CHAPTER 320 Sacral Fractures
Sacral fractures occur in conjunction with pelvic fractures in patients with multiple injuries. Despite being relatively common, sacral fractures are frequently undiagnosed and are treated inadequately.1 The number of sacral and pelvic fractures receiving treatment has increased, owing to improvements in the early evaluation and care of polytraumatized patients. However, as many as 49% of sacral fractures are not diagnosed during these patients’ initial hospitalization. The most commonly missed sacral injury is a transverse fracture at S2. Neurological deficits resulting from sacral injuries can also be overlooked in patients with multiple traumatic injuries. Because sacral fractures can be missed on routine radiographs of the spine and pelvis, the examiner’s index of suspicion for such fractures is paramount in making a prompt and accurate diagnosis. As reported by Malgaigne,2 Richerand first recognized the injury in 1847 in a 53-year-old man who had fallen from a second-story window. In 1945, Bonnin3 proposed the first classification system for fractures of the sacrum. In 1955, Macciocchi4 reported a series of 52 cases. Numerous single case reports and small series have been published, and several reviews, including classification schemes, have appeared in the literature.5,6 This chapter reviews the relevant anatomy, pathophysiology, and classification of sacral fractures and provides an overview of the clinical presentation, diagnosis, and recommended treatment.
Pathophysiology and Classification of Sacral Fractures
In discussions of stability, the sacrum and pelvis are considered one unit. The pelvic ring is a relatively rigid structure whose disruption requires discontinuity in at least two places. Discontinuity can occur as either a fracture or a ligamentous disruption. Gunterberg and coworkers7 performed biomechanical studies of cadaveric specimens loaded to failure to evaluate pelvic stability after major amputation of the sacrum. Specimens resected below S2, sparing the sacroiliac joints, were stable. Specimens resected between S1 and S2 had one third of the sacroiliac joint resected, and stability was reduced 30%. Specimens resected 1 cm below the sacral promontory had half of the sacroiliac joint removed, and the load-to-failure strength was reduced 50%. Overall, the load to failure far exceeded the anticipated physiologic loads.
Bonnin’s original classification divided sacral fractures into six categories3: (1) juxtailiac marginal fractures; (2) fractures involving the S1 or S2 foramen with upward displacement of the lateral mass; (3) fractures through the sacral foramina, which separate the lateral mass from the body of the sacrum; (4) comminuted fractures of the upper sacrum; (5) avulsion fractures of the attachment of the sacrotuberous ligament; and (6) transverse fractures of the sacrum. Bonnin’s classification delineates common fracture types but does not correlate the fracture with the mechanism of injury or aid in clinical evaluation and prognosis. A number of classification systems for sacral fractures have been proposed since Bonnin’s time. The goals of these classification schemes have been to correlate the observed fracture with the mechanism of injury and the clinical findings and to aid in treatment planning. In 1984, Schmidek and coworkers6 proposed a classification based on the mechanism of injury and the resulting fracture pattern. They divided sacral fractures into those caused by direct trauma to the sacrum and those resulting from forces applied indirectly to the sacrum. Direct forces include penetrating injuries that result in open fractures, often accompanied by extensive pelvic visceral injuries. Penetrating injuries are usually stable if the sacrum and the sacroiliac joints above the S1 foramina are intact. Direct closed fractures are often caused by a hard fall onto the buttocks, causing low transverse-type fractures near the kyphos of the sacrum. Although such fractures usually occur through the foramina of S4, any of the lower three vertebrae can be involved. The distal fragment is often displaced anteriorly and may perforate the rectum in more severe cases. Because this part of the sacrum is not involved in the transmission of weight, these fractures are typically stable.
Transverse fractures accounted for 5% to 10% of all sacral fractures in the series by Schmidek and colleagues.6 Indirect trauma to the sacrum follows injuries to the pelvic ring or lumbar spine. The mechanism, usually a flexion injury from a position of hip flexion with knee extension, causes traumatic spondylolisthesis through the S1 or S2 foramina, with forward displacement of the upper spinal segment. Typically, this type of injury occurs in younger patients before intersegmental ossification is complete. One fourth of transverse sacral fractures resulting from falls also have an associated thoracolumbar burst fracture. Thus, lower extremity motor weakness must prompt the examiner to look for associated spinal injuries. Lumbosacral fracture-dislocations are caused by mechanisms similar to those underlying high transverse sacral fractures, and they usually involve fracture of the S1 facet, with resultant instability.
Most fractures produced by indirect forces are vertical fractures of the sacrum, which almost always occur in conjunction with pelvic fractures. Schmidek and coworkers6 classified these fractures into four fracture patterns: (1) lateral mass fractures (extending from the sacral notch through the ventral foramina), (2) juxtaarticular fractures (lateral sacral mass fractures with fragments dissociated from the body of the sacrum), (3) cleaving fractures (vertically oriented fractures from the sacral notch through the sacrococcygeal region), and (4) avulsion fractures (along the convex margin of the sacrum at the attachments of the sacrotuberous and sacrospinous ligaments). Combination fractures, with features of more than one pattern, may also occur. Although this scheme categorizes the different types of sacral fractures, it is cumbersome to remember and apply. In 1988, Denis and colleagues1 published a series of 236 sacral fractures and proposed a simplified classification scheme that categorizes sacral fractures based on the sacrum’s division into three anatomic zones: zone I (alar region), zone II (foraminal region), and zone III (region of the central sacral canal). A zone II fracture can involve zone I but cannot extend into zone III, whereas a zone III fracture can involve zones I and II. In addition to being simple, this classification is relevant to the biomechanical forces applied to the sacrum and the probability of neural injury, and it aids in choosing among treatment options.
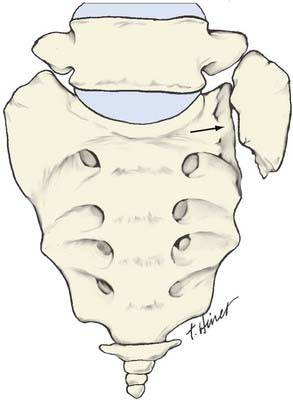
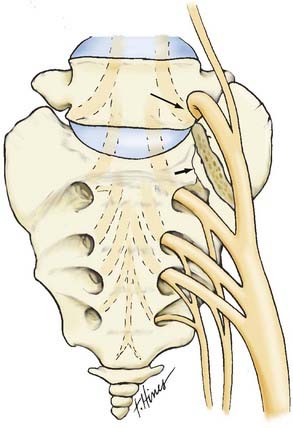
Zone I fractures pass through the ala without damaging the foramina or central canal (Fig. 320-1). They are usually caused by lateral compression of the pelvis during pedestrian accidents in which the posterior sacroiliac ligaments remain intact and a portion of the ala is compressed anteriorly. Zone I fractures are stable by virtue of the intact posterior ligaments. Vertical shear injuries of the pelvis can produce more severe zone I fractures, with superior displacement of the ala and compression of the L5 nerve root between the fracture fragment and the L5 transverse process (Fig. 320-2). Wiltse and colleagues named this mechanism of L5 root injury the traumatic far-out syndrome.8 Zone I fractures also include avulsion fractures at the bulbous enlargement of the sacrum adjacent to the S4 foramen, which is the point of attachment of the sacrospinous and sacrotuberous ligaments. A substantial degree of pelvic disruption occurs with avulsion fractures; therefore, the pelvis is often unstable.
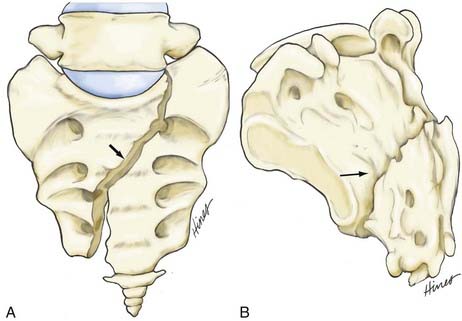
Zone II fractures involve one or several sacral foramina, but not the sacral canal (Fig. 320-3). They are often vertical shear fractures sustained by passengers involved in high-speed motor vehicle crashes, but they may also occur after lateral pelvic compression injuries such as those occurring in zone I fractures. Vertical shear injuries often involve zone II but may also involve zone III. Usually, they are part of an anterior-posterior vertical fracture (double vertical fracture) of the pelvis. These fractures result from a significant transmission of force through one leg or on one side of the pelvis. Vertical shear injuries are uniformly unstable, and the degree of disruption of the sacroiliac joint correlates with both the degree of pelvic instability and the likelihood of neurological deficit.6 Neurological injuries occur in 28% to 54% of zone II fractures.
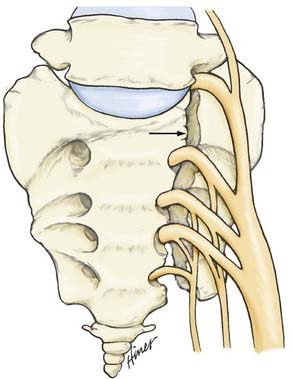
FIGURE 320-3 Zone II fractures (Denis classification) through the sacral foramina may involve one or several foramina.
Zone III fractures involve the sacral canal medial to the foramina and may involve zones I and II (Fig. 320-4). This group includes vertical shear injuries, high and low transverse fractures, and traumatic lumbosacral fracture-dislocations (or traumatic spondylolisthesis of L5 on S1). The transverse sacral fracture, also called the suicidal jumper’s fracture,9 commonly follows a fall from a height. This fracture typically crosses S2-3, just below the level of the sacroiliac joints, with anteroinferior displacement of the upper sacral segment.
These transverse fractures account for 5% to 10% of sacral fractures and are frequently accompanied by neurological injury.6 Fractures in zone III are associated with a high incidence of bilateral nerve root damage and cauda equina dysfunction. Certain features correlate with a high risk for instability: sacroiliac joint disruption, sacrospinous and sacrotuberous avulsion fractures, high transverse and bilateral sacral fractures, and vertical shear fractures. In contrast, lumbosacral fracture-dislocations are highly unstable during flexion.
Clinical Presentation
The Denis three-zone classification system can be useful in anticipating neurological deficits associated with sacral fractures. Zone I fractures are rarely associated with neurological injuries. In the series by Denis and coworkers, 5.9% of patients with zone I fractures presented with neurological deficits.1 Of these patients, 86% had L5 root lesions due to proximal displacement of the ala. Some patients with zone I injuries were impotent from pelvic or pudendal nerve injuries associated with bladder or urethral tears. In patients with zone II fractures, nerve root injuries can be expected if displacement is present. Denis and coworkers found that 28% of fractures of this type were associated with neurological deficits.1 Neurological deficits in zone II fractures correlate strongly with ipsilateral disruption of the sacroiliac joint.6 In displaced zone I and II fractures, the traumatic far-out syndrome, with L5 nerve root injury caused by cephalad displacement of the lateral mass of the sacrum and L5 nerve root compression against the L5 transverse process, may be a cause of radicular deficits. Fifty-seven percent of patients with zone III fractures had associated neurological deficits; of these patients, 76% had bowel or bladder impairment or both.1
Diagnostic Imaging
The sacrum is poorly visualized on standard anteroposterior radiographs of the pelvis because of the orientation of the sacrum at the lumbosacral junction. In one series,10 49% of sacral fractures were not diagnosed during the initial hospitalization, including 24% of patients with neurological deficits referable to these fractures. Only 30% had appropriate radiographic studies that confirmed the fracture and explained the neurological deficit.1 Therefore, unless a high degree of clinical suspicion is entertained, many sacral fractures will be missed on initial trauma radiographs. Certain findings on anteroposterior pelvic radiographs should arouse suspicion: (1) fracture of a lower lumbar transverse process, (2) significant anterior pelvic ring fracture without an identifiable posterior pelvic lesion, (3) asymmetry of the sacral notch, (4) clouding of the radiating trabecular pattern in the lateral sacral mass, or (5) irregularity of the arcuate lines of the upper three sacral foramina.
For patients with clinical signs of sacral injury or suspicious findings of anteroposterior pelvic films, or both, an appropriate imaging protocol includes a true anteroposterior sacral radiograph, performed with the x-ray beam directed 30 degrees cephalad (Ferguson’s view), and a lateral sacral radiograph that includes the entire coccyx. Thin-cut computed tomography (CT) scanning of the sacrum with reformatting is the most useful modality for evaluating complex sacral fractures and patients with neurological injuries.10 Sagittal CT reconstructions are especially helpful for diagnosing transversely oriented fractures and for evaluating the sacroiliac joint.
Bonnin J. Sacral fractures and injuries to the cauda equina. J Bone Joint Surg. 1945;27:113-127.
Denis F, Davis S, Comfort T. Sacral fractures: an important problem. Retrospective analysis of 236 cases. Clin Orthop. 1988;227:6741.
Fishman EK, Magid D, Brooker AE, Siegelman SS. Fractures of the sacrum and sacroiliac joint: evaluation by computerized tomography with multiplanar reconstruction. South Med J. 1988;81:171-177.
Gunterberg B, Rornanus B, Stener B. Pelvic strength after major amputation of the sacrum: an experimental study. Acta Orthop Scand. 1976;47:635-642.
Macciocchi B. Le fatture isolate del sacro. G Med Milit. 10, 1955. 787–784,791
Malgaigne JF. Treatise on Fracture. Philadelphia: JB Lippincott; 1959.
Roy-Camille R, Saillant G, Gagna G, Mazel C. Transverse fracture of the upper sacrum: suicidal jumper’s fracture. Spine. 1985;10:838-845.
Sabiston CP, Wing PC. Sacral fractures: classification and neurologic implications. J Trauma. 1986;26:1113-1115.
Schmidek HH, Smith DA, Kristiansen TK. Sacral fractures. Neurosurgery. 1984;15:735-746.
Wiltse LL, Guyer RD, Spencer CW, et al. Alar transverse process impingement of the L5 spinal nerve: the far-out syndrome. Spine. 1984;14(9):31-41.
1 Denis F, Davis S, Comfort T. Sacral fractures: an important problem. Retrospective analysis of 236 cases. Clin Orthop. 1988;227:6741.
2 Malgaigne JF. Treatise on Fracture. Philadelphia: JB Lippincott; 1959.
3 Bonnin J. Sacral fractures and injuries to the cauda equina. J Bone Joint Surg. 1945;27:113-127.
4 Macciocchi B. Le fatture isolate del sacro. G Med Milit. 10, 1955. 787–784, 791
5 Sabiston CP, Wing PC. Sacral fractures: Classification and neurologic implications. J Trauma. 1986;26:1113-1115.
6 Schmidek HH, Smith DA, Kristiansen TK. Sacral fractures. Neurosurgery. 1984;15:735-746.
7 Gunterberg B, Rornanus B, Stener B. Pelvic strength after major amputation of the sacrum: an experimental study. Acta Orthop Scand. 1976;47:635-642.
8 Wiltse LL, Guyer RD, Spencer CW, et al. Alar transverse process impingement of the L5 spinal nerve: the far-out syndrome. Spine. 1984;149:31-41.
9 Roy-Camille R, Saillant G, Gagna G, Mazel C. Transverse fracture of the upper sacrum: suicidal jumper’s fracture. Spine. 1985;10:838-845.
10 Fishman EK, Magid D, Brooker AE, Siegelman SS. Fractures of the sacrum and sacroiliac joint: evaluation by computerized tomography with multiplanar reconstruction. South Med J. 1988;81:171-177.