Knee
The knee joint is particularly susceptible to traumatic injury because it is located at the ends of two long lever arms, the tibia and the femur. In addition, because the joint connects one long bone “sitting” on another long bone, it depends on the ligaments and muscles that surround it for its strength and stability, not on its bony configuration.1
Because the knee joint depends on its ligaments to such a great extent, it is imperative that the ligaments be tested during the examination of the knee. Therefore the ligamentous tests are not included under the “Special Tests” section but instead are listed in a separate section to ensure that they are always included in the examination of the knee.
Because of its anatomical arrangement, the knee is a complicated area to assess, and the examiner must take time to ensure that all relevant structures are tested. It must also be remembered that the lumbar spine, hip, and ankle may refer pain to the knee, and these joints must be assessed if it appears that joints other than the knee may be involved. For example, a slipped capital femoral epiphysis at the hip commonly refers pain to the knee, and this knee pain may predominate.
Applied Anatomy
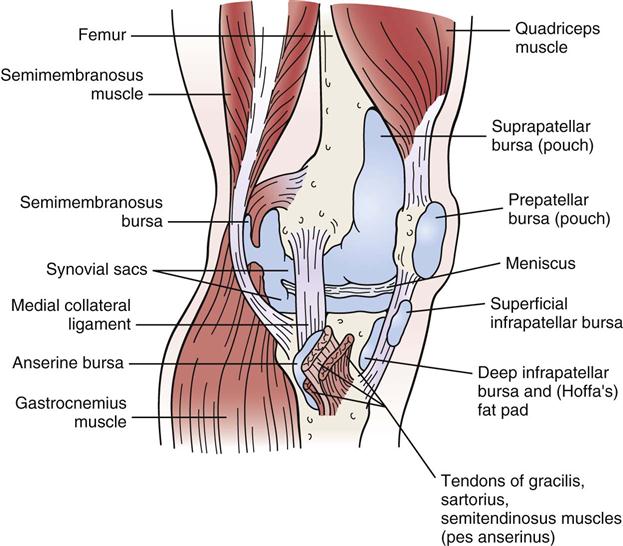
The tibiofemoral joint is the largest joint in the body. It is a modified hinge joint having 2° of freedom. The synovium around the joint is extensive; it communicates with many of the bursae and pouches around the knee joint. Although the synovial membrane “encapsulates” the entire knee joint, its distribution within the knee is such that the cruciate ligaments, which run from the middle of the tibial plateau to the intercondylar area of the femur, are extrasynovial. (Cruciate means that the ligaments cross each other.)
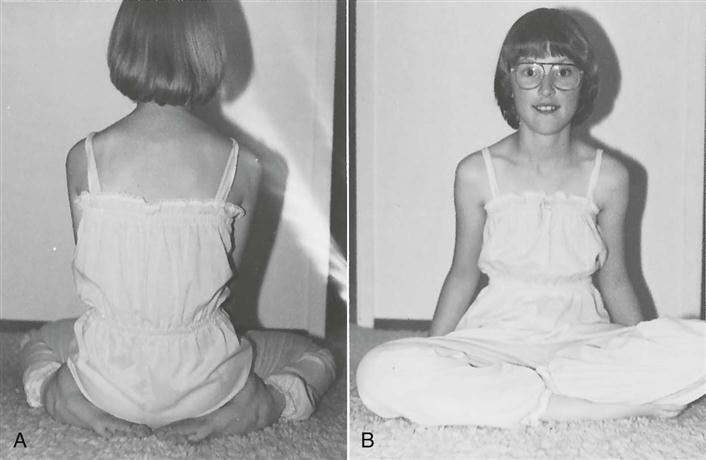
The articular surfaces of the tibia and femur are not congruent, which enables the two bones to move different amounts, guided by the muscles and ligaments. The two bones approach congruency in full extension, which is the close packed position. Kaltenborn2 has stated that the close packed position includes full lateral rotation of the tibia. The lateral femoral condyle projects anteriorly more than the medial femoral condyle to help prevent lateral dislocation of the patella. In females, this enlargement is important because of the female’s broader pelvis and increased inward angle of the femur, which allow the femoral condyles to be parallel with the ground (Figure 12-1). The resting position of the joint is approximately 25° of flexion, and the capsular pattern is flexion more limited than extension.
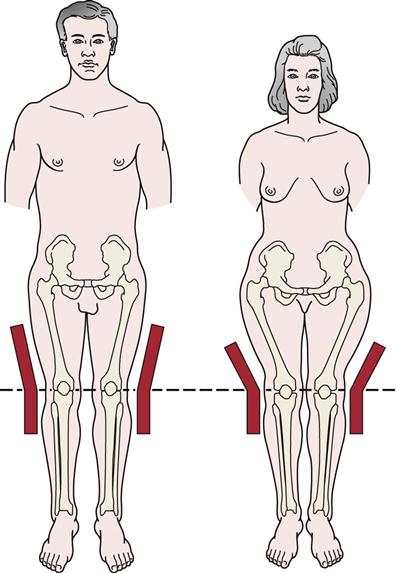
Because of the broader pelvis in the female, it is necessary for the femur to come inward at an increased angle to make the distal end of the condyles parallel with the ground. The quadriceps, patella, and patellar tendon form an angle centered at the patella. As the quadriceps contracts, the angle tends to straighten, which forces the patella laterally. (Redrawn from O’Donoghue D: Treatment of injuries to athletes, ed 4, Philadelphia, 1984, WB Saunders, p. 522.)
The space between the tibia and femur is partially filled by two menisci that are attached to the tibia to add congruency. The medial meniscus is a small part of a large circle (i.e., C shaped) and is thicker posteriorly than anteriorly. The lateral meniscus is a large part of a small circle (i.e., O shaped) and is generally of equal thickness throughout. Both menisci are thicker along the periphery and thinner along the inner margin.
During the movement from extension to flexion, both menisci move posteriorly, the lateral meniscus being displaced more than the medial meniscus. The lateral meniscus has an excursion of 10 mm, and the medial meniscus has an excursion of 2 mm. The menisci are avascular in their cartilaginous inner two thirds and are partly vascular and fibrous in their outer one third.3 They are held in place by the coronary ligaments attaching to the tibia.
The menisci serve several functions in the knee. They aid in lubrication and nutrition of the joint and act as shock absorbers (a meniscectomy can reduce shock absorption capacity at the knee by 20%),4 spreading the stress over the articular cartilage and decreasing cartilage wear. They make the joint surfaces more congruent and improve weight distribution by increasing the area of contact between the condyles. The menisci reduce friction during movement and aid the ligaments and capsule in preventing hyperextension. The menisci prevent the joint capsule from entering the joint and participate in the “locking” mechanism of the joint into close pack by directing the movement of the femoral articular condyles. Because more recent literature indicates that removal of the entire meniscus can lead to early degeneration of the joint,5,6 most surgeons today remove only the torn portion of the meniscus, or, if the tear is in the outer one third where there is sufficient circulation to aid healing, the surgeon may attempt to surgically repair (suture) the meniscus.
It is generally believed that the meniscus possesses minimal innervation so there is minimal or no pain when it is damaged unless the coronary ligaments have been damaged as well. Gray7 has reported, however, that the menisci possess innervation in their outer two thirds with the anterior and posterior horns being well innervated. Because the menisci are primarily avascular, especially in the inner two thirds, there is seldom bloody effusion in injury; however, there may be synovial effusion. Their poor blood supply, especially in the inner two thirds, gives the menisci a low regeneration potential.
The lateral meniscus is not as firmly attached to the tibia as the medial meniscus and therefore is less prone to injury. The coronary ligaments, also referred to as the meniscotibial ligaments, tend to be longer on the lateral aspect, and the horns of the lateral meniscus are closer together.
The patellofemoral joint is a modified plane joint, the lateral articular surface of the patella being wider. The patella contains the thickest layer of cartilage in the body and, in reality, is a sesamoid bone found within the patellar tendon. It has five facets, or ridges: superior, inferior, lateral, medial, and odd. It is the odd facet that is most frequently the first part of the patella to be affected in chondromalacia patellae (i.e., premature degeneration of the patellar cartilage) or patellofemoral syndrome.
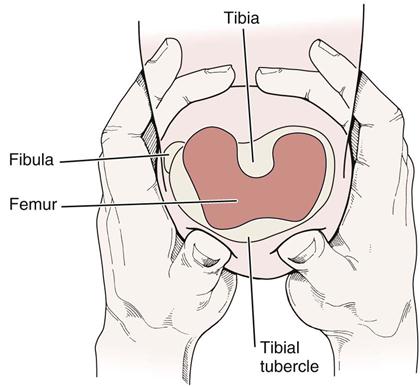
During the movement from flexion to extension, different parts of the patella articulate with the femoral condyles (Figure 12-2).8,9 The odd facet does not come into contact with the femoral condyles until at least 135° of flexion is reached. Incorrect alignment or malalignment of the patellar movement over the femoral condyles can lead to patellofemoral arthralgia. The capsule of this joint is continuous with the capsule of the tibiofemoral joint.
The patella improves the efficiency of extension during the last 30° of extension (i.e., 30° to 0° of extension with the straight leg being 0°), because it holds the quadriceps tendon away from the axis of movement. The patella also functions as a guide for the quadriceps or patellar tendon, decreases friction of the quadriceps mechanism, controls capsular tension in the knee, acts as a bony shield for the cartilage of the femoral condyles, and improves the aesthetic appearance of the knee (Figure 12-3).
The superior tibiofibular joint is a plane synovial joint between the tibia and the head of the fibula. It is supported by anterior and posterior ligaments of the same name. Movement occurs in this joint with any activity involving the ankle. Hypomobility at this joint can lead to pain in the knee area on activity, because the fibula can bear up to one sixth of the body weight. In approximately 10% of the population, the capsule of this joint is continuous with that of the tibiofemoral joint.
Patient History
In addition to the questions listed under the “Patient History” section in Chapter 1, the examiner should obtain the following information from the patient:
1. How did the accident occur, or what was the mechanism of injury?10,11 The primary mechanisms of injury in the knee are a valgus force (with or without rotation), hyperextension, flexion with posterior translation, and a varus force.12 The first often results in injury to the medial collateral ligament, frequently accompanied by injury to the posteromedial capsule, medial meniscus, and anterior cruciate (“terrible triad”). The second leads to anterior cruciate injuries, often associated with meniscus tears. The third mechanism of injury often involves the posterior cruciate ligament, and the fourth mechanism involves the lateral collateral ligament, the posterolateral capsule, and the posterior cruciate ligament. Was the injury the result of trauma, such as a direct or an indirect blow? Bauer, et al.13 developed a clinical prediction rule for determining whether a fracture was present in an acute knee injury (see the box on the next page). Was the patient bearing weight at the time of injury? From which direction did the injuring force come? For example, meniscal injuries, especially those on the medial side, occur as a result of a torsion injury that combines compression and rotation. Slowly developing forces tend to cause bony avulsions, whereas rapidly developing forces tend to tear ligaments. In young children, injuries to the growth plate or physis may occur instead of injury to the ligaments, especially during a rapid growth spurt when the physis is weaker than the ligaments. Injuries may occur to the distal femoral physis, the proximal tibial physis, and the tibial tubercle apophysis (traction epiphysis).14,15 Injury to this last structure is called Osgood-Schlatter disease. Table 12-1 lists typical mechanisms of injury to the knee and the structures injured. The lower limb may be viewed as an open (foot off the ground) or a closed (foot on the ground) kinetic chain (Figure 12-4). There is less chance of injury when the lower limb is an open kinetic chain. As a closed kinetic chain, the lower limb is an encapsulated system in which all parts work in concert. Forces applied to one part of the chain must be absorbed by that part as well as by other parts of the closed chain. If the forces are too great, injury results.
2. Has the knee been injured before, or does it have any feeling of weakness?
3. What is the patient able or unable to do functionally? Is there disability on running, cutting, pivoting, twisting, climbing, or descending stairs? Positive responses to these questions should alert the examiner to instability caused by injured ligaments, muscle dysfunction, joint articular problems, or meniscus problems.16
4. Is there any “clicking,” or was there a “pop” when the injury occurred? A distinct pop may indicate an anterior cruciate ligament tear or osteochondral fracture. Popping on the lateral aspect of the knee may be due to the popliteus tendon snapping over the lateral femoral inferoposterior tubercle within 2 cm of the muscle’s attachment into the femur.17
6. Is there any pain? If so, where? What type is it? Retropatellar? Does the patient point to one spot with one finger or a more general area indicating the problem is more diffuse, aching? Aching pain may indicate degenerative changes, whereas sharp, “catching” pain usually indicates a mechanical problem. Arthritic pain is more likely to be associated with stiffness in the morning and eases with activity. Anterior knee pain may be due to patellofemoral problems, bursa (prepatellar, infrapatellar) pathology, fat pad pathology, tendinosis, or Osgood-Schlatter disease.18,19 Patellofemoral pain tends to be insidious and occurs spontaneously, often from overuse, which makes establishing the source of the problem important.20,21 Pain at rest is not usually mechanical in origin. Pain during activity is usually seen in structural abnormalities, such as subluxation or patellar tracking disorders. Pain after activity or with overuse is characteristic of inflammatory disorders, such as synovial plica irritation or early tendinosis or paratenonitis leading to jumper’s knee or Sinding-Larsen-Johansson syndrome.22–27 Generalized pain in the area of the knee is usually characteristic of contusions or partial tears of muscles or ligaments. Instability rather than pain tends to be the major presenting factor in complex ligament disruptions or muscle dysfunction (e.g., quadriceps rupture). Pain in the knee on ankle movements may implicate the superior tibiofibular joint.
7. Do certain positions or activities have an increased or decreased effect on the pain? Which activities produce pain? How much activity is needed to produce pain? Which positions or activities ease the pain? Does the pain go away when activity ceases? The examiner must take note of constant pain that is unrelated to activity, time, or posture, because it usually indicates serious pathology, such as a tumor. Does the patient have confidence in the knee? Such a question gives the examiner some idea of the functional impairment from the patient’s perspective.28
8. Does the knee “give way?”28 This finding usually indicates instability in the knee, meniscus pathology, patellar subluxation (if present when rotation or stopping is involved), undisplaced osteochondritis dissecans, patellofemoral syndrome, plica, or loose body. Giving way when walking uphill or downhill is more likely the result of a retropatellar lesion.16,29 If the patient complains that the patella “slips out of place,” it may be because of patellar subluxation or a pathological plica.30
9. Has the knee ever locked? True locking of the knee is rare. Loose bodies may cause recurrent locking. Locking must be differentiated from catching, which is momentary locking or giving way as a result of reflex inhibition or pain.30 Locking in the knee usually means that the knee cannot fully extend with flexion often being normal, and it is related to meniscus pathology. Hamstring muscle spasm may also limit extension and is sometimes referred to as spasm locking.
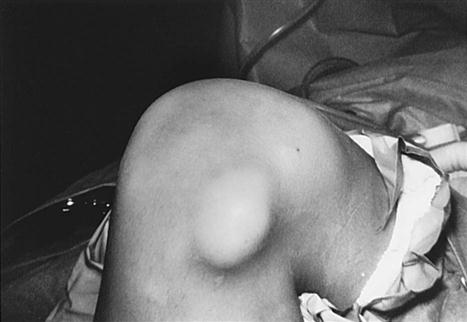
11. Is the joint swollen? Does the swelling occur with activity or several hours after activity, or does the joint feel tight at rest? Swelling with activity may be caused by instability, and tightness at rest may be caused by arthritic changes or patellofemoral dysfunction. Is the swelling recurrent? If so, what activity causes it? Swelling with pivoting or twisting may be a result of meniscus problems or instability at the tibiofemoral joint. Recurrent swelling caused by climbing or descending slopes or stairs may be related to patellofemoral dysfunction.30 Often there is no swelling in the knee after severe injury, because the fluid extravasates into the soft tissues surrounding the joint and because a number of structures around the knee joint are avascular and can be injured without bloody swelling occurring. Synovial swelling may occur 8 to 24 hours after the injury; swelling caused by blood begins to occur almost immediately. Localized swelling may be caused by an inflamed bursa (Figure 12-5).31 The deep infrapatellar bursa has been noted as a source of anterior knee pain and could be misdiagnosed as patellofemoral arthralgia or Osgood-Schlatter disease.32,33
TABLE 12-1
Mechanisms of Injury to the Knee and Possible Structures Injured
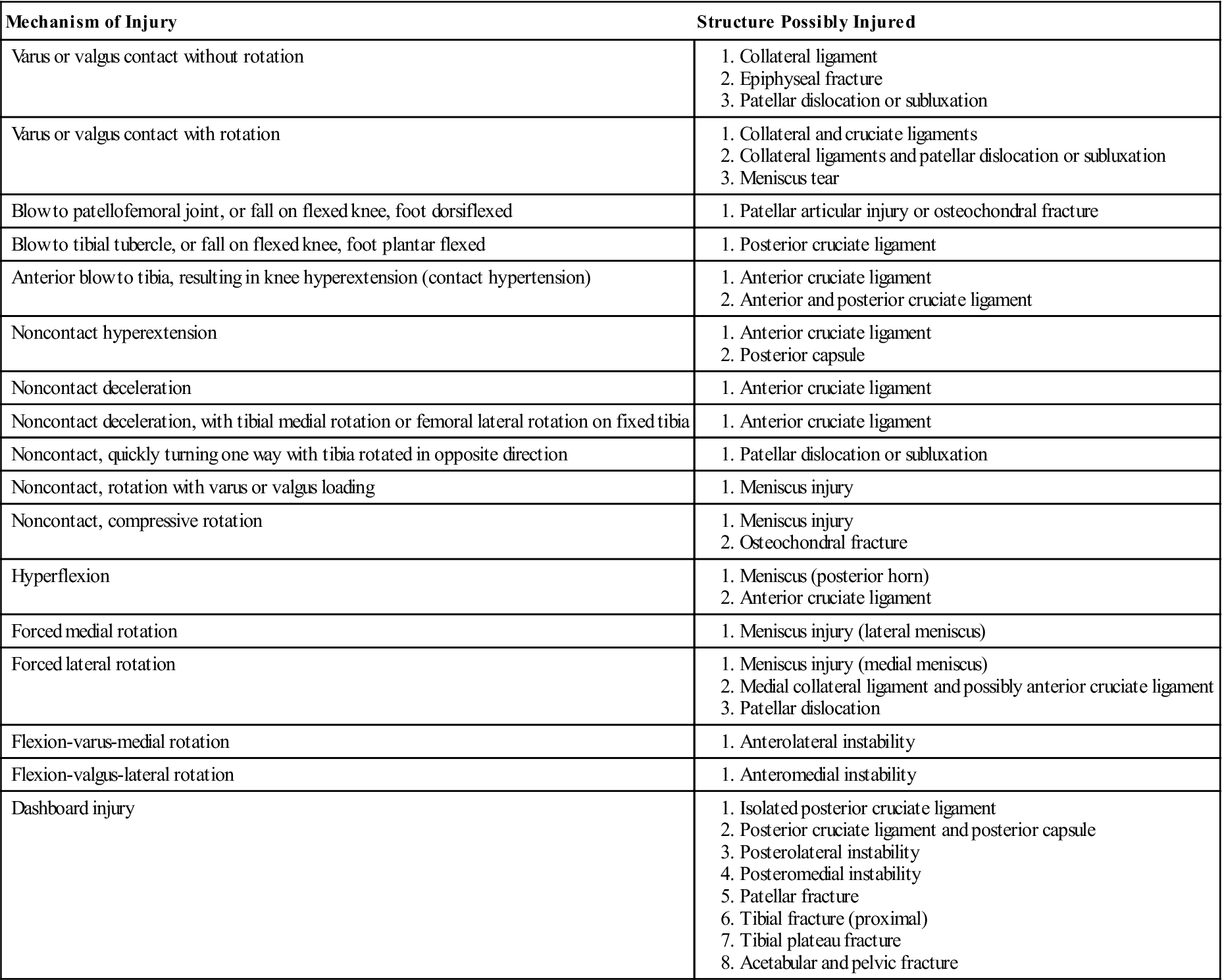
Adapted from Clancy W: Evaluation of acute knee injuries. In American Association of Orthopaedic Surgeons, Symposium on Sports Medicine: The knee, St Louis, 1985, Mosby; Strobel M, Stedtfeld HW: Diagnostic evaluation of the knee, Berlin, 1990, Springer-Verlag.
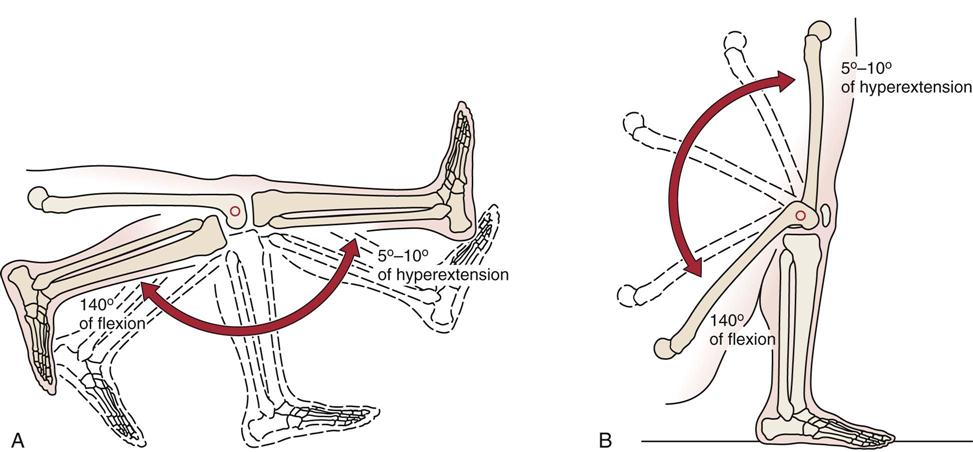
A, Tibial-on-femoral perspective (open kinetic chain). B, Femoral-on-tibial perspective (closed kinetic chain). (Modified from Neumann DA: Kinesiology of the musculoskeletal system—foundations for physical rehabilitation, St Louis, 2002, Mosby, p. 444.)
Observation
For a proper observation, the patient must be suitably undressed so that the examiner can observe the posture of the spine as well as the hips, knees, and ankles. Initially, the examiner should note whether the patient puts weight on the affected limb or stands with only a slight amount of weight on the affected side. In addition to the common observational items mentioned in Chapter 1, the examiner should look for the following alterations around the knee.
Anterior View, Standing
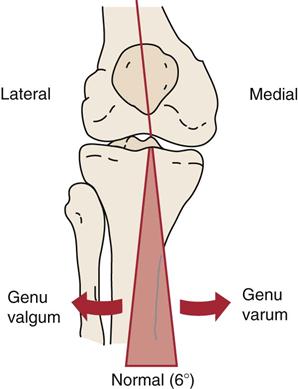
From the anterior aspect (Figure 12-6), the examiner should note any malalignment, including genu varum (bowleg) or genu valgum (knock-knee) deformity (Figure 12-7). Any observable malalignment may lead to or be the result of malalignment elsewhere (Table 12-2).34 These deformities may be unilateral or bilateral. Although in adults the legs should be relatively straight, in the child, the normal development of the knee is from genu varum to straight, to genu valgum, and then to straight. Initially, a child’s lower limbs are in genu varum until 18 or 19 months, when they straighten. The knee then goes into genu valgum until about 3 to 4 years of age (Figure 12-8). The limbs should be almost straight by age 6 years and should remain that way. In the adult, the knee is normally in approximately 6° of valgus.
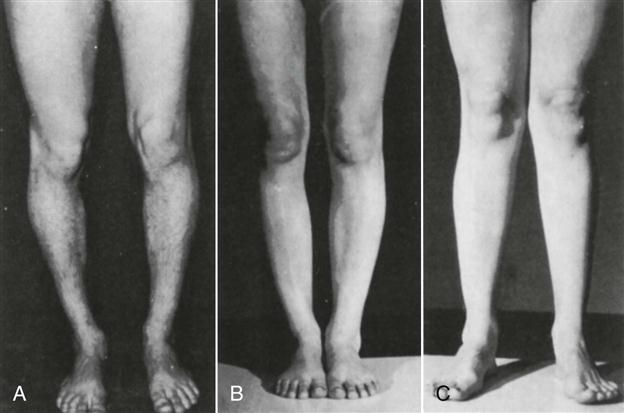
A, Tibia vara of proximal third. Genu varum deformity located mainly in proximal tibia. Along with lateral tibial torsion and medial femoral torsion, this gives a “bandy-legged” appearance. B, Genu varum of entire lower extremities. C, Genu valgum deformity of both lower extremities. (From Hughston JC, Walsh WM, Puddu G: Patellar subluxation and dislocation, Philadelphia, 1984, WB Saunders, p. 221.)
TABLE 12-2
Malalignment About the Knee and Possible Correlated and Compensatory Motions or Postures
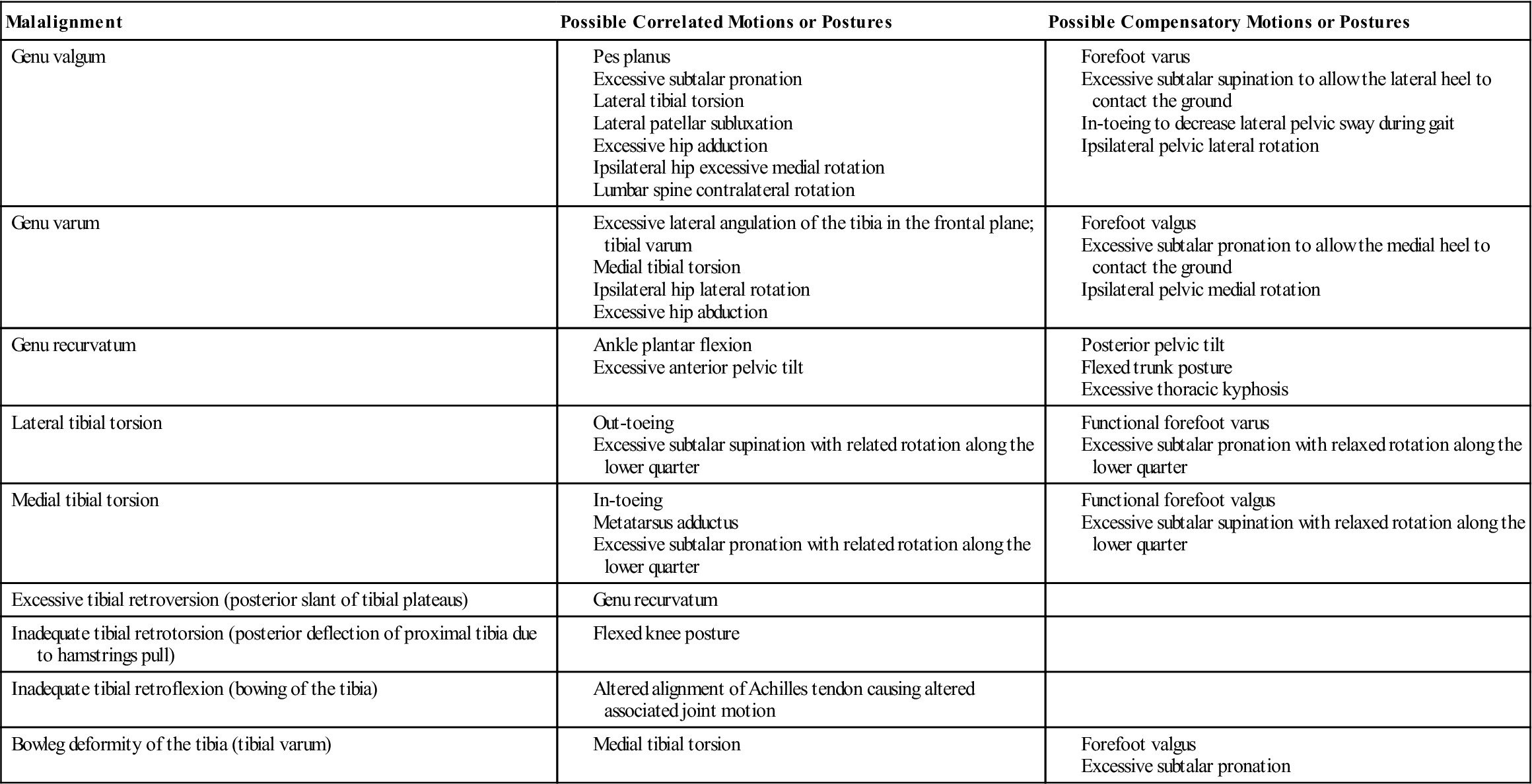
From Riegger-Krugh C, Keysor JJ: Skeletal malalignments of the lower quarter: correlated and compensatory motions and postures. J Orthop Sports Phys Ther 23:166–167, 1996.
To observe genu varum and genu valgum, the patient is positioned so that the patellae face forward and the medial aspects of the knees and medial malleoli of both limbs are as close together as possible. If the knees touch and the ankles do not, the patient has a genu valgum. A distance of 9 to 10 cm (3.5 to 4 inches) between the ankles is considered excessive. If two or more fingers (4 cm [1.6 inch]) fit between the knees when the ankles are together, the patient has a varus deformity or genu varum.35 On x-ray studies, the normal tibiofemoral shaft angle is approximately 6° (Figure 12-9).
Alignment is often different between males and females.36 Some of these misalignments, if excessive, can lead to patellofemoral symptoms or instability.37 These excessive differences are sometimes referred to as miserable malalignment syndrome and can include anterior pelvic tilt, increased hip anteversion, decreased tibiofemoral angle, genu recurvatum, navicular drop, and increased foot pronation (Figure 12-10).38
The patient is asked to extend the knees to see whether the movement can be performed and what effect it has on the knee. Both knees should extend equally. If not, something must be limiting the movement (swelling, loose body, or meniscus). Normally, a person does not stand with the knees fully extended. If, however, the patient has an excessive lordosis, the knees are often hyperextended to maintain the center of gravity. This change can lead to posterior knee pain.
Is there any apparent swelling or ecchymosis in or around the knees (see Figure 1-10)? If there is intracapsular swelling, or at least sufficient swelling, the knee assumes a position of 15° to 25° of flexion, which provides the synovial cavity with the maximum capacity to hold fluid. This position is also called the resting position of the knee. Is the swelling intracapsular or extracapsular? Intracapsular swelling is evident over the entire joint; extracapsular swelling tends to be more localized. An example of extracapsular swelling is shown in Figure 12-11, which illustrates prepatellar bursitis.

The examiner should ask the patient to contract the quadriceps muscles to see whether there is any visible wasting of the muscles, especially of the vastus medialis obliquus (VMO). The prominence of the vastus medialis results from the obliquity of the distal fibers, the inferior position of its insertion, and the thinness of the fascial covering compared with the other quadriceps muscles. Muscle defects (third-degree strain or rupture) should also be watched for when the patient contracts the muscles. Third-degree strains may be indicated by muscle “bunching,” abnormal mechanics (e.g., unilateral patella alta with patella tendon rupture), or a palpable defect.30
The position of the patella should be noted. When viewing the patellae, the examiner should note whether they face straight ahead, tilt outward (“grasshopper eyes” patellae), tilt inward (“squinting” patellae), or are rotated (“spin”) in or out39 (Figure 12-12). Rotation and tilt may be caused by tight structures that alter the position of the patella. These tight structures may include muscles (e.g., rectus femoris, iliotibial band, gastrocnemius) or fascia (e.g., lateral retinaculum). Normally, the patellae should face straight ahead with no lateral tilt or rotation. If these deviations are seen in the observation phase, they are considered static problems, and the examiner should test patellar movement passively and watch the patellae during active movements to see whether it is a dynamic problem as well.40 A squinting or rotated patella may indicate medial femoral or lateral tibial torsion (Figure 12-13). Patients with abnormal torsion are prone to patellofemoral instability.
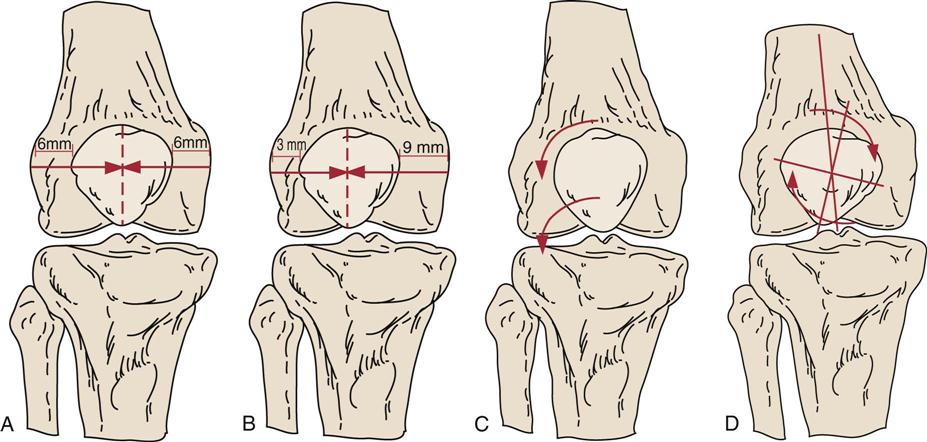
Ideally, the patella should be centered on the superior portion of the femoral articular surface at 20° flexion. A, Ideal alignment. B, Lateral glide of the patella. C, Lateral tilt of the patella. D, Lateral rotation (“spin”) of inferior pole of patella. (From McConnell J, Fulkerson J: The knee: patellofemoral and soft tissue injuries. In Zachazewski JE, et al, editors: Athletic injuries and rehabilitation, Philadelphia, 1996, WB Saunders, pp. 711–712.)
Any bruising or discoloration around the knee should also be noted, as well as any scars or signs indicating recent injury or surgery.
Lateral View, Standing
The examiner then views the patient from both sides for comparison. It should be noted whether genu recurvatum (hyperextended knee)41 is present and whether one or both patellae are higher (patella alta) or lower (patella baja or patella infera)42 than normal (Figure 12-14). For example, patella alta can increase the patellofemoral contact force during flexion, which may contribute to anterior knee pain.43 With an abnormally high patella, a “camel sign” may be present (Figure 12-15); because of the high patella (one “hump”), the infrapatellar fat pad (second hump) or an inflamed infrapatellar bursa (just anterior to the fat pad) becomes more prominent. This finding is especially noticeable in females. In this position, the examiner should also note (Figure 12-16) whether the inferior pole of the patella is tilted in (inferior tilt). Ideally, the plane of the patella and that of the femoral condyles should be the same. If the inferior pole tilts in, fat pad irritation may occur.44 Habitual genu recurvatum may make a patient prone to posterior cruciate tears because of the stretching of the posterior oblique ligament.30 If one knee (normal) hyperextends and the other one (injured) does not, it may indicate meniscus pathology that is limiting extension. Osteoarthritic lipping (Figure 12-17) or synovial hypertrophy (rheumatoid arthritis) may also limit movement.
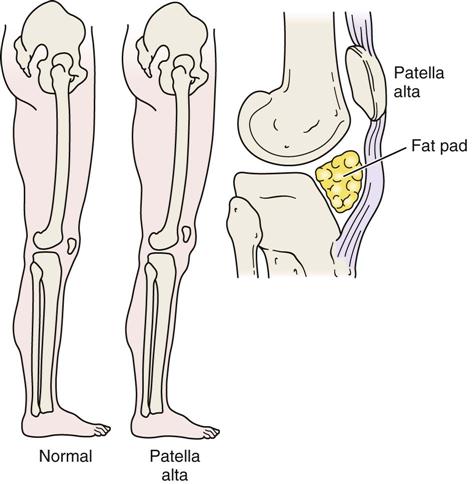
Double hump seen from side caused by high-riding patella and uncovered infrapatellar fat pad. (Modified from Hughston JC, Walsh WM, Puddu G: Patellar subluxation and dislocation, Philadelphia, 1984, WB Saunders, p. 22.)
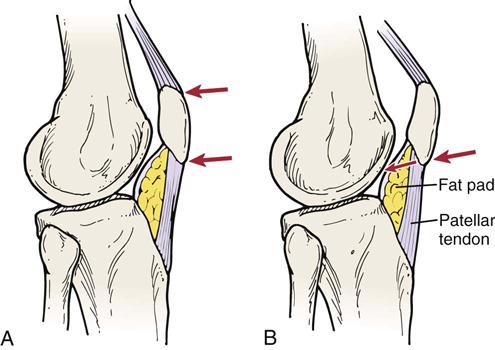
Ideally, the superior and inferior poles of the patella should be parallel in the sagittal plane of the knee, A. Commonly, in individuals with patellar malalignment, the inferior patellar pole pushes posteriorly into the infrapatellar fat pad, B. This may irritate the fat pad. (Redrawn from McConnell J, Fulkerson J: The knee: patellofemoral and soft tissue injuries. In Zachazewski JE, et al, editors: Athletic injuries and rehabilitation, Philadelphia, 1996, WB Saunders, p. 712.)
Posterior View, Standing
Next, the examiner views the patient from behind, looking for findings similar to those from the anterior aspect. In addition, the examiner looks for abnormal swellings, such as a popliteal (Baker’s) cyst, which is caused by herniation of synovial tissue through a weakening in the posterior capsule wall (Figure 12-18).
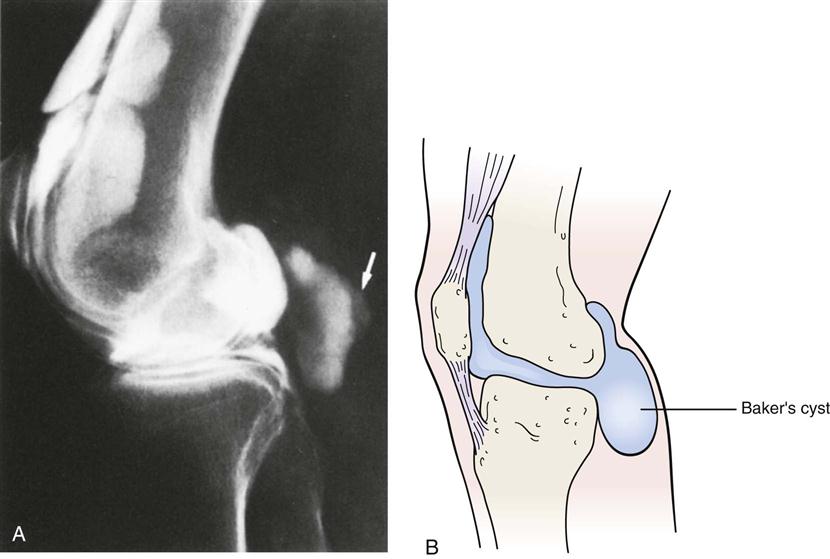
A, This 74-year-old man presented with the acute onset of calf pain and swelling without knee pain. The initial suspected diagnosis was popliteal thrombosis. A venogram was normal. The arthrogram revealed a collection of dye posterior to the joint space—a popliteal cyst (arrow). B, Schematic diagram of Baker’s cyst. (A, From Reilly BM: Practical strategies in outpatient medicine, Philadelphia, 1991, WB Saunders, p. 1179.)
Anterior and Lateral Views, Sitting
For the final part of the observation, the patient sits with the knee flexed to 90° and the feet either partially bearing weight (on a stool) or dangling free. The patient is observed from the front and from the side. In this position, the patella should face forward and should rest on the distal end of the femur. With patella alta, the patella becomes more aligned with the anterior surface of the femur (angled upward). If the patella is laterally displaced or laterally displaced with a patella alta, the patellae take on the appearance of “frog eyes” or “grasshopper eyes” (Figure 12-19), meaning that the patellae face upward and outward, away from each other. Patella alta sometimes causes a concavity proximal to the patella in thin patients.30 Any bony enlargements, such as those seen in Osgood-Schlatter disease (i.e., an enlarged tibial tubercle), should be noted (Figure 12-20), as should abnormal swelling. Swelling of the pes anserine bursa and a meniscal cyst (Figure 12-21) are best visualized in the seated position.30,45 Meniscal cysts may also present as isolated medial or lateral swelling.29
In the same position, any tibial torsion should be noted (Figure 12-22).44,46 If there is tibial torsion, it is medial torsion that is associated with genu varum; genu valgum is associated with lateral tibial torsion. Normally, the patella faces straight ahead while the foot faces slightly laterally (Fick angle). With medial tibial torsion, the feet point toward each other, resulting in a “pigeon-toed” foot deformity. These deformities can be exacerbated by habitual postures. The positions illustrated in Figures 12-23, 12-24, A, and 12-25 cause problems only if they are used habitually. Excessive tibial torsion can contribute to conditions such as chondromalacia patellae, patellofemoral instability, and fat pad entrapment. When standing, most people exhibit a lateral tibial torsion, the Fick angle (see Figure 13-13), which increases as the child grows. This angle is approximately 5° in babies and as much as 18° in adults. To test for tibial torsion, the examiner aligns the patient’s straight legs (knees extended) so that the patellae face straight ahead. The examiner then looks at the feet to determine their angle relative to the shaft of the tibia.
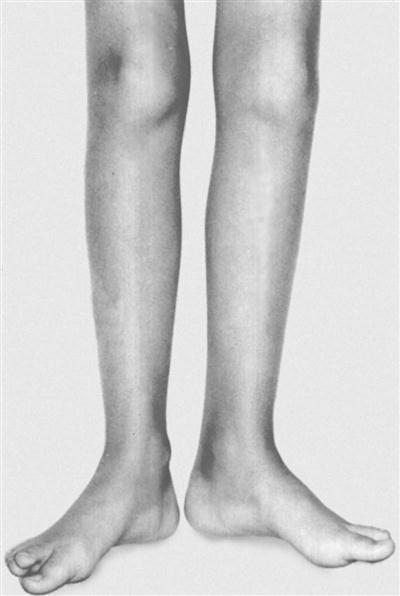
In stance, with the patellae facing straight forward, the feet point outward. (From Tachdjian MO: Pediatric orthopedics, Philadelphia, 1990, WB Saunders, p. 2816.)
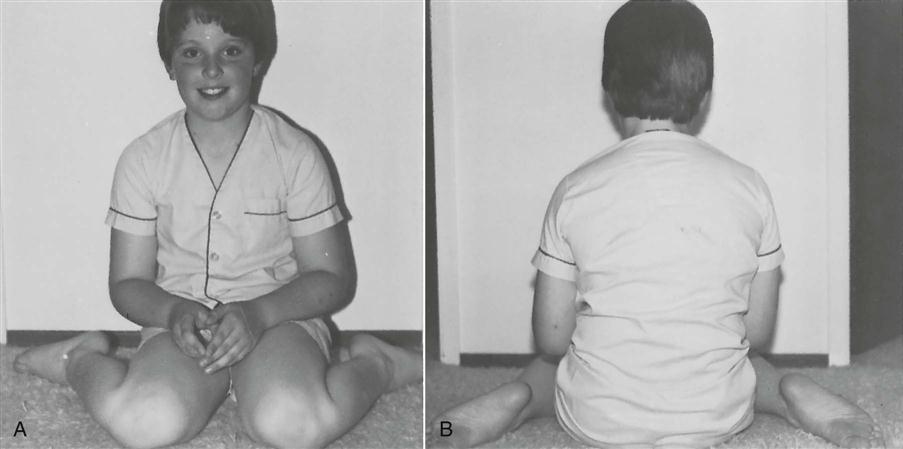
A, Anterior view. B, Posterior view.
A, Position to be avoided to prevent excessive medial tibial torsion. B, Tailor position maintains normal medial tibial torsion.

Femoral torsion, or anteversion (discussed in Chapter 11), can also affect the position of the patella relative to the femur and tibia.
Gait
The examiner should also observe the patient’s gait (see Chapter 14 ), noting any differences in stride length, walking speed, cadence, or linear and angular displacement. In addition, the examiner should watch for abnormal patellar movement, indicating possible patellar tracking problems, and abnormal motion of the tibia relative to the femur, indicating possible instability problems.
Movement at the pelvis, hip, and ankle should also be observed. For example, weak hip abductors (positive Trendelenburg sign) may lead to increased stress on the knee. If this is combined with medial tibial torsion, patellofemoral syndromes may result.30,47 Tight heel cords may result in gait with the knee flexed, which can put extra pressure on the patellofemoral joint. Similarly, pronation of the foot and lateral tibial torsion may lead to patellofemoral pathology or anteromedial joint pain.30 Tight hamstrings result in increased knee flexion, which can lead to the need for more ankle dorsiflexion. If no further dorsiflexion is possible, the foot pronates to compensate, thus increasing the dynamic Q-angle.48
Examination
Although the examination focuses primarily on the knee, the examiner must keep in mind that knee pathology may be the result of biomechanical (e.g., alignment, asymmetry) and pathological (e.g., hypomobility, hypermobility, muscle weakness, instability) issues in other joints in the kinetic chain, including the lumbar spine, pelvis, hips, ankles, and feet. Thus the examination, like the history and observation, may be extensive to rule out other kinetic chain contributors.49–54 For example, Dutton55 believed the gracilis and adductor longus and magnus play a significant role along with the iliotibial band in knee stability. Also, several muscles that are two joint muscles acting over the hip and knee (e.g., rectus femoris, hamstrings, sartorius, gracilis) and knee and ankle (gastrocnemius) should be tested for functional mobility, because their action at one joint can affect the other joint (Figure 12-26).
Active Movements
The examination is performed initially with the patient sitting and then with the patient in lying position. During the active movements, the examiner should observe 1) the excursion of the patella to ensure that it tracks freely and smoothly; 2) the range of motion (ROM) available; 3) whether pain occurs during the movement, and if so, where; and 4) what appears to be limiting the movement. The active movements may be done in the sitting or supine position, and, as always, the most painful movements should be done last (Figure 12-27).
Full knee flexion is 135° (0° being straight knee). As the patient moves the knee through flexion and extension, the examiner should watch the movement of the patella as it “tracks” along the femoral trochlea. The examiner should note whether the movement is smooth from beginning to end or whether there is a lag or abrupt jump of the patella as it attempts to center in the groove.56 The patella does not follow a straight path as the knee moves from extension to flexion. Normally, it follows a curved pattern moving medially in early flexion and then laterally (Figure 12-28).57 In the presence of pathological patellar tracking and patellar instability, an inverted “J” sign may be noted.58,59 During the initiation of flexion (e.g., going in to a squat), the laterally located patella moves suddenly medially to enter the trochlea. The key to the J sign is the sudden movement medially instead of the normal smooth movement pattern. As in the observation phase, the examiner should note whether dynamic movement causes lateral tilt, anteroposterior tilt, or rotation of the patella during movement.48,57
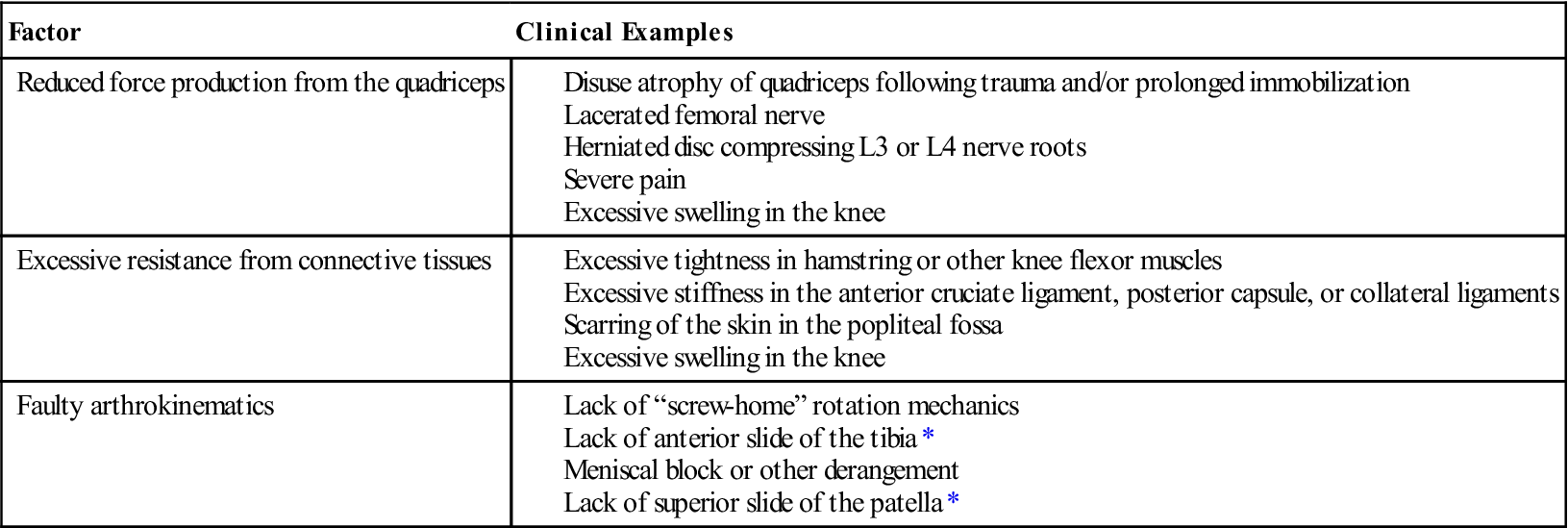
Active knee extension is approximately 0° but may be −15°, especially in women, who are more likely to have hyperextended knees (genu recurvatum). The knee extensor muscles develop the greatest force near 60°, and the knee flexor muscles develop their greatest force at 45° to 10°. To complete the last 15° of knee extension, a 60% increase in force of the quadriceps muscles is required. The examiner should also watch for evidence of quadriceps lag, which means the quadriceps muscles are not strong enough to fully extend the knee. The lag results from loss of mechanical advantage, muscle atrophy, decreasing power of the muscle as it shortens, adhesion formation, effusion, or reflex inhibition (Table 12-3). In non–weight-bearing, active medial rotation of the tibia on the femur should be 20° to 30°, whereas active lateral rotation should be 30° to 40° at 90° flexion in non–weight-bearing (Figure 12-29, A). In weight bearing (closed kinetic chain), the femur rotates on the tibia (Figure 12-29, B).
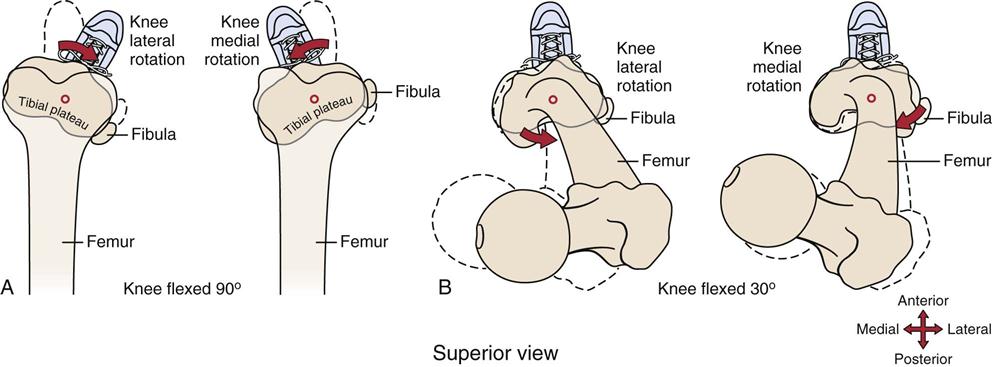
TABLE 12-3
Selected Factors That Contribute to the Inability to Completely Extend the Knee
| Factor | Clinical Examples |
| Reduced force production from the quadriceps | |
| Excessive resistance from connective tissues | |
| Faulty arthrokinematics |
*Assume tibial-on-femoral knee extension.
From Neumann DA: Kinesiology of the musculoskeletal system—foundations for physical rehabilitation, St Louis, 2002, Mosby, p. 460.
A, Tibial-on-femoral rotation at 90° flexion (open kinetic chain). B, Femoral-on-tibial rotation (closed kinetic chain). (Redrawn from Neumann DA: Kinesiology of the musculoskeletal system—foundations for physical rehabilitation, St Louis, 2002, Mosby, p. 445.)
If, during the history, the patient has complained that repetitive or combined movements or sustained postures have resulted in symptoms, these movements should also be tested.
Passive Movements
If, on active movements, the ROM is full, overpressure may gently be applied to test the end feel of the various movements in the tibiofemoral joint. This action would preclude the need to do passive movements to the tibiofemoral joint. However, the examiner must do movements of the patella passively (Figure 12-30).
At the tibiofemoral joint, the end feel of flexion is tissue approximation; the end feel of extension and of medial and lateral rotation of the tibia on the femur is tissue stretch. During passive movement, the examiner is also looking for a capsular pattern of the tibiofemoral joint.60 This pattern is more limitation of flexion than of extension. Passive medial rotation of the tibia on the femur should be approximately 30° when the knee is flexed to 90°. Passive lateral rotation of the tibia on the femur at 90° of knee flexion should be 40°.
Although full knee extension is usually preferable for everyday activities (e.g., standing, walking), full flexion (135°) is often not necessary except where people kneel back on their heels. However, approximately 117° of flexion is necessary for activities, such as squatting to tie a shoelace or to pull on a sock. Sitting in a chair requires approximately 90° of flexion, and climbing stairs (average height) requires approximately 80° of flexion.
Lancaster, et al.61 advocated doing a motion palpation test when assessing the knee for articular damage when the damage is severe. The patient sits on the edge of the examining table with the knees flexed to about 90°. The examiner passively moves the patient’s knee between 100° and 0° flexion three to four times at about 30°/sec. While doing this movement with one hand, the examiner applies about 2.3 kg (5 lbs) compression over the patellofemoral joint while the index finger of the same hand palpates immediately distal to the inferior pole of the patella (Figure 12-31). The examiner is palpating for joint crepitus and location, and severity of any discomfort that would indicate positive signs or possible articular damage.

Passive medial and lateral movement of the patella is also carried out to determine its mobility and to compare it with the unaffected side. Normally, the patella should move up to half its width medially and laterally in extension (Figure 12-32). When the patella is pushed medially or laterally, the examiner should note whether it stays parallel to the femoral condyles or whether it tilts or rotates.40 For example, if pushed medially when the medial structures are tight, the lateral border of the patella tilts up. Likewise, tight lateral structures cause the medial border to tilt up. If the lateral structures are tight superiorly, the inferior pole of the patella medially rotates. These are examples of dynamic tilt and rotation problems of the patella. The side-to-side passive motion of the patella should also be tested in 45° of flexion, which is a more functional position and gives a better indication of functional instability of the patella.62 The end feel of these movements is tissue stretch. Lateral displacement must be performed with care, especially in patients who have experienced a dislocated patella.
The examiner must also ensure full and normal flexibility of the quadriceps, hamstring, iliotibial band, and abductor and adductor muscles of the thigh, as well as the gastrocnemius muscles (Figure 12-33). Tightness of any of these structures or of the lateral retinaculum can alter gait and postural mechanics, which may lead to pathology. For example, tight hamstrings can contribute to patellofemoral pathology because of increased knee flexion at heel strike and during stance phase.48 Limitation of hip rotation in extension can lead to patellofemoral pathology as well.30 If the rectus femoris is tight, full excursion of the patella in the trochlea is not possible, especially if the hip is extended. A tight iliotibial band can lead to lateral tracking of the patella.48,63 Tests for the hamstring, abductor, adductor, and rectus femoris muscles have been described in Chapter 11. A functional test for the quadriceps (described under the “Special Tests” section in this chapter) is also a passive movement test (heel to buttock) for the femoral nerve. To test the gastrocnemius muscle, the examiner extends the patient’s knee and, while holding it straight, dorsiflexes the patient’s ankle. The examiner should be able to reach at least 90° (plantigrade), although 10° to 15° of dorsiflexion is more common.
Resisted Isometric Movements
For a proper test of the muscles, resisted isometric movements must be performed. In some cases (e.g., patellofemoral pain syndrome [PFPS]), hip strength should also be tested as hip abductors and lateral rotators have been found to be weak in PFPS patients.64 The patient should be tested in the supine position (Figure 12-34).
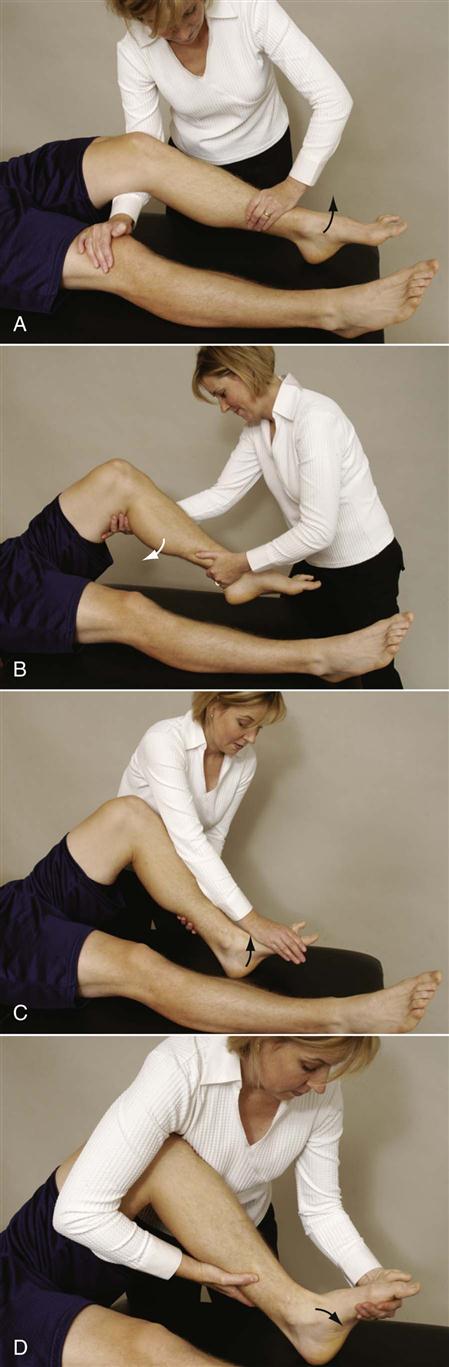
A, Knee extension. B, Knee flexion. C, Ankle dorsiflexion. D, Ankle plantar flexion.
Ideally, these resisted isometric movements are performed with the joint in its resting position. Segal and Jacob65 suggest testing the quadriceps muscle at 0°, 30°, 60°, and 90° while observing any abnormal tibial movement (e.g., ligament instability) or excessive pain from patellar compression (e.g., patellofemoral syndrome). Figure 12-35 shows the quadriceps complex components and their angle of pull. Table 12-4 lists the muscles acting at the knee.
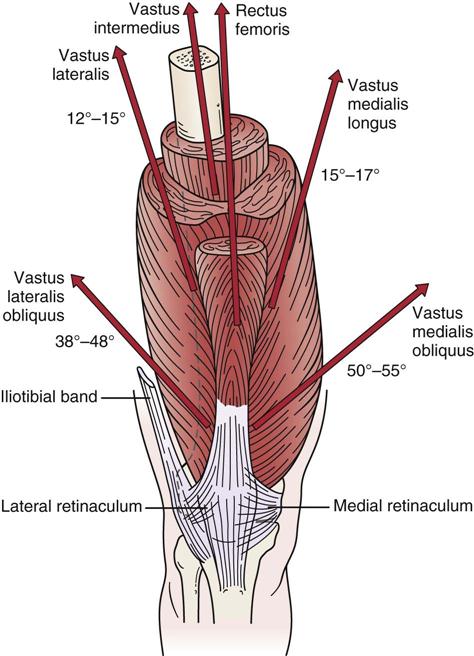
Note the angle of insertion of the various components of the complex. The orientation of the muscle fibers dictates the line of action and pull on the patella. (Redrawn from McConnell J, Fulkerson J: The knee: patellofemoral and soft tissue injuries. In Zachazewski JE, et al, editors: Athletic injuries and rehabilitation, Philadelphia, 1996, WB Saunders, p. 697.)
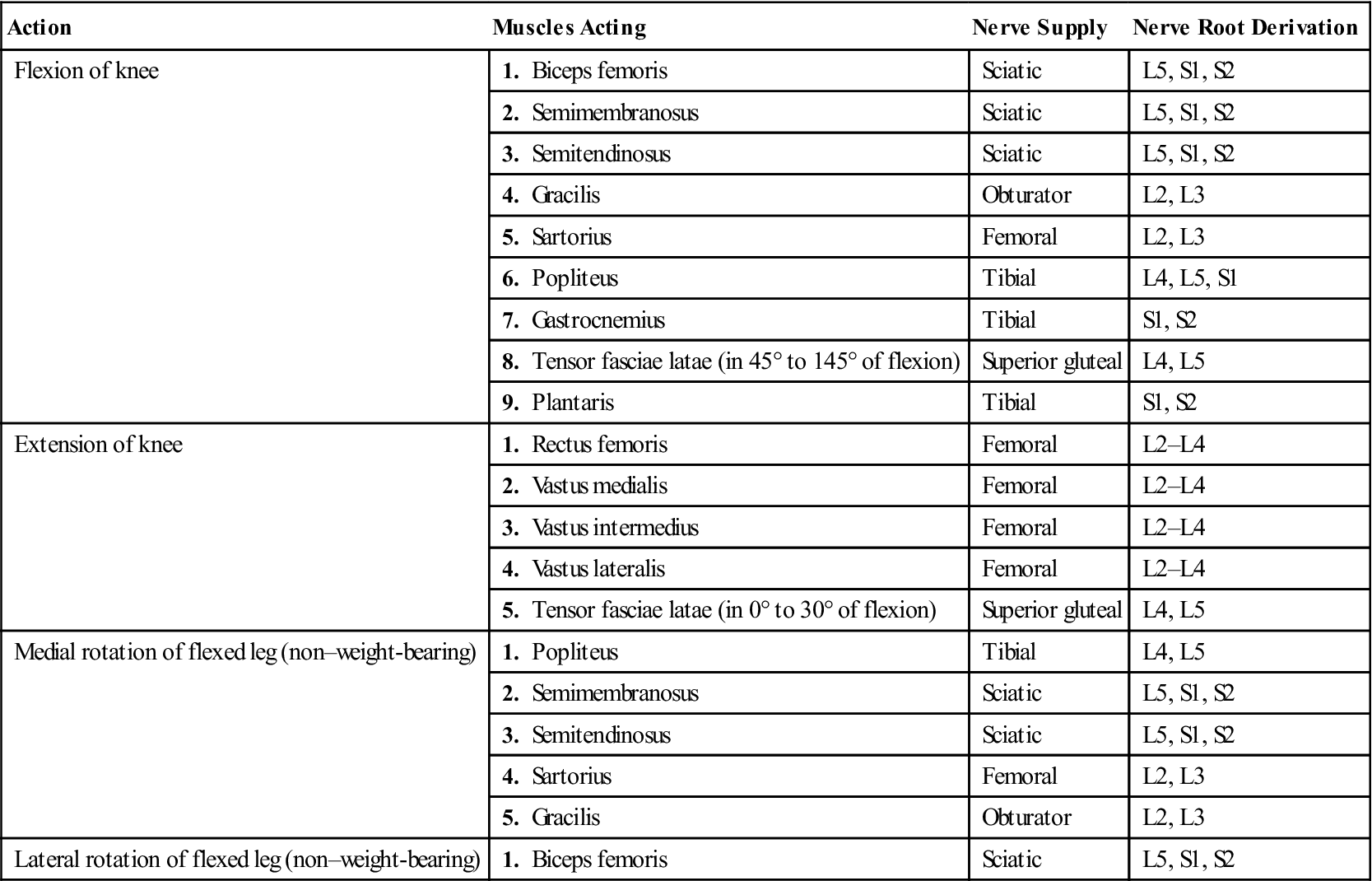
TABLE 12-4
Muscles of the Knee: Their Actions, Nerve Supply, and Nerve Root Derivation
| Action | Muscles Acting | Nerve Supply | Nerve Root Derivation |
| Flexion of knee | 1. Biceps femoris | Sciatic | L5, S1, S2 |
| 2. Semimembranosus | Sciatic | L5, S1, S2 | |
| 3. Semitendinosus | Sciatic | L5, S1, S2 | |
| 4. Gracilis | Obturator | L2, L3 | |
| 5. Sartorius | Femoral | L2, L3 | |
| 6. Popliteus | Tibial | L4, L5, S1 | |
| 7. Gastrocnemius | Tibial | S1, S2 | |
| 8. Tensor fasciae latae (in 45° to 145° of flexion) | Superior gluteal | L4, L5 | |
| 9. Plantaris | Tibial | S1, S2 | |
| Extension of knee | 1. Rectus femoris | Femoral | L2–L4 |
| 2. Vastus medialis | Femoral | L2–L4 | |
| 3. Vastus intermedius | Femoral | L2–L4 | |
| 4. Vastus lateralis | Femoral | L2–L4 | |
| 5. Tensor fasciae latae (in 0° to 30° of flexion) | Superior gluteal | L4, L5 | |
| Medial rotation of flexed leg (non–weight-bearing) | 1. Popliteus | Tibial | L4, L5 |
| 2. Semimembranosus | Sciatic | L5, S1, S2 | |
| 3. Semitendinosus | Sciatic | L5, S1, S2 | |
| 4. Sartorius | Femoral | L2, L3 | |
| 5. Gracilis | Obturator | L2, L3 | |
| Lateral rotation of flexed leg (non–weight-bearing) | 1. Biceps femoris | Sciatic | L5, S1, S2 |
Although these movements are tested with the patient in the supine-lying position, the hamstrings are often tested with the patient prone. If the knee is flexed to 90° and the heel is turned out, the greatest stretch is placed on the lateral hamstring muscle (biceps femoris). If the heel is turned in, the greatest stretch is placed on the medial hamstring (semimembranosus and semitendinosus) muscles.
Ankle movements are tested because the gastrocnemius muscle crosses the posterior knee and both plantar and dorsiflexion movements cause movement of the fibula. Dorsiflexion causes the fibula to move up and increases the stress being applied to the ligaments supporting the superior tibiofibular joint. Plantar flexion decreases the stress on these ligaments and also brings the gastrocnemius into play, supporting the posterior knee and assisting knee flexion.
If the history has indicated concentric, eccentric, or econcentric movements have caused symptoms, these types of contractions should be tested as well, but only after isometric testing has been performed.
Kannus and colleagues66 developed a scoring scale for measuring isokinetic and isometric strength (Figure 12-36). The scale can be used to show improvement in strength over time. When using isokinetic values, different test parameters may be used. It is important to realize, however, that most knee isokinetic tests are not done with the knee in a functional position.
Depending on the speed, the hamstring/quadriceps ratio is normally between 50% and 60%.67 As the speed of isokinetic testing increases, however, the ratio approaches 1 : 1, or 100%.68,69
Functional Assessment
Instabilities produced on the examining table are easily produced functionally, especially in athletes who participate in activities, such as vigorous cutting and jumping or rapid deceleration, which produce high physiological joint loads. Functional tests and numerous numerical knee rating systems have been developed for the knee, many of them for specific populations (e.g., athletes) or to assess outcomes after surgery or for specific conditions. The examiner must pick the appropriate test or scale, realizing that each has advantages and disadvantages.70–73
If the active, passive, and resisted isometric movements are performed with little difficulty, the examiner may put the patient through a series of functional tests to see whether these sequential activities produce pain or other symptoms. These tests may be scored by the time taken to do the test or by the distance or height attained when doing the test. If the results are so measured, three measurements should be taken and averaged. In some cases, the results of different tests may be combined. Fonseca and coworkers74 found that the time ratio of figure-eight running to straight running was one of the most effective ways of differentiating patients with anterior cruciate ligament deficiencies from normal patients (Figure 12-37). Some of these tests may involve walking (e.g., Timed “Up and Go” test [TUG test], sit-to-stand test). These walking tests may be used when any lower limb joint is affected but are primarily designed for elderly people.75 Boonstra et al.75 felt the TUG test could be used as a global functional test following total knee arthroplasty while the sit-to-stand was a more biomechanical function test.
These functional activities, which are provided as examples, must be geared to the individual patient, and in some cases, to specific pathology.76 Paxton et al.77 recommended doing knee-specific, activity-specific, and general health questionnaires to provide a more accurate assessment of outcomes. Squatting reveals limitations of flexion and may cause impingement with meniscal lesions. Duck waddle, if attempted, can demonstrate increased symptoms in meniscal and ligamentous lesions. Older patients should not be expected to accomplish the last five or six (see earlier) movements unless they have been doing these or similar activities in the recent past. Daniel and coworkers78 outlined different functional and intensity levels that are useful especially for getting an indication of functional activities from a patient’s perspective (Table 12-5). Functional strength tests for sedentary individuals are shown in Table 12-6.
TABLE 12-5
| Functional Levels | |
| Level I: | Activities of daily living |
| Level II: | Straight running; sports that do not involve lower-limb agility activities; occupations involving heavy lifting |
| Level III: | Activities that require lower-limb agility but not involving jumping, hard cutting, or pivoting |
| Level IV: | Activities involving jumping, hard cutting, or pivoting |
| Intensity | |
| W: | Work-related or occupational |
| LR: | Light recreational |
| VR: | Vigorous recreational |
| C: | Competitive |
| Exposure | |
| Number of hours per year of participation at any given functional level and intensity | |
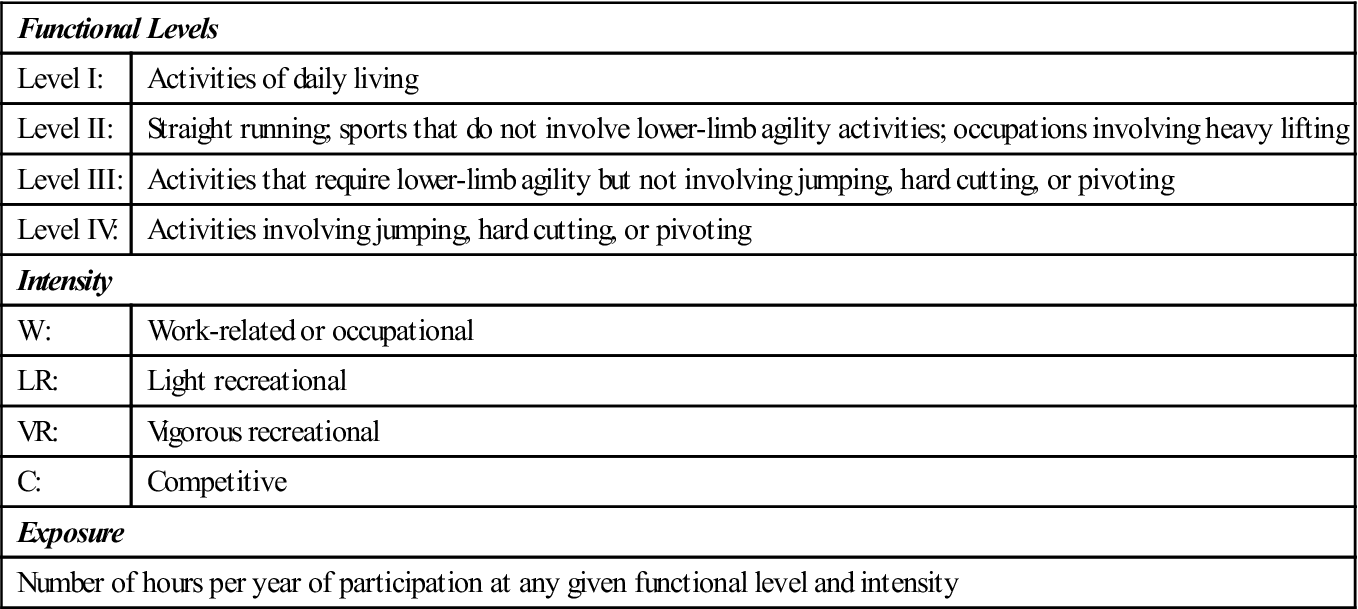
From Daniel D, et al, editors: Knee ligaments: structure, injury and repair, New York, 1990, Raven Press, p. 522.
TABLE 12-6
Functional Testing of the Knee
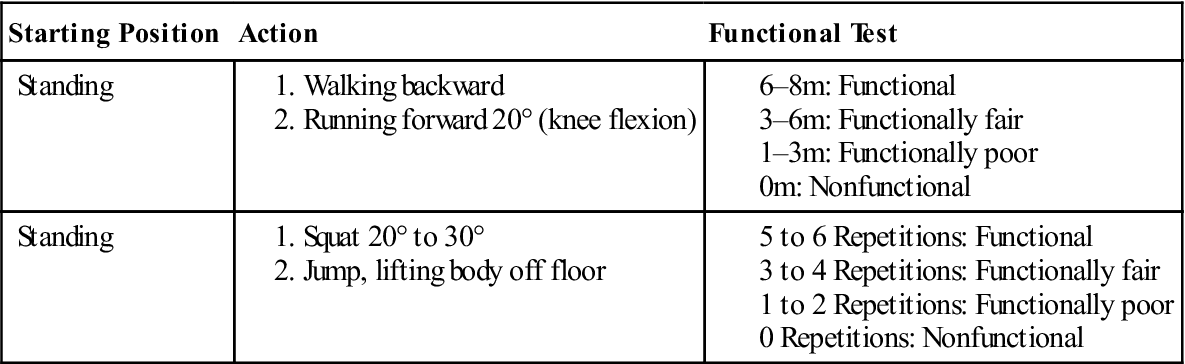
Data from Palmar ML, Epler M: Clinical assessment procedures in physical therapy, Philadelphia, 1990, JB Lippincott, pp. 275–276.
Strobel and Stedtfeld79 put forward the one-leg hop test. The patient stands and does a “long jump” hop on one leg while landing on the same leg. This is a single-leg hop for distance (Figure 12-38, A).80–83 Noyes and associates80 considered symmetry of less than 85% between the legs to be abnormal. The test is repeated three times alternately with each leg. If instability is evident, the distance for the affected leg is less than that for the normal leg. Any functional deficit between the two limbs has been called the limb symmetry index (LSI).84 Juris et al.85 advocated doing a maximal controlled leap in addition to the one-leg hop test. For this test, which is said to test force absorption, the patient stands on one foot and “leaps forward” to land on the opposite foot. Patients should be instructed to maintain the flexed hip/knee position during takeoff and extend the leg for landing. Patients must “stick” on landing with no movement of the landing foot and must be upright with hands on hips within 1 second. The distance is measured and the test repeated with the opposite start leg.
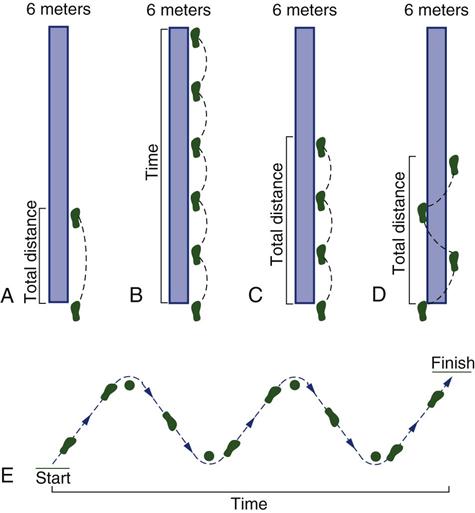
A, Single hop for distance. B, Timed hop. C, Triple hop for distance. D, Crossover hop for distance. E, 30-m agility hop test.
Since the advent of the single-leg hop, modifications have been developed.86 Each test is usually repeated three times, and the average of the three scores is used as the measured value. These modifications include the following:
1. Single-leg hop for time: With this test, the patient is assessed for the time taken to hop 6 m (20 ft) on one leg (Figure 12-38, B). The good leg is tested first, followed by the injured leg.80,81,87
2. Triple hop: With this test, the patient is asked to hop as far as possible, taking three hops. The distance for the good leg is compared with that for the injured leg (Figure 12-38, C).80,81,87
3. Crossover hop: A straight line is marked on the floor. The patient is asked to take three consecutive hops on one foot, crossing over the straight line each time (Figure 12-38, D). The good limb is tested, followed by the injured limb, and the average distances attained with each leg are compared.80 Risberg and Ekeland88 modified this test and called it the side jump test. For this test, two 6-meter parallel lines are placed 30 cm (12 inches) apart on the floor. Outside one line, ten marks are made at 60-cm (24-inch) intervals. Outside the other line, marks are made at 60-cm (24-inch) intervals but starting at 30 cm (12 inches) so that the marks are staggered from one side to the other. The patient is asked to hop from marker to marker on each line. The good leg is timed, followed by the injured leg.
4. Agility hop: This hop test requires a space of 30 m (100 ft). Cones are placed 6 m (20 ft) apart (see Figure 12-38, E). The patient is then timed as he or she hops through the cones. The good limb is tested, followed by the injured limb, and the average times attained with each leg are compared.87
5. Stairs hop test (stairs hopple test)88: The patient is timed as he or she hops up and down several steps (20 to 25 steps recommended), first on the good leg and then on the injured leg. Hopper et al.84 recommended a different stair hop test. For this test, patients are asked to hop up and then down a three-step platform, then turn about a marker fixed 1 meter from the platform, and then hop back up and down the step (Figure 12-39).
These functional tests are for active persons and can be quite demanding; however, they have been shown to have high test-retest reliability.84 Losee89 mentioned several additional tests. For example, in the deceleration test, the patient is asked to run at full speed and to stop suddenly on command.28 The test is positive for rotary instability if the patient stops without using the quadriceps or decelerates in a crouched position (more than 30° flexion of the knee). The effect of the test can be accentuated by having the patient turn away from the affected leg just as he or she is about to stop.90 As the patient does the test, the examiner should watch to ensure that the patient uses the affected leg to help stop. With instability problems, the patient uses only the good leg to stop, “hopping through” with the injured leg.
For the “disco test,” the patient stands on one leg with the knee flexed 10° to 20°. The patient is asked to rotate or twist left and right while holding the flexed position (Figure 12-40).28 Apprehension during the test or refusal to do the test is a positive sign for rotary instability. If pain is felt on the joint line, it may indicate meniscus pathology, in which case it is called Merke’s sign.79 Pain on medial rotation along the joint line implies medial meniscus pathology, and pain on lateral rotation implies lateral meniscus pathology.

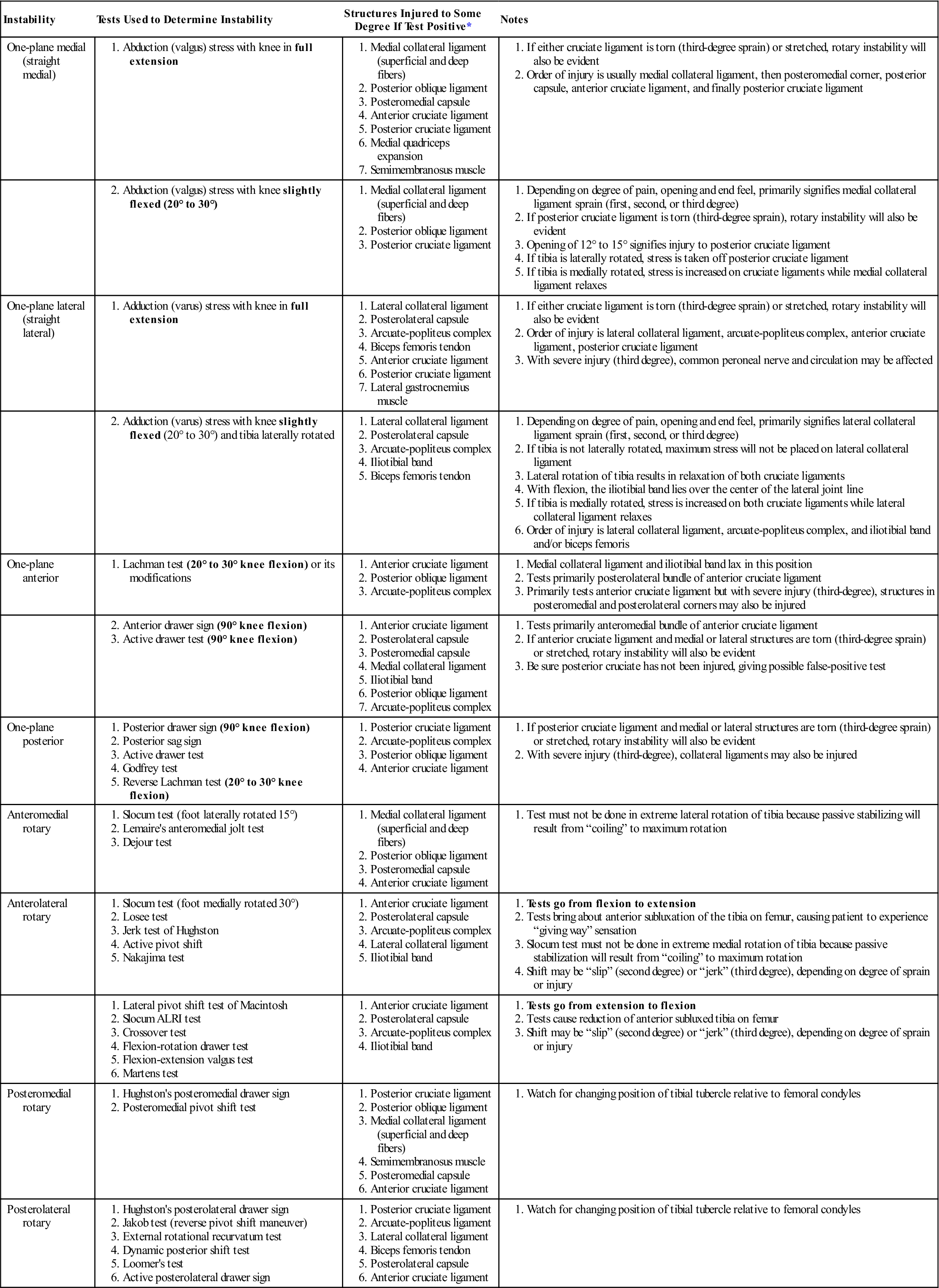
Flexion, compression, and rotation may lead to shift of femur on tibia, causing rotary instability.
Larson91 advocated the leaning hop test. For this test, the patient hops up and down on one leg while abducting the opposite leg. A positive test is apprehension during the test or refusal to do the test and is a positive sign for rotary instability.
Numerical rating systems are commonly done to determine the state of the knee. Most of these measures combine clinical (e.g., ROM) and functional (e.g., stair climbing) measures. Many of these scoring systems have not been tested on normal subjects and show possible interviewer bias, nor are the values given to each measure explained. In addition, there may be male and female differences.92,93
Noyes and colleagues94–97 developed the Cincinnati Knee Rating System (Figure 12-41), which deals with pain, swelling, stability, and activity level and is a good functional rating system for active persons. Irrgang and associates98 use two scales, an Activities of Daily Living Scale99 and a Sports Activity Scale (Figures 12-42 and 12-43), to detect clinically significant changes over time. The Knee Society100 also has a rating scale (Figure 12-44). The Knee Society advocates keeping knee rating and functional assessment separate. This knee-rating scale deals first with pain, ROM, and stability, giving positive points up to 100 and grouping deductions that can take away from the overall value. Function is dealt with separately on the scale.
Lysholm and Gillquist101 developed a frequently used scale primarily designed to score clinical instability that may also be used for chondral lesions of the knee (Table 12-7).102–106 The International Knee Documentation Committee has also developed a number of assessment forms, three of which are included here (Figures 12-45 to 12-47).97,107–112 The Tegner Activity Scale102,106,113 (Figure 12-48) is useful in determining the patient’s current level of activity relative to his or her previous level and can also be used as a guide for rehabilitation and the level of activity the patient hopes to achieve. Table 12-8 and the Kajula Score Questionnaire (Figure 12-49) show examples of a patellofemoral joint evaluation scale that can be used to assess functional levels in patients with patellofemoral syndrome after surgery or nonsurgery.114,115 Similar scales used to measure patellofemoral dysfunction also exist.116–119 Other scales, such as the Western Ontario and McMaster University Osteoarthritis Index (WOMAC), Knee Injury and Osteoarthritis Outcome Score (KOOS),103,112,120 and Lequesne Index, have been developed to determine the outcome of arthroplasties in osteoarthritis (see Chapter 11).121–131 Each of these knee-rating scales is slightly different. The scale that works best for the examiner and the examiner’s clientele should be used. Other knee-rating scales are also available.101,132–137
TABLE 12-7
| Points | |
| Limp (5 points) | |
| None | 5 |
| Slight or periodic | 3 |
| Severe and constant | 0 |
| Support (5 points) | |
| Full support | 5 |
| Stick or crutch | 3 |
| Weight bearing impossible | 0 |
| Stair climbing (10 points) | |
| No problems | 10 |
| Slightly impaired | 6 |
| One step at a time | 2 |
| Unable | 0 |
| Squatting (5 points) | |
| No problems | 5 |
| Slightly impaired | 4 |
| Not past 90° | 2 |
| Unable | 0 |
| Walking running and jumping (70 points) | |
| Instability | |
| Never giving way | 30 |
| Rarely during athletic or other severe exertion | 25 |
| Frequently during athletic or other severe exertion (or unable to participate) | 20 |
| Occasionally in daily activities | 10 |
| Often in daily activities | 5 |
| Every step | 0 |
| Pain | |
| None | 30 |
| Inconstant and slight during severe exertion | 25 |
| Marked on giving way | 20 |
| Marked during severe exertion | 15 |
| Marked on or after walking more than 2 km | 10 |
| Marked on or after walking less than 2 km | 5 |
| Constant and severe | 0 |
| Swelling | |
| None | 10 |
| With giving way | 7 |
| On severe exertion | 5 |
| On ordinary exertion | 2 |
| Constant | 0 |
| Atrophy of thigh (5 points) | |
| None | 5 |
| 1 to 2 cm | 3 |
| More than 2 cm | 0 |
| Total Score | 100 |
Modified from Lysholm, J, Gillquist J: Evaluation of knee ligament surgery results with special emphasis on use of a scoring scale. Am J Sports Med 10:150–154, 1982.
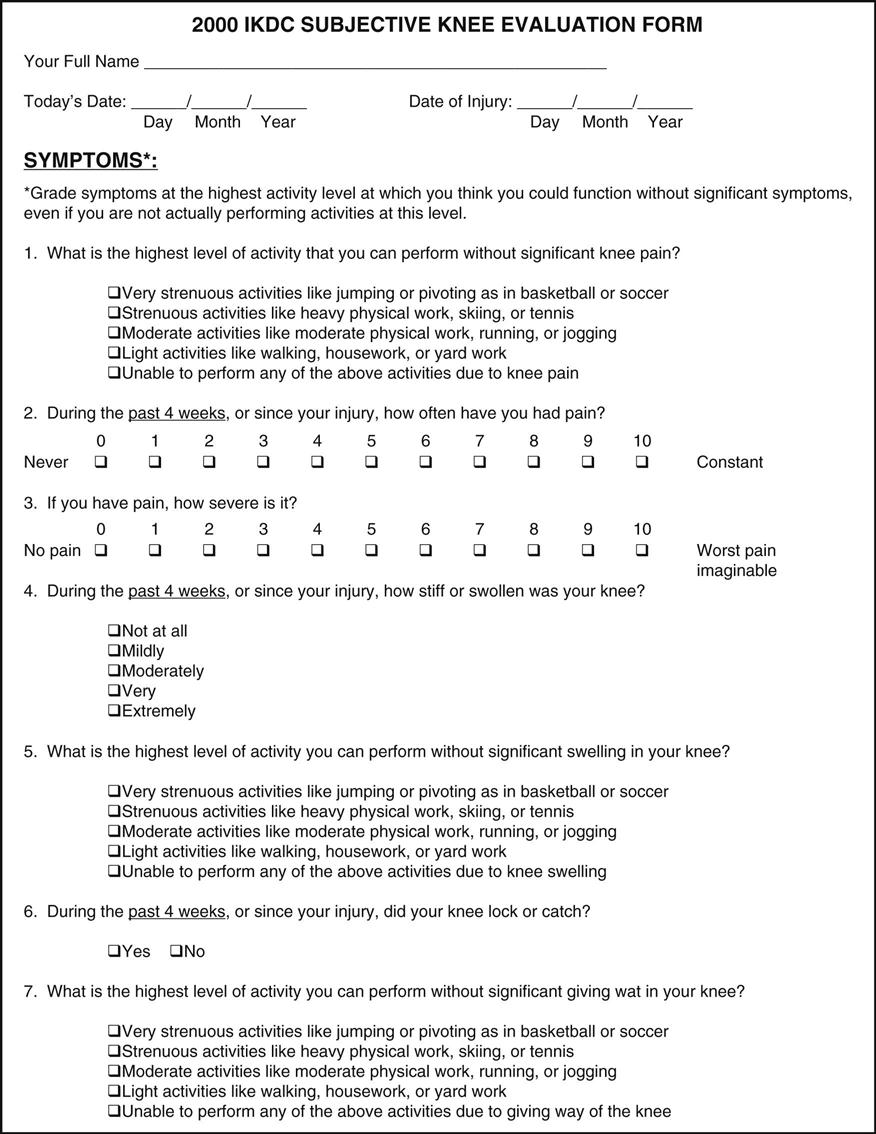
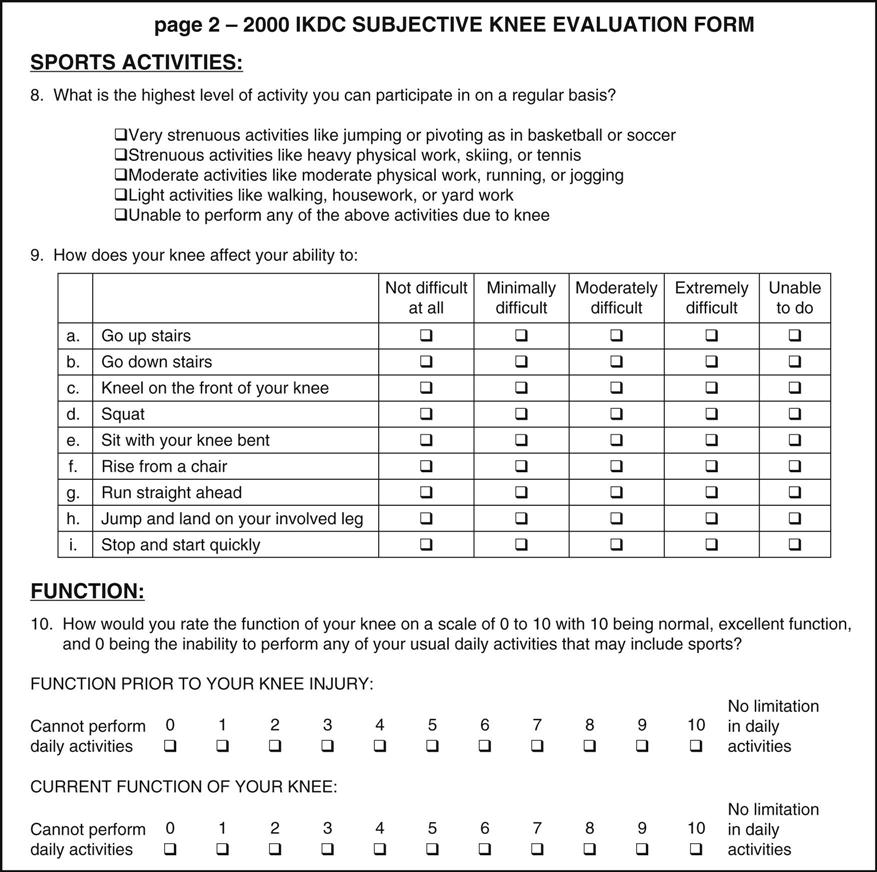
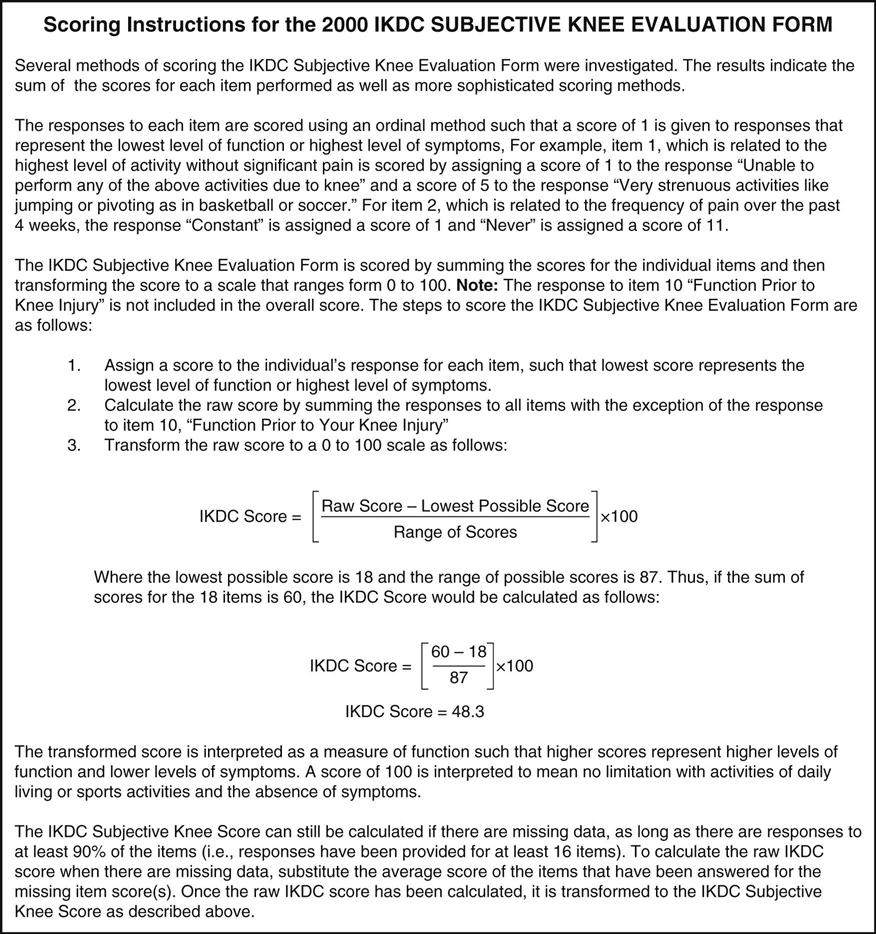
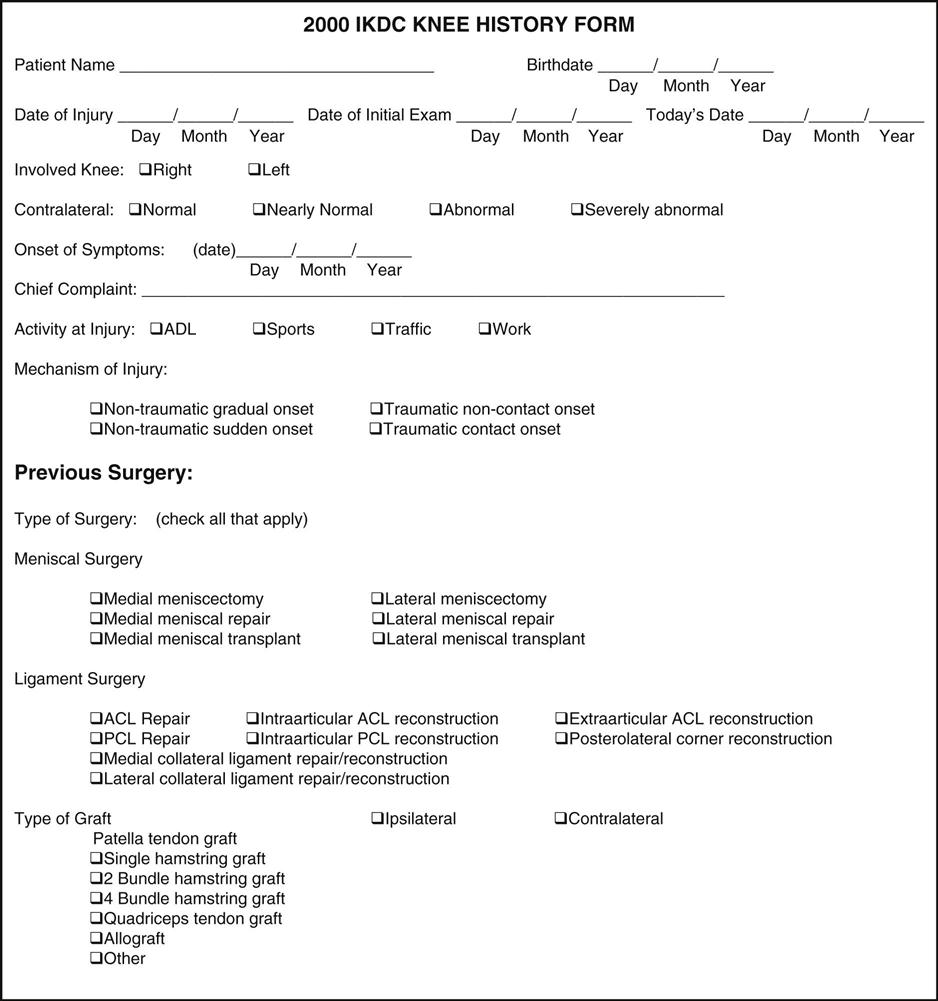
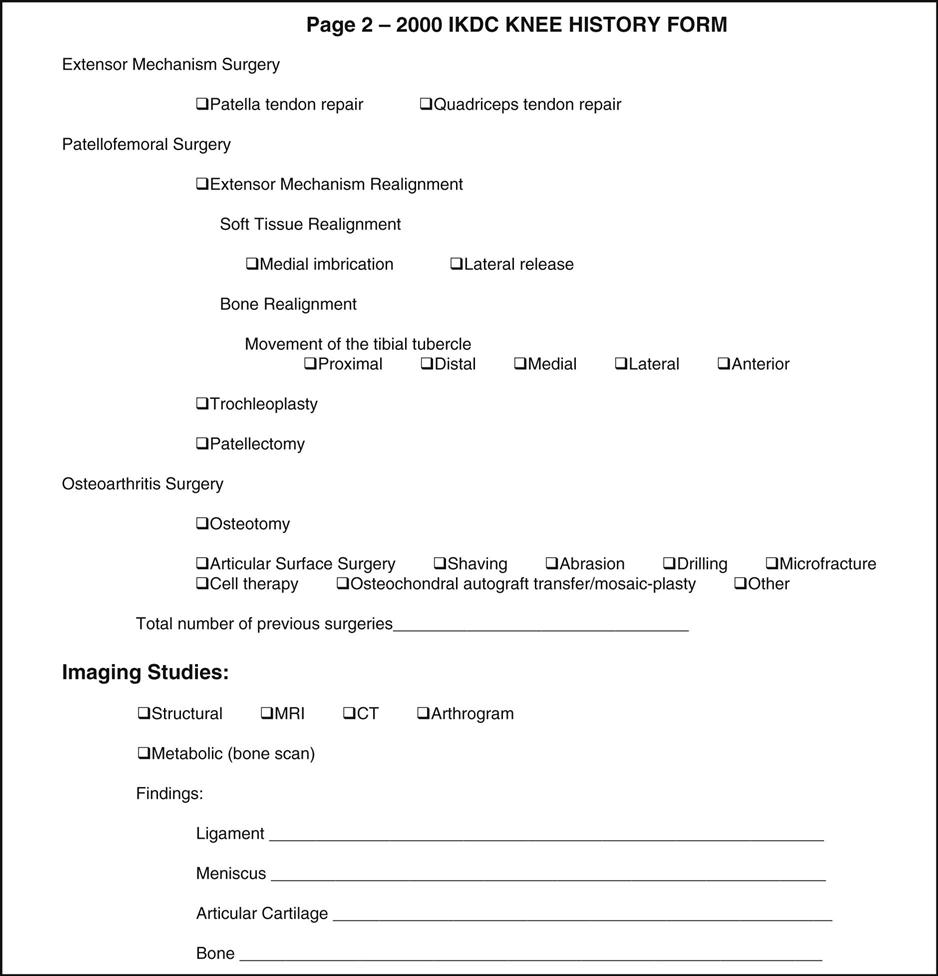
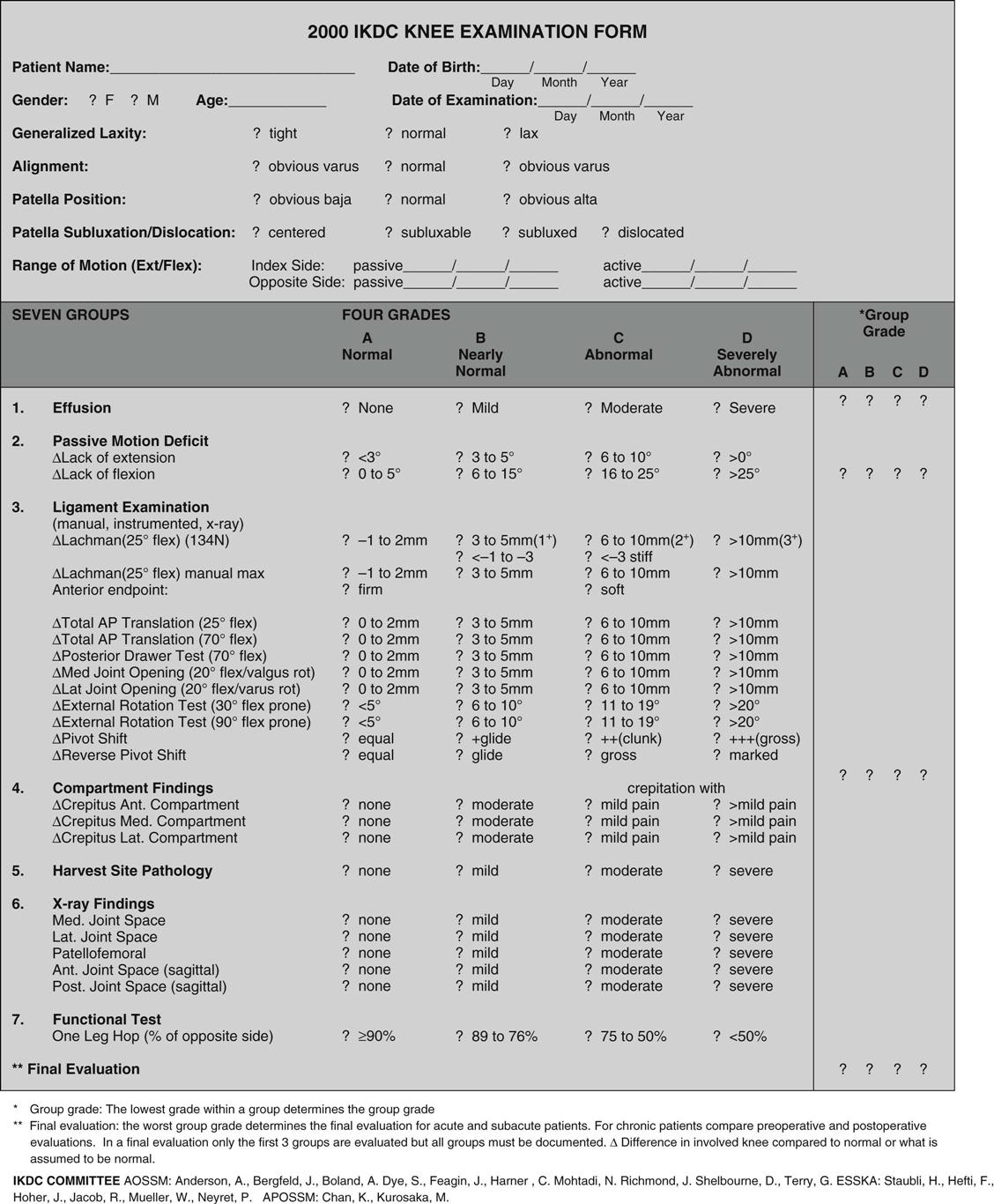
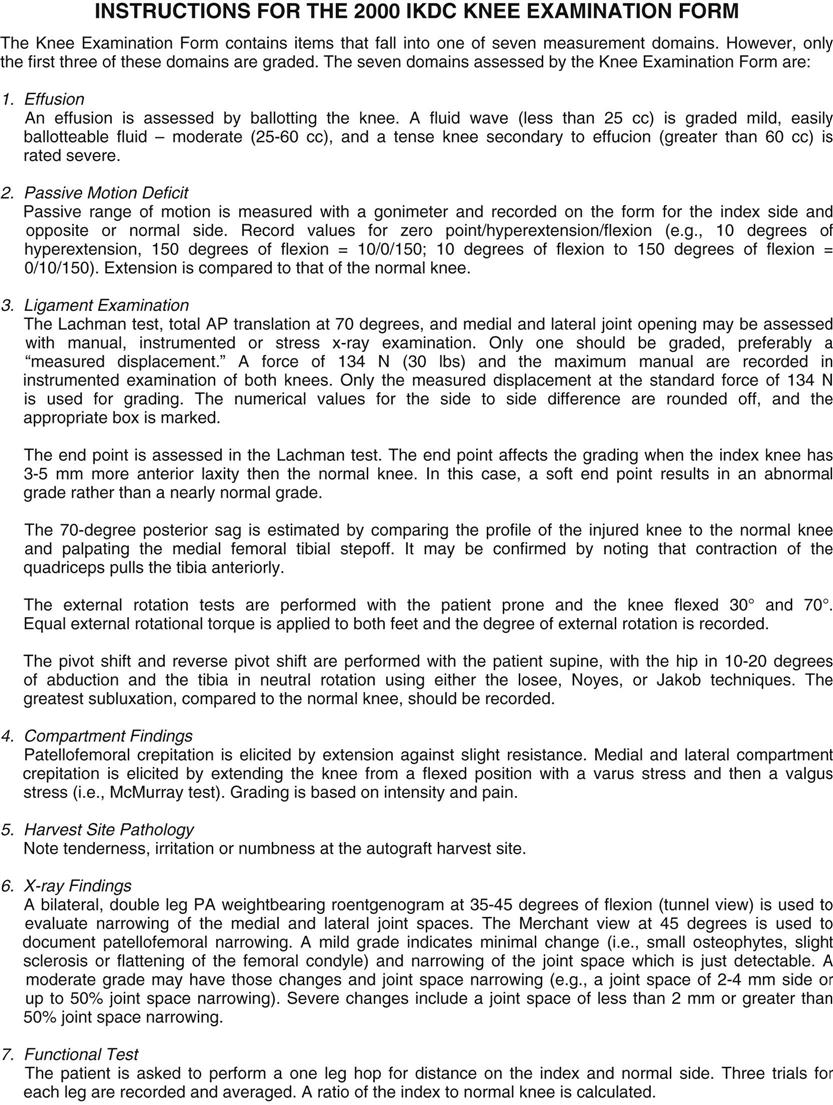
TABLE 12-8
Patellofemoral Joint Evaluation Scale*
| Points | |
| Limp | |
| None | 5 |
| Slight or episodie | 3 |
| Severe | 0 |
| Assistive devices | |
| None | 5 |
| Cane or brace | 3 |
| Unable to bear weight | 0 |
| Stair climbing | |
| No problem | 20 |
| Slight impairment | 25 |
| Very slowly | 10 |
| One step at a time, always same leg first | 5 |
| Unable | 0 |
| Crepitation | |
| None | 5 |
| Annoying | 3 |
| Limits activities | 2 |
| Severe | 0 |
| Inability, “Giving Way” | |
| Never | 20 |
| Occasionally with vigorous activities | 10 |
| Frequently with vigorous activities | 8 |
| Occasionally with daily activities | 5 |
| Frequently with daily activities | 2 |
| Every day | 0 |
| Swelling | |
| None | 10 |
| After vigorous activities only | 5 |
| After walking or mild activities | 2 |
| Constant | 0 |
| Pain | |
| None | 35 |
| Occasionally with vigorous activities | 30 |
| Marked with vigorous activities | 20 |
| Marked with walking 1 mile or mild to moderate rest pain | 15 |
| Marked with walking less than 1 mile | 10 |
| Constant and severe | 0 |
*Functional results were assessed according to the patellofemoral scoring scale. Excellent results equal 90 to 100 points, good equals 80 to 89 points, fair equals 60 to 79 points, and poor equals less than 60 points.
From Karlsson J, et al: Eleven year follow up of patellofemoral pain syndromes. Clin J Sport Med 6:23, 1996.
Ligament Stability
Because the knee, more than any other joint in the body, depends on its ligaments to maintain its integrity, it is imperative that the ligaments be tested. The ligaments of the knee joint act as primary stabilizers and guide the movement of the bones in proper relation to one another. Depending on the motion being tested, the ligaments act as primary or secondary restraints (Table 12-9). For example, the anterior cruciate ligament is the primary restraint to anterior tibial displacement and a secondary restraint to varus-valgus motion in full extension and rotation.98,138 If the primary restraint is injured, pathological motion occurs. If the secondary restraint is injured but the primary restraint is not, pathological motion in that direction does not occur. If both primary and secondary restraints are injured, the pathological motion is greater.98 There are several ligaments around the knee, but four deserve special mention (Figure 12-50).
TABLE 12-9
Primary and Secondary Restraints of the Knee
| Tibial Motion | Primary Restraints | Secondary Restraints |
| Anterior translation | ACL | MCL, LCL; middle third of mediolateral capsule; popliteus corner, semimembranosus corner, iliotibial band |
| Posterior translation | PCL | MCL, LCL; posterior third of mediolateral capsule; popliteus tendon; anterior and posterior meniscofemoral ligaments |
| Valgus rotation (medial gapping) | MCL | ACL, PCL; posterior capsule when knee fully extended, semimembranosus corner |
| Varus rotation (lateral gapping) | LCL | ACL, PCL; posterior capsule when knee fully extended, popliteus corner |
| Lateral rotation | MCL, LCL | Popliteus corner |
| Medial rotation | ACL, PCL | Anteroposterior meniscofemoral ligaments, semimembranosus corner |
Modified from Zachazewski JE, et al, editors: Athletic injuries and rehabilitation, Philadelphia, 1996, WB Saunders, p 627.
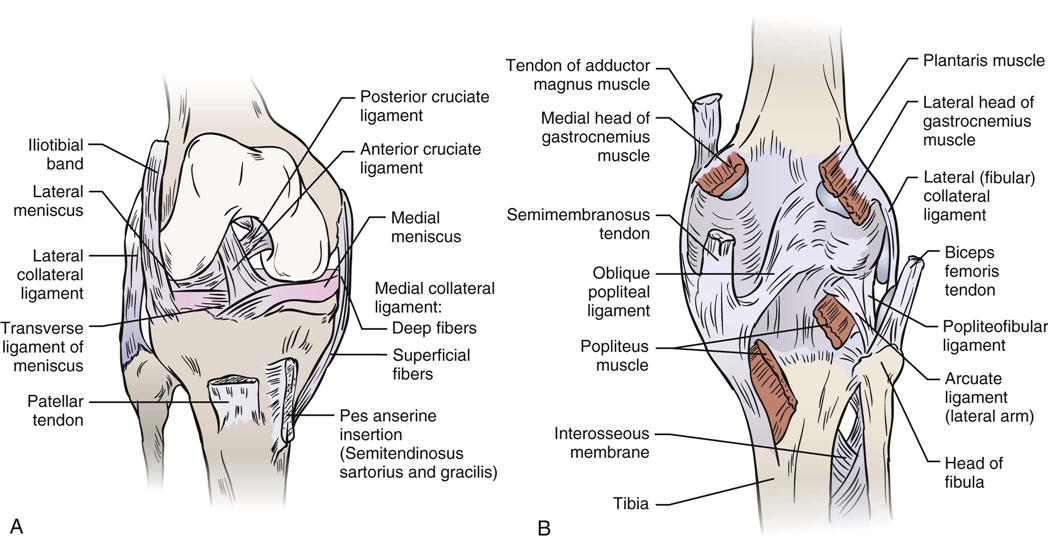
A, Anterior view. The patellar tendon is removed, and the knee is flexed. Note that the cruciate ligament rises in front of the anterior tibial spine, not from it. Note also that the medial meniscus is firmly attached to the medial collateral ligament. B, Posterior view with the knee extended and the posterior ligament removed. The two layers of the medial collateral ligament are shown, as is the tibial portion of the lateral collateral ligament. The posterior cruciate ligament rises behind the tibia, not on its upper surface. Note the femoral attachment of the anterior cruciate ligament on the back of the notch. C, Posterior oblique view showing superficial structures of posterolateral corner. D, Posterior oblique view showing deeper structures including popliteus.
Collateral and Cruciate Ligaments
Collateral Ligaments.
The medial (tibial) collateral ligament lies more posteriorly than anteriorly on the medial aspect of the tibiofemoral joint. It is made up of two layers, one superficial and one deep. The deep layer is a thickening of the joint capsule that blends with the medial meniscus; it is sometimes called the medial capsular ligament. The superficial layer is a strong, broad triangular strap. It starts distal to the adductor tubercle and extends to the medial surface of the tibia, approximately 6 cm (2.4 inches) below the joint line. It blends with the posterior capsule and is separated from the capsule and the medial meniscus by a bursa.
The entire medial collateral ligament is tight throughout the full ROM, although there is varying stress placed on different parts of the ligament as it moves through the full range because of the shape of the femoral condyles. All of its fibers are taut on full extension. In flexion, the anterior fibers are the most taut; in mid range, the posterior fibers are the most taut.139
The lateral (fibular) collateral ligament is round and lies under the tendon of the biceps femoris muscle. It runs from the lateral epicondyle of the femur to the fibular head. It also lies more posteriorly than anteriorly. This ligament is tight in extension and loosens in flexion, especially after 30° flexion. As the knee flexes, it provides protection to the lateral aspect of the knee. It is not attached to the lateral meniscus but rather is separated from it by a small fat pad.139
Cruciate Ligaments.
The cruciate ligaments cross each other and are the primary rotary stabilizers of the knee.140 These strong ligaments are named in relation to their attachment to the tibia and are intracapsular but extrasynovial. Each ligament has an anteromedial and a posterolateral portion. The anterior cruciate ligament has, in addition, an intermediate portion.
The anterior cruciate ligament extends superiorly, posteriorly, and laterally, twisting on itself as it extends from the tibia to the femur. Its main functions are to prevent anterior movement of the tibia on the femur, to check lateral rotation of the tibia in flexion, and, to a lesser extent, to check extension and hyperextension at the knee. It also helps to control the normal rolling and gliding movement of the knee. The anteromedial bundle is tight in both flexion and extension, limits anterior translation and helps stabilize medial and lateral rotation,141,142 whereas the posterolateral bundle is tight in low flexion angles (closer to extension) and medial rotation. It limits anterior translation, hyperextension, and rotation.141 As a whole, the ligament has the least amount of stress on it between 30° and 60° flexion.139,140,143,144
The posterior cruciate ligament extends superiorly, anteriorly, and medially from the tibia to the femur. This strong, fan-shaped ligament, the stoutest ligament in the knee, is a primary stabilizer of the knee against posterior movement of the tibia on the femur, and it checks extension and hyperextension. In addition, the ligament helps to maintain rotary stability and functions as the knee’s central axis of rotation. Along with the anterior cruciate ligament, it acts as a rotary guide to the “screwing home” mechanism of the knee.139,144 For the posterior cruciate ligament, the bulk of the fibers are tight at 30° flexion, but the posterolateral fibers are loose in early flexion.
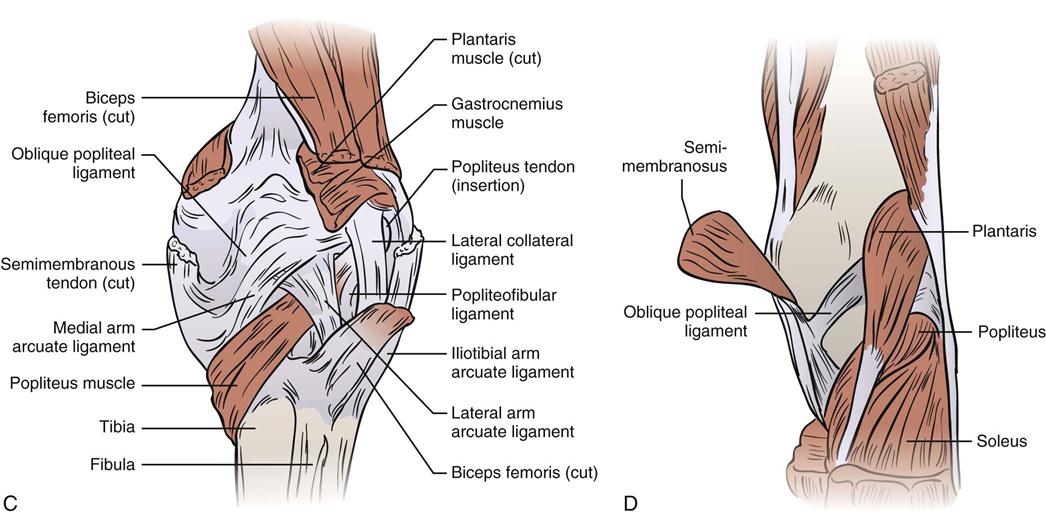
With lateral rotation of the tibia, both collateral ligaments become more taut, and the cruciate ligaments become relaxed (Figure 12-51). With medial rotation of the tibia, the reverse action occurs: the collateral ligaments become more relaxed, and the cruciate ligaments become tighter.139,145
A, The collateral ligament is taut; the cruciate ligament is lax. B, The collateral ligament is lax; the cruciate ligament is taut.
LaPrade et al.146 have stressed the importance of the popliteus in controlling rotation of the tibia on the femur by contributing to lateral rotation stability. They felt the muscle, in fact, acts like a dynamic ligament to help stabilize the knee (see Figure 12-50). Morgan et al.147 reported that the oblique popliteal ligament, which is an expansion of the semimembranosus tendon (see Figure 12-50), was the primary structure preventing hyperextension of the knee.
Testing of Ligaments
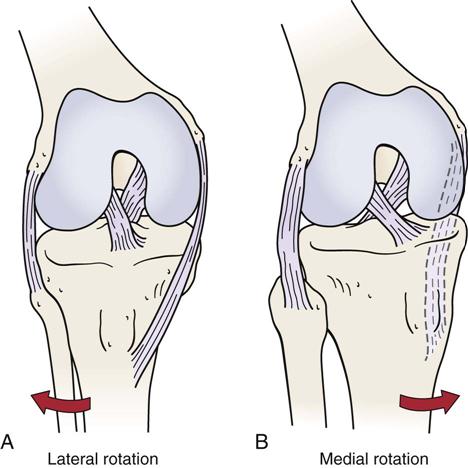
When testing the ligaments of the knee, the examiner must watch for four one-plane instabilities and four rotational instabilities (Table 12-10 and Figure 12-52).
TABLE 12-10
Tests for Ligamentous Instability around the Knee
| Instability | Tests Used to Determine Instability | Structures Injured to Some Degree If Test Positive* | Notes |
| One-plane medial (straight medial) | |||
| One-plane lateral (straight lateral) | |||
| One-plane anterior | |||
| One-plane posterior | |||
| Anteromedial rotary | |||
| Anterolateral rotary | |||
| Posteromedial rotary | |||
| Posterolateral rotary |
ALRI, Anterolateral rotary instability.
*The amount of displacement gives an indication of how badly and how much of the structures are injured (i.e., first-, second-, or third-degree sprain).
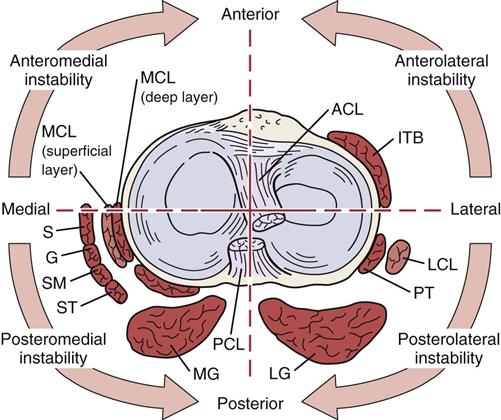
ACL, Anterior cruciate ligament; G, gracilis; ITB, iliotibial band; LCL, lateral collateral ligament; LG, lateral gastrocnemius, MCL, medial collateral ligament; MG, medial gastrocnemius; PCL, posterior cruciate ligament; POL, posterior oblique ligament; PT, popliteal tendon; S, sartorius; SM, semimembranosus; ST, semitendinosus.
There are a number of tests for each type of instability. The examiner should use the one or two tests that he or she believes gives the best results. It is not essential to do all of the tests discussed. The techniques chosen must be practiced diligently so that the examiner becomes proficient at doing them; only with practice will the examiner be able to determine which structures are injured. It is also important to understand that the direction of instability does not imply that only structures in that direction are injured. For example, with anterolateral rotary instability (ALRI), it is not necessarily structures on the anterolateral side of the knee that are injured. In fact, posterior structures are often commonly injured as well. With ALRI, the posterolateral capsule and the arcuate-popliteus complex may also be injured.28
When testing for ligament stability of the knee, the examiner should keep the following points in mind:
2. When one is comparing the normal and injured limbs, the test must be the same for both limbs. The examiner must use the same initial starting position and the same amount of force, apply the same force at the same point or throughout the range, and note the position at which the displacement occurs.148
4. The appropriate stress should be applied gently.
6. It is not only the degree of opening but also the quality of the opening (i.e., the end feel) that is of concern. Left-right differences of 3 mm or more are classified as pathological.148
7. If the ligament is intact, there should be an abrupt stop or end feel when the ligament is stressed. A soft or indistinct end feel usually signifies ligamentous injury.149
Tests for One-Plane Medial Instability
The abduction (valgus stress) test ![]() is an assessment for one-plane (straight) medial instability, which means that the tibia moves away from the femur (i.e., gaps) on the medial side (Figure 12-53). The examiner applies a valgus stress (pushes the knee medially) at the knee while the ankle is stabilized in slight lateral rotation either with the hand or with the leg held between the examiner’s arm and trunk. The knee is first in full extension, and then it is slightly flexed (20° to 30°) so that it is “unlocked.”86
is an assessment for one-plane (straight) medial instability, which means that the tibia moves away from the femur (i.e., gaps) on the medial side (Figure 12-53). The examiner applies a valgus stress (pushes the knee medially) at the knee while the ankle is stabilized in slight lateral rotation either with the hand or with the leg held between the examiner’s arm and trunk. The knee is first in full extension, and then it is slightly flexed (20° to 30°) so that it is “unlocked.”86
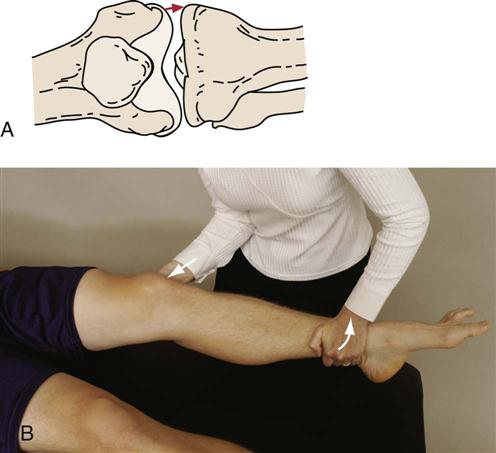
 Figure 12-53 Abduction (valgus stress) test.
Figure 12-53 Abduction (valgus stress) test.A, “Gapping” on the medial aspect of the knee. B, Positioning for testing the medial collateral ligament (extended knee).
It has been advocated that resting the test thigh on the examining table enables the patient to relax more and is easier for the examiner. The knee rests on the edge of the table; the lower leg is controlled by the examiner’s stabilizing the thigh on the table, and the lower leg is abducted, applying a valgus stress to the knee (Figure 12-54).30 Similarly, a varus stress may be applied to stress the lateral structures.
Hughston30 advocates a third way to do this test (Hughston’s valgus stress test ![]() ). The patient is positioned as described earlier, and the examiner faces the patient’s foot, placing his or her body against the patient’s thigh to help stabilize the upper leg in combination with one hand, which can also palpate the joint line. With the other hand, the examiner grasps the patient’s big toe and applies a valgus stress, allowing any natural rotation of the tibia (Figure 12-55). Similarly, a varus stress may be applied to test the lateral structures, but in this case, the examiner grasps the lateral aspect of the foot near the fifth and fourth toes. A varus stress is then applied to the knee. Doing the test in this fashion often allows the patient to relax more and is less likely to lead to muscle spasm limiting movement.
). The patient is positioned as described earlier, and the examiner faces the patient’s foot, placing his or her body against the patient’s thigh to help stabilize the upper leg in combination with one hand, which can also palpate the joint line. With the other hand, the examiner grasps the patient’s big toe and applies a valgus stress, allowing any natural rotation of the tibia (Figure 12-55). Similarly, a varus stress may be applied to test the lateral structures, but in this case, the examiner grasps the lateral aspect of the foot near the fifth and fourth toes. A varus stress is then applied to the knee. Doing the test in this fashion often allows the patient to relax more and is less likely to lead to muscle spasm limiting movement.

 Figure 12-55 Hughston’s valgus stress test.
Figure 12-55 Hughston’s valgus stress test.If the test is positive (i.e., the tibia moves away from the femur an excessive amount when a valgus stress is applied) when the knee is in extension, the following structures may have been injured to some degree:
1. Medial collateral ligament (superficial and deep fibers)
5. Posterior cruciate ligament
A positive finding on full extension is classified as a major disruption of the knee. The examiner usually finds that one or more of the rotary tests are also positive. If the examiner applies lateral rotation to the foot when performing the test in extension and finds excessive lateral rotation on the affected side, it is a sign of possible anteromedial rotary instability.
If the test is positive when the knee is flexed to 20° to 30°, the following structures may have been injured to some degree:
This flexed part of the valgus stress test would be classified as the true test for one-plane medial instability.
Lonergan and Taylor151 advocated doing the Swain test ![]() for the knee. For this test, the patient is seated with the knees flexed to 90° over the edge of the examining table. The examiner then passively laterally rotates the tibia on the femur of the good leg followed by the injured leg. A positive test is indicated by pain along the medial side of the joint indicating injury to the medial collateral ligament complex, because with the knee flexed to 90° the cruciates are lax, whereas the collateral ligaments are tight. Post surgery, pain on the medial joint line may indicate inadequate healing; or, in the chronic medial side laxity, joint line pain may be medial or posteromedial (Figure 12-56).152
for the knee. For this test, the patient is seated with the knees flexed to 90° over the edge of the examining table. The examiner then passively laterally rotates the tibia on the femur of the good leg followed by the injured leg. A positive test is indicated by pain along the medial side of the joint indicating injury to the medial collateral ligament complex, because with the knee flexed to 90° the cruciates are lax, whereas the collateral ligaments are tight. Post surgery, pain on the medial joint line may indicate inadequate healing; or, in the chronic medial side laxity, joint line pain may be medial or posteromedial (Figure 12-56).152

Pain along the medial side of the knee indicates medial collateral ligament complex injury.
If a stress radiograph is taken when the test is performed in full extension, a 5-mm opening indicates a grade 1 injury; up to 10 mm, a grade 2 injury; and more than 10 mm, a grade 3 injury.139,153 Both limbs should be viewed for differences.154
Tests for One-Plane Lateral Instability
The adduction (varus stress) test ![]() is an assessment for one-plane lateral instability (i.e., the tibia moves away from the femur an excessive amount on the lateral aspect of the leg). The examiner applies a varus stress (pushes the knee laterally) at the knee while the ankle is stabilized (Figure 12-57). The test is first done with the knee in full extension and then with the knee in 20° to 30° of flexion. If the tibia is laterally rotated in full extension before the test, the cruciate ligaments are uncoiled, and maximum stress is placed on the collateral ligaments.
is an assessment for one-plane lateral instability (i.e., the tibia moves away from the femur an excessive amount on the lateral aspect of the leg). The examiner applies a varus stress (pushes the knee laterally) at the knee while the ankle is stabilized (Figure 12-57). The test is first done with the knee in full extension and then with the knee in 20° to 30° of flexion. If the tibia is laterally rotated in full extension before the test, the cruciate ligaments are uncoiled, and maximum stress is placed on the collateral ligaments.
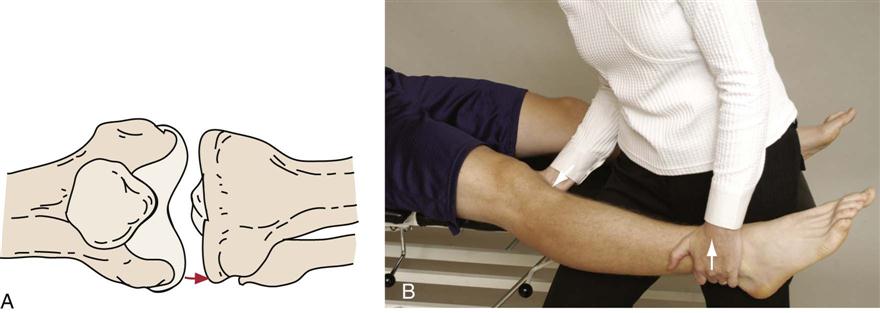
 Figure 12-57 Adduction (varus stress) test.
Figure 12-57 Adduction (varus stress) test.A, One-plane lateral instability “gapping” on the lateral aspect. B, Positioning for testing lateral collateral ligament in extension.
As previously mentioned (see the “Tests for One-Plane Medial Instability” section), Hughston’s varus stress test ![]() may be used. In this case, the examiner grasps the fifth and fourth toes and applies a varus stress to the knee in extension and slightly (20° to 30°) flexed.
may be used. In this case, the examiner grasps the fifth and fourth toes and applies a varus stress to the knee in extension and slightly (20° to 30°) flexed.
If the test is positive (i.e., the tibia moves away from the femur when a varus stress is applied) in extension, the following structures may have been injured to some degree:
1. Fibular or lateral collateral ligament
5. Posterior cruciate ligament
The examiner usually finds that one or more rotary instability tests are also positive. A positive test indicates major instability of the knee.
If the test is positive when the knee is flexed 20° to 30° with lateral rotation of the tibia, the following structures may have been injured to some degree:
This flexed part of the varus stress test is classified as the true test for one-plane lateral instability.
If a stress radiograph is taken when the test is performed in full extension, a 5-mm opening indicates a grade 1 injury; up to 8 mm, a grade 2 injury; and more than 8 mm, a grade 3 injury to the lateral ligaments of the knee.139,153
Both varus and valgus stress testing (varus-valgus test ![]() ) can be performed at the same time while the examiner palpates the joint line. The examiner holds the ankle between the examiner’s waist and forearm while the patient lies supine with the knee extended and then flexed. At the same time, the examiner palpates the medial and lateral joint lines with the fingers. Varus and valgus stresses are applied with the heels of the examiner’s hands (Figure 12-58).79
) can be performed at the same time while the examiner palpates the joint line. The examiner holds the ankle between the examiner’s waist and forearm while the patient lies supine with the knee extended and then flexed. At the same time, the examiner palpates the medial and lateral joint lines with the fingers. Varus and valgus stresses are applied with the heels of the examiner’s hands (Figure 12-58).79
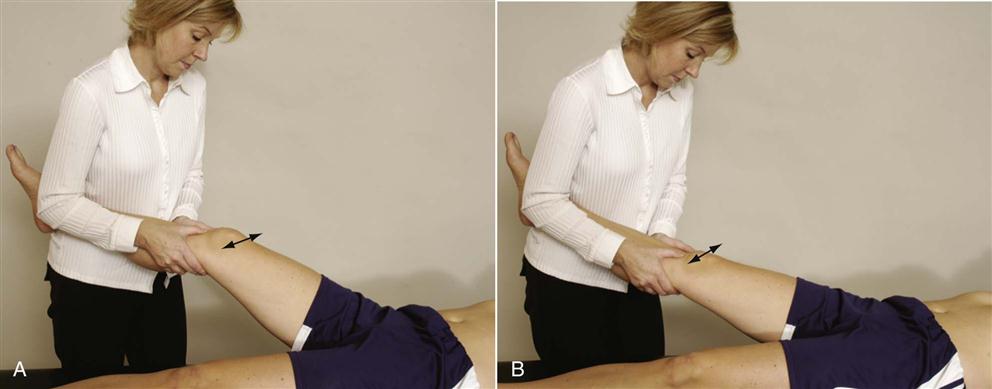
A, Knee flexed. B, Knee extended.
Tests for One-Plane Anterior Instability
Some clinicians28,30 believe that the posterior cruciate ligament should be tested (see the “Tests for One-Plane Posterior Instability” section) or observed for a posterior sag before the anterior cruciate ligament is tested to rule out false-positive tests for anterior translation. In either case, the examiner should be aware that a torn posterior cruciate can lead to a false-positive anterior translation test if the patient is tested in supine position with the knee flexed, because gravity causes the tibia to sag posteriorly.
 Active Drawer Test.
Active Drawer Test.
For the anterior drawer test (also called the quadriceps active test), the patient is positioned as for the normal drawer test. The examiner holds the patient’s foot down. The patient is asked to try to straighten the leg, and the examiner prevents the patient from doing so (isometric test). Muller139 advocated allowing the foot to be free and noting when the foot is lifted off the table, which occurs only after the tibia has shifted forward and stabilized. If the anterior cruciate ligament or posterior cruciate ligament is torn, the anterior contour of the knee changes as the tibia is drawn forward. If the posterior cruciate ligament is torn, a posterior sag is evident before the patient contracts the quadriceps. Contraction of the quadriceps causes the tibia to shift forward to its normal position, indicating a positive test for a torn posterior cruciate ligament.155,156 If there is no posterior sag present and if the tibia shifts forward more on the injured side than the noninjured side, it is a positive test for anterior cruciate ligament disruption (Figure 12-59).155 A second part of the test may be instituted by having the patient contract the hamstrings isometrically so that the tibial plateau moves posteriorly. This part of the test accentuates the posterior sag for posterior cruciate insufficiency, if present, and ensures maximum movement for anterior cruciate insufficiency if a quadriceps contraction is tried a second time.79 The active drawer test is a better expression of posterior cruciate insufficiency than of anterior cruciate insufficiency.157
With the drawer sign or test, if the anterior or posterior cruciate ligament is torn (third-degree sprain), some rotary instability is evident when the appropriate ligamentous tests are performed.
 Drawer Sign.
Drawer Sign.
The drawer sign is a test for one-plane anterior and one-plane posterior instabilities.158 The difficulty with this test is in determining the neutral starting position if the ligaments have been injured. The patient’s knee is flexed to 90°, and the hip is flexed to 45°. In this position, the anterior cruciate ligament is almost parallel with the tibial plateau. The patient’s foot is held on the table by the examiner’s body with the examiner sitting on the patient’s forefoot and the foot in neutral rotation. The examiner’s hands are placed around the tibia to ensure that the hamstring muscles are relaxed (Figures 12-60 and 12-61). The tibia is then drawn forward on the femur (anterior drawer test). The normal amount of movement that should be present is approximately 6 mm. This part of the test assesses one-plane anterior instability. If the test is positive (i.e., the tibia moves forward more than 6 mm on the femur), the following structures may have been injured to some degree:
1. Anterior cruciate ligament (especially the anteromedial bundle)

 Figure 12-60 Position for drawer sign.
Figure 12-60 Position for drawer sign.If only the anterior cruciate ligament is torn, the test is negative, because other structures (posterior capsule and posterolateral and posteromedial structures) limit movement. In addition, hemarthrosis, a torn medial meniscus (posterior horn) wedged against the medial femoral condyle, or hamstring spasm may result in a false-negative test. Hughston30 points out that tearing of the coronary or meniscotibial ligament can allow the tibia to translate forward more than normal, even in the presence of an intact anterior cruciate ligament. In this case, when the anterior drawer test is performed, anteromedial rotation (subluxation) of the tibia occurs.
When performing this test, the examiner must ensure that the posterior cruciate ligament is not torn or injured. If it has been torn, it allows the tibia to drop or slide back on the femur, and when the examiner pulls the tibia forward, a large amount of movement occurs, giving a false-positive sign (see the “Posterior Sag Sign” section). Therefore the test should be considered positive only if it is shown that the posterior sag is not present.
Weatherwax159 described a modified way of testing the anterior drawer (90–90 anterior drawer). The patient lies supine. The examiner flexes the patient’s hip and knee to 90° and supports the lower leg between the examiner’s trunk and forearm. The examiner places the hands around the tibia, as with the standard test, and applies sufficient force to slowly lift the patient’s buttock off the table (Figure 12-62).
If, when doing the anterior drawer test, there is an audible snap or palpable jerk (Finochietto jumping sign) when the tibia is pulled forward and the tibia moves forward excessively, a meniscus lesion is probably accompanying the torn anterior cruciate ligament.79
After the anterior movement of the tibia on the femur, the posterior movement of the tibia on the femur should be completed (posterior drawer test). In this part of the test, the tibia is pushed back on the femur. This phase is a test for one-plane posterior instability. If the test is positive or a posterior sag is evident, the following structures may have been injured to some degree:
If the arcuate-popliteus complex remains intact, a positive posterior drawer sign may not be elicited.160 If, when the tibia is pushed backward, the examiner forcefully rotates the tibia laterally and excessive movement occurs, the test is positive for posterolateral instability. Warren161 calls this maneuver the arcuate spin test.
Feagin162 advocated doing the drawer test with the patient sitting with the leg hanging relaxed over the end of the examining table (sitting anterior drawer test). The examiner places the hands as with the standardized test and slowly draws the tibia first forward and then backward to test the anterior and posterior drawer (Figure 12-63). The examiner uses the thumbs to palpate the tibial plateau movement relative to the femur. The examiner may also note any rotational deformity. The advantage of doing the test this way is that the posterior sag is eliminated because the effect of gravity is eliminated.
 Lachman Test.
Lachman Test.
The Lachman test, which may also be referred to as the Ritchie, Trillat, or Lachman-Trillat test, is the best indicator of injury to the anterior cruciate ligament, especially the posterolateral band,163–168 although this has been questioned.169 It is a test for one-plane anterior instability.86,170 The patient lies supine with the involved leg beside the examiner. The examiner holds the patient’s knee between full extension and 30° of flexion. This position is close to the functional position of the knee, in which the anterior cruciate ligament plays a major role. The patient’s femur is stabilized with one of the examiner’s hands (the “outside” hand) while the proximal aspect of the tibia is moved forward with the other (“inside”) hand (Figure 12-64). Frank171 reported that to achieve the best results, the tibia should be slightly laterally rotated and the anterior tibial translation force should be applied from the posteromedial aspect. Therefore the hand on the tibia should apply the translation force. A positive sign is indicated by a “mushy” or soft end feel when the tibia is moved forward on the femur (increased anterior translation with medial rotation of the tibia) and disappearance of the infrapatellar tendon slope.168 A false-negative test may occur if the femur is not properly stabilized, if a meniscus lesion blocks translation, or if the tibia is medially rotated.171 A positive sign indicates that the following structures may have been injured to some degree:

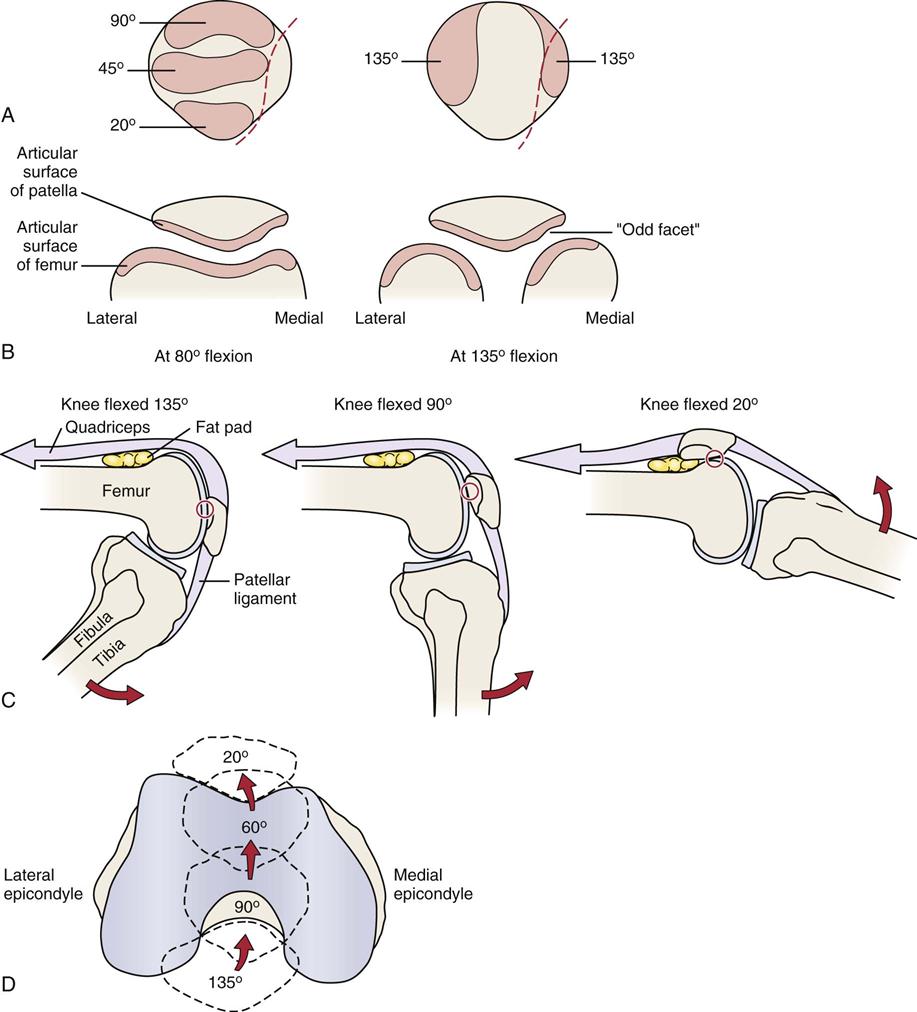
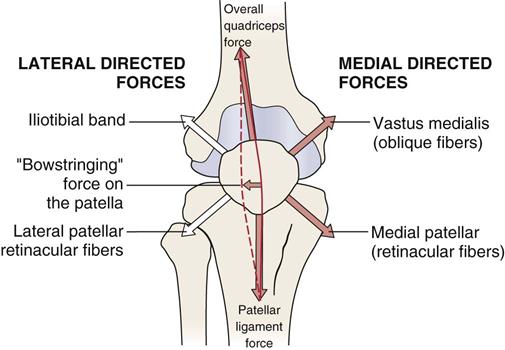

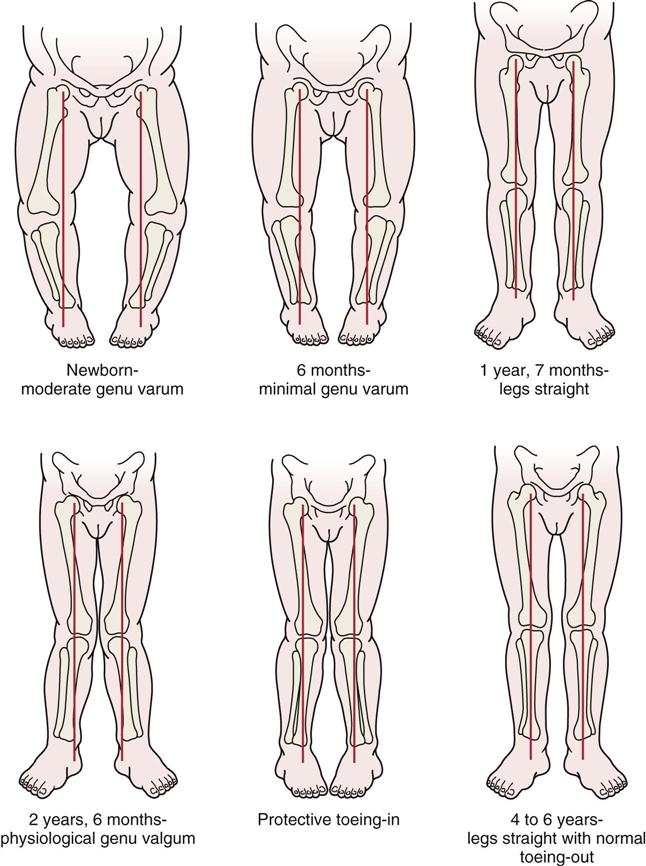
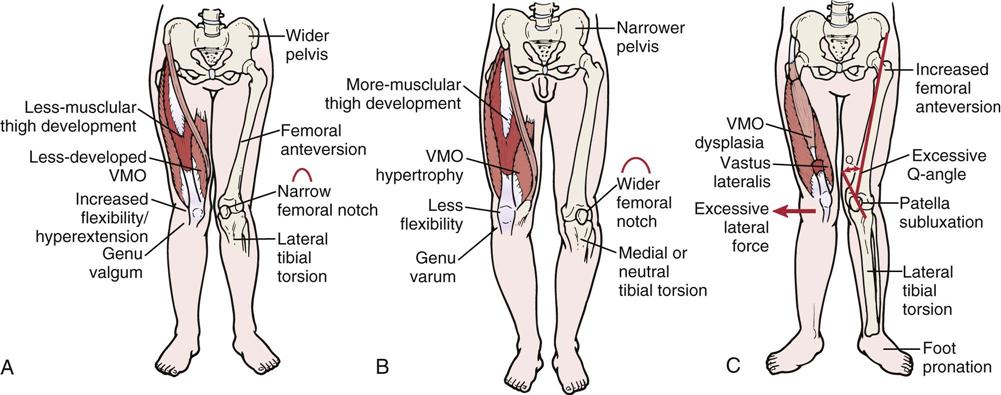
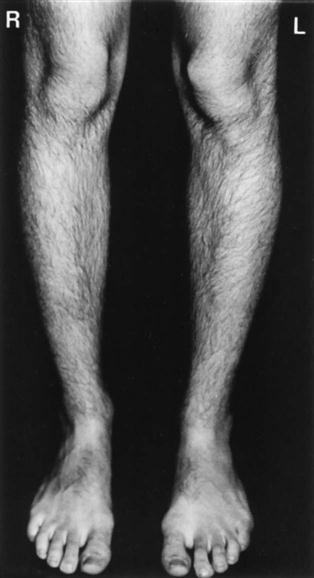
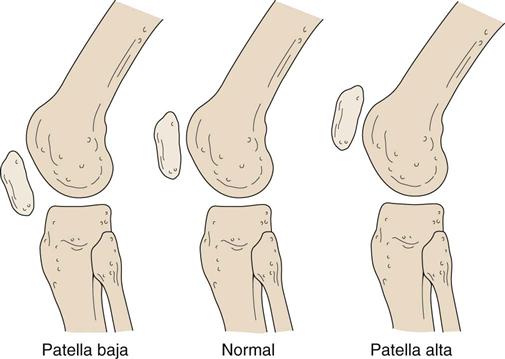

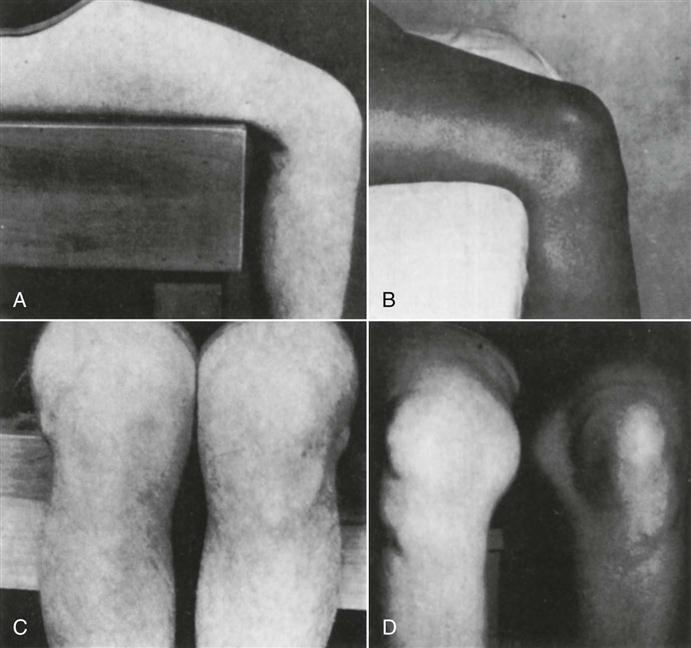

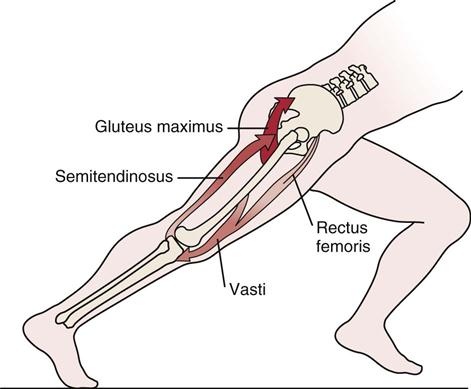
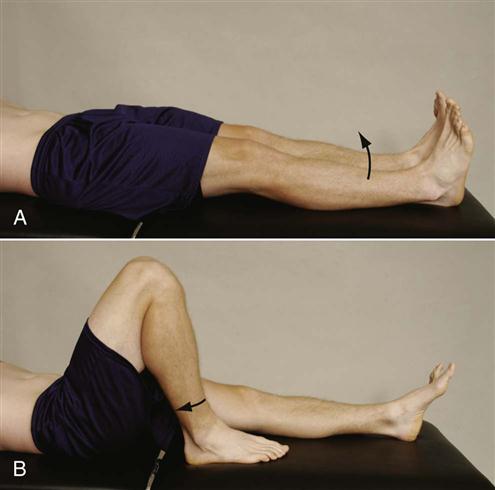
 Figure 12-27
Figure 12-27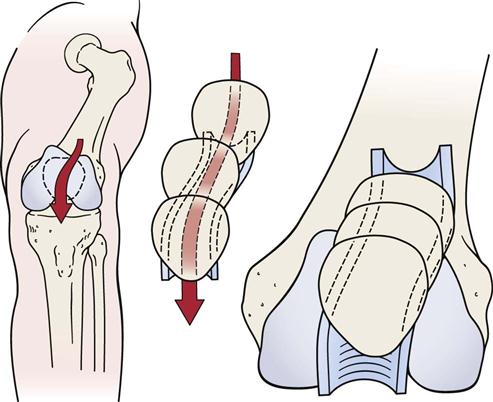
 Figure 12-28
Figure 12-28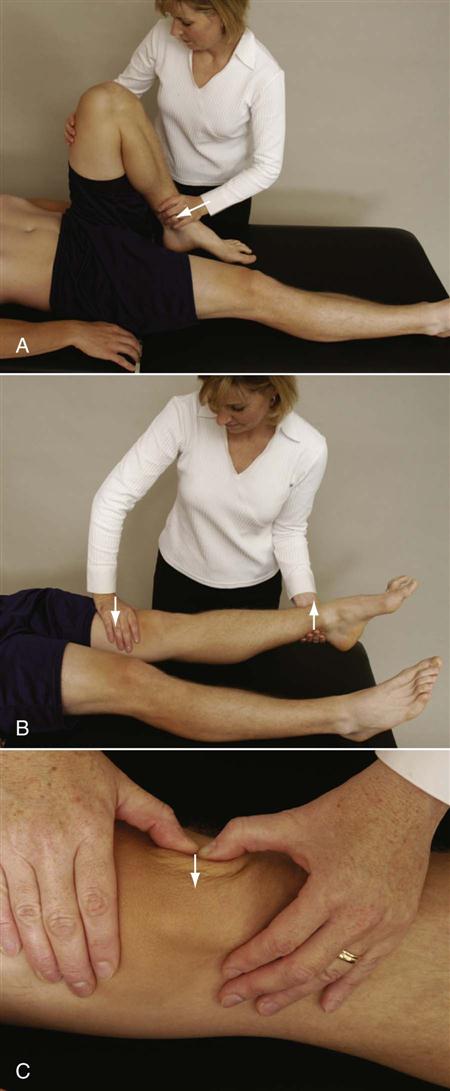
 Figure 12-30
Figure 12-30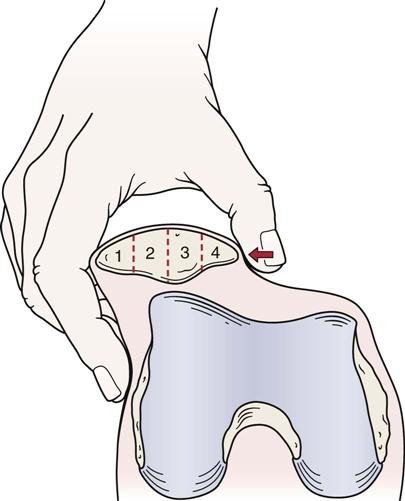
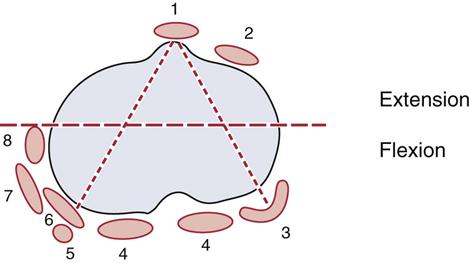
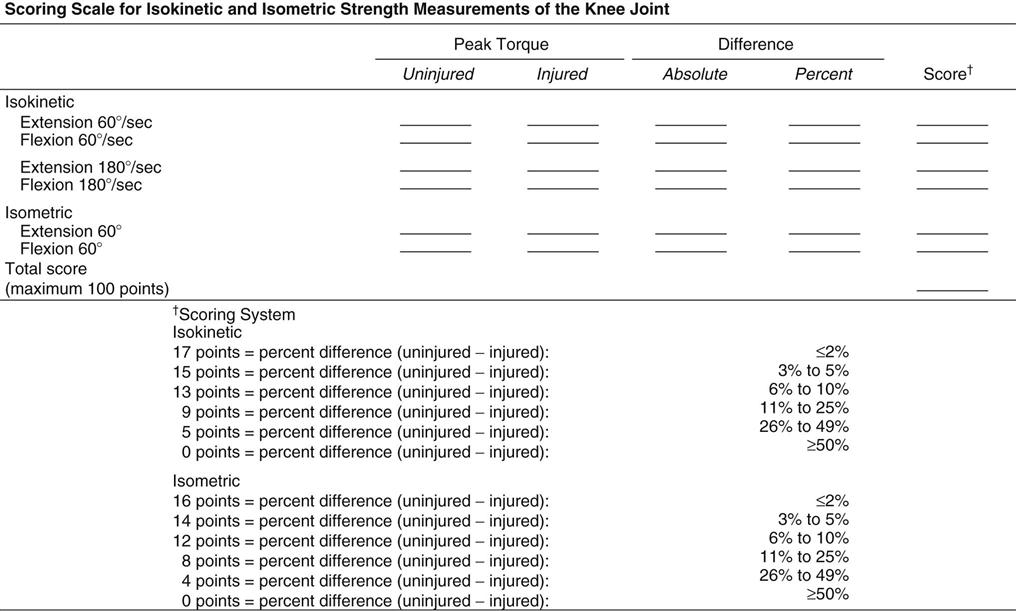
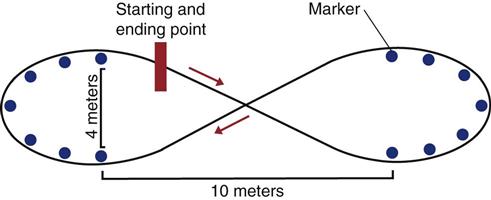
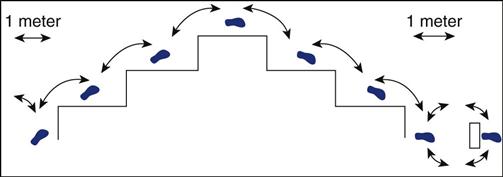
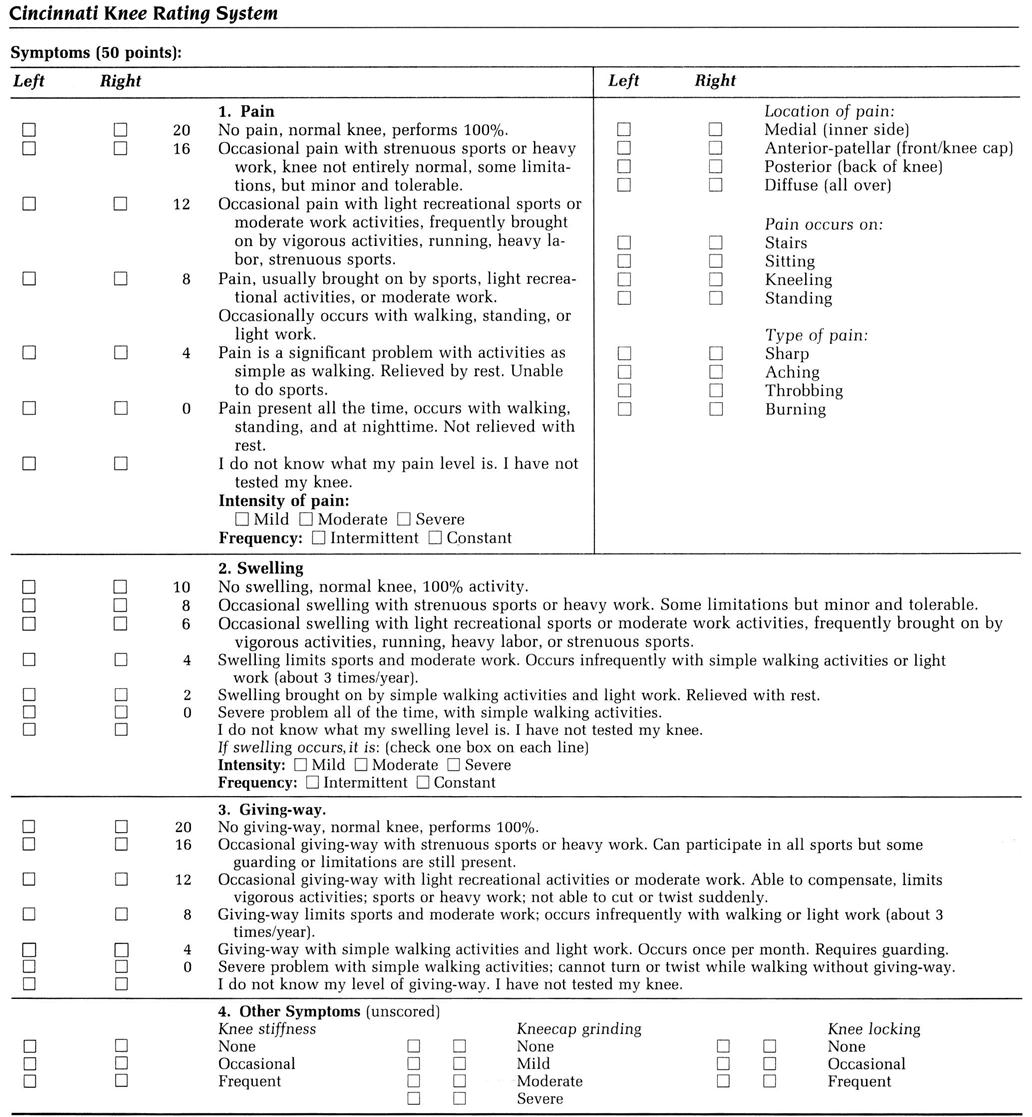
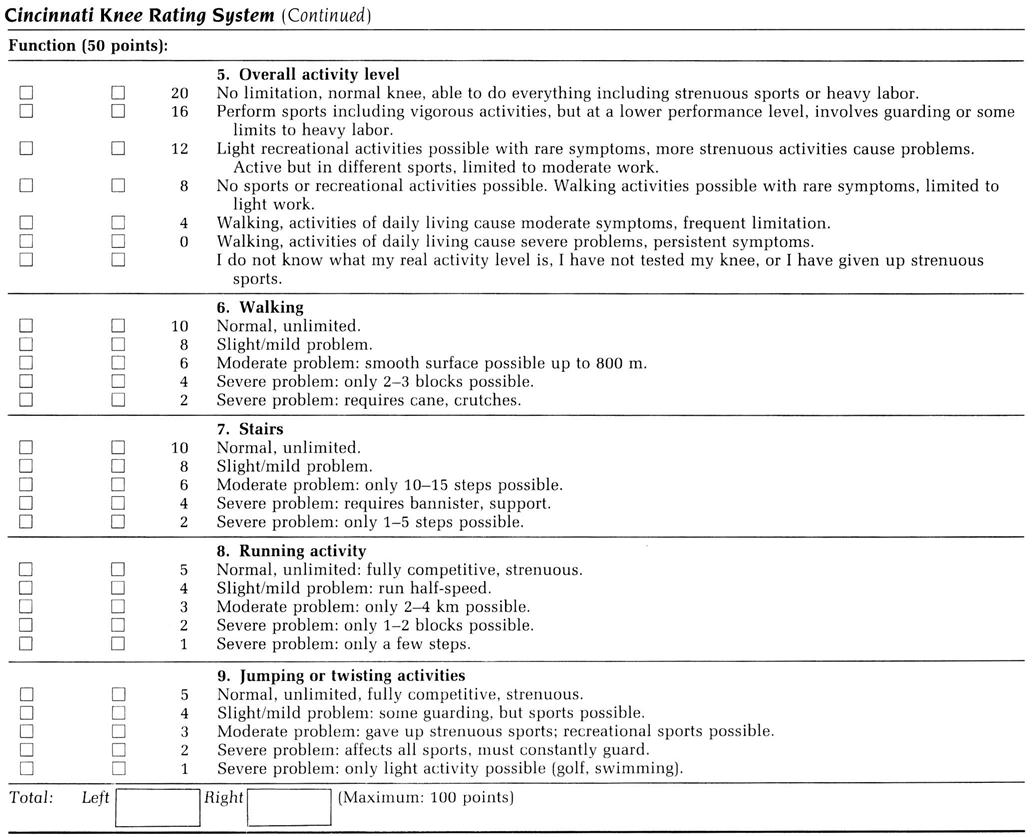
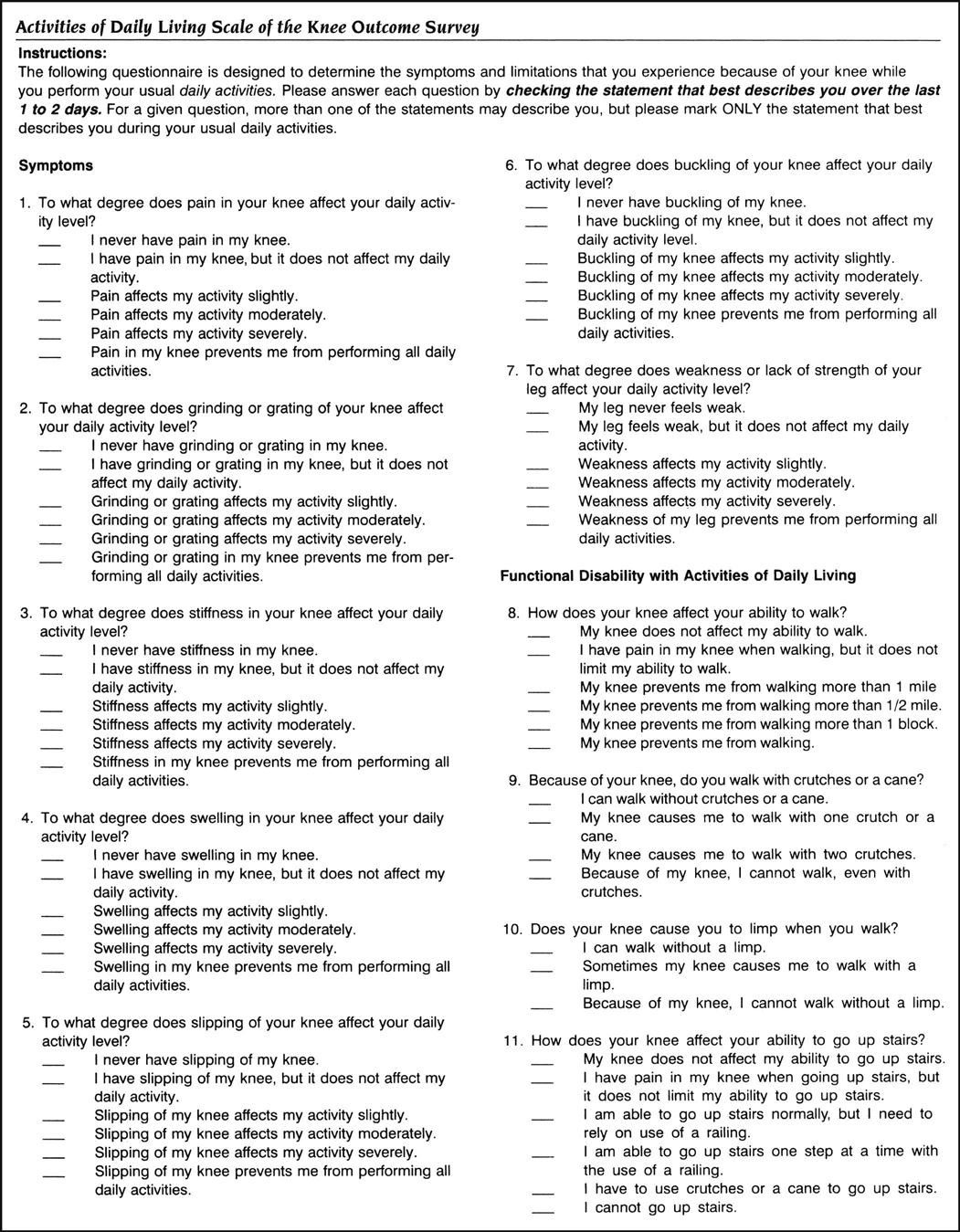
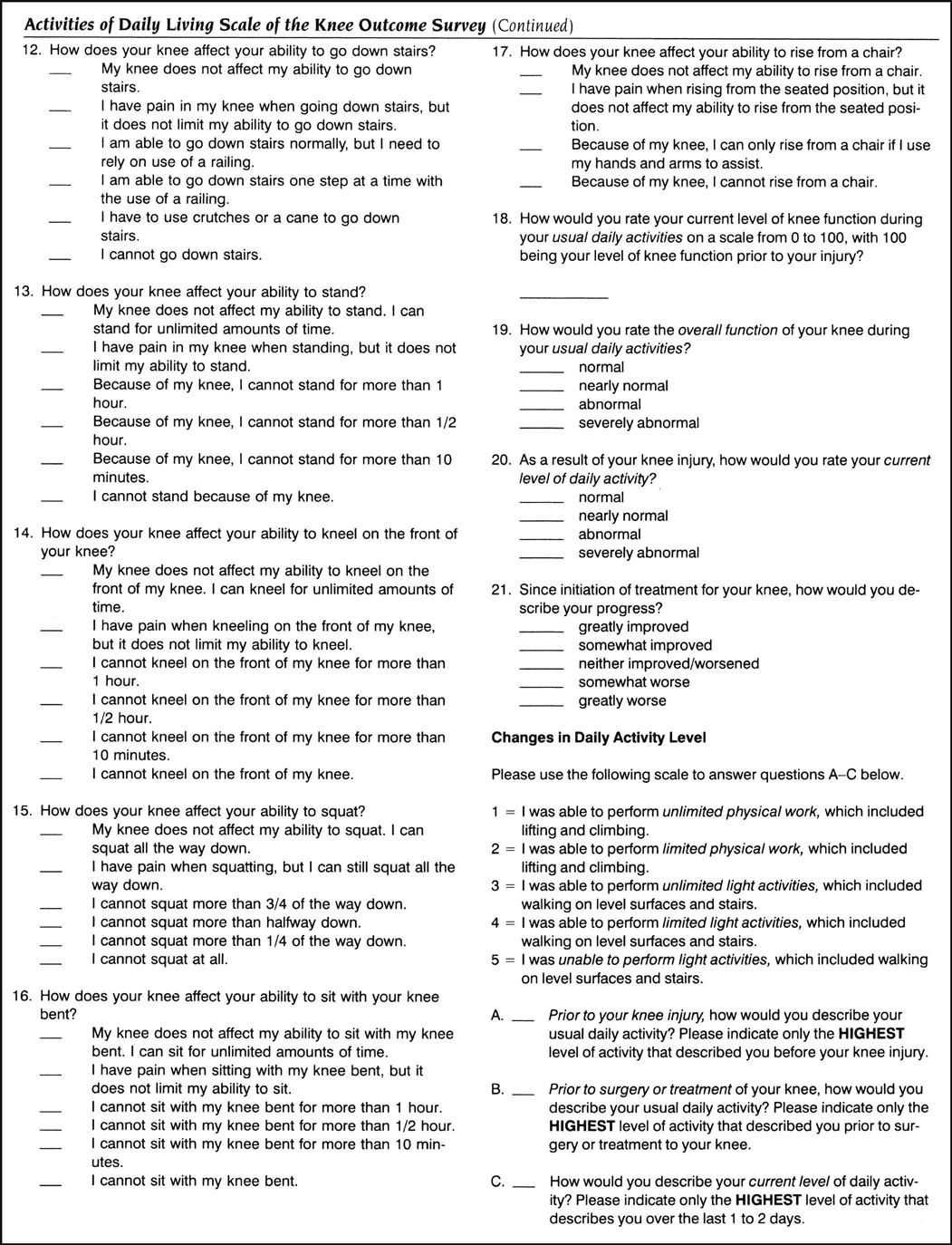
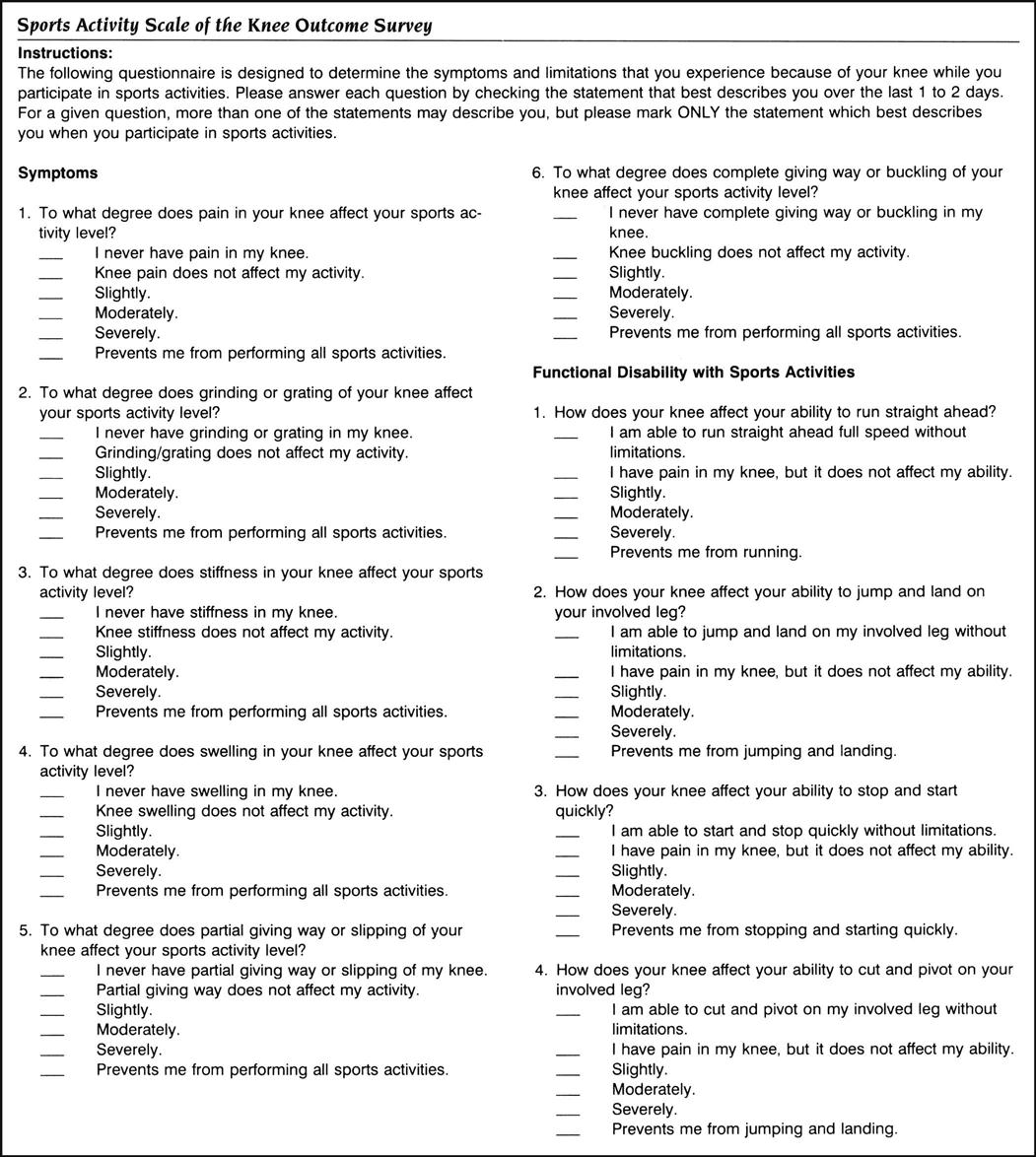
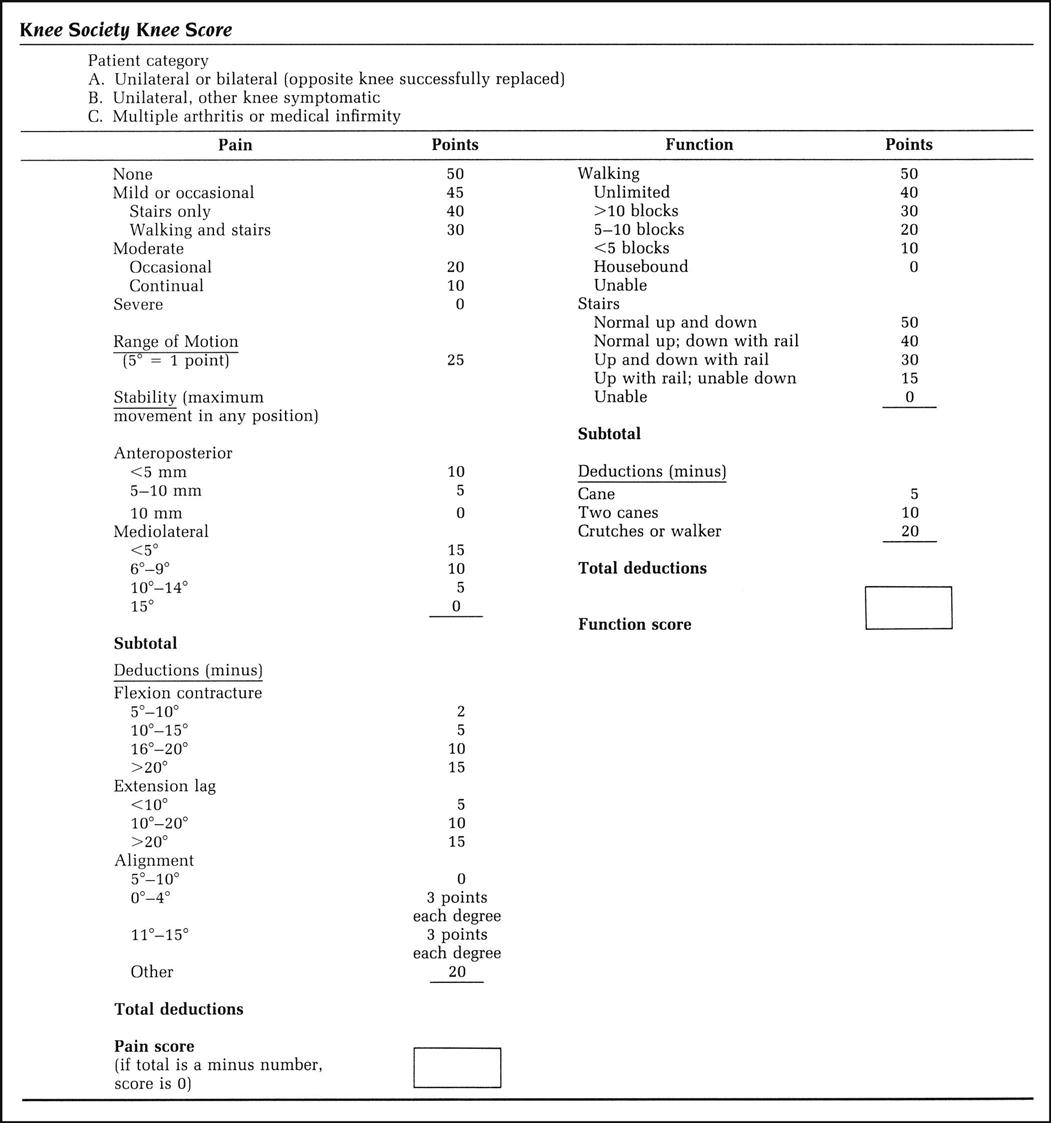
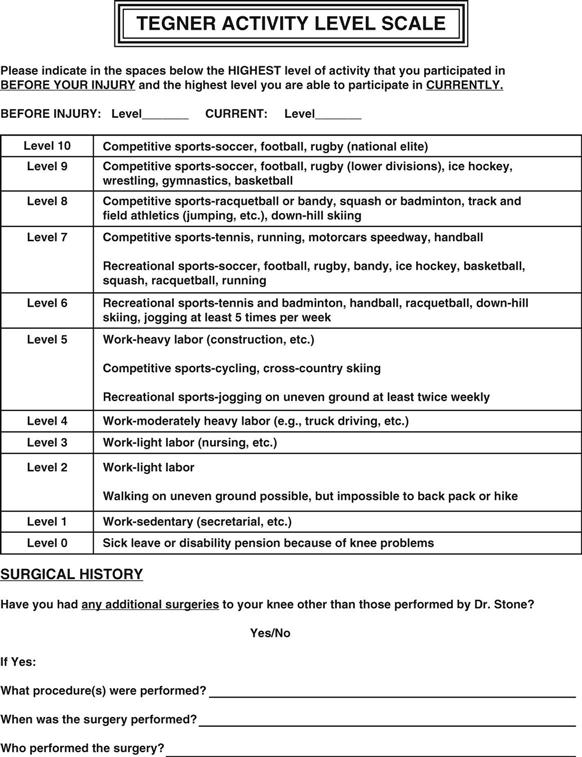
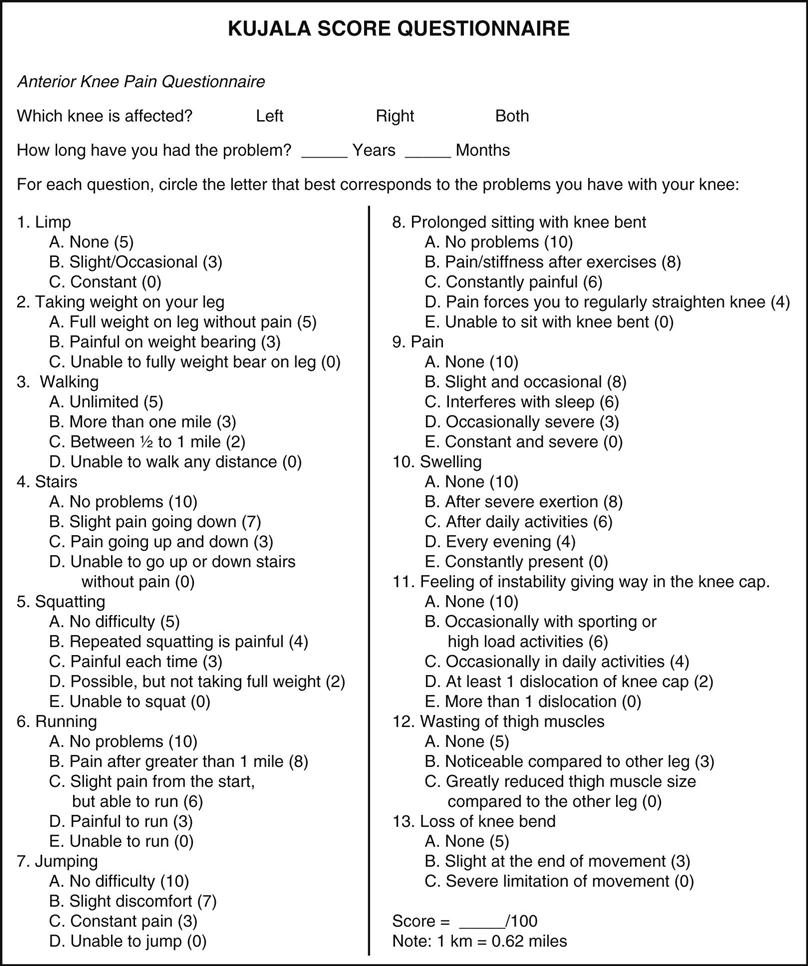


 Figure 12-59
Figure 12-59