change through the disrupted disc space (Fig. 64-7).
Dorsal Element Fractures
Spinous Process Fractures
Also known as clay-shoveler’s fractures, these injuries are most commonly seen at the C6, C7, or T1 levels. The injury mechanism can be hyperextension with forceful compression of the spinous processes, hyperflexion with avulsion of the spinous process, or direct blunt-force trauma to the neck. Displaced spinous process fractures due to avulsion or repetitive stress have a high rate of pseudarthrosis.42 Because spinous process fractures may be a component of a more severe injury pattern, it is important to search for evidence of other injuries when a spinous process fracture is seen. Isolated spinous process fractures are usually stable injuries. After a period of immobilization to allow healing, flexion-extension radiographs are useful to rule out further instability. In the absence of instability, the neck is generally mobilized even if evidence of a nonunion is present.
Lamina, Pedicle, and Lateral Mass Fractures
Lamina, pedicle, and lateral mass fractures are commonly seen in association with other fractures, and thus it is important to search for other injuries that may signify a more severe injury pattern. These injuries are generally thought to be produced by forceful extension and/or rotation of the spine.42 Like other minimally displaced posterior element fractures, these fractures are easily missed on plain radiographs. Although oblique plain radiographs were previously recommended for diagnosis, these have been largely supplanted by CT, which provides excellent visualization of the posterior element fractures.42 Most isolated, nondisplaced fractures in this category are stable and are successfully treated with immobilization in a cervical orthosis. After healing, flexion-extension lateral radiographs can be obtained before initiating a structured rehabilitation program.42
Fractures of the lateral mass may involve the articular processes and thus could compromise the stability of the segment. It is important to examine the imaging studies carefully, looking for evidence of subluxation, which may indicate a more severe instability pattern. According to Allen et al.,9 subluxation of the spinal segment, substantial comminution of the lateral mass, and/or significant displaced fractures that extend to the articular processes are criteria for surgical stabilization.43 When surgical stabilization is required, the surgeon can either pursue an anterior approach, which has the advantage of fusing only the compromised segment, or a posterior approach, which generally requires bridging the disrupted segment to obtain stability and thus involves fusion of an additional motion segment.
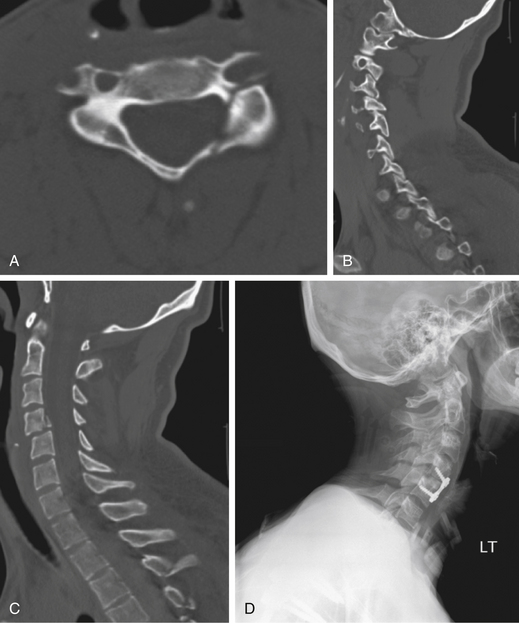
Kotani et al.,43 in a retrospective analysis of injuries to the lateral mass and facet joint, described an injury pattern involving an ipsilateral fracture of the lamina and pedicle, thus creating a “floating lateral mass” (Fig. 64-8). This injury is considered to be “unstable” by some because of the loss of both the superior and inferior articular process buttresses on the ipsilateral side of the spine.43 Others have recommended simple immobilization for the floating lateral mass injury without any evidence of subluxation. Some patients with fractures of the facet joint may experience radicular symptoms that can be managed with a dorsal foraminotomy with or without dorsal stabilization.42
Facet Fractures
Facet fractures make up a heterogeneous group of injuries, ranging from small avulsion fractures of the facet to shearing injuries that compromise a large portion of the articular process (Fig. 64-9). These fractures may result from either a hyperflexion or hyperextension mechanism, often combined with rotation. Facet fractures commonly occur in association with other cervical spinal trauma patterns, and thus a careful review of the imaging studies must be undertaken before characterizing a particular injury as an isolated facet fracture. For example, Johnson et al. found that two thirds of patients with an end plate compression fracture associated with a significant facet injury had an instability pattern that failed treatment with a ventral instrumented fusion.31
As reviewed by Kalayci et al., several authors have categorized cervical facet injuries.44 The management of a unilateral facet fracture remains controversial, with the exact indications for surgical stabilization being poorly defined. In part, this is due to the heterogeneous injury pattern and the variable levels of patient compliance with immobilization.
Although simple, minimally displaced fractures of the facet complex can be successfully treated with immobilization, displaced fractures or those involving large portions of the facet joint may be associated with instability and thus may require surgical stabilization. Lifeso et al.44 reviewed a cohort of patients with unilateral facet fractures and found coexisting spinal cord injury in 18% and root injury in 34%. Rorabeck et al.44 reported a series of 26 patients with unilateral facet fractures and found healing in only 20%, with a significant rate of chronic cervical pain and even late dislocations. In a series of 36 patients (24 of whom were treated nonoperatively), Beyer and Cabanela44 found a union rate of only 50%.
Surgical treatment has been suggested by some, using either an anterior or a posterior approach. In cadaver studies performed by Coe et al.,44 dorsal stabilization techniques (i.e., Rogers wiring, sublaminar wiring, Bohlman wiring, Roy-Camille dorsal plate fixation, oblique dorsal hook plate fixation) were compared without any significant biomechanical differences noted. However, wiring techniques generally are not useful in injuries with associated lamina or spinous process fractures; thus, lateral mass fixation has gained popularity in recent years. Lifeso et al.44 reported that dorsal stabilization and fusion procedures led to unsuccessful results in 5 of 11 patients using nonrigid stabilization techniques, with late kyphosis and/or poor rotational control of the injury pattern. Ventral discectomy and fusion with anterior cervical plating has also been suggested by some.44 Although ventral fusion is biomechanically less stable than dorsal fusion for injuries with severe dorsal disruption, it has proven successful for simple facet fractures requiring surgical stabilization.44 Garvey et al.44 found a lower rate of complications with a ventral, as opposed to a dorsal, approach. In a prospective study done by Lifeso et al.,44 patients treated by ventral stabilization with autogenous tricortical iliac crest bone graft demonstrated no nonunions and did not require any additional surgery during a minimum 2-year follow-up period.
Conclusion
Subaxial cervical trauma includes a heterogeneous group of injuries that have been characterized by both morphologic and mechanistic descriptions. It is useful to recognize the common injury patterns but also to note that within each injury pattern, a spectrum of disruption exists that produces advancing degrees of instability. Because the patient’s neurologic status is a key factor in determining treatment, a detailed examination according to ASIA standards should be undertaken. Definitions of mechanical stability remain somewhat elusive, although several classification systems provide a useful framework for the surgeon when defining the mechanical stability of the injury. The biomechanics of the injury should be a primary consideration when determining the treatment approach for stabilizing a cervical injury pattern.
Allen B.L., Ferguson R.L., Lehmann T.R., et al. A mechanistic classification of closed indirect fractures and dislocations of the lower cervical spine. Spine (Phila Pa 1976). 1982;7:1-27.
Anderson P.A., Moore T.A., Davis K.W., et al. Cervical spine injury severity score: assessment of reliability. J Bone Joint Surg [Am]. 2007;89:1057-1065.
Harris J., Edeiken-Monroe B., Kopaniky D. A practical classification of acute cervical spine injuries. Orthop Clin North Am. 1986;17:15-30.
Moore T.A., Vaccaro A.R., Anderson P.A. Classification of lower cervical spine injuries. Spine (Phila Pa 1976). 2006;31(Suppl 11):S37-S43.
Vaccaro A.R., Hulbert R.J., Patel A.A., et al. The subaxial cervical spine injury classification system: a novel approach to recognize the importance of morphology, neurology, and integrity of the disco-ligamentous complex. Spine (Phila Pa 1976). 2007;32:2365-2374.
White A.A.III, Panjabi M.M. Clinical biomechanics of the spine. Philadelphia: JB Lippincott; 1978. pp 102–107
Whitley J.E., Forsyth H.F. The classification of cervical spine injuries. Am J Roentgenol Radium Ther Nucl Med. 1960;83:633-644.
1. Moore T.A., Vaccaro A.R., Anderson P.A. Classification of lower cervical spine injuries. Spine (Phila Pa 1976). 2006;31(Suppl 11):S37-S43.
2. Watson-Jones R. The results of postural reduction of fractures of the spine. J Bone Joint Surg [Am]. 1938;20:567-586.
3. Vaccaro A.R., Hulbert R.J., Patel A.A., et al. The subaxial cervical spine injury classification system: a novel approach to recognize the importance of morphology, neurology, and integrity of the disco-ligamentous complex. Spine (Phila Pa 1976). 2007;32:2365-2374.
4. Holdsworth F. Fractures, dislocations and fracture-dislocations of the spine. J Bone Joint Surg [Br]. 1963;45:6-20.
5. White A.A.III, Panjabi M.M. Clinical biomechanics of the spine. Philadelphia: JB Lippincott; 1978. pp 102–107
6. Denis F. The three-column spine and its significance in classification of acute thoracolumbar spine injuries. Spine (Phila Pa 1976). 1989;8:817-831.
7. Stauffer E.S. Management of spine fractures C3 to C7. Orthop Clin North Am. 1977;17:45-53.
8. Whitley J.E., Forsyth H.F. The classification of cervical spine injuries. Am J Roentgenol Radium Ther Nucl Med. 1960;83:633-644.
9. Allen B.L., Ferguson R.L., Lehmann T.R., et al. A mechanistic classification of closed indirect fractures and dislocations of the lower cervical spine. Spine (Phila Pa 1976). 1982;7:1-27.
10. Harris J., Edeiken-Monroe B., Kopaniky D. A practical classification of acute cervical spine injuries. Orthop Clin North Am. 1986;17:15-30.
11. Anderson P.A., Moore T.A., Davis K.W., et al. Cervical spine injury severity score: assessment of reliability. J Bone Joint Surg [Am]. 2007;89:1057-1065.
12. Bernhardt M., White A.A.III, Panjabi M.M. Biomechanical considerations of spinal stability. In: Herkowitz H.N., Garfin S.R., Balderston R.A., et al, editors. Rothman-Simeone the spine. ed 4. Philadelphia: WB Saunders; 1999:1071-1096.
13. White A.A.III, Panjabi M.M. Kinematics of the spine. In: White A.A.III, Panjabi M.M., editors. Clinical biomechanics of the spine. ed 2. Philadelphia: JB Lippincott; 1990:85-278.
14. Roaf R.R. A study of the mechanics of spinal injuries. J Bone Joint Surg [Br]. 1960;42:810-823.
15. Beatson T.R. Fractures and dislocations of the cervical spine. J Bone Joint Surg [Br]. 1963;45:21-35.
16. Herkowitz H.N., Rothman R.H. Subacute instability of the cervical spine. Spine (Phila Pa 1976). 1984;9:348-357.
17. Bracken M.B., Shepard M.J., Collins W.F.Jr, et al. Methylprednisolone or naloxone treatment after acute spinal cord injury: 1-year follow-up data. Results of the second National Acute Spinal Cord Injury Study. J Neurosurg. 1992;76:23-31.
18. Maynard F.M.Jr, Bracken M.B., Creasey G., et al. International Standards for Neurological and Functional Classification of Spinal Cord Injury: American Spinal Injury Association. Spinal Cord. 1997;35:266-274.
19. Radiographic assessment of the cervical spine in asymptomatic trauma patients. Neurosurgery. 2002;50(Suppl 3):S30-S35.
20. Woodring J.H., Lee C. Limitations of cervical radiography in the evaluation of acute cervical trauma. J Trauma. 1993;34:32-39.
21. Núñez D.B.Jr, Ahmad A.A., Coin G.C., et al. Clearing the cervical spine in multiple trauma victims: a time-effective protocol using helical CT. Emerg Radiol. 1994;1:273-278.
22. Acheson M.B., Livingston R.R., Richardson M.L., et al. High-resolution CT scanning in the evaluation of cervical spine fractures: comparison with plain film examinations. AJR Am J Roentgenol. 1987;148:1179-1185.
23. Rubin G.D. Data explosion: the challenge of multidetector-row CT. Eur J Radiol. 2000;36:74-80.
24. Li A.E., Fishman E.K. Cervical spine trauma: evaluation by multidetector CT and three-dimensional volume rendering. Emerg Radiol. 2003;10:34-39.
25. Katzberg R.W., Benedetti P.F., Drake C.M., et al. Acute cervical spine injuries: prospective MR imaging assessment at a level 1 trauma center. Radiology. 1999;213:203-212.
26. Louw J.A., Mafoyane N.A., Small B., et al. Occlusion of the vertebral artery in cervical spine dislocations. J Bone Joint Surg [Br]. 1990;72:679-681.
27. Willis B.K., Greiner F., Orrison W.W., et al. The incidence of vertebral artery injury after midcervical spine fracture or subluxation. Neurosurgery. 1994;34:435-441. discussion 441–442
28. Jenkins A.L., Eichler M.E., Vollmer C. Cervical spine trauma. In: Winn H.R., editor. Youmans neurological surgery. ed 5. Philadelphia: Saunders; 2004:4885-4914.
29. Dvorak M.F., Fisher C.G., Fehlings M.G., et al. The surgical approach to subaxial cervical spine injuries: an evidence-based algorithm based on the SLIC classification system. Spine (Phila Pa 1976). 2007;32:2620-2629.
30. Anderson P.A., Bohlman H.H. Anterior decompression and arthrodesis of the cervical spine: long-term motor improvement: Part II. Improvement in complete traumatic quadriplegia. J Bone Joint Surg [Am]. 1992;74:683-692.
31. Johnson M, Dvorak MF, Fisher C: The radiographic failure of single-segment anterior cervical plate fixation in traumatic cervical flexion distraction injuries. Spine (Phila Pa 1976) 29:2815–2820.
32. Cotler J.M., Herbison G.J., Nasuti J.F., et al. Closed reduction of traumatic cervical spine dislocation using traction weights up to 140 pounds. Spine (Phila Pa 1976). 1993;18:386-390.
33. Eismont F.J., Arean M.J., Green B.A. Extrusion of an intervertebral disc associated with traumatic subluxation or dislocation of cervical facets: case report. J Bone Joint Surg [Am]. 1991;73:1555-1560.
34. Lee J.Y., Nassr A., Eck J.C., et al. Controversies in the treatment of cervical spine dislocations. Spine J. 2009;9:418-423.
35. Panjabi M.M., Simpson A.K., Ivancic P.C., et al. Cervical facet joint kinematics during bilateral facet dislocation. Eur Spine J. 2007;16:1680-1688.
36. Rabb C.H., Lopez J., Beauchamp K., et al. Unilateral cervical facet fractures with subluxation: injury patterns and treatment. J Spinal Disord Tech. 2007;20:416-422.
37. Duggal N., Chamberlain R.H., Park S.C., et al. Unilateral cervical facet dislocation: biomechanics of fixation. Spine (Phila Pa 1976). 2005;30:E164-E168.
38. Shapiro S., Snyder W., Kaufman K., et al. Outcome of 51 cases of unilateral locked cervical facets: interspinous braided cable for lateral mass plate fusion compared with interspinous wire and facet wiring with iliac crest. J Neurosurg. 1999;91:19-24.
39. Henriques T., Olerud C., Bergman A., et al. Distractive flexion injuries of the subaxial cervical spine treated with anterior plate alone. J Spinal Disord Tech. 2004;17:1-7.
40. Razack N., Green B.A., Levi A.D. The management of traumatic cervical bilateral facet fracture-dislocations with unicortical anterior plates. J Spinal Disord. 2000;13:374-381.
41. Allred C.D., Sledge J.B. Irreducible dislocations of the cervical spine with a prolapsed disc: preliminary results from a treatment technique. Spine (Phila Pa 1976). 2001;26:1927-1930.
42. Mirkovic S., Garfin S.R. Mini-symposium: cervical spine injuries. Curr Orthop. 1995;9:234-240.
43. Kotani Y., Abumi K., Ito M., et al. Cervical spine injuries associated with lateral mass and facet joint fractures: new classification and surgical treatment with pedicle screw fixation. Eur Spine J. 2005;14:69-77.
44. Kalayci M., Cagavi F., Acikgoz B. Unilateral cervical facet fracture: presentation of two cases and literature review. Spinal Cord. 2004;42:466-472.