Spinal anesthesia
The mechanism of action of spinal anesthesia is due to the effect of local anesthetic agents on the individual nerve roots, effects that depend on the size and myelin content of nerve fibers, concentration of the local anesthetic agent, and duration of contact between the nerve root and the local anesthetic agent. The loss of conductivity of impulses through the fibrils follows a fixed sequence—first, sympathetic and parasympathetic activity are lost, and then sensation in the C, B, and A fibers is lost. C—fibers quit firing first, progressing finally to loss of activity in the Aα fibers, which accounts for the loss of motor function lastly. Heavy myelinated fibers present in motor nerves are most resistant to the effects of local anesthetic agents; hence, loss of activity in these nerves is the last group of nerves to be blocked. Because of the increased sensitivity of autonomic nerve fibers, blockade of these nerves extends for two or more dermatomes above the level of skin anesthesia, and blockade of motor fibers is seen two or more levels below the level of skin anesthesia (Box 122-1, Table 122-1).
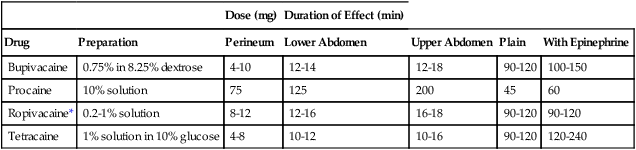
Table 122-1
Dose and Duration of Effect for Local Anesthetic Agents Commonly Administered Intrathecally
| Dose (mg) | Duration of Effect (min) | |||||
| Drug | Preparation | Perineum | Lower Abdomen | Upper Abdomen | Plain | With Epinephrine |
| Bupivacaine | 0.75% in 8.25% dextrose | 4-10 | 12-14 | 12-18 | 90-120 | 100-150 |
| Procaine | 10% solution | 75 | 125 | 200 | 45 | 60 |
| Ropivacaine* | 0.2-1% solution | 8-12 | 12-16 | 16-18 | 90-120 | 90-120 |
| Tetracaine | 1% solution in 10% glucose | 4-8 | 10-12 | 10-16 | 90-120 | 120-240 |
Contraindications to spinal anesthesia
Absolute contraindications include patient refusal, coagulation abnormalities, severe hypovolemia, increased intracranial pressure, infection, and severe stenotic aortic and mitral valvular heart disease (Box 122-2). Other relative and controversial contraindications are also listed in Box 122-2.





