Chapter 66 Severe and multiple trauma
Trauma can be defined as physical injury from mechanical energy. It is usually categorised as blunt or penetrating. In Western countries, severe blunt trauma is common, caused by road crashes, falls and, less frequently, blows and assault. Severe penetrating trauma, usually from stabbings and gunshots, is less common except in larger cities of the USA,1,2 South Africa and war zones. Blunt trauma is often more difficult to treat than penetrating trauma. Assessment is more difficult, because injuries are frequently internal, multiple and not obvious initially. The risk of missing serious injuries can only be lessened by a systematic approach and repeated assessments.3–5
ASSESSMENT AND PRIORITIES
TRIAGE
BASIC TREATMENT PRINCIPLES
A systematic approach to managing severe and multiple trauma is important. Effective programmes developed by the American College of Surgeons are now well established.6 A number of basic treatment principles apply to all severe trauma patients.
EMERGENCY ASSESSMENT (PRIMARY SURVEY)
The following must be recognised and treated before anything else:
OXYGEN AND VENTILATORY THERAPY
High-flow oxygen by mask is given to all trauma patients. However, patients with severe trauma frequently require ventilatory support. A restless uncooperative patient should be intubated under a rapid sequence induction to facilitate resuscitation.
BLOOD CROSSMATCH AND TESTS
Six units of red cells should be crossmatched urgently, but it is impossible to predict the amount of blood that will be required. Blood is concurrently sent for baseline haematological and biochemical tests, including blood ethanol level. Blood ethanol is clinically useful in assessing individual patients with depressed consciousness, quite apart from epidemiological and preventive medicine,7 and legal considerations.
CLINICAL EVALUATION OF INJURIES (SECONDARY SURVEY)
Injuries are easily missed in an emergency, especially when one injury is obvious. A secondary, and even a tertiary, survey should be performed.5 The back and the front of the patient should be examined. Special attention is paid to regions with external lacerations, contusions and abrasions. All body regions are examined systematically.
FACE
Bleeding into the airway should be excluded, and the face and jaws tested for abnormal mobility.
THORAX
Fractured ribs in themselves are not usually life-threatening but haemothorax, pneumothorax, lung contusion and chest wall instability (flail chest) will require attention if present. Less common but very serious injuries can occur to the heart and great vessels (see Chapter 69).
ABDOMEN
The spleen, liver and mesenteries are often damaged. Retroperitoneal haemorrhage is common. Injuries to the pancreas, duodenum and other hollow viscera are less frequent, and may be missed until signs of peritonitis occur. Renal injury with retroperitoneal haemorrhage is suggested by haematuria and loin pain (see Chapter 71).
SHOCK IN THE TRAUMA PATIENT
HYPOVOLAEMIC SHOCK
If the neck veins are empty, hypovolaemic shock should be inferred. Possible sites of blood loss causing shock are:
NEUROLOGICAL SHOCK
Patients with paraplegia or tetraplegia from spinal cord injury may have low blood pressure with warm dilated peripheries accompanied by lax anal tone and by priapism in the male (see Chapter 70). This is a diagnosis of exclusion and all causes of hypovolaemic shock (see above) must be sought.
ABDOMINAL ULTRASOUND
Its main usefulness is probably in the unstable patient when it is positive, to indicate the need for laparotomy without the necessity to proceed to diagnostic peritoneal lavage (DPL).9 FAST scans performed by enthusiastic amateurs in emergency departments without a treatment algorithm can be misleading and therefore worse than useless.
DIAGNOSTIC PERITONEAL LAVAGE
Diagnostic peritoneal lavage is indicated to diagnose intra-abdominal bleeding
Caution is needed with pregnancy, previous abdominal surgery or massive pelvic injury. Isotonic saline 1 l (or 10 ml/kg) is instilled into the peritoneal cavity, after drainage of the stomach and bladder. The presence of more than 10 ml frank blood on catheter aspiration necessitates immediate laparotomy; otherwise a lavage fluid specimen should be examined for red and white cell counts and amylase concentration. A red cell count over 100 000 per mm3, white cell count over 500 per mm3, or an increased amylase concentration suggests bleeding or viscus injury, and laparotomy should be undertaken immediately. These absolute figures are debatable and lower values are accepted in penetrating trauma.6,10 Peritoneal lavages inevitably result in some false-positive laparotomies. However, in severe trauma, morbidity of a non-therapeutic laparotomy (i.e. no definitive surgery) is small compared with the dire consequences of missing significant intra-abdominal injury.11
CT ABDOMEN
Abdominal CT is not indicated in shock, but can be useful in the stable patient. Improved availability of CT scanning, and technological advances with reduced scanning times and better definition, is increasingly favouring CT abdomen over DPL in patients who are sufficiently stable to tolerate the procedure safely. It needs to be performed quickly and safely, with gastric and i.v. contrast, and interpreted by radiologists experienced in trauma. Visualisation of abdominal and pelvic organs and haemorrhage is excellent,12,13 but results can be misleading and disastrous with poor technique.4
FLUID RESUSCITATION
FLUIDS
Almost all patients who are hypotensive or noticeably vasoconstricted will need blood transfusion. However, as crossmatched blood is not immediately available, other fluids are used first. Uncrossmatched group O Rh-negative blood is occasionally indicated in the exsanguinating patient, but in general transfusion of large quantities of blood is wasteful while bleeding is uncontrolled. The place of hypertonic fluids in trauma resuscitation is unresolved.
Isotonic saline or a balanced salt solution should be the first fluid infused. Shocked patients may need 2–3 l in the first few minutes. One litre bags or bottles and giving sets with in-line pumps should be used on all i.v. lines. If fluid resuscitation is likely to be extensive, warmed fluids and rapid infusion devices should be used. Albumin solutions (and probably other colloid resuscitation fluids) are contraindicated in trauma patients, since the SAFE study, conducted in ICU patients, showed higher mortality in patients given albumin, in the predetermined trauma subgroup, particularly in those with traumatic brain injury.14 By 20–30 minutes crossmatched red cells should be available. Platelets and fresh frozen plasma are reserved for documented or suspected coagulopathy (i.e. dilutional coagulopathy from fluids deficient in haemostatic factors, and disseminated intravascular coagulopathy (DIC) from prolonged shock).
LIMITED FLUID RESUSCITATION
In penetrating trauma, there is some evidence that extensive fluid resuscitation prior to haemostasis may be detrimental, presumably because of higher blood pressure, displacement of blood clot and dilution of coagulation factors.15
In contrast, in blunt trauma, the bleeding is often venous as well as arterial, with capillary oozing into the soft tissues which may continue for hours. It can often not be controlled, or can be only partly controlled, by operative surgery, interventional radiology or reduction and fixation of fractures. Accordingly, fluid resuscitation in the face of continuing blood loss is an important part of the treatment of circulatory shock in blunt trauma (see section on Inadequate resuscitation). Nevertheless, fluid resuscitation is not an alternative to haemostasis and must not be used as an excuse for delaying haemostasis in blunt trauma.
Furthermore, traumatic brain injury is often present in blunt trauma, which frequently involves several body regions. Hypotension is disastrous to an already injured brain, and must not be prolonged by deliberate underresuscitation (see Chapter 67, section on Traumatic brain injury – Emergency treatment).16–18
INADEQUATE RESUSCITATION
Patients in shock have depleted interstitial fluid as well as circulating blood volume, and need trauma resuscitation fluid volumes greater than the actual volume of blood lost. With blunt injury, volume losses often continue for 24–48 hours. Prolonged shock from delayed and inadequate resuscitation leads to renal failure, acute respiratory distress syndrome (ARDS), sepsis, DIC and multiple organ dysfunction.19,20
RADIOLOGY FOR TRAUMA PATIENTS
LATERAL CERVICAL SPINE
This should be performed in all patients with head injury or multiple injuries because cervical spine fractures are often missed. With head or facial injuries, a cervical fracture should be assumed initially and a cervical collar applied. The lateral cervical spine X-ray can be taken later. It is only an initial screening examination for cervical spine fractures and does not ‘clear’ the spine.
OTHER RADIOLOGICAL INVESTIGATIONS
THE EXSANGUINATING PATIENT
With exsanguination secondary to penetrating thoracic injury, there is a place for Emergency Room thoracotomy, but this approach has little place in blunt trauma.25 The exsanguinating blunt trauma patient needs rapid intubation, volume resuscitation, bilateral intrapleural drains or thoracostomies, chest and pelvic X-ray, and a rapid trip to the operating room if it seems likely that the bleeding is in the thorax or abdomen.
TRAUMATIC BRAIN INJURY (SEE CHAPTER 67)
EMERGENCY TREATMENT
Resuscitation measures, as in the Emergency assessment (primary survey) section above, are undertaken. Victims with one or both dilated unreactive pupils, or a rapidly deteriorating level of consciousness not due to hypoxia or shock, should be given mannitol 1 g/kg i.v. to relieve brainstem compression, until definitive diagnosis and treatment can be arranged. Mannitol should be given only if the patient has been adequately volume resuscitated as it may add to hypovolaemia. There is much interest in hypertonic saline, particularly in head trauma, and concentrated salt may eventually turn out to be a better agent than mannitol in this setting because it does not produce hypovolaemia.26,27
Shocked trauma patients with or without traumatic brain injuries require the same crystalloid resuscitation fluids. Treatment of shock and maintenance of cerebral perfusion are vital, as hypotension is disastrous to an already damaged brain.16–18 Contrary to common belief, sodium-containing fluids are not inherently dangerous in traumatic brain injury. However, after adequate resuscitation, further sodium administration is usually not indicated. Excessive (free) water is potentially dangerous, as it can lead to hypo-osmolar brain swelling.28
NEUROLOGICAL EVALUATION
Factors such as hypoxaemia, shock, alcohol, analgesics, anaesthetic agents, muscle relaxants and other drugs depress consciousness and confound neurological signs. Clinical neurological evaluation includes the Glasgow Coma Scale (GCS)29,30 and a search for lateralising signs.
CT scanning is indicated in all patients who will not obey verbal commands, especially if they are rendered neurologically inaccessible by sedative and relaxant agents. Lateralising motor or pupillary signs with a deteriorating level of consciousness are indications for immediate CT scanning (or, if unavailable, emergency burr holes). In an unstable patient, a laparotomy for intra-abdominal haemorrhage should take priority over a head CT scan.31
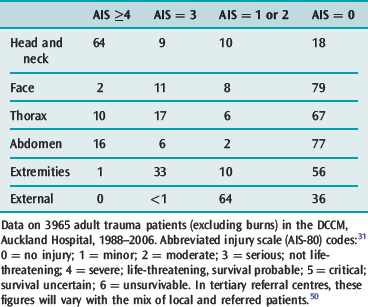
SEVERITY AND MORBIDITY OF TRAUMA
Severity of injury is measured by the abbreviated injury scale (AIS), updated over the years, most recently in 2005.32–34 AIS divides the body into six regions: head and neck, face, thorax, abdomen, pelvis and extremities, and external. Specific injuries in each body region are coded on a scale of 1 (minor), 2 (moderate), 3 (serious, not life-threatening), 4 (severe, life-threatening, survival probable), 5 (critical, survival uncertain) and 6 (unsurvivable). The AIS was designed for motor vehicle injuries, but has been validated for blunt and penetrating trauma. It can provide a basis for research, education, audit and allocation of resources.
Severity of trauma is related not just to the severity of individual injuries, but also to the combined effects of multiple injuries. Multiple injuries are graded by the injury severity score (ISS), which is an empirical system based on the AIS grades for the three worst body regions.35,36 ISS gives a score between 0 and 75 for total body injury; 16 or more indicates major trauma. Death with an ISS below 24 should be rare. Above an ISS of 25, there is a stepwise increase in mortality, with very high rates over 50.37,38
AIS and ISS study mostly the anatomy of injury. Other factors influence trauma mortality and morbidity, including age, pre-existing health, degree of physiological derangement, standard of prehospital and early hospital care and complications. Degree of physiological derangement can be measured by the revised trauma score,39 which is computed from the coded values of GCS, systolic blood pressure and respiratory rate, usually at admission to the emergency department. The TRISS severity index is based on the revised trauma score, ISS, and patient age.40 It correlates well with outcome, and has been used to compile survival norms for blunt and penetrating trauma.37,38 Physiological scoring systems such as APACHE (acute physiology, age and chronic health evaluation) do not work well for trauma patients (see Chapter 3).41,42 Preinjury illness (comorbidity) has a profound effect on trauma outcome.43
Shock influences trauma mortality and morbidity. The ‘golden hour’ is a catchy concept based on the observation that the longer the patient is in shock, the higher the probability of immediate or delayed complications. However, the specific timeframe of an hour has no real validity. Complications of shock include renal failure, acute respiratory distress syndrome, sepsis, liver failure and multiorgan dysfunction.19,20,44 Acute oliguric renal failure on the first day after trauma is now rare, but non-oliguric renal failure is often seen 2–4 days later, caused by the shock and delayed or inadequate resuscitation. It is often heralded by polyuria, which is misinterpreted as a sign of adequate resuscitation.
EPIDEMIOLOGY OF INJURIES
Only a minority of victims of severe trauma reach hospital alive.45,46 The majority of deaths are immediate (within minutes) at the scene of injury. Some deaths are early (within hours) in the emergency department or the operating room, and a few are late (after days or weeks) and occur in the ICU or ward.47 Those in the ICU are mostly from severe head injury within a few days and, less commonly, multiorgan dysfunction later.
Of trauma admissions to hospital, only a minority have severe or multiple trauma.48 In order of frequency, life-threatening injuries involve the head, abdomen and chest (Table 66.1), and are often multiple. The hospital services which this small number of severely injured patients use out of proportion to their numbers are major surgery, intensive care, radiography and CT scanning.48 Major trauma outcome studies in the USA,37 the UK38 and Australia49 offer valuable epidemiological data. The USA study found that the mortality of direct admissions is strongly related to serious head injury.
ORGANISATION OF TRAUMA CARE
Many of the problems of trauma care are organisational. Problems faced by health authorities are the provision of advanced care at the scene of injury, rapid transportation to hospital, policies on which hospitals should receive trauma patients, systems for rapid evaluation and decision-making in hospitals, and rapid, safe patient transfer between hospitals. If survival from major trauma is to be maximised, prehospital and hospital care must be coordinated.
Regionalisation of trauma care has become an accepted concept.2,51 Trauma centres are designated hospitals which meet certain requirements. Main prerequisites are rapidly available experienced surgeons, anaesthetists and neurosurgeons, and a minimum number of patients seen annually for staff expertise. Regionalisation involves the concept of ambulances bypassing non-designated hospitals.2 Helicopters are used increasingly to speed patient transportation.52 Trauma teams are teams of surgeons and intensivists or anaesthetists who immediately attend the trauma victim on arrival at hospital.2–444
Trauma registries and databases are important tools in organising and improving trauma care. The UK major trauma outcome study38 showed that the doctors in charge of resuscitation were often junior, delays in performing urgent operations were common, and the number of preventable deaths was significant. A hospital may not see enough trauma patients to justify a trauma team or supply adequate experience for its staff, and may not have all the facilities required by trauma patients. Transfer to a trauma hospital may be desirable, but geography and limited transport facilities may make such transfers hazardous.
In Western countries, trauma is a leading cause of death and disability under the age of 38 years.37 Reduction of mortality and morbidity depends on public education, new legislations, on-site advanced care, rapid evacuation (see Chapter 4), hospital trauma expertise and coordination of services.53,54
1 Trunkey DD. Trauma. Sci Am. 1983;249:20-27.
2 Trunkey DD. Overview of trauma. Surg Clin North Am. 1982;62:3-7.
3 Trunkey DD. Initial treatment of patients with extensive trauma. N Engl J Med. 1991;324:1159-1263.
4 Enderson BL, Maull KI. Missed injuries: the trauma surgeon’s nemesis. Surg Clin North Am. 1991;71:399-418.
5 Janjua KJ, Sugrue M, Deane SA. Prospective evaluation of early missed injuries and the role of tertiary trauma survey. J Trauma. 1998;44:1000-1006.
6 Committee on Trauma, American College of Surgeons. Advanced Trauma Life Support (ATLS) Program for Physicians, 7th edn. Chicago: American College of Surgeons, 2004.
7 Soderstrom CA, Cowley RA. A national alcohol and trauma center survey: missed opportunities, failures of responsibility. Arch Surg. 1987;122:1067-1071.
8 Shackford SR, Rogers FB, Osler TM, et al. Focused abdominal sonogram for trauma: the learning curve of nonradiologist clinicians in detecting hemoperitoneum. J Trauma. 1999;46:553-564.
9 Branney SW, Moore EE, Cantrill SV, et al. Ultrasound based key clinical pathway reduces the use of hospital resources for the evaluation of blunt abdominal trauma. J Trauma. 1997;42:1086-1090.
10 Day AC, Rankin N, Charlesworth P. Diagnostic peritoneal lavage: integration with clinical information to improve diagnostic performance. J Trauma. 1992;32:52-57.
11 Weigelt JA, Kingman RG. Complications of negative laparotomy for trauma. Am J Surg. 1988;156:544-547.
12 Trunkey DD, Federle MP. Computed tomography in perspective [editorial]. J Trauma. 1986;26:660-661.
13 Padbani HR, Watson CJE, Clements L, et al. Computed tomography in abdominal trauma: an audit of usage and image quality. Br J Radiol. 1992;65:397-402.
14 Finfer S, Bellomo R, Boyce N, et al. A comparison of albumin and saline for fluid resuscitation in the intensive care unit. N Engl J Med. 2004;350:2247-2256.
15 Bickell WH, Wall MJ, Pepe PE, et al. Immediate versus delayed fluid resuscitation for hypotensive patients with penetrating torso injuries. N Engl J Med. 1994;331:1105-1109.
16 Chestnut RM, Marshall LF, Klauber MR, et al. The role of secondary brain injury in determining outcome from severe head injury. J Trauma. 1993;34:216-292.
17 Wilden JN. Rapid resuscitation in severe head injury. Lancet. 1993;342:1378.
18 Brain Trauma Foundation. Guidelines for the Management of Severe Traumatic Brain Injury. Brain Trauma Foundation, New York, 2007. http://www.braintrauma.org/.
19 Cowley RA, Trump BF. Editors’ summary: Organ dysfunction in shock. In: Cowley RA, Trump BF, editors. Pathophysiology of Shock, Anoxia, and Ischaemia. Baltimore, MD: Williams & Wilkins; 1982:281-284.
20 Faist E, Baue AE, Dittmer H, et al. Multiple organ failure in polytrauma patients. J Trauma. 1983;23:775-787.
21 Daffner RH, Sciulli RL, Rodriguez A, et al. Imaging for evaluation of suspected cervical spine trauma: a 2-year analysis. Injury. 2006;37:652-658.
22 Paul A, Blostein PA, Hodgman CG. Computed tomography of the chest in blunt thoracic trauma: results of a prospective study. J Trauma. 1997;43:13-18.
23 Nzewi O, Slight RD, Zamvar V. Management of blunt thoracic aortic injury. Eur J Vasc Endovasc Surg. 2006;31:18-27.
24 Panetta T, Sclafani SJA, Goldstein AS, et al. Percutaneous transcatheter embolisation for massive bleeding from pelvic fractures. J Trauma. 1985;26:1021-1029.
25 Boyd M, Vanek VW, Bourguet CC. Emergency room resuscitative thoracotomy: when is it indicated? J Trauma. 1992;33:714-721.
26 Suarez JI, Qureshi AI, Bhardwaj A, et al. Treatment of refractory intracranial hypertension with 23.4% saline. Crit Care Med. 1998;26:1118-1122.
27 Prough DS, Zornow MH. Mannitol: an old friend on the skids? Crit Care Med. 1998;26:997-998.
28 Fishman RA. Effects of isotonic intravenous solutions on normal and increased intracranial pressure. Arch Neural Psychiatry. 1953;70:350-360.
29 Teasdale G, Jennett B. Assessment of coma and impaired consciousness: a practical scale. Lancet. 1974;2:81-84.
30 Jennett B, Teasdale G. Aspects of coma after severe head injury. Lancet. 1977;1:878-881.
31 Thomason M, Messick J, Rutledge R, et al. Head CT scanning versus urgent exploration in the hypotensive blunt trauma patient. J Trauma. 1993;34:40-45.
32 American Medical Association Committee on Medical Aspects of Automotive Safety. Rating the severity of tissue damage: I – the abbreviated scale. JAMA. 1971;215:277-280.
33 Committee on Injury Scaling. The Abbreviated Injury Scale – 1980 Revision. Morton Grove, IL: American Association for Automotive Medicine, 1980.
34 Committee on Injury Scaling. The Abbreviated Injury Scale – 2005 Revision. Des Plaines, IL: American Association for Automotive Medicine, 2005.
35 Baker SP, O’Neill B, Haddon W, et al. The injury severity score: a method for describing patients with multiple injuries and evaluating emergency care. J Trauma. 1974;14:187-196.
36 Baker SP, O’Neill B. The injury severity score: an update. J Trauma. 1976;16:882-885.
37 Champion HR, Copes WS, Sacco WJ, et al. The major trauma outcome study: establishing national norms for trauma care. J Trauma. 1990;30:1356-1365.
38 Yates DW, Woodford M, Hollis S. Preliminary analysis of the care of injured patients in 33 British hospitals: first report of the United Kingdom major trauma outcome study. BMJ. 1992;305:737-740.
39 Champion HR, Sacco WJ, Copes WS, et al. A revision of the trauma score. J Trauma. 1989;29:623-629.
40 Boyd CR, Tolson MA, Copes WS. Evaluating trauma care: the TRISS method. J Trauma. 1987;27:370-378.
41 McAnena OJ, Moore FA, Moore EE, et al. Invalidation of the APACHE II scoring system for patients with acute trauma. J Trauma. 1992;33:504-507.
42 Roumen RMH, Redl H, Schlag G, et al. Scoring systems and blood lactate concentrations in relation to the development of adult respiratory distress syndrome and multiple organ failure in severely traumatized patients. J Trauma. 1993;35:349-355.
43 Sacco WJ, Copes WS, Bain LW, et al. Effect of pre-injury illness on trauma patient survival outcome. J Trauma. 1993;35:538-543.
44 Cowley RA, Dunham CM, editors. Shock Trauma/Critical Care Manual. Baltimore, MD: University Park Press, 1982.
45 Baker CC, Oppenheimer L, Stephens B, et al. Epidemiology of trauma deaths. Am J Surg. 1980;140:144-150.
46 Smeeton WMI, Judson JA, Synek BJ, et al. Deaths from trauma in Auckland: a one year study. N Z Med J. 1987;100:337-340.
47 Sauaia A, Moore FA, Moore EE, et al. Epidemiology of trauma deaths: a reassessment. J Trauma. 1995;38:185-193.
48 Streat SJ, Donaldson ML, Judson JA. Trauma in Auckland: an overview. N Z Med J. 1987;100:441-444.
49 Cameron P, Dziukas L, Hadj A, et al. Major trauma in Australia: a regional analysis. J Trauma. 1995;39:545-552.
50 Data updated from that published inGardiner JP, Judson JA, Smith GS, et al. A decade of ICU trauma admissions in Auckland, New Zealand. N Z Med J. 2000;113:326-327.
51 Eggold R. Trauma care regionalisation: a necessity. J Trauma. 1983;23:260-262.
52 Freeark RJ. The trauma center: its hospitals, head injuries, helicopters, and heroes (1982 AAST presidential address). J Trauma. 1983;23:173-178.
53 Judson JA. Trauma management: modern concepts [editorial]. N Z Med J. 1985;98:8-9.
54 Trunkey DD. On the nature of things that go bang in the night. Surgery. 1982;92:123.