Spine
2.1
Scoliosis
Idiopathic
2% prevalence for curves > 10°.
1. Infantile – diagnosed before the age of 4 years. 90% are thoracic and concave to the right. More common in boys. 90% resolve spontaneously.
2. Juvenile – diagnosed between 4 and 9 years. More common in girls. Almost always progressive.
3. Adolescent – diagnosed between 10 years and maturity. More common in females. Majority are concave to the left in the thoracic region.
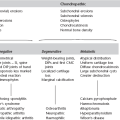
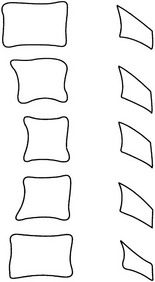
Congenital
Prognosis is dependent on the anatomical abnormality and a classification (see figure on p. 37) is, therefore, important.
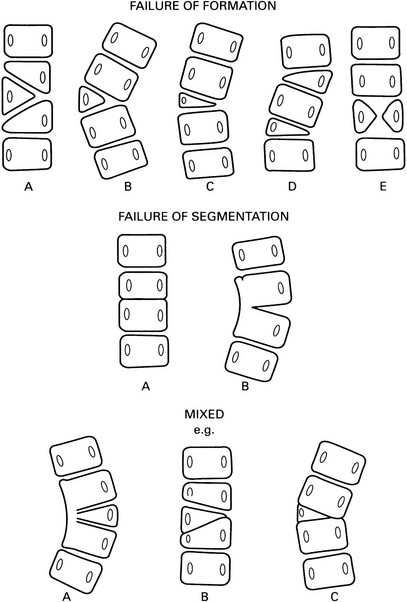
A Incarcerated hemivertebra – a straight spine with little tendency to progression.
B Free hemivertebra – may be progressive.
C Wedge vertebra – better prognosis than a free hemivertebra.
D Multiple hemivertebrae – failure of formation on the same side results in a severe curve. Hemivertebrae on opposite sides may compensate each other.
A Bilateral → block vertebra and a short spine, e.g. Klippel–Feil.
B Unilateral unsegmented bar – severely progressive curve with varying degrees of kyphosis or lordosis depending on the position of the bar.
Mesodermal and neuroectodermal diseases
1. Neurofibromatosis* – in up to 40% of patients. Classically a sharply angled short segment scoliosis with a severe kyphosis. The apical vertebrae are irregular and wedged with adjacent dysplastic ribs. 25% have a congenital vertebral anomaly.
2. Marfan’s syndrome* – scoliosis in 40–60%. Double structural curves are typical.
3. Homocystinuria* – similar to Marfan’s syndrome.
4. Other skeletal dysplasias – spondyloepiphyseal dysplasia congenita, spondyloepimetaphyseal dysplasia, pseudoachondroplasia, metatropic dwarfism, diastrophic dwarfism, Kniest disease, spondylocostal dysostosis.
Leg length discrepancy
A flexible lumbar curve, convex to the side of the shorter leg. Disparity of iliac crest level.
2.2
Solitary collapsed vertebra
(a) Metastasis – breast, bronchus, prostate, kidney and thyroid account for the majority of patients with a solitary spinal metastasis. The disc spaces are preserved until late. The bone may be lytic, sclerotic or mixed. ± Destruction of a pedicle.
(b) Multiple myeloma/plasmacytoma* – a common site, especially for plasmacytoma. May mimic an osteolytic metastasis or be expansile and resemble an aneurysmal bone cyst.
2. Osteoporosis (q.v.) – generalized osteopenia. Coarsened trabecular pattern in adjacent vertebrae due to resorption of secondary trabeculae.
4. Infection – with destruction of vertebral end-plates and adjacent disc spaces.
5. Langerhans’ cell histiocytosis* – eosinophil granuloma is the most frequent cause of a solitary vertebra plana in childhood. The posterior elements are usually spared.
6. Benign tumours – haemangioma, giant cell tumour and aneurysmal bone cyst.
7. Paget’s disease* – diagnosis is difficult when a solitary vertebra is involved. Neural arch is affected in most cases. Sclerosis and expansion. If other non-collapsed vertebrae are affected then diagnosis becomes much easier.
2.3
Multiple collapsed vertebrae
2. Neoplastic disease – wedge fractures are particularly related to osteolytic metastases and osteolytic marrow tumours, e.g. multiple myeloma, leukaemia and lymphoma. Altered or obliterated normal trabeculae. Disc spaces are usually preserved until late. Paravertebral soft-tissue mass is more common in myeloma than metastases.
3. Trauma – discontinuity of trabeculae, sclerosis of the fracture line due to compressed and overlapped trabeculae. Disc space usually preserved. The lower cervical, lower dorsal and upper lumbar spine are most commonly affected. Usually no soft-tissue mass. MRI usually shows the end-plates to be spared, cf. pyogenic infection.
4. Scheuermann’s disease – irregular end-plates and numerous Schmorl’s nodes in the thoracic spine of children and young adults. Disc-space narrowing. Often progresses to a severe kyphosis. Secondary degenerative changes later.
5. Infection – destruction of end-plates adjacent to a destroyed disc.
6. Langerhans’ cell histiocytosis* – the spine is more frequently involved in eosinophilic granuloma and Hand–Schüller–Christian disease than in Letterer–Siwe disease. Most common in young people. The thoracic and lumbosacral spine are the usual sites of disease. Disc spaces are preserved.
7. Sickle-cell anaemia* – characteristic step-like depression in the central part of the end-plate.
2.4
Erosion, destruction or absence of a pedicle
3. Neurofibroma – often causes erosion of adjacent pedicle or pedicles. Chronic intramedullary tumours, typically ependymoma, cause flattening of both pedicles at affected levels, with a widened interpedicular distance.
4. TB – uncommonly. With a large paravertebral abscess.
5. Benign bone tumour – aneurysmal bone cyst or giant cell tumour.
6. Congenital absence – ± sclerosis of the contralateral pedicle.
2.5
Solitary dense pedicle
1. Osteoblastic metastasis – no change in size.
2. Osteoid osteoma* – some enlargement of the pedicle ± radiolucent nidus ± scoliosis.
3. Osteoblastoma* – larger than osteoid osteoma and more frequently a lucency with a sclerotic margin rather than a purely sclerotic pedicle.
4. Secondary to spondylolysis – ipsilateral or contralateral.
5. Secondary to congenitally absent or hypoplastic contralateral posterior elements.
2.6
Enlarged vertebral body
Local (single or multiple)
(a) Aneurysmal bone cyst* – typically purely lytic and expansile. Involves the anterior and posterior elements more commonly than the anterior or posterior elements alone. Rapid growth ± fluid–fluid levels.
(b) Haemangioma* – with a prominent vertical trabecular pattern.
(c) Giant cell tumour* – involvement of the body alone is most common. Expansion is minimal.
3. Hydatid – over 40% of cases of hydatid disease in bone occur in vertebrae.
2.8
Block vertebrae
1. Klippel–Feil syndrome – segmentation defects in the cervical spine, short neck, low hairline and limited cervical movement, especially rotation. The radiological appearance of the cervical spine resembles (1) above. C2–C3 and C5–C6 are most commonly affected. Other anomalies are frequently associated, the most important being:
(a) Scoliosis > 20° in more than 50% of patients.
(b) Sprengel’s shoulder in 30%, ± an omovertebral body.
(d) Genitourinary abnormalities in 66%; renal agenesis in 33%.
2. Isolated congenital – a failure of segmentation.
3. Rheumatoid arthritis* – especially juvenile onset rheumatoid arthritis and juvenile chronic arthritis with polyarticular onset. There may be angulation at the fusion site and this is not a feature of the congenital variety. The spinous processes do not fuse.
4. Ankylosing spondylitis* – squaring of anterior vertebral margins and calcification in the intervertebral discs and anterior and posterior longitudinal ligaments.
5. TB – vertebral body collapse and destruction of the disc space, paraspinal calcification. There may be angulation of the spine.
2.9
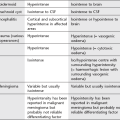
Ivory vertebral body
Single or multiple very dense vertebrae. The list excludes those causes where increased density is due to compaction of bone following collapse. If there is generalized involvement of the spine see 1.1.
2.10
Atlantoaxial subluxation
Trauma arthritides
1. Rheumatoid arthritis* – in 20–25% of patients with severe disease. Associated erosion of the odontoid may be severe enough to reduce it to a small spicule of bone.
2. Psoriatic arthropathy* – in 45% of patients with spondylitis.
3. Juvenile idiopathic arthritis* – most commonly in seropositive juvenile onset adult rheumatoid arthritis.
4. Systemic lupus erythematosus*.
5. Ankylosing spondylitis* – in 2% of cases. Usually a late feature.
Congenital
1. Down’s syndrome* – in 20% of cases. ± Odontoid hypoplasia. May, rarely, have atlanto-occipital instability.
3. Spondyloepiphyseal dysplasia.
4. Congenital absence/hypoplasia of the odontoid process – many have a history of previous trauma. (NB. In children < 9 years it is normal for the tip of the odontoid to fall well below the top of the anterior arch of the atlas.)
2.11
Intervertebral disc calcification
1. Degenerative spondylosis – in the nucleus pulposus. Usually confined to the dorsal region.
3. Calcium pyrophosphate dihydrate deposition disease*.
5. Juvenile idiopathic arthritis*.
7. Diffuse idiopathic skeletal hyperostosis (DISH) – may mimic ankylosing spondylitis.
9. Idiopathic – a transient phenomenon in children. The cervical spine is most often affected. Clinically associated with neck pain and fever but may be asymptomatic. Persistent in adults.
2.12
Bony outgrowths of the spine
Claw osteophytes

Arising from the vertebral margin with no gap and having an obvious claw appearance.
2.13
Posterior scalloping of vertebral bodies
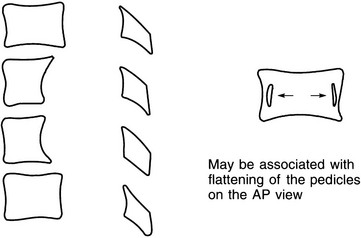
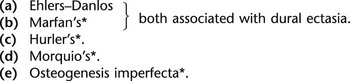
1. Tumours in the spinal canal – ependymoma (especially of the filum terminale and conus), dermoid, lipoma, neurofibroma and, less commonly, meningioma. Chronic raised intraspinal pressure distal to a tumour producing spinal block also causes extensive vertebral scalloping.
2. Neurofibromatosis* – scalloping is due to a mesodermal dysplasia and is associated with dural ectasia. Localized scalloping can also result from pressure resorption by a neurofibroma, in which case there may also be enlargement of an intervertebral foramen and flattening of one pedicle (‘dumbbell tumour’). However, multiple wide thoracic intervertebral foramina are more likely owing to lateral meningocoeles than to local tumours.
3. Acromegaly* – other spinal changes include increased AP and transverse diameters of the vertebral bodies giving a spurious impression of decreased vertebral height, osteoporosis, spur formation and calcified discs.
4. Achondroplasia* – with spinal stenosis and anterior vertebral body beaks.
5. Communicating hydrocephalus – if severe and untreated.
6. Syringomyelia – especially if the onset is before 30 years of age.
2.14
Anterior scalloping of vertebral bodies
1. Aortic aneurysm – intervertebral discs remain intact. Well-defined anterior vertebral margin. ± Calcification in the wall of the aorta.
2. Tuberculous spondylitis – with marginal erosions of the affected vertebral bodies. Disc-space destruction. Widening of the paraspinal soft tissues.
3. Lymphadenopathy – pressure resorption of bone results in a well-defined anterior vertebral body margin unless there is malignant infiltration of the bone.
2.15
Widened interpedicular distance
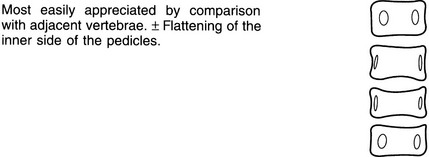
1. Meningomyelocoele – fusiform distribution of widened interpedicular distances with the greatest separation at the mid-point of the involved segment. Disc spaces are narrowed and bodies appear to be widened. Spinous processes and laminae are not identifiable. Facets may be fused into a continuous mass. Scoliosis (congenital or developmental) in 50–70% of cases ± kyphosis.
2. Intraspinal mass (see 2.16) – especially ependymoma.
3. Diastematomyelia – 50% occur between L1 and L3; 25% between T7 and T12. Widened interpedicular distances are common but not necessarily at the same level as the spur. The spur is visible in 33% of cases and extends from the neural arch forward. Laminar fusion associated with a neural arch defect at the same or adjacent level is an important sign in predicting the presence of diastematomyelia. ± Associated meningocoele, neurenteric cyst or dermoid.
2.16
Intraspinal masses
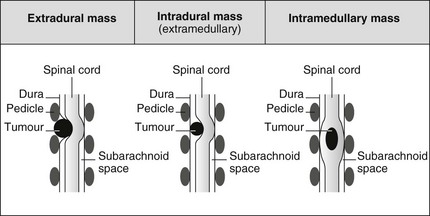
Extradural mass
1. Prolapsed or sequestrated intervertebral disc – occurs at all levels. Usually extradural, but occasionally penetrates dura, especially in thoracic region. May calcify, especially thoracic disc prolapse.
2. Metastases, myeloma and lymphoma deposits – common; look for associated vertebral infiltration. Most common sites of primary tumours are prostate, breast and lung. Thoracic spine is the most common site affected.
3. Neurofibroma – solitary, or multiple in neurofibromatosis. Lateral indentation of theca at the level of the intervertebral foramen.
4. Neuroblastoma and ganglioneuroma – tumours of childhood arising in adrenal or sympathetic chain, close to spine: direct invasion of spinal canal may occur.
5. Meningioma – may be extradural, but most are largely intradural (see below). Commonest site is thoracic; middle-aged females predominate.
6. Haematoma – may be due to trauma, dural AVM, anticoagulant therapy; some spontaneous. Long-segment extradural mass on MRI, which may show signal characteristics of blood.
7. Abscess – usually secondary to disc or vertebral sepsis. Long-segment extradural mass, with marginal enhancement on CT and MRI.
8. Arachnoid cyst – secondary to developmental dural defect. Uncommon; most spinal arachnoid cysts are intradural.
Intradural mass
1. Meningioma – as above commonly thoracic, mainly in middle-aged females. Occasional calcification.
2. Neurofibroma – usually extradural, but intradural neurofibromas occur, especially in cauda equina.
3. Metastases – from remote primary tumours, or due to CSF seeding in CNS tumours, e.g. pineal tumours, ependymoma, medulloblastoma and PNET. Lymphoma may also occur intradurally, particularly in lumbosacral canal.
Intramedullary mass
1. Ependymoma – can occur anywhere in spinal canal, but commonest at conus and in lumbar canal (from filum terminale). Very slow-growing, and bone remodelling is often seen with expansion of the spinal canal. Best shown on MRI: high signal mass on T2W images, low on T1W, but with enhancement. Associated cord cavitation may occur.
2. Astrocytoma – commonest intramedullary tumour. Appearances similar to ependymoma, but faster growing, and bone changes not a feature.
3. Dermoid (including lipoma, teratoma) – most commonly seen in conus medullaris. Different tissue elements include lipomatous tissue: low attenuation on CT, bright on T1W MRI, cystic spaces (low attenuation on CT, low signal on T1W, high on T2W MRI), and soft tissue (intermediate density on CT, and intermediate signal on T1W MRI, enhancing after gadolinium).
4. Infarct – expanding in acute phase.
5. Haematoma – cord swelling only on CT, but features of blood on MRI.