CHAPTER 25 Sexuality
25A. Sexual Development and Sexual Behavior Problems
Sexual behavior problems (SBPs) are deviations from typical sexual development and are defined as child-initiated behaviors that involve sexual body parts (i.e., genitals, anus, buttocks, or breasts) and are developmentally inappropriate or potentially harmful to themselves or others.1 Information about sexual development and guidelines for differentiating typical sexual behaviors from SBPs are rarely integrated in child development books or other types of parent educational materials. Thus, parents are often unsure how to determine whether sexual behaviors, such as interactions between children involving touching of genitals, are just “playing doctor” or something of concern. Parental guidance on sexual matters provided by developmental pediatricians facilitates caregiver’s education and decision making. Sexual behaviors occur on a continuum ranging from typical to problematic; therefore, to accurately identify and manage problems related to sexual behavior of children and youth, a good foundation in sexual development is necessary. Research on childhood SBPs is relatively new, although significant progress has been made since the 1980s in distinguishing typical development from SBPs, as well as in understanding the origins, trajectory, and treatment of SBPs in youth.
This chapter provides an overview of typical sexual development, knowledge, and behavior of preschoolers, school-aged children, and adolescents. To facilitate understanding of the terms and concepts, definitions of key variables are provided. SBPs are defined with information on origins of the behavior, developmental progression, assessment, and treatment outcome research for children and adolescents. Guidelines for distinguishing typical sexual behavior from SBPs are provided, as are references for parental education guidelines. Gender identity disorder is not discussed in this section; it is addressed in Chapters 25B and 25C.
We are not aware of another text designed specifically for developmental-behavioral pediatricians that covers both sexual development and the identification, assessment, treatment of, and response to SBPs across childhood and adolescence. A number of references provide pediatricians with information about typical sexual development and parental guidance suggestions, including provision of sex education.2–6 In addition, Horner provided a pediatric-focused brief review of sexual development and SBPs in children, including two case studies.7 The Association for the Treatment of Sexual Abusers (ATSA) Task Force on Children with Sexual Behavior Problems published a report on the identification, assessment, treatment, and public policies on children with SBPs, but this report does not address adolescence.8 Older reviews include an excellent book on sexually aggressive youth by Araji9; a chapter that also includes information on children with SBPs, adolescent sexual offenders, and adult sexual offenders10; and practice parameters provided by the American Academy of Child and Adolescent Psychiatry.11 Readers of these older reviews are advised to recognize that research published more recently updates previous assumptions, particularly regarding trajectory of the behaviors, long-term risk, and treatment outcome.
TERMINOLOGY
For this chapter, sex and gender are distinguished as follows: Sex is the classification by male or female reproductive organs,12 whereas gender is the behavioral, cultural, or psychological traits typically associated with one sex.13 Genitals refers specifically to external organs of the reproductive system, but references to “private parts” also include buttocks, anus, and breasts. Before specific information about how sexual knowledge and behavior evolve over the course of childhood and adolescents is provided, clarification in terminology would facilitate understanding of the research. In regard to knowledge about sexual matters, researchers have examined a wide range of children’s understanding of sex and sexual matters. Table 25A-1 lists the terms used in this chapter with their definitions.
TABLE 25A-1 Terms Used in This Chapter, Their Definitions, and Areas of Knowledge
| Term | Definition | Reference |
|---|---|---|
| Term Used in This Chapter | ||
| Gender | Behavioral, cultural, or psychological traits typically associated with one sex | 13 |
| Sex | Classification by male or female reproductive organs | 12 |
| Genitals | The organs of the reproductive system; especially the external genital organs | 13 |
| Private parts or sexual body parts | Genitals, buttocks, anus, and breasts | |
| Sex role or gender role | The degree to which an individual acts out a stereotypical masculine or feminine role in everyday behavior | 157 |
| Sexual orientation | The inclination of an individual with regard to heterosexual, homosexual, and bisexual behavior | 13 |
| Sex preferences | Sex that children prefer to be like, to identify with, and to imitate in regard to sex role behavior | 16 |
| Childhood sexual behavior | Child-initiated behaviors involving sexual body parts (i.e., genitals, anus, buttocks, or breasts) | 1 |
| Sex play | Childhood sexual behavior that occurs spontaneously and intermittently, is mutual and noncoercive when it involves other children, and does not cause emotional distress | 1 |
| Sexual curiosity | Sexual behavior or questions about sexual matters motivated by inquisitive interest | |
| Sexual behavior problems in children and adolescents | Child and adolescents-initiated behaviors involving sexual body parts (i.e., genitals, anus, buttocks, or breasts) that are developmentally inappropriate or potentially harmful to themselves or others | 1 |
| Interpersonal or intrusive sexual behavior problems | Sexual behavior problems that involve two or more individuals and direct physical contact | 146 |
| Aggressive sexual behaviors | Sexual behavior problems that involve coercion, force, hostile intent, harm, or threatened harm | |
| Adolescent sexual offender | Adolescents between the ages of 13 and 17 years who commit illegal sexual behavior as defined by the sex crime statutes of the jurisdiction in which the offense occurred | 121 |
| Areas of Knowledge | ||
| Labels of female genitalia | Terms for female genitalia, such as vagina or a slang term | 18 |
| Labels of male genitalia | Terms for male genitalia, such as penis or slang term | 18 |
| Physiological distinctions between sexes | Understanding of the basic genitalia differences between sexes (i.e., boys/men have penises and girls/women have vaginas) rather than basing sex differences on other physical, behavioral, or character differences, often related to cultural gender distinctions (e.g., for white American children, beliefs that boys/men have short hair and girls/women have long hair) | 18 |
| Pregnancy and birth | Knowledge related to conception, roles of both father and mother in conception, intrauterine growth, and birth process (i.e., cesarean or vaginal delivery) | 18 |
| Adult sexual behavior | Behavior of adults related to intimate interactions, arousal, and/or stimulation of genitals, including kissing, masturbation, and sexual intercourse; not limited to procreation | 18 |
| Knowledge of sexual abuse | Conceptualizations of sexual abuse, abusers, victims, and consequences of abuse | 18 |
SEXUAL DEVELOPMENT
Early Childhood: Infants, Toddlers, and Preschoolers (Aged 0 to 6 years)
PHYSICAL DEVELOPMENT
Even as infants, children are capable of sexual arousal; newborn boys have penile erections, and baby girls are capable of vaginal lubrication.14–16 Otherwise, until puberty, there is limited change in physical sexual development (including hormonal and gonad changes) during early childhood.3
SEXUAL KNOWLEDGE
Children as young as 3 years of age can identify their own sex and, soon after, identify the sex of others.17,18 Initially distinctions between the sexes are based on visual factors found in the culture (such as hair), although by age 3 or 4 years, many children are aware of genital differences.18,19 Both girls and boys have been found to be more likely to know labels of male than of female genitalia.20–22
Much of the research on sexual knowledge of preschool children was conducted before 1997.19,20,23–26 Interestingly, the same pattern of results for toddlers and preschoolers have been found in a more recent study on knowledge of genital differences, pregnancy, birth, procreation, sexual activities, and sexual abuse.18 Preschool children’s understanding of pregnancy and birth tends to be vague until age 6, when most report knowledge of intrauterine growth, a third know about the concept of fertilization, and most know about birth by cesarean or vaginal delivery. Knowledge of adult sexual behavior was most often limited to behaviors such as kissing and cuddling; only 9% of 3-year-olds mention explicit sexual behaviors, increasing to 21% for the 6-year-olds, and another 8% of 6-year-olds can give detailed descriptions of the acts. The rate of this behavior is affected by abuse: Sexually abused 2- to 5-year-olds have been found to talk more about sex than do preschool-aged children in normative samples of (33% and 2%, respectively).27
SEXUAL BEHAVIOR
Preschool-aged children are curious in general and tend to actively learn about the world through listening, looking, touching, and imitating. Children as young as 7 months have been found to touch and play with their own genitalia; this behavior is found in both sexes but is more common in boys.15,16 Infants’ and young children’s self-touch appear largely related to curiosity and pleasure seeking.3 Children aged 2 to 5 years look at others when they are nude, intrude on others’ physical boundaries (e.g., stand too close to others), touch their own genitalia even in public, and touch women’s breasts (occurring in at least 25% of normative samples27,28). Preschool-aged children’s general curiosity about the world manifests with questions and exploratory and imitative behaviors concerning sexual body parts.3 Although gender role behavior is seen as early as age 1, dressing like the opposite sex is also not unusual throughout this developmental period (14% of boys and 10% of girls).27,28 Boys demonstrate strong same-sex preferences early in the preschool years that increase in strength over time, whereas girls’ same-sex preferences, strong in the preschool years, wanes in later years.16
Nonintrusive sexual play of showing sex parts to other children was found in 9% of preschoolers, and 4.5% were reported to have touched another child’s sexual body parts (reported by mothers).27 Sexual play is discussed in more details in the next section. Culture and social context affects the incidence of these typical behaviors, inasmuch as frequencies of these behaviors have been found to differ by the population and the situation studied.29–32 Cultural effects are described in more detail later in this chapter.
Intrusive (putting finger or objects in another child’s vagina or rectum), planned, and aggressive sexual acts were not reported by anyone in a normative sample of mothers of preschool children.33 Other rare behaviors include putting objects in vagina/rectum, putting the mouth on sexual body parts, and pretending toys are having sex.29,27,32
School-Aged Children (Aged 7 to 12 Years)
PHYSICAL DEVELOPMENT
Pubertal development on average begins around 10 years of age, with girls starting earlier then boys, and can begin as early as 7 or 8 years of age. For girls, early puberty starts with a growth spurt in height, followed by a growth spurt in weight. Boys’ growth spurts are often later than girls,2 and occurs with acceleration of the growth of the testes and scrotum, enlargement of the larynx, and deepening of the voice.16 There is wide variation, affected by a variety of factors (e.g., nutrition, heredity, race), in the onset and course of puberty, including a 4- to 5-year age range for the onset of puberty.16 This variability can have significant effects on social adjustment of youth. Further information about puberty is provided later in the section on adolescent sexual development.
SEXUAL KNOWLEDGE
Knowledge of pregnancy, birth, and adult sexual activity increases during the school-age period. By age 10, most children have basic and more realistic understanding of puberty, reproductive processes, and birth.3 Accuracy of knowledge depends in part on the child’s exposure to correct informal and formal educational material.
SEXUAL BEHAVIOR
School-age children’s behaviors become more guided by societal rules, which restrict the types of sexual behavior demonstrated in public. Sexual behavior continues to occur throughout the school-age period, but it is more concealed, and thus caregivers may not be directly aware of the behavior. In contrast to younger children, school-aged children are much less likely to touch their private parts in public or women’s breasts.27 However, they are more interested in media and are more likely to seek out television and pictures that include nudity.27 Masturbatory behaviors occur, with an increase in frequency in boys during this developmental period.16 Modesty emerges during this developmental period, particularly in girls, who become more shy and private about undressing and hygiene activities.34
During the early school years, children tend to seek out and interact with children of the same sex.35 Interest in the opposite sex increases near the end of this developmental period with puberty, and interactive behaviors initiates with playful teasing of others. A small but substantial portion is involved in more explicit sexual activity, including sexual intercourse, at the end of this developmental period.36
SEXUAL PLAY
Sexual play is distinguished from problematic behaviors in that childhood sexual play involves behaviors that occur spontaneously and intermittently, are mutual and noncoercive when they involve other children, and do not cause emotional distress.1,8 Sexual play typically occurs among children of similar age and ability who know and play with each other, rather than between strangers. Interpersonal sexual play often occurs between children of the same sex and can include siblings.16,37,38 Experiencing sexual play at least once during childhood appears prevalent (reported by more than 66% to 80% of adults in retrospective research) and can occur in children as young as 2 or 3 years. Many incidents of sexual play in school-aged children may be unknown by caregivers, because the behaviors are more likely to be hidden with increased awareness of social norms.37–39 Some degree of behavior focused on sexual body parts, curiosity about sexual behavior, and interest in sexual stimulation are a normal part of child development. This type of exploratory sexual play (periodic and without coercion or force and between children of similar age/abilities) has not been found to negatively affect long-term adjustment,37,40–42 although inconsistent results have been found with sibling involvement.43
Childhood sexual play and exploration are not a preoccupation and usually do not involve advanced sexual behaviors such as intercourse or oral sex. Intrusive, planned, coerced, and aggressive sexual acts are not part of typical or normative sexual play of school-aged children; rather, they are perceived as problematic.33 SBPs are discussed more extensively later in the chapter.
Adolescent Sexual Development (Ages 13 to 19 Years)
PHYSIOLOGICAL DEVELOPMENT
During adolescence, changes associated with puberty continue, including enlargement and maturation of the genitalia and secondary sex characteristics.44 Most girls by age 16 have begun to menstruate; the average age at onset is 12 years.3,45,46 Current research indicates that Caucasian girls enter puberty approximately 1 year earlier and African-American girls approximately 2 years earlier than previous studies have shown. The mean age for the beginning of breast development (sexual maturation rating stage 2) in African-American girls has been found to be 8.87 years, and that for white girls, 9.96 years.47 By age 15, most boys are capable of ejaculation.3 About 2 years after pubic hair growth begins, there is development of axillary and facial hair, as well as an acceleration of muscular strength. Hormonal changes that occur during puberty affect sexual interest, behavior, and fantasies.48–50
SEXUAL KNOWLEDGE AND BEHAVIOR
It is expected that adolescents have knowledge about sexual intercourse, contraception, and sexually transmitted diseases.3 However, the quality of the knowledge they possess varies greatly across individuals. Evaluations of a variety of sex education programs (e.g., sex education, human immunodeficiency virus [HIV] education, teen pregnancy prevention) targeted at adolescents suggest that such programs do not lead to earlier onset of sex, more frequent sex, or more sexual partners. Many programs have been found to be associated with better outcomes for youths, including delay in the onset of sexual intercourse, increase in the use of contraceptives, and reduction in the number of sex partners. Programs more likely to affect teenagers’ behavior contain several common characteristics, including having and reinforcing messages about abstinence and/or use of contraception, focusing on reducing at least one sexual behavior that leads to pregnancy or HIV infection and sexually transmitted diseases, and providing information about the risks of adolescent sexual activity.51,52
Many studies indicate that increases in sexual behavior during adolescence are not only influenced by hormones but are also affected by social factors, including parental supervision, peer influences, and community characteristics.53–55 Several factors have been identified as being associated with the onset of sexual activity in adolescents: (1) less educated mothers; (2) having a boyfriend or girlfriend; (3) lower educational expectations (i.e., no intention of going to college); (4) authoritarian parenting; (5) poor communication with parents about sexuality; and (6) older siblings who are sexually active.45
The majority of teenagers engage in some form of sexual activity, whether masturbation or sexual intercourse. Studies have shown that 25% to 40% of adolescent girls and 45% to 90% of adolescent boys masturbate with or without sex toys like dildos.49,56 Sexual activity rates in adolescents have increased more than 79% since 1970.57 In 2003, 47% of students in grades 9 to 12 reported that they had had sexual intercourse. Of these high school students, 14% reported having had sexual intercourse with four or more partners.58 Research studies have revealed that 10% to 49% of adolescents have engaged in oral-genital contact, and the incidence is increasing.59–61 Sexual experimentation and exploration is normative and may include behaviors with same-sex peers.
Risks associated with increased and early-onset sexual activity are notable, including sexually transmitted diseases, pregnancy, substance use, and exposure to and experiences of assault and unwanted sexual experiences. Although condom use has increased, it is not consistent, and approximately 25% of sexually active youths have been found to contract sexually transmitted diseases each year.36 Furthermore, use of substances before sexual activity has increased.62 Youths are at risk for experiences of sexual assault, force, coercion, and violence.2 Other youths are often the offenders in these assaults, and information about management of adolescent sexual offenders is provided later in the chapter.
A summary of sexual development information by age group is provided in Table 25A-2.
TABLE 25A-2 Sexual Development by Age
| Development Description | Reference |
|---|---|
| Neonatal Period and Infancy | |
| Boys may have penile erections, and girls are capable of vaginal lubrication. | 14, 15 |
| Babies as young as 7 months touch their own genitalia. | 15 |
| Preschool Years (Ages 3-6 Years) | |
| Most 3-year-olds’ knowledge of adult sexual behavior is limited to kissing and cuddling, and approximately 30% of 6-year-olds know about more explicit sexual acts. | 18, 27 |
| Children identify their own sex and sex of others, initially differentiating sexes by external characteristics (e.g., hair). | 18 |
| Children are aware of genital differences of the sexes by the end of this developmental period. | 18, 19 |
| Their understanding of pregnancy and birth tends to be vague. | 18 |
| They often have questions about, as well as exploratory and imitative behaviors concerning, sexual body parts. | 3 |
| They have a vague understanding of pregnancy and birth, with some knowledge of intrauterine growth and birth by cesarean or vaginal delivery by the end of this developmental period. | 18 |
| Nudity, looking at other people’s bodies (particularly during hygiene activities), dressing like the opposite sex, and non intrusive sex play are not unusual. | 27, 28 |
| School Years (Ages 7-12 Years) | |
| Children tend to seek out and interact with same-sex children. | 3 |
| Girls become more shy and private about undressing and hygiene activities. | 34 |
| Children have a basic understanding of puberty, reproductive processes, and birth. | 3 |
| Pubertal development begins, with girls starting before boys. | 2 |
| Breast development begins in girls. | 47 |
| There is a wide variation in the onset and course of puberty. | 16 |
| Sexual behavior, including sexual play, occurs but is more likely to be concealed than during preschool years. | 3 |
| Sexual play typically occurs with children with whom they are interacting, including other children of the same sex and siblings. | 16, 37, 38 |
| Sexual play (periodic and without coercion or force and between children of similar age/abilities) has not been found to negatively affect long-term adjustment. | 37, 41 |
| Masturbatory behavior increases during this developmental period, particularly in boys. | 16 |
| Interest in the opposite sex increases with the onset of puberty. | 35 |
| Adolescence (Ages 13-17 Years) | |
| Enlargement and maturation of the genitalia and secondary sex characteristics occur. | 44 |
| Most boys by age 15 are capable of ejaculation. | 3 |
| Most girls by age 16 have begun to menstruate. | 3, 45 |
| Knowledge about sexual intercourse, contraception, and sexually transmitted diseases varies greatly across individuals. | 3 |
| Majority of adolescents engage in some form of sexual activity, whether masturbation, oral-genital contact, or sexual intercourse. | 49, 56, 58–61 |
| Experimentation and exploration of a range of sexual behaviors, including sexual behavior with the same and opposite sex, occurs. | 2, 49 |
SPECIAL TOPICS ON SEXUAL DEVELOPMENT: CULTURAL FACTORS, SEXUAL ORIENTATION, DEVELOPMENTAL DISABILITIES, AND SEXUAL ABUSE
Cultural Factors Affecting Sexual Development and Behavior
Children’s public and private sexual behavior, modesty, intimacy, and relationships are affected by their family’s and communities’ cultural values, beliefs, norms, religion, spirituality, socioeconomic, historical, and other factors. For example, social environments with norms in which nudity is acceptable, privacy is not reinforced, and exposure to sexualized material is common have been found to be related to higher frequencies of sexual behaviors in the children than are social environments that reinforce modesty and privacy.28
Parents’ attitudes toward children’s sexuality have been found to affect children’s sexual knowledge and behavior.19 Cultural beliefs may explain normative differences found in cross-cultural studies. For example, mothers of Dutch children report greater frequencies of sexual behaviors in their preschool-aged children than do mothers of American children, which may be related to a more permissive, positive attitude about sexuality and nudity in The Netherlands than in the United States.30 Cultural differences in children’s sexual knowledge (such as physiological distinctions between sexes, pregnancy, and birth) have also been found. For example, preschool-aged girls in the Western hemisphere have been found to perceive that babies were always in their mother’s bellies, whereas Asian boys thought the baby was swallowed.16
Factors may interact, and differences in regard to norms between boys and girls are not uncommon. Implicit and explicit messages about sexual behavior are provided to children and youths through family, friends, neighbors, and the community, as well as a variety of media (including television, movies, music videos, music lyrics, video games, magazines, the Internet, and communications with cell phones). How children sort out the multiple and often conflicting messages about sex, sexuality, and relationships are not clearly understood. However, reduced risk-related behaviors have been found with attentive parenting with close supervision and good communication. Entertainment television can also have a positive effect on youth knowledge, particularly when paired with good communication with parents.63 Ways in which culture may affect educational and intervention approaches are discussed later in the section on intervention.
Homosexuality
Homosexuality does not begin during adolescence. However, adolescence is the most likely time during childhood that concerns about sexuality, sexual orientation, and sexual behavior are presented to the developmental-behavioral pediatrician.
Many youths experiment with and explore a range of sexual behaviors, including sexual behavior with people of the same and opposite sex.2,49 Sexual exploration and behavior are not synonymous with sexual orientation.64 With whom youths have sexual behavior may be more strongly related to who is regularly in their social environment than with sexual orientation. Adolescents with homosexual experiences may identify themselves as having a heterosexual orientation. Furthermore, adolescents with no sexual experience or only heterosexual experiences may identify themselves as homosexual or bisexual.49
National data suggest that 2.3% of men and 1.3% of women in the United States are self-identified as homosexual.60 In the same survey, 1.8% of men and 2.8% of women described themselves as bisexual.60 Accurate prevalence rates are difficult to calculate because of the continuing stigmatization of homosexuality.64 In a survey of junior and high school students from Minnesota, approximately 88% self-identified as heterosexual, 1.6% of boys and 0.9% of girls identified themselves as either primarily homosexual or bisexual, and more than 10% were “not sure” of their sexual orientation.65 More information on homosexuality and development is available in Chapter 25C.
Children and Adolescents with Developmental Delays and Disabilities
Sexual development can be more variable when children and youth have developmental delays or disabilities or chronic medical conditions. Developmental disabilities and medical conditions may be associated with precocious or early-onset puberty (e.g., Down syndrome, traumatic brain injuries, and tumors, including hamartoma), delayed puberty (e.g., Prader-Willi syndrome), or disrupted sexual development (e.g., spinal cord injuries).3,66,67 Historically, professionals and family members have inadequately understood, accepted, and responded to sexual development in individuals with disabilities.3,67 However, as in all children, sexual arousal and sexual behaviors begins at or around birth, pubertal development with the associated sexual feelings typically occurs, and many adolescents with developmental disabilities date and are sexually active.68 Unfortunately, many youths with developmental disabilities have not been provided developmentally appropriate sexual education.67,69 Providing sex education for children with developmental delays is discussed in the section on recommendations concerning clinical care later in this chapter.
Effect of Sexual Abuse on Childhood Sexual Knowledge and Behavior
Sexual abuse affects children’s sexual knowledge, as well as their sexual behavior. Furthermore, sexually abused children have been found to have greater frequencies of a wide range of sexual behaviors in comparison with normative samples and with children who were clinically referred with no known history of sexual abuse.28,70,71 Sexually abused preschool-aged children are at greater risk for inappropriate sexual behaviors (35%) than are sexually abused school-aged children (6%).70
Although most sexually abused children do not demonstrate SBPs, the presence of SBPs raises concern about child sexual abuse and exposure to sexual material. Professionals need to be well aware of the child abuse reporting statutes in their jurisdiction, because reports of suspected sexual abuse may be necessary. Specific sexual behaviors (such as playing with dolls imitating explicit sexual acts and inserting objects in their own vaginas or rectums) are more likely to occur in children who have been sexually abused than in those who do not have a suspected history.27,30,72 The presence of sexual behavior maybe enough to suspect sexual abuse and report to authorities for investigation; however, sexual behavior itself cannot be a sole determining factor for diagnosing sexual abuse.8 Confirming sexual abuse in young children is quite complex, because often there is no physical evidence and no witnesses, and aspects of the abuse (e.g., threats by the perpetrator) hamper clear reporting by the child.73 Additional information on identification and reporting of and response to suspected sexual abuse is provided in The APSAC Handbook on Child Maltreatment (2ed) by Myers JEB, Berliner L, Briere J et al, 2002.
SEXUAL BEHAVIOR PROBLEMS
Not all sexual behavior among youth is normative or appropriate. In the following discussion, SBPs in youth are defined, with information about the prevalence, origins, and trajectory of SBPs, as well as current findings on assessment, treatment, and management. Because of developmental and legal distinctions, children with SBPs are discussed separately from adolescents.
Problematic Sexual Behavior during Childhood (Ages 3 to 12 Years)
Sexual behavior in childhood occurs on a continuum from typical to concerning to problematic.74 SBPs do not represent a medical/psychological syndrome or a specific diagnosable disorder; rather, they represent a set of behaviors that are well outside acceptable societal limits.8 SBPs in this context are defined as child-initiated behaviors that involve sexual body parts (i.e., genitals, anus, buttocks, or breasts) and are developmentally inappropriate or potentially harmful to themselves or others.1 SBPs may range from problematic self-stimulation (causing physical harm or damage) to nonintrusive behaviors (such as preoccupation with nudity, looking at others) to sexual interactions with other children that include behaviors more explicit than sexual play (such as intercourse) to coercive or aggressive sexual behaviors (of most concern, particularly when paired with large age differences between children).
Although the term sexual is used, the intentions and motivations for these behaviors may not be related to sexual gratification or sexual stimulation. Rather, the behaviors may be related to curiosity, anxiety, reenacting trauma, imitation, attention-seeking, self-calming, or other reasons.1
Children as young as 3 and 4 years of age with SBPs have been described in the literature.75–78 Girls may be somewhat more likely than boys to be referred for services for SBPs during preschool years78 and boys during the school years.79,80 However, no population-based statistics on the incidence or prevalence of SBPs in children are available. By definition, most of the sexual behaviors involved are fairly rare.28 Since the 1980s, there has been an increase in the number of children with SBPs who have been referred for child protective services, juvenile services, and treatment in both outpatient and inpatient settings.81 The increase in referrals may represent an actual increase incidence of such behaviors, changing definitions of problematic sexual behavior, improved awareness and reporting of what has always existed, or some combination of these factors.8
The prevalence of sexual behavior for specific races, ethnic groups, religious groups, and socioeconomic groups is unknown. In groups in which there are extremely high rates of sexual abuse at a young age, the children are at higher risk for developing problematic sexual behaviors.
ORIGINS OF SEXUAL BEHAVIOR PROBLEMS IN CHILDREN
Social context, individual characteristics, disruptive experiences, and the interactions of these factors affect the course of sexual development.9 Sexual abuse is one type of disruptive experience affecting sexual development. Children, particularly preschool age children,70 who have been sexually abused are more likely to demonstrate SBPs than are children without such a history.28 However, many children with SBPs have no known history of sexual abuse.76,78,79,82 The development of SBPs appears to have multiple origins, including exposure to family violence, physical abuse, parenting practices, exposure to sexual material, absence of or disruption in attachments, heredity, and the development of other disruptive behavior problems.33,83–85 For some children, SBPs may be one part of an overall pattern of disruptive behavior problems,83,86,87 rather than an isolated or specialized behavioral disturbance.
RISKS AND COMORBIDITY OF SEXUAL BEHAVIOR PROBLEMS
Regardless of the causal pathway, a young child’s demonstration of SBPs is associated with a variety of negative consequences in adjustment and development. Trauma histories and related trauma symptoms are common, particularly in young children with SBPs.78,87 Children with SBPs often exhibit other behavior problems and disruptive behavior disorders.78,79,84,87,88 Poor impulse-control skills, aggressive behaviors, and inaccurate perceptions of social stimuli hinder social relationships and cause problems at school.9,79,88–90 Socialization difficulties and stigmatizing responses from peers and adults may impede developing self-concepts.91 Poor boundaries and indiscriminate friendliness may increase risk of future victimization.78,92 Furthermore, children with SBPs are at risk of separation from parents and of placement disruptions.78,79,93,94
CLASSIFICATION
There is much to be learned about subtypes of SBPs, because the research in this area is limited to a few studies. Youths with more frequent and more intrusive SBPs are more likely to have other behavior and emotional problems, to have caregivers with histories of trauma, and to have learning difficulties than are children with less frequent or nonintrusive sexual behaviors.95,96 Typological examinations of comorbidity have suggested the differential effects of trauma and disruptive behavior, as well as gender’s effect on rate of sexual behaviors.87 Otherwise, how types of SBPs affect the functioning of the children demonstrating the behavior, the trajectory of SBPs and related concerns, and responsiveness to interventions are unknown.
EFFECT OF SEXUAL BEHAVIOR PROBLEMS ON OTHER CHILDREN
When children experience sexual behaviors initiated by other children, there can be a range of effects. The literature is scant but appears to suggest that sexual behaviors between children of similar age and ability that was of mutual agreement and without intrusive or aggressive behaviors is retrospectively viewed as neutral or positive. However, when the sexual behavior experienced is considered to be an SBP as previously defined, the experience can have potentially negative effects, perhaps similar to those of sexual abuse perpetrated by adolescents or adults. The research on the effect of child sexual abuse indicates that the level and severity of the effect are influenced by the duration; frequency; relationship with the initiator of the sexual acts; use of aggression, coercion, or force; the child’s previous functioning; and the response and support by the caregivers.97 Response can range from no or limited discernible symptoms to the development of trauma symptoms, other internalizing symptoms, behavior problems, sexual behaviors themselves, and/or social and peer problems.
ASSESSMENT OF SEXUAL BEHAVIOR PROBLEMS (AGES 3 TO 12 YEARS)
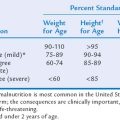
When caregivers report concern about the sexual behavior of children, an initial screening can facilitate the need for further clinical assessment. Gathering information about the type, frequency, duration, level of intrusiveness, harm, use of coercion, and course of behaviors can facilitate distinguishing typical from problematic sexual behaviors. The Child Sexual Behavior Inventory (CSBI)27 is the only norm-based parental report measure of child sexual behavior with gender and age norms for ages 2 to 12 years. It is a 38-item measure used to assess boundary issues, showing of private parts, self-stimulation, sexual anxiety, sexual interest, sexual knowledge, interpersonal and intrusive sexual behavior, and looking at others’ private parts. It is easy to administer and score; the Total Scale Score provides a T-score and a percentile that are based on age and gender norms. The published manual recommends that the CSBI be administered by mental health professionals with training in psychological assessments. It is important to note that this published version does not include any items concerning sexual aggression. Friedrich33 evaluated four such items and found none of them to be endorsed by mothers in a normative sample. Friedrich also provided a checklist to assess exposure to sexualized material, supervision, and privacy, which facilitates developing a safety plan with the family.33
Assessment of the situations or circumstances under which SBPs seem to occur, the social ecology, exposure to sexualized materials, and success of attempts made to correct the behaviors can guide identifying points of intervention and treatment recommendations. The Child Sexual Behavior Checklist, 2nd revision, can help assess contributing factors and identify environmental intervention area, as it lists 150 behaviors related to sex and sexuality in children, asks about environmental issues that can increase problematic sexual behaviors in children, gathers details of children’s sexual behaviors with other children, and lists 26 problematic characteristics of children’s sexual behaviors.98 However, the no norms have been published for the Child Sexual Behavior Checklist.
Comorbid disruptive behavior disorders, affective disorders, trauma-related symptoms, and learning deficits are not uncommon in children with SBPs.78–80,84,87 Thus, a broad assessment is warranted and may include such measures as the Child Behavior Checklist (which includes items on sexual behavior),99,100 or the Behavior Assessment System for Children.101 To specifically assess trauma symptoms, the Trauma Symptom Checklist for Children (child report) and the Trauma Symptom Checklist for Young Children (caregiver report) are useful instruments that include subscales related to sexual concerns.102,103 For preschool children, the Weekly Behavior Report104 is useful in assessing a wide range of emotional and behavior problems, including SBPs, and in tracking progress over time.
A common misunderstanding is that if a child has SBPs, he or she must have a history of sexual victimization. Although a history of previous or ongoing sexual abuse increases the risk for developing SBPs,70,72 there appear to be multiple pathways to the development of SBPs, and the presence of SBPs should not be presumed sufficient evidence of sexual abuse. However, when a child exhibits SBPs, it is appropriate for assessors to make direct inquiries into whether the child has been or is being sexually abused.8 Suspected sexual abuse that had not been previously investigated by Child Protective Services necessitates responses consistent with state and regional child abuse reporting statutes. Additional information on management of suspected child sexual abuse is available in The APSAC Handbook on Child Maltreatment (2ed) by Myers JEB, Berliner L, Briere J, et al, 2002.
CASE EXAMPLE
A description of the application of these measures and assessment procedures to a case may facilitate application of the information. An example case of a young child follows:
Jill Doe is a 6-year-old girl who was referred by Child Protective Services after their investigation into possible sexual abuse. Their investigation was inconclusive. There were continued concerns regarding her sexual behaviors. Jill lives with her father and 3-year-old sister. She has sporadic visitations with her mother, who has a substance abuse problem. Jill’s father provided the history of sexual behavior, in which he reported that Jill was found on top of a 4-year-old girl, kissing her and touching her genital area over the clothes. This behavior was followed by observing her embracing and kissing two different young boys at a local park. A couple of months ago, she was found to be making her dolls “have sex,” upon which her father responded by taking the dolls away. Around that time, she also found Jill visually examining her 3-year-old sister’s vaginal area and touching their dog’s private parts. All of these sexual behaviors have continued despite the father’s efforts to stop the behaviors through distraction, removal of toys, and punishment (grounding). In addition to these sexual behaviors, Jill’s father expressed concern about Jill’s sleep problems, nightmares, moodiness, and temper tantrums.
Jill’s father completed the CSBI and Child Behavior Checklist. On the CSBI, he endorsed items reflecting the sexual behaviors noted previously and the Total Standard Score of 23, which falls at the T-score of 108, in the clinical range. Thus, the sexual behaviors Jill has been exhibiting according to her father’s report are much greater in frequency than those of the normative sample of girls her age. Problems were noted in regard to boundaries and interpersonal sexual behavior problems. The Safety Checklist suggested that Jill has been exposed to sexualized materials while in her mother’s care. Furthermore, she often sleeps and bathes with her sister and, at times, her cousins. Jill was reported to have been exposed to violence and substance use. The Child Behavior Checklist scores were 68 for Total Problems, 67 for Externalizing Problems, and 65 for Internalizing Problems. The Weekly Behavior Report indicated that Jill is exhibiting sexual behavior problems a couple of times a week, as well is experiencing nightmares and temper tantrums four times a week. Services for sexual behavior problems and integrating strategies to address behavior problems, nightmares, and abuse prevention skills appear warranted. Work with the caregivers regarding privacy rules, boundaries, and protection from trauma and stress is also indicated. The Weekly Behavior Report measure is brief enough that frequent administration is not burdensome and can track treatment progress.
TREATMENT FOR SEXUAL BEHAVIOR PROBLEMS (AGES 3 TO 12 YEARS)
SBPs have been successfully treated with SBP-specific therapy services for school-age children and preschool children.8,79,105,106 Further, Trauma-Focused Cognitive Behavior Therapy as a treatment for the effects child sexual abuse that includes SBP-specific elements effectively reduces SBPs in sexually abused preschool-aged children.107–110 These treatments have been found to be more effective than time (wait periods), play therapy, and nondirective supportive treatment approaches. The types of SBPs found in the children involved in the studies have been wide ranging, with most children demonstrating interpersonal sexual behaviors, and include aggressive sexual behaviors.
One study provided results from a 10-year follow-up on children with SBPs who had been randomly assigned to receive group cognitive-behavioral treatment (CBT) or group play therapy. The study included a clinic comparison group of children with disruptive behavior problems but no SBPs.105 Child welfare, juvenile justice, and criminal administrative data on all the children were collected and were aggregated. The CBT recipients were found to have had significantly fewer future sex offenses than the play therapy recipients (2% vs. 10%) and did not differ from the general clinic comparison (3%).105 The overall rate of future sexual offenses not only was quite low with short-term outpatient CBT that involved families but also was indistinguishable from that of the comparison sample.
Common elements of the effective treatments are outpatient, short-term, cognitive-behavioral and educational approaches; caregiver direct involvement; teaching of rules about sexual behaviors and skills to facilitate maintaining these rules (such as feeling identification, impulse control, and problem-solving skills); sex education; and teaching caregivers efficacious behavior management strategies (such as praise, reinforcement, timeout, and logical consequences). This treatment should be distinguished from CBT approaches to treating adolescent and adult sexual offenders. Efficacious treatment for childhood SBPs have not included components more characteristic of treatment of adults, such as concepts of grooming, offense cycles, predation, or use of techniques such as confrontation or arousal reconditioning.105 For children who have histories of sexual abuse and trauma-related symptoms, a trauma-focused CBT approach that includes SBP-specific strategies has been successful.111–113
For some children, the SBP may be part of a general pattern of disruptive and oppositional behaviors. Research on treatment for disruptive behaviors has consistently identified behavior management training as an effective modality.114,115 Integrating SBP-specific treatment components with well-supported treatment models for early disruptive behavior disorders (such as Parent-Child Interaction Therapy,114 The Incredible Years,116 Barkley’s Defiant Child protocol,117 or the Triple P program118) might be considered; however, this approach has yet to be tested in regard to reducing SBPs.
The presence of attention-deficit-hyperactivity disorder is not uncommon in these youth,106 and appropriate treatment is warranted to facilitate control of impulsive behaviors (see Chapter 16). In cases of neglectful, conflicted, or chaotic family environments, interventions focused on creating a safe, healthy, stable, and predictable environment may be the top priority.119 For cases in which insecure attachment is a major concern, short-term interventions emphasizing parental sensitivity have been found to be the most effective.120 Family-based attachment-based treatment may be considered for complex cases involving significant family relationship concerns, as well as comorbid conditions,86 although this approach has yet to be empirically validated.
Problematic Sexual Behavior during Adolescence
Adolescent sexual offenders are adolescents between the ages of 13 and 17 years who commit sexual behavior that is illegal as defined by the sex crime statutes of the jurisdiction in which the offense occurred.121 In general, the legal system (i.e., family or juvenile court, probation officer, judge, district attorney) is involved when an adolescent commits a sexual crime, because of the adolescent’s assumed culpability in committing the crime. The response of the legal system to an adolescent’s sexual crime varies greatly by state and may include court-ordered treatment, probation, imprisonment in a juvenile or adult correctional facility, and/or inclusion in registrations and public notification systems. Approximately one third of sexual offenses against children are committed by adolescents. Sexual offenses against children younger than 12 years tend to be committed by boys aged 12 to 15 years.122,123 The majority of adolescent sexual offenders are male, accounting for 93% of all juvenile arrests for sex offenses, excluding prostitution.124
ORIGINS OF SEXUAL BEHAVIOR PROBLEMS IN ADOLESCENTS
Adolescents with SBPs are a heterogeneous population.125,126 Although it is commonly believed that adolescent sexual offenders were sexually abused themselves, most in fact were not childhood sexual abuse victims.127,128 Some differences in maltreatment history between adolescent boys and girls with SBPs have been found. Adolescent girls with SBPs have been shown to have more severe physical and sexual abuse histories than have adolescent boys with SBPs. For adolescents with SBPs and who have been sexually abused, the girls tended to be sexually abused at younger ages and were more likely to have been abused by multiple perpetrators.127–131 There appears to be multiple origins, including abuse history, family stability, and psychiatric disturbances in the development of SBPs in adolescence; however, for many adolescents, there is no known cause.10
RISKS, COMORBIDITY, AND TYPOLOGY
Although professionals have proposed subtypes of adolescent sexual offenders, these subtypes have not yet been confirmed in the literature. What is known is that adolescent sexual offenders are diverse. There are adolescent sexual offenders with few other behavioral or psychological problems and those with many nonsexual behavior problems or other (nonsexual) delinquent offenses. Some have psychiatric disorders. Some adolescent sexual offenders come from well-functioning families; others come from poorly functioning or abusive families.10 Adolescents with SBPs tend to have poorer social skills, more behavior problems, learning disabilities, depression, and impulse control problems in comparison with nonoffending adolescents (see Becker125 for a review). Some differences have been found between adolescents who rape peers and those whose sexual behavior is with younger children. Adolescents whose sexual behavior is with younger children have been found to be younger, to be less socially competent, to have less same-age sexual activity, to be more withdrawn, and to have fewer nonsexual behavior problems than do adolescents who rape peers.132,133 Risk predictors that have been identified for sexual and nonsexual repeated offending, include antisocial tendencies, psychopathy, and larger numbers of victims.134
CONTRASTING ADOLESCENTS WITH SEXUAL BEHAVIOR PROBLEMS WITH ADULT SEXUAL OFFENDERS
Adolescents are different from adult sexual offenders in several important ways: (1) Adolescents are considered more responsive to treatment than are adults135; (2) of sexual offenders who receive treatment, adolescents have a lower sexual recidivism rate than do adults136; (3) adolescents have fewer victims and tend to engage in less aggressive behaviors than do adults137; and (4) most adolescents do not meet the criteria for pedophilia.138 With regard to recidivism, adolescent sexual offenders are less likely to have sexual repeated offenses and are more likely to have nonsexual repeated offenses than are adults.139
ASSESSMENT OF ADOLESCENTS
There are no psychological tests available that can establish guilt or innocence of committing a sexual offense. However, there are some measures under development to assess the risk of future sexual offenses of adolescent sexual offenses. The National Center on Sexual Behavior of Youth (www.ncsby.org) provides more guidelines about assessment of adolescent sexual offenders.
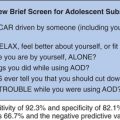
For adolescents with histories (e.g., maltreatment, life stressors, behavior problems) that make it more likely that they will engage in high-risk sexual behaviors or have sexual concerns, it is important for clinicians to assess their sexual practices and concerns to guide intervention. The Adolescent Clinical Sexual Behavior Inventory (ACSBI) can be used as a screening tool with such adolescent clinical samples. The ACSBI has parent- and self-report versions (45 items each), responses to which can provide information about adolescent’s high-risk sexual behavior and help determine appropriate interventions. The ACSBI measures a range of sexual behaviors and yields five factors: sexual knowledge/interest, divergent sexual interest, sexual risk/misuse, fear/discomfort, and concerns about appearance.140
TREATMENT FOR ADOLESCENT SEXUAL OFFENDERS (AGED 13 TO 17 YEARS)
Rigorous research regarding treatment of adolescent sexual offenders is lacking. However, there is some evidence to support the use of sex offender–specific treatment for adolescent sexual offenders. Two randomized clinical trials with small sample sizes yielded results in support of the use of multisystemic therapy with adolescent sexual offenders. Multisystemic therapy is a home-based treatment intervention that targets the systems in which youth are embedded, as well as the factors that are associated with delinquency. Results from these studies indicated that youths who received multisystemic therapy had lower rates of sexual and nonsexual recidivism than did youths who received the usual services (e.g., individual or group treatment).139,141,142 On the basis of what is known about juvenile sex offenders, state-of-the-art treatment recipients should include caregivers, so that relevant factors (e.g., parental monitoring and engagement) associated with delinquent behavior can be addressed.139 Because of the low rates of pedophilia among adolescent sexual offenders, it is generally inappropriate to apply adult sexual reconditioning techniques to adolescent sexual offenders. The widely held belief that most adolescent sexual offenders will become adult sex offenders is not supported by research.135
RECOMMENDATIONS CONCERNING CLINICAL CARE
Parent Education and Clinical Management: Children (Aged 3 to 12 Years)
Concerns about sexual behavior of youth may manifest in a variety of ways in the medical office. During assessment of a wide range of behavior problems, concerns about respect of other’s boundaries and sexual acts may arise. As sexual behavior, particularly in young children, often raises suspicion of sexual abuse, such children’s caregivers may express concern about possible victimization of the child. Families and other professionals may seek advice for follow-up and management once SBPs have been identified.
Parents are generally interested in and expect pediatricians to discuss normal sexuality and sexual abuse prevention.143 When there are concerns about SBPs, information provided depends on the results of the initial screening and, if warranted, further evaluation. In determining whether sexual behavior is inappropriate, it is important to consider whether the behavior is common or rare for the child’s developmental stage and culture, the frequency of the behaviors, the extent to which sex and sexual behavior have become a preoccupation for the child, and whether the child responds to normal correction from adults or whether the behavior continues after normal corrective efforts.119 In determining whether the behavior involves potential for harm, it is important to consider the age/developmental differences of the children involved; any use of force, intimidation, or coercion; the presence of any emotional distress in the children involved; whether the behavior appears to be interfering with the children’s social development; and whether the behavior causes physical injury.9,144,145
Parent education may include information about typical sexual development and how to distinguish SBPs from sex play; specific instructions for reducing exposure to sexually stimulating media or situations in the home; instructions for monitoring interactions with other children; suggestions for how parents should respond to sexualized behaviors; and teaching children rules about privacy, sexual behavior, and boundaries.119,146
Parents and caregivers often are understandably concerned about the causes of the SBP. In some cases, there appears to be relatively clear sequence of events that explain the development of the SBP (such as young child’s being sexually abused by an uncle, followed by the child’s repeating the behavior with another child at daycare). However, such direct pathways are often not present, inasmuch as causes for human behavior can involve the interplay of multiple factors, and may not be fully knowable.8 Parents can be reassured that children with SBPs can be treated successfully without clear evidence of the origins of the behavior, with the exception of situations of ongoing sexual abuse.
Ongoing sexual abuse is of serious concern, both for the child’s welfare and for the success of intervention efforts. Indeed, subsequent sexual abuse appears to increase the likelihood of future SBPs.105 In cases in which the Child Protective Services investigation of sexual abuse yields inconclusive results, interventions focused on educating children about sexual abuse, identifying whom children may tell if they were being abused, having significant adults support this message, and building support systems around the child have been recommended.73 Repeated questioning and interviewing the child after thorough investigations are not recommended, because they may lead to inaccurate information and have potential deleterious effects on the child.119
Other parental concerns often relate to the misunderstanding about the meaning of childhood SBPs and likelihood of problematic adult sexual behavior, including pedophilia. The results of a 10-year prospective study of children with SBPs indicated low rates of future sexual offenses (2% to 10%, depending on treatment type).105 A continuation of SBPs from childhood into adolescence and adulthood appears rare. Calm parental responses to these situations are advised.147 Efficacious treatments have been outpatient and short-term and have involved helping the children while living in their natural environment and while attending school. Restricted environments and treatments should be reserved for children who pose immediate risk because of coercive, aggressive, harmful sexual behavior that has not been readily modifiable with appropriate parental interventions and treatment.8
Resources are available to professionals in their work with parents. Fact sheets addressing typical sexual development, SBPs, and common misconceptions about child with SBPs can be found on the Website of the National Center on the Sexual Behavior of Youth (www.ncsby.org). An information booklet on child sexual development and SBPs145 is useful to supplement education for the caregivers (www.TCavJohn.com). Anticipatory guidelines on issues related to sexual development and behavior throughout childhood and adolescents with information on ways to approach issues of sexual development, sexuality, sexual behavior, and sexual abuse prevention designed for pediatric practice are available.2,147 In addition, the report from the Task Force on Children with Sexual Behavior Problems of the Association of the Treatment of Sexual Abusers is a useful resource for professionals (www.atsa.org).8 This report provides more a detailed review of the research and guidelines on the identification, clinical assessment, treatment, and policy issues relevant to children with SBPs.
Parent Education and Clinical Management: Adolescents (Aged 13 to 17 Years)
Caregivers and referring providers may need support in how to address sexual topics with youth. Furthermore, because of the sensitive and, at times, taboo nature of the topic, cultural considerations and sensitivity are necessary in approaching and educating about sexual matters. Guidelines for pediatricians and family practitioners on assessment and management sexual topics with adolescents and caregivers are available.2,6,147 Caregivers often require education in addition to the youth. Helpful resources for caregivers can be found at www.advocatesforyouth.org and www.talkingwithkids.org.
When an adolescent is suspected of engaging in illegal sexual behavior, providers need to respond in a manner consistent with the reporting requirements for their state, including reporting suspected illegal sexual behavior with children as indicated. Developmental-behavioral pediatricians can help caregivers and adolescents by referring youths for clinical assessment and efficacious treatment when available.
Unfortunately, efficacious treatment is not available in all areas of the United States. If efficacious treatment is not available, then the developmental-behavioral pediatrician should look for cognitive-behavioral treatment programs that involve both adolescents and caregivers and do not use adult sex offender treatment interventions (e.g., penile plethysmograph, polygraph) that may be inappropriate for adolescents.
Typically, adolescent sexual offenders can be treated in the community in outpatient treatment programs. Most adolescent sexual offenders can remain in the community with appropriate supervision by caregivers and probation officers and can be treated on an outpatient basis.135 In general, adolescent sexual offenders who are being treated in the community can attend school and engage in other activities, such as team sports and church. However, a small number of adolescent sexual offenders may need a higher level of care (i.e., residential or custodial placement).
Currently, there is no scientifically supported test to determine which adolescent sexual offenders are at high risk for recidivism. Usually, it is appropriate to treat an adolescent sexual offender as being at low risk for recidivism and in an outpatient setting, unless there is evidence that they are at higher risk. There are clinical guidelines to help identify youths at higher risk in order to help determine the level of care (outpatient vs. residential) that they may require. These factors are important in determining risk: (1) a history of multiple sexual offenses, particularly if sexual offenses continue despite appropriate treatment; (2) a history of multiple nonsexual juvenile offenses; (3) sexual attraction to children; (4) noncompliance with an adolescent sexual offender treatment program; (5) other “self-evident risk signs,” including significant behavior problems and stated intent to commit repeated sexual offenses; and (6) caregivers’ not providing the appropriate and recommended supervision and/or caregivers who are not compliant with treatment or probation.121
Collaboration with Family and Other Professionals and Agencies (Ages 3 to 17 Years)
As discussed in Chapter 8A, family-centered and collaborative approaches to service delivery are crucial for all children with developmental and behavioral needs. This is particularly true for children with SBPs and adolescent sexual offenders, for whom not only parents and caregivers but also other treatment providers, child welfare workers, schools, child care providers, juvenile justice staff, and court officials are involved in the care. The extent of collaboration and who may need to be included can be expected to vary considerably across cases. Main purposes of coordination and information sharing are to define service goals, articulate a clear plan and timetable of specific tasks needed to reach those goals, identify who on the team is responsible for each aspect of the plan, and evaluate plan implementation and goal attainment.8
OTHER RELEVANT TOPICS
Homosexuality
The sexual behavior of youth who identify themselves as gay, lesbian, or bisexual or who report homosexual or bisexual experiences are to be assessed with sensitivity and with nonjudgmental response and information. Education and intervention (e.g., information about relationships, decision making, self-care, reproduction, sexually transmitted diseases, protection) similar to that given to heterosexual youths often needs to be provided. In addition, the clinician should also be aware of the increased risk for other problems in homosexual or bisexual youths. These youths may feel extremely isolated from their peers and/or families and may have been the victims of violence and harassment.148 Nonheterosexual youth are at higher risk for behavioral and emotional problems and risky behaviors, including drug use and abuse, self-harm, school problems, and suicide.2,149 The American Academy of Pediatrics’ Committee on Adolescence’s clinical report on sexual orientation and adolescents provides useful information and guidelines for the care and support of youths.64
Children and Adolescents with Developmental Delays and Disabilities
In addition to the typical topics for sexual education, youths with disabilities may need focused information on ways to express physical affection, with whom, and under what circumstances, with an understanding of the youth’s need for intimacy and affection. Because of the increased risk of sexual abuse of such children, education should include sexual abuse prevention components. Self identity, developing relationships, and intimacy are important areas neglected in many sexual education programs for all youths. Caregivers and providers can be encouraged to provide guidance and education based on individual learning styles and disability-specific challenges, considering the use of visual supports (e.g., pictures, dolls), repeating information over time, and having the youth demonstrate or practice the information learned.2,67 Issues of consent, marriage, and family planning are complicated and require collaborative care and an understanding of individuals’ desires, choices, capabilities, supports, and needs. Curriculum on sex education for children and youths with disabilities are available150 (see also the University of South Carolina Center for Disability Resource Library at http://uscm.med.sc.edu/CDR/sexualeducation.htm), as well as other useful information including one from the American Academy of Pediatrics.67,151
Cultural Factors Affecting Parental Education and Other Service Provision
Consideration of the child and family’s cultural values, beliefs, and norms are of foremost importance in the provision of any mental health and social services. Race, ethnicity, religion, spirituality, socioeconomic factors, and other cultural factors can strongly affect individuals’ and families’ receptivity and response to treatment of child SBPs. Professionals are advised to account for the effect of the specific social ecology experience of the child. Significant variation among children exists, inasmuch as cultural and social context, as well as family attitudes and educational practices, affect children’s knowledge and behavior.18,19,30
Because of the sensitive nature of the topic, clinicians must become knowledgeable about the family’s and community’s beliefs, values, traditions, and practices concerning sex, including the spoken and unspoken rules about public and private behavior, relationships, intimacy, and modesty. For example, discussions on sexual behavior with children may be considered appropriate for some individuals (e.g., aunts teaching nieces) but taboo for others (e.g., fathers talking with daughters). Provision of education in a manner consistent with the culture and family beliefs are recommended. African-American mothers have been found to integrate story telling in process of providing sex education.152 Storytelling is also integral for American Indron Alaska Native, and Native Hawaiian families.153 Beliefs about the appropriateness of children’s touching their own private parts and about masturbation tend to be strong and directly affect receptiveness to treatment. Understanding and respecting the cultural beliefs and values of families and providing services to enhance the family’s ability to accept and receive the services is crucial not only for outcome but also for initiation and retention of families in services.
FUTURE DIRECTIONS
Although research on children and adolescent sexual knowledge began decades ago, research on children and adolescents with SBPs is a relatively new area of research. There remain many questions about knowledge and behavior of children and adolescents, particularly in the origins, typology, course, assessment, treatment, and long-term outcome for children and adolescents with SBPs. The following sections address some of the methodological challenges to research on the sexual knowledge and behavior of children and youth, as well as recommendations for future research.
Methodological Issues
Conducting research on the sexual knowledge and sexual behavior of children and youth has multiple challenges. Parents who allow their young children to participate in research on sexual knowledge may have distinct values and parenting practices from those who do not allow their children to participate. In one study, researchers noted that the majority of parents approached chose not to have their child participate; the concern about topic reported was the reason for declining.18 The unknown effect of participation bias limits the generalizability of results.
Much of the research on children’s sexual behavior has relied on caregivers’ or teachers’ reports. Self-reports of sexual behavior from adolescents suggest higher prevalence of sexual behaviors and sexual assaults than has been detected by administrative systems (such as child protective services, juvenile court system). Furthermore, retrospective research with adults suggests that caregivers are often unaware of sexual behavior that occurs among children. Retrospective research, although useful, relies on the memory of the adults, which is affected by a variety of factors. Administrative data sources track only the more severely maladaptive sexual behaviors and are also subjected to a variety of biases. The hidden nature of the sexual behavior of youths, particularly school-aged children and adolescents, challenges direct observations. Direct questioning of children and even adolescents about their sexual behavior is often restricted, particularly in the United States. Thus, reliable and valid information about children and adolescents sexual behavior is difficult to obtain, which further affects researchers’ ability to track and examine factors that affect the trajectory of sexual behaviors.
Examination of treatment efficacy for SBPs of children and adolescent poses additional challenges. Because of the concerns about the ramifications of ongoing SBPs, randomized trials with no treatment or placebo control conditions are generally considered unethical. Quasi-experimental designs and preintervention/postintervention evaluations limit clinicians’ ability to progress in understanding intervention efficacy. Randomly assigning children to receive one of two treatments when both interventions are believed to be efficacious requires a considerable sample size, perhaps multisite studies, to determine differences in effect sizes.
Recommendations for Future Research
Even basic information about SBPs in children and adolescents, such as prevalence and incidence data, is unavailable. National data on the incidence, prevalence, and frequency of types of sexual behaviors in children and youth would greatly enhance the literature. Clear, consistent definitions of types of sexual behaviors are necessary. Furthermore, because no single state or federal agency is designated as responsible for assessing and responding to sexual behavior of youths, the collection of incidence and prevalence data is challenged.
There is considerable research to be done in the area of clinical assessment of children and adolescents with SBPs. The CSBI88 is the only norm-based measure of sexual behaviors of youth and is quite useful for clinical assessment, as well as monitoring treatment progress. The published version of the measure does not include items to assess aggressive or coercive sexual behaviors; however, Friedrich evaluated four such items after the published measure.33 The published norms are based predominately on data from Caucasian and African-American children. Cross-cultural research with normative data from other populations is needed. No norms are available for the accompanying Safety Checklist.33 The Child Sexual Behavior Checklist98 includes items that assess broad issues such as environmental factors, in addition to specifics about the types and other details about SBPs. Although the measure is clinically useful, no norms have yet been published. Research is also needed in how to sensitively and culturally appropriately measure children’s sexual thoughts and understanding of their sexual behaviors.
There is one measure of adolescent sexual behavior: the ACSBI.140 This is a useful measure for clinically referred adolescents and can help guide treatment. However, there is no normative sample for this measure. The clinical sample used for development was primarily white and of middle to upper middle socioeconomic status. Research on normative sexual behavior of adolescents, including cross-cultural and economically diverse samples, is needed. One important assessment question is estimating the likelihood of sexual and nonsexual repeated offense. Although there are some adolescent sexual offender actuarial systems under development, this is still an area for continued research.
An untapped area of measurement concerns the caregivers’ knowledge of, reaction to, and perception of their child and the sexual acts. Mothers’ emotional reaction and support has been found to mediate treatment outcomes for preschool- and school-aged sexually abused children.107,154,155 Clinically, caregivers’ perceptions of their children who have demonstrated SBPs appear to strongly affect their willingness to support the child, engage in services, and respond to intervention. Psychometrically supported measures of caregiver’s emotional reaction to, support of, and perceptions for this specific population would facilitate research in this area.
Origins, trajectory, risk factors, and treatment outcome probably vary for subgroups of children and adolescents with SBPs. Typologies have been proposed on the basis of the types of sexual behavior exhibited, as well as other factors (such as gender, comorbid conditions and nonsexual delinquent acts). No clear classification has yet emerged to advance understanding in this area.
Additional research on such service factors as group versus individual/family services, use of direct practice of skills with families in session, and need of specific components of treatment (such as acknowledging past SBPs) would advance the field. Because of the low base rates of subsequent sexual offenses in children,105 it is unlikely that refined services would significantly lower this rate any further. However, researchers could examine improvements of less severe sexual behaviors, receptivity of services by families, reduced treatment burden, treatment attrition, comorbid symptom relief, and gains in coping skills and resiliency factors.
Research on services in more restrictive settings (i.e., inpatient and residential interventions) for children and adolescents with persistent, aggressive SBPs is limited to clinical descriptions and quasi-experimental designs. These youths are also more likely to have histories of severe trauma, comorbid conditions, and problematic family histories and situations (e.g., mental illness, substance abuse, maltreatment, community and domestic violence).
Many youths with SBPs have comorbid conditions of post-traumatic stress disorder, separation anxiety, and/or disruptive behavior disorders (including oppositional defiant disorder, attention-deficit/hyperactivity disorder, and conduct disorder). Although evidence-based treatments exist for each of these conditions, research on the most efficacious and efficient manner to integrate these services for children with comorbid conditions, in such a way that it is also palatable for families, is needed.
In many ways, the treatment outcome research on children with SBPs is more advanced than the research literature on adolescent and adult sex offender treatment outcomes. Only investigations of multisystemic therapy have amassed any controlled trial data with adolescents. Thus, many treatment questions remain. Comparisons of community-based treatments with residential treatment are particularly important, in view of the possible iatrogenic effects of residential placement.
The results of the prospective studies on children and adolescents with SBPs are encouraging but limited to a few studies focusing on administrative data sources. Longitudinal research integrating administrative data with self- and caregiver-disclosed rates of SBPs, other delinquent acts, victimization, and trauma experiences is warranted. Preschool-aged children with SBPs have been found to have much more frequent SBPs, more severe comorbid conditions, and greater rates of placement disruptions than do school-aged children with SBPs.78 Trajectories of nonsexual disruptive behaviors (particularly physical aggression) have been found to be distinct, depending in part on age at onset, wherein a younger onset is related to more severe and pervasive problems (e.g., Broidy et al156). Longitudinal research with preschool- as well as school-age onset of SBPs would facilitate the examination of whether SBPs have a pattern similar to that of other disruptive behaviors.
In summary, initial results in this relatively new area of research are encouraging, but further research is warranted for prevalence and incidence data, assessment, typology, treatment mediators and outcome, and longitudinal trajectories.
SUMMARY
Children are sexual beings from birth, capable of sexual arousal and behavior even as infants. Sexual knowledge and behavior are affected not only by physiology but also by family, culture, and societal factors. Curiosity and exploratory play are typical in early childhood. Sexual activity and risky sexual behaviors increase throughout childhood, particularly with the onset of puberty. Sensitivity in provision of care is recommended, particularly for populations who have experienced disparities in health care, including nonheterosexual youths, individuals with disabilities, and individuals from nondominant cultures.
SBPs are, by definition, deviations from the normal course of sexual development and have been found in children as young as 3 years of age. Sexual abuse is a significant risk factor for the development of SBPs, but multiple factors appear to contribute to the onset and maintenance of SBPs, including exposure to family violence, physical abuse, parenting practices, exposure to sexual material, absence of or disruption in attachments, heredity, and comorbidity (including disruptive behavior disorders and trauma-related symptoms). Most children and youth with SBPs can be successfully treated in their community with outpatient services. Collaborative care is crucial for the success of interventions.
1 Silovsky JF, Bonner BL. Sexual behavior problems. In: Ollendick TH, Schroeder CS, editors. Encyclopedia of Clinical Child and Pediatric Psychology. New York: Kluwer Press; 2003:589-591.
2 Duncan P, Dixon R, Carlson J. Childhood and adolescent sexuality. Pediatr Clin North Am. 2003;50:765-780.
3 Gordon BN, Schroder C. Sexuality: A Developmental Approach to Problems. New York: Plenum Press, 1995.
4 Lipsius SH. Normal sexual development of children: Physician roles in bridging gaps in parent-child communication. Md Med J. 1992;41:401-405.
5 Smith M. Pediatric Sexuality: Promoting normal sexual development in children. Nurse Pract. 1993;18:37-44.
6 Thornton AC, Collins JD. Teaching parents to talk to their children about sexual topics. Clin Fam Pract. 2004;6:801-819.
7 Horner G. Sexual behavior in children: Normal or not? Pediatrics. 2004;18:57-64.
8 Chaffin M, Berliner L, Block R, et al. Report of the ATSA Task Force on Children with Sexual Behavior Problems. Beaverton, OR: Association for the Treatment of Sexual Abusers, 2006.
9 Araji SK. Sexually aggressive children: Coming to understand them. Thousand Oaks, CA: Sage Publications, 1997.
10 Chaffin M, Letourneau E, Silovsky JF. Adults, adolescents and children who sexually abuse children. In: Berliner L, Myers J, Briere J, et al, editors. The APSAC Handbook on Child Maltreatment. Thousand Oaks, CA: Sage Publications, 2002.
11 American Academy of Child and Adolescent Psychiatry. Practice parameters for the assessment and treatment of children and adolescents who are sexually abusive of others. J Am Acad Child Adolesc Psychiatry. 1999;38(12):55-76.
12 ten Bensel RW. Integrated glossary of normal child sexuality and child sexual abuse terms for juvenile justice professionals. Reno, NV: National Council of Juvenile and Family Court Judges, 1987.
13 National Institutes of Health, National Institutes of Health: Medline Plus Medical Dictionary, 2006. (Available at: www.nlm.nih.gov/medlineplus/mplusdictionary.html; accessed 2/16/07).
14 Masters WH, Johnson VE, Kolodny RC. Human Sexuality. Toronto, Ontario: Little, Brown, 1982.
15 Martinson FM. Eroticism in infancy and childhood. In: Constantine LL, Martinson FM, editors. Children and Sex: New Findings, New Perspectives. Boston: Little, Brown; 1981:23-35.
16 Rutter M. Normal psychosexual development. J Child Psychol Psychiatry. 1971;11:259-283.
17 Gessell A. The First Five Years of Life. London: Methuen, 1940.
18 Volbert R. Sexual knowledge of preschool children. J Psychol Hum Sex. 2000;12:5-26.
19 Gordon BN, Schoeder CS, Abrams M. Age and social-class differences in children’s knowledge of sexuality. J Clin Child Psychol. 1990;19:33-43.
20 Bem SL. Genital Knowledge and gender constancy in preschool children. Child Dev. 1989;60:649-662.
21 Fraley MC, Nelson EC, Wolf AW, et al. Early genital naming. Dev Behav Pediatr. 1991;12:301-305.
22 Moore JE, Kendall DC. Children’s concepts of reproduction. J Sex Res. 1971;7:42-61.
23 Cohen B, Parker S. Sex information among nursery-school children. In: Oremland EK, Ormland JD, editors. The Sexual Gender Development of Young Children: The Role of the Educator. Cambridge, MA: Ballinger, 1977.
24 Goldman R, Goldman J. Children’s Sexual Thinking. London: Rutledge & Kegan Paul, 1982.
25 Goldman R, Goldman J. Children’s perceptions of sex differences in babies and adolescents: A cross-national study. Arch Sex Behav. 1983;12:277-294.
26 Kreitler H, Krietler S. Children’s concepts of sexuality and birth. Child Dev. 1996;37:363-378.
27 Friedrich WN. Child Sexual Behavior Inventory: Professional Manual. Odessa, FL: Psychological Assessment Resources, 1997.
28 Friedrich WN, Fisher J, Dittner C, et al. Child Sexual Behavior Inventory: Normative, psychiatric, and sexual abuse comparisons. Child Maltreat. 2001;6:37-49.
29 Davies SL, Glaser D, Kossoff R. Children’s sexual play and behavior in preschool settings: Staff’s perceptions, reports, and response. Child Abuse Negl. 2000;24:1329-1343.
30 Friedrich WN, Sandfort TGM., Oostveen J, et al. Cultural differences in sexual behavior: 2–6 Year old Dutch and American Children. J Psychol Hum Sex. 2000;12:117-129.
31 Larsson I, Svedin CG, Friedrich WN. Differences and similarities in sexual behaviour among preschoolers in Sweden and USA. Nord J Psychiatry. 2000;54:251-257.
32 Larsson I, Svedin CG. Sexual behaviour in Swedish preschool children, as observed by their parents. Acta Paediatr. 2001;90:436-438.
33 Friedrich WN. Psychological Assessment of Sexually Abused Children and Their Families. Thousand Oaks, CA: Sage Publications, 2002.
34 Gordon B. Sexual development. In: Ollendick TH, Schroeder CS, editors. Encyclopedia of Clinical Child and Pediatric Psychology. New York: Kluwer Academic/Plenum; 2003:591-594.
35 Schroeder CS, Gordon BN. Assessment and Treatment of Childhood Problems. New York: Guilford, 1991.
36 Centers for Disease Control and Prevention. Trends in sexual risk behaviors among high school students-United States: 1991–2001. MMWR Morb Mortal Wkly Rep. 2002;51:856-861.
37 Lamb S, Coakley M. “Normal” childhood play and games: Differentiating play from abuse. Child Abuse Negl. 1993;17:515-526.
38 Larsson I: Children and Sexuality: “Normal” Sexual Behavior and Experiences in Childhood. Linköping, Sweden: Linköping University, Department of Health and Environment, Division of Child and Adolescent Psychiatry, 2001.
39 Reynolds M, Herbenick D, Bancroft J. The nature of childhood sexual experiences: Two studies 50 years apart. In: Bancroft J, editor. Sexual development. Bloomington: Indiana University Press; 2003:134-155.
40 Friedrich WN, Whiteside SP, Talley NJ. Noncoercive sexual contact with similarly aged individuals: What is the impact? J Interpers Violence. 2004;19:1075-1084.
41 Greenwald E, Leitenberg H. Long-term effects of sexua l experiences with siblings and non-siblings during childhood. Arch Sex Behav. 1989;18:389-399.
42 Okami P, Olmstead R, Abramson PR. Sexual experiences in early childhood: 18-Year longitudinal data from the UCLA Family Lifestyles Project. J Sex Res. 1997;34:339-347.
43 Finkelhor D. Sex among siblings: A survey of prevalence, variety, and effects. Arch Sex Behav. 1980;9:171-194.
44 Tanner JM. Puberty. McLaren A, editor. Advances in Reproductive Physiology. New York: Academic Press; 1967;2:311-347.
45 Ollendick TH, Schroeder CS. Encyclopedia of Clinical Child and Pediatric Psychology. New York: Kluwer Academic/Plenum, 2003.
46 Kinsey AC, Pomeroy WB, Martin CE. Sexual Behavior in the Human Male. Oxford, UK: WB Saunders, 1948.
47 Herman-Gidden M, Slora E, Wasserman R, et al. Secondary sexual characteristics and menses in young girls seen in office practice: A study from the Pediatric Research in Office Settings Network. Pediatrics. 1997;99:505-512.
48 Halpern CT, Udry JR, Suchindran C. Testosterone predicts initiation of coitus in adolescent females. Psy-chosom Med. 1997;59:161-171.
49 Blythe MJ, Rosenthal SL. Female adolescent sexuality: Promoting healthy sexual development. Obstet Gynecol Clin North Am. 2000;27:125-141.
50 DeLatmter J, Friedrich W. Human sexual development. J Sex Res. 2002;39:10-14.
51 Kirby D. Emerging Answers: Research Findings on Programs to Reduce Teen Pregnancy (Summary). Washington, DC: National Campaign to Prevent Teen Pregnancy, 2001.
52 Alford S. Science and Success: Sex Education and Other Programs That Work to Prevent Teen Pregnancy, HIV, and Sexually Transmitted Infections. Washington: Advocates for Youth, 2003.
53 Miller BC. Families Matter: A Research Synthesis of Family Influences on Adolescent Pregnancy. Washington, DC: National Campaign to Prevent Teen Pregnancy, 1998.
54 Kinsman SB, Romer D, Furstenberg FF, et al. Early sexual initiation: The role of peer norms. Pediatrics. 1998;102:1185-1192.
55 Santelli JS, DiClemente RJ, Miller KS, et al. Sexually transmitted diseases, unintended pregnancy, and adolescent health promotion. Adolesc Med. 1999;10:87-108.
56 Neinstein LS. Adolescent sexuality. In: Neinstein LS, editor. Adolescent Health Care: A Practical Guide. Baltimore: Williams & Wilkins; 1996:628-629.
57 Maynard R. Kids Having Kids: A Robin Hood Foundation Special Report on the Costs of Adolescent Childbearing. New York: Robin Hood Foundation, 1996.
58 Grunbaum JA, Kann L, Kinchen S, et al. Youth risk behavior surveillance-United States, 2003. MMWR Surveill Summ. 2004;53(2):1-96.
59 Gates G, Sonenstein FL. Heterosexual genital sexual activity among adolescent males: 1988 and 1995. Fam Plann Perspect. 2000;32:295-297.
60 Mosher WD, Chandra A, Jones J. Sexual behavior and selected health measures: Men and women 15–44 years of age, United States, 2002. Adv Data. 2005;362:1-55.
61 Prinstein MJ, Meade CS, Cohen GL. Adolescent oral sex, peer popularity, and perceptions of best friends’ sexual behavior. J Pediatr Psychol. 2003;28:243-249.
62 Terry E, Manlove J. Trends in Sexual Activity and Contraceptive Use among Teens. Washington: Child Trends, 2000.
63 Collins RL, Elliott MN, Berry SH, et al. Entertainment television as a healthy sex educator: The impact of condom-efficacy information in an episode of Friends. Pediatrics. 2003;112:1115-1121.
64 Frankowski BL. American Academy of Pediatrics, Committee on Adolescence: Sexual orientation and adolescents. Pediatrics. 2004;113:1827-1832.
65 Remafedi G, Resnick M, Blum R, et al. Demography of sexual orientation in adolescents. Pediatrics. 1992;89:714-721.
66 Siddiqi S, Van Dyke DC, Donohoue P, et al. Premature sexual development in individuals with neurodevelopmental disabilities. Dev Med Child Neurol. 1999;41:392-395.
67 Woodward LJ. Sexuality and disability. Clin Fam Pract. 2004;6:941-954.
68 Gordon BN, Schroder C. Sexuality: A Developmental Approach to Problems. New York: Plenum Press, 1995.
69 Berman H, Harris D, Enright R, et al. Sexuality and the adolescent with a physical disability: Understandings and misunderstandings. Issues Comprehens Pediatr Nurs. 1999;22:183-196.
70 Kendall-Tackett K, Williams LM, Finkelhor D. Impact of sexual abuse on children: A review and synthesis of recent empirical studies. Psychol Bull. 1993;113:164-180.
71 White S, Haplin BM, Strom GA, et al. Behavioral comparisons of young sexually abused, neglected, and nonreferred children. J Clin Child Psychol. 1988;17:53-61.
72 Friedrich WN. Sexual victimization and sexual behavior in children: A review of recent literature. Child Abuse Negl. 1993;17:59-66.
73 Hewitt SK. Assessing allegation of sexual abuse in preschool children: Understanding small voices. Interpersonal Violence: The Practice Series. Thousand Oaks, CA: Sage Publications, 1999.
74 Johnson TC. Children who act out sexually. In: McNamara J, McNamara BH, editors. Adoption and the Sexually Abused Children. Portland: University of Maine; 1990:63-73.
75 Friedrich WN. Behavior problems in sexually abused children: An adaptational perspective. In: Wyatt GE, Powell GJ, editors. Lasting Effects of Child Sexual Abuse. Newbury Park, CA: Sage Publications; 1988:171-191.
76 Johnson TC. Child perpetrators-Children who molest other children: Preliminary findings. Child Abuse Negl. 1988;12:219-229.
77 Johnson TC. Female child perpetrators: Children who molest other children. Child Abuse Negl. 1989;13:571-585.
78 Silovsky JF, Niec L. Characteristics of young children with sexual behavior problems: A pilot study. Child Maltreat. 2002;7:187-197.
79 Bonner BL, Walker CE, Berliner L. Children with Sexual Behavior Problems: Assessment and Treatment (Final Report, Grant No. 90-CA-1469). Washington, DC: Administration of Children, Youth, and Families, U.S. Department of Health and Human Services, 1999.
80 Gray A, Busconi A, Houchens P, et al. Children with sexual behavior problems and their caregivers: Demographics, functioning, and clinical patterns. Sex Abuse. 1997;9:267-290.
81 Vermont Social and Rehabilitation Services: Vermont Child Abuse and Neglect. Waterbury, VT: Social and Rehabilitative Services, July 1996.
82 Bonner BL, Fahey WE. Children with aggressive sexual behavior. In: Singh NN, Winton ASW, editors. Comprehensive Clinical Psychology Special Population. Oxford, UK: Elsevier Science; 1998:453-466.
83 Friedrich WN, Davies W, Fehrer E, et al. Sexual behavior problems in preteen children: Developmental, ecological, and behavioral correlates. Ann N Y Acad Sci. 2003;989:95-104.
84 Gray A, Pithers WD, Busconi A, et al. Developmental and etiological characteristics of children with sexual behavior problems: Treatment implications. Child Abuse Negl. 1999;23:601-621.
85 Langstrom N, Grann M, Lichtenstein P. Genetic and environmental influences on problematic masturbatory behavior in children: A study of same-sex twins. Arch Sex Behav. 2002;31:343-350.
86 Friedrich WN: Children with Sexual Behavior Problems: Family-Based, Attachment-Focused Therapy. New York: WW Norton, in press.
87 Pithers WD, Gray A, Busconi A, et al. Children with sexual behavior problems: Identification of five distinct child types and related treatment considerations. Child Maltreat. 1998;3:384-406.
88 Friedrich WN, Luecke W, Beilke RL, et al. Psychotherapy outcome with sexually abused boys: An agency study. J Interpers Violence. 1998;7:396-409.
89 Gil E, Johnson TC. Sexualized children: Assessment and treatment of sexualized children and children who molest. Rockville, MD: Launch Press, 1993.
90 Horton CB. Children who molest other children: The school psychologist’s response to the sexually aggressive child. School Psychol Rev. 1996;25:540-557.
91 Heiman M. Helping parents address their child’s sexual behavior problems. J Child Sex Abuse. 2001;10:35-37.
92 Pearce J: Intervention Strategies with Preadolescent Children with Sexual Behavior Problems. Presented at the 11th Oklahoma Conference on Child Abuse and Neglect and Healthy Families, Norman, OK, September 17–19, 2003.
93 Baker AJL, Schneiderman M, Parker R. A survey of problematic sexualized behaviors in the New York City child welfare system: Estimates of problem, impact on services, and need for training. J Child Sex Abuse. 2002;10:67-80.
94 McKenzie W, English D, Henderson J. Family centered case management with sexually aggressive youth: Final report of the Sexually Aggressive Youth Project. Olympia: Washington State Department of Social and Health Services, Division of Children, Youth and Family Services, 1987.
95 Bonner BL, Walker CE, Berliner L, et al: Cluster Analyses of Children with Sexual Behavior Problems. Manuscript in preparation.
96 Hall DK, Mathews F, Pearce J. Sexual behavior problems in sexually abused children: A preliminary typology. Child Abuse Negl. 2002;26:389-390.
97 Berliner L, Elliott D. Sexual abuse of children. In: Berliner L, Meyers JE, Briere J, et al, editors. The APSAC Handbook on Child Maltreatment. Thousand Oaks, CA: Sage Publishing; 2002:55-78.
98 Johnson TC, Friend C. Assessing young children’s sexual behaviors in the context of child sexual abuse evaluations. In: Ney T, editor. True and False Allegations of Child Sexual Abuse: Assessment and Case Management. Philadelphia: Brunner/Mazel; 1995:49-72.
99 Achenbach TM, Rescorla LA. Manual for ASEBA Preschool Forms & Profiles. Burlington: University of Vermont, Research Center for Children, Youth, and Families, 2000.
100 Achenbach TM, Rescorla LA. Manual for ASEBA School-Age Forms & Profiles. Burlington: University of Vermont, Research Center for Children, Youth & Families, 2001.
101 Reynolds C, Kamphaus R. Behavior Assessment System for Children Manual. Circle Pines, MN: American Guidance Service, 1992.
102 Briere J. Trauma Symptom Checklist for Children: Professional Manual. Odessa, FL: Psychological Assessment Resources, 1996.
103 Briere J, Johnson K, Bissada A, et al. The Trauma Symptom Checklist for Young Children (TSCYC): Reliability and association with abuse exposure in a multisite study. Child Abuse Negl. 2001;25:1001-1014.
104 Cohen JA, Mannarino AP. The weekly behavior report: A parent-report instrument for sexually abused preschoolers. Child Maltreat. 1996;1:353-360.
105 Carpentier M, Silovsky JF, Chaffin M. Randomized trial of treatment for children with sexual behavior problems: Ten year follow-up. J Consult Clin Psychol. 2006;74:482-488.
106 Pithers WD, Gray A, Busconi A, et al. Children with sexual behavior problems: Identification of five distinct child types and related treatment considerations. Child Maltreat. 1999;3:384-406.
107 Cohen JA, Mannarino AP. A treatment outcome study for sexually abused preschool children: Initial findings. J Am Acad Child Adolesc Psychiatry. 1996;35:42-50.
108 Cohen JA, Mannarino AP. A treatment study for sexually abused preschool children: Outcome during one-year follow-up. J Am Acad Child Adolesc Psychiatry. 1997;36:1228-1235.
109 Hall-Marley SE, Damon L. Impact of structured group therapy on young victims of sexual abuse. J Child Adolesc Group Ther. 1993;3:41-48.
110 Stauffer LB, Deblinger E. Cognitive behavioral groups for nonoffending mothers and their young sexually abused children: A preliminary treatment outcome study. Child Maltreat. 1996;1:65-76.
111 Cohen JA, Mannarino AP. A treatment model for sexually abused preschoolers. J Interpers Violence. 1993;8:115-131.
112 Cohen JA, Mannarino AP, Deblinger E. Treatment Trauma and Traumatic Grief in Children and Adolescents. New York: Guilford, 2006.
113 Deblinger E, Heflin AH. Treating sexually abused children and their nonoffending parents: A cognitive behavioral approach. Thousand Oaks, CA: Sage Publications, 1996.
114 Brestan EV, Eyberg SM. Effective psychosocial treatments of conduct-disordered children and adolescents: 29 Years, 82 studies, and 5,272 kids. J Clin Child Psychol. 1998;27:180-189.
115 Nixon R. Treatment of behavior problems in preschoolers: A review of parent training programs. Clin Psychol Rev. 2002;22:525-546.
116 Webster-Stratton C. The Incredible Years: A training series for the prevention and treatment of conduct problems in young children. In: Hibbs ED, Jensen PS, editors. Psychosocial Treatments for Child and Adolescent Disorders: Empirically Based Strategies for Clinical Practice. Washington, DC: American Psychological Association; 2005:507-555.
117 Barkley R, Benton C. Your Defiant Child: Eight Steps to Better Behavior. New York: Guilford, 1998.
118 Sanders MR, Cann W, Markie-Dadds C. The Triple P-Positive parenting programme: A universal population-level approach to the prevention of child abuse. Child Abuse Rev. 2003;12:155-171.
119 Chaffin M, Berliner L, Block R, et al. Draft Report of the ATSA Task Force on Children with Sexual Behavior Problems. Beaverton, OR: Association for the Treatment of Sexual Abusers, 2005.
120 Bakersman-Kranenburg MJ, Van Uzendoorn MH, Juffer F. Less is more: Meta-analyses of sensitivity and attachment interventions in early childhood. Psychol Bull. 2003;129:195-215.
121 Chaffin M, Bonner B, Pierce K. What Research Shows about Adolescent Sexual Offenders. Fact Sheet Oklahoma City. National Center on the Sexual Behavior of Youth, 2003.
122 Synder HN, Sickmund M. Juvenile Offenders and Victims: 1999 National Report. Washington, DC: U.S. Department of Justice, Office of Juvenile Justice and Delinquency Prevention, 1999.
123 Davis GE, Leitenberg H. Adolescent sexual offenders. Psychol Bull. 1987;101:417-427.
124 Snyder H. Juvenile Arrests 2000 (Cooperative Agreement No. 1999-JN-FX-K002). In: OJJDP Juvenile Justice Bulletin. Washington, DC: U.S. Department of Justice, Office of Juvenile Justice and Delinquency Prevention; 2002:1-12.
125 Becker JV. What we know about the characteristics and treatment of adolescents who have committed sexual offenses. Child Maltreat. 1998;3:317-329.
126 Knight RA, Prentky RA. Exploring characteristics for classifying juvenile sex offenders. In: Barbaree HE, Marshall WL, Hudson SM, editors. The Juvenile Sex Offender. New York: Guilford; 1993:45-83.
127 Hanson RK, Slater S. Sexual victimization in the history of sexual abusers: A review. Ann Sex Res. 1988;1:485-499.
128 Widom CS. Victims of Childhood Sexual Abuse-Later Criminal Consequences. Washington, DC: U.S. Department of Justice, Office of Justice Programs, National Institute of Justice, 1995.
129 Mathews R, Hunter JA, Vuz J. Juvenile female sexual offenders: Clinical characteristics and treatment issues. Sex Abuse. 1997;9:187-199.
130 Bumby KM, Bumby NH. Adolescent female sex offenders. In: Schwartz BK, Cellini HR, editors. The Sex Offender: Corrections, Treatment and Legal Practice. Kingston, NJ: Civic Research Institute; 1997:10.1-10.16.
131 Hunter JA, Lexier LJ, Goodwin DW, et al. Psychosexual attitudinal, and developmental characteristics of juvenile female sexual perpetrators in a residential treatment setting. J Child Fam Stud. 1993;2:317-326.
132 Krauth AA. A comparative study of male juvenile sex offenders. Diss Abstr Int B Sci Eng. 1998;58:4455.
133 Carpenter DR, Peed SF, Eastman B. Personality characteristics of adolescent sexual offenders: A pilot study. Sex Abuse. 1995;7:195-203.
134 Prentky RA, Harrris B, Frizell K, et al. An actuarial procedure for assessing risk with juvenile sex offenders. Sex Abuse. 2000;12:71-93.
135 Association for the Treatment of Sexual Abusers: The Effective Legal Management of Juvenile Sex Offenders. Beaverton, OR: Association for the Treatment of Sexual Abusers, 2000. (Available at: http://www.atsa.com/ppjuvenile.html; accessed 2/16/07.)
136 Alexander MA. Sexual offender treatment efficacy revisited. Sex Abuse. 1999;11:101-116.
137 Miranda AO, Corcoran CL. Comparison of perpetration characteristics between male juvenile and adult sexual offenders: Preliminary results. Sex Abuse. 2000;12:179-188.
138 American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 4th ed. Washington: American Psychiatric Press, 1994.
139 Letourneau EJ, Miner MH. Juvenile sex offenders: A case against the legal and clinical status quo. Sex Abuse. 2005;17:293-312.
140 Friedrich WN, Lysne M, Sim L, et al. Assessing sexual behavior in high-risk adolescents with the Adolescent Clinical Sexual Behavior Inventory (ACSBI). Child Maltreat. 2004;9:239-250.
141 Borduin CM, Henggeler SW, Blaske DM, et al. Multisystemic treatment of adolescent sexual offenders. Int J Offender Ther Comp Criminol. 1990;34:105-113.
142 Borduin CM, Schaeffer CM. Multisystemic treatment of juvenile sex offenders: A progress report. J Psychol Hum Sex. 2002;13:25-42.
143 Thomas D, Flahery E, Binns H. Parent expectations and comfort with discussion of normal childhood sexuality and sexual abuse prevention during office visits. Ambul Pediatr. 2004;4:232-236.
144 Hall DK, Mathews F, Pearce J. Factors associated with sexual behavior problems in young sexually abused children. Child Abuse Negl. 1998;22:1045-1063.
145 Johnson TC. Helping Children with Sexual Behavior Problems-A Guidebook for Parents and Substitute Caregivers, 2nd ed. South Pasadena, CA: Toni Cava-nagh Johnson, 2004.
146 Silovsky JF, Niec L, Bard D, et al: Treatment for Preschool Children with Sexual Behavior Problems: Pilot study. Journal of Clinical Child and Adolescent Psychology, in press.
147 Grant L. Sex and the Adolescent. In: Zwellerman B, Parker S, editors. Behavioral and Developmental Pediatrics. Boston: Little, Brown; 1995:269-277.
148 Russell ST, Franz BT, Driscoll AK. Same-sex romantic attraction and experiences of violence in adolescence. Am J Public Health. 2001;91:903-906.
149 Russell ST, Driscoll AK, Truong N. Adolescent same-sex romantic attractions and relationships: Implications for substance use and abuse. Am J Public Health. 2002;92:198-202.
150 Kupper L. Comprehensive sexuality education for children and youth with disabilities. SIECUS Rep. 1995;23:3-8.
151 American Academy of Pediatrics, Committee on Children with Disabilities. Sexuality education of children and adolescents with developmental disabilities. Pediatrics. 2000;97:275-278.
152 Nwoga IA. African American mothers use stories for family sexuality education. MCN Am J Matern Child Nurs. 2000;25:31-36.
153 Bigfoot DS, Dunlap M. Storytelling as a healing tool for American Indians. In: Witko TM, editor. Mental Health Care for Urban Indians-Clinical Insights from Native Practitioners. Washington, DC: American Psychological Association, 2006.
154 Cohen JA, Mannarino AP. Factors that mediate treatment outcome of sexually abused preschool children: Six and twelve month follow up. J Am Acad Child Adolesc Psychiatry. 1998;37:44-51.
155 Cohen JA, Mannarino AP. Predictors of treatment outcome in sexually abused children. Child Abuse Negl. 2000;24:983-994.
156 Broidy L, Cauffman E, Espelage DL, et al. Sex differences in empathy and its relation to juvenile offending. Violence Victims. 2003;18:503-516.
157 Sex role [definition]. In Online Medical Dictionary. Newcastle upon Tyne, UK: University of Newcastle upon Tyne, Centre for Cancer Education, 2000. (Available at: http://cancerweb.ncl.ac.uk/cgi-bin/omd?sex+role; accessed 2/16/07.)
25B. Gender Identity
This chapter focuses on children and adolescents with sex-typed behavioral patterns that correspond to the diagnosis of Gender Identity Disorder (GID), as defined in the fourth edition, text revision, of the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV-TR).1 Most children who meet DSM-IV-TR criteria for GID do not show any gross clinical signs of an abnormal or atypical physical sex differentiation (e.g., the sex chromosomes, the prenatal hormonal milieu); however, some children with physical intersex conditions (disorders of sex differentiation) do exhibit problems in their gender development; accordingly, some consideration is also given to this population.
Numerous television series have had story lines on the topic, and several critically acclaimed films, such as Ma Vie en Rose (My Life in Pink) in 1997, Boys Don’t Cry in 1999, and Transamerica in 2005, have also focused an artistic gaze on the subject. The print media has also given attention to GID, including articles in Time2 and Saturday Night.3 On May 12, 2004, the Oprah Winfrey Show, with over 20 million viewers in the United States alone, featured several prepubertal “transgendered” children and their families, and on March 12, 2006, 60 Minutes, with about 14 million viewers, provided a snapshot of 9-year-old fraternal twin boys markedly discordant for gender behavior: one boy was conventionally masculine, and the other boy was conventionally feminine and expressed the desire to be a girl. Thus, it is timely to provide an updated review on children and youth who experience discomfort about their gender identity.
CLINICAL AND SCIENTIFIC SIGNIFICANCE
Parents commonly rely on health professionals to help them sort out whether the behavior of their child warrants clinical attention. This is as true for gender and sexuality issues as it is for any other behavioral developmental matter. Thus, pediatricians are at the forefront in helping parents appraise their child’s development. Moreover, primary care pediatricians can consult with pediatricians with expertise in developmental and behavioral issues in helping them differentiate between behavioral or emotional difficulties that are transient and those that are more pervasive.4
Issues surrounding gender and sexual development often cause intense anxiety for parents. Are the behaviors in question “only a phase” that the child will grow out of, or are the behaviors in question prognostic of longer term developmental issues? Regarding gender development, parents often want to know whether the behaviors of their young child are prognostic of a later homosexual sexual orientation or of transsexualism, the desire to receive contrasex hormonal treatment and physical sex change (e.g., in men, penectomy/castration and the surgical creation of a neovagina; in women, mastectomy and the surgical creation of a neophallus). Parents also often worry about the stigma that their child’s pervasive cross-gender behavior might elicit within the peer group and in society at large. Similarly, when an adolescent engages in atypical sexual behavior (e.g., the use of women’s undergarments for the purpose of sexual arousal), parents wonder what the behavior means. Is it only an experimental phase of sexual exploration and curiosity, or does it signify something else that might cause problems and complications in their adolescent’s intimate life?
These kinds of questions require a familiarity with normative gender and sexual development, which allows the developmental-behavioral pediatrician to make decisions about differential diagnosis and to consider therapeutic options. This requires a good understanding of what is known about the basic mechanisms that underlie typical gender and sexual development.
TERMINOLOGY
Table 25B-1 provides a brief description of several terms that are used throughout this chapter.5–15
| Term | Brief Definition | References |
|---|---|---|
| Sex | Attributes that collectively, and usually harmoniously, characterize biological maleness and femaleness (e.g., the sex-determining genes, the sex chromosomes, the H-Y antigen, the gonads, sex hormones, the internal reproductive structures, and the external genitalia) | 5, 6 |
| Gender | Psychological or behavioral characteristics associated with boys/men and girls/women | 7 |
| Gender identity | Basic sense of self as a boy/man or a girl/woman | 8, 9 |
| Gender role | Behaviors, attitudes, and personality traits that a society, in a given culture and historical period, designates as masculine or feminine: that is, more “appropriate” to or typical of the male or female social role | 7 |
| Sexual orientation | A person’s relative responsiveness to sexual stimuli (erotic preference); the most salient dimension of sexual orientation is probably the sex of the person to whom one is attracted sexually, as in heterosexual, bisexual, or homosexual | 10–12 |
| Sexual identity | Self-labeling of one’s sexual orientation | |
| Paraphilias | A sexual orientation or erotic preference that is considered abnormal or atypical, as in transvestic fetishism or pedophilia | 14, 15, 17 |
PREVALENCE
The prevalence of GID in children has not been formally studied by epidemiological methods. Prevalence estimates of GID in adults suggest an occurrence of 1 per 11,000 to 37,000 men and 1 per 30,400 to 150,000 women.1,16
Among children, some information can be derived from the widely used Child Behavior Checklist (CBCL),18–19 a parent-report behavior problem questionnaire. The CBCL includes 2 items (of 118) that pertain to cross-gender identification: “behaves like opposite sex” and “wishes to be of opposite sex.” On the CBCL, ratings are made on a 3-point scale (0 = not true, 1 = somewhat or sometimes true, and 2 = very true or often true). In the standardization study, answering both items affirmatively was more common for girls than for boys, regardless of age and clinical status (referred vs. nonreferred).20
Among nonreferred boys (aged 4 to 11 years), 3.8% received a rating of 1 and 1.0% received a rating of 2 for the item “behaves like opposite sex,” but only 1.0% received a rating of 1 and 0.0% received a rating of 2 for the item “wishes to be of opposite sex.” The comparable percentages among nonreferred girls were 8.3%, 2.3%, 2.5%, and 1.0%, respectively. Comparable findings have been reported in an epidemiological sample of twins.21 Collectively, these data suggest that there is a sex difference in the occurrence of mild displays of cross-gender behavior but not with regard to more extreme cross-gender behavior. The main problem with such data, however, is that they do not identify adequately patterns of cross-gender behavior that would be of use in determining caseness. Thus, such data may be best viewed as screening devices for more intensive evaluation.
SEX DIFFERENCES IN REFERRAL RATES
Among children between the ages of 3 to 12, boys are referred clinically more often than girls for concerns regarding gender identity. In my own clinic, Cohen-Kettenis and colleagues reported a boy-to-girl ratio of 5.75 : 1 (N = 358) on the basis of consecutive referrals from 1975 to 2000.22 In this study, comparative data were available from children evaluated at the sole gender identity clinic for children in Utrecht, The Netherlands. Although the sex ratio was significantly smaller at 2.93 : 1 (N = 130), it still reflected referral of more boys than girls. Among adolescents between the ages of 13 to 20, however, the sex ratio in my clinic narrowed considerably, at 1.32 : 1 (N = 72).23 This ratio was remarkably similar to the 1.20 : 1 (N = 133) boy-to-girl ratio reported by Cohen-Kettenis and Pfäfflin24 in the Netherlands. Thus, across both clinics, there was a sex-related skew in referrals during childhood, but this lessened considerably during adolescence.
DIAGNOSIS AND ASSESSMENT
Reliability and Validity
In the clinical research literature, very little attention has been paid to reliability of diagnosis for GID. One study demonstrated that clinicians can reliably make the diagnosis in children25 but, to my knowledge, no investigators have evaluated the reliability of the diagnosis for adolescents.26
It is relatively uncommon, at least in specialized child and adolescent gender identity clinics, to encounter an adolescent who has only very mild gender dysphoria. Thus, it is important to keep in mind that the indicators of GID are meant to capture a “strong and persistent cross-gender identification” and a “persistent discomfort” with one’s gender, not transient feelings.27–28
The DSM-IV-TR criterion with regard to the “preoccupation” with primary and secondary sex characteristics (Point B-2) reflects well the adolescent expression of gender dysphoria as it pertains to discomfort with somatic sex, inasmuch as the distress over physical sex markers is so pervasive (Table 25B-2).
TABLE 25B-2 DSM-IV-TR Diagnostic Criteria for Gender Identity Disorder
|
A. A strong and persistent cross-gender identification (not merely a desire for any perceived cultural advantages of being the other sex).
In children, the disturbance is manifested by at least four (or more) of the following:
2. In boys, preference for cross-dressing or simulating female attire; in girls, insistence on wearing only stereotypical masculine clothing
In adolescents… the disturbance is manifested by symptoms such as a stated desire to be the other sex, frequent passing as the other sex, desire to live or be treated as the other sex, or the conviction that he or she has the typical feelings and reactions of the other sex.
B. Persistent discomfort with his or her sex or sense of inappropriateness in the gender role of that sex.
In children, the disturbance is manifested by any of the following: in boys, assertion that his penis or testes are disgusting or will disappear or assertion that it would be better not to have a penis, or aversion toward rough-and-tumble play and rejection of male stereotypical toys, games, and activities; in girls, rejection of urinating in a sitting position, assertion that she has or will grow a penis, or assertion that she does not want to grow breasts or menstruate, or marked aversion toward normative feminine clothing.
In adolescents… the disturbance is manifested by symptoms of such as preoccupation with getting rid of primary and secondary sex characteristics (e.g., request for hormones, surgery, or other procedures to physically alter sexual characteristics to simulate the other sex) or belief that he or she was born the wrong sex.
|
From the American Psychiatric Association: Diagnostic and Statistical Manual of Mental Disorders, 4th ed, text revision [DSM-IV-TR]. Washington, DC: American Psychiatric Press, 2000.
As noted previously, there is only one clinician-based reliability study of GID in children; however, there is a much more extensive literature in which its discriminant validity has been examined. Since the early 1970s, a variety of measurement approaches have been developed to assess the sex-typed behavior in children referred clinically for GID, including observation of sex-typed behavior in free play tasks, on semiprojective or projective tasks, and on a structured Gender Identity Interview schedule. In addition, several parent-report questionnaires pertaining to various aspects of sex-typed behavior have been developed. In this line of research, several comparison groups have typically been used: siblings of children with GID, clinical controls, and nonreferred (or “normal”) controls.29–31
The results of these studies have demonstrated strong evidence for the discriminant validity of the various measures, with large effect sizes.29 In addition, several studies have shown that gender-referred children can be distinguished as a function of whether they met the complete DSM-IV-TR criteria for GID (i.e., threshold vs. subthreshold cases).31–35
Two self-report and one parent report instruments are described. All three of these measures have practical utility in an office-based practice and can complement a detailed clinical interview. The first is the Gender Identity Interview for Children, which contains 11 items. Each item is coded on a 3-point response scale. On the basis of factor analysis, Zucker and associates32 identified two factors, which were labeled affective gender confusion (seven items) and cognitive gender confusion (four items) and accounted for 38.2% and 9.8% of the variance, respectively. An item example from the first factor is “In your mind, do you ever think that you would like to be a girl (boy)?” and an item example from the second factor is “Are you a boy or a girl?” Both mean factor scores significantly differentiated gender-referred probands (n = 85) from controls (n = 98). Cutoff scores of either three or four deviant responses yielded high specificity rates (88.8% and 93.9%, respectively), but lower sensitivity rates (54.1% and 65.8%, respectively).
The second instrument is the Gender Identity Questionnaire for Children, a parent-report questionnaire.33–34 This questionnaire consists of 16 items pertaining to various aspects of sex-typed behavior that are reflected in the GID diagnostic criteria, each rated on a 5-point response scale. A factor analysis based on 325 gender-referred children and 504 controls (siblings, clinic-referred, and nonreferred), with a mean age of 7.6 years, identified a one-factor solution containing 14 items, accounting for 43.7% of the variance. The gender-referred children had a significantly more total deviant score than did the controls, with a large effect size of 3.70, established by Cohen’s d. With a specificity rate set at 95% for the controls, the sensitivity rate for the probands was 86.8%.
The third instrument is the Gender Identity/Gender Dysphoria Questionnaire for Adolescents and Adults (GIDQ-AA), another self-report questionnaire.36 The GIDQ-AA consists of 27 items pertaining to various aspects of gender dysphoria, each rated on a 5-point response scale and with the past 12 months used as a time frame. In the female version, for example, items included: “In the past 12 months, have you felt more like a man than like a woman?” and “In the past 12 months, have you wished to have an operation to change your body into a man’s (e.g., to have your breasts removed or to have a penis made)?” A factor analysis based on 389 university students (heterosexual and nonheterosexual) and 73 clinic-referred patients with GID identified a one-factor solution containing all 27 items, which accounted for 61.3% of the variance. The GIDQ-AA strongly distinguished the GID patients from both the heterosexual and nonheterosexual controls. With a cutpoint of 3.00, sensitivity was 90.4% for the patients with GID, and specificity was 99.7% for the controls.
Associated Behavior Problems
A considerable amount of evidence suggests that in the presence of GID symptoms, it is important to assess for the presence of behavior problems. The most systematic information on general behavior problems in children with GID comes from parent-report data on the CBCL. On the CBCL, clinic-referred boys and girls with GID display, on average, significantly more general behavior problems than do their siblings and nonreferred children22,31 and levels comparable to those of demographically matched clinical controls31; moreover, CBCL-identified behavior problems are significantly more prevalent among adolescents with GID than among their GID child counterparts.23,26
According to the CBCL responses, boys with GID have a predominance of internalizing behavioral difficulties, whereas girls with GID do not.31 Two studies have shown that boys with GID demonstrate high rates of separation anxiety traits.37,38 Several studies have shown that increasing age was significantly associated with degree of behavior problems in boys with GID, which is probably mediated by peer ostracism,20,22,31 and another study has shown that a composite index of maternal psychopathology was also a strong predictor of behavior problems.39
DEVELOPMENTAL TRAJECTORIES
Adolescents and adults with GID, particularly those who have a homosexual orientation (i.e., sexual attraction to members of one’s birth sex), invariably recall a pattern of cross-sex–typed behavior during childhood that corresponds to the DSM-IV-TR criteria for GID.36 Another line of research showed that adults with a homosexual sexual orientation, unselected for gender identity, were also more likely, on average, to recall patterns of childhood cross-sex–typed behavior in comparison with their heterosexual counterparts.40 According to these retrospective studies, therefore, children with GID (which is at the extreme end of a continuum of cross-gender identification) monitored prospectively may be disproportionately likely to have persistent GID and/or a homosexual sexual orientation.
Follow-up Studies of Boys
Green’s study41 constitutes the most comprehensive long-term follow-up of behaviorally feminine boys, the majority of whom would likely have met DSM-IV-TR criteria for GID. His study contained 66 feminine and 56 control boys (unselected for gender identity) assessed initially at a mean age of 7.1 years (range, 4 to 12). Forty-four feminine boys and 30 control boys were available for follow-up at a mean age of 18.9 years (range, 14 to 24). The majority of the boys were not in therapy between assessment and follow-up. Sexual orientation in fantasy and behavior was assessed by means of a semistructured interview. Kinsey ratings were made on a 7-point continuum, ranging from exclusive heterosexuality (a Kinsey rating of 0) to exclusive homosexuality (a Kinsey rating of 6).42 Depending on the measure (fantasy or behavior), 75% to 80% of the previously feminine boys were either bisexual or homosexual (Kinsey ratings between 2 and 6) at follow-up, in contrast to 0% to 4% of the control boys. Green also reported on the gender identity status of the 44 previously feminine boys. He found that only one youth, at the age of 18 years, was gender-dysphoric to the extent of considering sex-reassignment surgery.
Data from six other follow-up reports on 55 boys with GID were summarized by Zucker and Bradley.31 In these studies, the percentage of boys who exhibited persistent GID was higher than that reported by Green (11.9% vs. 2.2%, respectively), but the percentage who were homosexual (62.1%) was somewhat lower.
Zucker and Bradley31 reported preliminary follow-up data on a sample of 40 boys first observed in childhood (mean age at assessment, 8.2 years; range, 3 to 12). At follow-up, these boys were, on average, 16.5 years old (range, 14 to 23). Gender identity was assessed by means of a semistructured clinical interview and by questionnaire. Sexual orientation (for a 12-month period before the time of evaluation) was assessed for fantasy and behavior with the Kinsey scale in a manner identical to Green’s study.41
Of the 40 boys, 8 (20%) were classified as gender-dysphoric at follow-up. With regard to sexual orientation in fantasy, 20 (50%) were classified as heterosexual, 17 (42.5%) were classified as bisexual/homosexual, and 3 (7.5%) were classified as “asexual” (i.e., they did not report any sexual fantasies). Regarding sexual orientation in behavior, 9 (22.5%) were classified as heterosexual, 11 (27.5%) were classified as bisexual/homosexual, and 20 (50.0%) were classified as “asexual” (i.e., they did not report any interpersonal sexual experiences).
Cohen-Kettenis43 reported preliminary data on a sample of 56 boys first observed in childhood (mean age at assessment, 9 years; range, 6 to 12) and who had now reached adolescence. Of these, 9 (16.1%) requested sex-reassignment, and all 9 had a homosexual sexual orientation (P. T. Cohen-Kettenis, personal communication, February 1, 2003). Thus, the rate of GID persistence, at least into adolescence, was higher than that reported by Green41 and comparable to the rate obtained by Zucker and Bradley,31 as noted previously.
Follow-up Studies of Girls
To date, the most systematic follow-up of girls with GID was conducted by Drummond44 of patients seen in my clinic. A total of 25 girls, originally assessed at a mean age of 8.8 years (range, 3 to 12), were interviewed at follow-up at a mean age of 23.2 years (range, 15 to 36). Of these 25 girls, 3 (12%) had persistent GID (at follow-up ages of 17, 21, and 23 years), of whom 2 had a homosexual sexual orientation and 1 was “asexual” (i.e., did not report any sexual orientation). The remaining 22 girls (88%) had a “normal” gender identity.
With regard to sexual orientation in fantasy (Kinsey ratings) for the 12 months preceding the follow-up assessment, 15 (60%) girls were classified as exclusively heterosexual, 8 (32%) were classified as bisexual/homosexual, and 2 (8%) were classified as “asexual” (i.e., did not report any sexual fantasies). Regarding sexual orientation in behavior, 11 (44%) girls were classified as exclusively heterosexual, 6 (24%) were classified as bisexual/homosexual, and 8 (32%) were classified as “asexual” (i.e., they did not report any interpersonal sexual experiences).
In another study, Cohen-Kettenis43 reported preliminary data from a sample of 18 girls first seen in childhood (mean age at assessment, 9 years; range, 6 to 12) and who had now reached adolescence. Of these, 8 (44.4%) requested sex reassignment, and all had a homosexual orientation (P. T. Cohen-Kettenis, personal communication, February 1, 2003). Thus, the rate of GID persistence, at least into adolescence, was high (and much higher than the rate of persistence for the boys with GID).
Summary
In taking stock of these outcome data, Green’s41 study clearly showed that boys with GID were disproportionately, and substantially, more likely than the control boys to differentiate a bisexual/homosexual orientation. The other follow-up studies yielded somewhat lower estimates of a bisexual/homosexual orientation. In this regard, at least one caveat is in order. In Zucker and Bradley’s31 follow-up, for example, the boys were somewhat younger than were the boys in Green’s follow-up; thus, their lower rate of a bisexual/homosexual orientation outcome should be interpreted cautiously, inasmuch as, if anything, these youth would be expected to underreport an atypical sexual orientation because of social desirability considerations. But even these lower rates of a bisexual/homosexual orientation are substantially higher than the currently acknowledged base rate of about 2% to 3% of men with a homosexual orientation that has been identified in epidemiological studies.13 A similar conclusion can be drawn with regard to girls with GID. Using prevalence estimates of bisexuality/homosexuality in fantasy among biological females (anywhere between 2% and 5%), Drummond44 reported that the odds of reporting bisexuality/homosexuality in fantasy was 8.9 to 23.1 times higher than in the general population. The odds of reporting bisexuality/homosexuality in behavior was 6.7 to 15.5 times higher than in the general population.
A more substantive difference between Green’s41 study and the other follow-up reports of boys pertains to the persistence of gender dysphoria. Both Zucker and Bradley31 and Cohen-Kettenis,43 for example, found higher rates of persistence than did Green. At present, the reasons for this are unclear. One possible explanation pertains to sampling differences. Green’s study was carried out in the context of an advertised research study, whereas Zucker and Bradley’s and Cohen-Kettenis’s samples were clinic-referred. Thus, it is conceivable that their samples may have included more extreme cases of childhood GID than did the sample ascertained by Green.
With regard to girls with GID, the odds of persistent gender dysphoria in Drummond’s44 sample was 4084 times the odds of gender dysphoria in the general population.16
DISJUNCTIONS BETWEEN RETROSPECTIVE AND PROSPECTIVE DATA
A key challenge for developmental theories of psychosexual differentiation is to account for the disjunction between retrospective and prospective data with regard to GID persistence: It is clear that only a minority of children monitored prospectively show a persistence of GID into adolescence and young adulthood.
One explanation concerns referral bias. Green45 argued that children with GID who are referred for clinical assessment (and then, in some cases, therapy) may come from families in which there is more concern than is the case for adolescents and adults, the majority of whom did not receive a clinical evaluation and treatment during childhood. Thus, a clinical evaluation and subsequent therapeutic intervention during childhood may alter the natural history of GID. Another possibility is that the diagnostic criteria for GID, at least as they are currently formulated, simply are not sharp enough to distinguish children who are more likely to show a persistence in the disorder from those who are not.
An additional clue comes from consideration of the concepts of developmental malleability and plasticity. It is possible, for example, that gender identity shows relative malleability during childhood, with a gradual narrowing of plasticity as the gender-related sense of self consolidates as a child approaches adolescence. Some support for this idea comes from follow-up studies of adolescents with GID, who appear to show a much higher rate of GID persistence as they are monitored into young adulthood.46,47
ETIOLOGY
The cause of GID has been examined with regard to both biological and psychosocial mechanisms. Research on etiology is controversial because it is embedded in complex “political” matters, and the developmental-behavioral pediatrician needs to be aware of this social context. Parents, for example, hold all kinds of biases and beliefs regarding causality. Some parents adhere to a biological explanation for their child’s cross-gender behavior (“He must have been born that way”), whereas others adhere to a psychosocial explanation (“His father was never around”). In many respects, parental perspectives mirror the general scientific debate on the relative roles of nature and nurture with regard to psychosexual differentiation. Regardless of their accuracy, parental perspectives on etiology are important because they may be correlated with their views on their child more generally, what they want from the clinician, and their attitudes and goals about therapeutics.
Biological Mechanisms
Contemporary biological research on human psychosexual differentiation includes investigations of molecular genetics, behavioral genetics, prenatal sex hormones, prenatal maternal stress, maternal immunization, neurodevelopmental processes, pheromones, temperament, anthropometrics, and neuroanatomical substrates. Some of these parameters have been studied with regard to both children and adults with GID, some have been investigated in relation to sexual orientation, and others have been examined in nonclinic populations (e.g., twin studies).
Experimental studies—from mice to monkeys—have shown quite clearly how manipulation of the prenatal hormonal milieu can affect postnatal sex-dimorphic behavior.48 In humans, the effects of the prenatal hormonal environment have been examined in various physical intersex conditions. Consider, for example, studies of congenital adrenal hyperplasia (CAH), the most common physical intersex condition that affects genetically female humans. CAH is an autosomal recessive disorder associated with enzyme defects that result in abnormal adrenal steroid biosynthesis. Indeed, for affected genetically female fetuses, testosterone assayed from amniotic fluid during midgestation shows values in the range of unaffected genetically male fetuses. Because of this high level of androgen production during fetal development, masculinization of the external genitalia is common. On the basis of data from lower animals and on theory, it has been presumed that some masculinization of the fetal brain may also have occurred.
There is very clear evidence that the gender role behavior of girls with CAH is more masculine and/or less feminine than that of unaffected control girls.29,49 Moreover, adult follow-up studies of girls with CAH indicate that they have higher rates of bisexuality and homosexuality (particularly in fantasy) than do controls. Thus, for both gender role behavior and sexual orientation, there is a shift away from the female-typical pattern and toward the male-typical pattern. The evidence that CAH results in an altered gender identity is much less convincing. Although the percentage of genetically female girls with CAH—about 5%—who develop gender dysphoria or change gender from female to male is higher than that of girls in the general population, most girls and women with CAH appear to have an uncomplicated female gender identity.50 Together, these findings suggest that the prenatal hormonal milieu may have a greater effect on gender role and sexual orientation than it does on gender identity in girls and women with CAH.
As applied to GID (in both children and adults), classical prenatal hormone theory has, at least in its simple form, been challenged because there is no compelling evidence that the prenatal hormonal milieu is grossly abnormal because the differentiation of the external genitalia is normal. Thus, at least in terms of gross markers of biological sex, it appears that most individuals with GID are somatically normal.51 This has led some researchers to consider alternative biological pathways that might affect psychosexual differentiation or to reconsider prenatal hormone theory in terms of behavioral-genital dissociations: that is, hormonal effects on the brain but not the genitals. Such researchers have has examined behavior genetics (the liability for cross-gender behavior),21,52 altered ratio of the length of the second digit to that of the fourth digit,53 handedness,54,55 sibling sex ratio and birth order,56–58 and neuroanatomical substrates.59,60 This line of research reviewed has begun to identify some characteristics of children and adults with GID that may well have a biological basis. In some respects, however, it has been easier to rule out candidate biological explanations, such as the influence of gross anomalies in prenatal hormonal exposure.61–62 Nonetheless, the study of new potential biological markers of variation in psychosexual differentiation has opened up avenues for novel empirical inquiry that will probably be pursued in the years to come.
Psychosocial Mechanisms
Psychosocial factors, to truly merit causal status, must be shown to influence the emergence of marked cross-gender behavior in the first few years of life. Otherwise, such factors are better conceptualized as perpetuating rather than predisposing. A few of the more prominent hypotheses and relevant data are discussed as follows.
PRENATAL GENDER PREFERENCE
It is common for parents to express a gender preference before a child is born. Other things being equal, parents have a child of the nonpreferred sex about 50% of the time. Are parents of children with GID more likely than control parents to report having had a desire for a child of the opposite sex? The simple answer appears to be no, at least with regard to the mothers of boys with GID.63 We did find, however, that the maternal wish for a girl was significantly associated with the sex composition and birth order of the sibship. In families of affected boys with only older brothers, the percentage of mothers who recalled a desire for a daughter was significantly higher than among the families of probands with other sibship combinations; however, the same pattern was observed in a control group.63 It was, noted, however, that among mothers of boys with GID who had desired daughters, a small subgroup appeared to experience what might be termed pathological gender mourning.31 The wish for a daughter was acted out (e.g., by cross-dressing the boy) or expressed in other ways. These mothers often had severe depression, which was lifted only when the boy began to act in a certain feminine manner. This clinical observation, however, must be examined in much greater detail, including understanding how the wish for a girl, when it occurs, is resolved in most cases.
SOCIAL REINFORCEMENT
Understanding the role of parent socialization in the genesis and/or perpetuation of GID (e.g., through reinforcement principles or modeling) has been influenced by the normative developmental literature on sex-dimorphic sex-typed behavior.7 It has also been influenced by the seminal but controversial observations of Money and colleagues61 that the rearing environment was the predominant determinant of gender identity in children with physical intersex conditions.
Clinicians of diverse theoretical persuasions have consistently reported that the parental response to early cross-gender behavior in children with GID is typically neutral (tolerance) or even encouraging.31 Regarding boys with GID, Green45 concluded that “what comes closest so far to being a necessary variable is that, as any feminine behavior begins to emerge, there is no discouragement of that behavior by the child’s principal caretaker” (p 238; italics in original). An example of this is illustrated in the following email correspondence from a mother, who was considering an assessment of her 5-year-old son, who strongly desired to be a girl:
We adore Darryl just the way he is and wouldn’t want to change a thing about him. We indulge him in Barbies, My Little Ponies, and princess dress-up clothing… whatever he wants, he gets.
In my clinic, Mitchell,64 in a structured interview study, found that mothers of GID boys were more likely to tolerate/encourage feminine behaviors and less likely to encourage masculine behaviors than were the mothers of both clinical patients and normal control boys. The reasons for such tolerance appear to be quite variable, including parental values and goals regarding psychosexual development; feedback from professionals that the behavior is within normal limits and “only a phase”; parental conflicts about issues of masculinity and femininity; and parental psychopathology and discord, which leave the parents relatively preoccupied and thus unresponsive to their child’s behavior. Such underlying motivations can be examined only in a thorough clinical evaluation.
TRANSACTIONAL PROCESSES
Many scholars adhere to a transactional model of gender differentiation.7 A child’s gender identity is constructed gradually over time: even if a biological predisposition does affect the likelihood of a child engaging in varying degrees of sex-typical versus sex-atypical behavior, many other factors probably either accentuate or attenuate its expression. Parental responses, as noted earlier, may be one such factor. Children themselves contribute to this process as they develop complex cognitive constructions of what it means to be a boy or a girl.65 The child’s behavior may be both affected by and influence the quality of the relationship with his or her parents. A child’s gender identity will affect emerging peer relationships, and the peer group may play a role in further gender differentiation.7
As another example of the direction-of-effect conundrum, consider the literature on parent-child relationships. In clinical studies of boys with GID, Stoller66 described a situation in which the relationship between mother and son was overly close and that between father and son was distant and peripheral. Stoller claimed that such qualities were of etiological relevance: “The more mother and the less father, the more femininity” (p 25). He argued that GID in boys was a “developmental arrest… in which an excessively close and gratifying mother-infant symbiosis, undisturbed by father’s presence, prevents a boy from adequately separating himself from his mother’s female body and feminine behavior” (p 25). Green41 assessed quantitatively the amount of shared time between fathers of feminine boys and control boys during the first 5 years of life. The fathers of feminine boys reported spending less time with their sons from the second to fifth year than did the fathers of the controls.
The picture that emerges for GID boys, then, is one in which they feel closer to their mothers than to their fathers.41 From a causal perspective, however, the direction-of-effect question can be raised: Do GID boys feel this way because their own behavior influences the quality of parent-child relations, or are there predisposing parental characteristics that are influential? Or are both factors involved, resulting in a complex transactional chain?
SUMMARY
The research reviewed here has identified several psychosocial mechanisms thought to be involved in the genesis and perpetuation of GID. Some specific, relatively simple hypotheses have been shown to be incorrect. Others, such as parental response to cross-gender behavior when it first emerges, appear to have greater clinical and empirical support. The emphasis here, however, has also been to highlight the complex psychosocial chain and the difficulties in identifying direction-of-effect processes. On this point, considerably more research attention is clearly warranted.
THERAPEUTICS
Ethical Considerations
Consider the following clinical scenarios:
Any contemporary pediatric clinician responsible for the therapeutic care of children and adolescents with GID is quickly introduced to complex social and ethical issues pertaining to the politics of sex and gender in post-modern Western culture and will have to think them through carefully. The scenarios just described, as well as many others, require the clinician to think long and hard about theoretical, ethical, and treatment issues.
Treatment of Children
Elsewhere, I have identified five rationales for intervention in the treatment literature on children with GID: (1) reduction in social ostracism, (2) treatment of underlying psychopathology, (3) treatment of the underlying distress, (4) prevention of transsexualism in adulthood, and (5) prevention of homosexuality in adulthood.67
In my view, the first four rationales are clinically defensible, but the fifth is not. Therefore, on this last point, further explication is warranted. Some critics have argued that clinicians consciously or unconsciously accept the prevention of homosexuality as a legitimate therapeutic goal.68 Others have asserted, albeit without empirical documentation, that treatment of GID results in harm to children who are “homosexual” or “prehomosexual.”69
The various issues regarding the relation between GID and homosexuality are complex, both clinically and ethically. Three points, although brief, can be made. First, until it has been shown that any form of treatment for GID during childhood affects later sexual orientation, Green’s41 discussion of whether parents have the right to seek treatment to maximize the likelihood of their child becoming heterosexual is moot. From an ethical standpoint, however, the treating clinician has an obligation to inform parents about the state of the empirical database. Second, I have argued elsewhere that some critics incorrectly conflate gender identity and sexual orientation, regarding them as isomorphic phenomena, as do some parents.70 In psychoeducational work with parents, clinicians can review the various explanatory models regarding the statistical linkage between gender identity and sexual orientation71 but also discuss their distinctness as psychological constructs. Third, many contemporary pediatric clinicians emphasize that the primary goal of treatment with children with GID is to resolve the conflicts that are associated with the disorder, regardless of the child’s eventual sexual orientation.
If the clinician is to provide treatment for a child with GID, it is important to bear in mind that there has been no single randomized controlled treatment trial. The practitioner must rely largely on the “clinical wisdom” that has accumulated in the case report literature and the conceptual underpinnings that inform the various approaches to intervention.
Behavior Therapy
The literature contains 13 single-case reports in which investigators employed a behavior therapy approach to the treatment of GID in children.67,71 The classical behavioral approach is to assume that children learn sex-typed behaviors much as they learn any other behaviors and that sex-typed behaviors can be shaped, at least initially, by encouraging some and discouraging others. Accordingly, behavior therapy for GID systematically arranges to have rewards follow gender-typical behaviors and to have no rewards (or perhaps punishments) follow cross-gender behaviors.
One type of intervention employed has been termed differential social attention or social reinforcement. This type of intervention has been applied in clinic settings, particularly to sex-typed play behaviors. The therapist first establishes with baseline measures that the child prefers playing with cross-sex toys or dress-up apparel rather than same-sex toys or dress-up apparel. A parent or stranger is then introduced into the playroom and instructed to attend to the child’s same-sex play (e.g., by looking, smiling, and verbal praise) and to ignore the child’s cross-sex play (e.g., by looking away and pretending to read). Such adult responses seem to elicit rather sharp changes in play behavior.
The field of behavior therapy has produced no new case reports since the 1980s, although its principles are often used in broader treatment approaches that involve the parents. This publication gap is odd, because more contemporary behavioral approaches, such as cognitive-behavior therapy, are now used so widely with other disorders.
Behavior therapy with an emphasis on the child’s cognitive structures regarding gender could be an interesting and novel approach to treatment. There is now a fairly large literature on the development of cognitive gender schemas in nonreferred children.65 It is possible that children with GID have more elaborately developed cross-gender schemas than same-gender schemas and that more positive affective appraisals are differentiated for the latter than for the former (e.g., in boys, “Girls get to wear prettier clothes” vs. “Boys are too rough”). A cognitive approach to treatment might help children with GID to develop more flexible and realistic notions about gender-related traits (e.g., “Boys can wear pretty cool clothes, too” or “There are lots of boys who don’t like to be rough”), which may result in more positive gender feelings about being a boy or being a girl.
Psychotherapy
There is a large case report literature on the treatment of children with GID through psychoanalysis, psychoanalytic psychotherapy, or psychotherapy, some reports of which are quite detailed and rich in content.67,71 The psychoanalytic treatment literature is more diverse than the behavior therapy literature, including varied theoretical approaches to understanding the putative cause of GID (e.g., classical, object relations, and self psychology); nevertheless, a number of recurring themes can be gleaned from this case report literature.
Psychoanalytic clinicians generally emphasize that the cross-gender behavior emerges during the “pre-oedipal” years;66 accordingly, they stress the importance of understanding how the GID relates to other developmental phenomena salient during these years (e.g., attachment relations and the emergence of the autonomous self). Oedipal issues are also deemed important, but these are understood within the context of prior developmental interferences and conflicts. Psychoanalytic clinicians also place great weight on the child’s overall adaptive functioning, which they view as critical in determining the therapeutic approach to the specific referral problem.
Apart from the general developmental perspective inherent to a psychoanalytic understanding of psychopathology, there is also a gender-specific perspective on development.7 Many developmental psychologists, for example, note that the first signs of normative gender development appear during the toddler years, including the ability to correctly self-label as a boy or a girl. Thus, early gender identity formation intersects quite neatly with analytical views on the early development of the sense of self in more global terms. It is likely, therefore, that the putative pathogenic mechanisms identified in the development of GID are likely to have a greater effect only if they occur during the alleged sensitive period for gender identity formation.61
An overall examination of the available case reports suggests that psychotherapy, like behavior therapy, does have some beneficial influence on the sex-typed behavior of children with GID. However, the effectiveness of psychoanalytic psychotherapy, like that of behavior therapy, has never been demonstrated in an outcome study comparing children randomly assigned to treated and untreated conditions. Moreover, many of the cases cited previously did not consist solely of psychoanalytic treatment of the child. The parents were often also in therapy, and, in some of the cases, the child was an inpatient and thus exposed to other interventions. It is impossible to disentangle these other potential therapeutic influences from the effect of the psychotherapy alone.
Treatment for the Parents
Two rationales have been offered for parental involvement in treatment. The first emphasizes the hypothesized role of parental dynamics and psychopathology in the genesis or maintenance of the disorder. According to this perspective, individual therapy with the child probably proceeds more smoothly and quickly if the parents are able to gain some insight into their own contribution to their child’s difficulties. Many clinicians who have worked extensively with gender-disturbed children subscribe to this rationale.72,73,74 Assessment of psychopathology and the marital relationship in the parents of children with GID reveals great variability in adaptive functioning, which may well prove to be a prognostic factor.31,39
In addition, parents benefit from regular, formalized contact with the therapist to discuss day-to-day management issues that arise in carrying out the overall therapeutic plan. Work with parents can focus on the setting of limits with regard to cross-gender behavior, such as cross-dressing, cross-gender role and fantasy play, and cross-gender toy play and, at the same time, attempting to provide alternative activities (e.g., encouragement of same-sex peer relations and involvement in more gender-typical and neutral activities). In addition, parents can work on conveying to their child that they are trying to help him or her feel better about being a boy or a girl and that they want their child to be happier in this regard. Some parents, especially the well-functioning and intellectually sophisticated ones, are able to carry out these recommendations relatively easily and without ambivalence. Many parents, however, require ongoing support in implementing the recommendations, perhaps because of their own ambivalence and reservations about gender identity issues.71
Supportive Treatments
Clinicians critical of conceptualizing marked cross-gender behavior in children as a disorder have provided a dissenting perspective to the treatment approaches described so far.75–77 These clinicians conceptualize GID or pervasive gender-variant behavior from an essentialist perspective—that it is fully constitutional or congenital in origin—and are skeptical about the role of psychosocial or psychodynamic factors. As an example of this perspective, Bockting and Ehrbar78 argued that “instead of attempts to change the child’s gender identity or role, treatment should assist the family to accept the child’s authentic gender identity and affirm a gender role expression that is most comfortable for that child” (p 128). Along similar lines, Menvielle and Tuerk75 noted that although it might be helpful to set limits on pervasive cross-gender behaviors that may contribute to social ostracism, their primary treatment goal (offered in the context of a parent support group) was “not at changing the children’s behavior, but at helping parents to be supportive and to maximize opportunities for the children’s adjustment” (p 1010). Menvielle and associates76 took a somewhat stronger position, by arguing that “Therapists who advocate changing gender-variant behaviors should be avoided” (p 45).
Because comparative treatment approaches are not available, it is not possible to say whether this supportive or “cross-gender affirming” approach will result in both short-term and long-term outcomes any different from the more traditional approaches to treatment. The supportive approach does, however, highlight a variety of theoretical and clinical disagreements, which will be resolved only by more systematic research on therapeutics.
Adolescents
In adolescents with GID, there are three broad clinical issues that require evaluation: (1) the phenomena pertaining to the GID itself, (2) sexual orientation, and (3) psychiatric comorbidity. Gender-dysphoric adolescents with a childhood onset of cross-gender behavior typically have a homosexual orientation (i.e., they are attracted to members of their own “birth sex”). Some such adolescents may not report any sexual feelings, but follow-up typically reveals the emergence of same-sex attractions. Thus, the clinician must evaluate simultaneously two dimensions of the patient’s psychosexual development: current gender identity and current sexual orientation.
The psychotherapy treatment literature on adolescents with GID has been very poorly developed and is confined to a few case reports.31,67,71 In general, the prognosis for adolescents in resolving the GID is more guarded than it is for children. This state of affairs is similar to that of other child psychiatric disorders: The longer a disorder persists, the less is the likelihood that it will remit, with or without treatment. From a clinical management point of view, two key issues need to be considered: (1) Some adolescents with GID are not particularly good candidates for psychotherapy because of comorbid disorders and general life circumstances, and (2) some adolescents with GID have little interest in psychologically oriented treatment and are quite adamant about proceeding with hormonal and surgical sex reassignment.
Before recommending hormonal and surgical interventions, many clinicians encourage adolescents with GID to consider alternatives to this invasive and expensive treatment. One area of inquiry can, therefore, explore the meaning behind the adolescent’s desire for sex reassignment and whether there are viable alternative lifestyle adaptations. The most common area of exploration in this regard pertains to the patient’s sexual orientation. Some adolescents with GID recall that they always felt uncomfortable growing up as boys or as girls but that the idea of “sex change” did not occur until they became aware of homoerotic attractions. For some of these youngsters, the idea that they might be gay or homosexual is abhorrent (internalized homophobia).
For some such adolescents, psychoeducational work can explore their attitudes and feelings about homosexuality. Youth support groups or group therapy may provide an opportunity for youngsters to meet gay adolescents and can be a useful intervention. In some cases, the gender dysphoria may resolve, and a homosexual adaptation ensues.
For adolescents with persistent gender dysphoria, there is considerable evidence that it often interferes with general social adaptation, including general psychiatric impairment, conflicted family relations, and dropping out of school. For these youngsters, therefore, the treating clinician can consider two main options: (1) supportive management until the adolescent turns 18 and can be referred to an adult gender identity clinic or (2) “early” institution of contrasex hormonal treatment.
An option for treatment of gender-dysphoric adolescents is to prescribe puberty-blocking luteinizing hormone–release agonists (e.g., depot leuprolide or depot triptorelin) that facilitate more successful passing as the opposite sex.79 Such medication can suppress the development of secondary sex characteristics, such as facial hair growth and voice deepening in adolescent boys, which make it more difficult to pass in the female social role. Cohen-Kettenis and van Goozen46 reported that early cross-sex hormone treatment for adolescents younger than 18 years facilitated the complex psychosexual and psychosocial transition to living as a member of the opposite sex and resulted in a lessening of the gender dysphoria (see also Smith et al47). Although such early hormonal treatment remains controversial,80 it may be the treatment of choice once the clinician is confident that other options have been exhausted.26,81
Summary
The treatment literature on GID in children and adolescents has many gaps. As reviewed previously, the literature for children has been confined to a lot of case reports from varying theoretical perspectives, with little in the way of comparative evaluation. Clinicians have varied perspectives on what to treat, and thus the developmental-behavioral pediatrician needs to be aware of the complex ideological, political, and theoretical perspectives that underlie the different positions. For adolescents, there is an emerging consensus by clinicians who work with gender-dysphoric adolescents that cross-sex hormone treatment may well be a reasonable early therapeutic intervention once it becomes clear that psychosocial approaches have not resulted in a reduction of the gender dysphoria.82 For both children and adolescents, it is advisable, in my view, that referrals be made to clinicians with a strong background in child and adolescent developmental psychopathology and, when feasible, to therapists with at least some familiarity with the literature on both normative and applied gender development.
FUTURE DIRECTIONS
Although gender development and its disorders has been studied by a relatively small number of trained clinicians and researchers, considerable progress has been made in a number of areas since the introduction of the GID diagnosis to the third edition of the Diagnostic and Statistical Manual of Mental Disorders in 1980. This has included careful description of phenomena, the development of valid assessment techniques, some studies on causes, and follow-up studies on natural history.
Nonetheless, various issues require further attention. These include consideration of refinements to the DSM-IV-TR criteria for GID, a better understanding of body image development in children with GID, more research on causes, and continued study of long-term outcome. Of most importance, perhaps, is what is lacking in the literature: well-designed treatment studies, particularly for children. In an era in which increasing emphasis is placed on best-practice and evidence-based treatment, it is important to fill this gap in order to resolve the contemporary debates regarding how to most effectively provide clinical care for children and adolescents who experience tremendous distress and conflict about their gender identity.
1 American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 4th ed. Washington, DC: American Psychiatric Association, 2000. Text Revision
2 Cloud J: His name is Aurora. Time (September 25):90–91, 2000. (Available at: http://www.time.com/time/maga-zine/article/0,9171,998007,00.html; accessed 2/18/07.)
3 Bauer G. Gender bender. Saturday Night. 2002;117(6):60-62. 64
4 Sroufe LA. Considering normal and abnormal together: The essence of developmental psychopathology. Dev Psychopathol. 1990;2:335-347.
5 Grumbach MM, Hughes IA, Conte FA. Disorders of sex differentiation. In: Larsen PR, Kronenberg HM, Melmed S, et al, editors. Williams Textbook of Endocrinology. 10th ed. Philadelphia: WB Saunders; 2003:842-1002.
6 Vilain E. Genetics of sexual development. Annu Rev Sex Res. 2000;11:1-25.
7 Ruble DN, Martin CL, Berenbaum SA. Gender development. In: Eisenberg N, Damon W, Lerner RM, editors. Handbook of Child Psychology, Volume 3: Social, Emotional, and Personality Development. 6th ed. New York: Wiley; 2006:858-932.
8 Kohlberg L. A cognitive-developmental analysis of children’s sex-role concepts and attitudes. In: Maccoby EE, editor. The Development of Sex Differences. Stanford, CA: Stanford University Press; 1966:82-173.
9 Stoller RJ. The hermaphroditic identity of hermaphrodites. J Nerv Ment Dis. 1964;139:453-457.
10 Chivers ML, Rieger G, Latty E, et al. A sex difference in the specificity of sexual arousal. Psychol Sci. 2004;15:736-744.
11 Rosen RC, Beck JG. Patterns of Sexual Arousal: Psy-chophysiological Processes and Clinical Applications. New York: Guilford, 1988.
12 Schrimshaw EW, Rosario M, Meyer-Bahlburg HFL, et al. Test-retest reliability of self-reported sexual behavior, sexual orientation, and psychosexual milestones among gay, lesbian, and bisexual youths. Arch Sex Behav. 2006;35:225-234.
13 Laumann EO, Gagnon JH, Michael RT, et al. The Social Organization of Sexuality: Sexual Practices in the United States. Chicago: University of Chicago Press, 1994.
14 Freund K, Watson R, Rienzo D. Heterosexua lit y, homosexuality, and erotic age preference. J Sex Res. 1989;26:107-117.
15 Zucker KJ, Blanchard R. Transvestic fetishism: Psychopathology and theory. In: Laws DR, O’Donohue W, editors. Sexual Deviance: Theory, Assessment, and Treatment. New York: Guilford; 1997:253-279.
16 Bakker A, van Kesteren PJM, Gooren LJG, et al. The prevalence of transsexualism in The Netherlands. Acta Psychiatr Scand. 1993;87:237-238.
17 Långström N, Zucker KJ. Transvestic fetishism in the general population: Prevalence and correlates. J Sex Marital Ther. 2005;31:87-95.
18 Zucker KJ. Cross-gender-identified children. In: Steiner BW, editor. Gender Dysphoria: Development, Research, Management. New York: Plenum Press; 1985:75-174.
19 Achenbach TM, Edelbrock C. Manual for the Child Behavior Checklist and Revised Child Behavior Profile. Burlington: University of Vermont, Department of Psychiatry, 1983.
20 Zucker KJ, Bradley SJ, Sanikhani M. Sex differences in referral rates of children with gender identity disorder: Some hypotheses. J Abnorm Child Psychol. 1997;25:217-227.
21 Beijsterveldt CEM, Hudziak JJ, Boomsma DI. Genetic and environmental influences on cross-gender behavior and relation to behavior problems: A study of Dutch twins at ages 7 and 10 years. Arch Sex Behav. 2006;35:647-658.
22 Cohen-Kettenis PT, Owen A, Kaijser VG, et al. Demographic characteristics, social competence, and behavior problems in children with gender identity disorder: A cross-national, cross-clinic comparative analysis. J Abnorm Child Psychol. 2003;31:41-53.
23 Zucker KJ, Owen A, Bradley SJ, et al. Gender-dysphoric children and adolescents: A comparative analysis of demographic characteristics and behavioral problems. Clin Child Psychol Psychiatry. 2002;7:398-411.
24 Cohen-Kettenis PT, Pfäfflin F. Transgenderism and Intersexuality in Childhood and Adolescence: Making Choices. Thousand Oaks, CA: Sage Publications, 2003.
25 Zucker KJ, Finegan JK, Doering RW, et al. Two subgroups of gender-problem children. Arch Sex Behav. 1984;13:27-39.
26 Zucker KJ. Gender identity disorder. In: Wolfe DA, Mash EJ, editors. Behavioral and Emotional Disorders in Adolescents: Nature, Assessment, and Treatment. New York: Guilford; 2006:535-562.
27 Lee T. Trans(re)lations: Lesbian and female to male transsexual accounts of identity. Womens Stud Int Forum. 2001;24:347-357.
28 McCarthy L: Off That Spectrum Entirely: A Study of Female-Bodied Transgender-Identified Individuals. Unpublished doctoral dissertation, University of Massachusetts, Amherst, 2003.
29 Zucker KJ. Measurement of psychosexual differentiation. Arch Sex Behav. 2005;34:375-388.
30 Zucker KJ. Gender identity disorder. In: Hooper SR, Hynd GW, Mattison RE, editors. Child Psychopathology: Diagnostic Criteria and Clinical Assessment. Hillsdale, NJ: Erlbaum; 1992:305-342.
31 Zucker KJ, Bradley SJ. Gender Identity Disorder and Psychosexual Problems in Children and Adolescents. New York: Guilford, 1995.
32 Zucker KJ, Bradley SJ, Lowry Sullivan CB, et al. A gender identity interview for children. J Pers Assess. 1993;61:443-456.
33 Johnson LL, Bradley SJ, Birkenfeld-Adams AS, et al. A parent-report Gender Identity Questionnaire for Children. Arch Sex Behav. 2004;33:105-116.
34 Cohen-Kettenis PT, Wallien M, Johnson LL, et al. A parent-report Gender Identity Questionnaire for Children: A cross-national, cross-clinic comparative analysis. Clin Child Psychol Psychiatry. 2006;11:397-405.
35 Fridell SR, Owen-Anderson A, Johnson LL, et al. The Playmate and Play Style Preferences Structured Interview: A comparison of children with gender identity disorder and controls. Arch Sex Behav. 2006;35:729-737.
36 Deogracias JJ, Johnson LL, Meyer-Bahlburg HFL, et al: The Gender Identity/Gender Dysphoria Questionnaire for Adolescents and Adults. J Sex Res, in press.
37 Coates S, Person ES. Extreme boyhood femininity: Isolated behavior or pervasive disorder? J Am Acad Child Psychiatry. 1985;24:702-709.
38 Zucker KJ, Bradley SJ, Lowry Sullivan CB. Traits of separation anxiety in boys with gender identity disorder. J Am Acad Child Adolesc Psychiatry. 1996;35:791-798.
39 Zucker KJ: Predictors of Psychopathology in Boys with Gender Identity Disorder. Presented in the Institute on Gender Identity Disorder in Children and Adolescents (Bradley SJ, Chair), American Academy of Child and Adolescent Psychiatry and Canadian Academy of Child Psychiatry, Toronto, October 2005.
40 Bailey JM, Zucker KJ. Childhood sex-typed behavior and sexual orientation: A conceptual analysis and quantitative review. Dev Psychol. 1995;31:43-55.
41 Green R. The “Sissy Boy Syndrome” and the Development of Homosexuality. New Haven, CT: Yale University Press, 1987.
42 Kinsey AC, Pomeroy WB, Martin CE. Sexual Behavior in the Human Male. Philadelphia: WB Saunders, 1948.
43 Cohen-Kettenis PT. Gender identity disorder in DSM? [Letter]. J Am Acad Child Adolesc Psychiatry. 2001;40:391.
44 Drummond KD: A follow-up study of girls with gender identity disorder. Unpublished master’s thesis, Ontario Institute for Studies in Education of the University of Toronto, 2006.
45 Green R. Sexual Identity Conflict in Children and Adults. New York: Penguin, 1974.
46 Cohen-Kettenis PT, van Goozen SHM. Sex reassignment of adolescent transsexuals: A follow-up study. J Am Acad Child Adolesc Psychiatry. 1997;36:263-271.
47 Smith YLS, van Goozen SHM, Cohen-Kettenis PT. Adolescents with gender identity disorder who were accepted or rejected for sex reassignment surgery: A prospective follow-up study. J Am Acad Child Adolesc Psychiatry. 2001;40:472-481.
48 Wallen K, Baum MJ. Masculinization and defeminization in altricial and precocial mammals: Comparative aspects of steroid hormone action. Horm Brain Behav. 2002;4:385-423.
49 Cohen-Bendahan CCC, van de Beek C, Berenbaum SA. Prenatal sex hormone effects on child and adult sex-typed behavior: Methods and findings. Neurosci Bio-behav Rev. 2005;29:353-384.
50 Dessens AB, Slijper FME, Drop SLS. Gender dysphoria and gender change in chromosomal females with congenital adrenal hyperplasia. Arch Sex Behav. 2005;34:389-397.
51 Meyer-Bahlburg HFL. Introduction: Gender dysphoria and gender change in persons with intersexuality. Arch Sex Behav. 2005;34:371-373.
52 Coolidge FL, Thede LL, Young SE. The heritability of gender identity disorder in a child and adolescent twin sample. Behav Genet. 2002;32:251-257.
53 Schneider HJ, Pickel J, Stalla GK. Typical female 2nd-4th finger length (2D: 4D) ratios in male-to-female transsexuals-Possible implications for prenatal androgen exposure. Psychoneuroendocrinology. 2006;31:265-269.
54 Zucker KJ, Beaulieu N, Bradley SJ, et al. Handedness in boys with gender identity disorder. J Child Psychol Psychiatry. 2001;42:767-776.
55 Green R, Young R. Hand preference, sexual preference, and transsexualism. Arch Sex Behav. 2001;30:565-574.
56 Blanchard R, Zucker KJ, Bradley SJ, et al. Birth order and sibling sex ratio in homosexual male adolescents and probably prehomosexual feminine boys. Dev Psychol. 1995;31:22-30.
57 Zucker KJ, Green R, Coates S, et al. Sibling sex ratio of boys with gender identity disorder. J Child Psychol Psychiatry. 1997;38:543-551.
58 Green R. Birth order and ratio of brothers to sisters in transsexuals. Psychol Med. 2000;30:789-795.
59 J-N Zhou, Hofman MA, Gooren LJ, et al. A sex difference in the human brain and its relation to transsexu-ality. Nature. 1995;378:68-70.
60 Kruiver FPM, J-N Zhou, Pool CW, et al. Male-to-female transsexuals have female neuron numbers in a limbic nucleus. J Clin Endocrinol Metab. 2000;85:2034-2041.
61 Money J, Hampson J, Hampson J. Imprinting and the establishment of gender role. Arch Neurol Psychiatry. 1957;77:333-336.
62 Meyer-Bahlburg HFL, Gruen RS, New MI. Gender change from female to male in classical congenital adrenal hyperplasia. Horm Behav. 1996;30:319-332.
63 Zucker KJ, Green R, Garofano C, et al. Prenatal gender preference of mothers of feminine and masculine boys: Relation to sibling sex composition and birth order. J Abnorm Child Psychol. 1994;22:1-13.
64 Mitchell JN: Maternal Influences on Gender Identity Disorder in Boys: Searching for Specificity. Unpublished doctoral dissertation, York University, Downsview, Ontario, 1991.
65 Martin CL, Ruble DN, Szkrybalo J. Cognitive theories of early gender development. Psychol Bull. 2002;128:903-933.
66 Stoller RJ. Presentations of Gender. New Haven, CT: Yale University Press, 1985.
67 Zucker KJ: Gender identity disorder in children, adolescents, and adults. In Gabbard GO, ed: Gabbard’s Treatments of Psychiatric Disorders, 4th ed. Washington, DC: American Psychiatric Press, in press.
68 Pleak RR. Ethical issues in diagnosing and treating gender-dysphoric children and adolescents. In: Rottnek M, editor. Sissies & Tomboys: Gender Nonconformity & Homosexual Childhood. New York: New York University Press; 1999:44-51.
69 Isay RA. Remove Gender Identity Disorder in DSM. Psychiatric News. 1997;32(Nov 21):9. 13
70 Zucker KJ. Gender Identity Disorder in the DSM-IV [Letter]. J Sex Marital Ther. 1999;25:5-9.
71 Zucker KJ. Gender identity disorder in children and adolescents. Gabbard GO, editor. Treatments of Psychiatric Disorders, 3rd ed, 2. Washington, DC: American Psychiatric Press, 2001;2069-2094.
72 Coates S, Wolfe S. Gender identity disorder in boys: The interface of constitution and early experience. Psy-choanal Inq. 1995;15:6-38.
73 Newman LE. Treatment for the parents of feminine boys. Am J Psychiatry. 1976;133:683-687.
74 Zucker KJ, Bradley SJ, Doering RW, et al. Sex-typed behavior in cross-gender-identified children: Stability and change at a one-year follow-up. J Am Acad Child Psychiatry. 1985;24:710-719.
75 Menvielle EJ, Tuerk C. A support group for parents of gender non-conforming boys. J Am Acad Child Adolesc Psychiatry. 2002;41:1010-1013.
76 Menvielle EJ, Tuerk C, Perrin EC. To the beat of a different drummer: The gender-variant child. Contemp Pediatr. 2005;22(2):38-39. 41, 43, 45-46
77 Lev AI. Transgender Emergence: Therapeutic Guidelines for Working with Gender-Variant People and Their Families. New York: Haworth, 2004.
78 Bockting WO, Ehrbar RD. Commentary: Gender variance, dissonance, or identity disorder? J Psychol Hum Sex. 2005;17(3/4):125-134.
79 Gooren L, Delemarre-van de Waal H. The feasibility of endocrine interventions in juvenile transsexuals. J Psychol Hum Sex. 1996;8(4):69-84.
80 Beh H, Diamond M. Ethical concerns related to treating gender nonconformity in childhood and adolescence: Lessons from the Family Court of Australia. Health Matrix Clevel. 2005;15:239-283.
81 Cohen-Kettenis PT. Gender identity disorders. In: Gillberg C, Harrington R, H-C Steinhausen, editors. A Clinician’s Handbook of Child and Adolescent Psychiatry. Cambridge, UK: Cambridge University Press; 2005:695-725.
82 Meyer W, Bockting WO, Cohen-Kettenis P, et al. The Harry Benjamin International Gender Dysphoria Association’s Standards of Care for Gender Identity Disorders, Sixth version. J Psychol Hum Sex. 2001;13(1):1-30.
25C. Variations in Sexual Orientation and Sexual Expression
The majority of adults are content with gender definitions that are consistent with their anatomical sex and are physically and emotionally attracted to adults of different sex. An increasingly visible minority of adults are convinced that their social and emotional gender is discordant with their biological sex (i.e., they are transgendered) or are attracted to people of the same sex (i.e., they are homosexual). Teenagers and occasionally even preteenagers may find themselves believing that or questioning whether they are in either of these categories. Because both homosexuality and transgenderism are severely stigmatized in society, this process of a person’s wondering and coming to believe that he or she is gay, lesbian, bisexual, or transgender is frequently associated with considerable distress for these young people and their families. Family and social support may provide protection against some of the disastrous effects of stigmatization. Pediatricians in primary care, adolescent medicine, and developmental-behavioral pediatrics, and their professional colleagues, have an important role to play in providing and bolstering this support.
This section of the chapter on sexuality is in four sections: (1) current theories about the genesis of variations in sexual orientations; (2) the development of a gay, lesbian, or trangender identity; (3) the well-being of children whose parents are gay or lesbian; and (4) opportunities for pediatric interventions.
Only a few general reviews have covered this particular assortment of topics since the 1990s. Summaries of the trajectory of gay and lesbian development, concerns about these adolescents, and resources for improvement are included in several recent reviews1,2,4 and form the basis of the American Academy of Pediatrics’ revised Clinical Statement on Homosexuality.3
Two reviews of the well-being of children who were raised by lesbian or gay parents have been published.5,6 In addition, these data are summarized in support of marriage as a potential benefit for these children.7
[/level-membership-for-pediatrics-category]