Sports Medicine
SECTION 2 THIGH, HIP, AND PELVIS
SECTION 3 LEG, FOOT, AND ANKLE
V. Impingement Syndrome/Rotator Cuff Disease
VI. Superior Labral and Biceps Tendon Injuries
VII. Acromioclavicular and Sternoclavicular Injuries
section 1 Knee
1. Hinge joint that also incorporates both gliding and rolling, which are essential to its kinematics
2. See Chapter 2, Anatomy, for a thorough discussion of knee anatomy.
 Anterior cruciate ligament (ACL)
Anterior cruciate ligament (ACL)
 Despite intensive research, the function and anatomy of the ACL are still debated.
Despite intensive research, the function and anatomy of the ACL are still debated.
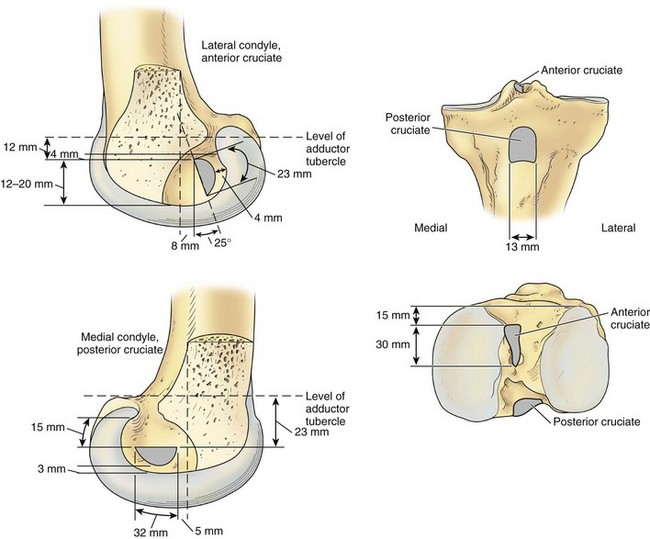
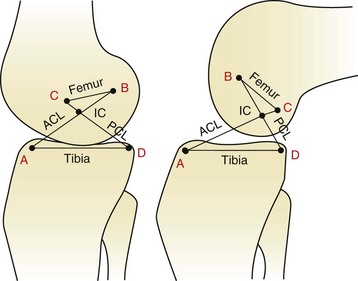
 Femoral attachment: semicircular area on the posteromedial aspect of the lateral femoral condyle (Figure 4-1)
Femoral attachment: semicircular area on the posteromedial aspect of the lateral femoral condyle (Figure 4-1)
 Tibial insertion: broad, irregular, oval area just anterior to and between the intercondylar eminences of the tibia
Tibial insertion: broad, irregular, oval area just anterior to and between the intercondylar eminences of the tibia
 Has two “bundles” named on the basis of tibial insertion:
Has two “bundles” named on the basis of tibial insertion:
 Anteromedial: tight in flexion; primarily an anterior restraint; evaluated by Lachman and anterior drawer tests
Anteromedial: tight in flexion; primarily an anterior restraint; evaluated by Lachman and anterior drawer tests
 Posterolateral: tight in extension; primarily a rotatory restraint; evaluated by pivot shift test
Posterolateral: tight in extension; primarily a rotatory restraint; evaluated by pivot shift test
 Composition: 90% type I collagen and 10% type III collagen
Composition: 90% type I collagen and 10% type III collagen
 Blood supply: Both cruciate ligaments receive their blood supply via branches of the middle geniculate artery and the fat pad.
Blood supply: Both cruciate ligaments receive their blood supply via branches of the middle geniculate artery and the fat pad.
 Mechanoreceptor nerve fibers within the ACL have been found and may have a proprioceptive role.
Mechanoreceptor nerve fibers within the ACL have been found and may have a proprioceptive role.
 Posterior cruciate ligament (PCL)
Posterior cruciate ligament (PCL)
 Femoral attachment: broad, crescent-shaped area on the anterolateral medial femoral condyle
Femoral attachment: broad, crescent-shaped area on the anterolateral medial femoral condyle
 Tibial insertion: tibial sulcus below articular surface (see Figure 4-1)
Tibial insertion: tibial sulcus below articular surface (see Figure 4-1)
 Variable meniscofemoral ligaments originate from the posterior horn of the lateral meniscus and insert into the substance of the PCL.
Variable meniscofemoral ligaments originate from the posterior horn of the lateral meniscus and insert into the substance of the PCL.
 Medial collateral ligament (MCL)
Medial collateral ligament (MCL)
 Superficial MCL (tibial collateral ligament)
Superficial MCL (tibial collateral ligament)
 Lies deep to the gracilis and semitendinosus tendons
Lies deep to the gracilis and semitendinosus tendons
 Originates 3.2 mm proximal and 4.8 mm posterior from the medial femoral epicondyle
Originates 3.2 mm proximal and 4.8 mm posterior from the medial femoral epicondyle
 Inserts onto the periosteum of the proximal tibia, deep to the pes anserinus
Inserts onto the periosteum of the proximal tibia, deep to the pes anserinus
 Superficial fibers insert 61.2 mm distal to the knee joint.
Superficial fibers insert 61.2 mm distal to the knee joint.
 Anterior fibers tighten during first 90 degrees of motion; posterior fibers tighten during extension.
Anterior fibers tighten during first 90 degrees of motion; posterior fibers tighten during extension.
 Lateral collateral ligament (LCL); also known as the fibular collateral ligament
Lateral collateral ligament (LCL); also known as the fibular collateral ligament
 Origin: lateral femoral epicondyle
Origin: lateral femoral epicondyle
 Insertion: anterolateral aspect of the fibular head
Insertion: anterolateral aspect of the fibular head
 Tight in extension and lax in flexion because of its location behind the axis of knee rotation
Tight in extension and lax in flexion because of its location behind the axis of knee rotation
 Deep and posterior to the superficial MCL, contiguous with the deep MCL
Deep and posterior to the superficial MCL, contiguous with the deep MCL
 Increasingly important factor in the treatment of the multiple ligament injured knee
Increasingly important factor in the treatment of the multiple ligament injured knee
 Originates on the back of the tibia
Originates on the back of the tibia
 The femoral insertion is inferior, anterior, and deep to the LCL.
The femoral insertion is inferior, anterior, and deep to the LCL.
 Arcuate ligament (which is contiguous with the oblique popliteal ligament medially)
Arcuate ligament (which is contiguous with the oblique popliteal ligament medially)
 Fabellofibular ligament (lateral two are really just thickenings of the joint capsule)
Fabellofibular ligament (lateral two are really just thickenings of the joint capsule)
 The PLC is the primary stabilizer of external tibial rotation.
The PLC is the primary stabilizer of external tibial rotation.
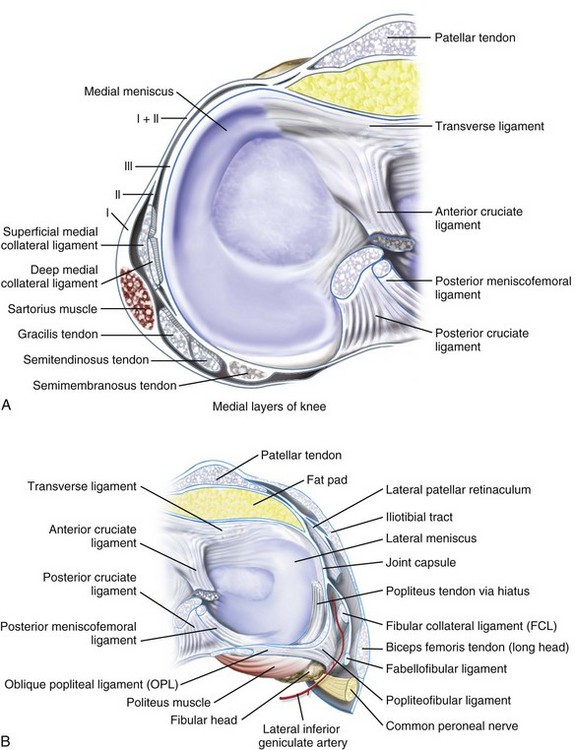
4. Medial structures of the knee (three layers) (Table 4-1; Figure 4-2)
Table 4-1
| Layer | Components |
| I | Sartorius and fascia |
| II | Superficial MCL, posterior oblique ligament, semimembranosus |
| III | Deep MCL, capsule |
MCL, medial collateral ligament.
Note: The gracilis, semitendinosus, and saphenous nerves run between layers I and II.
5. Lateral structures of the knee (three layers) (Table 4-2; see Figure 4-2)
Table 4-2
Lateral Structures of the Knee
| Layer | Components |
| I | Iliotibial tract, biceps, fascia |
| II | Patellar retinaculum, patellofemoral ligament |
| III | Arcuate ligament, fabellofibular ligament, capsule, LCL |
 The order of insertion of structures on the proximal fibula is, from anterior to posterior, the LCL, the popliteofibular ligament, and the biceps femoris.
The order of insertion of structures on the proximal fibula is, from anterior to posterior, the LCL, the popliteofibular ligament, and the biceps femoris.
 Crescent-shaped, fibrocartilagenous structures
Crescent-shaped, fibrocartilagenous structures
 Composed predominantly of type 1 collagen
Composed predominantly of type 1 collagen
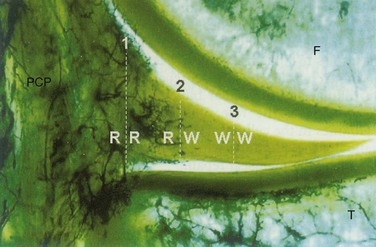
 Only the peripheral 20% to 30% of the medial meniscus and the peripheral 10% to 25% of the lateral meniscus are vascularized (medial and lateral genicular arteries, respectively; see Figure 4-1).
Only the peripheral 20% to 30% of the medial meniscus and the peripheral 10% to 25% of the lateral meniscus are vascularized (medial and lateral genicular arteries, respectively; see Figure 4-1).
 Medial meniscus is more C-shaped; lateral meniscus is more circular (see Figure 4-1).
Medial meniscus is more C-shaped; lateral meniscus is more circular (see Figure 4-1).
 Role: to deepen the articular surfaces of the tibial plateau and function in stability, lubrication, and joint nutrition
Role: to deepen the articular surfaces of the tibial plateau and function in stability, lubrication, and joint nutrition
 The two menisci are connected anteriorly by the transverse (intermeniscal) ligament.
The two menisci are connected anteriorly by the transverse (intermeniscal) ligament.
 They are attached peripherally by coronary ligaments.
They are attached peripherally by coronary ligaments.
 The menisci move anteriorly in extension and posteriorly with flexion. The lateral meniscus has fewer soft tissue attachments and is more mobile than the medial meniscus.
The menisci move anteriorly in extension and posteriorly with flexion. The lateral meniscus has fewer soft tissue attachments and is more mobile than the medial meniscus.
 Articulation between the patella and femoral trochlea
Articulation between the patella and femoral trochlea
 Patella has variably sized medial and lateral facets.
Patella has variably sized medial and lateral facets.
 Articular surface of the patella is the thickest in the body.
Articular surface of the patella is the thickest in the body.
 The patella can withstand forces several times those of body weight.
The patella can withstand forces several times those of body weight.
 The patella is restrained in trochlea by the valgus axis of the quadriceps mechanism (Q angle), the oblique fibers of the vastus medialis oblique and lateralis muscles (and their extensions, all of which constitute the patella retinaculum), the bony and cartilaginous anatomy of the trochlea, and the patellofemoral ligaments.
The patella is restrained in trochlea by the valgus axis of the quadriceps mechanism (Q angle), the oblique fibers of the vastus medialis oblique and lateralis muscles (and their extensions, all of which constitute the patella retinaculum), the bony and cartilaginous anatomy of the trochlea, and the patellofemoral ligaments.
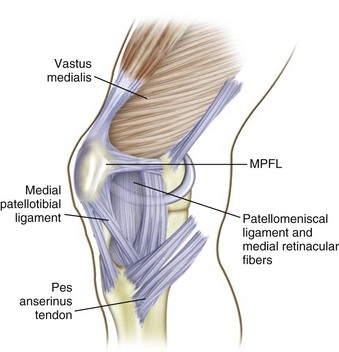
 The medial patellofemoral ligament is present in the second medial layer (Figure 4-4).
The medial patellofemoral ligament is present in the second medial layer (Figure 4-4).
 Origin: just anterior and distal to the adductor tubercle or just superior to the origin of the superficial medial collateral ligament
Origin: just anterior and distal to the adductor tubercle or just superior to the origin of the superficial medial collateral ligament
 Insertion: junction of proximal and middle third on the medial border of the patella as well as the undersurface of the vastus medialis oblique muscle
Insertion: junction of proximal and middle third on the medial border of the patella as well as the undersurface of the vastus medialis oblique muscle
 Role: to prevent lateral displacement of the patella, contributing more than 50% of the total medial restraint to lateral subluxation
Role: to prevent lateral displacement of the patella, contributing more than 50% of the total medial restraint to lateral subluxation
1. Ligamentous biomechanics: The role of the ligaments of the knee is to provide passive restraints against abnormal motion (Table 4-3).
Table 4-3
Biomechanics of Knee Ligaments
| Ligament | Restraint |
| ACL | Minimizing anterior translation of the tibia in relation to the femur (85%) |
| PCL | Minimizing posterior tibial displacement (95%) |
| MCL | Minimizing valgus angulation |
| LCL | Minimizing varus angulation |
| MCL and LCL | Acting in concert with posterior structures to control axial rotation of the tibia on the femur |
| PCL and posterolateral corner | Acting synergistically to resist posterior translation and posterolateral rotary instability |
2. Structural properties of ligaments: The tensile strength of a ligament, or maximal stress that a ligament can sustain before failure, has been characterized for all knee ligaments. However, it is important to consider age, ligament orientation, preparation of the specimen, and other factors before determining which graft to use.
 ACL: approximately 2200 N and up to 2500 N in young individuals
ACL: approximately 2200 N and up to 2500 N in young individuals
 The tensile strength of a 10-mm patellar tendon graft (young specimen) is more than 2900 N and is about 30% stronger when it is rotated 90 degrees. However, this strength quickly diminishes in vivo.
The tensile strength of a 10-mm patellar tendon graft (young specimen) is more than 2900 N and is about 30% stronger when it is rotated 90 degrees. However, this strength quickly diminishes in vivo.
 Studies suggest that the quadrupled hamstring graft has even greater tensile strength but is dependent on graft fixation.
Studies suggest that the quadrupled hamstring graft has even greater tensile strength but is dependent on graft fixation.
 PCL: approximately 2500 to 3000 N, but this has been disputed
PCL: approximately 2500 to 3000 N, but this has been disputed
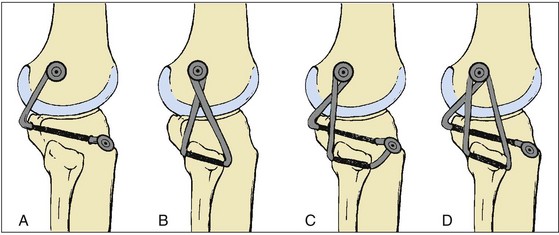
3. Kinematics: The motion of the knee joint and interplay of ligaments have been described as a four-bar cruciate linkage system (Figure 4-5).
 As the knee flexes, the center of joint rotation (intersection of the cruciate ligaments) moves posteriorly, causing rolling and gliding at the articulating surfaces.
As the knee flexes, the center of joint rotation (intersection of the cruciate ligaments) moves posteriorly, causing rolling and gliding at the articulating surfaces.
 The concept of ligament “isometry” remains controversial.
The concept of ligament “isometry” remains controversial.
 Reconstructed ligaments should approximate normal anatomy and lie within the flexion axis in all positions of knee motion.
Reconstructed ligaments should approximate normal anatomy and lie within the flexion axis in all positions of knee motion.
 As the joint flexes, ligaments anterior to the flexion axis stretch, and ligaments posterior to the axis shorten.
As the joint flexes, ligaments anterior to the flexion axis stretch, and ligaments posterior to the axis shorten.
 Although many instruments have been designed to achieve isometry, other considerations, such as graft impingement and avoiding flexion contractures, may be of more importance for ligament reconstructions.
Although many instruments have been designed to achieve isometry, other considerations, such as graft impingement and avoiding flexion contractures, may be of more importance for ligament reconstructions.
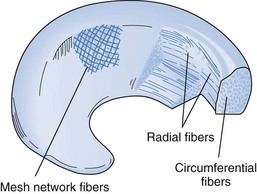
 The collagen fibers of the menisci are arranged radially and longitudinally (Figure 4-6).
The collagen fibers of the menisci are arranged radially and longitudinally (Figure 4-6).
 The longitudinal fibers help dissipate the hoop stresses in the menisci.
The longitudinal fibers help dissipate the hoop stresses in the menisci.
 The combination of fibers allows the meniscus to expand under compressive forces and increase the contact area of the joint.
The combination of fibers allows the meniscus to expand under compressive forces and increase the contact area of the joint.
 The lateral meniscus has twice the excursion of the medial meniscus during range of motion (ROM) and rotation of the knee.
The lateral meniscus has twice the excursion of the medial meniscus during range of motion (ROM) and rotation of the knee.
 Studies have shown that an ACL deficiency may result in abnormal meniscal strain, particularly in the posterior horn of the medial meniscus (Figure 4-7).
Studies have shown that an ACL deficiency may result in abnormal meniscal strain, particularly in the posterior horn of the medial meniscus (Figure 4-7).
 Mensical root tears completely disrupt the circumferential fibers of the meniscus, leading to meniscal extrusion.
Mensical root tears completely disrupt the circumferential fibers of the meniscus, leading to meniscal extrusion.
 Biomechanical studies have shown similar load patterns between posterior root tear and complete meniscectomy.
Biomechanical studies have shown similar load patterns between posterior root tear and complete meniscectomy.
1. Complete history of the injury
2. Clarification of mechanism of injury
4. Important key historical points (Table 4-4)
Table 4-4![]()
Key Historical Points That Indicate Mechanism of Injury
| History | Significance |
| Pain after sitting or climbing stairs | Patellofemoral cause |
| Locking or pain with squatting | Meniscal tear |
| Noncontact injury with “popping” sound/sensation | ACL tear, patellar dislocation |
| Contact injury with “popping” sound | Collateral ligament tear, meniscal tear, fracture |
| Acute swelling | ACL tear, peripheral meniscal tear, osteochondral fracture, capsule tear |
| Knee “gives way” | Ligamentous laxity, patellar instability |
| Anterior force: dorsiflexed foot | Patellar injury |
| Anterior force: plantar-flexed foot | PCL injury |
| Dashboard injury | PCL or patellar injury |
| Hyperextension, varus angulation, and tibial external rotation | Posterolateral corner injury |
ACL, anterior cruciate ligament; PCL, posterior cruciate ligament.
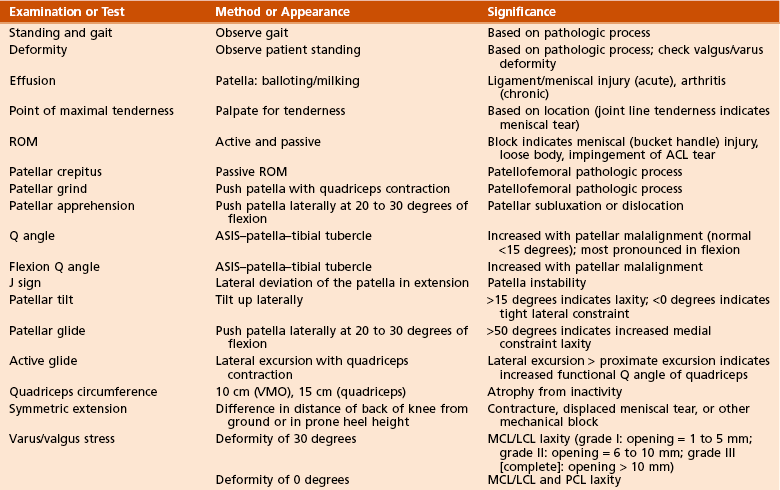
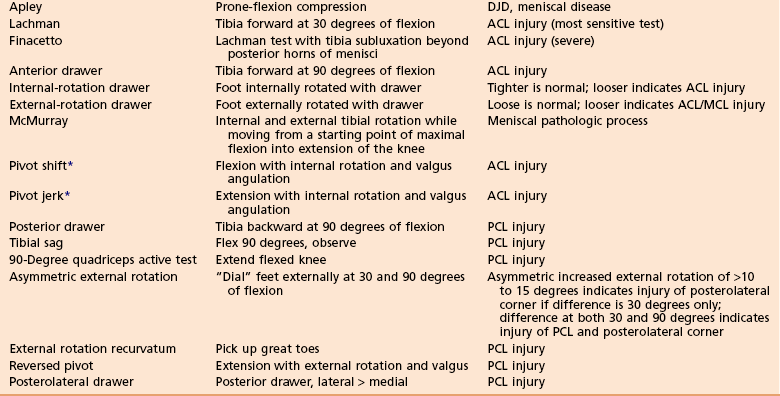
1. Key examination points are shown in Table 4-5.
Table 4-5![]()
 Most common causes of an acute hemarthrosis: ACL tear (70%), patella dislocation, osteochondral fracture, and isolated meniscal tear
Most common causes of an acute hemarthrosis: ACL tear (70%), patella dislocation, osteochondral fracture, and isolated meniscal tear
2. Examination performed with the patient under anesthesia may be helpful in some cases.
C Instrumented measurement of knee laxity
1. KT-1000 and KT-2000 Knee Ligament Arthrometers (MEDmetric, San Diego, California) are the devices most commonly used for standardized laxity measurement.
 ACL laxity is measured with the knee in slight flexion (20 to 30 degrees) with the application of a standard force (30 pounds [13.6 kg]).
ACL laxity is measured with the knee in slight flexion (20 to 30 degrees) with the application of a standard force (30 pounds [13.6 kg]).
 Values are reported as millimeters of anterior displacement, with comparisons with the opposite (normal) side.
Values are reported as millimeters of anterior displacement, with comparisons with the opposite (normal) side.
 A difference of more than 3 mm between sides is considered significant.
A difference of more than 3 mm between sides is considered significant.
 PCL laxity can also be measured with this device, although it is less accurate.
PCL laxity can also be measured with this device, although it is less accurate.
 Weight-bearing 45-degree posteroanterior view
Weight-bearing 45-degree posteroanterior view
 Merchant or Laurin view of the patella
Merchant or Laurin view of the patella
 Additional views include long-cassette, lower extremity hip-to-ankle views; oblique views; stress radiographs.
Additional views include long-cassette, lower extremity hip-to-ankle views; oblique views; stress radiographs.
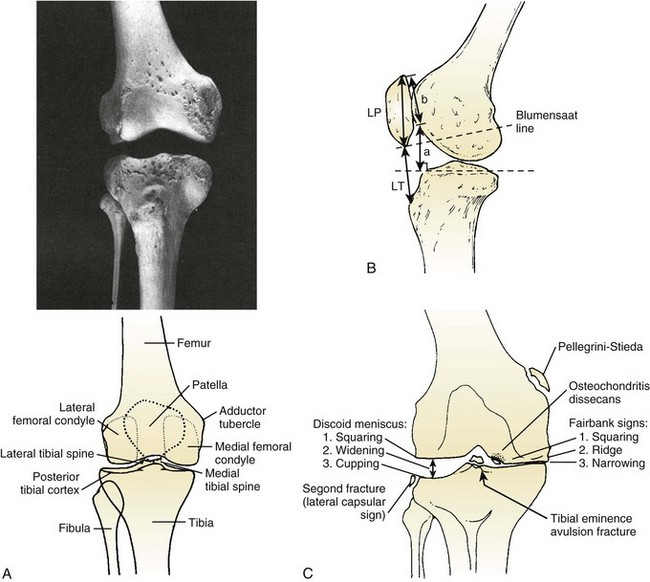
 Several findings and their significance are listed in Table 4-6.
Several findings and their significance are listed in Table 4-6.
Table 4-6![]()
Knee Injuries: Radiographic Findings
| View/Sign | Findings | Significance |
| Lateral-high patella | Patella alta | Patellofemoral pathologic process |
| Congruence angle | µ = −6 degrees; SD = 11 degrees | Patellofemoral pathologic process |
| Tooth sign | Irregular anterior patella | Patellofemoral chondrosis |
| Varus/valgus stress view | Opening | Collateral ligament injury; Salter-Harris fracture |
| Lateral capsule (Segond) sign | Small tibial avulsion off lateral tibia | ACL tear |
| Pellegrini-Stieda lesion | Avulsion of medial femoral condyle | Chronic MCL injury |
| Lateral-stress view: stress to anterior tibia with knee flexed 70 degrees | Asymmetric posterior tibial displacement | PCL injury |
| Weight-bearing posteroanterior view flexion | Early DJD, OCD, notch evaluation | |
| Fairbank changes | Square condyle, peak eminences, ridging, narrowing | Early DJD (postmeniscectomy) |
| Square lateral condyle | Thickened joint space | Discoid meniscus |
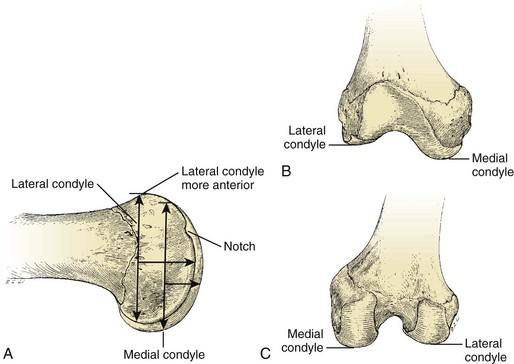
 Normal bony anatomy is demonstrated in Figure 4-8, A. Many of these findings are illustrated in Figure 4-8, B.
Normal bony anatomy is demonstrated in Figure 4-8, A. Many of these findings are illustrated in Figure 4-8, B.
 Evaluation of patella height is accomplished by one of three commonly used methods (see Figure 4-8, C).
Evaluation of patella height is accomplished by one of three commonly used methods (see Figure 4-8, C).
2. Stress radiographs: These are useful for evaluating injuries to the femoral physis (to differentiate from MCL injury) and are becoming the “gold standard” in diagnosing and quantifying PCL injury. They can also be used to evaluate LCL and PLC injuries.
3. Nuclear imaging: Technetium-99m bone scans are useful in diagnosing stress fractures, early degenerative joint disease, and complex regional pain syndrome.
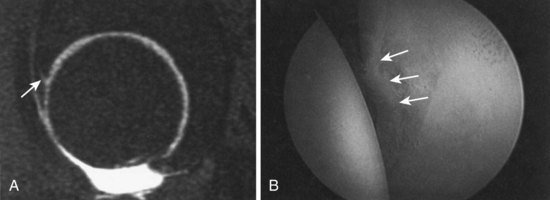
4. Magnetic resonance imaging (MRI): This has become the imaging modality of choice for diagnosis of ligament injuries, meniscal disease, avascular necrosis, spontaneous osteonecrosis of the knee, and articular cartilage defects and has replaced the use of arthrography. On coronal MRI sequences, meniscal root tears are seen as a band of low-signal fibrocartilage. Occult fractures of the knee can be identified by a double fluid-fluid layer, which signifies lipohemarthrosis.
5. Magnetic resonance arthrography: Intraarticular magnetic resonance arthrography is the most accurate imaging method for confirming the diagnosis of repeated meniscal tears after repair.
6. Computed tomography (CT): CT has been replaced largely by MRI, but it is still useful in the evaluation of bony tumors, patellar tilt, and fractures. CT has been advocated as a tool to assist in operative planning for patellar realignment by allowing measurement of the tibial tuberosity–trochlear groove (TT-TG) distance; authors recommend distal realignment procedures for a TT-TG distance exceeding 20 mm. MRI can also be used to measure TT-TG distance.
7. Arthrography: This technique was useful historically for the diagnosis of MCL tears and has been supplanted by MRI. However, it can be useful when MRI is not available or tolerated by the patient, and it can be combined with CT.
8. Tomography: Tomograms are preferred to CT in the evaluation of tibial plateau fractures at some medical centers.
9. Ultrasonography: This technique is useful for detecting soft tissue lesions about the knee, including patellar tendinitis, hematomas, and extensor mechanism ruptures, in some centers. Ultrasonography has begun to be used to evaluate meniscal tears but is not as sensitive as MRI.
See Supplemental Images on expertconsult.com.
1. The “gold standard” for the diagnosis of knee disease
2. The benefits of arthroscopic over open techniques include smaller incisions, less morbidity, improved visualization, and decreased recovery time.
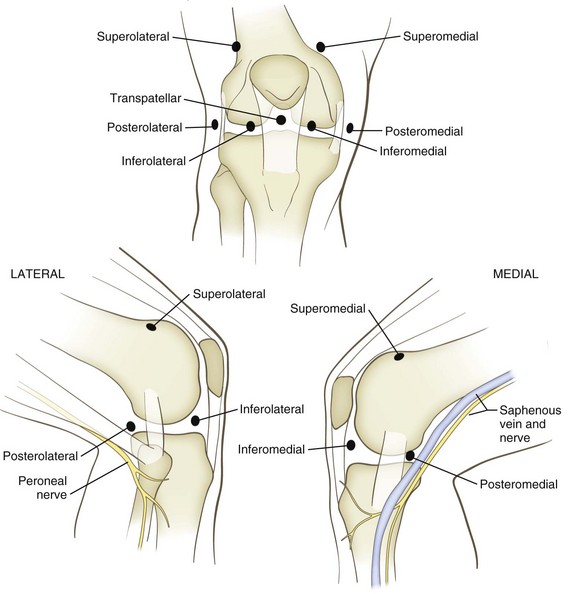
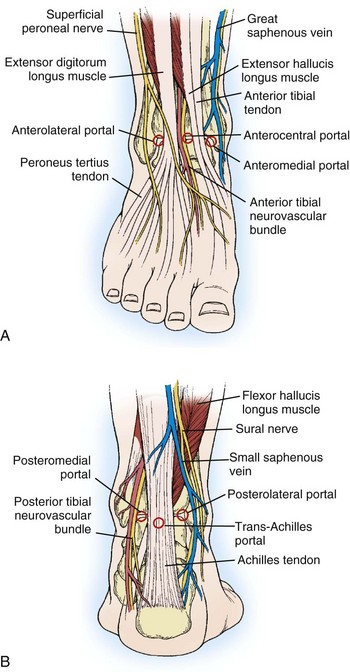
2. Accessory portals, sometimes helpful for visualizing the posterior horns of the menisci and PCL
 Posteromedial portal: 1 cm above the joint line behind the MCL (be careful to avoid saphenous nerve branches)
Posteromedial portal: 1 cm above the joint line behind the MCL (be careful to avoid saphenous nerve branches)
 Posterolateral portal: 1 cm above the joint line between the LCL and biceps tendon (avoiding the common peroneal nerve)
Posterolateral portal: 1 cm above the joint line between the LCL and biceps tendon (avoiding the common peroneal nerve)
 Transpatellar portal: 1 cm distal to the patella, splitting the patellar tendon fibers; can be used for central viewing or grabbing but should be avoided in patients who require subsequent harvesting of autogenous patellar tendon
Transpatellar portal: 1 cm distal to the patella, splitting the patellar tendon fibers; can be used for central viewing or grabbing but should be avoided in patients who require subsequent harvesting of autogenous patellar tendon
1. Each knee arthroscopy should include an evaluation of the suprapatellar pouch; patellofemoral joint and tracking; medial and lateral gutters; medial compartment, including the medial meniscus and the articular surface; the lateral compartment, including the lateral meniscus and the articular surface; and the intercondylar notch to visualize the ACL and PCL.
2. The posteromedial corner can be best visualized with a 70-degree arthroscope placed through the notch (modified Gillquist view) or a posteromedial portal.
 Meniscal tears are the most common injury to the knee that necessitates surgery.
Meniscal tears are the most common injury to the knee that necessitates surgery.
 The medial meniscus is torn approximately three times more often than the lateral meniscus.
The medial meniscus is torn approximately three times more often than the lateral meniscus.
 There is an increased rate of osteoarthritis in knees after both meniscal tears and meniscectomy.
There is an increased rate of osteoarthritis in knees after both meniscal tears and meniscectomy.
 Traumatic meniscal tears are common in young patients with sports-related injuries.
Traumatic meniscal tears are common in young patients with sports-related injuries.
 Degenerative tears usually occur in older patients and can have an insidious onset.
Degenerative tears usually occur in older patients and can have an insidious onset.
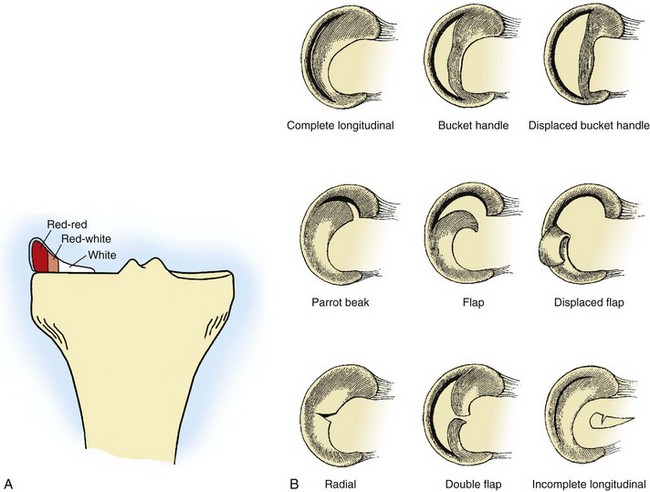
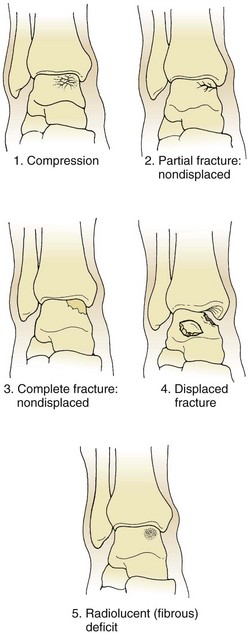
 Meniscal tears can be classified according to their location in relation to the vascular supply, their position (anterior, middle, or posterior third), and their appearance and orientation (Figure 4-10).
Meniscal tears can be classified according to their location in relation to the vascular supply, their position (anterior, middle, or posterior third), and their appearance and orientation (Figure 4-10).
 Meniscal root tears completely disrupt the circumferential fibers of the meniscus and can lead to meniscal extrusion.
Meniscal root tears completely disrupt the circumferential fibers of the meniscus and can lead to meniscal extrusion.
 The vascular supply of the meniscus is a primary determinant of healing potential.
The vascular supply of the meniscus is a primary determinant of healing potential.
 In the absence of intermittent swelling, catching, locking, or giving way, meniscal tears—particularly those degenerative in nature—may be treated conservatively.
In the absence of intermittent swelling, catching, locking, or giving way, meniscal tears—particularly those degenerative in nature—may be treated conservatively.
 Younger patients with acute tears, patients with tears causing mechanical symptoms, and patients with tears that fail to improve with conservative measures may benefit from operative treatment.
Younger patients with acute tears, patients with tears causing mechanical symptoms, and patients with tears that fail to improve with conservative measures may benefit from operative treatment.
 Tears that are not amenable to repair (e.g., peripheral, longitudinal tears)—excluding those that do not necessitate any treatment (e.g., partial-thickness tears, those <5 to 10 mm in length, and those that cannot be displaced >1 to 2 mm)—are best treated by partial meniscectomy.
Tears that are not amenable to repair (e.g., peripheral, longitudinal tears)—excluding those that do not necessitate any treatment (e.g., partial-thickness tears, those <5 to 10 mm in length, and those that cannot be displaced >1 to 2 mm)—are best treated by partial meniscectomy.
 In general, complex, degenerative, and central/radial tears are treated with resection of a minimal amount of normal meniscus. A motorized shaver is helpful for creating a smooth transition zone.
In general, complex, degenerative, and central/radial tears are treated with resection of a minimal amount of normal meniscus. A motorized shaver is helpful for creating a smooth transition zone.
 The role of lasers or other devices for this purpose is still under investigation. There is concern about possible iatrogenic chondral injury caused by lasers and other thermal devices.
The role of lasers or other devices for this purpose is still under investigation. There is concern about possible iatrogenic chondral injury caused by lasers and other thermal devices.
 Should be done for all peripheral longitudinal tears, especially in young patients and in conjunction with an ACL reconstruction
Should be done for all peripheral longitudinal tears, especially in young patients and in conjunction with an ACL reconstruction
 Augmentation techniques (fibrin clot, vascular access channels, synovial rasping) may extend the indications for repair.
Augmentation techniques (fibrin clot, vascular access channels, synovial rasping) may extend the indications for repair.
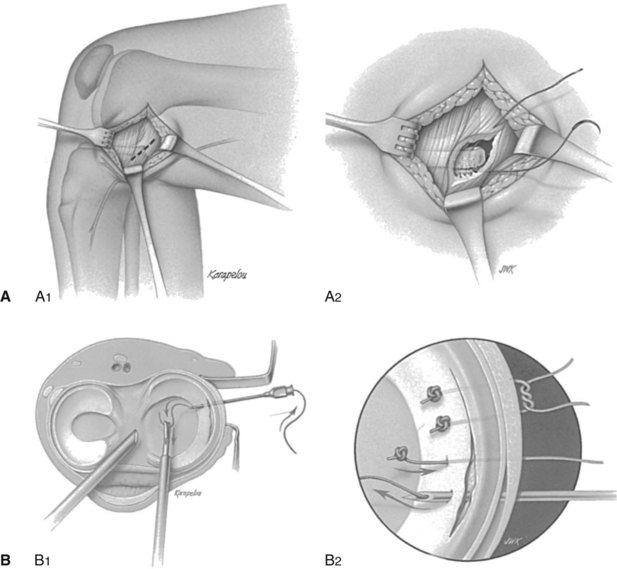
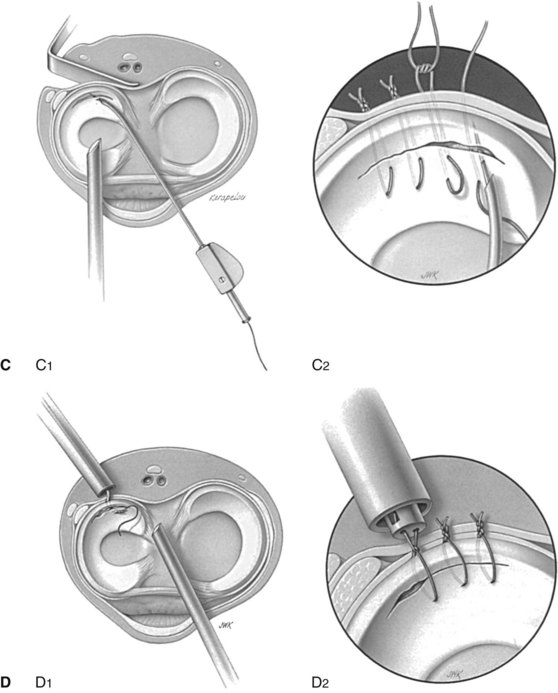
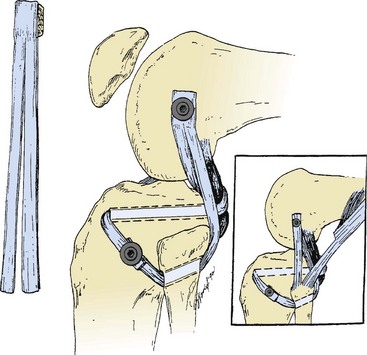
 Four techniques are commonly used: open, “outside-in,” “inside-out,” and “all-inside” (Figure 4-12).
Four techniques are commonly used: open, “outside-in,” “inside-out,” and “all-inside” (Figure 4-12).
 Newer techniques for all-inside repairs (e.g., arrows, darts, staples, screws) are popular because of their ease of use; however, they are probably not as reliable as vertical mattress sutures.
Newer techniques for all-inside repairs (e.g., arrows, darts, staples, screws) are popular because of their ease of use; however, they are probably not as reliable as vertical mattress sutures.
 The latest generation of “all-inside” devices allows tensioning of the construct.
The latest generation of “all-inside” devices allows tensioning of the construct.
 The “gold standard” for meniscal repair remains the inside-out technique with vertical mattress sutures.
The “gold standard” for meniscal repair remains the inside-out technique with vertical mattress sutures.
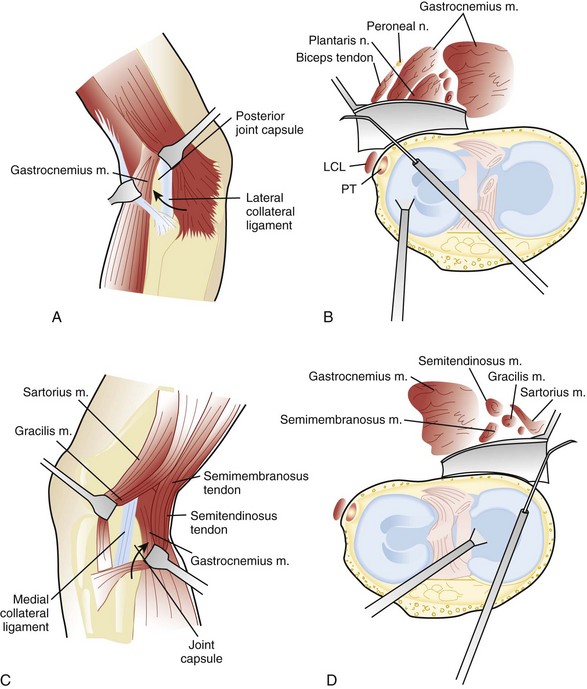
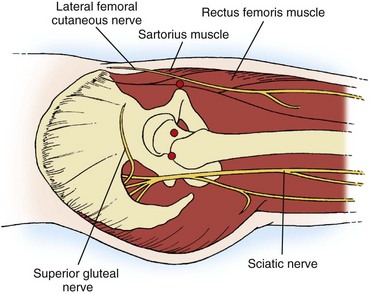
 Regardless of the technique used, it is essential to protect the saphenous nerve branches (anterior to both the semitendinosis and gracilis muscles and posterior to the inferior border of the sartorius muscle) during medial repairs and to protect the peroneal nerve (posterior to the biceps femoris) during lateral repairs (Figure 4-13).
Regardless of the technique used, it is essential to protect the saphenous nerve branches (anterior to both the semitendinosis and gracilis muscles and posterior to the inferior border of the sartorius muscle) during medial repairs and to protect the peroneal nerve (posterior to the biceps femoris) during lateral repairs (Figure 4-13).
 In several studies, 80% to 90% success rates with meniscal repairs have been reported. However, success depends on location, type of tear, and chronicity.
In several studies, 80% to 90% success rates with meniscal repairs have been reported. However, success depends on location, type of tear, and chronicity.
 It is generally accepted that the results of meniscal repair are best with acute peripheral tears in young patients with concurrent ACL reconstruction.
It is generally accepted that the results of meniscal repair are best with acute peripheral tears in young patients with concurrent ACL reconstruction.
 In general, success rates are 90% when meniscal repair is performed in conjunction with an ACL reconstruction, 60% with a repair in which the ACL is intact, and 30% with a repair in which the ACL is deficient.
In general, success rates are 90% when meniscal repair is performed in conjunction with an ACL reconstruction, 60% with a repair in which the ACL is intact, and 30% with a repair in which the ACL is deficient.
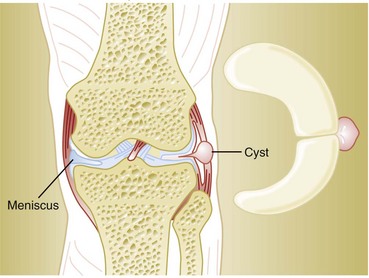
1. Occur primarily in conjunction with horizontal cleavage tears of the lateral meniscus (Figure 4-14)
2. Operative treatment consisting of arthroscopic partial meniscectomy and decompression through the tear (sometimes including “needling” of the cyst) has been shown to be effective.
3. En bloc excision is no longer favored for most meniscal cysts.
4. Popliteal (Baker) cysts are commonly related to meniscal disorders and usually resolve with treatment of the primary disorder.
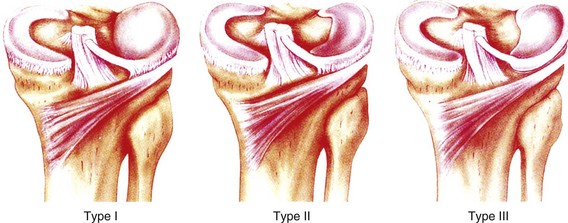
C Discoid menisci (“popping knee syndrome”)
1. Can be classified as (I) incomplete, (II) complete, or (III) the Wrisberg variant (Figure 4-15).
2. Patients may develop mechanical symptoms, or “popping,” with the knee in extension.
3. Plain radiographs may demonstrate a widened joint space, squaring of the lateral femoral condyle, cupping of the lateral tibial plateau, and a hypoplastic lateral intercondylar spine.
4. Appearance of a contiguous lateral meniscus on three consecutive sagittal images on MRI is diagnostic; MRI may also demonstrate associated tears. Treatment includes partial meniscectomy (saucerization) for tears, meniscal repair for peripheral detachments (Wrisberg variant), and simple observation for discoid menisci without tears.
1. Remains controversial but may be indicated for young patients who have had near-total meniscectomy (especially lateral meniscectomy) and who have early symptomatic chondrosis
2. Relative contraindications include diffuse grades III and IV chondral lesions, so-called kissing lesions (chondral lesions adjacent to each other on the femur and tibia), advanced age of patient, and joint space narrowing.
3. ACL deficiency, as well as limb alignment, must be addressed to increase the success rates of meniscal transplantation.
4. Graft size accurate to within 5% of the native meniscus is crucial for success.
5. Pain relief is the most consistent benefit; most studies have short-term to 5-year data available.
6. Three-phase bone scans can be used diagnostically in patients who fit inclusion criteria to help determine whether they are good surgical candidates. Allograft tissue needs to be appropriately sized and is typically harvested with a sterile technique, appropriately screened, and frozen.
7. Techniques for implantation include the use of individual bone plugs for the anterior and posterior horns and the use of a bone bridge, especially laterally.
8. Collagen meniscal implantation has yielded promising initial results for irreparable medial meniscal tears with new meniscus-like matrix formation, in comparison with partial meniscectomy. However, long-term results, especially by independent sources, have not been reported.
 Controversy continues with regard to the development of late arthritis in ACL-deficient versus reconstructed knees.
Controversy continues with regard to the development of late arthritis in ACL-deficient versus reconstructed knees.
 Chronic ACL deficiency is associated with a higher incidence of complex meniscal tears not amenable to repair and chondral injury.
Chronic ACL deficiency is associated with a higher incidence of complex meniscal tears not amenable to repair and chondral injury.
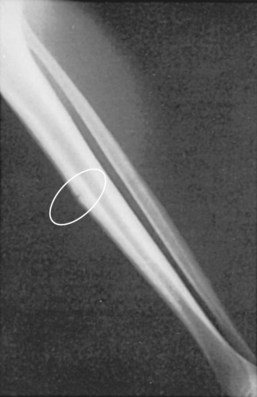
 Bone bruises (trabecular microfractures) occur in more than half of acute ACL injuries.
Bone bruises (trabecular microfractures) occur in more than half of acute ACL injuries.
 Bone bruises are typically located near the sulcus terminalis on the lateral femoral condyle and the posterolateral aspect of the tibia.
Bone bruises are typically located near the sulcus terminalis on the lateral femoral condyle and the posterolateral aspect of the tibia.
 Although the long-term significance of these injuries is unknown, they may be related to late cartilage degeneration.
Although the long-term significance of these injuries is unknown, they may be related to late cartilage degeneration.
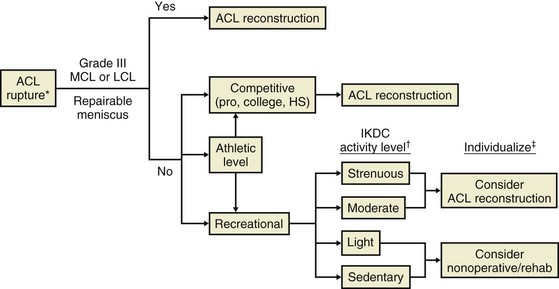
 Treatment decisions should be individualized on the basis of age, activity level, instability, associated injuries, and other medical factors (Figure 4-16).
Treatment decisions should be individualized on the basis of age, activity level, instability, associated injuries, and other medical factors (Figure 4-16).
 The ACL injury rate is higher in women than in men.
The ACL injury rate is higher in women than in men.
 This higher rate is thought to occur because women have smaller notches, smaller ligaments, increased generalized ligament laxity, increased knee laxity, and different landing biomechanics.
This higher rate is thought to occur because women have smaller notches, smaller ligaments, increased generalized ligament laxity, increased knee laxity, and different landing biomechanics.
 The in situ force of the ACL is highest at 30 degrees of flexion in response to anterior tibial load.
The in situ force of the ACL is highest at 30 degrees of flexion in response to anterior tibial load.
 ACL injury prevention programs emphasize proprioceptive training and the strengthening of knee flexors.
ACL injury prevention programs emphasize proprioceptive training and the strengthening of knee flexors.
2. History and physical examination
 ACL injuries are often the result of noncontact pivoting injuries.
ACL injuries are often the result of noncontact pivoting injuries.
 They are commonly associated with an audible “pop” and an immediate hemarthrosis.
They are commonly associated with an audible “pop” and an immediate hemarthrosis.
 Associated injuries, including meniscal tears (75%), are common.
Associated injuries, including meniscal tears (75%), are common.
 Acute lateral meniscal tears are more common than acute medial tears, whereas medial tears occur more often with chronic ACL deficiency.
Acute lateral meniscal tears are more common than acute medial tears, whereas medial tears occur more often with chronic ACL deficiency.
 The Lachman test is the most sensitive examination for acute ACL injuries.
The Lachman test is the most sensitive examination for acute ACL injuries.
 Performance on the pivot shift test is most closely correlated with outcome after ACL reconstruction.
Performance on the pivot shift test is most closely correlated with outcome after ACL reconstruction.
 This test is also helpful in evaluating an ACL-deficient knee, especially in an examination with the patient under anesthesia.
This test is also helpful in evaluating an ACL-deficient knee, especially in an examination with the patient under anesthesia.
 The KT-1000 and KT-2000 Knee Ligament Arthrometers are useful in quantifying laxity.
The KT-1000 and KT-2000 Knee Ligament Arthrometers are useful in quantifying laxity.
 Initial management consists of physical therapy for mobilization. Immobilization is avoided.
Initial management consists of physical therapy for mobilization. Immobilization is avoided.
 Intraarticular reconstruction is currently favored for patients who meet the criteria indicated in Figure 4-15.
Intraarticular reconstruction is currently favored for patients who meet the criteria indicated in Figure 4-15.
 Graft selection depends on patient’s factors and surgeon’s preference and usually includes (1) a bone-patella, tendon-bone (BPTB) autograft; (2) a four-strand hamstring autograft, (3) a quadriceps tendon autograft, and (4) an allograft.
Graft selection depends on patient’s factors and surgeon’s preference and usually includes (1) a bone-patella, tendon-bone (BPTB) autograft; (2) a four-strand hamstring autograft, (3) a quadriceps tendon autograft, and (4) an allograft.
 BPTB demonstrates faster incorporation into the bone tunnels than does hamstring autograft and, for the authors, is often the graft of choice for patients who desire an early return to sports activity.
BPTB demonstrates faster incorporation into the bone tunnels than does hamstring autograft and, for the authors, is often the graft of choice for patients who desire an early return to sports activity.
 Several studies have, however, demonstrated a higher incidence of arthritis associated with the use of BPTB autograft than with hamstring autograft 5 to 7 years after ACL reconstruction.
Several studies have, however, demonstrated a higher incidence of arthritis associated with the use of BPTB autograft than with hamstring autograft 5 to 7 years after ACL reconstruction.
 Primary repair of ACL tears is not currently recommended.
Primary repair of ACL tears is not currently recommended.
 Significant controversy exists regarding the double-bundle ACL reconstruction.
Significant controversy exists regarding the double-bundle ACL reconstruction.
 Single-bundle reconstruction is still the most commonly performed reconstruction.
Single-bundle reconstruction is still the most commonly performed reconstruction.
 Placement of a more horizontal femoral tunnel (10 or 2 o’clock position) to center the graft in the middle of the femoral ACL footprint has been the focus of newer anteromedial or “far medial” portal drilling techniques (in contrast to traditional transtibial-femoral drilling techniques).
Placement of a more horizontal femoral tunnel (10 or 2 o’clock position) to center the graft in the middle of the femoral ACL footprint has been the focus of newer anteromedial or “far medial” portal drilling techniques (in contrast to traditional transtibial-femoral drilling techniques).
 The existence and treatment of “partial” ACL tears are controversial, although clinical examination and functional stability remain the most important considerations in determining the need for reconstruction.
The existence and treatment of “partial” ACL tears are controversial, although clinical examination and functional stability remain the most important considerations in determining the need for reconstruction.
 Single-bundle tears can occur and may be addressed with reconstruction of the injured bundle and preservation of the intact bundle.
Single-bundle tears can occur and may be addressed with reconstruction of the injured bundle and preservation of the intact bundle.
6. Postoperative rehabilitation
 Rehabilitation has evolved, and early motion (emphasis on extension) and weight bearing are encouraged in most protocols.
Rehabilitation has evolved, and early motion (emphasis on extension) and weight bearing are encouraged in most protocols.
 Closed-chain rehabilitation (fixation of the terminal segment of extremity) and compressive loading have been emphasized because they allow physiologic co-contraction of the muscles around the knee.
Closed-chain rehabilitation (fixation of the terminal segment of extremity) and compressive loading have been emphasized because they allow physiologic co-contraction of the muscles around the knee.
 Open-chain extension exercises place increased stress on the reconstructed ACL and should be avoided for the first 6 weeks.
Open-chain extension exercises place increased stress on the reconstructed ACL and should be avoided for the first 6 weeks.
 No difference in outcome has been found between accelerated and nonaccelerated rehabilitation programs.
No difference in outcome has been found between accelerated and nonaccelerated rehabilitation programs.
 Postoperative bracing has not proved beneficial after ACL reconstruction except in downhill skiers.
Postoperative bracing has not proved beneficial after ACL reconstruction except in downhill skiers.
 Early progressive eccentric exercise has yielded good initial results in terms of quadriceps and gluteus maximus muscle size and function after ACL reconstruction.
Early progressive eccentric exercise has yielded good initial results in terms of quadriceps and gluteus maximus muscle size and function after ACL reconstruction.
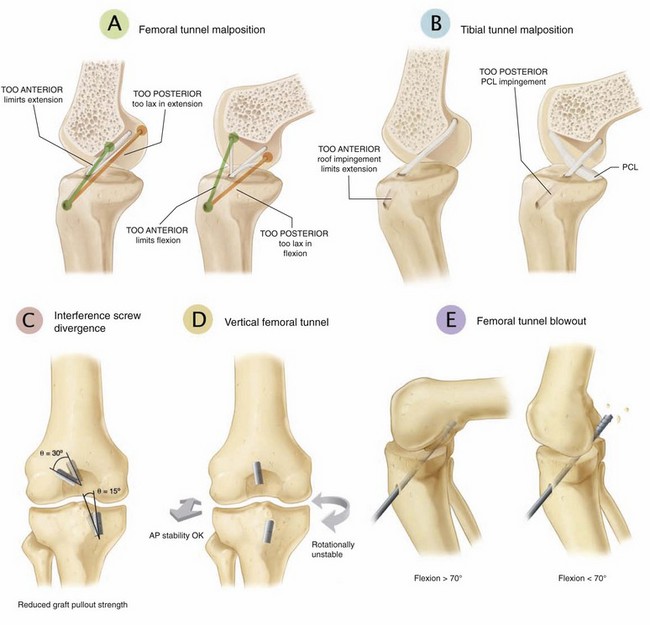
 Complications in ACL surgery are usually a result of aberrant tunnel placement.
Complications in ACL surgery are usually a result of aberrant tunnel placement.
 The most common technical error is placement of the femoral tunnel too far anteriorly, which results in limited flexion.
The most common technical error is placement of the femoral tunnel too far anteriorly, which results in limited flexion.
 Vertical graft placement results in decreased rotational stability.
Vertical graft placement results in decreased rotational stability.
 Arthrofibrosis often occurs with reconstruction for acute ACL tears.
Arthrofibrosis often occurs with reconstruction for acute ACL tears.
 Aberrant hardware placement (interference screw divergence of >30 degrees [for endoscopic femoral tunnels] and >15 degrees [for tibial tunnels]) can also result in complications.
Aberrant hardware placement (interference screw divergence of >30 degrees [for endoscopic femoral tunnels] and >15 degrees [for tibial tunnels]) can also result in complications.
 BPTB autograft harvest carries the risk of anterior knee pain, pain with kneeling, loss of extension, and poorer recovery of quadriceps strength.
BPTB autograft harvest carries the risk of anterior knee pain, pain with kneeling, loss of extension, and poorer recovery of quadriceps strength.
 Hamstring autograft harvest carries the risk of weakness of knee flexion and internal rotation, along with injury to branches of the saphenous nerve.
Hamstring autograft harvest carries the risk of weakness of knee flexion and internal rotation, along with injury to branches of the saphenous nerve.
 Use of a horizontal incision at the harvest site decreases the risk of damaging the infrapatellar branch of the saphenous nerve.
Use of a horizontal incision at the harvest site decreases the risk of damaging the infrapatellar branch of the saphenous nerve.
 The use of allograft with ACL reconstruction in younger, more active patients may be associated with a higher rate of rerupture.
The use of allograft with ACL reconstruction in younger, more active patients may be associated with a higher rate of rerupture.
 Injuries occur most commonly as a result of a direct blow to the anterior tibia with the knee flexed (the “dashboard injury”), with hyperflexion, or with hyperextension.
Injuries occur most commonly as a result of a direct blow to the anterior tibia with the knee flexed (the “dashboard injury”), with hyperflexion, or with hyperextension.
 A fall onto the ground with a plantar-flexed foot is also a mechanism of injury for PCL tears.
A fall onto the ground with a plantar-flexed foot is also a mechanism of injury for PCL tears.
2. Physical examination and classification
 The key examination is the posterior drawer test; diagnostic results are an absent or posteriorly directed tibial step-off.
The key examination is the posterior drawer test; diagnostic results are an absent or posteriorly directed tibial step-off.
 Grade I injury: an isolated PCL injury in which the tibia remains anterior to the femoral condyles
Grade I injury: an isolated PCL injury in which the tibia remains anterior to the femoral condyles
 Grade II injury: an isolated, complete PCL injury in which the anterior tibia becomes flush with the femoral condyles
Grade II injury: an isolated, complete PCL injury in which the anterior tibia becomes flush with the femoral condyles
 Grade III injury: an injury in which the tibia is posterior to the femoral condyles and is usually indicative of associated ACL or PLC injuries or both
Grade III injury: an injury in which the tibia is posterior to the femoral condyles and is usually indicative of associated ACL or PLC injuries or both
 Plain radiographs should be obtained to evaluate for avulsion injuries (acute) and arthrosis of the medial and patellofemoral compartments (chronic).
Plain radiographs should be obtained to evaluate for avulsion injuries (acute) and arthrosis of the medial and patellofemoral compartments (chronic).
 Stress radiographs are becoming the standard for evaluation and grading of PCL injuries; side-to-side differences of more than 12 mm on stress radiographs are suggestive of a combined PCL and PLC injury.
Stress radiographs are becoming the standard for evaluation and grading of PCL injuries; side-to-side differences of more than 12 mm on stress radiographs are suggestive of a combined PCL and PLC injury.
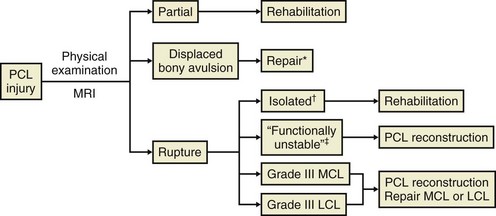
 Nonoperative treatment is favored for most grades I and II (isolated) PCL injuries.
Nonoperative treatment is favored for most grades I and II (isolated) PCL injuries.
 Grade III injuries are indicative of a combined injury, usually to the posterolateral corner.
Grade III injuries are indicative of a combined injury, usually to the posterolateral corner.
 Bony avulsion fractures can be repaired primarily with good results, although primary repair of midsubstance PCL (and ACL) injuries has not been successful.
Bony avulsion fractures can be repaired primarily with good results, although primary repair of midsubstance PCL (and ACL) injuries has not been successful.
 Chronic PCL deficiency can result in late chondrosis of the patellofemoral compartment or medial femoral condyle, or both.
Chronic PCL deficiency can result in late chondrosis of the patellofemoral compartment or medial femoral condyle, or both.
 PCL reconstruction is recommended for functionally unstable or combined injuries (Figure 4-17).
PCL reconstruction is recommended for functionally unstable or combined injuries (Figure 4-17).
 In general, the results of PCL reconstruction are not as good as those of ACL reconstruction, and some residual posterior laxity often remains.
In general, the results of PCL reconstruction are not as good as those of ACL reconstruction, and some residual posterior laxity often remains.
 For successful reconstruction, concomitant ligament injuries must be addressed.
For successful reconstruction, concomitant ligament injuries must be addressed.
 Many techniques for PCL reconstruction have been published, and they can generally be divided into tibial inlay versus transtibial methods and single-bundle versus double-bundle methods.
Many techniques for PCL reconstruction have been published, and they can generally be divided into tibial inlay versus transtibial methods and single-bundle versus double-bundle methods.
 Single-bundle reconstructions should be tensioned in 90 degrees of flexion.
Single-bundle reconstructions should be tensioned in 90 degrees of flexion.
 Tibial inlay has biomechanical advantages, such as a decrease in the “killer turn” and decreased attenuation of the graft.
Tibial inlay has biomechanical advantages, such as a decrease in the “killer turn” and decreased attenuation of the graft.
 In the tibial inlay technique, the average distance from screws used for fixation to the popliteal artery is 20 mm.
In the tibial inlay technique, the average distance from screws used for fixation to the popliteal artery is 20 mm.
 Double-bundle techniques may improve biomechanical function in both extension and flexion, but a clinical advantage to those techniques has not yet been shown.
Double-bundle techniques may improve biomechanical function in both extension and flexion, but a clinical advantage to those techniques has not yet been shown.
 History and physical examination
History and physical examination
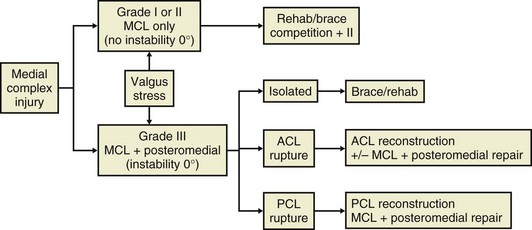
 MCL injury occurs as a result of valgus stress to the knee.
MCL injury occurs as a result of valgus stress to the knee.
 Pain and instability with valgus stress testing at 30 degrees of flexion (and not in full extension) is diagnostic.
Pain and instability with valgus stress testing at 30 degrees of flexion (and not in full extension) is diagnostic.
 Opening in full extension usually signifies other concurrent injuries (ACL and PCL).
Opening in full extension usually signifies other concurrent injuries (ACL and PCL).
 Injuries most commonly occur at the femoral insertion of the ligament.
Injuries most commonly occur at the femoral insertion of the ligament.
 Nonoperative treatment (hinged knee brace) is highly successful in alleviating isolated MCL injuries.
Nonoperative treatment (hinged knee brace) is highly successful in alleviating isolated MCL injuries.
 Clinical work has shown the advantage of nonoperative treatment (bracing) of an associated MCL injury in patients receiving an ACL reconstruction.
Clinical work has shown the advantage of nonoperative treatment (bracing) of an associated MCL injury in patients receiving an ACL reconstruction.
 Distal injuries have less healing potential than do proximal injuries.
Distal injuries have less healing potential than do proximal injuries.
 Prophylactic bracing may be helpful for football players, especially interior linemen.
Prophylactic bracing may be helpful for football players, especially interior linemen.
 Advancement and reinforcement of the ligament are rarely necessary for chronic injuries that do not respond to conservative treatment (Figure 4-18).
Advancement and reinforcement of the ligament are rarely necessary for chronic injuries that do not respond to conservative treatment (Figure 4-18).
 In chronic injuries, calcification may be present at the medial femoral condyle insertion (Pellegrini-Stieda sign).
In chronic injuries, calcification may be present at the medial femoral condyle insertion (Pellegrini-Stieda sign).
 Pellegrini-Stieda syndrome, which can occur with chronic MCL injury, usually responds to a brief period of immobilization followed by progressive motion.
Pellegrini-Stieda syndrome, which can occur with chronic MCL injury, usually responds to a brief period of immobilization followed by progressive motion.
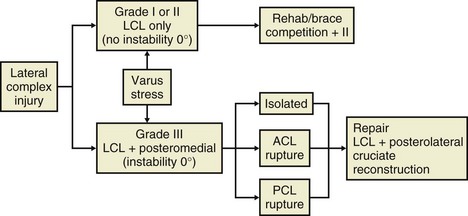
D Posterolateral corner injury
 Rarely isolated and are usually associated with other ligamentous injuries (especially those of the PCL)
Rarely isolated and are usually associated with other ligamentous injuries (especially those of the PCL)
 Because of poor results with reconstructions with chronic injury, repair of acute injury combined with reconstruction is advocated.
Because of poor results with reconstructions with chronic injury, repair of acute injury combined with reconstruction is advocated.
 Examination for increased external rotation (dial test), the external rotation recurvatum test, the posterolateral drawer test, and the reverse pivot shift test are important (see Table 4-5).
Examination for increased external rotation (dial test), the external rotation recurvatum test, the posterolateral drawer test, and the reverse pivot shift test are important (see Table 4-5).
 Long-leg standing radiographs are necessary, especially with chronic injuries, to determine mechanical axis and whether a proximal tibial osteotomy is necessary for varus correction.
Long-leg standing radiographs are necessary, especially with chronic injuries, to determine mechanical axis and whether a proximal tibial osteotomy is necessary for varus correction.
 Evaluation for triple varus alignment should always be performed.
Evaluation for triple varus alignment should always be performed.
 Early anatomic repair is often successful, but these injuries are frequently missed.
Early anatomic repair is often successful, but these injuries are frequently missed.
 Procedures recommended for chronic injuries include posterolateral corner advancement (only if structures are attenuated but intact); popliteal bypass (not currently favored); two- and three-tailed reconstruction; biceps tenodesis; and (more recent) “split” grafts and anatomic reconstructions, which are used to reconstruct both the LCL and the popliteal/posterolateral corner (Figures 4-20 and 4-21).
Procedures recommended for chronic injuries include posterolateral corner advancement (only if structures are attenuated but intact); popliteal bypass (not currently favored); two- and three-tailed reconstruction; biceps tenodesis; and (more recent) “split” grafts and anatomic reconstructions, which are used to reconstruct both the LCL and the popliteal/posterolateral corner (Figures 4-20 and 4-21).
 The treatment of choice for chronic PLC injuries is often a valgus opening wedge osteotomy.
The treatment of choice for chronic PLC injuries is often a valgus opening wedge osteotomy.
1. History and physical examination
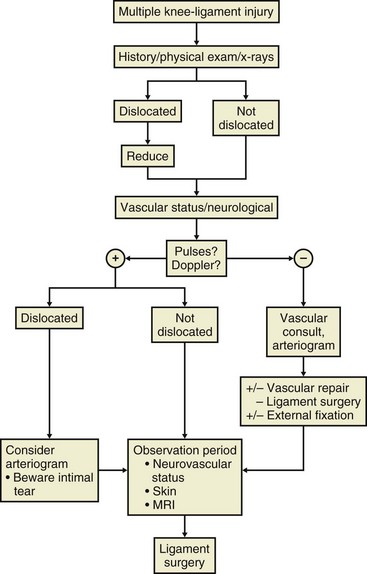
 Combined ligamentous injuries (especially ACL-PCL injuries) can be a result of a knee dislocation, and neurovascular injury must be suspected (Table 4-7).
Combined ligamentous injuries (especially ACL-PCL injuries) can be a result of a knee dislocation, and neurovascular injury must be suspected (Table 4-7).
Table 4-7
Schenck Classification of Knee Dislocations
| Classification | Ligaments Affected |
| KDI | ACL + either MCL or LCL or PCL + either MCL or LCL |
| KDII | ACL + PCL |
| KDIII | ACL + PCL + one collateral ligament |
| KDIIIM | MCL |
| KDIIIL | LCL |
| KDIV | ACL + PCL + MCL + LCL |
Data from SchenK RC, Jr: The dislocated knee, Instr Course Lect 43: 127–136, 1994.
 The incidence of vascular injury after anterior knee dislocation is 30% to 50%.
The incidence of vascular injury after anterior knee dislocation is 30% to 50%.
 Liberal use of vascular studies is recommended early (Figure 4-22).
Liberal use of vascular studies is recommended early (Figure 4-22).
 In one study by Stannard et al (2004) serial examinations—including ankle-brachial index exceeding 90% over 48 hours—were used to determine whether arteriography was necessary. The authors noted success with this technique and noted that a four-ligament injury was associated with a higher rate of vascular injury.
In one study by Stannard et al (2004) serial examinations—including ankle-brachial index exceeding 90% over 48 hours—were used to determine whether arteriography was necessary. The authors noted success with this technique and noted that a four-ligament injury was associated with a higher rate of vascular injury.
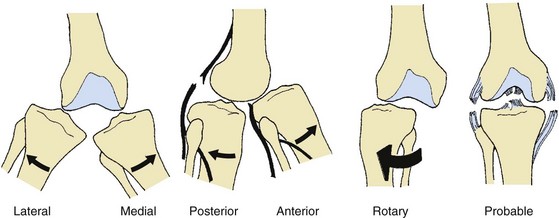
 Dislocations are classified on the basis of the direction of tibial displacement (Figure 4-23).
Dislocations are classified on the basis of the direction of tibial displacement (Figure 4-23).
 Initial treatment involves immediate reduction and neurovascular examination.
Initial treatment involves immediate reduction and neurovascular examination.
 Definitive treatment is usually operative.
Definitive treatment is usually operative.
 Emergency surgical indications include popliteal artery injury, compartment syndrome, open dislocations, and irreducible dislocations.
Emergency surgical indications include popliteal artery injury, compartment syndrome, open dislocations, and irreducible dislocations.
 Most surgeons recommend delaying surgery 1 to 2 weeks to ensure that no vascular injury occurs.
Most surgeons recommend delaying surgery 1 to 2 weeks to ensure that no vascular injury occurs.
 The use of the arthroscope, especially with a pump, must be limited during these procedures because of the risk of fluid extravasation. Avulsion injuries can be repaired primarily; however, interstitial injuries must be reconstructed.
The use of the arthroscope, especially with a pump, must be limited during these procedures because of the risk of fluid extravasation. Avulsion injuries can be repaired primarily; however, interstitial injuries must be reconstructed.
 The incidence of stiff knee after these combined procedures is high; early motion is crucial for avoiding it.
The incidence of stiff knee after these combined procedures is high; early motion is crucial for avoiding it.
 According to a meta-analysis, staged treatment might have produced better subjective outcomes but, like acute treatment, was associated with additional procedures to treat joint stiffness. Early mobility was associated with better subjective outcomes than was immobilization after acute surgical treatment.
According to a meta-analysis, staged treatment might have produced better subjective outcomes but, like acute treatment, was associated with additional procedures to treat joint stiffness. Early mobility was associated with better subjective outcomes than was immobilization after acute surgical treatment.
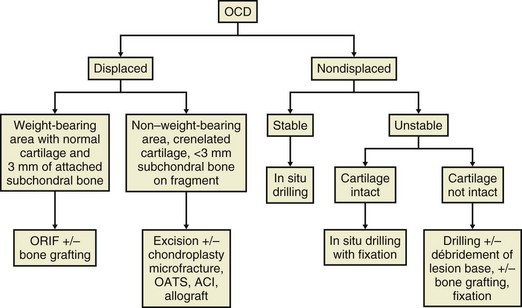
 Involves subchondral bone and overlying cartilage separation, probably as a result of occult trauma
Involves subchondral bone and overlying cartilage separation, probably as a result of occult trauma
 Most often involves the lateral aspect of the medial femoral condyle
Most often involves the lateral aspect of the medial femoral condyle
 The lateral femoral condyle is involved in 15% to 20% of cases; the patella is rarely involved.
The lateral femoral condyle is involved in 15% to 20% of cases; the patella is rarely involved.
 The condition resolves spontaneously in the majority of the juvenile cases, in about 50% of adolescents, and rarely in adults.
The condition resolves spontaneously in the majority of the juvenile cases, in about 50% of adolescents, and rarely in adults.
 Patients usually have poorly localized, vague complaints. Radiographs, nuclear imaging, and MRI can be helpful in determining the size, location, and characteristics of the lesion.
Patients usually have poorly localized, vague complaints. Radiographs, nuclear imaging, and MRI can be helpful in determining the size, location, and characteristics of the lesion.
 Children with open growth plates have the best prognosis, and often these lesions can be simply observed.
Children with open growth plates have the best prognosis, and often these lesions can be simply observed.
 In situ lesions can be treated with retrograde drilling.
In situ lesions can be treated with retrograde drilling.
 Detached lesions may necessitate abrasion chondroplasty or newer, more aggressive techniques.
Detached lesions may necessitate abrasion chondroplasty or newer, more aggressive techniques.
 Osteochondritis dissecans in adults is usually symptomatic and leads to arthritis if left untreated.
Osteochondritis dissecans in adults is usually symptomatic and leads to arthritis if left untreated.
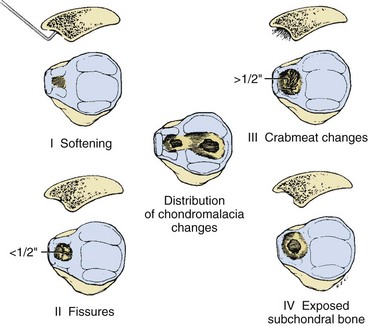
 The distinction between articular cartilage injury and osteochondritis dissecans is not often clear, but articular cartilage injury occurs as a result of rotational forces in direct trauma. It usually occurs on the medial femoral condyle. The lesions are classified according to their arthroscopic appearance.
The distinction between articular cartilage injury and osteochondritis dissecans is not often clear, but articular cartilage injury occurs as a result of rotational forces in direct trauma. It usually occurs on the medial femoral condyle. The lesions are classified according to their arthroscopic appearance.
 Débridement and chondroplasty are currently recommended for symptomatic lesions.
Débridement and chondroplasty are currently recommended for symptomatic lesions.
 Displaced osteochondral fragments can sometimes be replaced and secured with small, recessed screws or absorbable pins.
Displaced osteochondral fragments can sometimes be replaced and secured with small, recessed screws or absorbable pins.
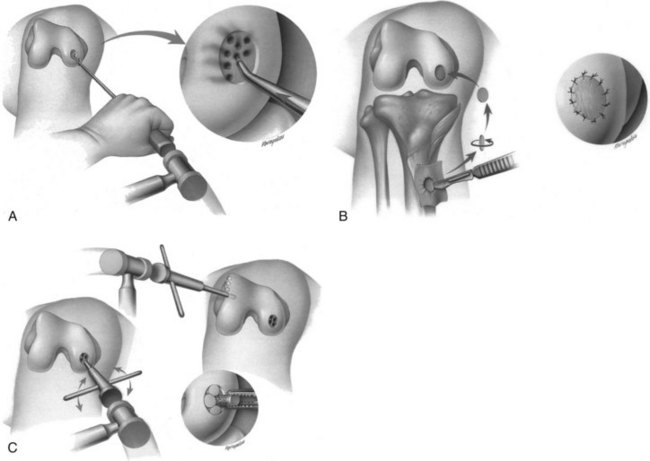
 For discrete, isolated, full-thickness cartilage injuries, several treatment options are in clinical use: microfracture, periosteal patches (chondrocyte implantation), and osteochondral transfer (plugs), including autograft and allograft options (Figure 4-24).
For discrete, isolated, full-thickness cartilage injuries, several treatment options are in clinical use: microfracture, periosteal patches (chondrocyte implantation), and osteochondral transfer (plugs), including autograft and allograft options (Figure 4-24).
 Donor-site problems and the creation of true articular cartilage at the recipient site are still challenges.
Donor-site problems and the creation of true articular cartilage at the recipient site are still challenges.
 Age, lesion size, patient’s desired activity level, alignment, meniscal integrity, and ligamentous stability must all be taken into consideration in selecting the appropriate treatment option. An algorithm is presented in Figure 4-25.
Age, lesion size, patient’s desired activity level, alignment, meniscal integrity, and ligamentous stability must all be taken into consideration in selecting the appropriate treatment option. An algorithm is presented in Figure 4-25.
 Marrow-stimulating techniques—including microfracture, drilling, and abrasion arthroplasty—involve perforation of the subchondral bone after removal of the “tidemark” cartilage with eventual clot formation and fibrocartilaginous repair tissue (type I collagen with inferior wear characteristics). Good clinical results in small defects (<4 cm2) are obtained in 60% to 80% patients.
Marrow-stimulating techniques—including microfracture, drilling, and abrasion arthroplasty—involve perforation of the subchondral bone after removal of the “tidemark” cartilage with eventual clot formation and fibrocartilaginous repair tissue (type I collagen with inferior wear characteristics). Good clinical results in small defects (<4 cm2) are obtained in 60% to 80% patients.
 Autologous chondrocyte implantation allows for the creation of type II–rich hyaline-like cartilage. It is indicated for medium-sized to larger chondral lesions without bony defects. Multiple surgical procedures are required for biopsy/harvest and then definitive repair. Complications related to autologous chondrocyte implantation include chondrocyte overgrowth and periosteal flap hypertrophy along with the morbidity of the second surgical procedure.
Autologous chondrocyte implantation allows for the creation of type II–rich hyaline-like cartilage. It is indicated for medium-sized to larger chondral lesions without bony defects. Multiple surgical procedures are required for biopsy/harvest and then definitive repair. Complications related to autologous chondrocyte implantation include chondrocyte overgrowth and periosteal flap hypertrophy along with the morbidity of the second surgical procedure.
 Osteochondral autografts (i.e., osteochondral autograft transplantation, mosaicplasty) can be used to address medium-sized lesions (3 cm2) that include subchondral bone loss. Complications include donor site morbidity.
Osteochondral autografts (i.e., osteochondral autograft transplantation, mosaicplasty) can be used to address medium-sized lesions (3 cm2) that include subchondral bone loss. Complications include donor site morbidity.
 Osteochondral allografts can be used for larger lesions, especially with bone loss. The main concerns include the small risk of disease transmission and condrocyte viability, which has improved with graft preservation techniques (storage at 4° C).
Osteochondral allografts can be used for larger lesions, especially with bone loss. The main concerns include the small risk of disease transmission and condrocyte viability, which has improved with graft preservation techniques (storage at 4° C).
1. Diffuse chondral damage is usually not considered “sports medicine,” but treatment modalities include medications, nutritional supplements such as glucosamine with chondroitin sulfate, hyaluronic acid injections, arthroscopic débridement, osteotomies, and arthroplasty. These treatment modalities are addressed in detail in Chapter 5, Adult Reconstruction.
1. Atraumatic osteonecrosis is similar to idiopathic osteonecrosis of the hip. Risk factors are similar to those of the hip and are common in elderly women.
2. Spontaneous osteonecrosis of the knee is thought to represent a subchondral insufficiency fracture and is typically a self-limiting condition. This condition can follow knee arthroscopy in middle-aged women. It should be treated with limited weight bearing until it resolves.
3. One hypothesis for the cause of spontaneous osteonecrosis of the knee involves a meniscal root tear.
A Pigmented villonodular synovitis
1. Affected patients may present with pain and swelling and may have a palpable mass.
2. MRI demonstrates intraarticular nodular masses of low signal intensity on T1- and T2-weighted images.
1. This proliferative disease of the synovium is associated with cartilaginous metaplasia, which results in multiple intraarticular loose bodies.
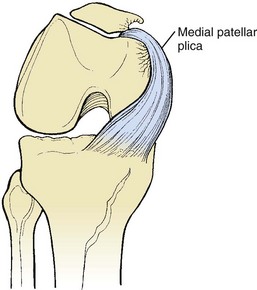
1. Synovial folds that are embryologic remnants
2. They are occasionally pathologic, particularly the medial patellar plica, which can cause abrasion of the medial femoral condyle and sometimes responds to arthroscopic excision (Figure 4-26).
D Other synovial lesions that respond to synovectomy include chondromatosis, osteochondromatosis, pauciarticular juvenile rheumatoid arthritis, and hemophilia. Additional arthroscopic portals are required for complete synovectomy.
1. Anterior knee pain is classified based on etiologic factors (Box 4-1). The term chondromalacia should be replaced with a specific diagnosis that is based on this classification.
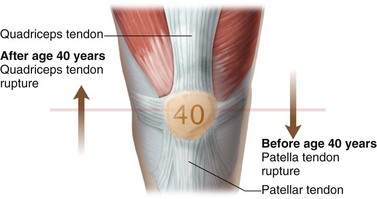
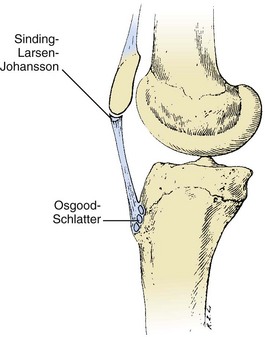
1. Includes fractures of the patella (discussed in Chapter 11, Trauma) and tendon injuries (Figure 4-27).
 Quadriceps tendon ruptures are more common than patellar tendon ruptures and occur most often with indirect trauma in patients older than 40 years. In younger patients, patellar tendon ruptures occur with direct or indirect trauma.
Quadriceps tendon ruptures are more common than patellar tendon ruptures and occur most often with indirect trauma in patients older than 40 years. In younger patients, patellar tendon ruptures occur with direct or indirect trauma.
 Both types of tendon rupture are more common in patients with underlying disorders of the tendon.
Both types of tendon rupture are more common in patients with underlying disorders of the tendon.
 A palpable defect and the inability to extend the knee are diagnostic signs.
A palpable defect and the inability to extend the knee are diagnostic signs.
 Patella alta is a consistent finding with patella tendon rupture.
Patella alta is a consistent finding with patella tendon rupture.
 Primary repair with temporary stabilization (McLaughlin wire or suture) is indicated.
Primary repair with temporary stabilization (McLaughlin wire or suture) is indicated.
3. Repetitive trauma: overuse injuries
 Patellar tendinitis (jumper’s knee)
Patellar tendinitis (jumper’s knee)
 This condition is perhaps better termed tendinosis.
This condition is perhaps better termed tendinosis.
 Most common in athletes who participate in sports such as basketball and volleyball
Most common in athletes who participate in sports such as basketball and volleyball
 Associated with pain and tenderness near the inferior border of the patella (worse in extension than in flexion)
Associated with pain and tenderness near the inferior border of the patella (worse in extension than in flexion)
 Treatment includes nonsteroidal anti-inflammatory drugs (NSAIDs), physical therapy (strengthening including eccentric exercise and ultrasonography), and orthoses (patella tendon strap).
Treatment includes nonsteroidal anti-inflammatory drugs (NSAIDs), physical therapy (strengthening including eccentric exercise and ultrasonography), and orthoses (patella tendon strap).
 Surgery involving excision of necrotic tendon fibers is rarely indicated.
Surgery involving excision of necrotic tendon fibers is rarely indicated.
 Less common than patella tendinosis but just as painful
Less common than patella tendinosis but just as painful
 Patients may note painful clicking and localized pain at the superior border of the patella.
Patients may note painful clicking and localized pain at the superior border of the patella.
 Prepatellar bursitis (housemaid’s knee)
Prepatellar bursitis (housemaid’s knee)
 The most common form of bursitis of the knee and associated with a history of prolonged kneeling
The most common form of bursitis of the knee and associated with a history of prolonged kneeling
 Supportive treatment (knee pads, occasional steroid injections) and, in rare cases, bursal excision are recommended.
Supportive treatment (knee pads, occasional steroid injections) and, in rare cases, bursal excision are recommended.
 Aspiration is advocated in wrestlers to rule out infection because wrestling requires kneeling on the flexed knee.
Aspiration is advocated in wrestlers to rule out infection because wrestling requires kneeling on the flexed knee.
 Iliotibial band friction syndrome
Iliotibial band friction syndrome
 Can occur in runners (especially those running hills) and cyclists
Can occur in runners (especially those running hills) and cyclists
 Result of abrasion between the iliotibial band and the lateral femoral condyle
Result of abrasion between the iliotibial band and the lateral femoral condyle
 Localized tenderness, worse with the knee flexed 30 degrees, is common.
Localized tenderness, worse with the knee flexed 30 degrees, is common.
 The Ober test (patient lies in lateral decubitus position with hyperextension of the ipsilateral hip; the leg can be brought from abduction to adduction to demonstrate tightness of the iliotibial band) is helpful in making the diagnosis.
The Ober test (patient lies in lateral decubitus position with hyperextension of the ipsilateral hip; the leg can be brought from abduction to adduction to demonstrate tightness of the iliotibial band) is helpful in making the diagnosis.
 Rehabilitation is usually successful.
Rehabilitation is usually successful.
 Surgical excision of an ellipse of the iliotibial band is occasionally necessary.
Surgical excision of an ellipse of the iliotibial band is occasionally necessary.
 Most common in male athletes in their early thirties
Most common in male athletes in their early thirties
 Can be diagnosed with MRI or nuclear imaging and often responds to stretching and strengthening exercises
Can be diagnosed with MRI or nuclear imaging and often responds to stretching and strengthening exercises
 Characterized by localized pain, tenderness, and swelling over the proximal anteromedial tibia at the insertion site of the sartorius, gracilis, and semitendinosus (approximately 6 cm inferior to the joint line)
Characterized by localized pain, tenderness, and swelling over the proximal anteromedial tibia at the insertion site of the sartorius, gracilis, and semitendinosus (approximately 6 cm inferior to the joint line)
 Treated conservatively with oral anti-inflammatory medication, localized corticosteroid injections, and activity modification
Treated conservatively with oral anti-inflammatory medication, localized corticosteroid injections, and activity modification
 Injury and malalignment can contribute to patellar degenerative joint disease.
Injury and malalignment can contribute to patellar degenerative joint disease.
 Lateral release may be beneficial early only if there is objective evidence of patellar tilting.
Lateral release may be beneficial early only if there is objective evidence of patellar tilting.
 Other procedures may be required for advanced patellar arthritis.
Other procedures may be required for advanced patellar arthritis.
 Options include anterior (Maquet) or anteromedial (Fulkerson) transfer of the tibial tubercle or patellectomy for severe cases.
Options include anterior (Maquet) or anteromedial (Fulkerson) transfer of the tibial tubercle or patellectomy for severe cases.
 Tibial rotational alignment and overall lower extremity alignment should always be assessed in evaluating the cause of patellofemoral disease. Patellofemoral arthroplasty has been introduced as another treatment option but remains controversial.
Tibial rotational alignment and overall lower extremity alignment should always be assessed in evaluating the cause of patellofemoral disease. Patellofemoral arthroplasty has been introduced as another treatment option but remains controversial.
2. Anterior fat pad syndrome (Hoffa disease)
 Trauma to the anterior fat pad can lead to fibrous changes and pinching of the fat pad, especially in patients with genu recurvatum.
Trauma to the anterior fat pad can lead to fibrous changes and pinching of the fat pad, especially in patients with genu recurvatum.
 Activity modification, ice, knee padding, and injection can be helpful.
Activity modification, ice, knee padding, and injection can be helpful.
3. Complex regional pain syndrome (formerly known as reflex sympathetic dystrophy)
 Characterized by pain out of proportion to physical findings, this condition is an exaggerated response to injury.
Characterized by pain out of proportion to physical findings, this condition is an exaggerated response to injury.
 Three stages are typical: (1) swelling, warmth, and hyperhidrosis; (2) brawny edema and trophic changes; and (3) glossy, cool, dry skin and stiffness.
Three stages are typical: (1) swelling, warmth, and hyperhidrosis; (2) brawny edema and trophic changes; and (3) glossy, cool, dry skin and stiffness.
 Patellar osteopenia and a “flamingo gait” are also common.
Patellar osteopenia and a “flamingo gait” are also common.
 Treatment includes nerve stimulation, NSAIDs, and sympathetic or epidural blocks—response to which can be diagnostic.
Treatment includes nerve stimulation, NSAIDs, and sympathetic or epidural blocks—response to which can be diagnostic.
1. Lateral patellar facet compression syndrome
 This problem is associated with a tight lateral retinaculum and excessive lateral tilt without excessive patellar mobility.
This problem is associated with a tight lateral retinaculum and excessive lateral tilt without excessive patellar mobility.
 Treatment includes activity modification, NSAIDs, and strengthening of the vastus medialis oblique muscle.
Treatment includes activity modification, NSAIDs, and strengthening of the vastus medialis oblique muscle.
 Arthroscopy and lateral release are occasionally required but indicated only in the setting of objective evidence of lateral tilt that has not responded to extensive nonoperative management.
Arthroscopy and lateral release are occasionally required but indicated only in the setting of objective evidence of lateral tilt that has not responded to extensive nonoperative management.
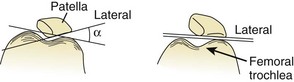
 Lateral tilt is best evaluated by measurement of the lateral patellofemoral angle (Figure 4-28).
Lateral tilt is best evaluated by measurement of the lateral patellofemoral angle (Figure 4-28).
 The best candidates for arthroscopy and lateral release have a neutral or negative tilt with a medial patellar glide of less than one quadrant and a lateral patellar glide of less than three quadrants. Arthroscopic visualization through a superior portal demonstrates that the patella does not articulate medially with 40 degrees of knee flexion.
The best candidates for arthroscopy and lateral release have a neutral or negative tilt with a medial patellar glide of less than one quadrant and a lateral patellar glide of less than three quadrants. Arthroscopic visualization through a superior portal demonstrates that the patella does not articulate medially with 40 degrees of knee flexion.
 Recurrent subluxation or dislocation of the patella can be characterized by lateral displacement of the patella, a shallow intercondylar sulcus, or patellar incongruence.
Recurrent subluxation or dislocation of the patella can be characterized by lateral displacement of the patella, a shallow intercondylar sulcus, or patellar incongruence.
 The articular cartilage on the medial facet of the patella is most commonly injured after a patellar dislocation.
The articular cartilage on the medial facet of the patella is most commonly injured after a patellar dislocation.
 If this injury is associated with femoral anteversion, genu valgum, and pronated feet, the symptoms can be exacerbated, especially in adolescents (“miserable malalignment syndrome”).
If this injury is associated with femoral anteversion, genu valgum, and pronated feet, the symptoms can be exacerbated, especially in adolescents (“miserable malalignment syndrome”).
 Extensive rehabilitation is often curative.
Extensive rehabilitation is often curative.
 Girls and women with previous instability are at increased risk.
Girls and women with previous instability are at increased risk.
 Several radiographic findings are somewhat helpful in diagnosing patellar malalignment (see Figure 4-28). Tibial rotational alignment can also influence patellar alignment and tracking.
Several radiographic findings are somewhat helpful in diagnosing patellar malalignment (see Figure 4-28). Tibial rotational alignment can also influence patellar alignment and tracking.
 Surgical procedures include proximal and distal realignment.
Surgical procedures include proximal and distal realignment.
 Acute, first-time patella dislocations have traditionally been treated nonoperatively, but some surgeons advocate early surgical treatment with arthroscopic evaluation or débridement and acute repair of the medial patellofemoral ligament (usually at the medial epicondyle). This protocol is still somewhat controversial.
Acute, first-time patella dislocations have traditionally been treated nonoperatively, but some surgeons advocate early surgical treatment with arthroscopic evaluation or débridement and acute repair of the medial patellofemoral ligament (usually at the medial epicondyle). This protocol is still somewhat controversial.
 Affected patients should be evaluated with radiographs for an avulsion fracture of the medial patellofemoral ligament that occurs at the middle third of the patella.
Affected patients should be evaluated with radiographs for an avulsion fracture of the medial patellofemoral ligament that occurs at the middle third of the patella.
 The articular cartilage of the medial patellar facet is the most common donor site.
The articular cartilage of the medial patellar facet is the most common donor site.
 Distal realignment, typically tibial tubercle anterior medialization, is indicated for patients with an increased Q angle or a TT-TG distance exceeding 20 mm.
Distal realignment, typically tibial tubercle anterior medialization, is indicated for patients with an increased Q angle or a TT-TG distance exceeding 20 mm.
 Proximal arthrosis of the medial patellar facet is a contraindication to this procedure.
Proximal arthrosis of the medial patellar facet is a contraindication to this procedure.
 Abnormalities of patellar height:
Abnormalities of patellar height:
 Patella alta (high-riding patella) and patella baja (low-riding patella) are determined on the basis of various measurements made on lateral radiographs of the knee (see Figure 4-8).
Patella alta (high-riding patella) and patella baja (low-riding patella) are determined on the basis of various measurements made on lateral radiographs of the knee (see Figure 4-8).
 Patella alta can be associated with patellar instability because the patella may not articulate with the sulcus, which normally constrains the patella.
Patella alta can be associated with patellar instability because the patella may not articulate with the sulcus, which normally constrains the patella.
 Patella baja is often the result of fat pad and tendon fibrosis, and proximal transfer of the tubercle may be required in refractory cases.
Patella baja is often the result of fat pad and tendon fibrosis, and proximal transfer of the tubercle may be required in refractory cases.
E Idiopathic chondromalacia patellae
1. Articular damage and changes to the patella have traditionally been referred to as idiopathic chondromalacia patellae; however, this term has fallen into disfavor.
2. Treatment is usually symptomatic, and physical therapy is emphasized heavily.
3. Débridement procedures are of questionable benefit.
4. The Outerbridge classification system is still in common use today (Figure 4-29).
1. Most often involve Salter-Harris II fractures of the distal femoral physis
2. Pain, swelling, and an inability to ambulate are common.
3. Stress radiographs and/or MRI may be necessary to make the diagnosis.
4. Open reduction and internal fixation are indicated for displaced Salter-Harris II, III and IV fractures and Salter-Harris I that cannot be adequately reduced.
5. It is important to counsel the parents that knee physeal injuries, and particularly distal femoral physeal injuries, may have a worse prognosis than other physeal fractures.
1. Classification: Avulsion fractures of the intercondylar eminence of the tibia are described as types I through IV.
 Type I: displacement of less than 3 mm
Type I: displacement of less than 3 mm
 Type II: avulsion and elevation of the anterior third to half
Type II: avulsion and elevation of the anterior third to half
2. Types I and II avulsion fractures are usually amenable to closed treatment.
3. Types III and IV fractures, and types I and II fractures for which closed treatment fails, are amenable to open or arthroscopic reduction and fixation of the fragment.
4. The medial or lateral menisci may become trapped beneath the bony fragment and thus prevent reduction if not addressed. Medial meniscal entrapment is more common in the Kocher et al series (2003).
1. Classification: Ogden modification of the Watson-Jones classification
 Type 1A: incomplete separation of fragment from metaphysis
Type 1A: incomplete separation of fragment from metaphysis
 Type 1B: compete separation through secondary ossification center
Type 1B: compete separation through secondary ossification center
 Type 2A: complete tubercle fracture through cartilaginous bridge between the proximal tibia epiphysis and tuberosity without displacement at articular surface proximally
Type 2A: complete tubercle fracture through cartilaginous bridge between the proximal tibia epiphysis and tuberosity without displacement at articular surface proximally
 Type 2B: same as type 2A fracture pattern plus comminution
Type 2B: same as type 2A fracture pattern plus comminution
 Type 3A: compete tubercle fracture with displacement through the proximal tibial epiphysis and articular surface.
Type 3A: compete tubercle fracture with displacement through the proximal tibial epiphysis and articular surface.
2. Treatment: Displaced (>5 mm) type 2 and 3 fractures necessitate open reduction with internal fixation. Postoperative care includes immobilization in extension for approximately 6 weeks.
1. Treatment: ACL injury in skeletally immature athletes has received increased attention; the incidence is probably increasing because more children participate in athletics, and the condition is more often diagnosed because of increasing awareness.
 Midsubstance ACL injuries in skeletally immature individuals remain a subject of considerable debate.
Midsubstance ACL injuries in skeletally immature individuals remain a subject of considerable debate.
 Procedures that do not violate the growth plate, especially on the femoral side, are usually recommended for young patients with wide, open physes. Delay in treatment is associated with medial meniscal tears.
Procedures that do not violate the growth plate, especially on the femoral side, are usually recommended for young patients with wide, open physes. Delay in treatment is associated with medial meniscal tears.
 In several studies, investigators have reported no angular deformities or bony bridges in children at Tanner stages 2 to 4 after ACL reconstruction despite the use of multiple grafts and different techniques.
In several studies, investigators have reported no angular deformities or bony bridges in children at Tanner stages 2 to 4 after ACL reconstruction despite the use of multiple grafts and different techniques.
 Techniques: Kocher and colleagues (2005, 2007) demonstrated good results with physeal sparing, combined intraarticular and extraarticular reconstruction in patients at Tanner stage 1 or 2, and transphyseal reconstruction with autologous quadrupled hamstring graft with metaphyseal fixation in patients at Tanner stage 3.
Techniques: Kocher and colleagues (2005, 2007) demonstrated good results with physeal sparing, combined intraarticular and extraarticular reconstruction in patients at Tanner stage 1 or 2, and transphyseal reconstruction with autologous quadrupled hamstring graft with metaphyseal fixation in patients at Tanner stage 3.
 Other authors have recommended newer all-epiphyseal reconstruction techniques.
Other authors have recommended newer all-epiphyseal reconstruction techniques.
 Other techniques that have been successful with no growth arrest include a central vertical tibial tunnel and “over-the-top” placement of the femoral side with a soft tissue graft.
Other techniques that have been successful with no growth arrest include a central vertical tibial tunnel and “over-the-top” placement of the femoral side with a soft tissue graft.
section 2 Thigh, Hip, and Pelvis
A Iliac crest contusions (“hip pointer”)
1. Direct trauma to this area can occur in contact sports.
2. An avulsion of the iliac apophysis should be confirmed or ruled out in adolescent athletes.
3. Treatment consists of ice, compression, pain control, and placing the affected leg on maximal stretch.
4. Corticosteroid injections have occasionally been advocated.
1. This common injury is often the result of sudden stretch on the musculotendinous junction during sprinting.
2. It can occur anywhere in the posterior thigh.
3. Treatment is supportive, followed by stretching and strengthening.
4. To prevent recurrence, return to play should be delayed until strength is approximately 90% that of the opposite side.
B Athletic pubalgia (“sports hernia”)
1. Common in sports such as soccer, these injuries must be differentiated from subtle hernias.
2. Injury to the muscles of the abdominal wall or adductor longus produce anterior pelvis or groin pain, or both, without the classic physical findings of a true inguinal hernia.
3. Can result from acute trauma or microtrauma associated with overuse of the affected muscle.
4. Confirm or rule out other causes of pain with radiography, bone scan, or MRI, or a combination of these.
5. Treat nonoperatively for 6 to 8 weeks with rest and therapy.
6. Repair or reinforcement of the anterior abdominal wall is indicated after conservative measures have failed and after other causes have been excluded.
7. Decompression of the genital branch of the genitofemoral nerve is also favored by some authors in patients presenting with athletic pubalgia.
1. Occurs frequently in female runners and is associated with training on banked surfaces
2. Treatment includes oral anti-inflammatory drugs, stretching, and rest.
A Ilioinguinal nerve entrapment
1. This nerve can be constricted by hypertrophied abdominal muscles as a result of intensive training.
2. Hyperextension of the hip may exacerbate the pain that patients experience, and hyperesthesia symptoms are common. Surgical release is occasionally necessary.
1. Can lead to chronic medial thigh pain, especially in athletes with well-developed hip adductor muscles (e.g., skaters)
2. Nerve conduction studies are helpful for establishing the diagnosis.
1. A history of overuse, an insidious onset of pain, and localized tenderness and swelling are typical.
2. Stress fractures occur via propagation of a crack.
3. Bone scan can be diagnostic, even with normal plain radiographs.
4. MRI is the most specific test for detecting stress fractures.
5. Treatment includes protected weight bearing, rest, cross-training, analgesics, and therapeutic modalities.
6. There are several especially problematic stress fractures:
 Anterior tibial stress fracture: This is especially worrisome with the appearance of the “dreaded black line” on imaging. Persistence of the “dreaded black line” for more than 6 months, especially with a positive bone scan, can be an indication for bone grafting, intramedullary nailing, or both.
Anterior tibial stress fracture: This is especially worrisome with the appearance of the “dreaded black line” on imaging. Persistence of the “dreaded black line” for more than 6 months, especially with a positive bone scan, can be an indication for bone grafting, intramedullary nailing, or both.
 Femoral neck stress fractures: Tension (transverse) fractures are more serious than compression fractures (on the medial side of the neck), and operative stabilization may be required.
Femoral neck stress fractures: Tension (transverse) fractures are more serious than compression fractures (on the medial side of the neck), and operative stabilization may be required.
 Femoral shaft stress fractures: These usually respond to protected weight bearing but can progress to complete fractures if unrecognized. The fulcrum test may be helpful in making this diagnosis.
Femoral shaft stress fractures: These usually respond to protected weight bearing but can progress to complete fractures if unrecognized. The fulcrum test may be helpful in making this diagnosis.
 Pelvic stress fractures: Stress fractures to the sacrum and pubis are rare but must be considered.
Pelvic stress fractures: Stress fractures to the sacrum and pubis are rare but must be considered.
1. Can occur in athletes, especially cross-country skiers (skier’s hip)
2. Release bindings have reduced the incidence of these injuries.
1. Traumatic hip subluxation can disrupt the arterial blood supply to the hip and result in avascular necrosis.
2. Early recognition of these injuries, which are seen in football players, is essential.
3. With posterior subluxation or dislocation, one study revealed a 25% incidence of avascular necrosis.
4. Obturator oblique radiographs (to determine the presence of an avulsion injury) and MRI are recommended.
5. Such imaging should be followed by aspiration of the hip if a large hemarthrosis is present, 6 weeks of minimal weight bearing, and a repeat MRI.
6. With atraumatic injuries, other causative factors (alcohol, catabolic steroids, and decompression sickness) should be sought.
1. Often result from trauma or diseases such as synovial chondromatosis
2. Should be removed, either in an open procedure or arthroscopically, to prevent third-body wear
1. Often a cause of mechanical hip pain manifesting with vague symptoms
2. Magnetic resonance arthrography has greater than 90% sensitivity and is often used for diagnosis, but arthroscopy is the “gold standard” test (Figure 4-31).
3. The incidence of labral tears is highest in patients with acetabular dysplasia.
4. Underlying hip disease should be addressed in addition to the labral tear for the best results.
5. Arthroscopic labral débridement has yielded good short-term and midterm results.
6. Labral repair may yield better results than débridement, according to emerging data on new techniques.
VII FEMOROACETABULAR IMPINGEMENT
1. Abnormal contact between proximal femur and acetabulum that leads to chondral damage and symptoms.
1. Cam, pincer, and a combination of cam and pincer
 Cam impingement is a disorder of proximal femoral head and neck structure whereby the head loses sphericity and has decreased offset.
Cam impingement is a disorder of proximal femoral head and neck structure whereby the head loses sphericity and has decreased offset.
 This results in abnormal loading of the cartilage on the femoral and acetabular sides along with the labrum.
This results in abnormal loading of the cartilage on the femoral and acetabular sides along with the labrum.
 Pincer impingement is a disorder of acetabular structure and can be caused by inadequate acetabular anteversion or acetabular protrusio.
Pincer impingement is a disorder of acetabular structure and can be caused by inadequate acetabular anteversion or acetabular protrusio.
1. Acetabular retroversion; an old slipped capital femoral epiphysis; a nonspherical head; decreased femoral offset or decreased head/neck ratio; overhang of the anterosuperior acetabular rim; protrusio; and a retroverted femoral neck (after fracture).
1. Groin or hip pain in association with limitation in ROM, especially in flexion, can be a symptom.
2. Patients generally have more passive external rotation than internal rotation.
3. A positive result of an anterior impingement test is the reproduction of symptoms with passive flexion, adduction, and internal rotation.
1. Plain radiographs should include anteroposterior pelvis and true lateral views with hip in 15 degrees of internal rotation.
2. CT or MRI can give additional information about femoral-acetabular mismatch and chondral or labral lesions.
3. The false profile view (faux profil) was originally described by Lequesne to assist in the diagnosis of early osteoarthritis and developmental dysplasia of the hip. It is obtained by having the patient stand next to a vertical radiograph cassette. The hip of interest is closest to the cassette. The ipsilateral foot is parallel to the cassette also. The pelvis is rotated 25 degrees backward (the back of the patient is at a 65-degree angle with the cassette).
1. Treatment options include open or arthroscopic procedures to trim the femoral head and neck or acetabular rim; periacetabular osteotomy; femoral osteotomy; a combinations of these procedures with labral débridement; and repair.
2. Total hip arthroplasty is reserved for patients with significant arthritic changes.
1. Condition in which the iliotibial band abruptly catches on the greater trochanter or the iliopsoas impinges on the hip capsule.
2. The iliotibial condition (external snapping hip) is more common in women with wide pelvises and prominent trochanters and can be exacerbated by running on banked surfaces.
3. The snapping may be reproduced with passive hip flexion from an adducted position.
4. Stretching and strengthening exercises, modalities such as ultrasonography, and occasionally surgical release may relieve the snapping.
5. This condition must be differentiated from the less common snapping iliopsoas tendon (internal snapping hip), which can be diagnosed with extension and internal rotation of the hip from a flexed and externally rotated position.
6. Dynamic ultrasonography, arthrography, and bursography may also be helpful in determining the diagnosis.
See Supplemental Images on expertconsult.com.
1. As techniques improve, so do the indications. Hip arthroscopy is currently effective for the treatment of loose bodies, labral tears, chondral injuries, femoroacetabular impingement, avascular necrosis, synovial disease, ruptured ligamentum teres, impinging osteophytes, and unexplained mechanical symptoms.
1. Hip arthroscopy is typically performed with the patient in the supine or lateral position with approximately 50 lb (22.7 kg) of traction and a well-padded perineal post.
1. Three portals are commonly used for instrumentation: one on each side of the greater trochanter and an additional anterior portal (Figure 4-32).
1. Three compartments are described:
 The central compartment refers to the intraarticular portion of the hip joint between the cartilagenous portions of the proximal femur and acetabulum.
The central compartment refers to the intraarticular portion of the hip joint between the cartilagenous portions of the proximal femur and acetabulum.
 The peripheral compartment refers to the intraarticular portion of the hip joint along the neck of the femur and the edge of the acetabulum.
The peripheral compartment refers to the intraarticular portion of the hip joint along the neck of the femur and the edge of the acetabulum.
 The lateral compartment refers to the extraarticular portion in the peritrochanteric region and trochanteric bursa.
The lateral compartment refers to the extraarticular portion in the peritrochanteric region and trochanteric bursa.
1. Complications, which are rare, are associated with traction injuries, iatrogenic chondral injuries, and neurovascular injury caused by aberrant portal placement.
2. The anterior portal puts the lateral femoral cutaneous nerve at risk.
 Also at risk are the ascending branch of the lateral femoral circumflex artery and the femoral neurovascular bundle.
Also at risk are the ascending branch of the lateral femoral circumflex artery and the femoral neurovascular bundle.
3. The anterolateral portal is associated with injury to the superior gluteal nerve.
4. The posterolateral portal places the sciatic nerve at risk, particularly when the hip is externally rotated.
section 3 Leg, Foot, and Ankle
1. When compressed at the Hunter canal or in the proximal leg, the saphenous nerve can cause painful symptoms inferior and medial to the knee.
1. The common peroneal nerve can be compressed behind the fibula or injured by a direct blow to this area.
2. The superficial peroneal nerve can be entrapped about 12 cm proximal to the tip of the lateral malleolus, where it exits the fascia of the anterolateral leg, as a result of inversion injuries.
3. Superficial peroneal nerve entrapment manifests with numbness and tingling over the dorsum of the foot that worsens with plantar flexion and inversion of the foot.
4. The deep peroneal nerve can be compressed by the inferior extensor retinaculum, which leads to anterior tarsal tunnel syndrome and sometimes necessitates release of this retinaculum.
1. Compression of the tibial nerve under the flexor retinaculum behind the medial malleolus may result in tarsal tunnel syndrome. Electromyography or nerve conduction evaluation is helpful, and surgical release is sometimes indicated.
2. Distal entrapment of the first branch of the lateral plantar nerve (Baxter nerve) (to the adductor digiti quinti), between the fascia of the abductor hallucis and the medial side of the quadratus plantae, has also been described.
D Medial plantar nerve entrapment
1. Occurs at the point where the flexor digitorum longus and flexor hallucis longus cross (knot of Henry)
2. Most commonly caused by external compression from orthoses
3. Commonly called jogger’s foot, this condition usually responds to conservative measures
4. Orthotics can exacerbate symptoms and should thus be avoided.
1. Can occur anywhere along the course of the nerve, but the nerve is most vulnerable 12 to 15 mm distal to the tip of the fibula as the foot rests in equinus position
F Interdigital nerve entrapment
1. Commonly called a Morton neuroma
2. Entrapment can occur during the push-off phase during running in athletes and with the demi-pointe position in dancers.
3. It usually occurs between the third and fourth metatarsals plantar to the transverse metatarsal ligament and responds to surgical resection if conservative measures fail.
1. Subluxation and dislocation
 Violent dorsiflexion of the inverted foot can result in injury of the fibroosseous peroneal tendon sheath.
Violent dorsiflexion of the inverted foot can result in injury of the fibroosseous peroneal tendon sheath.
 Diagnosis is confirmed by observing the subluxation or dislocation by means of eversion and dorsiflexion of the foot.
Diagnosis is confirmed by observing the subluxation or dislocation by means of eversion and dorsiflexion of the foot.
 Plain radiographs may demonstrate a rim fracture of the lateral aspect of the distal fibula.
Plain radiographs may demonstrate a rim fracture of the lateral aspect of the distal fibula.
 Treatment of acute injuries includes restoration of the normal anatomy (Figure 4-33).
Treatment of acute injuries includes restoration of the normal anatomy (Figure 4-33).
 Chronic reconstruction involves direct repair, groove-deepening procedures, tissue transfers, or bone block techniques.
Chronic reconstruction involves direct repair, groove-deepening procedures, tissue transfers, or bone block techniques.
 These injuries, which are being recognized more frequently with MRI, often lead to tears of the peroneal tendons.
These injuries, which are being recognized more frequently with MRI, often lead to tears of the peroneal tendons.
3. Longitudinal tears of the peroneal tendons (especially the peroneus brevis tendon)
B Posterior tibialis tendon injury
1. This injury often occurs in older athletes.
2. Patients complain of midarch foot pain, with difficulty pushing off.
3. Débridement of partial ruptures and flexor digitorum longus transfer for chronic injuries are recommended.
C Anterior tibialis tendon injury
 Overuse injury to the Achilles tendon usually responds to rest and physical therapy, with an eccentric loading program and local modalities such as ultrasound. Progression to partial rupture may necessitate surgical excision of scar and granulation tissue.
Overuse injury to the Achilles tendon usually responds to rest and physical therapy, with an eccentric loading program and local modalities such as ultrasound. Progression to partial rupture may necessitate surgical excision of scar and granulation tissue.
 Complete rupture of the tendon is caused by maximal plantar flexion with the foot planted.
Complete rupture of the tendon is caused by maximal plantar flexion with the foot planted.
 Patients may relate that they felt as if they were “shot.”
Patients may relate that they felt as if they were “shot.”
 The Thompson test (squeezing the calf should result in normal plantar flexion of the foot) is helpful for confirming the diagnosis.
The Thompson test (squeezing the calf should result in normal plantar flexion of the foot) is helpful for confirming the diagnosis.
 Treatment remains controversial; however, recurrence rates are reduced with primary repair, and other complications (i.e., wound problems) are increased with surgical repair.
Treatment remains controversial; however, recurrence rates are reduced with primary repair, and other complications (i.e., wound problems) are increased with surgical repair.
 Early weight bearing after repair has been advocated with improved subjective outcomes.
Early weight bearing after repair has been advocated with improved subjective outcomes.
IV CHRONIC EXERTIONAL COMPARTMENT SYNDROME
A Although it is more commonly encountered with trauma, compartment syndrome is becoming more frequently diagnosed in athletes.
B Athletes (especially runners and cyclists) may note pain that has a gradual onset during exercise, ultimately restricting their performance.
C Compartment pressures should be measured before, during, and after exercise.
1. Pressures higher than 20 mm Hg 5 minutes after exercise, absolute values higher than 15 mm Hg during rest, or pressures higher than 30 mm Hg 1 minute after exercise can help establish the diagnosis.
D The anterior compartment of the leg is the most frequently involved and has the best prognosis.
E Fasciotomy is sometimes indicated for refractory cases (Figure 4-34).
F Popliteal artery entrapment syndrome is often confused with chronic posterior compartment syndrome.
1. Patients present with intermittent claudication, including intermittent calf pain, cramping, coolness, and, at times, paresthesias into the foot.
2. Provocative clinical tests for the syndrome of popliteal artery entrapment include obliteration of pedal pulses by active plantar flexion or passive dorsiflexion of the ankle as detected by Doppler recordings.
3. Treatment is release and recession of the medial head of the gastrocnemius.
1. Common in athletes who have undergone a change in their training routines and in female endurance athletes (examiner must ask about the menstrual history).
2. Usually responds to rest and activity modification
3. Recalcitrant fractures may necessitate operative fixation.
 This is a complication of unrecognized tibial stress fractures and can be a difficult problem.
This is a complication of unrecognized tibial stress fractures and can be a difficult problem.
 Persistence of the “dreaded black line” (Figure 4-35) for more than 6 months, especially with a positive bone scan, can be an indication for bone grafting or intramedullary nailing, or both.
Persistence of the “dreaded black line” (Figure 4-35) for more than 6 months, especially with a positive bone scan, can be an indication for bone grafting or intramedullary nailing, or both.
1. Fractures at the metaphyseal-diaphyseal junction of the fifth metatarsal in an athlete.
2. Early intramedullary screw fixation allows for earlier healing and an earlier return to conditioning activities.
3. A screw with a minimal diameter of 4 mm should be used (Figure 4-37).

Figure 4-37 Radiographic appearance of Jones fracture after open reduction with internal fixation with a 6.5-mm screw.
4. Returning to sports activity before radiographic union increases the risk of nonunion.
VI OTHER FOOT AND ANKLE DISORDERS
1. Inflammation of the plantar fascia, usually in the central to medial subcalcaneal region, is common in runners.
2. Plantar fasciitis is associated with a tight heel cord on physical examination.
3. Rest, orthoses, stretching, NSAIDs, and local steroid injections are helpful.
4. Partial plantar fasciotomy is occasionally necessary, but recovery can be protracted.
5. Refractory cases may be treated with extracorporeal shock wave therapy.
B Os trigonum (posterior impingement) syndrome
1. Can cause impingement with plantar flexion of the foot, especially in ballet dancers
2. Treatment may include local anesthetic injection and other supportive measures.
3. Surgical excision of the offending bone with or without release of the flexor hallucis longus is occasionally necessary, and arthroscopic techniques have been described.
C Ankle sprains and instability
1. Common in athletes and most often involve the anterior talofibular ligament and occasionally involve the calcaneofibular ligament
2. The posterior talofibular ligament is rarely involved.
3. The Ottawa ankle rules (Stiell et al, 1995) indicate that radiographs are required only in patients with tenderness at the distal (especially posterior) tibia or fibula, tenderness at the base of the fifth metatarsal or navicular, and an inability to bear weight.
4. Surgical treatment is reserved for recurrent, symptomatic ankle instability with excessive tilt and a positive finding of the anterior drawer test on examination or on stress radiographs that have not responded to orthoses and peroneal strengthening and proprioceptive exercises over an extended period.
5. Anatomic procedures (modified Broström procedure) are usually successful.
6. Involvement of the subtalar joint necessitates tendon rerouting procedures that include this joint.
7. Patients with “high” ankle sprains involving the syndesmosis require recovery periods almost twice as long as those for patients with common ankle sprains.
1. Severe dorsiflexion of the metatarsophalangeal joint of the great toe (injuring the plantar plate) can result in tenderness, stiffness, and swelling of the toe.
2. Treatment includes physical therapy, ice, and taping in plantar flexion.
3. If symptoms persist, a stress fracture of the proximal phalanx should be ruled out with a bone scan or MRI.
E Snowboarder’s foot and ankle
1. Fracture of the lateral process of the talus (Figure 4-38).
2. The injury involves the leading leg on the board.
3. CT can help confirm the diagnosis.
4. Fracture with small fragments (<2 mm) can be treated in a short leg cast for 6 weeks, whereas a fracture with large fragments should should be treated with open reduction with internal fixation.
1. Soft tissue or bony conditions leading to decreased ROM, chronic pain around the ankle, or both
 Common in ballet dancers and football, basketball, and soccer players
Common in ballet dancers and football, basketball, and soccer players
 Pain with dorsiflexion along with cutting and pivoting maneuvers are common symptoms.
Pain with dorsiflexion along with cutting and pivoting maneuvers are common symptoms.
 Lateral radiographs reveal a combination of anterior osteophyte formation on the distal anterior tibia and divot-like formation on the dorsal aspect of the talar neck.
Lateral radiographs reveal a combination of anterior osteophyte formation on the distal anterior tibia and divot-like formation on the dorsal aspect of the talar neck.
 Also common in ballet dancers, gymnasts, soccer players, and downhill runners
Also common in ballet dancers, gymnasts, soccer players, and downhill runners
 Known as os trigonum syndrome or talar compression syndrome
Known as os trigonum syndrome or talar compression syndrome
 Pain is worse with plantar flexion and push-off maneuvers.
Pain is worse with plantar flexion and push-off maneuvers.
 Soft tissue can become trapped between the distal posterior tibia and calcaneus during plantar flexion.
Soft tissue can become trapped between the distal posterior tibia and calcaneus during plantar flexion.
 Bony lesions that can contribute include os trigonum (present in 7% of adults), Stieda process (elongated lateral talar tubercle), and loose bodies.
Bony lesions that can contribute include os trigonum (present in 7% of adults), Stieda process (elongated lateral talar tubercle), and loose bodies.
 Soft tissue causes include flexor hallucis longus synovitis and posterior recesses of the subtalar and tibiotalar joints. Excision (open or arthroscopic) of the os trigonum is often effective.
Soft tissue causes include flexor hallucis longus synovitis and posterior recesses of the subtalar and tibiotalar joints. Excision (open or arthroscopic) of the os trigonum is often effective.
See Supplemental Images on expertconsult.com.
1. Include treatment of osteochondral injuries of the talus, débridement of post-traumatic synovitis, anterolateral impingement secondary to chronic pain from an ankle sprain, removal of anterior tibiotalar spurring, os trigonum excision, and cartilage débridement in conjunction with ankle fusions.
2. Osteochondral injuries of the talus
3. Lateral lesions are usually traumatic, shallow, and anterior, whereas medial lesions are atraumatic, deeper, and posterior.
 Lateral lesions are usually associated with inversion and dorsiflexion. Medial lesions are seen with inversion, plantar flexion, and rotation.
Lateral lesions are usually associated with inversion and dorsiflexion. Medial lesions are seen with inversion, plantar flexion, and rotation.
4. The modification to the Berndt and Harty classification scheme (Figure 4-39) by Loomer and coworkers (1993) is helpful in the management of these osteochondral lesions of the talus.
1. Supine positioning with the leg over a well-padded bolster and an external traction device are currently popular.
2. Meticulous attention to portal placement is required because the most common complication of ankle arthroscopy is nerve injury.
3. Five portals—anteromedial, anterolateral, posterolateral, posteromedial, and anterocentral—have been suggested (Figure 4-40), but most surgeons avoid both the posteromedial portal (because of the risk to the posterior tibial artery and tibial nerve) and the anterocentral portal (because of the risk to the dorsalis pedis and deep peroneal nerve).
4. The “nick and spread” method is advocated for the anterolateral portal (superficial peroneal nerve) and the anteromedial portal (saphenous vein).