Chapter 107 Spondylectomy for Spinal Tumors
Spondylectomy is defined as removal of an entire segment of the spine, including the vertebral body, pedicles, superior and inferior articulating processes, pars, transverse processes, lamina, and spinous process. Removal of the entire spinal segment en bloc is possible only with sacrifice of the spinal cord or the cauda equina, as the spinal cord and cauda equina lie within the spinal canal, incarcerated by the spine. Tumors within the spine can be removed either in a piecemeal fashion (intralesional) or en bloc (in one piece, without violation of the tumor margin). To achieve an en bloc resection of a tumor, the technique of a total spondylectomy can be employed (Fig. 107-1). As a point of semantics, the tumor is removed en bloc, but the spondylectomy is usually not an en bloc spondylectomy.1
General Concepts and Surgical Planning
The anatomic location of the tumor to be removed within a particular vertebral segment or segments will dictate the steps in achieving an en bloc resection via a spondylectomy.1 For simplicity, the planning can be divided into two stages: a preparatory stage and a stage in which the tumor is delivered. Accomplishment of the first stage, the preparatory stage, may require multiple procedures.
The vascular structures involved in the resection vary at different levels of the spine. In the cervical spine, a vertebral artery might need to be sacrificed to achieve a resection, and doing so might result in posterior fossa ischemia and stroke. In the thoracic spine, multiple segmental vessels might need to be ligated, increasing the risk of ischemia to the spinal cord. In the lumbar spine, the iliac arteries and veins might need to be manipulated or even bypassed, potentially causing ischemia to the bowel, kidneys, or lower extremities. Manipulation or sacrifice of the inferior vena cava and iliac vessels increases the chance for thrombus formation and consequent pulmonary embolus.
Neurologic sacrifice can be entertained only if the deficit that will be produced is tolerable to the patient’s expectations and lifestyle acceptance. Sacrifice of a certain root alone might not produce a significant deficit, but combinations of roots sacrificed can be crippling (Table 107-1). C1-4 can usually be sacrificed without significant morbidity. Sacrifice of C3 and C4 together could result in diaphragm weakness. Cutting C5, C6, C8, or T1 usually results in profound weakness. Sacrifice in the thoracic spine (T2-12) will result in a bandlike distribution of numbness but usually has inconsequential motor loss. Sacrifice of L1 or L2 in isolation will produce weakness, but over time, patients usually are able to compensate for the loss quite well. L3 loss will result in quadriceps weakness and may require bracing of the knee to walk. L4 sacrifice can also result in quadriceps weakness, but the problem that is usually noted is proprioceptive difficulty of the knee joint. Without proper proprioception of the knee, a patient may find the knee week and can complain of the knee buckling at times during ambulation. L5 loss results in footdrop. S1 sacrifice is usually well tolerated but does results in gastocnemius weakness, which can make it difficult for a patient to stand on the toes. S4, S5, and the coccygeal nerves can usually be sacrificed without significant consequences. Loss of bilateral S2 and S3 nerve roots will result in loss of bowel, bladder, and sexual function. Unilateral S2 and S3 sacrifice usually allows a patient to have fairly normal bowel, bladder, and sexual function. Bilateral S3 sacrifice and S2 preservation will provide some function, but most patients will have difficulty with bowel, bladder, and sexual function.
| Nerve Sacrifice | Deficit |
|---|---|
| C3 and C4 | Possible diaphragm weakness |
| C5 | Deltoid weakness |
| C6 | Bicep weakness |
| C8 or T1 | Hand intrinsics weakness |
| T2–T12 | Dermatomal sensory loss |
| L1 or L2 | Iliopsoas weakness, usually compensated over time |
| L3 | Quadriceps weakness |
| L4 | Quadriceps weakness, knee proprioceptive difficulty, and footdrop |
| L5 | Footdrop |
| S1 | Minimal deficit |
| Unilateral S2 and S3 | Bowel/bladder/sexual function abnormal but functional |
| Bilateral S2 and S3 | Loss of bowel/bladder/sexual function |
| Bilateral S3 with S2 sparing | Some bowel/bladder/sexual function |
| S4, S5, and coccygeal nerves | Dermatomal sensory loss |
Level-Specific Challenges
Thoracic Spine (T2-12)
The thoracic spine (T2-12) has a unique advantage over other spinal segments in that the nerve roots in this region can be sacrificed with minimal morbidity. In performing a multilevel spondylectomy, increasing the number of nerve roots and segmental vessels that are sacrificed increases the risk of ischemic injury to the cord. The exact tolerance of the human spinal cord for ischemia has not yet been defined, and there is probably a fair amount of variability between patients. Kato et al. have described a canine model, in which they set out to determine the number of segmental vessels that can be ligated before ischemia occurs.2 They found that the interruption of bilateral segmental arteries of four or more consecutive levels, including the level of the Adamkiewicz artery, risks producing ischemic spinal cord dysfunction.
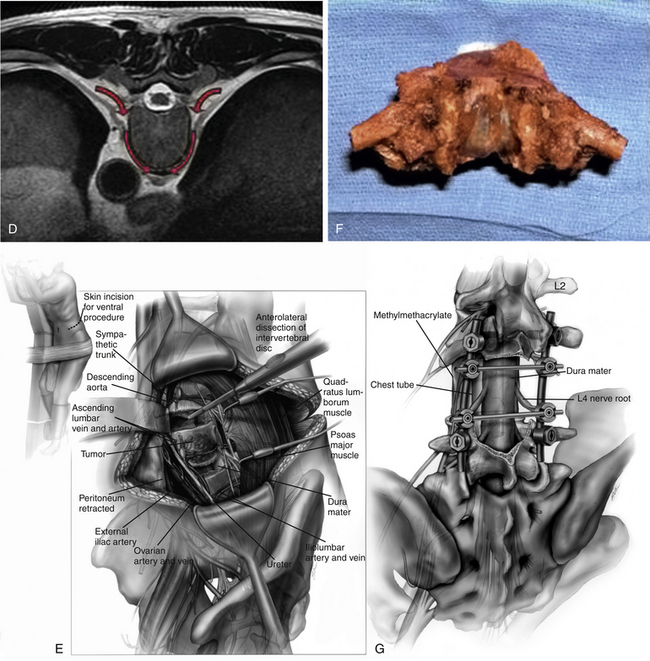
Tumors that are located ventrally, in the vertebral body, will need to undergo a preparatory stage from a dorsal approach. The approach is a standard midline approach with a subperiosteal exposure and exposure of the level of interest and two to three levels above and below index level(s) (Fig. 107-2A). Laterally, the exposure is carried out over the ribs for at least 6 cm on either side. Preoperatively, the MRI and CT are examined critically to understand exactly how far into the dorsal elements the tumor might extend. If the tumor extends into the pedicles and transverse process, this portion of the vertebral segment cannot be violated and must be dissected such that it can remain in continuity with the specimen3 (Fig. 107-2B). The dorsal elements that are uninvolved with tumor at the index level(s) are removed, as are the dorsal elements above and below this level (Fig. 107-2C). Because the spinal column will be completely destabilized after the resection, instrumentation is placed at this part of the operation. The ribs at the index level(s) and the level above and below are cut 6 cm lateral to the transverse processes and, if not involved in tumor, are removed and retained as graft material. Care is taken not to injure the neurovascular bundle or pleura ventral to the rib.
The segmental vessels are traced from the rib to the foramen. A dissection plane is opened, keeping the segmental vessels ventral, opening the fatty plane between the vessel and the vertebral body. Staying in this plane with the dissection will allow the inferior vena cava and the aorta to remain ventral and away from the vertebral body and tumor. The radicular branches coming off the segmental vessels that supply the spinal roots and spinal cord are ligated and cut. Staying in this plane, keeping the segmental vessels ventral in the dissection plane, will eventually allow the dissection to be carried ventral the vertebral body and dorsal to the aorta and vena cava. As this dissection plane is developed from both the left and right sides of the patient, the aorta, vena cava, and esophagus will be kept out of the field and protected from the spine (Fig. 107-2D). A silastic sheet can be placed in this dissection plane, protecting these vascular structures and the pleura. Attention is then turned to the spinal canal. The nerve roots of the index level(s) are ligated proximal to the dorsal root ganglia and are cut. Ligating the roots proximal to the dorsal root ganglia minimizes the chance of developing long-term chronic pain. The epidural plane is then defined, and if tumor capsule enters this plane, the epidural space is dissected, preserving the tumor capsule. Tomita saws are placed encircling the spinal column, one rostral and one caudal to the tumor. The final assembly of the instrumentation is completed, and by using the Tomita saws, the osteotomies are completed. The specimen is now free, completing the preparatory stage. The en bloc specimen is now gently rotated away from the spinal cord and delivered out through the space created by removing the ribs (Figs. 107-2E and F). The ventral vertebral defect is reconstructed, and the grafting and closure are then performed (Fig. 107-2G).
Tumors bounded by pleura, in which the pleura will need to remain with the specimen to obtain a negative margin, will need to be prepared in a slightly different fashion. Rather than approaching the tumor from an entirely dorsal approach, a ventral approach is added. The first steps of the preparatory stage are the same as those in the entirely dorsal approach. In contrast to the entirely dorsal approach, however, the ventral aspect of the spine will need to be dissected from a ventral approach to leave the pleura intact over the specimen (Fig. 107-3). The ribs need not be dissected as far laterally as is done in the entirely dorsal approach, and rather than resecting the ribs, the ribs need to be sectioned only beyond the lateral extent of the tumor. The sectioning of the pleura, osteotomies through the disc space, and then the delivery of the tumor will take place through a ventral exposure. The ventral exposure will take the form of either a thoracotomy or a thoracoscopic approach. After the exposure is completed, the segmental vessels coming off the aorta and going to the vena cava are identified, ligated, and cut. The pleura is cut in such a way as to create a margin for the tumor. The rostral and caudal osteotomies are completed, and the tumor specimen is delivered. The ventral spinal reconstruction is then completed, and the thoracotomy is closed.
Cervical Spine (C2-T1)
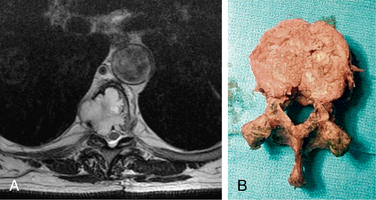
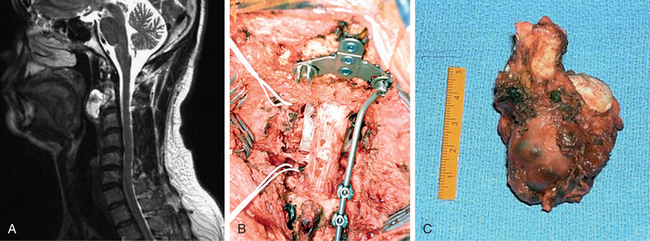
In the cervical spine, an en bloc resection of a tumor will only be realistic if the tumor is not involved in both vertebral arteries, and if the vertebral artery that remains after the tumor removal is able to provide an adequate blood supply to the posterior fossa. This will need to be determined in the preoperative period. If a cervical tumor involves one of the vertebral arteries (Fig. 107-4A) and would therefore require sacrifice of that vertebral artery, then it must be determined preoperatively whether the contralateral vertebral artery will be sufficient to provide the necessary vascular supply.4 This determination can be made by estimating which artery is dominant. It the nondominant artery is involved in the tumor, no further investigation is usually required. If the dominant artery is involved in the tumor or dominance is not clear, then ancillary testing can be helpful. A conventional cerebral angiogram is useful in determining the patency of the circle of Willis to determine whether the anterior circulation could possibly provide the blood supply to the posterior circulation. In addition, a vertebral artery balloon occlusion test can be performed to predict functionally whether a patient will tolerate the sacrifice. Even if it is determined preoperatively that a patient may tolerate unilateral sacrifice of a vertebral artery, this must be undertaken with caution, as vasospasm, embolization, or thrombosis of the remaining vertebral artery could lead to disaster.
After it has been determined whether a vertebral artery will need to be sacrificed and that the patient will most likely tolerate the loss of the vertebral artery, the consequences of the nerve root sacrifice must be weighed by having the patient understand the postoperative disability that he or she will endure. If this is acceptable to the patient, then proceeding with the resection is a possibility. As in the thoracic spine, the preparatory stage begins on the side of the spinal canal opposite the tumor. In general, ventrally located tumors will first be approached dorsally, and the tumor will be delivered away from the ventral aspect of the spinal cord.
During the dorsal approach, the dorsal elements of the spine are removed, exposing the normal thecal sac. A tumor that is ventrally situated and extends laterally to involve a vertebral artery and nerve roots will require that the artery and the nerve roots are sectioned during the preparatory stage. The nerve roots to be sacrificed are identified within the spinal canal and are ligated and sectioned proximal to the dorsal root ganglion. The lateral masses rostral and caudal to the tumor are carefully resected with a high-speed diamond bur. As the lateral masses are resected, the foramina for the nerve roots will be encountered. Ventral to the nerve roots lies the vertebral artery. As the vertebral artery is dissected, great care must be taken, as there is an exuberant venous plexus surrounding the vertebral artery. Bleeding from this plexus can be carefully controlled with thrombin and powdered hemostatic gelatin (Gelfoam). The vertebral artery is identified rostral and caudal to the tumor. It is circumferentially identified and then ligated and sectioned (Fig. 107-4B). Prior to ligation, a test occlusion of the vertebral artery can be made with aneurysm clips while monitoring brainstem auditory evoked potentials and the electroencephalogram. If any changes are recorded during the test occlusion, then the plan for vertebral artery sacrifice must be aborted unless a vertebral artery bypass is contemplated.
After the ventral cervical approach has been completed, the osteotomies rostral and caudal to the tumor need to be completed. These osteotomies need to be taken dorsally, all the way through the posterior longitudinal ligament. After these osteotomies have been completed, the specimen should be mobile, and the tumor is removed en bloc (Fig. 107-4C). The operation is then completed with a ventral reconstruction and arthrodesis.
Lumbar Spine (L1-5)
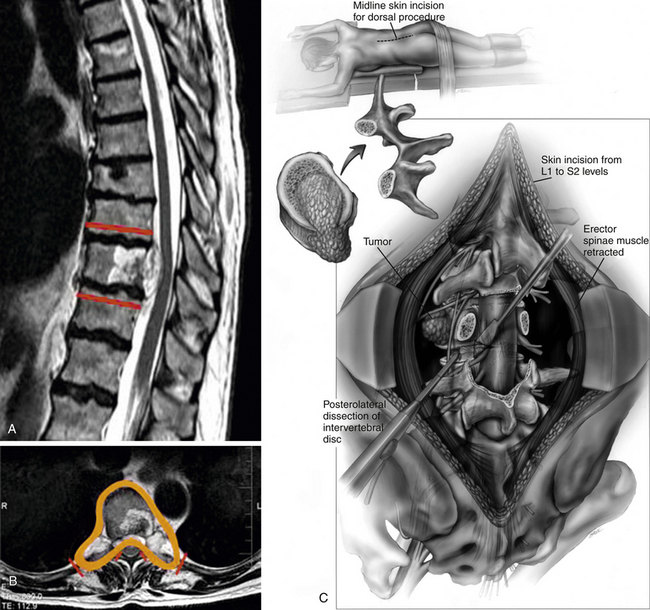
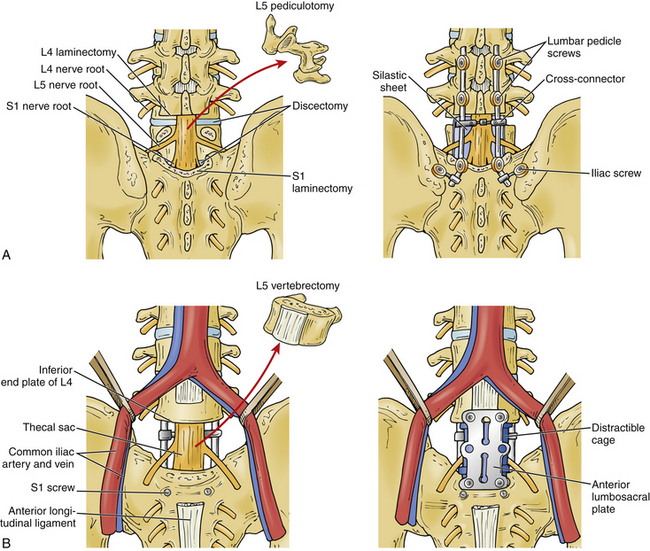
The lumbar spine is very similar to the cervical spine in regard to the challenges and limitations of nerve root sacrifice, but the lumbar spine has the advantage that it does not have the added complication of the vertebral artery. A ventrally located lumbar tumor will be approached in two stages: The preparatory stage will be a standard dorsal approach (Fig. 107-5A), and the delivery stage will be a ventral approach.5 For L5 lesions, this will be a midline retroperitoneal or transperitoneal approach (Fig. 107-5B). For lesions above L5, this will usually be a lateral retroperitoneal approach, usually from the side that the tumor presents itself. If a tumor is located ventrally but on both sides of the vertebral body, then a midline approach for lesions rostral to L5 is considered, but this will entail significant mobilization of the aorta and inferior vena cava.
Complications
As has been mentioned, spondylectomy operations result in severe destabilization of the spine. Delayed instrumentation failures can result in cage dislodgement or dorsal instrumentation failure, which can result in devastating vascular or neurologic injury. In addition, even if a vascular or neurologic impairment does not result from instrumentation failure, revision operations for instrumentation failure in this setting can be quite challenging, and in some circumstances impossible, dooming a potentially cured patient to a life of chronic pain.
Thoracic spondylectomies may result in a potential devastating complication of a chyle leak from injury to the thoracic duct. During the initial dissection, the thoracic duct may not be obvious and can be inadvertently injured. At the time of injury, this might also not be very apparent, as the chylous output may be small and the fluid can be colorless. If a chyle leak is suspected at the time of surgery, administration of cream through the nasogastric tube can stimulate the output of milky chyle and make the injury more apparent. If a chyle leak becomes uncontrolled, the patient may have a protracted postoperative course with nutritional difficulty.
Boriani S., Weinstein J.N., Biagini R. Primary bone tumors of the spine. Terminology and surgical staging. Spine (Phila Pa 1976). 1997;22(9):1036-1044.
Gallia G.L., Suk I., Witham T.F., et al. Lumbopelvic reconstruction after combined L5 spondylectomy and total sacrectomy for en bloc resection of a malignant fibrous histiocytoma. Neurosurgery. 2010;67(2):E498-E502.
Hsieh P.C., Galia G.L., Sciubba D.M., et al. En-bloc excision of chordomas in the cervical spine: review of 5 consecutive cases with over 4-year follow-up. Spine (Phila Pa 1976). 2011;36(24):E1581-E1587.
Hsieh P.C., Li K.W., Sciubba D.M., et al. Posterior-only approach for total en bloc spondylectomy for malignant primary spinal neoplasms: anatomic considerations and operative nuances. Neurosurgery. 2009;65(Suppl 6):173-181. discussion 181
Kato S., Kawahara N., Tomita K., et al. Effects on spinal cord blood flow and neurologic function secondary to interruption of bilateral segmental arteries which supply the artery of Adamkiewicz: an experimental study using a dog model. Spine (Phila Pa 1976). 2008;33(14):1533-1541.
1. Boriani S., Weinstein J.N., Biagini R. Primary bone tumors of the spine. Terminology and surgical staging. Spine (Phila Pa 1976). 1997;22(9):1036-1044.
2. Kato S., Kawahara N., Tomita K., et al. Effects on spinal cord blood flow and neurologic function secondary to interruption of bilateral segmental arteries which supply the artery of Adamkiewicz: an experimental study using a dog model. Spine (Phila Pa 1976). 2008;33(14):1533-1541.
3. Hsieh P.C., Li K.W., Sciubba D.M., et al. Posterior-only approach for total en bloc spondylectomy for malignant primary spinal neoplasms: anatomic considerations and operative nuances. Neurosurgery. 2009;65(Suppl 6):173-181. discussion 181
4. Hsieh P.C., Galia G.L., Sciubba D.M., et al. En-bloc excision of chordomas in the cervical spine: review of 5 consecutive cases with over 4-year follow-up. Spine (Phila Pa 1976). 2011;36(24):E1581-E1587.
5. Gallia G.L., Suk I., Witham T.F., et al. Lumbopelvic reconstruction after combined L5 spondylectomy and total sacrectomy for en bloc resection of a malignant fibrous histiocytoma. Neurosurgery. 2010;67(2):E498-E502.