Shoulder
The prerequisite to any treatment of a patient with pain in the shoulder region is a precise and comprehensive picture of the signs and symptoms as they present during the assessment and as they existed until that time. This knowledge ensures that the techniques used will suit the condition and that the degree of success will be estimated against this background. Shoulder pain can be caused by intrinsic disease of the shoulder joints or pathology in the periarticular structures, or it may originate from the cervical spine, chest, or visceral structures. Pathology is commonly related to the level of activity, and age can play a significant role. The shoulder complex is difficult to assess because of its many structures (most of which are located in a small area), its many movements, and the many lesions that can occur either inside or outside the joints. Influences such as referred pain from the cervical spine and the possibility of more than one lesion being present at one time, as well as the difficulty in deciding what weight to give to each response, make the examination even more difficult to understand. Assessment of the shoulder region often necessitates an evaluation of the cervical spine (see Chapter 3) and thoracic spine (see Chapter 8), especially the ribs to rule out referred symptoms, and the examiner must be prepared to include the cervical spine and its scanning examination in any shoulder assessment.
Applied Anatomy
The glenohumeral joint is a multiaxial, ball-and-socket, synovial joint that depends primarily on the muscles and ligaments rather than bones for its support, stability, and integrity.1 Thus, the assessment of the muscles and ligaments/capsule can play a major role in the assessment of the shoulder. The labrum, which is the ring of fibrocartilage, surrounds and deepens the glenoid cavity of the scapula about 50% (Figure 5-1).2 Only part of the humeral head is in contact with the glenoid at any one time. This joint has three axes and three degrees of freedom. The resting position of the glenohumeral joint is 55° of abduction and 30° of horizontal adduction. The close packed position of the joint is full abduction and lateral rotation. When relaxed, the humerus sits centered in the glenoid cavity; with contraction of the rotator cuff muscles, it is pushed or translated anteriorly, posteriorly, inferiorly, superiorly, or in any combination of these movements. This movement is small, but if it does not occur, full movement is impossible. The glenoid in the resting position has a 5° superior tilt or inclination and a 7° retroversion (slight medial rotation). The angle between the humeral neck and shaft is about 130°, and the humeral head is retroverted 30° to 40° relative to the line joining the epicondyle (Figure 5-2).3
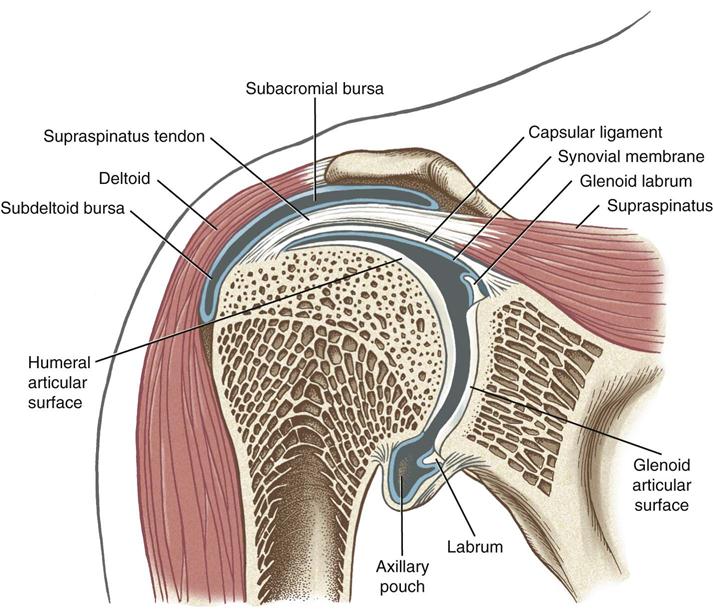
Note the subacromial and subdeltoid bursa within the subacromial space. Bursa and synovial lining are depicted in blue. The deltoid and supraspinatus muscles are also shown. (From Neuman DA: Kinesiology of the musculoskeletal system: foundations for rehabilitation, ed 2, St Louis, 2010, Mosby/Elsevier, p. 143.)
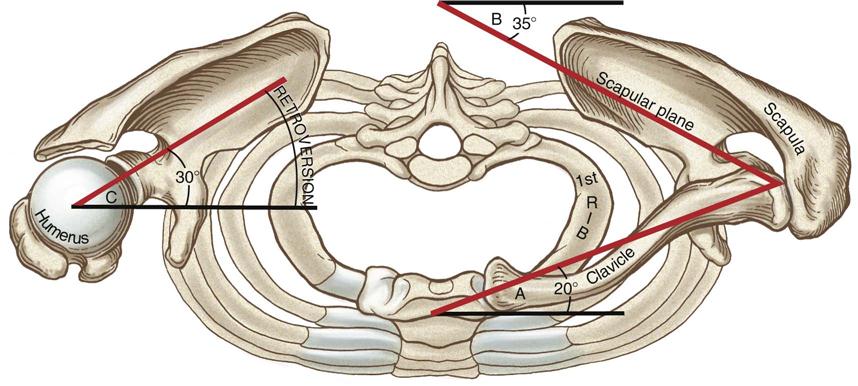
Angle A: The clavicle is deviated about 20° posterior to the frontal plane. Angle B: The scapula (scapular plane or “scaption”) is deviated about 35° anterior to the front plane. Angle C: Retroversion of the humeral head about 30° posterior to the medial-lateral axis at the elbow. The right clavicle and acromion have been removed to expose the top of the right glenohumeral joint. (From Neuman DA: Kinesiology of the musculoskeletal system: foundations for rehabilitation, ed 2, St Louis, 2010, Mosby/Elsevier, p. 123.)
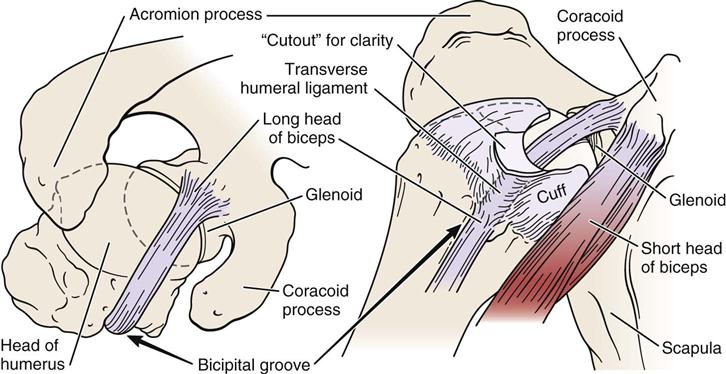
The rotator cuff muscles play an integral role in shoulder movement. Their positioning on the humerus may be visualized by “cupping” the shoulder with the thumb anteriorly, as shown in Figure 5-3. The biceps tendon (Figure 5-4) runs between the thumb and index finger just anterior to the index finger. The rotator cuff controls osteokinematic and arthrokinematic motion of the humeral head in the glenoid and along with the biceps depresses the humeral head during movements into elevation.
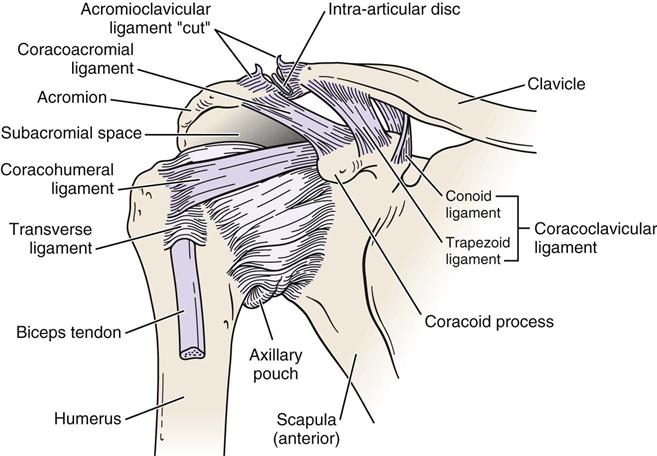
The primary ligaments of the glenohumeral joint—the superior, middle, and inferior glenohumeral ligaments—play an important role in stabilizing the shoulder (Figure 5-5).3,4 The superior glenohumeral ligament’s primary role is limiting inferior translation in adduction. It also restrains anterior translation and lateral rotation up to 45° abduction. The middle glenohumeral ligament, which is absent in 30% of the population, limits lateral rotation between 45° and 90° abduction. The inferior glenohumeral ligament is the most important of the three ligaments. It has an anterior and posterior band with a thin “axillary pouch” in between, so it acts much like a hammock or sling. It supports the humeral head above 90° abduction, limiting inferior translation while the anterior band tightens on lateral rotation and the posterior band tightens on medial rotation.5 Excessive lateral rotation, as seen in throwing, may lead to stretching of the anterior portion of the ligament (and capsule), thereby increasing glenohumeral laxity.6 The coracohumeral ligament primarily limits inferior translation and helps limit lateral rotation below 60° abduction. This ligament is found in the rotator interval between the anterior border of the supraspinatus tendon and the superior border of the subscapularis tendon, thus the ligament unites the two tendons anteriorly (Figure 5-6).7–9 The rotator interval consists of fibers of the coracohumeral ligament, superior glenohumeral ligament, glenohumeral joint capsule, and part of the tendons of supraspinatus and subscapularis.9 Injury to these structures can lead to contractures, biceps tendon instability, and anterior glenohumeral instability.9 See Table 5-1 for structures limiting movement in different degrees of abduction.5,10 The coracoacromial ligament forms an arch over the humeral head, acting as a block to superior translation.11 The transverse humeral ligament forms a roof over the bicipital groove to hold the long head of biceps tendon within the groove. The capsular pattern of the glenohumeral joint is lateral rotation most limited, followed by abduction and medial rotation. Branches of the posterior cord of the brachial plexus and the suprascapular, axillary, and lateral pectoral nerves innervate the joint.
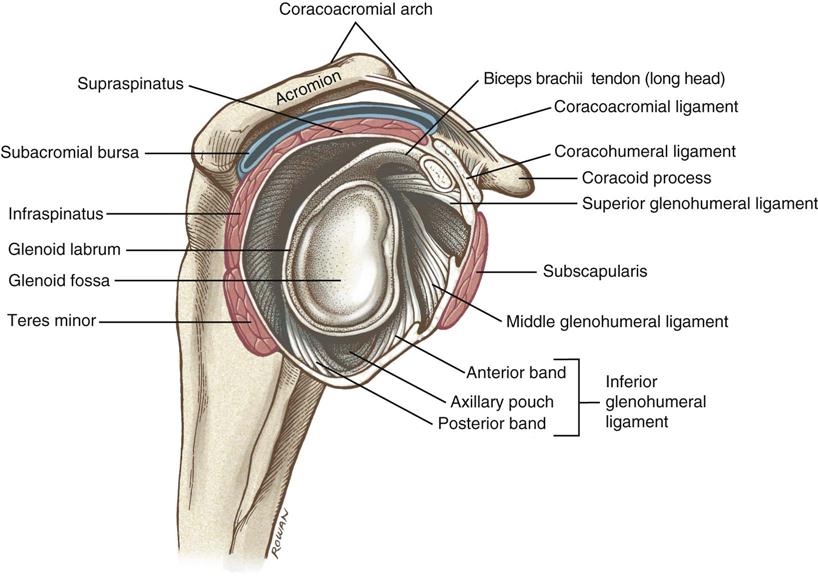
The humerus has been removed to expose the capsular ligaments and the glenoid fossa. Note the prominent coracoacromial arch and underlying subacromial bursa (blue). The four rotator cuff muscles are shown in red. (From Neuman DA: Kinesiology of the musculoskeletal system: foundations for rehabilitation, ed 2, St Louis, 2010, Mosby/Elsevier, p. 139.)
TABLE 5-1
Structures Limiting Movement in Different Degrees of Abduction
| Angle of Abduction | Lateral Rotation | Neutral | Medial Rotation |
| 0° | Superior GH ligament Anterior capsule |
Coracohumeral ligament Superior GH ligament Capsule (anterior and posterior) Supraspinatus |
Posterior capsule |
| 0° to 45° (note: 30° to 45° abduction in scapular plane [resting position]—maximum looseness of shoulder) |
Coracohumeral ligament Superior GH ligament Anterior capsule |
Middle GH ligament Posterior capsule Subscapularis Infraspinatus Teres minor |
Posterior capsule |
| 45° to 60° | Middle GH ligament Coracohumeral ligament Inferior GH ligament (anterior band) Anterior capsule |
Middle GH ligament Inferior GH ligament (especially anterior portion) Subscapularis Infraspinatus Teres minor |
Inferior GH ligament (posterior band) Posterior capsule |
| 60° to 90° | Inferior GH ligament (anterior band) Anterior capsule |
Inferior GH ligament (especially posterior portion) Middle GH ligament |
Inferior GH ligament (posterior band) Posterior capsule |
| 90° to 120° | Inferior GH ligament (anterior band) Anterior capsule |
Inferior GH ligament | Inferior GH ligament (posterior band) Posterior capsule |
| 120° to 180° | Inferior GH ligament (anterior band) Anterior capsule |
Inferior GH ligament | Inferior -H ligament (posterior band) Posterior capsule |
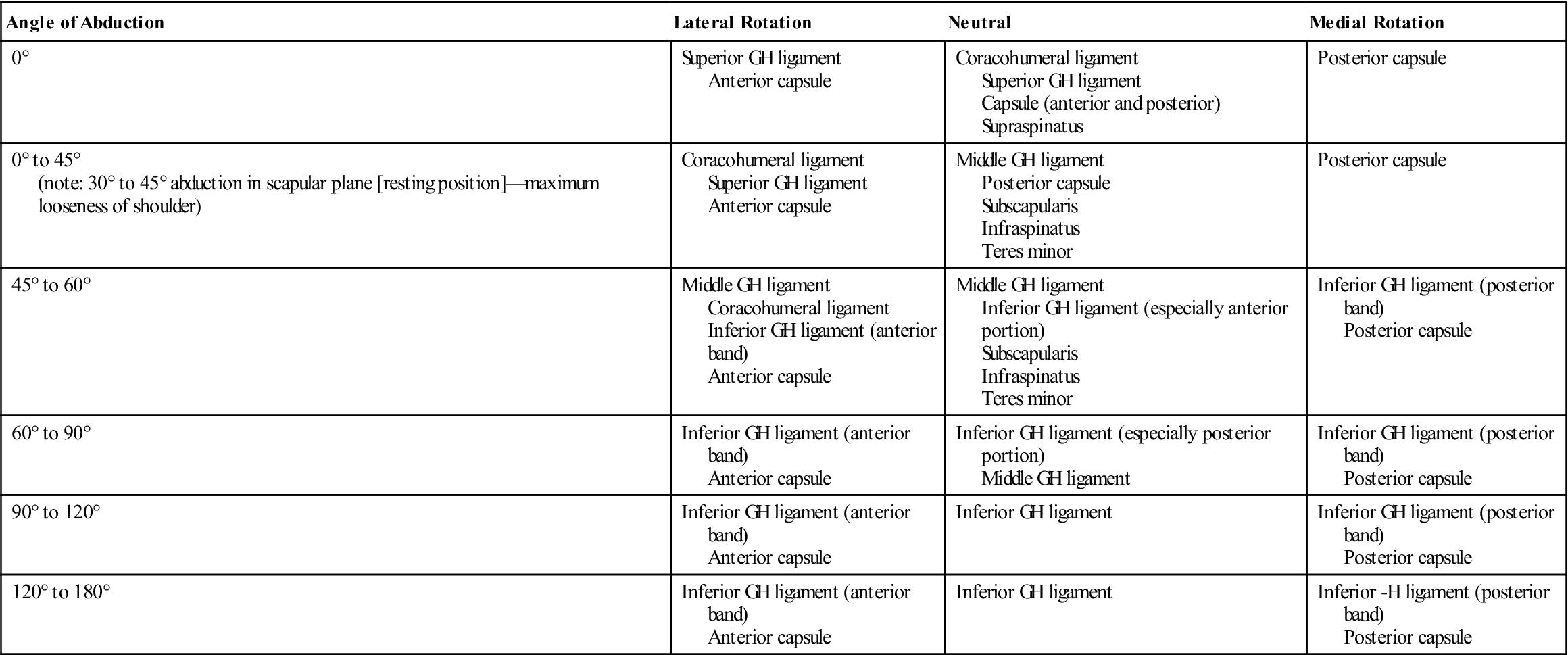
Data from Curl LA, Warren RF: Glenohumeral joint stability—selective cutting studies on the static capsular restraints. Clin Orthop Relat Res 330:54–65, 1996; and Peat M, Culham E: Functional anatomy of the shoulder complex. In Andrews JR, Wilks KE, editors: The athlete’s shoulder, New York, 1994, Churchill Livingstone.
The acromioclavicular joint is a plane synovial joint that augments the range of motion (ROM) of the humerus in the glenoid (Figure 5-7). The bones making up this joint are the acromion process of the scapula and the lateral end of the clavicle. The acromion may have different undersurface shapes or types: type I—flat (17%), type II—curved (43%), type III—hooked (39%), and type IV—convex (upturned) (1%) (Figure 5-8).12 About 70% of rotator cuff tears are associated with a hooked acromion.12 Some believe the hooked acromion is not an anatomical variant but is the result of ossification of the coracoacromial ligament at its attachment to the acromion.13 The joint has three degrees of freedom. The capsule, which is fibrous, surrounds the joint. An articular disc may be found within the joint. Rarely does the disc separate the acromion and clavicular articular surfaces. This joint depends on ligaments for its strength. The acromioclavicular ligaments surround the joint and control horizontal motion of the clavicle.14 These are commonly the first ligaments injured when the joint is stressed. The coracoclavicular ligament is the primary support of the acromioclavicular joint. It has two portions: the conoid (medial) and trapezoid (lateral) parts, and they control the vertical motion of the clavicle.14,15 If a step deformity occurs, this ligament has been torn. In the resting position of the joint, the arm rests by the side in the normal, standing position. In the close packed position of the acromioclavicular joint, the arm is abducted to 90°. The indication of a capsular pattern in the joint is pain at the extreme ROM, especially in horizontal adduction (cross-flexion) and full elevation. This joint is innervated by branches of the suprascapular and lateral pectoral nerve.
Note the subacromial space or supraspinatus outlet located between the top of the humeral head and the underside of the acromion. (Modified from Neumann DA: Kinesiology of the musculoskeletal system: foundations for rehabilitation, St Louis, 2002, Mosby, p. 107.)
The sternoclavicular joint, along with the acromioclavicular joint, enables the humerus in the glenoid to move through a full 180° of abduction (Figure 5-9). It is a saddle-shaped synovial joint with 3° of freedom and is made up of the medial end of the clavicle, the manubrium sternum, and the cartilage of the first rib. It is the joint that joins the appendicular skeleton to the axial skeleton.16 A substantial disc is between the two bony joint surfaces, and the capsule is thicker anteriorly than posteriorly. The disc separates the articular surfaces of the clavicle and sternum and adds significant strength to the joint because of attachments, thereby preventing medial displacement of the clavicle. Like the acromioclavicular joint, the joint depends on ligaments for its strength. The ligaments of the sternoclavicular joint include the anterior and posterior sternoclavicular ligaments, which support the joint anteriorly and posteriorly, the interclavicular ligament, and the costoclavicular ligament running from the clavicle to the first rib and its costal cartilage. This is the main ligament maintaining the integrity of the sternoclavicular joint. The movements possible at this joint and at the acromioclavicular joint are elevation, depression, protrusion, retraction, and rotation. The close packed position of the sternoclavicular joint is full or maximum rotation of the clavicle, which occurs when the upper arm is in full elevation. The resting position and capsular pattern are the same as with the acromioclavicular joint. The joint is innervated by branches of the anterior supraclavicular nerve and the nerve to the subclavius muscle. Major vessels and the trachea lie close behind the sternum and the sternoclavicular joint (see Figure 5-9, B).16
Although the scapulothoracic joint is not a true joint, it functions as an integral part of the shoulder complex and must be considered in any assessment because a stable scapula enables the rest of the shoulder to function correctly. Some texts call this structure the scapulocostal joint. This “joint” consists of the body of the scapula and the muscles covering the posterior chest wall. The muscles acting on the scapula help to control its movements. The medial border of the scapula is not parallel with the spinous processes but is angled about 3° away (top to bottom), and the scapula lies 20° to 30° forward relative to the sagittal plane.3 Because it is not a true joint, it does not have a capsular pattern nor a close packed position. The resting position of this joint is the same as for the acromioclavicular joint. The scapula extends from the level of T2 spinous process to T7 or T9 spinous process, depending on the size of the scapula. Because the scapula acts as a stable base for the rotator cuff muscles, the muscles controlling its movements must be strong and balanced because the joint funnels the forces of the trunk and legs into the arm.17
Patient History
In addition to the questions listed under “Patient History” in Chapter 1, the examiner should obtain the following information from the patient.18 Most commonly, the patient complains of pain, especially on movement, restricted motion, or shoulder instability.
1. What is the patient’s age? Many problems of the shoulder can be age-related. For example, rotator cuff degeneration usually occurs in patients who are between 40 and 60 years of age. Rotator cuff tears, though, can occur at any age.19 Litaker, et al.20 suggested that external rotation weakness, night pain, and age over 65 are indicative of rotator cuff tears. Primary impingement due to degeneration and weakness is usually seen in patients older than 35, whereas secondary impingement due to instability caused by weakness in the scapular or humeral control muscles is more common in people in their late teens or twenties, especially those involved in vigorous overhead activities, such as swimmers or pitchers in baseball.21 Calcium deposits may occur between the ages of 20 and 40.22 Chondrosarcomas may be seen in those older than 30 years of age, whereas frozen shoulder is seen in persons between the ages of 45 and 60 years if it results from causes other than trauma (Tables 5-2 and 5-3). Frozen shoulder due to trauma can occur at any age but is more common with increased age.
2. Does the patient support the upper limb in a protected position (Figure 5-10) or hesitate to move it? This action could mean that one of the joints of the shoulder complex is unstable or that there is an acute problem in the shoulder. In some cases, patients with lax shoulders ask, “What happens when I do this?” In effect, the patient is subluxing the shoulder (Figure 5-11 ). This may or may not be pathological, but it is a sign of voluntary instability in which the patient uses his or her muscles to sublux the humerus in the glenoid, stressing the labrum and inert tissues.
3. If there was an injury, what exactly was the mechanism of injury? Did the patient injure themself with a fall on out-stretched hand (FOOSH), which could indicate a fracture or dislocation of the glenohumeral joint? Did the patient fall on or receive a blow to the tip of the shoulder, or did the patient land on the elbow, driving the humerus up against the acromion? This finding may indicate an acromioclavicular dislocation or subluxation.23,24 Does the shoulder feel unstable or feel like it is “coming out” during movement? Does the arm “go dead” when doing activity? “Going dead” implies the patient cannot use the arm functionally because of pain and a subjective feeling of unease when using the arm.25 Patients with instability may appear normal on clinical examination, especially if shoulder muscles are not fatigued. Many overuse injuries are more evident immediately after the patient does repeated activity.26 This may indicate gross or anatomical instability, such as in recurrent shoulder dislocation, subluxation, or subtle translational instability. The spectrum of instability varies from gross or anatomical instability—the TUBS type (Traumatic onset, Unidirectional anterior with a Bankart lesion responding to Surgery) to a more subtle translational instability—the AMBRI type (Atraumatic cause, Multidirectional with Bilateral shoulder findings with Rehabilitation as appropriate treatment and, rarely, Inferior capsular shift surgery).
4. Are there any movements or positions that cause the patient pain or symptoms? If so, which ones? The examiner must keep in mind that cervical spine movements may cause pain in the shoulder. Persons who have had recurrent dislocations/instability of the shoulder may find that any movement involving lateral rotation bothers them, because this movement is involved in anterior dislocations of the shoulder. Questions related to instability should include27:
a. How many episodes have there been in the last year?
b. Was there an injury that precipitated this?
c. What direction does the shoulder “go out” most times?
d. Have you ever needed help getting the shoulder back into proper position within the joint?
Recurrent dislocators may sometimes show pain at extreme of medial rotation when the humeral head is “tightened” against the anterior glenoid. Long head of biceps pathology causes pain that moves medially and laterally with medial and lateral rotation of the shoulder.28 Excessive abduction and lateral rotation may lead to dead-arm syndrome in which the patient feels a sudden paralyzing pain and weakness in the shoulder.25 This finding often indicates altered shoulder mechanics commonly involving a tight posterior capsule, altered arthrokinematics of the glenohumeral joint, and scapular dyskinesia.25,29,30 In throwers, the condition may be referred to as a “SICK” scapula (malposition of Scapula, prominence of Inferior medial border of scapula, Coracoid pain and malposition, and scapular dysKinesia).31 If the patient complains of pain during specific phases of pitching (for example, during the late cocking and acceleration phases), anterior instability should be considered even in the presence of minimal clinical signs.32 Commonly, instability and secondary impingement occur together. Secondary impingement implies that although impingement signs are present, they result from a primary problem somewhere else, commonly in the scapular or humeral control or stabilizer muscles. Primary impingement implies that impingement or pinching is the primary cause of the pain.
Stability of the shoulder depends on both dynamic stabilizers (the muscles) and static stabilizers (e.g., the capsule, labrum).5 Night pain and resting pain are often related to rotator cuff tears and, on occasion, to tumors; activity-related pain usually signifies paratenonitis. Arthritis pain commonly shows, at least initially, at the extremes of motion. Acromioclavicular pain is especially evident at greater than 90° of abduction and tends to be localized to the joint. Similarly, sternoclavicular pain is localized to the joint and increases on horizontal adduction.
5. What is the extent and behavior of the patient’s pain? For example, deep, boring, toothache-like pain in the neck, shoulder region, or both may indicate thoracic outlet syndrome33 (Figure 5-12) or acute brachial plexus neuropathy. Strains of the rotator cuff usually cause dull, toothache-like pain that is worse at night, whereas acute calcific tendinitis usually causes a hot, burning type of pain. Sprain of the first or second rib from direct trauma or sudden contraction of the scaleni may mimic an acute impingement or rotator cuff injury.34
6. Are there any activities that cause or increase the pain? For example, bicipital paratenonitis or tendinosis35 are often seen in skiers and may result from holding on to a ski tow; in cross-country skiing, it may result from poling (using the pole for propulsion). Paratenonitis is inflammation of the paratenon of the tendon. The paratenon is the outer covering of the tendon whether or not it is lined with synovium. Tendinosis is actual degeneration of the tendon itself. With chronic overuse, tendinosis is more likely than paratenonitis35,36 (Table 5-4; see Table 1-20). Elite swimmers may train for more than 15,000 m daily, which can lead to stress overload (repetitive microtrauma) of the structures of the shoulder. Does throwing or reaching alter the pain? If so, what positions cause pain or discomfort? These questions may indicate which structures are injured.
8. What is the patient unable to do functionally? Is the patient able to talk or swallow? Is the patient hoarse? These signs could indicate an injury to the sternoclavicular joint (if there is swelling) or a posterior dislocation of the joint because pressure is being applied to the trachea. In addition, determining whether the shoulder has been overstressed or overused is important.37 For example, in swimmers and baseball pitchers, it is important to determine38:
a. The age when the patient first began the activity
b. The total years throwing/swimming
c. The number of pitches thrown per outing
d. The number of games/innings pitched per year
e. The distances swam per week
f. The strokes used/types of pitches thrown
g. The amount of rest between outings
h. Whether there was any complete rest from activity during year
i. Whether there was any previous injury related to the activity
j. The phase of activity that produces the symptoms
9. How long has the problem bothered the patient? For example, an idiopathic frozen shoulder goes through three stages: the condition becomes progressively worse, plateaus, and then progressively improves, with each stage lasting 3 to 5 months.39,40
10. Is there any indication of muscle spasm, deformity, bruising, wasting, paresthesia, or numbness?41 These findings can help the examiner determine the acuteness of the condition and, potentially, the structures injured.
11. Does the patient complain of weakness and heaviness in the limb after activity? Does the limb tire easily? These findings may indicate vascular involvement. Are there any venous symptoms, such as swelling or stiffness, that may extend all the way to the fingers? Are there any arterial symptoms, such as coolness or pallor in the upper limb? These complaints may result from pressure on an artery, a vein, or both. An example is thoracic outlet syndrome (see Figure 5-12), in which pressure may be applied to the vascular or neurological structures as they enter the upper limb in three locations: at the scalene triangle, at the costoclavicular space, and under the pectoralis minor and the coracoid process.42,43 Excessive repetitive demands placed on the shoulder (such as, those seen in pitching) may lead to thoracic outlet syndrome, axillary artery occlusion, effort thrombosis, or pressure in the quadrilateral space. (The quadrilateral space has as its boundaries the medial border of the humerus laterally, the lateral border of the long head of triceps medially, the inferior border of teres minor, and the superior border of teres major.)44
12. Is there any indication of nerve injury? The examiner should evaluate the nerves and the muscles supplied by the nerves to determine possible nerve injury. Any history of weakness, numbness, or paresthesia may indicate nerve injury (Table 5-5). For example, the suprascapular nerve may be injured as it passes through the suprascapular notch under the transverse scapular ligament, leading to atrophy and paralysis of the supraspinatus and infraspinatus muscles. The examiner should listen to the patient history carefully, because this condition could mimic a third-degree (rupture) strain of the supraspinatus tendon. Another potential nerve injury is one to the axillary (circumflex) nerve (Figure 5-13) or musculocutaneous nerve (Figure 5-14) after dislocation of the glenohumeral joint. With an axillary nerve injury, the deltoid muscle and the teres minor muscle are atrophied and weak or paralyzed. The radial nerve (see Figure 5-13 ) is sometimes injured as it winds around the posterior aspect of the shaft of the humerus. The injury frequently occurs when the humeral shaft is fractured. If the nerve is damaged in this location, the extensors of the elbow, wrist, and fingers are affected, and an altered sensation occurs in the radial nerve sensory distribution.
13. Which hand is dominant? Often the dominant shoulder is lower than the nondominant shoulder and the ROM may not be the same for both. Usually, the dominant shoulder shows greater muscularity and can show different ROM from the nondominant shoulder.45
TABLE 5-2
| Rotator Cuff Lesions | Frozen Shoulder | Atraumatic Instability | Cervical Spondylosis | |
| History | Age 30 to 50 years Pain and weakness after eccentric load |
Age 45+ (insidious type) Insidious onset or after trauma or surgery Functional restriction of lateral rotation, abduction, and medial rotation |
Age 10 to 35 years Pain and instability with activity No history of trauma |
Age 50+ years Acute or chronic |
| Observation | Normal bone and soft tissue outlines Protective shoulder hike may be seen |
Normal bone and soft-tissue outlines | Normal bone and soft-tissue outlines | Minimal or no cervical spine movement Torticollis may be present |
| Active movement | Weakness of abduction or rotation, or both Crepitus may be present |
Restricted ROM Shoulder hiking |
Full or excessive ROM | Limited ROM with pain |
| Passive movement | Pain if impingement occurs | Limited ROM, especially in lateral, rotation, abduction, and medial rotation (capsular pattern) | Normal or excessive ROM | Limited ROM (symptoms may be exacerbated) |
| Resisted isometric movement | Pain and weakness on abduction and lateral rotation | Normal, when arm by side | Normal | Normal, except if nerve root compressed Myotome may be affected |
| Special tests | Drop-arm test positive Empty can test positive |
None | Load and shift test positive Apprehension test positive Relocation test positive Augmentation tests positive |
Spurling’s test positive Distraction test positive ULNT positive Shoulder abduction test positive |
| Sensory function and reflexes | Not affected | Not affected | Dermatomes affected Reflexes affected |
|
| Palpation | Tender over rotator cuff | Not painful unless capsule is stretched | Anterior or posterior pain | Tender over appropriate vertebra or facet |
| Diagnostic imaging | Radiography: Upward displacement of humeral head; acromial spurring MRI diagnostic |
Radiography: Negative Arthrography: Decreased capsular size |
Negative | Radiography: Narrowing osteophytes |
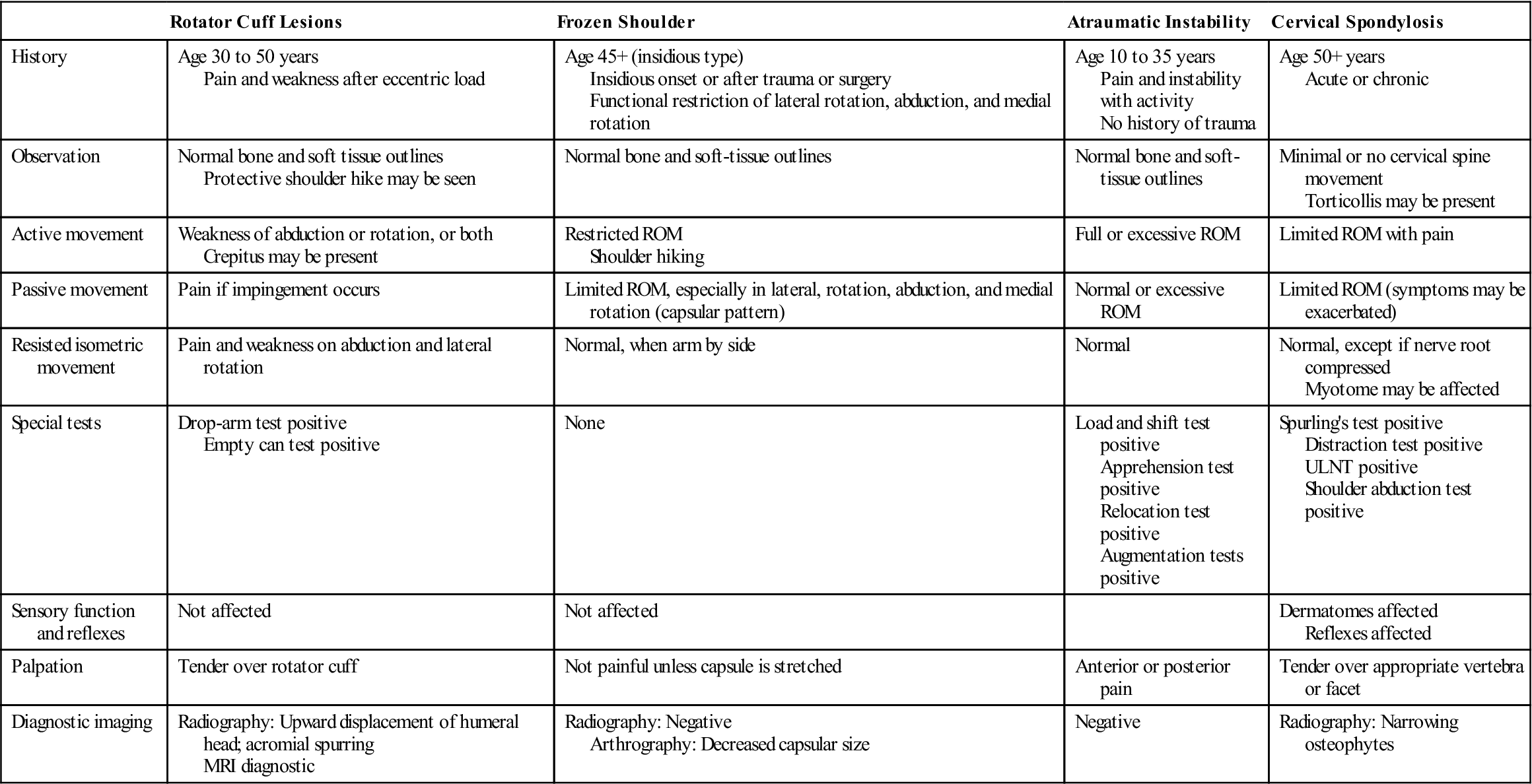
MRI, Magnetic resonance imaging; ROM, range of motion; ULNT, upper limb neurodynamic (tension) test.
TABLE 5-3
Differential Diagnosis of Shoulder Pathology
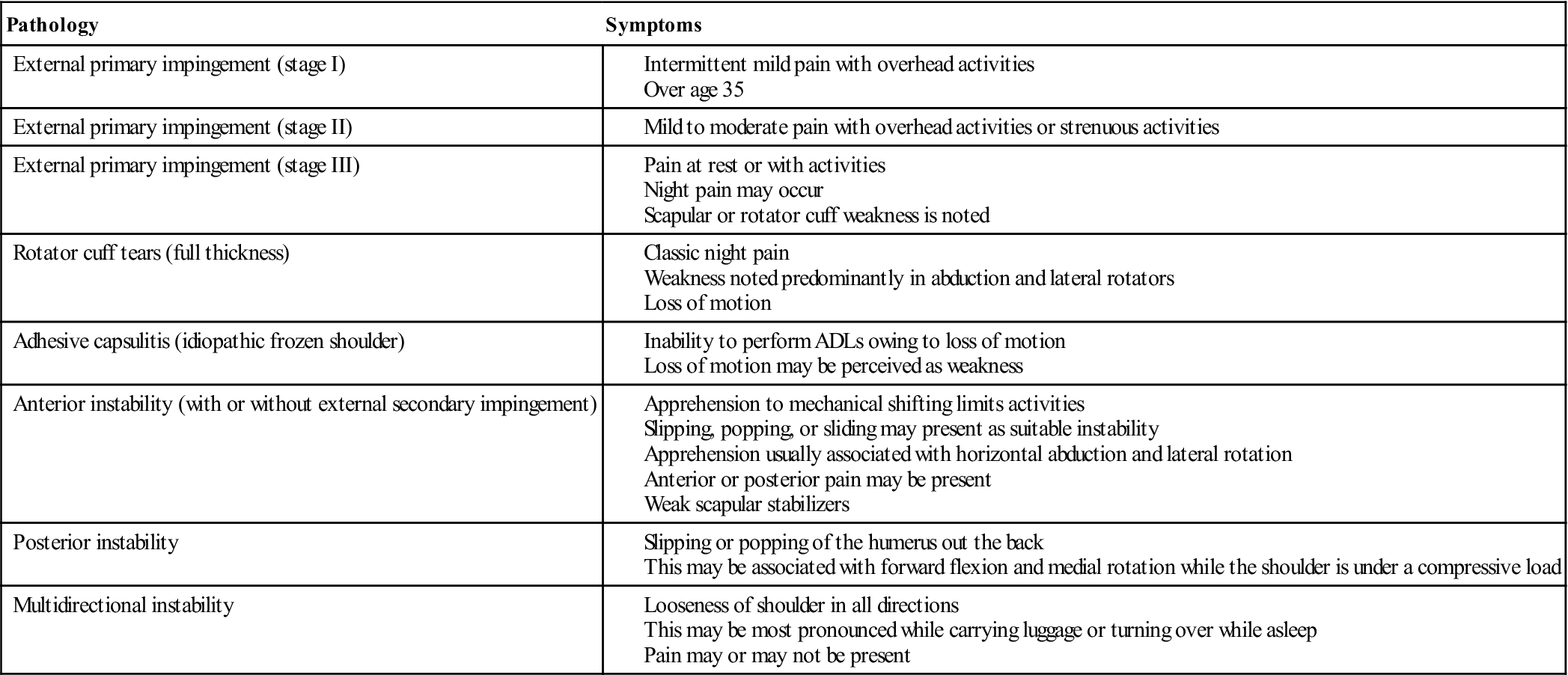
ADL, Activity of daily living.
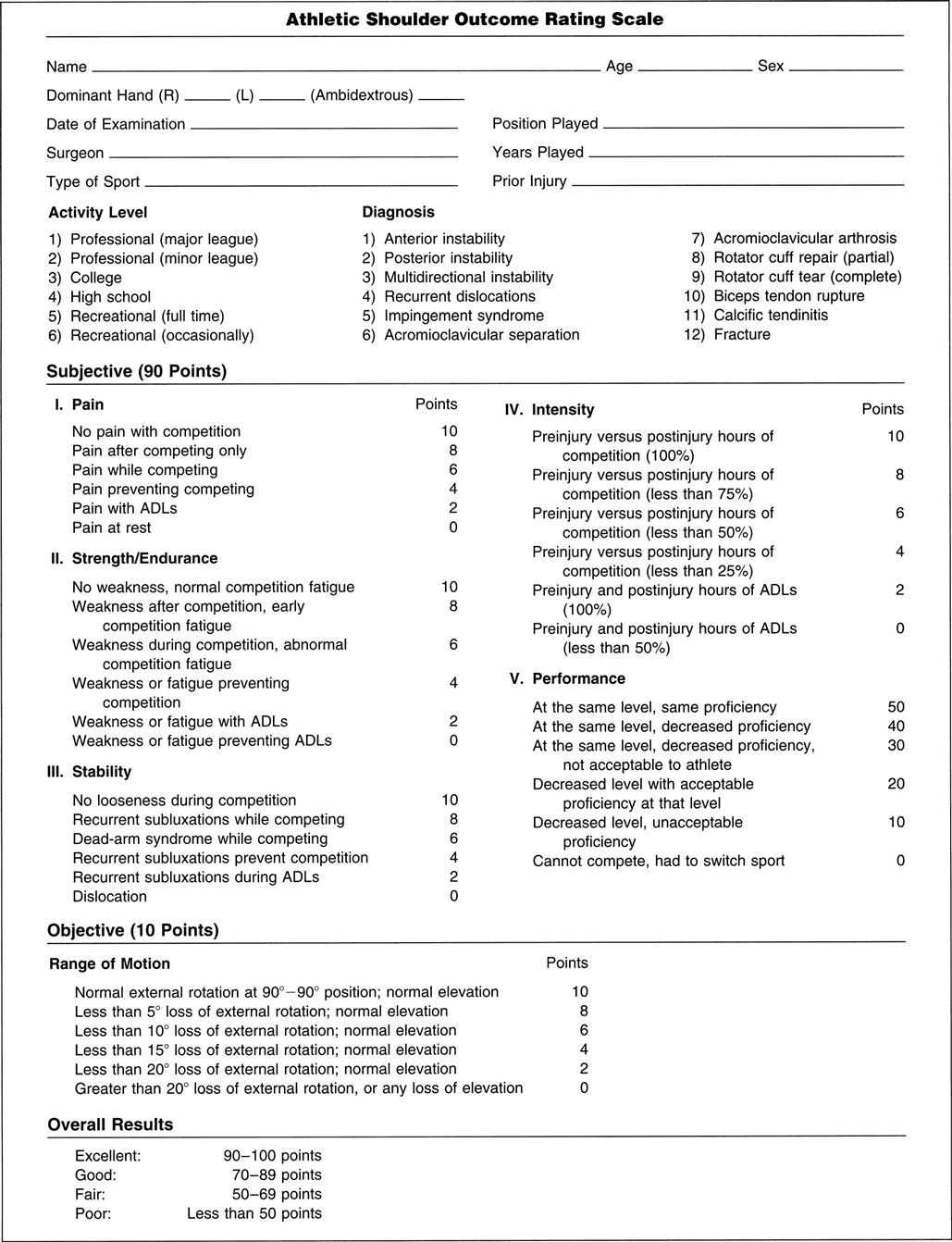
Modified from Maughon TS, Andrews JR: The subjective evaluation of the shoulder in the athlete. In Andrews JR, Wilk KE, editors: The athlete’s shoulder, New York, 1994, Churchill-Livingstone, p. 36.

Note how the patient uses her muscles to sublux the humerus in the glenoid, resulting in an anterior sulcus in each shoulder.
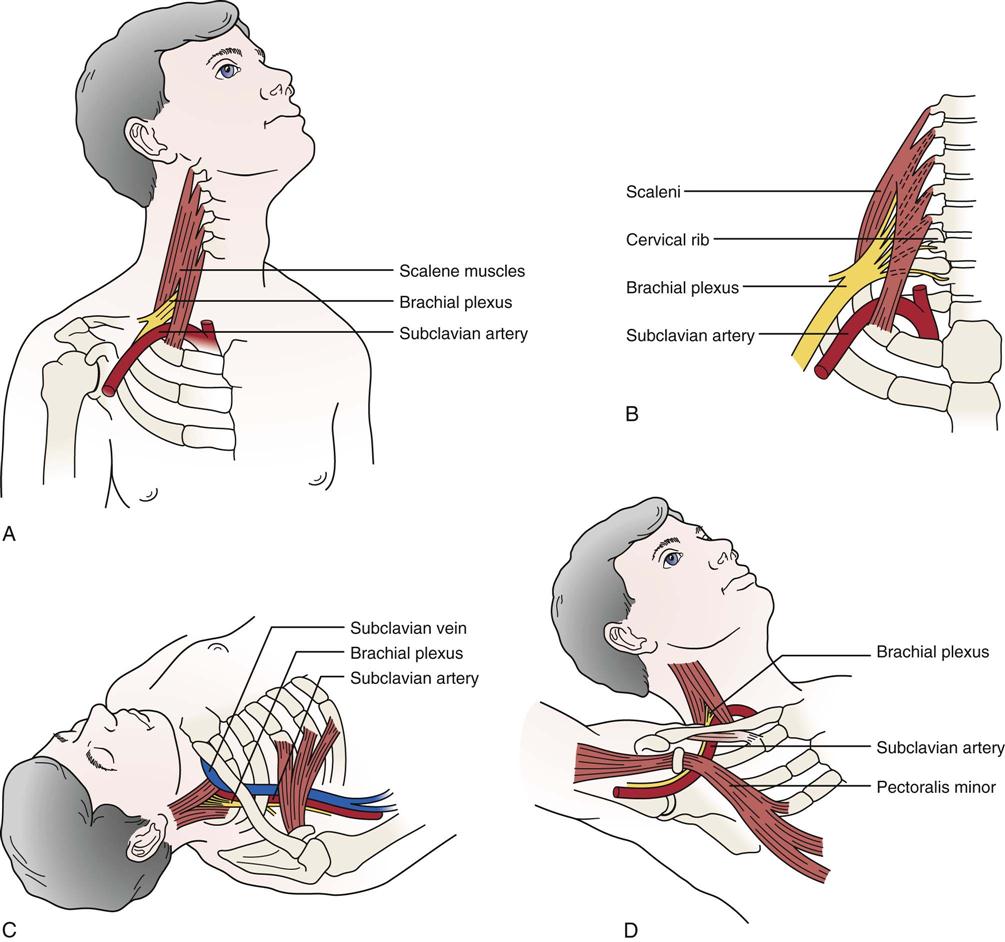
A, Scalenus anterior syndrome. B, Cervical rib syndrome. C, Costoclavicular space syndrome. D, Hyperabduction syndrome (abduction, extension, and lateral rotation).
TABLE 5-4
Implications of the Diagnosis of Tendinosis Compared with Tendinitis
| Trait | Overuse Tendinosis | Overuse Tendinitis |
| Prevalence | Common | Rare |
| Time for recovery, early presentation | 6 to 10 weeks | Several days to 2 weeks |
| Time for full recovery, chronic presentation | 3 to 6 months | 4 to 6 weeks |
| Likelihood of full recovery to sport from chronic symptoms | Approximately 80% | 99% |
| Focus of conservative therapy | Encouragement of collagen-synthesis maturation and strength | Anti-inflammatory modalities and drugs |
| Role of surgery | Excise abnormal tissue | Not known |
| Prognosis for surgery | 70% to 85% | 95% |
| Time for recovery from surgery | 4 to 6 months | 3 to 4 weeks |
From Khan KM, et al: Overuse tendinosis, not tendonitis. Part 1: a new paradigm for a difficult clinical problem. Phys Sportsmed 28:43, 2000. Reproduced with permission of McGraw-Hill.
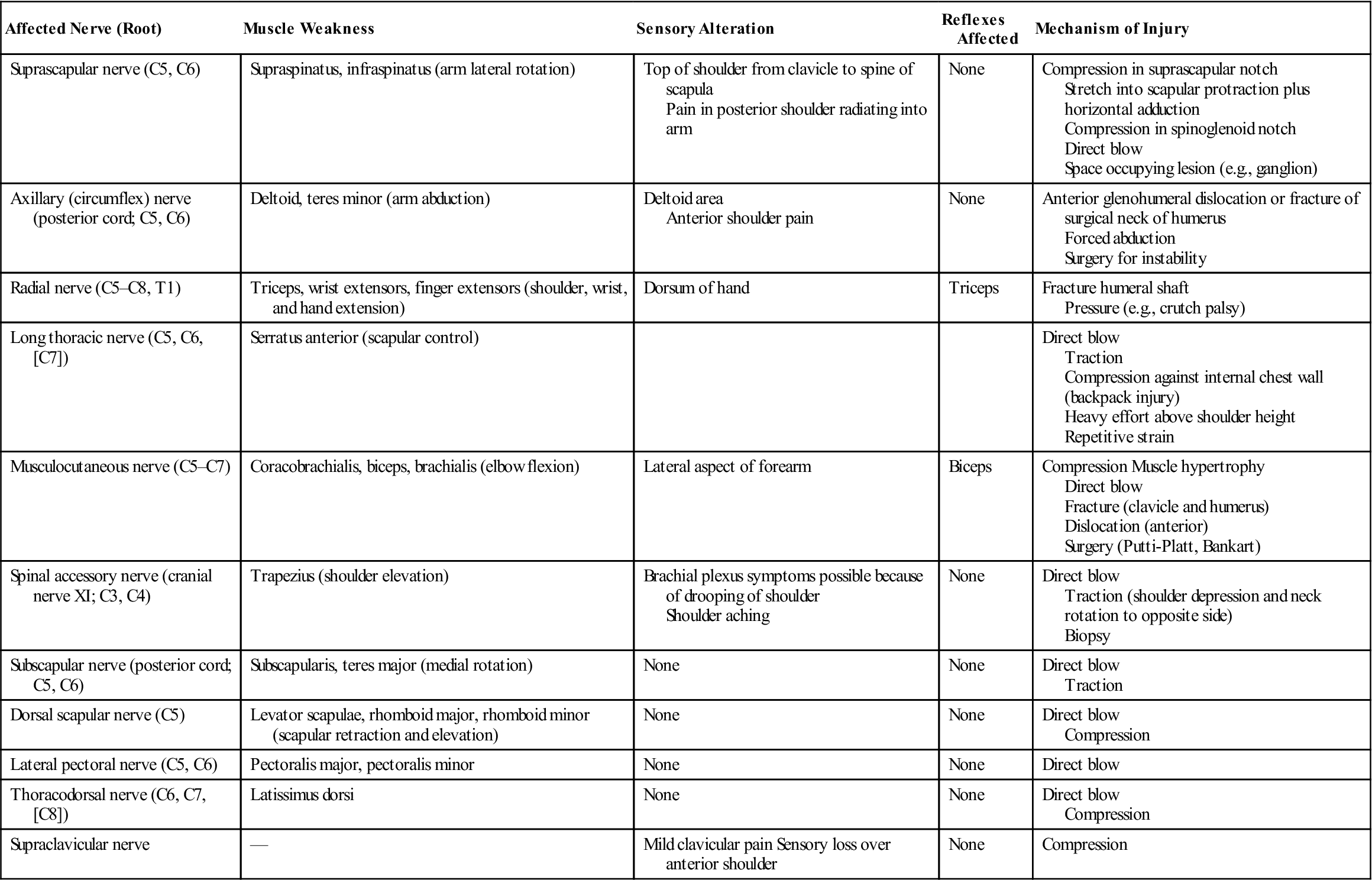
TABLE 5-5
Peripheral Nerve Injuries (Neuropathy) About the Shoulder
| Affected Nerve (Root) | Muscle Weakness | Sensory Alteration | Reflexes Affected | Mechanism of Injury |
| Suprascapular nerve (C5, C6) | Supraspinatus, infraspinatus (arm lateral rotation) | Top of shoulder from clavicle to spine of scapula Pain in posterior shoulder radiating into arm |
None | Compression in suprascapular notch Stretch into scapular protraction plus horizontal adduction Compression in spinoglenoid notch Direct blow Space occupying lesion (e.g., ganglion) |
| Axillary (circumflex) nerve (posterior cord; C5, C6) | Deltoid, teres minor (arm abduction) | Deltoid area Anterior shoulder pain |
None | Anterior glenohumeral dislocation or fracture of surgical neck of humerus Forced abduction Surgery for instability |
| Radial nerve (C5–C8, T1) | Triceps, wrist extensors, finger extensors (shoulder, wrist, and hand extension) | Dorsum of hand | Triceps | Fracture humeral shaft Pressure (e.g., crutch palsy) |
| Long thoracic nerve (C5, C6, [C7]) | Serratus anterior (scapular control) | Direct blow Traction Compression against internal chest wall (backpack injury) Heavy effort above shoulder height Repetitive strain |
||
| Musculocutaneous nerve (C5–C7) | Coracobrachialis, biceps, brachialis (elbow flexion) | Lateral aspect of forearm | Biceps | Compression Muscle hypertrophy Direct blow Fracture (clavicle and humerus) Dislocation (anterior) Surgery (Putti-Platt, Bankart) |
| Spinal accessory nerve (cranial nerve XI; C3, C4) | Trapezius (shoulder elevation) | Brachial plexus symptoms possible because of drooping of shoulder Shoulder aching |
None | Direct blow Traction (shoulder depression and neck rotation to opposite side) Biopsy |
| Subscapular nerve (posterior cord; C5, C6) | Subscapularis, teres major (medial rotation) | None | None | Direct blow Traction |
| Dorsal scapular nerve (C5) | Levator scapulae, rhomboid major, rhomboid minor (scapular retraction and elevation) | None | None | Direct blow Compression |
| Lateral pectoral nerve (C5, C6) | Pectoralis major, pectoralis minor | None | None | Direct blow |
| Thoracodorsal nerve (C6, C7, [C8]) | Latissimus dorsi | None | None | Direct blow Compression |
| Supraclavicular nerve | — | Mild clavicular pain Sensory loss over anterior shoulder | None | Compression |
Observation
The patient must be suitably undressed so that the examiner can observe the bony and soft-tissue contours of both shoulders and determine whether they are normal and symmetric. When observing the shoulder, the examiner looks at the head, the cervical spine, the thorax (especially the posterior aspect), and the entire upper limb. The hand, for example, may show vasomotor changes that result from problems in the shoulder, including shiny skin, hair loss, swelling, and muscle atrophy.
It is important to observe the patient as he or she removes clothes from the upper body and later replaces them. For example, does the patient undress the affected arm last or dress it first? This pattern indicates that the patient is limiting the movement of the arm as much as possible, signifying possible pathology. The patient’s actions give some indication of functional restriction, pain, or weakness in the upper limb.
As part of the observation, noting whether the patient can assume a “neutral pelvis” position is important, because an abnormal pelvic position can lead to an abnormal scapulothoracic, glenohumeral, and cervical spine position and abnormal kinematics in these joints. In addition, kinematics plays a role in how much force can be generated by the lower quadrant that contributes to an activity. For example, about 50% of the force of throwing is normally generated by the lower quadrant. Three questions must be asked by the examiner related to the “neutral pelvic” position:
1. Can the patient get into the “neutral pelvis” position?
3. Can the patient control a dynamic “neutral pelvis” while doing dynamic shoulder movements?
If the answer to any of the questions is negative, the examiner has to consider including the pelvis in the treatment plan for the shoulder.
Anterior View
When looking at the patient from the anterior view (Figure 5-15, A), the examiner should begin by ensuring that the head and neck are in the midline of the body and observing their relation to the shoulders. A forward head posture is often associated with rounded shoulders, a medially rotated humerus and a protracted scapula resulting in the humeral head translating anteriorly, a tight posterior capsule, tightness of the pectoral, upper trapezius, and levator scapulae muscles, and weakness of the lower scapular stabilizers and deep neck flexors.46 While observing the shoulder, the examiner should look for the possibility of a step deformity (Figure 5-16, A). Such a deformity may be caused by an acromioclavicular dislocation with the distal end of the clavicle lying superior to the acromion process. Seen at rest, a step deformity indicates both the acromioclavicular and coracoclavicular ligaments have been torn. The deformity may be accentuated by asking the patient to horizontally adduct the arm or to medially rotate the shoulder and bring the hand up the back as high as possible. Occasionally, swelling is evident anterior to the acromioclavicular joint. This is called the Fountain sign and indicates that degeneration has caused communication between the acromioclavicular joint and swollen subacromial bursa underneath.47 If a sulcus deformity appears when traction is applied to the arm, it may be caused by multidirectional instability or loss of muscle control due to nerve injury or a stroke, leading to inferior subluxation of the glenohumeral joint (Figure 5-16, C). This deformity is lateral to the acromion and should not be confused with a step deformity. This is also referred to as a sulcus sign because of the appearance of a sulcus or groove below the acromion process (Figure 5-16, B). Flattening of the normally round deltoid muscle area may indicate an anterior dislocation of the glenohumeral joint or paralysis of the deltoid muscle (Figure 5-17). With an anterior dislocation, note also how the arm is held abducted because of the location of the humeral head below the glenoid. If the examiner palpated in the axilla, he or she would feel the head of the humerus. The examiner should note any abnormal bumps or malalignment in the bones that may indicate past injury, such as a healed fracture of the clavicle.
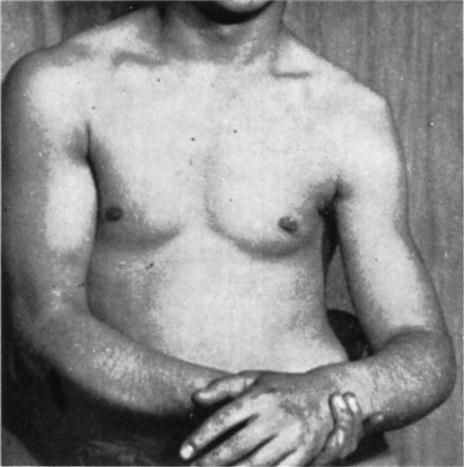
Note the prominent acromion, the arm held away from the side, and the flat deltoid. (From McLaughlin HL: Trauma, Philadelphia, 1959, WB Saunders, p. 246.)
In most people, the dominant side is lower than the nondominant side. This difference may be caused by the extra use of the dominant side, which stretches the ligaments, joint capsules, and muscles, allowing the arm to sag slightly. Tennis players48 and others who stretch their upper limbs in a reaching action show even greater differences, along with gross hypertrophy of the muscles on the dominant side (Figure 5-18). If the patient is protective of the shoulder, however, it may appear that the injured shoulder, whether dominant or nondominant, is higher than the normal side (see Figure 5-10).
The examiner notes whether the patient is able to assume the normal functional position for the shoulder, which is in the scapular plane with 60° of abduction and the arm in neutral or no rotation. In this position, or with the arm abducted to 90°, rupture or congenital absence of the pectoralis major may be evident (Figures 5-19 and 5-20).49–51 Rupture of the pectoralis major is often accompanied by a tearing sensation and pop along with weakness, painful limitation of movement, and ecchymosis.49 If the patient’s arm is medially rotated from this position to bring the hand into midline, the biceps tendon is forced against the lesser tuberosity of the medial wall of the bicipital (intertubercular) groove. If this position is maintained for long periods, there may be increased wear of the biceps tendon, which can lead to bicipital tendinitis or paratenonitis. If the arm is horizontally adducted while it is medially rotated, anterior pain indicates impingement symptoms (Hawkins-Kennedy test—see the “Special Tests” section). The width and depth of the bicipital groove may vary (Figure 5-21), possibly leading to problems if the shoulder is overused. Especially wide or deep grooves lead to the greatest problems. The wide grooves tend to allow the tendon too much lateral movement, leading to inflammation of the paratenon (paratenonitis);35 the deep grooves tend to be too narrow, compressing the tendon, especially if it becomes inflammed.52

A, Ecchymosis and swelling with arrow illustrating the sternal head rupture of pectoralis major. B, Massive swelling and bruising after pectoralis major rupture. C, Loss of axillary fold on the left side due to a pectoralis major tear creates an asymmetry compared with the normal right side. (From Provencher MT, et al: Injuries to the pectoralis major muscle—diagnosis and management. Am J Sports Med 38:1693–1705, 2010.)
Posterior View
When viewing the patient from behind (Figure 5-15, B), the examiner again notes bony and soft-tissue contours and body alignment especially scapular malpositioning.53 The scapula plays a major role in the shoulder.54 First, it provides an origin for the rotator cuff muscles as well as the biceps and triceps muscles and, therefore, provides a stable dynamic base from which these muscles act. Second, it maintains the glenohumeral alignment within physiological limits that facilitates congruency and concavity compression capability at the glenohumeral joint through the full ROM. Third, the attachment of the acromion to the clavicle leads to scapular upward rotation and posterior tilt to allow maximum arm elevation. Finally, the scapula facilitates force transfer from the shoulder to the core (and vice versa) acting like a funnel for efficient energy transfer. This transfer of forces can involve the whole kinetic chain, and by using this “chain” correctly, the patient can decrease the stresses to the shoulder itself.
Atrophy of the upper trapezius may indicate spinal accessory nerve palsy, whereas atrophy of supraspinatus or infraspinatus may indicate supraspinous nerve palsy.55 The spines of the scapulae, which begin medially at the level of the third thoracic (T3) vertebra, should be at the same angle. The scapula itself should extend from the T2 or T3 spinous process to the T7 or T9 spinous process of the thoracic vertebrae. Sobush and associates developed a method for measuring the scapular position called the Lennie test.56 In this test, they measured from the spinous processes horizontally to three scapular positions: the medial aspect of the most superior point (superior angle), the root of the spine of the scapula, and the inferior angle (Figure 5-22).56 If the scapula is sitting lower than normal against the chest wall, the superior medial border of the scapula may “washboard” over the ribs, causing a snapping or clunking sound (snapping scapula) during abduction and adduction.57–61 Other causes of snapping may be spinal kyphosis, rounded shoulders, forward tipped scapula, and a chin poking posture.62 The inferior angles of the scapulae should be equidistant from the spine.
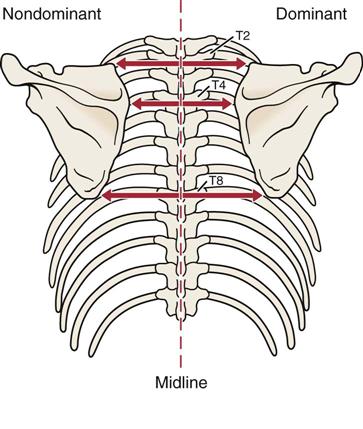
Measurements are taken at three positions on the scapula, and the dominant and nondominant sides are compared.
Scapular dyskinesia, or scapular dysfunction, although not an injury itself, can lead to altered glenohumeral joint angulation, abnormal stress on shoulder ligaments, altered subacromial space, overload of the acromioclavicular joint, increased strain on the scapular stabilizing muscles, altered muscle activation, and modified arm position and motion.54 These alterations are commonly the result of an excessively protracted scapula during arm motion. Kibler, et al.63 divided scapular dysfunction or dyskinesia into four movement patterns. Type I shows the inferior medial border being prominent at rest and the inferior angle tilts dorsally with movement (scapular tilt), while the acromion tilts anteriorly over the top of the thorax. It may be seen at rest or during concentric or eccentric movement. If the inferior border tilts away from the chest wall, it may indicate the presence of weak muscles (e.g., lower trapezius, latissimus dorsi, serratus anterior) or a tight pectoralis minor or major pulling, or tilting, the scapula forward from above.31 Type II is the classic winging of the scapula with the whole medial border of the scapula being prominent and lifting away from the posterior chest wall both statically and dynamically (Figure 5-23). It too may be seen at rest or during eccentric or concentric movements. This deformity may indicate the presence of a superior labrum anterior to posterior (SLAP) to the biceps lesion; weakness of the serratus anterior; rhomboids; lower, middle, and upper trapezius; a long thoracic nerve problem; or tight humeral rotators.31 Type III is illustrated by the superior border of the scapula being elevated at rest and during movement; a shoulder shrug initiates the movement, and there is minimal winging. This deformity is seen with active movement and may result from overactivity of the levator scapula and upper trapezius along with imbalance of the upper and lower trapezius force couple (Figure 5-24). It is associated with impingement and rotator cuff lesions.31 In the type IV pattern, both scapulae are symmetrical at rest and during motion; they rotate symmetrically upward with the inferior angles rotating laterally away from midline (rotary winging). It is seen during movement and may indicate that the scapular control muscles are not stabilizing the scapula.
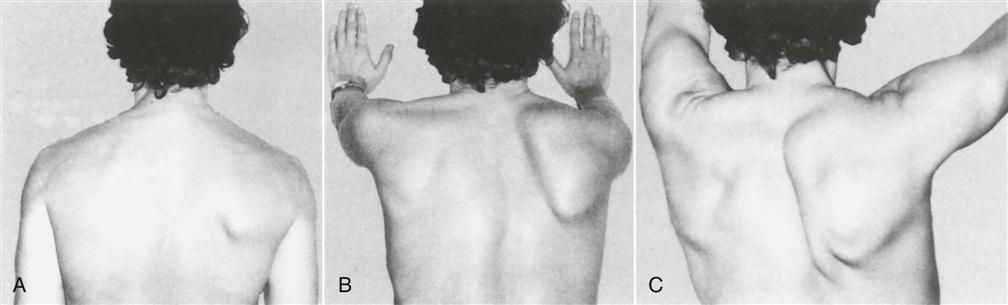
A, The shoulders are at rest. B, Winging is apparent when the patient is pushing forward. C, Winging when attempting full abduction. (From Foo CL, Swann M: Isolated paralysis of the serratus anterior: a report of 20 cases. J Bone Joint Surg Br 65:554, 1983.)
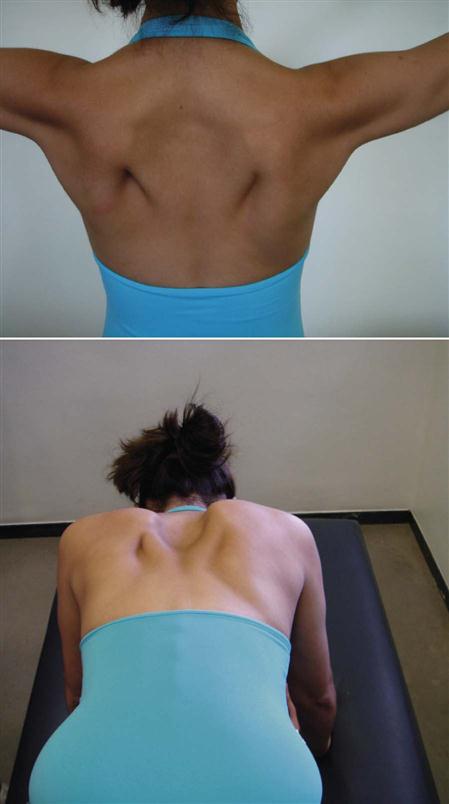
Note overdevelopment of upper trapezius and lower trapezius working to prevent rotary winging.
Kibler, et al.54 advocated a dynamic scapular motion test ![]() to test for scapular dyskinesia. The patient, while holding a 3 lb to 5 lb (1.4 kg to 2.3 kg) weight in the hand, is asked to fully elevate and lower the arms three to five times into forward flexion or scaption. The examiner watches for prominence of the medial border of the scapula (classic winging), which indicates a positive test.64
to test for scapular dyskinesia. The patient, while holding a 3 lb to 5 lb (1.4 kg to 2.3 kg) weight in the hand, is asked to fully elevate and lower the arms three to five times into forward flexion or scaption. The examiner watches for prominence of the medial border of the scapula (classic winging), which indicates a positive test.64
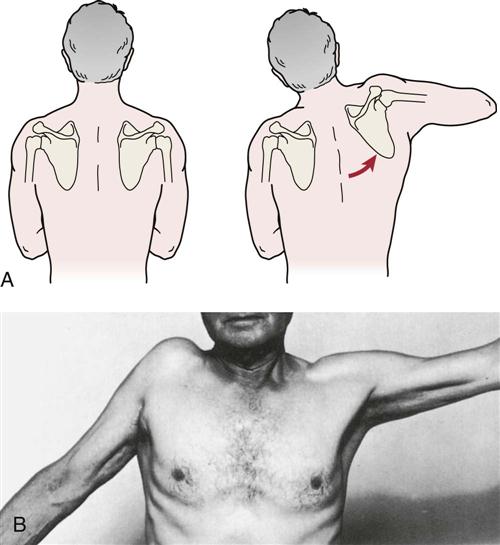
Primary scapular winging implies the winging is the result of muscle weakness of one of the scapular muscle stabilizers that, in turn, disrupts the normal muscle force couple balance of the scapulothoracic complex.65 Secondary scapular winging implies that the normal movement of the scapula is altered because of pathology in the glenohumeral joint.65 Dynamic scapular winging (i.e., winging with movement) may be caused by a lesion of the long thoracic nerve affecting serratus anterior, trapezius palsy (spinal accessory nerve), rhomboid weakness, multidirectional instability, voluntary action, or a painful shoulder resulting in splinting of the glenohumeral joint, which in turn causes reverse scapulohumeral rhythm.66 This splinting of the glenohumeral joint leads to reverse origin-insertion of the rotator cuff muscles so that instead of moving the humerus as they normally would, they work in reverse fashion and move the scapula. Commonly, with pathology, the scapular control muscles are weak and cannot counteract this action, resulting in protraction of the scapula and dynamic winging. The two other common causes of dynamic winging—long thoracic nerve palsy and spinal accessory nerve palsy—cause different scapula positioning and different winging patterns. Spinal accessory nerve palsy causes the scapula to depress and move laterally with the inferior angle rotated laterally. If the trapezius is weak or paralyzed, the winging of the scapula occurs before 90° abduction, and there is little winging on forward flexion.67 Long thoracic nerve palsy causes the scapula to elevate and move medially with the inferior angle rotating medially (Figure 5-25).68,69 If the serratus anterior is weak or paralyzed, the winging of the scapula occurs on abduction and forward flexion (especially with a “punch out” forward against resistance) (see Figure 5-23).67,70 Radiculopathies at C3, C4 (trapezius), C5 (rhomboids), and C7 (serratus anterior, rhomboids) can also cause winging.71,72
Static winging (i.e., winging occurring at rest) is usually caused by a structural deformity of the scapula, clavicle, spine, or ribs.73
Sprengel’s deformity, which is a developmental condition leading to a high or undescended scapula (Figure 5-26), is rare, but it is the most common congenital deformity of the shoulder complex.74–77 With this deformity, the scapular muscles are poorly developed or are replaced by a fibrous band. The condition may be unilateral or bilateral, and the range of the shoulder abduction decreases, leading to decreased shoulder function. Usually, the scapula is smaller than normal and is medially rotated. It may be associated with other anomalies (e.g., scoliosis, Klippel-Feil syndrome, rib anomalies).77
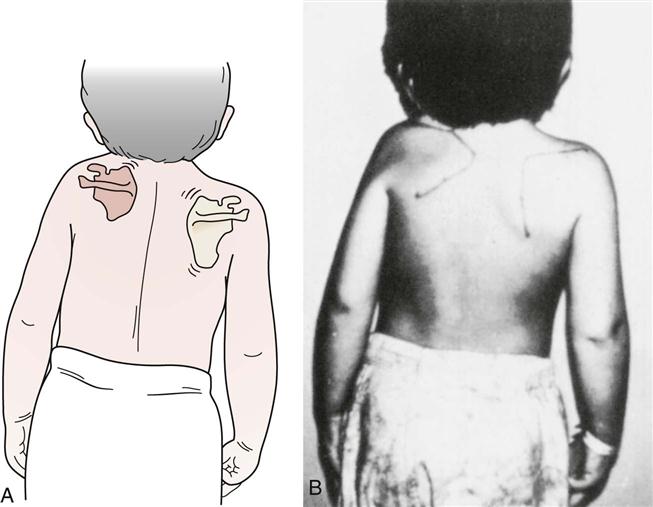
Diagram (A) and photograph (B) of child with Sprengel’s deformity. Note elevated shoulder and poorly developed scapula on the left. (A, Modified from Gartland JJ: Fundamentals of orthopaedics, Philadelphia, 1979, WB Saunders, p. 73. B, Courtesy of Dr. Roshen Irani.)
The shoulder muscles may be accentuated by having the patient place the hands on the hips and contract the muscles. The examiner should check closely for wasting in the supraspinatus and infraspinatus muscles (suprascapular nerve palsy), the serratus anterior muscle (long thoracic nerve palsy), and the trapezius muscle (spinal accessory nerve palsy), all of which can lead to winging of the scapula.
Examination
Because assessment of the shoulder may include an assessment of the cervical spine, the examination can be an extensive one. If the examiner has any doubt as to the location of the lesion, a cervical spine assessment (see Chapter 3) should be performed. In addition, the examiner must remember that the arm, of which the shoulder is an integral part, may act as an open kinetic chain when the hand is free to move, or as a closed kinetic chain when the hand is fixed to some relatively immovable object. For example, scapular instability may be evident in closed kinetic chain when the arm is fixed and the rotator cuff muscles work in reverse order (reverse origin-insertion; for example, the insertion of the muscles into the humerus becomes the stable part because the arm is fixed, whereas the scapula becomes the mobile part and is more likely to move) (Figure 5-27). It may also be evident in open kinetic chain, especially during high-speed movements when the scapula needs to be stabilized (e.g., when hitting a ball) or when the scapular muscles should be working eccentrically to slow or stop a movement (i.e., they are unable to do so because of weakness). In open kinetic chain, the scapula acts as the base or origin of the muscles, whereas the insertion into the humerus is more mobile. Knowledge of muscle balance and muscle force couples becomes imperative in determining a diagnosis. For example, the legs, pelvis, and trunk act as force generators, whereas the shoulder acts as a funnel and force regulator with the arm acting as the force delivery system.31 These kinetic chains and the intricate and complex interplay of the components of the kinetic chain have different effects on the shoulder. Eating, reaching, and dressing are considered open kinetic chain activities, whereas crutch walking and pushing up from a chair are considered closed kinetic chain movements.
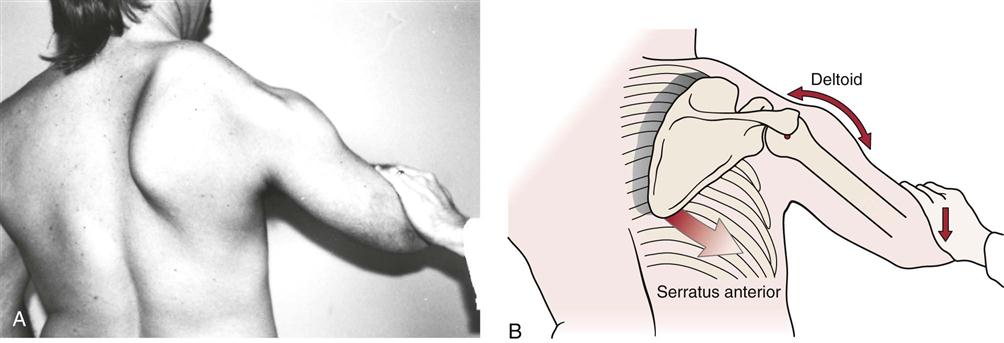
A, Winging of the right scapula caused by marked weakness of the right serratus anterior. The winging is exaggerated when resistance is applied against a shoulder abduction effort. Note how the stabilization occurs where the examiner’s hand is offering resistance. Instead of the arm moving, the scapula moves because its stabilizing muscles are weak. B, Kinesiologic analysis of the winging scapula. Without an adequate upward rotation force from the serratus anterior (fading arrow), the scapula becomes unstable and cannot resist the pull of the deltoid. Subsequently, the force of the deltoid (bidirectional arrow) causes the scapula to downwardly rotate and the glenohumeral joint to partially abduct (reverse origin-insertion). (From Neumann DA: Kinesiology of the musculoskeletal system: foundations for physical rehabilitation, St Louis, 2002, Mosby, p. 107.)
As with any assessment, the examiner is comparing one side of the body with the other. This comparison is necessary because of individual differences among normal people.
Active Movements
The first movements to be examined are the active movements. These movements are usually done in such a way that the painful movements are performed last so that pain does not carry over to the next movement. It is important to remember that shoulder movements are a combination of not only glenohumeral, scapulothoracic, acromioclavicular and sternoclavicular movements, but maximum end range movement may also involve the thoracic spine and ribs.78 Thus, being able to differentiate between scapular movement and glenohumeral movements as well as these other movements when watching active movements is essential, because scapular movement often compensates for restricted glenohumeral movement leading to weak and often lengthened scapular control muscles.
An understanding of the force couples acting on the shoulder complex and the necessity of balancing the muscle strength and endurance of these muscles is especially important when assessing the shoulder.79 Force couples are groups of counteracting muscles that show obvious action when a movement is loaded or done quickly.80 With a particular movement, one group of muscles (the agonists) acts concentrically, whereas the other group (the antagonists) acts eccentrically in a controlled, harmonized fashion to produce smooth movement. In addition, these muscles may work by co-contraction or co-activation to provide a stabilizing effect and joint control. Table 5-6 gives examples of some of the force couples acting about the shoulder.
TABLE 5-6
Force Couples About the Shoulder
| Movement | Agonist/Stabilizer | Antagonist/Stabilizer |
| Protraction (scapula) | Serratus anterior* Pectoralis major† and minor† |
Trapezius Rhomboids |
| Retraction (scapula) | Trapezius Rhomboids |
Serratus anterior* Pectoralis major† and minor† |
| Elevation (scapula) | Upper trapezius† Levator scapulae† |
Serratus anterior* Lower trapezius* |
| Depression (scapula) | Serratus anterior* Lower trapezius* |
Upper trapezius† Levator scapulae† |
| Lateral rotation (upward rotation of inferior angle of scapula) | Trapezius (upper† and lower* fibers) Serratus anterior* |
Levator scapulae† Rhomboids Pectoralis minor† |
| Medial rotation (downward rotation of inferior angle of scapula) | Levator scapulae† Rhomboids Pectoralis minor† |
Trapezius (upper† and lower* fibers) Serratus anterior* |
| Scapular stabilization | Upper trapezius† Lower trapezius* Rhomboids |
Serratus anterior* |
| Abduction (humerus) | Deltoid | Supraspinatus |
| Medial rotation (humerus) | Subscapularis† Pectoralis major† Latissimus doris Anterior deltoid |
Infraspinatus* Teres minor Posterior deltoid |
| Lateral rotation (humerus) | Infraspinatus Teres minor Posterior deltoid |
Subscapularis† Pectoralis major† Latissimus dorsi Anterior deltoid |
Active elevation through abduction is normally 170° to 180°. The extreme of the ROM occurs when the arm is abducted and lies against the ear on the same side of the head (Figure 5-28). As the patient elevates the upper extremity by abducting the shoulder, the examiner should note whether a painful arc ![]() is present (Figure 5-29).81 A painful arc may be caused by subacromial bursitis, calcium deposits, a peritenonitis or tendinosis35,36 of the rotator cuff muscles, or most commonly by an unstable scapula. The pain results from pinching of inflamed or tender structures under the acromion process and the coracoacromial ligament. Initially, the structures are not pinched under the acromion process, so the patient is able to abduct the arm 45° to 60° with little difficulty. As the patient abducts further (60° to 120°), the structures (e.g., subacromial bursa, rotator cuff tendon insertions, especially supraspinatus) become pinched, and the patient is often unable to abduct fully because of pain. If full abduction is possible, however, the pain diminishes after approximately 120° because the pinched soft tissues have passed under the acromion process and are no longer being pinched. Often, the pain is greater going up (against gravity) than coming down, and there is more pain on active abduction than on passive abduction. If the movement is very painful, the patient often elevates the arm through forward flexion or hikes the shoulder using upper trapezius and levator scapulae in an attempt to decrease the pain. In some cases, retracting the scapula and holding it retracted slightly enlarges the space under the coracoacromial space, which may decrease pain. A second painful arc in the shoulder may be seen during the same abduction movement. This painful arc (see Figure 5-29 ) occurs toward the end of abduction, in the last 10° to 20° of elevation, and is caused by pathology in the acromioclavicular joint or by a positive impingement test. In the case of the acromioclavicular joint lesion, the pain tends to be localized to the joint. With the impingement syndrome, the pain is usually found in the anterior shoulder region. Table 5-7 presents the signs and symptoms of three types of painful arc in the shoulder with the superior type being the most common. The arc of pain may be present also during elevation through forward flexion and scaption, although the pain is usually less severe on these movements. The interconnection of the subacromial, subcoracoid, and subscapularis bursae with each other and with the glenohumeral joint capsule often produces a broad area of signs and symptoms, which may result in a painful arc.
is present (Figure 5-29).81 A painful arc may be caused by subacromial bursitis, calcium deposits, a peritenonitis or tendinosis35,36 of the rotator cuff muscles, or most commonly by an unstable scapula. The pain results from pinching of inflamed or tender structures under the acromion process and the coracoacromial ligament. Initially, the structures are not pinched under the acromion process, so the patient is able to abduct the arm 45° to 60° with little difficulty. As the patient abducts further (60° to 120°), the structures (e.g., subacromial bursa, rotator cuff tendon insertions, especially supraspinatus) become pinched, and the patient is often unable to abduct fully because of pain. If full abduction is possible, however, the pain diminishes after approximately 120° because the pinched soft tissues have passed under the acromion process and are no longer being pinched. Often, the pain is greater going up (against gravity) than coming down, and there is more pain on active abduction than on passive abduction. If the movement is very painful, the patient often elevates the arm through forward flexion or hikes the shoulder using upper trapezius and levator scapulae in an attempt to decrease the pain. In some cases, retracting the scapula and holding it retracted slightly enlarges the space under the coracoacromial space, which may decrease pain. A second painful arc in the shoulder may be seen during the same abduction movement. This painful arc (see Figure 5-29 ) occurs toward the end of abduction, in the last 10° to 20° of elevation, and is caused by pathology in the acromioclavicular joint or by a positive impingement test. In the case of the acromioclavicular joint lesion, the pain tends to be localized to the joint. With the impingement syndrome, the pain is usually found in the anterior shoulder region. Table 5-7 presents the signs and symptoms of three types of painful arc in the shoulder with the superior type being the most common. The arc of pain may be present also during elevation through forward flexion and scaption, although the pain is usually less severe on these movements. The interconnection of the subacromial, subcoracoid, and subscapularis bursae with each other and with the glenohumeral joint capsule often produces a broad area of signs and symptoms, which may result in a painful arc.
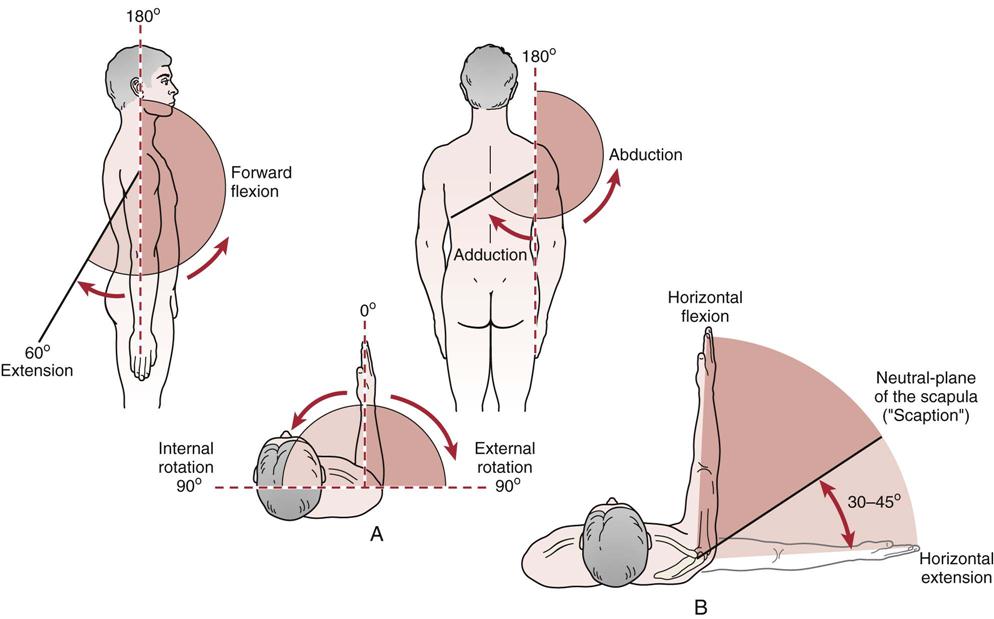
 Figure 5-28 Movement in the shoulder complex.
Figure 5-28 Movement in the shoulder complex.A, Range of motion (ROM) of the shoulder. B, Axes of arm elevation. (Adapted from Perry J: Anatomy and biomechanics of the shoulder in throwing, swimming, gymnastics, and tennis. Clin Sports Med 2:255, 1983.)
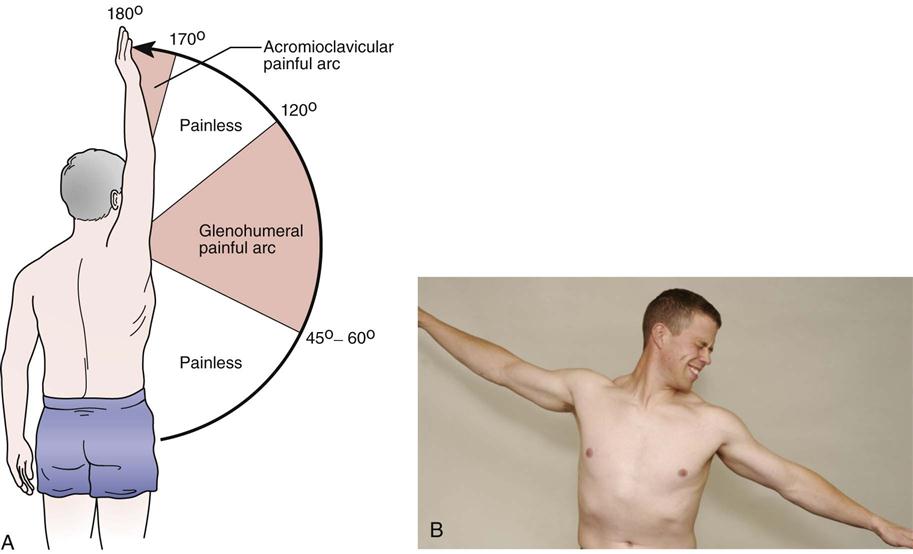
A, Painful arc of the glenohumeral joint. In the case of acromioclavicular joint problems only, the range of 170° to 180° would elicit pain. B, Note the impingement causing pain on the right at approximately 85°. (A, Modified from Hawkins RJ, Hobeika PE: Impingement syndrome in the athletic shoulder. Clin Sports Med 2:391, 1983.)
TABLE 5-7
Classification of Glenohumeral Painful Arcs
| Anterior | Posterior | Superior | |
| Night pain | Yes | Yes | Maybe |
| Age | 50+ | 50+ | 40+ |
| Sex ratio | F > M | F > M | M > F |
| Aggravated by | Lateral rotation and abduction | Medial rotation and abduction | Abduction |
| Tenderness | Lesser tuberosity | Posterior aspect of greater tuberosity | Greater tuberosity |
| Acromioclavicular joint involvement | No | No | Often |
| Calcification (if present) | Supraspinatus, infraspinatus, and/or subscapularis | Supraspinatus and/or infraspinatus | Supraspinatus and/or subscapularis |
| Third-degree strain biceps brachii (long head) | No | No | Occasional |
| Prognosis | Good | Very good | Poor (without surgery) |
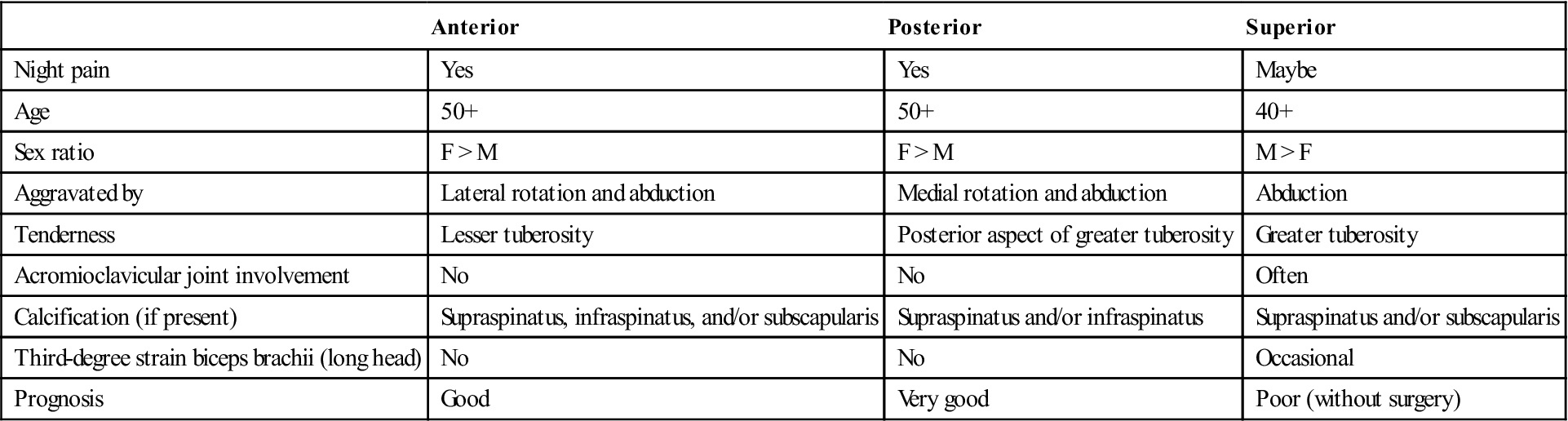
From Kessel L, Watson M: The painful arc syndrome. J Bone Joint Surg Br 59:166, 1977.
When examining the movement of elevation through abduction, the examiner must take time to observe scapulohumeral rhythm of the shoulder complex (Figure 5-30), both anteriorly and posteriorly.82–84 That is, during 180° of abduction, there is roughly a 2 : 1 ratio of movement of the humerus to the scapula with 120° of movement occurring at the glenohumeral joint and 60° at the scapulothoracic joint; one should be aware, however, that there is a great deal of variability among individuals and may depend on the speed of movement,85 and authors do not totally agree on the exact amounts of each movement.83,84,86 Although all authors concede that there is more movement in the glenohumeral joint than in the scapulothoracic joint, Davies and Dickoff-Hoffman believe the ratio is greater, at least to 120° of abduction,87 whereas Poppen and Walker88 and others7,89 believe the ratio is less (5 : 4 or 3 : 2) after 30° of abduction. During this total simultaneous movement at the four joints, there are three phases; the reader should understand that others will give values of the amount of each movement that vary from those noted here.
1. In the first phase of 30° of elevation through abduction, the scapula is said to be “setting.” This setting phase means that the scapula may rotate slightly in, rotate slightly out, or not move at all.70 Thus, there is no 2 : 1 ratio of movement during this phase. The angle between the scapular spine and the clavicle may also increase up to 5° by elevating at the sternoclavicular and acromioclavicular joints,82 but this depends on whether the scapula moves during this phase. The clavicle rotates minimally during this stage.
2. During the next 60° of elevation (second phase), the scapula rotates upward (inferior angle moves out) about 20°, and the humerus elevates 40° with minimal protraction or elevation of the scapula.82 Thus, there is a 2 : 1 ratio of scapulohumeral movement. During phase 2, the clavicle elevates because of the scapular rotation7,82 and begins to posteriorly rotate. During the second and third phase, the rotation of the scapula (total: 60°) is possible because there is 20° of motion at the acromioclavicular joint and 40° at the sternoclavicular joint.
3. During the final 90° of motion (third phase), the 2 : 1 ratio of scapulohumeral movement continues, and the angle between the scapular spine and the clavicle increases an additional 10°. Thus, the scapula continues to rotate and now begins to elevate. The amount of protraction continues to be minimal when the abduction movement is performed. It is in this stage that the clavicle rotates posteriorly 30° to 50° on a long axis and elevates up to a further 15°.7 In reality, the clavicle only rotates 5° to 8° relative to the acromion because of scapular rotation.90,91 Also, during this final stage, the humerus finishes its lateral rotation to 90° so that the greater tuberosity of the humerus avoids the acromion process. Tables 5-8 and 5-9 outline the shoulder kinematics in healthy and pathological states.92
TABLE 5-8
Summary of Scapular Kinematics During Arm Elevation in Healthy and Pathologic States
| Group | Healthy (Normal) | Impingement or Rotator Cuff Disease | Glenohumeral Joint Instability | Adhesive Capsulitis |
| Primary scapular motion | Upward rotation | Lesser upward rotation | Lesser upward rotation | Greater upward rotation |
| Secondary scapular motion | Posterior tilting | Lesser posterior tilting | No consistent evidence for alteration | No consistent evidence for alteration |
| Accessory scapular motion | Variable medial/lateral rotation | Greater medial rotation | Greater medial rotation | No consistent evidence for alteration |
| Presumed implications | Maximize shoulder ROM and available sub-acromial space | Presumed contributory to subacromial or internal impingement | Presumed contributory to lesser inferior and anterior joint stability | Presumed compensatory to minimize functional shoulder ROM loss |
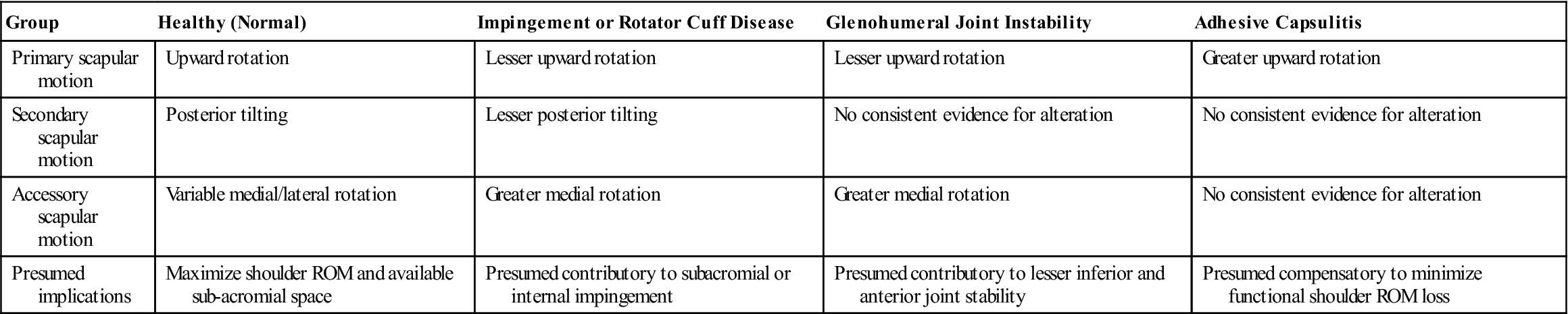
Modified from Ludewig PM, Reynolds JF: The association of scapular kinematics and glenohumeral joint pathologies. J Orthop Sports Phys Ther 39:95, 2009.
TABLE 5-9
Mechanisms of Scapular Dyskinesia
| Mechanism | Associated Effects |
| Inadequate serratus anterior activation | Lesser scapular upward rotation and posterior tilt |
| Excess upper trapezius activation | Greater clavicular elevation |
| Pectoralis minor tightness | Greater scapular medial rotation and anterior tilt |
| Posterior glenohumeral joint soft tissue tightness | Greater scapular anterior tilt |
| Thoracic kyphosis or flexed posture | Greater scapular medial rotation and anterior tilt, lesser scapular upward rotation |
Modified from Ludewig PM, Reynolds JF: The association of scapular kinematics and glenohumeral joint pathologies. J Orthop Sports Phys Ther 39:97, 2009.
In the unstable shoulder, scapulohumeral rhythm is commonly altered because of incorrect dynamic functioning of the scapular or humeral stabilizers or both.93 This may be related to incorrect arthrokinematics at the glenohumeral joint, and so the examiner must be sure to check for normal joint play and the presence of hypomobile structures that could lead to these abnormal motions.93
Kibler pointed out that it is important to watch the movement, especially of the scapula, in both the ascending and descending phases of abduction.94 Commonly, weakness of the scapular control muscles is more evident during descent, and an instability jog, hitch, or jump may occur when the patient loses control of the scapula.
The speed of abduction may also have an effect on the ratio.95 Therefore, it is more important to look for asymmetry between the injured and the good sides than to be concerned with the actual degrees of movement occurring at each joint. That being said, if the clavicle does not rotate and elevate, elevation through abduction at the glenohumeral joint is limited to 120°.82 If the glenohumeral joint does not move, elevation through abduction is limited to 60°, which occurs totally in the scapulothoracic joint. If there is no lateral rotation of the humerus during abduction, the total movement available is 120°, 60° of which occurs at the glenohumeral joint and 60° of which occurs at the scapulothoracic articulation.7 The normal end of ROM is reached when there is contact of a surgical neck of humerus with the acromion process. Reverse scapulohumeral rhythm (Figure 5-31) means that the scapula moves more than the humerus. This occurs in conditions like the frozen shoulder. The patient appears to “hike” the entire shoulder complex rather than produce a smooth coordinated abduction movement.
Examples include frozen shoulder (A) or tear of rotator cuff (B). (B, From Beetham WP, Polley HF, Slocum CH, et al: Physical examination of the joints. Philadelphia, 1965, WB Saunders, p. 41.)
Active elevation through forward flexion is normally 160° to 180°, and at the extreme of the ROM, the arm is in the same position as for active elevation through abduction. Active elevation (170° to 180°) through the plane of the scapula (30° to 45° of forward flexion), termed scaption, is the most natural and functional motion of elevation (see Figure 5-28). Elevation in this position is sometimes called neutral elevation. The exact angle is determined by the contour of the chest wall on which the scapula rests. Often, movement into elevation is less painful in this position than elevation through abduction in which the glenohumeral joint is actually in extension, or elevation in forward flexion. Movement in the plane of the scapula puts less stress on the capsule and surrounding musculature and is the position in which most of the functions of daily activity are commonly performed. Strength testing in this plane also gives higher values. Patients with weakness spontaneously choose this plane when elevating the arm.96,97 During scaption elevation, scapulohumeral rhythm is similar to that of abduction although there is greater individual variability. The three phases are similar, but there are differences. For example, in scaption elevation, there is little or no lateral rotation of the head of the humerus in the third phase.89 Also, the total elevation in scaption is about 170° with scapular rotation being about 65° and humeral abduction about 105°; although there is slightly more scapular rotation in scaption, this difference again may result from individual variation.89 More scapular protraction is likely to occur in scaption elevation, especially in elevation through forward flexion.
Active lateral rotation is normally 80° to 90° but may be greater in some athletes, such as gymnasts and baseball pitchers. Care must be taken when applying overpressure with this movement, because it could lead to anterior dislocation of the glenohumeral joint, especially in those with recurrent dislocation problems. If glenohumeral lateral rotation is limited, the patient will compensate by retracting the scapula. To minimize scapular movement, lateral rotation may be measured in supine or side lying with the arm abducted 90° (Figure 5-32). Wilk, et al.98 have recommended that rotation be tested in supine lying with the arm abducted to 90° and the scapula stabilized to increase reliability.
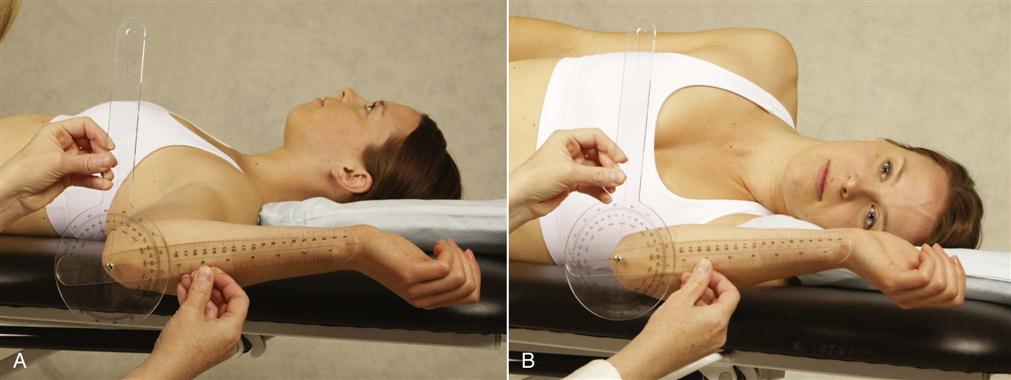
A, Supine. The patient’s arm is rotated until the scapula is felt to move and until an endpoint is reached. A handheld goniometer is used to measure medial and lateral rotation. B, Side lying. The examiner rotates the arm until the scapula is seen to move and resistance is felt. The amount of lateral and medial rotation can be examined in this manner with a handheld goniometer.
Active medial rotation is normally 60° to 100°. This is usually assessed by measuring the height of the “hitchhiking” thumb (thumb in extension) reaching up the patient’s back (Figure 5-33, A and B). Common reference points include the greater trochanter, buttock, waist, and spinous processes with T5 to T10 representing the normal degree of medial rotation.99 When doing the test in this fashion, the examiner must be aware that, in reality, the range measured is not that of the glenohumeral joint alone. In fact, much of the range is gained by winging the scapula. In the presence of tight medial glenohumeral motion, greater winging and protraction of the scapula occurs.
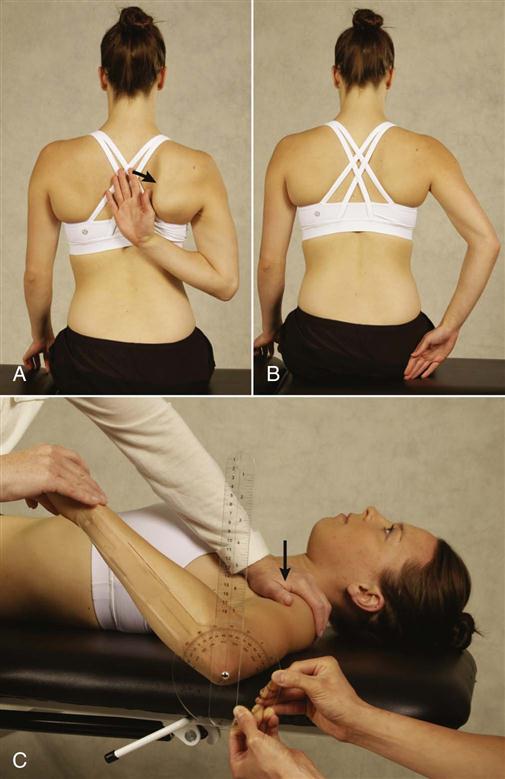
A, Reaching up the patient’s back. Note winging of scapula (arrow). B, Position of hand when scapula begins to wing indicates end of true medial rotation at the glenohumeral joint. C, Supine. Glenohumeral medial rotation passive range of motion measurement using stabilization of the scapula by holding the coracoid process and the scapula down.
Doing the rotation testing in 90° abduction (if the patient can achieve this position) will give a clearer indication of true glenohumeral joint medial and lateral rotation, which are measured when the scapula starts to move (Figure 5-33, C). If rotation is tested in 90° abduction and crepitus is present on rotation, it indicates abrasion of torn tendon margins against the coracoacromial arch and is called the “abrasion sign.”57
It is important to compare medial and lateral rotation, especially in active people who use their dominant arm at extremes of motion and under high load situations. Normally, any gain in lateral rotation is commonly accompanied by a comparable loss in medial rotation. Thus, it is important to note any glenohumeral internal (medial) rotation deficit (GIRD) (Figure 5-34),25 which is the difference in medial rotation between the patient’s two shoulders. Small changes in GIRD can lead to biomechanical changes in passive glenohumeral motion.100 For example, the loss of medial rotation may be due to contracture of the posteroinferior capsule, which in turn can lead to a SLAP lesion.37 Normally, the difference should be within 20° or 10% of total rotation of the opposite arm.25,101,102 This may also be compared with the glenohumeral external (lateral) rotation gain (GERG) (see Figure 5-34). If the GIRD/GERG ratio is greater than 1, the patient will probably develop shoulder problems.31,103
In the unstable shoulder, it has been advocated that the examiner do the dynamic rotary stability test (DRST), ![]() which assesses the rotator cuff’s ability to maintain the humeral head in the glenoid through the arc of rotation (i.e., the ability of the rotator cuff to maintain arthrokinematic control).104–106 The patient is positioned in sitting or lying with the arm abducted to about 90° and the elbow flexed to about 90°. The examiner controls the patient’s arm position with one hand while the other hand palpates the position of the humerus in the glenoid (it is best to palpate the joint line). (Figure 5-35). The examiner places the patient’s glenohumeral joint in different positions of flexion and abduction close to the position where the patient has symptoms. The patient is asked to do an isometric contraction against light to moderate resistance then isotonically (concentrically or eccentrically [eccentric break] depending on what movements caused the patient’s symptoms). While the patient does the contraction, the examiner palpates the joint line to see if and when arthrokinematic control is lost (i.e., does the humeral head slip or translate?).105 During the test, the scapula should be stable and not translate. If the scapula protracts during the test, it indicates lack of scapular control.
which assesses the rotator cuff’s ability to maintain the humeral head in the glenoid through the arc of rotation (i.e., the ability of the rotator cuff to maintain arthrokinematic control).104–106 The patient is positioned in sitting or lying with the arm abducted to about 90° and the elbow flexed to about 90°. The examiner controls the patient’s arm position with one hand while the other hand palpates the position of the humerus in the glenoid (it is best to palpate the joint line). (Figure 5-35). The examiner places the patient’s glenohumeral joint in different positions of flexion and abduction close to the position where the patient has symptoms. The patient is asked to do an isometric contraction against light to moderate resistance then isotonically (concentrically or eccentrically [eccentric break] depending on what movements caused the patient’s symptoms). While the patient does the contraction, the examiner palpates the joint line to see if and when arthrokinematic control is lost (i.e., does the humeral head slip or translate?).105 During the test, the scapula should be stable and not translate. If the scapula protracts during the test, it indicates lack of scapular control.
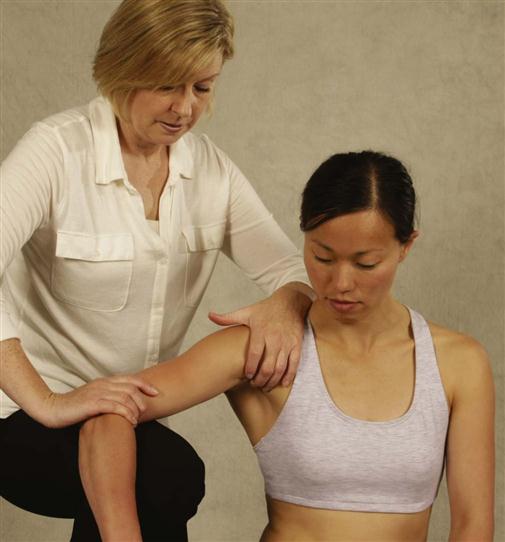
Magarey and Jones105 also advocated doing the Dynamic Relocation Test (DRT), ![]() which tests the ability of the rotator cuff to stabilize the humeral head through co-contraction of the rotator cuff muscles. The patient is seated with the arm supported in 60° to 80° abduction in the scapular plane (scaption) (Figure 5-36). With the middle finger of one hand palpating the subscapularis and the thumb along the outer edge of the acromion, the examiner uses the other hand to apply traction (longitudinal distraction) to the arm while asking the patient to pull the arm up into the socket. As the patient pulls the arm in and up, the examiner should feel for contraction of the rotator cuff, especially the subscapularis. If the pectoral muscles are overactive, the examiner may palpate the rotator cuff posteriorly.104 During the test, the scapula should not move. If the scapula protracts, it indicates an unstable scapula.
which tests the ability of the rotator cuff to stabilize the humeral head through co-contraction of the rotator cuff muscles. The patient is seated with the arm supported in 60° to 80° abduction in the scapular plane (scaption) (Figure 5-36). With the middle finger of one hand palpating the subscapularis and the thumb along the outer edge of the acromion, the examiner uses the other hand to apply traction (longitudinal distraction) to the arm while asking the patient to pull the arm up into the socket. As the patient pulls the arm in and up, the examiner should feel for contraction of the rotator cuff, especially the subscapularis. If the pectoral muscles are overactive, the examiner may palpate the rotator cuff posteriorly.104 During the test, the scapula should not move. If the scapula protracts, it indicates an unstable scapula.
Active extension is normally 50° to 60°. The examiner must ensure that the movement is in the shoulder and not in the spine because some patients may flex the spine or bend forward, giving the appearance of increased shoulder extension. Similarly, retraction of the scapula increases the appearance of glenohumeral extension. Weakness of full extension commonly implies weakness of the posterior deltoid in one arm and is sometimes called the swallow tail sign, because both arms do not extend the same amount either due to injury to the muscle itself or to the axillary nerve.107
Adduction is normally 50° to 75° if the arm is brought in front of the body. Horizontal adduction, or cross-flexion, is normally 130°. To accomplish this movement, the patient first abducts the arm to 90° and then moves the arm across the front of the body. Horizontal abduction, or cross-extension, is approximately 45°. After abducting the arm to 90°, the patient moves the straight arm in a backward direction. In both cases, the examiner should watch the relative amount of scapular movement between the normal and pathological sides. If movement is limited in the glenohumeral joint, greater scapular movement occurs. Circumduction is normally approximately 200° and involves taking the arm in a circle in the vertical plane.
In addition to the aforementioned movements, several of which involve movement of the humerus and scapula, the patient should actively perform two distinct movements of the scapulae: scapular retraction and scapular protraction (Figure 5-37). For scapular retraction, the examiner asks the patient to squeeze the shoulder blades (scapula) together. Normally, the medial borders of the scapula remain parallel to the spine but move toward the spine with the soft tissue bunching up between the scapula (see Figure 5-37, B). Ideally, the patient should be able to do this movement without excessive contraction of the upper trapezius muscles. For scapular protraction, the patient tries to bring the shoulders together anteriorly so that the scapula move away from midline with the inferior angle of the scapula commonly moving laterally more than the superior angle so that some lateral rotation of the inferior angle occurs (see Figure 5-37, C). This protraction/retraction cycle may cause a clicking or snapping near the inferior angle or supramedial corner, which is sometimes called a snapping scapula, caused by the scapula rubbing over the underlying ribs.60
Injury to the individual muscles can affect several movements. For example, if the serratus anterior muscle is weak or paralyzed, the scapula “wings” away from the thorax on its medial border. It also assists upper rotation of the scapula during abduction. Injury to the muscle or its nerve may therefore limit abduction. In fact, loss or weakness of serratus anterior affects all shoulder movements because scapular stabilization is lost.80 Similarly, weakness of the lower trapezius muscle can alter scapular mechanics resulting in anterior secondary impingement. Many of the tests for these muscles are described in the “Special Tests” section.
When observing these movements, the examiner may ask the patient to perform them in combination, especially if the patient history has indicated that combined movements are bothersome. For example, Apley’s scratch test combines medial rotation with adduction and lateral rotation with abduction (Figure 5-38). This method may decrease the time required to do the assessment. In addition, by having the patient do the combined movements, the examiner gains some idea of the functional capacity of the patient. For example, abduction combined with flexion and lateral rotation or adduction combined with extension and medial rotation is needed to comb the hair, to zip a back zipper, or to reach for a wallet in a back pocket. However, the examiner must take care to notice which movements are restricted and which ones are not, because several movements are performed at the same time. Some examiners prefer doing the same motion in both arms at the same time: neck reach (abduction, flexion, and lateral rotation at the glenohumeral joint) and back reach (adduction, extension, and medial rotation at the glenohumeral joint). Some believe this method makes comparison easier (Figure 5-39).47 Often, the dominant shoulder shows greater restriction than the nondominant shoulder, even in normal people. An exception would be patients who continually use their arms at the extremes of motion (e.g., baseball pitchers). Because of the extra ROM developed over time doing the activity, the dominant arm may show greater ROM. However, the examiner must always be aware that shoulder movements include movements of the scapula and clavicle as well as the glenohumeral joint and that many of the perceived glenohumeral joint problems are, in reality, scapular muscle control problems, which may secondarily lead to glenohumeral joint problems, especially in people under 40 years of age. If, in the history, the patient has complained that shoulder movements in certain postures are painful or that sustained or repetitive movements increase symptoms, the examiner should consider having the patient hold a sustained arm position (10 to 60 seconds) or do the movements repetitively (ten to twenty repetitions). Ideally, these repeated movements should be performed at the speed and with the load that the patient was using when the symptoms were elicited. Thus, the volleyball player should do the spiking motion in which he or she jumps up to hit the imaginary ball.
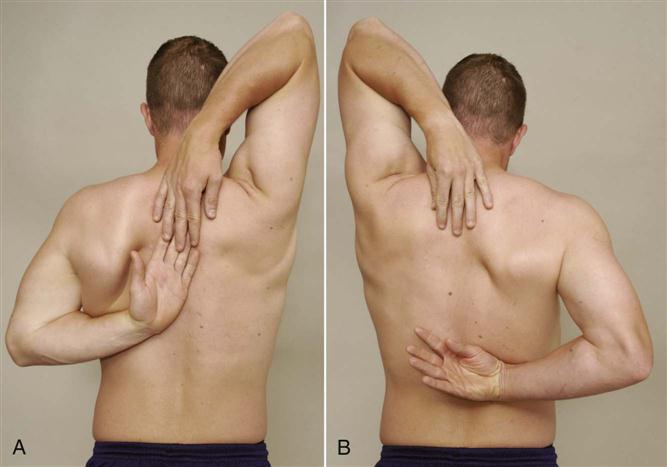
 Figure 5-38 Apley’s scratch test.
Figure 5-38 Apley’s scratch test.A, The right arm is in lateral rotation, flexion, and abduction; and the left arm is in medial rotation, extension, and adduction. B, The left arm is in lateral rotation, flexion, and abduction; and the right arm is in medial rotation, extension, and adduction. Note the difference in medial rotation and scapular winging in the right arm compared to the left arm in A.
Capsular tightness, although commonly tested during passive movement, can affect active movement by limiting some or all movements in the glenohumeral joint with compensating excessive movement of the scapula. Just as a frozen shoulder can affect all movements, selected tightness due to particular pathologies may affect only part of the capsule. For example, with anterior shoulder instability, posterior capsular tightness is a common finding combined with weak lower trapezius and serratus anterior muscles. Table 5-10 shows common selected capsular tightness and states their effect on movement.
TABLE 5-10
Capsular Tightness: Its Effect and Resulting Humeral Head Translation
| Where | Effect (Signs and Symptoms) | Resulting Translation |
| Posterior | Cross flexion decreased Medial rotation decreased Flexion (end range) decreased Decreased posterior glide Impingement signs in medial rotation Weak external rotators Weak scapular stabilizers |
Anterior (with medial rotation) |
| Posteroinferior | Elevation anteriorly Medial rotation of elevated arm decreased Horizontal adduction decreased |
Superior Anterosuperior Anterosuperior |
| Posterosuperior | Medial rotation limited | Anterosuperior |
| Anterosuperior | Flexion (end range) decreased Extension (end range) decreased Lateral rotation decreased Horizontal extension decreased Abduction (end range) decreased Decreased posteroinferior glide Impingement in medial rotation and cross flexion Increased night pain Weak rotator cuff May have positive ULNT Biceps tests may be positive |
Posterior (with lateral rotation) |
| Anteroinferior | Abduction decreased Extension decreased Lateral rotation decreased Horizontal extension decreased Increased posterior glide |
Posterior (with lateral rotation of elevated arm) |
ULNT, Upper limb neurodynamic test.
Data from Matsen FA, et al: Practice evaluation and management of the shoulder, Philadelphia, 1994, WB Saunders.
Likewise, muscle tightness can affect both active and passive movement. For example, with anterior shoulder instability, the following muscles may be found to be tight: subscapularis, pectoralis minor and major, latissimus dorsi, upper trapezius, levator scapulae, sternocleidomastoid, scalenes, and rectus capitus. Weak muscles include serratus anterior, middle and lower trapezius, infraspinatus, teres minor, posterior deltoid, rhomboids, longus colli, and longus capitus.60
The biceps tendon does not move in the bicipital groove during movement; rather, the humerus moves over the fixed tendon. From adduction to full elevation of abduction, a given point in the groove moves along the tendon at least 4 cm. If the examiner wants to keep excursion of the bicipital groove along the biceps tendon to a minimum, the arm should be elevated with the humerus in medial rotation; elevating the arm with the humerus laterally rotated causes maximum excursion of the bicipital groove along the biceps tendon. Patients who have deltoid or supraspinatus pathology sometimes use this laterally rotated position because lateral rotation allows the biceps tendon to be used as a shoulder abductor in a “cheating” movement.
As the patient does the various movements, the examiner watches to see whether the components of the shoulder complex move in normal, coordinated sequence and whether the patient exhibits any apprehension when doing a movement. With anterior instability of the shoulder, the shoulder girdle often droops, and excessive scapulothoracic movement may occur on abduction. With posterior instability, horizontal adduction (cross-flexion) may cause excessive scapulothoracic movement. Any apprehension on movement suggests the possibility of instability. The examiner should also watch for winging of the scapula on active movements. Winging of the medial border of the scapula indicates injury to the serratus anterior muscle or the long thoracic nerve; rotary winging of the scapula or scapular tilt indicates upper trapezius pathology or injury to the spinal accessory nerve (cranial nerve XI; Table 5-11).55,99,108 Scapular tilt (inferior angle of scapula moves away from rib cage) may also be caused by weak lower trapezius or a tight pectoralis minor. In some cases, it may be necessary to load the appropriate muscle isometrically (hold the contraction for 10 to 15 seconds) to demonstrate abnormal scapular stability. It has been reported that application of a resistance to adduction at 30° and at 60° of shoulder abduction is the best way to show scapular winging.99 Eccentric loading of the shoulder in different positions, especially into horizontal adduction, may also demonstrate winging or loss of scapular control. Weakness of the scapular control muscles often leads to overactivity of the rotator cuff and biceps muscle leading to overuse pathology in those structures.
TABLE 5-11
Winging of the Scapula: Dynamic Causes and Effects
| Cause | Effect (Signs and Symptoms) |
| Trapezius or spinal accessory nerve lesion | Inability to shrug shoulder |
| Serratus anterior or long thoracic nerve lesion | Difficulty elevating arm above 120° |
| Strain of rhomboids | Difficulty pushing elbow back against resistance (with hand on hip) |
| Muscle imbalance or contractures | Winging of upper margin of scapula on adduction and lateral rotation |
If the scapula appears to wing, the examiner asks the patient to forward flex the shoulder to 90°. The examiner then pushes the straight arm toward the patient’s body while the patient resists. If there is weakness of the upper or lower trapezius muscle, the serratus anterior muscle, or the nerves supplying these muscles, their inability to contract will cause the scapula to wing. Another way to test winging of the scapula is to have the patient stand and lean against the wall. The examiner then asks the patient to do a pushup away from the wall while the examiner watches for winging (see Figure 5-23; Figure 5-40, A). Similarly, asking the patient to do a floor pushup may demonstrate this winging (Figure 5-40, B). The patient should be tested in a relaxed starting position and be asked to do the pushup. Sometimes the winging is visible at rest only (static winging), sometimes during rest and activity, and sometimes only with the activity (dynamic winging).
Injury to other nerves in the shoulder region must not be overlooked (Table 5-12). As previously mentioned, damage to the suprascapular nerve may affect both the supraspinatus and infraspinatus muscles, or it may affect only the infraspinatus, depending on where the pathology lies (see Figure 5-161), whereas injury to the musculocutaneous nerve can lead to paralysis of the coracobrachialis, biceps, and brachialis muscles. These changes affect elbow flexion and supination and forward flexion of the shoulder. There is also a loss of the biceps reflex. Injury to the axillary (circumflex) nerve leads to paralysis of the deltoid and teres minor muscles, affecting abduction and lateral rotation of the shoulder. A sensory loss over the deltoid insertion area also occurs. Damage to the radial nerve affects all of the extensor muscles of the upper limb, including the triceps. Triceps paralysis may be overlooked when examining the shoulder unless arm extension is attempted along with elbow extension against gravity. Both of these movements are affected in high radial nerve palsy, although some triceps function may remain (e.g., in radial nerve palsy after a humeral shaft fracture).
TABLE 5-12
Signs and Symptoms of Possible Peripheral Nerve Involvement
| Spinal accessory nerve | Inability to abduct arm beyond 90° |
| Pain in shoulder on abduction | |
| Long thoracic nerve | Pain on flexing fully extended arm |
| Inability to flex fully extended arm | |
| Winging starts at 90° forward flexion | |
| Suprascapular nerve | Increased pain on forward shoulder flexion |
| Shoulder weakness (partial loss of humeral control) | |
| Pain increases with scapular abduction | |
| Pain increases with cervical rotation to opposite side | |
| Axillary (circumflex) nerve | Inability to abduct arm with neutral rotation |
| Musculocutaneous nerve | Weak elbow flexion with forearm supinated |
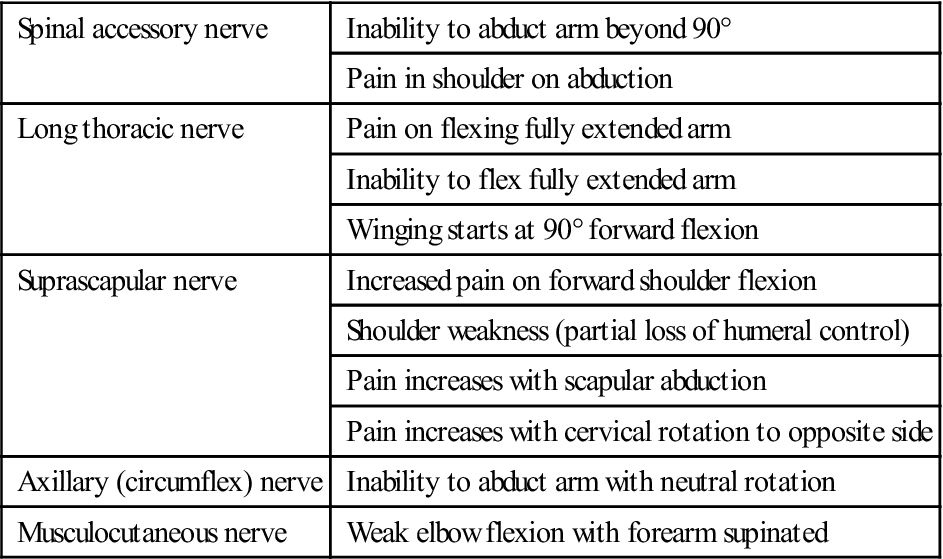
Passive Movements
If the ROM is not full during the active movements and the examiner is unable to test the end feel, the examiner should perform all passive movements of the shoulder to determine the end feel, and any restriction should be noted. This passive examination should include not only the mobility of the four shoulder joints but also the ribs and spine as limitations in rib and spinal movement can restrict shoulder movement.
The end feel of capsular tightness is different from the tissue stretch end feel of muscle tightness.109 Capsular tightness has a more hard elastic feel to it, and it usually occurs earlier in the ROM. If one is unsure of the end feel, the examiner can ask the patient to contract the muscles acting in the opposite direction 10% to 20% of maximum voluntary contraction (MVC) and then relax. The examiner then attempts to move the limb further into range. If the range increases, the problem was muscular not capsular.
If the problem is capsular, capsular tightness should be measured. For example, a tight posterior capsule can cause increased scapular protraction and depression leading to ante-tilting and insufficient scapular elevation, which in turn can lead to impingement.37 In addition, it can limit horizontal adduction, and posteroinferior tightness can increase the risk of injury to the rotator cuff.110 To measure posterior capsular tightness, the patient, suitably undressed (no shirt for males; bra for females), is placed in supine lying with the arm forward flexed to 90° and the elbow flexed to 90°. The examiner stands beside the patient and, while palpating the lateral edge of the scapula, horizontally adducts the patient’s arm. As soon as the examiner feels the scapula begin to move, the horizontal adduction is stopped, and the angle relative to the vertical position is measured. Both sides, starting with the normal side, are measured (Figure 5-41, A).111 The test may also be done in side lying but it is harder to stabilize the scapula (Figure 5-41, B).112,113 The angle from the vertical to the arm indicates the passive ROM available. If the pathological side has less ROM and the end feel is capsular, capsular tightness is present. This capsular tightness should correlate well with decreased medial rotation provided the scapula is not allowed to move in compensation.112,113

A, Supine lying. Angle created by the end position of the humerus with respect to the starting position to determine glenohumeral horizontal adduction range of motion. Note stabilization of scapula (arrow). B, Starting position for the posterior shoulder flexibility measurement with the patient positioned in side lying. Note the scapular stabilization (arrow) with the torso perpendicular to the examining table. As soon as the scapula begins to move, the examiner stops.
Particular attention must be paid to passive medial and lateral rotation if the examiner suspects a problem with the glenohumeral joint capsule (see previous discussion of GIRD). Lunden, et al.114 have recommended that rotation, especially medial rotation, should be measured in side lying for greater reliability (Figure 5-42). Excessive scapular movement may be seen as compensation for a tight glenohumeral joint. Subcoracoid bursitis may limit full lateral rotation, and subacromial bursitis may limit full abduction because of compression or pinching of these structures. If lateral rotation of the shoulder is limited, the examiner should check forearm supination with the arm forward flexed to 90°. Patients who have a posterior dislocation at the glenohumeral joint exhibit restricted lateral rotation of the shoulder and limited supination in forward flexion (Rowe sign ![]() ).115 Even if overpressure has been applied on active movement, it is still necessary for the examiner to perform elevation through abduction of the glenohumeral joint only (Figure 5-43) and the quadrant test.
).115 Even if overpressure has been applied on active movement, it is still necessary for the examiner to perform elevation through abduction of the glenohumeral joint only (Figure 5-43) and the quadrant test.
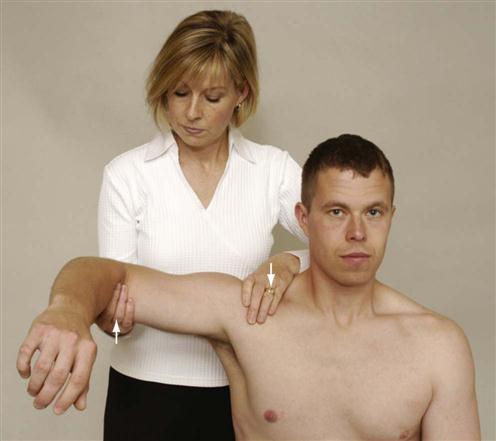
The examiner performs passive elevation through abduction or scaption of the glenohumeral joint with the clavicle and scapula fixed to determine the amount of abduction in the glenohumeral joint alone. This can give an indication of capsular tightness or subacromial space pathology.47 Normally, this movement should be up to 120°, although Gagey and Gagey116 have stated that anything greater than 105° indicates laxity in the inferior glenohumeral ligament (Gagey hyperabduction test ![]() ).117
).117
The rotation of the humerus in the quadrant position demonstrates Codman’s “pivotal paradox”97,118 and MacConaill’s119 conjunct rotation (rotation that automatically or subconsciously occurs with movement) in diadochal movement (a succession of two or more distinct movements). For example, if the arm, with the elbow flexed, is laterally rotated when the arm is at the side and then abducted in the coronal plane to 180°, the shoulder will be in 90° of medial rotation even though no apparent rotation has occurred. The path traced by the humerus during the quadrant test, in which the humerus moves forward at approximately 120° of abduction, is the unconscious rotation occurring at the glenohumeral joint. Thus, the quadrant test is designed to demonstrate whether the automatic or subconscious rotation is occurring during movement. The examiner should not only feel the movement but also determine the quality of the movement and the amount of anterior humeral movement. This test and the following locked quadrant test assess one area or quadrant of the 200° of circumduction. The humerus must rotate in the quadrant of the circumduction movement to allow full pain-free movement. Although both of these tests should normally be pain-free, the examiner should be aware that they place a high level of stress on the soft tissues of the glenohumeral joint, and discomfort should not be misinterpreted as pathological pain. If movement is painful and restricted, the tests indicate early stages of shoulder pathology.120
To test the quadrant position,121,122 the examiner stabilizes the scapula and clavicle by placing the forearm under the patient’s scapula on the side to be tested and extending the hand over the shoulder to hold the trapezius muscle and prevent shoulder shrugging (Figure 5-44). To test the position, the upper limb is elevated to rest alongside the patient’s head with the shoulder laterally rotated. The patient’s shoulder is then adducted. Because adduction occurs on the coronal plane, a point (the quadrant position) is reached at which the arm moves forward slightly from the coronal plane. At approximately 60° of adduction (from the arm beside the head), this position of maximum forward movement occurs (i.e., at about 120° of abduction) even if a backward pressure is applied. As the shoulder is further adducted, the arm falls back to the previous coronal plane. The quadrant position indicates the position at which the arm has medially rotated during its descent to the patient’s side.
The quadrant position also may be found by abducting the medially rotated shoulder while maintaining extension. In this case, the quadrant position is reached (at approximately 120° of abduction) when the shoulder no longer abducts, because it is prevented from laterally rotating by the catching of the greater tuberosity in the subacromial space. This position is referred to as the locked quadrant position.122 If the arm is allowed to move forward, lateral rotation occurs and full abduction can be achieved. Both the quadrant and locked quadrant simply indicate where the rotation normally occurs during shoulder abduction/adduction.
The capsular pattern of the shoulder is lateral rotation showing the greatest restriction, followed by abduction and medial rotation. Each of these movements normally has a tissue-stretch end feel. Other movements may be limited, but not in the same order and not with as much restriction. Early capsular patterns may exhibit only limitations of lateral rotation or possibly lateral rotation and abduction. Finding of limitation, but not in the order described, indicates a noncapsular pattern.
Resisted Isometric Movements
Having completed the active and passive movements, which are done while the patient is standing, sitting, or lying supine (in the case of quadrant test), the patient lies supine to do the resisted isometric movements (Figure 5-45). The disadvantage of this position is that the examiner cannot observe the stabilization of the scapula during the testing. Normally, the scapula should not move during isometric testing. Scapular protraction, winging, or tilting during isometric testing indicates weakness of the scapular control muscles. Although all the muscles around the shoulder can be tested in supine lying, it has been advocated that the muscles should be tested in more than one position (for example, different amounts of abduction or forward flexion) to determine the mechanical effect of the contraction in different situations. If, in the history, the patient complained of pain in one or more positions, these positions should be tested as well. If the initial position causes pain, other positions (e.g., position of injury, position of mechanical advantage) may be tried to further differentiate the specific contractile tissue that has been injured. During the active movements, the examiner should have noted which movements caused discomfort or pain so that this information can be correlated with that obtained from resisted isometric movements. By carefully noting which movements cause pain on isometric testing, the examiner should be able to determine which muscle or muscles are at fault (Table 5-13). For example, if the patient experiences pain primarily on medial rotation but also on abduction and adduction, the examiner would suspect a problem in the subscapularis muscle, because the other muscles involved in these actions were found to be pain-free in other movements. To do the initial resisted isometric tests, the examiner positions the patient’s arm at the side with the elbow flexed to 90°. The muscles of the shoulder are then tested isometrically with the examiner positioning the patient and saying, “Don’t let me move you.”
TABLE 5-13
Muscles About the Shoulder: Their Actions, Nerve Supply, and Nerve Root Derivation
| Action | Muscles Acting | Nerve Supply | Nerve Root Derivation Retraction |
| Forward flexion | 1. Deltoid (anterior fibers) | Axillary (circumflex) | C5, C6 (posterior cord) |
| 2. Pectoralis major (clavicular fibers) | Lateral pectoral | C5, C6 (lateral cord) | |
| 3. Coracobrachialis | Musculocutaneous | C5–C7 (lateral cord) | |
| 4. Biceps (when strong contraction required) | Musculocutaneous | C5–C7 (lateral cord) | |
| Extension | 1. Deltoid (posterior fibers) | Axillary (circumflex) | C5, C6 (posterior cord) |
| 2. Teres major | Subscapular | C5, C6 (posterior cord) | |
| 3. Teres minor | Axillary (circumflex) | C5, C6 (posterior cord) | |
| 4. Latissimus dorsi | Thoracodorsal | C6–C8 (posterior cord) | |
| 5. Pectoralis major (sternocostal fibers) | Lateral pectoral | C5, C6 (lateral cord) | |
| Medial pectoral | C8, T1 (medial cord) | ||
| 6. Triceps (long head) | Radial | C5–C8, T1 (posterior cord) | |
| Horizontal adduction | 1. Pectoralis major | Lateral pectoral | C5, C6 (lateral cord) |
| 2. Deltoid (anterior fibers) | Axillary (circumflex) | C5, C6 (posterior cord) | |
| Horizontal abduction | 1. Deltoid (posterior fibers) | Axillary (circumflex) | C5, C6 (posterior cord) |
| 2. Teres major | Subscapular | C5, C6 (posterior cord) | |
| 3. Teres minor | Axillary (circumflex) | C5, C6 (brachial plexus trunk) | |
| 4. Infraspinatus | Suprascapular | C5, C6 (brachial plexus trunk) | |
| Abduction | 1. Deltoid | Axillary (circumflex) | C5, C6 (posterior cord) |
| 2. Supraspinatus | Suprascapular | C5, C6 (brachial plexus trunk) | |
| 3. Infraspinatus | Suprascapular | C5, C6 (brachial plexus trunk) | |
| 4. Subscapularis | Subscapular | C5, C6 (posterior cord) | |
| 5. Teres minor | Axillary (circumflex) | C5, C6 (posterior cord) | |
| 6. Long head of biceps (if arm laterally rotated first, trick movement) | Musculocutaneous | C5–C7 (lateral cord) | |
| Adduction | 1. Pectoralis major | Lateral pectoral | C5, C6 (lateral cord) |
| 2. Latissimus dorsi | Thoracodorsal | C6–C8 (posterior cord) | |
| 3. Teres major | Subscapular | C5, C6 (posterior cord) | |
| 4. Subscapularis | Subscapular | C5, C6 (posterior cord) | |
| Medial rotation | 1. Pectoralis major | Lateral pectoral | C5, C6 (lateral cord) |
| 2. Deltoid (anterior fibers) | Axillary (circumflex) | C5, C6 (posterior cord) | |
| 3. Latissimus dorsi | Thoracodorsal | C6–C8 (posterior cord) | |
| 4. Teres major | Subscapular | C5, C6 (posterior cord) | |
| 5. Subscapularis (when arm is by side) | Subscapular | C5, C6 (posterior cord) | |
| Lateral rotation | 1. Infraspinatus | Suprascapular | C5, C6 (brachial plexus trunk) |
| 2. Deltoid (posterior fibers) | Axillary (circumflex) | C5, C6 (posterior cord) | |
| 3. Teres minor | Axillary (circumflex) | C5, C6 (posterior cord) | |
| Elevation of scapula | 1. Trapezius (upper fibers) | Accessory | Cranial nerve XI |
| C3, C4 nerve roots | C3, C4 | ||
| 2. Levator scapulae | C3, C4 nerve roots | C3, C4 | |
| Dorsal scapular | C5 | ||
| 3. Rhomboid major | Dorsal scapular | (C4), C5 | |
| 4. Rhomboid minor | Dorsal scapular | (C4), C5 | |
| Depression of scapula | 1. Serratus anterior | Long thoracic | C5, C6, (C7) |
| 2. Pectoralis major | Lateral pectoral | C5, C6 (lateral cord) | |
| 3. Pectoralis minor | Medial pectoral | C8, T1 (medial cord) | |
| 4. Latissimus dorsi | Thoracodorsal | C6–C8 (posterior cord) | |
| 5. Trapezius (lower fibers) | Accessory | Cranial nerve XI | |
| C3, C4 nerve roots | C3, C4 | ||
| Protraction (forward movement) of scapula | 1. Serratus anterior | Long thoracic | C5, C6, (C7) |
| 2. Pectoralis major | Lateral pectoral | C5, C6 (lateral cord) | |
| 3. Pectoralis minor | Medial pectoral | C8, T1 (medial cord) | |
| 4. Latissimus dorsi | Thoracodorsal | C6–C8 (posterior cord) | |
| Retraction (backward movement) of scapula | 1. Trapezius | Accessory | Cranial nerve XI |
| 2. Rhomboid major | Dorsal scapular | (C4), C5 | |
| 3. Rhomboid minor | Dorsal scapular | (C4), C5 | |
| Lateral (upward) rotation of inferior angle of scapula | 1. Trapezius (upper and lower fibers) | Accessory | Cranial nerve XI |
| C3, C4 nerve roots | C3, C4 | ||
| 2. Serratus anterior | Long thoracic | C5, C6, (C7) | |
| Medial (downward) rotation of inferior angle of scapula | 1. Levator scapulae | C3, C4 nerve roots | C3, C4 |
| 2. Rhomboid major | Dorsal scapular | C5 | |
| 3. Rhomboid minor | Dorsal scapular | (C4), C5 | |
| 4. Pectoralis minor | Dorsal scapular | (C4), C5 | |
| Medial pectoral | C8, T1 (medial cord) | ||
| Flexion of elbow | 1. Brachialis | Musculocutaneous | C5, C6, (C7) |
| 2. Biceps brachii | Musculocutaneous | C5, C6 | |
| 3. Brachioradialis | Radial | C5, C6, (C7) | |
| 4. Pronator teres | Median | C6, C7 | |
| 5. Flexor carpi ulnaris | Ulnar | C7, C8 | |
| Extension of elbow | 1. Triceps | Radial | C6–C8 |
| 2. Anconeus | Radial | C7, C8, (T1) |
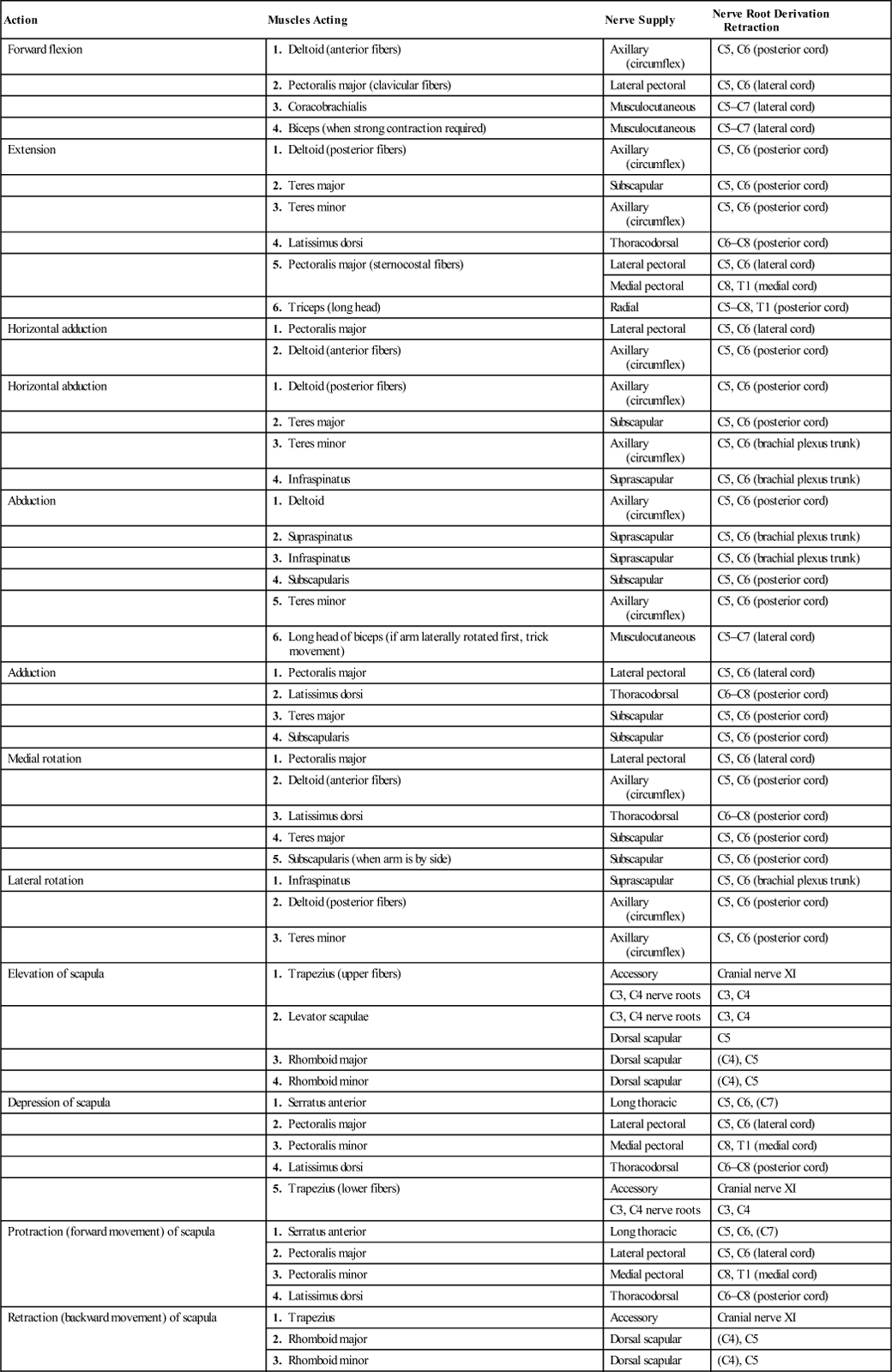
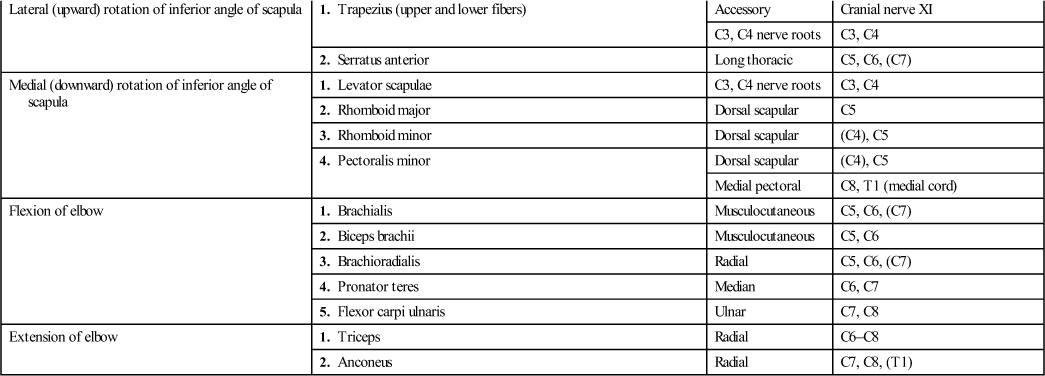
Resisted isometric elbow flexion and extension must be performed, because some of the muscles (e.g., biceps, triceps) act over the elbow as well as the shoulder. The examiner should watch for the possibility of a third-degree strain (rupture) of the long head of biceps tendon (“Popeye muscle” or Popeye sign) when testing isometric elbow flexion (Figure 5-46).

Rupture of the long head of the biceps brachii caused by the patient’s awkward catch of partner in gymnastics. Bunching of muscle is attended by complete loss of function of the long head of biceps. (From O’Donoghue DH: Treatment of injuries to athletes, ed 4, Philadelphia, 1984, WB Saunders, p. 53.)
During testing, the examiner will find differences in the relative strengths of the various muscle groups around the shoulder. The relative percentages for isometric testing will be altered for tests at faster speeds and tests in different planes. If, in the history, the patient complained that concentric, eccentric, or econcentric (biceps and triceps) movements were painful or caused symptoms, these movements should also be tested, with loading or no loading, as required.
Functional Assessment
The shoulder complex plays an integral role in the ADLs, sometimes acting as part of an open kinetic chain and sometimes acting as part of a closed kinetic chain. Assessment of function plays an important part of the shoulder evaluation.123 Limitation of function can greatly affect the patient. For example, placing the hand behind the head (e.g., to comb the hair) requires almost full lateral rotation, whereas placing the hand in the small of the back (e.g., to get a wallet out of a back pocket or undo a bra) requires almost full medial rotation. Matsen, et al.57 have listed the functional ROM necessary to do some of the functional ADLs (Table 5-14) and Mannerkorpi, et al.124 and Dutton125 have outlined functional movements of the arm (Table 5-15). The tables point out that although full ROM is desirable, most functional tasks can be performed with less than full ROM.126 Test 1 in Table 5-15 measures the ability to do activities such as arm reach, pulling or hanging an object overhead, combing hair, or drinking from a cup. Test 2 measures the ability to do activities such as getting something out of a back pocket, scratching the back, or hooking a bra. Test 3 measures the ability to do such tasks as fastening a car seatbelt or turning a steering wheel.124,125
TABLE 5-14
Range of Motion Necessary at the Shoulder to Do Certain Activities of Daily Living
| Activity | Range of Motion | Activity | Range of Motion |
| Eating | 70° to 100° horizontal adduction* 45° to 60° abduction |
Hand behind head | 10° to 15° horizontal adduction* 110° to 125° forward flexion 90° lateral rotation |
| Combing hair | 30° to 70° horizontal adduction* 105° to 120° abduction 90° lateral rotation |
Put something on shelf | 70° to 80° horizontal adduction* 70° to 80° forward flexion 45° lateral rotation |
| Reach perineum | 75° to 90° horizontal abduction 30° to 45° abduction 90°+ medial rotation |
Wash opposite shoulder | 60° to 90° forward flexion 60° to 120° horizontal adduction* |
| Tuck in shirt | 50° to 60° horizontal abduction 55° to 65° abduction 90° medial rotation |
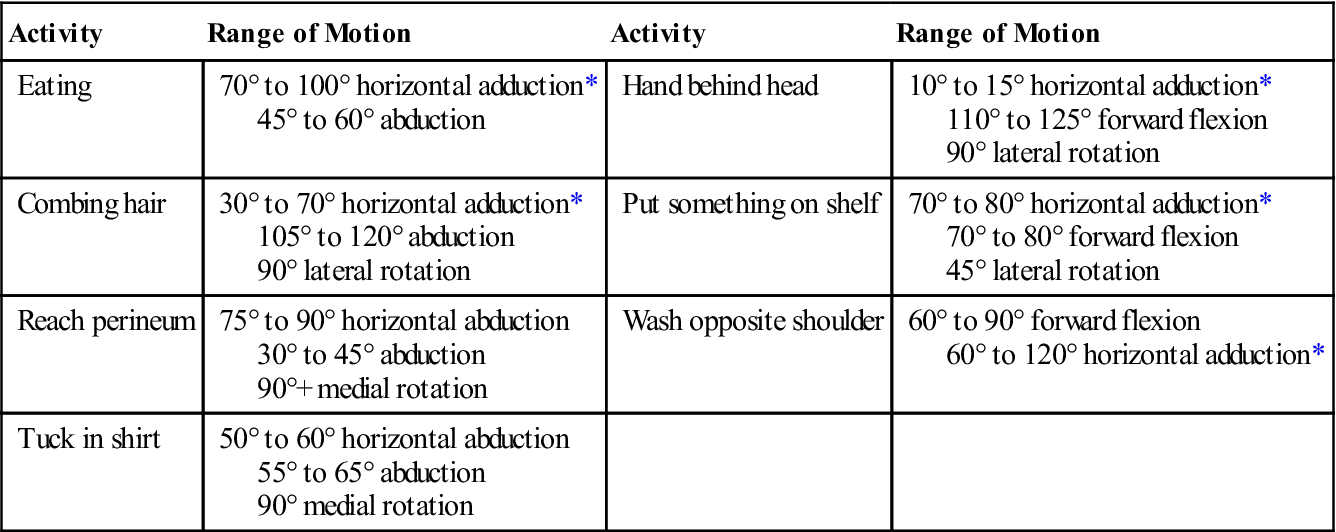
*Horizontal adduction is from 0° to 90° of abduction.
Adapted from Matsen FA, et al: Practical evaluation and management of the shoulder, Philadelphia, 1994, WB Saunders, pp. 20, 24.
TABLE 5-15
Scoring for Functional Shoulder Movements of the Arm
| Hand-To-Back of Neck (Test 1) | |
| 0 | The fingers reach the posterior median line of the neck with the shoulder in full abduction and lateral rotation. The wrist is not dorsally extended. |
| 1 | The fingers reach the median line of the neck but do not have full abduction and/or lateral rotation. |
| 2 | The fingers reach the median line of the neck, but with compensation by adduction (over 20° in the horizontal plane) or by shoulder elevation. |
| 3 | The fingers touch the neck. |
| 4 | The fingers do not reach the neck. |
| Hand-To-Scapula (From Behind) (Test 2) | |
| 0 | The hand reaches behind the trunk to the opposite scapula or 5 cm beneath it in full medial rotation. The wrist is not laterally deviated. |
| 1 | The hand reaches the opposite scapula 6 cm to 15 cm beneath it. |
| 2 | The hand reaches the opposite iliac crest. |
| 3 | The hand reaches the buttock. |
| 4 | Cannot move the hand behind the trunk. |
| Hand-To-Opposite Scapula (From in Front) (Test 3) | |
| 0 | The hand reaches the spine of the opposite scapula in full adduction without wrist flexion. |
| 1 | The hand reaches the spine of the opposite scapula in full adduction. |
| 2 | The hand passes the midline of the trunk. |
| 3 | The hand cannot pass the midline of the trunk. |
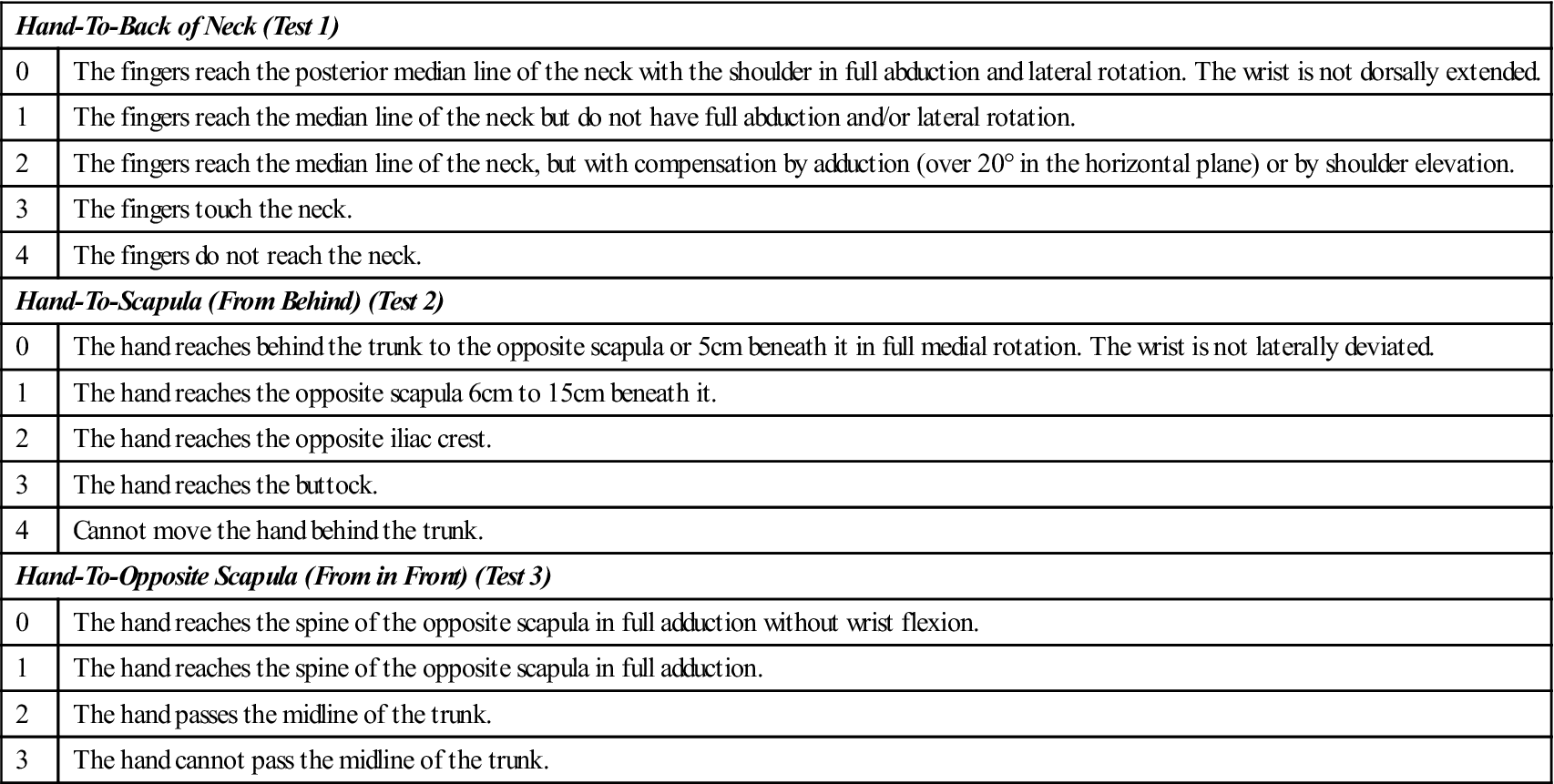
Modified from Mannerkorpi K, et al: Tests of functional limitations in fibromyalgia syndrome: a reliability study. Arthr Care Res 12(3):195, 1999; and Dutton M: Dutton’s orthopedic examination, evaluation and intervention, ed 3, New York, 2012, McGraw-Hill, p. 511.
The functional assessment may be based on ADLs, work, or recreation and outcomes measures,127 because these activities are of most concern to the patient (Figure 5-47),128–130 or it may be based on numerical scoring charts (Figures 5-48 to 5-51 are examples), which are derived from clinical measures as well as functional measures. Some numerical evaluation scales are designed for specific populations, such as athletes (see Figure 5-48), level of disability131–134 (see Figure 5-49), or specific injuries, such as instability (see Figure 5-51). Other shoulder rating scales are also available.135–146 When using numerical scoring charts, the examiner should not place total reliance on the scores, because most of these charts are based primarily on the examiner’s clinical measures and not the patient’s subjective functional, hoped-for outcome, which is the patient’s primary concern.147,148 Probably the most functional numerical shoulder tests from a patient’s perspective are the simple shoulder test (Figure 5-52) developed by Lippitt, Matsen, and associates,57,130,149,150 the Disabilities of the Arm, Shoulder, and Hand (DASH) test by Hudak, et al.130,151 (Figure 5-53) and its modification—the Quick DASH,152 the Shoulder Pain and Disability Index (SPADI) (see Figure 5-49),133 and the Penn Shoulder Score by Leggin, et al.153,154 Table 5-16 provides the examiner with a method of determining the patient’s functional shoulder strength and endurance. This table is based on the general population and would not indicate a true functional reading of athletes or persons who do heavy work involving the shoulders. For athletes or those applying significant load to their shoulders while forward flexed, the one-arm hop test has been developed (Figure 5-54). To do this test, the patient assumes the pushup position, balancing on one arm. The patient then hops up onto a 10-cm (4-inch) step and then back to the floor. The hop is repeated five times and the time noted. The patient starts with the good arm and then uses the injured arm, and the two times are compared. Provided that the patient is trained, completing this action in less than 10 seconds is considered normal.155
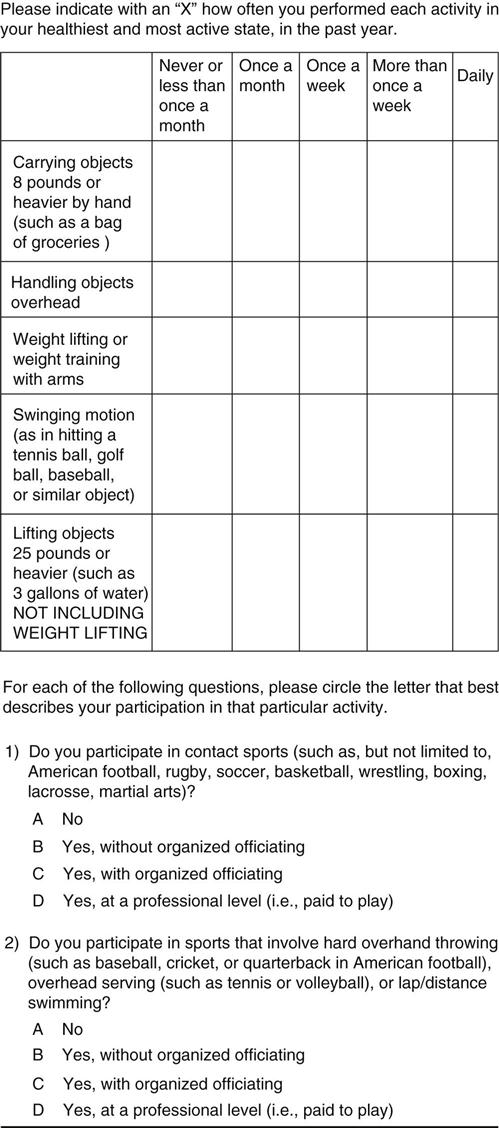
It includes five numerically-scored items and two alpha-scored items. (From Brophy RH, Beauvais RL, Jones EC, et al: Measurement of shoulder activity level. Clin Orthop Relat Res 439:105, 2005.)
TABLE 5-16
Functional Testing of the Shoulder
| Starting Position | Action | Function Test* |
| Sitting | Forward flex arm to 90° | |
| Sitting | Shoulder extension | |
| Side lying (may be done in sitting with pulley) | Shoulder medial rotation | |
| Side lying (may be done in sitting with pulley) | Shoulder lateral rotation | |
| Sitting | Shoulder abduction | |
| Sitting | Shoulder adduction (using wall pulley) | |
| Sitting | Shoulder elevation (shoulder shrug) | |
| Sitting | Sitting pushup (shoulder dysfunction) |
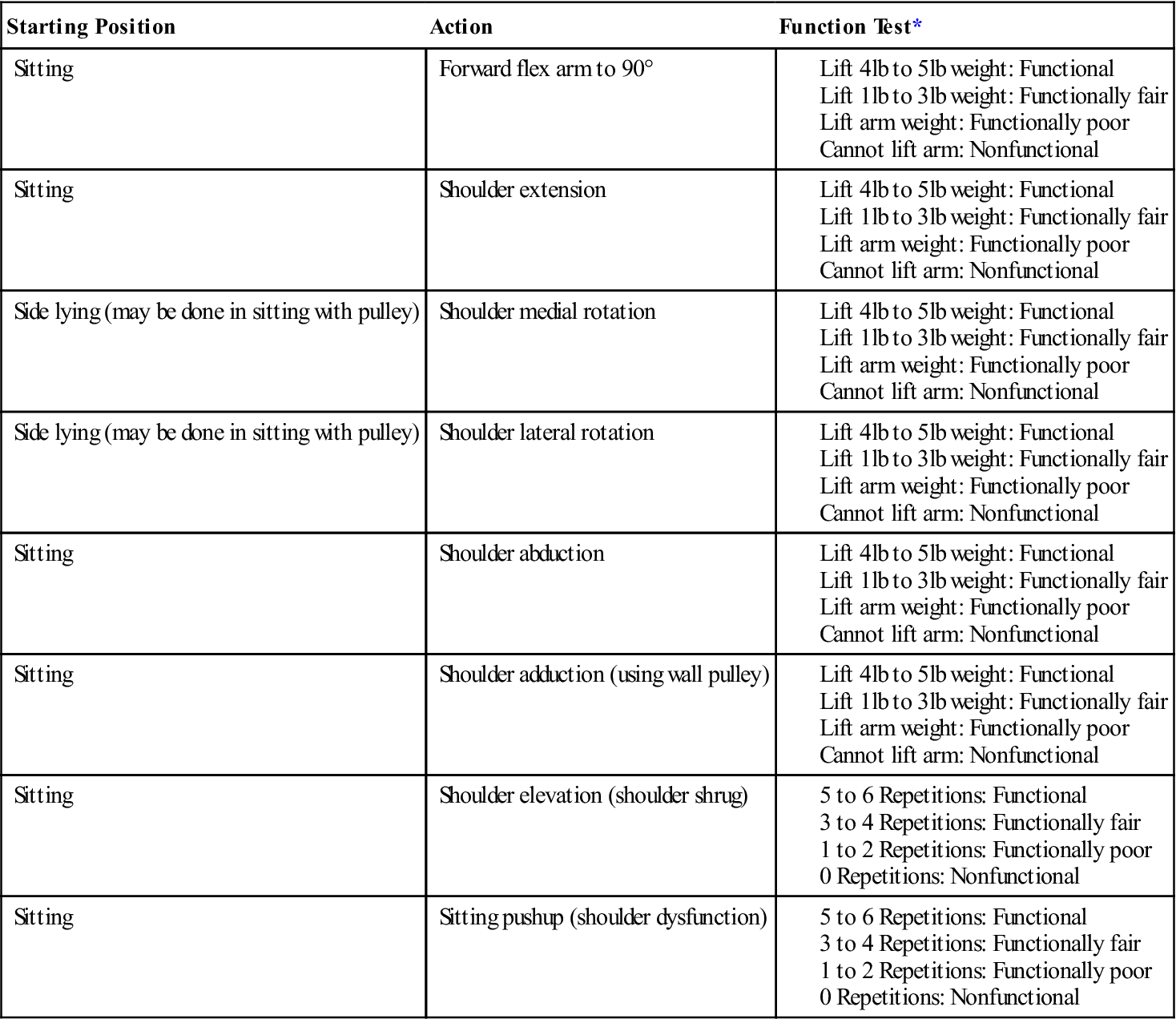
*Younger, more fit patients should easily be able to do more than the values given for these tests. A comparison between the good side and the injured side gives the examiner some idea about the patient’s functional strength capacity.
Data from Palmer ML, Epler M: Clinical assessment procedures in physical therapy, Philadelphia, 1990, JB Lippincott, pp. 68–73.
Burkhart, et al. felt it was important to test core stability (i.e., testing kinetic chain function) and flexibility when assessing the shoulder to ensure the proper transfer of forces from the legs to the trunk and the shoulder as part of the kinetic chain.31 They advocated testing one-legged stance (no Trendelenburg), one-legged squat (stable pelvis), one-legged step up and step down (stable pelvis), normal hip medial rotation bilaterally, and strength of hip abductors, trunk flexors, and abdominal muscles.
Special Tests
Special tests are often used in shoulder examinations to confirm findings or a tentative diagnosis. Many of the tests, especially those involving the labrum, have not shown high sensitivity or specificity; so, often a combination of tests (i.e., test clusters, clinical prediction rules) may be more helpful156,157 although even in these cases, the tests are not necessarily definitive. The examiner must be proficient in those tests that he or she decides to use. Proficiency increases the reliability of the findings, although the reliability of some of the tests has been questioned.158 Depending on the patient history, some tests are compulsory, and others may be used as confirming or excluding tests. As with all passive tests, results are more likely to be positive in the presence of pathology when the muscles are relaxed, the patient is supported, and there is minimal or no muscle spasm.
For the reader who would like to review them, the reliability, validity, specificity, sensitivity, and odds ratios of some of the special tests used in the shoulder are available on the Evolve website.
Instability and Pseudolaxity Impingement
Anterior shoulder pain is commonly seen in patients young and old complaining of shoulder pain and dysfunction. Instability at the shoulder manifests itself as symptomatic abnormal motion within the shoulder complex, including the scapula. This abnormal motion may be the result of abnormal scapular or glenohumeral muscle patterning, hypo- or hypermobility of the capsule (most commonly a tight posterior capsule) or ribs, a labral tear (a Bankart or SLAP lesion), a rotator cuff or biceps injury, altered surface area of contact between the glenoid and humeral head, and/or a problem with the central or peripheral nervous system.104
In the older patient (40-years-old or older), mechanical impingement occurs because of degenerative changes to the rotator cuff, the acromion process, the coracoid process, and the anterior tissues from stress overload resulting in impingement. In this case, impingement is the primary problem (thus, the term primary impingement). It may be intrinsic because of rotator cuff degeneration or extrinsic because of the shape of the acromion and degeneration of the coracoacromial ligament.166
In the young patient (15 to 35-years-old), anterior shoulder pain is primarily caused by problems with muscle dynamics with an upset in the normal force couple action leading to muscle imbalance and abnormal movement patterns at both the glenohumeral joint and the scapulothoracic articulation. These altered muscle dynamics lead to symptoms of anterior impingement (thus, the term secondary impingement). The impingement signs are a secondary result of altered muscle dynamics in the scapula or glenohumeral joint.166
APPENDIX 5-1
Reliability, Validity, Specificity and Sensitivity of Special/Diagnostic Tests Used in the Shoulder
| ACROMIOCLAVICULAR-RESISTED EXTENSION TEST | ||
| Specificity | Sensitivity | Odds Ratio |
| ANTERIOR APPREHENSION TEST | ||
| Specificity | Sensitivity | Odds Ratio |
| ANTERIOR RELEASE TEST | ||||
| Reliability | Validity | Specificity | Sensitivity | Odds Ratio |
| AUGMENTATION TEST |
| Reliability |
| BICEPS LOAD TEST I | |||
| Reliability | Specificity | Sensitivity | Odds Ratio |
| BICEPS LOAD TEST II FOR SLAP LESIONS | |||
| Reliability | Specificity | Sensitivity | Odds Ratio |
| BICIPITAL GROOVE TENDERNESS | ||
| Specificity | Sensitivity | Odds Ratio |
| CLUNK TEST | ||
| Specificity | Sensitivity | Odds Ratio |
| COMBINATION FOR SLAP AND LABRAL LESIONS | |||
| Test | Specificity | Sensitivity | Odds Ratio |
| Jobe and O’Brien | |||
| Jobe and apprehension | |||
| O’Brien and apprehension | |||
| Jobe, O’Brien, and apprehension | |||

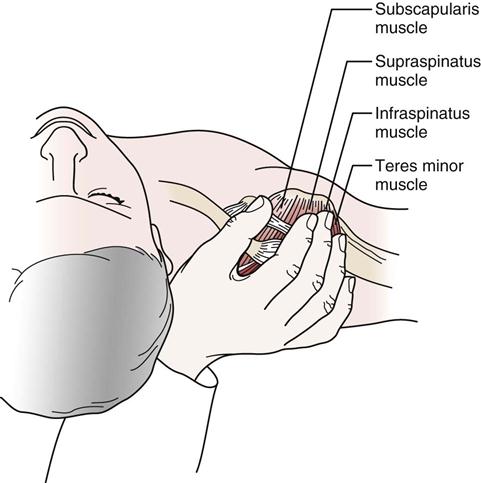
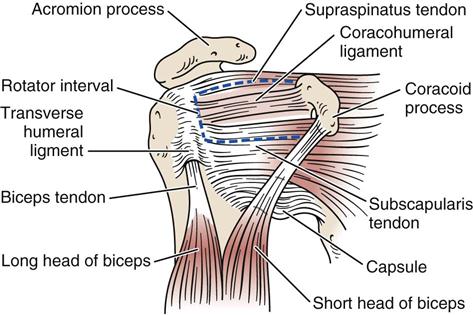
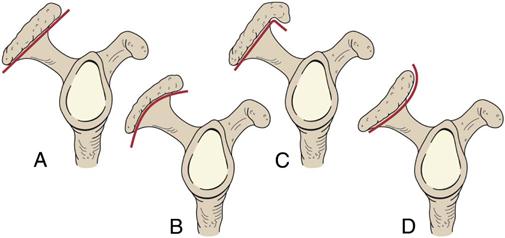
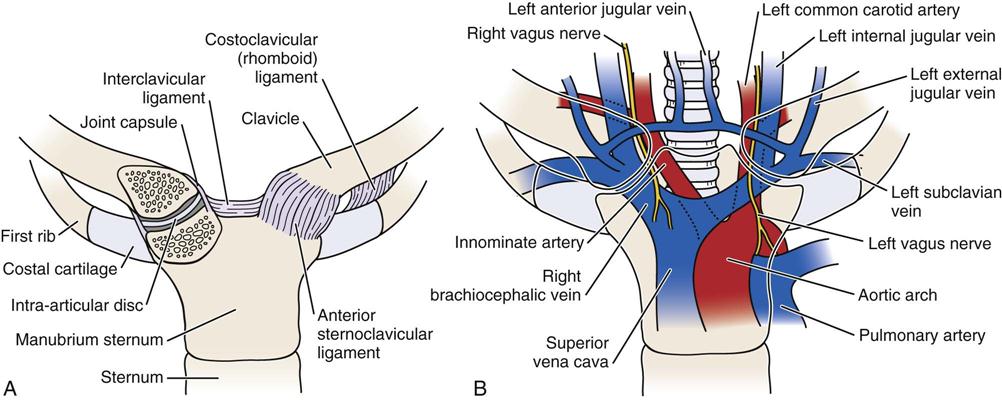

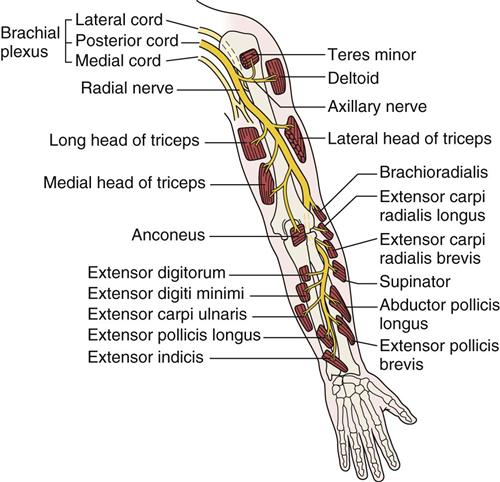
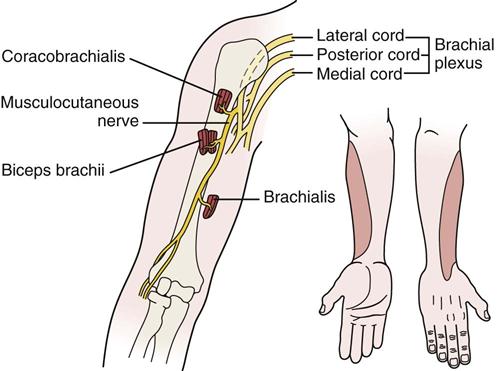
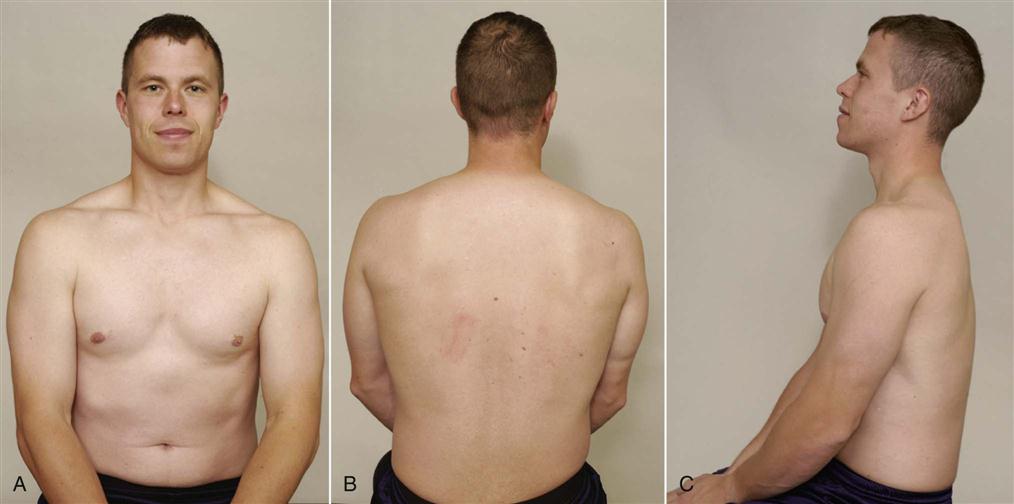
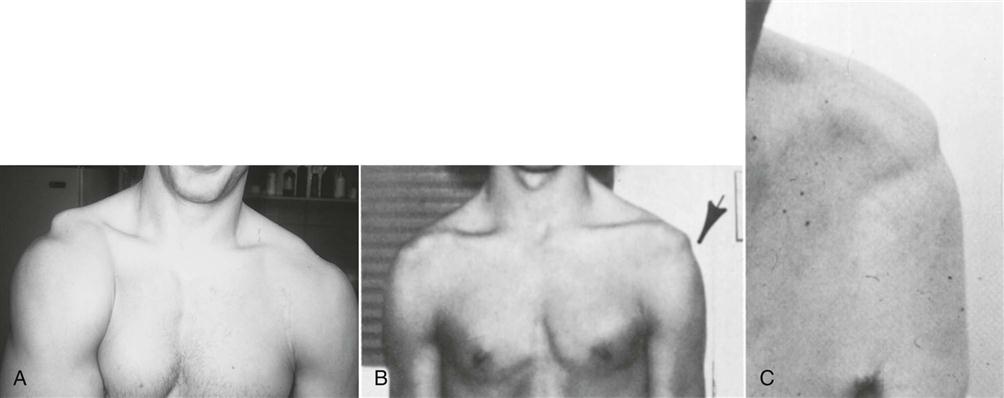
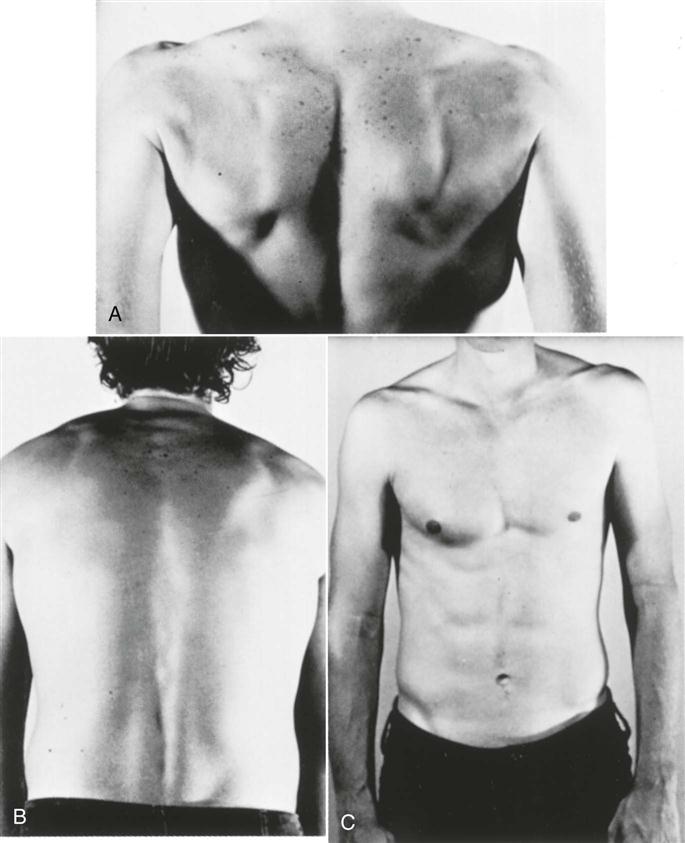

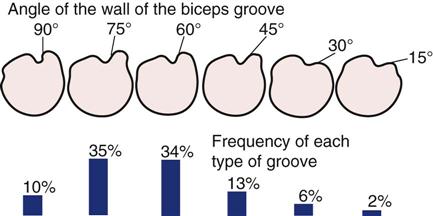
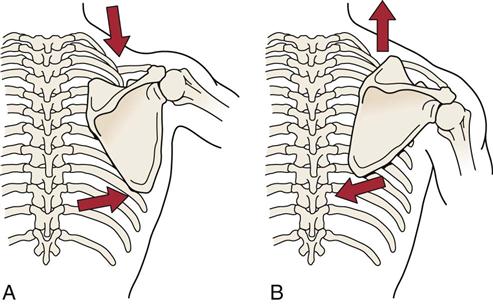
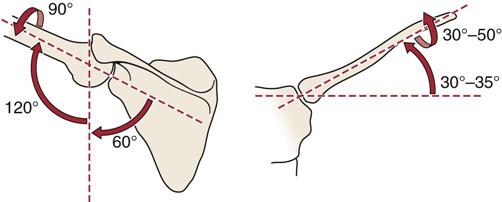
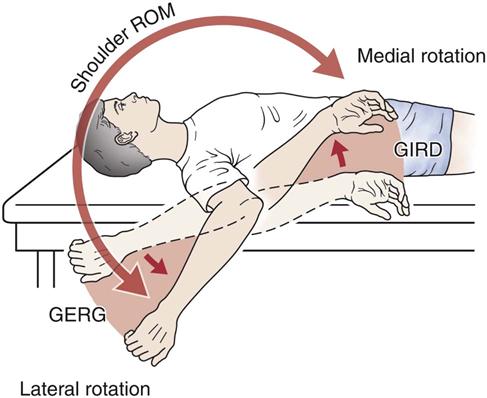
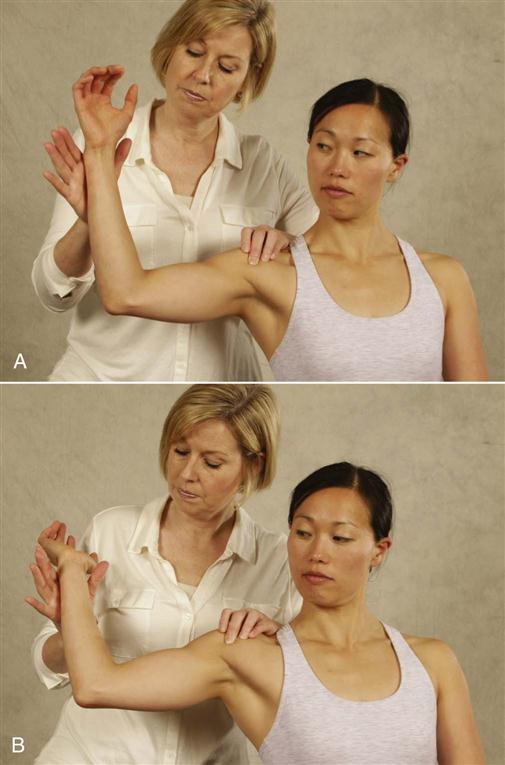
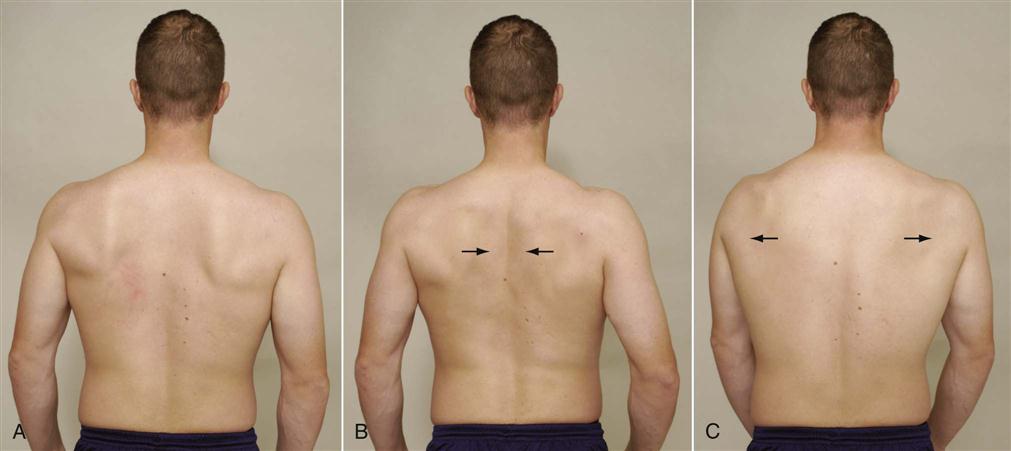
 Figure 5-37
Figure 5-37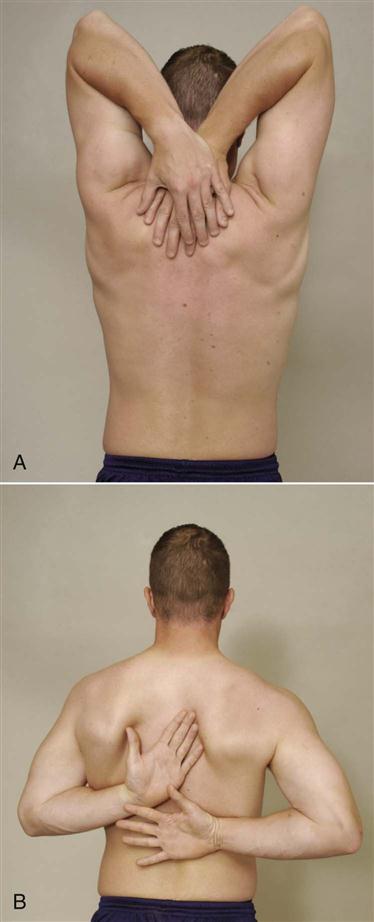
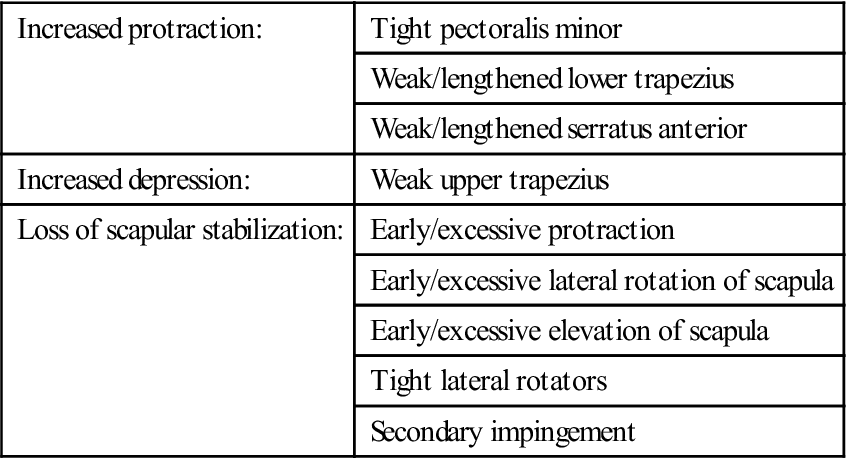
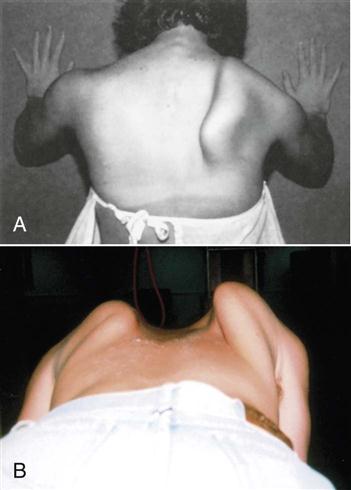

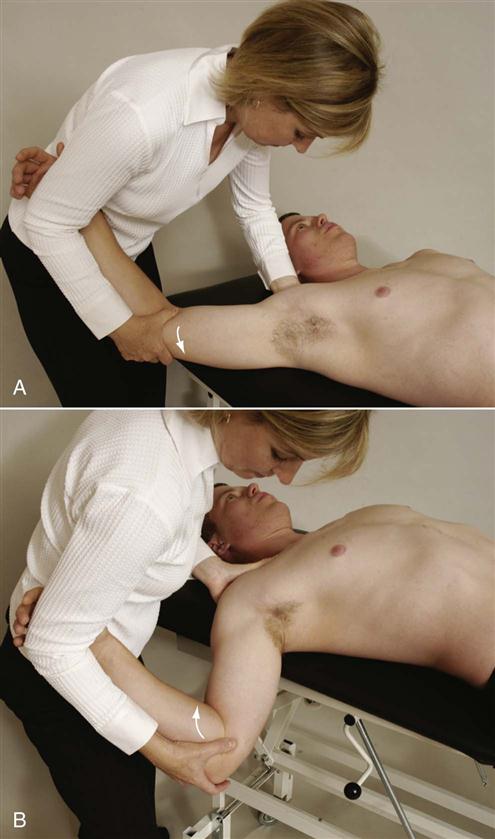

 Figure 5-45
Figure 5-45