Chapter 99 Stereotactic Radiosurgery for Trigeminal Neuralgia
Trigeminal neuralgia (TN) has been defined as sudden, paroxysmal, recurring stabbing pains of one or more branches of the trigeminal nerve that are generally unilateral.1 Classic TN is typically secondary to vascular compression or is idiopathic. Patients may recognize different pain triggers, such as chewing, talking, washing, shaving, smoking, or tooth brushing. Between pain episodes, patients tend to be asymptomatic, although a minority of patients continue to experience background pain.2,3 Many interventions exist for the treatment of TN. Application of stereotactically delivered radiation to treat TN has become a useful, minimally to noninvasive treatment option.
Historical Background
Ionizing radiation for the treatment of TN dates to within a few years of when x-rays were discovered, but it eventually grew out of favor.4 When stereotactic radiosurgery (SRS) was invented, the use of radiation for TN was revisited. In 1971, Leksell reported on two patients with classic TN whom he treated in 1953 with a single dose of ionizing radiation targeted on the gasserian ganglion and root entry zone.5 Results were unsatisfactory until the target was moved from the gasserian ganglion to the proximal trigeminal root near the pons.6 The effects of stereotactically delivered radiation at the root entry zone produces focal axonal degeneration and necrosis of the trigeminal nerve without affecting the gasserian ganglion, which is thought to be the mechanism resulting in pain relief in TN patients.7 Use of SRS, usually with the gamma knife machine, became widely acceptable in 1996 after a multi-institutional study demonstrated favorable results.8 Other technologies delivering stereotactic radiation to treat TN have also been reported. In 2003, Romanelli et al. reported the first use of the CyberKnife to treat TN.9 In the same year, Smith et al. reported the first series of patients with TN treated with linear accelerator (LINAC) radiosurgery.10
Indications
The initial treatment for TN is medical therapy, with carbamazepine being the gold standard and oxcarbazepine, a keto derivative of carbamazepine, a suitable alternative with more tolerable side effects. SRS is recommended for patients with medically refractory TN who are not surgical candidates, since microvascular decompression (MVD) has the highest rates of pain control in patients who are surgical candidates.11 SRS is regarded as the safest minimally invasive therapy for TN and is particularly useful in patients who are older than 70 years, have significant medical comorbidities, or decide not to undergo MVD.4,12 However, pain relief is not immediate and may take months.13 Ideally, SRS should be performed in patients who can undergo magnetic resonance imaging (MRI) for treatment planning. For patients with MRI-incompatible pacemakers or defibrillators, computed tomography (CT) with contrast cisternography can be used.14
As with other surgical treatments for TN, patients with typical TN symptomatology fare the best after SRS. Therefore, an accurate diagnosis is critical, because SRS may not be the best treatment option for patients with atypical features. For example, TN pain related to multiple sclerosis can be satisfactorily treated with SRS but not with the same success as classic TN.15 SRS can be used as a first-time interventional treatment and as repeat or salvage treatment for those who continue to have pain following SRS or other procedures.
Gamma Knife Technique
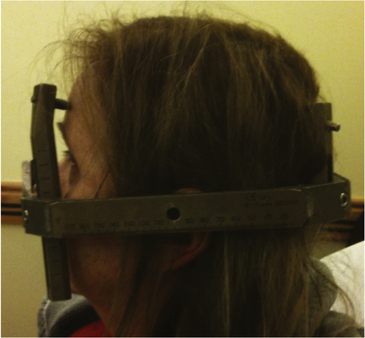
Gamma knife radiosurgery is a frame-based technique that delivers radiation from a fixed cobalt source. Planning and treatment occur the same day in a single session. On the day of treatment, the first step involves the placement of the stereotactic Leksell frame under local anesthesia. Typically, four points (two anterolateral and two occipital) are chosen to ensure appropriate fixation of the frame (Fig. 99-1). The insertion points are injected with a mixture of 2% lidocaine with sodium bicarbonate for local anesthesia. Bupivacaine can be injected concurrently for long-term analgesia. The screws are then inserted into the frame and skull. The appropriate screw should be selected so that it sits flush with the frame. If a screw is too long, it will lie outside of the frame, create additional artifact during the MRI, and possibly interfere with the treatment beams. It is also critical that the anterior screws be applied while the eyes of the patient are closed. If the screws are applied while the patient’s eyes are open, complete eye closure may not be possible, making it uncomfortable for the patient and risking corneal ulceration.
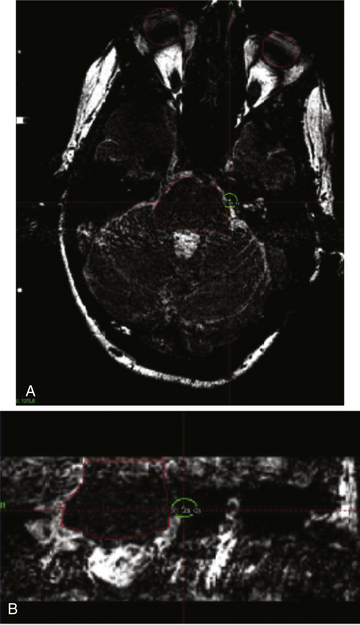
After application of the Leksell frame is completed, a 1-mm-slice MRI with gadolinium is obtained. T1, T2, and fast imaging employing steady-state acquisition (FIESTA) sequences allow trigeminal nerve identification and its relationship to adjacent blood vessels to be examined.16 The target is a single, 4-mm isocenter positioned at the trigeminal nerve root entry zone, 2 to 4 mm from the junction of the nerve and the pons8,13,17 (Fig. 99-2). Maintenance of this buffer zone between the nerve and the pons keeps the radiation delivered to the brain stem between 20% and 30% of the isodose.8 Final dose selection and calculation of the dosage delivery plans are done in conjunction with a radiation oncologist and a physicist.
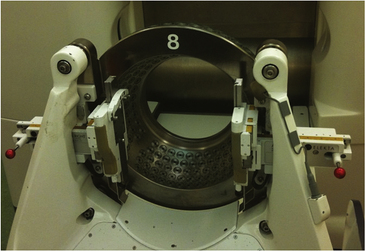
Once the planning is complete, treatment can proceed. The patient is placed on the treatment bed, and the collimator helmet is affixed (Fig. 99-3). Once the target coordinates for the beam have been confirmed, the treatment commences. After the treatment is complete, the Leksell frame is taken off by sequentially removing the screws opposite each other. The pin site defects are covered with gauze and antibiotic ointment.
Linear Accelerator
Other frame-based technologies have emerged, such as LINAC radiosurgery. Similar to gamma knife radiosurgery, frame placement on the patient, treatment planning, and the radiosurgical treatment session take place in the same day. The dose fallout areas have been shown to be comparable to those of gamma knife.18
Cyberknife Technique
An MRI FIESTA sequence with 1.25-mm thin cuts and a CT with 1.25-mm thin cuts should be obtained. The MRI is used to localize and target the trigeminal nerve root entry zone.19–21 The CT images are used as a template for localization during the treatment. The images from CT and MRI are fused together to combine the two data sets for treatment. The CT/MRI fusion technique has become standard practice at centers utilizing CyberKnife for the treatment of TN and has obviated the need for obtaining a CT-cisternogram to localize and target the trigeminal nerve root entry zone.20 As a result, treatment of TN with CyberKnife has become a noninvasive procedure.
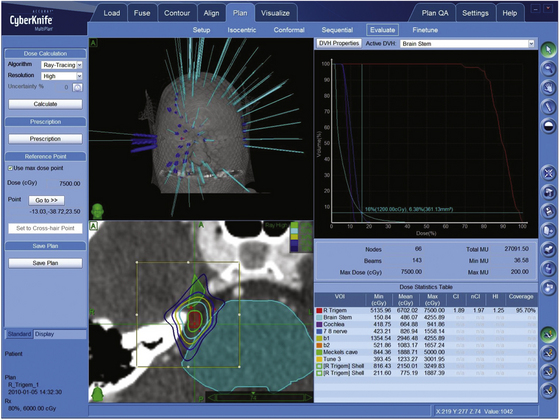
Once the trigeminal nerve and its root entry zone have been identified, a segment of the nerve is targeted for treatment. The segment should be 2 to 3 mm from the dorsal root entry zone to minimize the dose delivered to the brain stem. At this distance, the brain stem receives between 30% and 50% of the maximum treatment dose20 (Fig. 99-4). Likewise, extension into the gasserian ganglion in Meckel’s cave should be avoided. To minimize hot spots and heterogenous radiation dosages delivered to the nerve, a nonisocentric plan is used.
Once the planning is complete, the patient is placed supine on the treatment bed and kept in place using a custom-made thermoplastic mask. During the treatment session, orthogonal cranial x-rays are taken between every three to five treatment shots. The x-ray films are analyzed with reference to the previously loaded CT data and compared during the session to detect patient movement. When patient movement has occurred, the target coordinates are recalculated and the movements of the robotic arm movements are adjusted accordingly.22,23 Approximately 30 x-rays are taken during the treatment session, which is roughly equivalent to the radiation dose delivered during a routine CT scan.20 Using a 1.25-mm-slice CT scan in the data set, the accuracy of the target is roughly within 1.1 mm.24
Ideal Dosage and Targeting
Several factors affect the outcomes and side effects from treatment of TN with radiosurgery. These include the specific portion of the nerve treated, the dose delivered, and the length of nerve treated. Targeting of the gasserian ganglion was shown by multiple groups to reduce pain in a select number of patients but had poor long-term results.25,26 Improved short- and long-term results have been seen when the proximal nerve is targeted shortly after its takeoff from the pons. In this segment, the source of myelin of the nerve changes from oligodendrocytes (central) to Schwann cells (peripheral). It has been hypothesized that this zone is more sensitive to radiation.17 At the same time, minimizing the radiation delivered to the brain stem is of paramount importance.
In the first multi-institutional study conducted by Kondziolka et al., the effect of different dosages delivered to the trigeminal nerve using the gamma knife was examined. A significantly higher number of patients (72% vs. 9%) had complete pain relief with treatment doses greater than 70 Gy compared to those treated with doses less than 70 Gy.4,8 As the doses delivered increase above 70 Gy, the benefits are tempered by the associated morbidity. Pollock et al. examined the differences in treating patients with 70 and 90 Gy. A nonsignificant trend toward improved facial pain was seen. However, there was a significantly higher incidence of dysesthesias, corneal ulceration, and permanent trigeminal nerve dysfunction. Therefore, the dose delivered should be greater than 70 Gy but less than 90 Gy.7,27
The effect of radiating a longer length of the trigeminal nerve using the gamma knife was explored by Flickinger et al. In their study, 87 patients were randomized to either one isocenter or two isocenters on the proximal trigeminal nerve, receiving a maximum of 75 Gy to each isocenter. Pain control was equivalent in the two groups, and a significantly higher number of patients experienced complications (numbness or paresthesias) in the two-isocenter group.28 Therefore, treating a longer segment of the trigeminal nerve is not recommended.
The optimal dose and length of trigeminal nerve targeted for treatment by CyberKnife is still being refined. Lim et al. reported a series of 38 patients with TN treated with CyberKnife and divided them into two groups: Group 1 received a lower maximum dose (71.4 – 79.5 Gy), a lower minimum dose to the nerve margin (60 – 65.5 Gy), and had a shorter length of nerve treated; Group 2 received a higher maximum dose (80 – 86.3 Gy), a higher minimum dose to the nerve margin (66 – 70 Gy), and a longer length of nerve treated.29 While there was also no difference in pain response or recurrence based on length of nerve treated, the mean degree of numbness was significantly less when a shorter length (5-6.5 mm; median 6 mm) than a longer length (7-12 mm; median 8 mm) of nerve was treated. A subsequent study of 95 patients demonstrated that using higher radiation doses and treating longer nerve segments resulted in better pain relief.20 However, there was also a higher rate of numbness. This larger study suggested the treatment cohort with a median maximum dose of 78 Gy and a median treated nerve length of 6 mm had the optimal outcome of balancing pain relief with less numbness and side effects.
Outcomes
SRS is the least invasive treatment option, but pain relief is not as immediate as it is for other trigeminal rhizotomy procedures and MVD. Most studies on SRS have been retrospective case series with a large proportion of patients who had prior surgical interventions. Patients who underwent SRS as their first procedure had a longer duration without pain. The median time to pain relief is 2 weeks to 1 month, but relief can occur as fast as 1 day or as long as 6 months.8,19,20,30 With gamma knife, initial pain relief occurs in about 75% of patients. Three years following treatment, approximately 50% have sustained pain relief.12 However, reported results on treatment effectiveness vary widely among studies.31
All complications due to gamma knife radiation are related to trigeminal nerve dysfunction. The most common side effects are facial paresthesias, which occur in 6% to 13%. The risk of complications increases with higher doses, especially greater than 90 Gy.27,32 Repeat gamma knife radiation at a lower dose has similar pain relief rates, but the risk of complications is greater than with first-time use.33,34 Salvage gamma knife radiation for patients who have refractory TN following MVD provides pain relief for 50% and complete resolution for 20% at 5 years.35 Gamma knife radiation is also useful to treat TN related to multiple sclerosis but less effective than treating patients without multiple sclerosis. Reasonable pain control is reported in 80% to 97.3% of these patients overall and 82.6% at 1 year, 73.9% at 3 years, and 54.0% at 5 years after treatment in this patient population.15,36
In a large, prospective, controlled trial of gamma knife radiosurgery in 100 evaluable patients, initial pain relief occurred in 94% of patients at a median of 10 days. In this trial, 34 patients had pain recurrence at a median time of 6 months following treatment, with 17 patients undergoing additional surgeries. Overall, 83 patients were pain free at last follow-up, which was, at a minimum, 1 year after the procedure, and 69% were pain free without requiring another procedure. In addition, 10 patients had complications, all related to trigeminal nerve injury.31
The time to pain relief is arguably shorter by as much as 7 days with CyberKnife compared to gamma knife or LINAC radiation.29 The rate of initial pain relief with CyberKnife is as great as 92% to 94%.19,20,29 However, the proportion of patients with continous pain relief 3 years following treatment decreases by as much as 50%.20 Better pain relief is achieved with higher radiation doses or with a longer segment of nerve treated—but with higher rates of hypesthesia.20 Success of treatment is also improved when CyberKnife is used as the first treatment. For patients with no prior interventional treatment, 94% had initial pain relief, which was sustained in 78% at 1 year and 67% at 2 years after treatment.19 The use of CyberKnife for atypical TN has not been as well studied. In a series of seven patients with atypical TN, four experienced complete pain at a mean follow-up time of 28 months.21
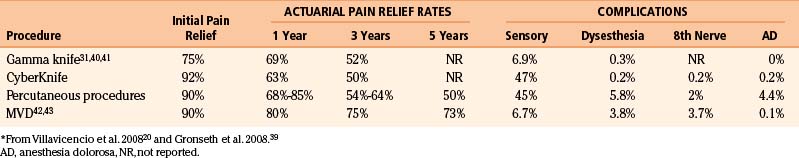
Comparison of Radiosurgery as Whole to Other Treatment Modalities
SRS is just one of many treatment options for medically refractory TN patients (Table 99-1). It is the newest treatment modality; therefore, long-term results have not been as extensively published as with the other modalities. It is an attractive option since it is the least invasive. However, patients who are surgical candidates are recommended to undergo MVD unless they prefer to avoid open surgery. In a prospective, nonrandomized cohort study of 80 consecutive patients comparing MVD and gamma knife radiosurgery, the actuarial pain-free rates were significantly higher with MVD initially (100% vs. 78%), at 2 years (88% vs. 50%), and at 5 years (80% vs. 33%).11 The relative risk in this study of no longer being pain free at 5 years after treatment was 3.35 for MVD versus gamma knife. Compared to SRS, the other trigeminal rhizolysis treatments (glycerol rhizotomy, radiofrequency ablation, and balloon microcompression) require at least intravenous sedation and needle insertion to or past the foramen ovale. Gamma knife radiation can be performed with only local anesthesia for frame placement, whereas CyberKnife radiosurgery is frameless and noninvasive.
For patients who are not surgical candidates, the percutaneous ablative techniques, particularly radiofrequency thermocoagulation, seem to have better sustained pain relief compared to gamma knife but with a higher risk of complications. The complication rate with gamma knife is less than with the percutaneous procedures, and side effects are limited to trigeminal nerve dysfunction.37 These conclusions have been made from systematic reviews, and a trial directly comparing SRS to the percutaneous procedures has yet to be completed.37
The literature thus far shows a higher rate of numbness with CyberKnife radiation.20 As experience grows, this is likely to be reduced as dose and target selection is optimized to best balance treatment effectiveness and complications. When only 6 mm of the trigeminal nerve was treated with CyberKnife, 5 out of 30 patients (17%) experienced post-treatment numbness and 1 out of 30 patients (3.3%) had a decreased corneal reflex.20 Complications not due to trigeminal nerve dysfunction, such as diplopia, decreased hearing, dry eyes, and right foot paresthesias, are reported with CyberKnife and are usually due to inadvertent excessive radiation of the brain stem.20
Rare complications such as meningitis, nontrigeminal cranial nerve dysfunction, accidental vascular injury, and decreased hearing can occur with the percutaneous rhizolysis techniques but should not occur with SRS if proper treatment planning is performed.38 Therefore, SRS is preferable for the subset of patients with contralateral hearing loss, because there is no risk of hearing impairment. Patients who are considering SRS should be counseled that pain relief may not occur for weeks. Patients who need immediate relief from debilitating pain may prefer the percutaneous therapies. Overall, SRS appears to be the safest treatment option for TN.
Barker F.G., Jannetta P.J., Bissonette D.J., et al. The long-term outcome of microvascular decompression for trigeminal neuralgia. N Engl J Med. 1996;334:1077-1083.
Chavez G.D., De Salles A.A., Solberg T.D., et al. Three-dimensional fast imaging employing steady-state acquisition magnetic resonance imaging for stereotactic radiosurgery of trigeminal neuralgia. Neurosurgery. 56, 2005. E628; discussion E
de Lotbiniere A. Gamma knife surgery for trigeminal neuralgia and facial pain. In: Lozano A.M., Gildenberg P.L., Tasker R.R. Textbook of Stereotactic and Functional Neurosurgery. Berlin, Heidelberg: Springer Berlin Heidelberg; 2009:2475-2481.
Dhople A.A., Adams J.R., Maggio W.W., et al. Long-term outcomes of gamma knife radiosurgery for classic trigeminal neuralgia: implications of treatment and critical review of the literature. J Neurosurg. 2009;111(2):351-358.
Fariselli L., Marras C., De Santis M., et al. CyberKnife radiosurgery as a first treatment for idiopathic trigeminal neuralgia. Neurosurgery. 2009;64:A96-101.
Flickinger J.C., Pollock B.E., Kondziolka D., et al. Does increased nerve length within the treatment volume improve trigeminal neuralgia radiosurgery? A prospective double-blind, randomized study. Int J Radiat Oncol Biol Phys. 2001;51:449-454.
Gronseth G., Cruccu G., Alksne J., et al. Practice parameter: the diagnostic evaluation and treatment of trigeminal neuralgia (an evidence-based review): report of the Quality Standards Subcommittee of the American Academy of Neurology and the European Federation of Neurological Societies. Neurology. 2008;71:1183-1190.
Hasegawa T., Kondziolka D., Spiro R., et al. Repeat radiosurgery for refractory trigeminal neuralgia. Neurosurgery. 2002;50:494-500. discussion 500-502
Kondziolka D., Flickinger J.C., Lunsford L.D., Habeck M. Trigeminal neuralgia radiosurgery: the University of Pittsburgh experience. Stereotact Funct Neurosurg. 1996;66(Suppl 1):343-348.
Kondziolka D., Lunsford L.D., Flickinger J.C., et al. Stereotactic radiosurgery for trigeminal neuralgia: a multiinstitutional study using the gamma unit. J Neurosurg. 1996;84:940-945.
Kondziolka D., Perez B., Flickinger J.C., et al. Gamma knife radiosurgery for trigeminal neuralgia: results and expectations. Arch Neurol. 1998;55:1524-1529.
Lim M., Villavicencio A.T., Burneikiene S., et al. CyberKnife radiosurgery for idiopathic trigeminal neuralgia. Neurosurg Focus. 2005;18:E9.
Linskey M.E., Ratanatharathorn V., Peñagaricano J. A prospective cohort study of microvascular decompression and gamma knife surgery in patients with trigeminal neuralgia. J Neurosurg. 2008;109(Suppl):160-172.
Ma L., Kwok Y., Chin L.S., et al. Comparative analyses of LINAC and gamma knife radiosurgery for trigeminal neuralgia treatments. Phys Med Biol. 2005;50:5217-5227.
Merskey H., Bogduk N. Classification of Chronic Pain: Description of Chronic Pain Syndromes and Definition of Pain Terms, 2nd ed. Seattle: IASP; 1994.
Nurmikko T.J., Eldridge P.R. Trigeminal neuralgia—pathophysiology, diagnosis and current treatment. British Journal of Anaesthesia. 2001;87:117-132.
Patil C.G., Veeravagu A., Bower R.S., et al. CyberKnife radiosurgical rhizotomy for the treatment of atypical trigeminal nerve pain. Neurosurg Focus. 2007;23:E9.
Pollock B.E., Phuong L.K., Foote R.L., et al. High-dose trigeminal neuralgia radiosurgery associated with increased risk of trigeminal nerve dysfunction. Neurosurgery. 2001;49:58-62. discussion -4
Regis J., Metellus P., Hayashi M., et al. Prospective controlled trial of gamma knife surgery for essential trigeminal neuralgia. J Neurosurg. 2006;104:913-924.
Rogers C.L., Shetter A.G., Ponce F.A., et al. Gamma knife radiosurgery for trigeminal neuralgia associated with multiple sclerosis. J Neurosurg. 2002;97:529-532.
Smith Z.A., De Salles A.A., Frighetto L., et al. Dedicated linear accelerator radiosurgery for the treatment of trigeminal neuralgia. J Neurosurg. 2003;99:511-516.
The International Classification of Headache Disorders: 2nd ed. Cephalalgia. 2004;24(Suppl 1):9-160.
Zakrzewska J.M. Diagnosis and differential diagnosis of trigeminal neuralgia. Clin J Pain. 2002;18:14-21.
Zakrzewska J.M., Lopez B.C., Kim S.E., Coakham H.B. Patient reports of satisfaction after microvascular decompression and partial sensory rhizotomy for trigeminal neuralgia. Neurosurgery. 2005;56:1304-1311. discussion 1311-1312
Zorro O., Lobato-Polo J., Kano H., et al. Gamma knife radiosurgery for multiple sclerosis–related trigeminal neuralgia. Neurology. 2009;73:1149-1154.
1. Merskey H., Bogduk N. Classification of Chronic Pain: Description of Chronic Pain Syndromes and Definition of Pain Terms, 2nd ed. Seattle: IASP; 1994.
2. The International Classification of Headache Disorders: 2nd ed. Cephalalgia. 2004;24(Suppl 1):9-160.
3. Zakrzewska J.M. Diagnosis and differential diagnosis of trigeminal neuralgia. Clin J Pain. 2002;18:14-21.
4. de Lotbiniere A. Gamma knife surgery for trigeminal neuralgia and facial pain. In: Lozano A.M., Gildenberg P.L., Tasker R.R. Textbook of Stereotactic and Functional Neurosurgery. Berlin, Heidelberg: Springer Berlin Heidelberg; 2009:2475-2481.
5. Leksell L. Sterotaxic radiosurgery in trigeminal neuralgia. Acta Chir Scand. 1971;137:311-314.
6. Nurmikko T.J., Eldridge P.R. Trigeminal neuralgia—pathophysiology, diagnosis and current treatment. British Journal of Anaesthesia. 2001;87:117-132.
7. Kondziolka D., Lacomis D., Niranjan A., et al. Histological effects of trigeminal nerve radiosurgery in a primate model: implications for trigeminal neuralgia radiosurgery, Neurosurgery, 2000 46:971-976; discussion 976-977
8. Kondziolka D., Lunsford L.D., Flickinger J.C., et al. Stereotactic radiosurgery for trigeminal neuralgia: a multiinstitutional study using the gamma unit. J Neurosurg. 1996;84:940-945.
9. Romanelli P., Heit G., Chang S.D., et al. CyberKnife radiosurgery for trigeminal neuralgia. Stereotact Funct Neurosurg. 2003;81:105-109.
10. Smith Z.A., De Salles A.A., Frighetto L., et al. Dedicated linear accelerator radiosurgery for the treatment of trigeminal neuralgia. J Neurosurg. 2003;99:511-516.
11. Linskey M.E., Ratanatharathorn V., Peñagaricano J. A prospective cohort study of microvascular decompression and gamma knife surgery in patients with trigeminal neuralgia. J Neurosurg. 2008;109(Suppl):160-172.
12. Lopez B.C., Hamlyn P.J., Zakrzewska J.M. Stereotactic radiosurgery for primary trigeminal neuralgia: state of the evidence and recommendations for future reports. J Neurol Neurosurg Psychiatry. 2004;75:1019-1024.
13. Kondziolka D., Perez B., Flickinger J.C., et al. Gamma knife radiosurgery for trigeminal neuralgia: results and expectations. Arch Neurol. 1998;55:1524-1529.
14. Worthington C., Hutson K., Boulware R., et al. Computerized tomography cisternography of the trigeminal nerve for stereotactic radiosurgery. Case report. J Neurosurg. 2000;93(Suppl 3):169-171.
15. Zorro O., Lobato-Polo J., Kano H., et al. Gamma knife radiosurgery for multiple sclerosis–related trigeminal neuralgia. Neurology. 2009;73:1149-1154.
16. Chavez G.D., De Salles A.A., Solberg T.D., et al. Three-dimensional fast imaging employing steady-state acquisition magnetic resonance imaging for stereotactic radiosurgery of trigeminal neuralgia. Neurosurgery. 56, 2005. E628; discussion E
17. Kondziolka D., Flickinger J.C., Lunsford L.D., Habeck M. Trigeminal neuralgia radiosurgery: the University of Pittsburgh experience. Stereotact Funct Neurosurg. 1996;66(Suppl 1):343-348.
18. Ma L., Kwok Y., Chin L.S., et al. Comparative analyses of LINAC and gamma knife radiosurgery for trigeminal neuralgia treatments. Phys Med Biol. 2005;50:5217-5227.
19. Fariselli L., Marras C., De Santis M., et al. CyberKnife radiosurgery as a first treatment for idiopathic trigeminal neuralgia. Neurosurgery. 2009;64:A96-101.
20. Villavicencio A.T., Lim M., Burneikiene S., et al. CyberKnife radiosurgery for trigeminal neuralgia treatment: a preliminary multicenter experience. Neurosurgery. 2008;62:647-655. discussion 655
21. Patil C.G., Veeravagu A., Bower R.S., et al. CyberKnife radiosurgical rhizotomy for the treatment of atypical trigeminal nerve pain. Neurosurg Focus. 23, 2007. E9
22. Adler J.R.Jr., Murphy M.J., Chang S.D., Hancock S.L. Image-guided robotic radiosurgery. Neurosurgery. 1999;44:1299-1306. discussion 306-307
23. Murphy M.J. An automatic six-degree-of-freedom image registration algorithm for image-guided frameless stereotaxic radiosurgery. Med Phys. 1997;24:857-866.
24. Chang S.D., Main W., Martin D.P., et al. An analysis of the accuracy of the CyberKnife: a robotic frameless stereotactic radiosurgical system. Neurosurgery. 2003;52:140-146. discussion 146-147
25. Rand R.W., Jacques D.B., Melbye R.W., et al. Leksell gamma knife treatment of tic douloureux. Stereotact Funct Neurosurg. 1993;61(Suppl 1):93-102.
26. Lindquist C., Kihlstrom L., Hellstrand E. Functional neurosurgery—a future for the gamma knife? Stereotact Funct Neurosurg. 1991;57:72-81.
27. Pollock B.E., Phuong L.K., Foote R.L., et al. High-dose trigeminal neuralgia radiosurgery associated with increased risk of trigeminal nerve dysfunction. Neurosurgery. 2001;49:58-62. discussion 62-64
28. Flickinger J.C., Pollock B.E., Kondziolka D., et al. Does increased nerve length within the treatment volume improve trigeminal neuralgia radiosurgery? A prospective double-blind, randomized study. Int J Radiat Oncol Biol Phys. 2001;51:449-454.
29. Lim M., Villavicencio A.T., Burneikiene S., et al. CyberKnife radiosurgery for idiopathic trigeminal neuralgia. Neurosurg Focus. 2005;18:E9.
30. Dhople A.A., Adams J.R., Maggio W.W., et al. Long-term outcomes of gamma knife radiosurgery for classic trigeminal neuralgia: implications of treatment and critical review of the literature. J Neurosurg. 2009;111(2):351-358.
31. Regis J., Metellus P., Hayashi M., et al. Prospective controlled trial of gamma knife surgery for essential trigeminal neuralgia. J Neurosurg. 2006;104:913-924.
32. Nicol B., Regine W.F., Courtney C., et al. Gamma knife radiosurgery using 90 Gy for trigeminal neuralgia. J Neurosurg. 2000;93(Suppl 3):152-154.
33. Dvorak T., Finn A., Price L.L., et al. Retreatment of trigeminal neuralgia with gamma knife radiosurgery: is there an appropriate cumulative dose? Clinical article. J Neurosurg. 2009;111:359-364.
34. Hasegawa T., Kondziolka D., Spiro R., et al. Repeat radiosurgery for refractory trigeminal neuralgia. Neurosurgery. 2002;50:494-500. discussion-2
35. Little A.S., Shetter A.G., Shetter M.E., et al. Salvage gamma knife stereotactic radiosurgery for surgically refractory trigeminal neuralgia. Int J Radiat Oncol Biol Phys. 2009;74:522-527.
36. Rogers C.L., Shetter A.G., Ponce F.A., et al. Gamma knife radiosurgery for trigeminal neuralgia associated with multiple sclerosis. J Neurosurg. 2002;97:529-532.
37. Gronseth G., Cruccu G., Alksne J., et al. Practice parameter: the diagnostic evaluation and treatment of trigeminal neuralgia (an evidence-based review): report of the Quality Standards Subcommittee of the American Academy of Neurology and the European Federation of Neurological Societies. Neurology. 2008;71:1183-1190.
38. Lopez B.C., Hamlyn P.J., Zakrzewska J.M. Systematic review of ablative neurosurgical techniques for the treatment of trigeminal neuralgia. Neurosurgery. 2004;54:973-982. discussion 982-983
39. Gronseth G., Cruccu G., Alksne J., et al. Practice parameter: the diagnostic evaluation and treatment of trigeminal neuralgia (an evidence-based review): report of the Quality Standards Subcommittee of the American Academy of Neurology and the European Federation of Neurological Societies. Neurology. 2008;71:1183-1190.
40. Maesawa S., Salame C., Flickinger J.C., et al. Clinical outcomes after stereotactic radiosurgery for idiopathic trigeminal neuralgia. J Neurosurg. 2001;94:14-20.
41. Petit J.H., Herman J.M., Nagda S., et al. Radiosurgical treatment of trigeminal neuralgia: evaluating quality of life and treatment outcomes. Int J Radiat Oncol Biol Phys. 2003;56:1147-1153.
42. Zakrzewska J.M., Lopez B.C., Kim S.E., Coakham H.B. Patient reports of satisfaction after microvascular decompression and partial sensory rhizotomy for trigeminal neuralgia. Neurosurgery. 2005;56:1304-1311. discussion 1311-1312
43. Barker F.G., Jannetta P.J., Bissonette D.J., et al. The long-term outcome of microvascular decompression for trigeminal neuralgia. N Engl J Med. 1996;334:1077-1083.