63
Rickettsial Diseases
Rickettsial infections often have cutaneous manifestations that can vary from nonspecific maculopapular eruptions to an eschar at the site of inoculation (by the vector) to petechiae and retiform purpura (Table 63.1). These gram-negative bacteria reside within an arthropod – tick, flea, mite, or louse – during a portion of their life cycle and are transmitted to humans while feeding, either via saliva or via feces (Table 63.2). As a result, rickettsial diseases exhibit both seasonality and geographic diversity.
Table 63.1
Dermatologic manifestations of rickettsial infections.
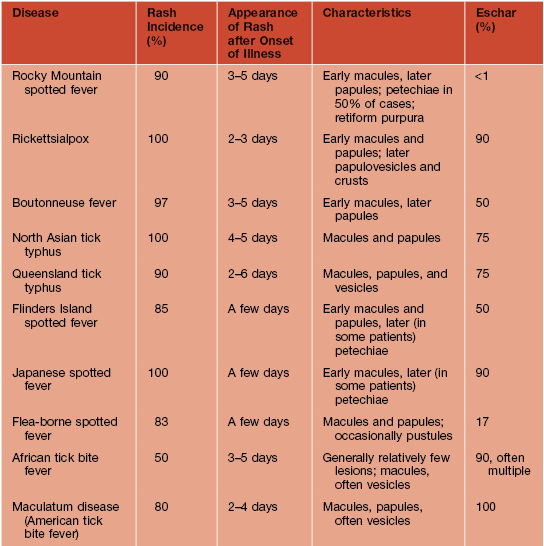
NA, not applicable.
Courtesy, David H. Walker, MD.
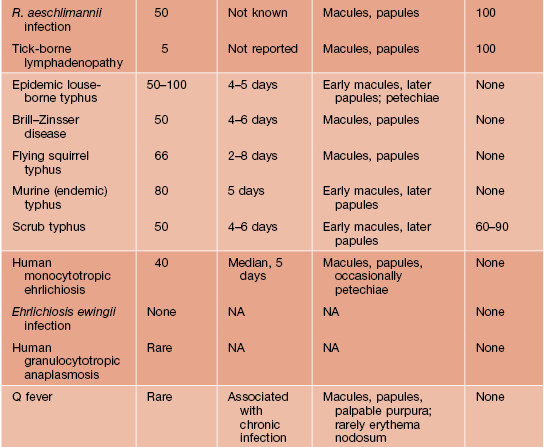
Table 63.2
Epidemiology of rickettsial infections.
A new Ehrlichia species transmitted by Ixodes scapularis, provisionally called E. muris-like, was recently found to cause a febrile illness in the upper midwestern United States.
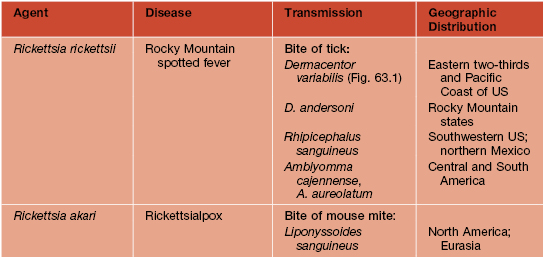
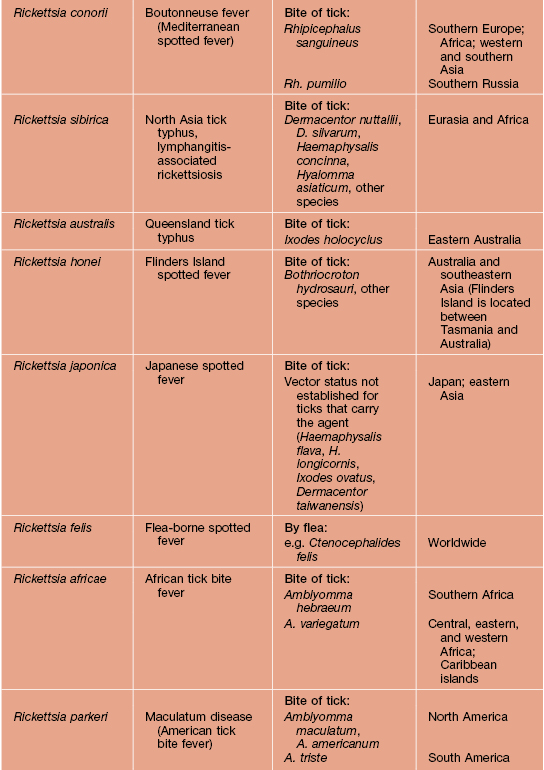
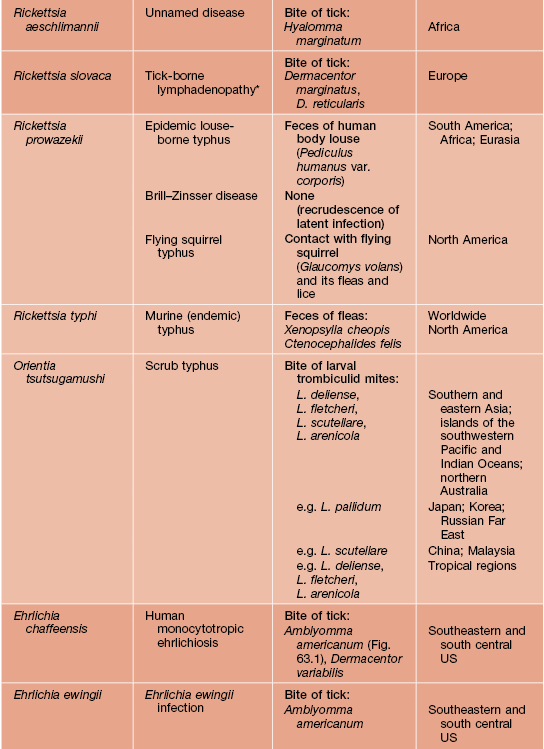
* Also reported to be caused by Rickettsia raoultii.
** Less common means of transmission include ingestion of contaminated dairy products and tick bites (e.g. Dermacentor spp.).
Courtesy, David H. Walker, MD.
Rickettsia and Orientia spp. target endothelial cells of multiple organs, including the skin, whereas Ehrlichia, Anaplasma, and Coxiella spp. target monocytes or neutrophils, neutrophils, and macrophages, respectively.
Rocky Mountain Spotted Fever (RMSF)
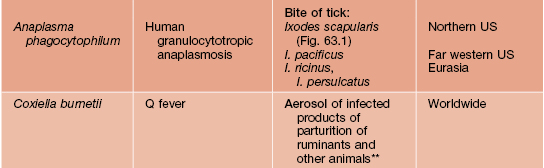
• Due to transmission of Rickettsia rickettsia by the bite of a tick, most commonly Dermacentor spp. (Fig. 63.1); the incubation period is 2–14 days (mean, 7 days) following the bite.
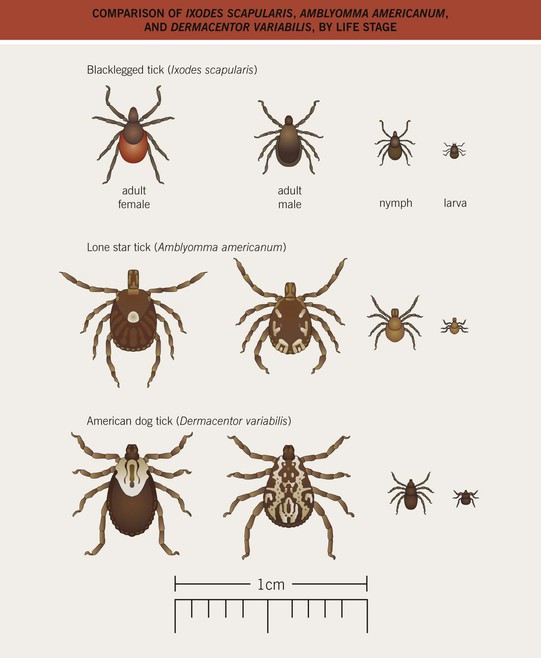
Fig. 63.1 Comparison of Ixodes scapularis (blacklegged tick), Amblyomma americanum (lone star tick), and Dermacentor variabilis (American dog tick), by life stage. From Chapman, A. S., et al. MMWR Recomm. Rep. 2006;55:1–27.
• Highest incidence in the South Atlantic and South Central states (Fig. 63.2), not the Rocky Mountain states, with peak incidence from late spring to the end of summer (tick season).
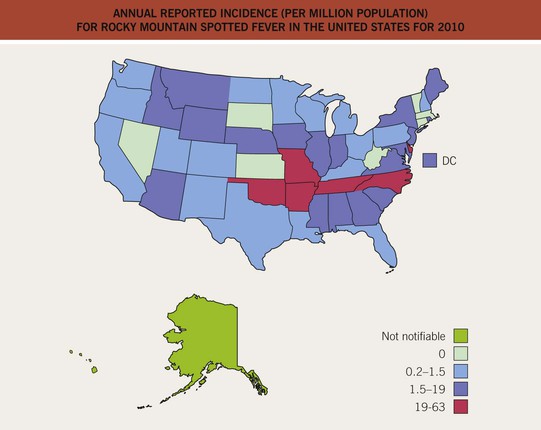
Fig. 63.2 Annual reported incidence (per million population) for Rocky Mountain spotted fever in the United States for 2010. Five states account for >60% of cases. From www.cdc.gov/rmsf/stats/#reportsurv.
• Begins as a subtle cutaneous eruption with pink to erythematous macules then papules, initially in acral sites (e.g. wrists, ankles); over time central petechiae develop and lesions become more widespread (Figs. 63.3–63.6).

Fig. 63.3 Rocky Mountain spotted fever. The cutaneous lesions often first appear on the ankles and wrists. These are nonblanching due to hemorrhage within the skin. Courtesy, Philippe Berbis, MD.

Fig. 63.4 Rocky Mountain spotted fever. Petechiae on the palms and soles often develop relatively later in the disease course. Courtesy, Ronald Rapini, MD.

Fig. 63.5 Rocky Mountain spotted fever. Petechiae are present within erythematous papules and plaques on the buttocks. Some of the lesions have a retiform pattern.

Fig. 63.6 Rocky Mountain spotted fever. Retiform purpura on the distal lower extremity in a patient with more severe disease.
• Dx: biopsy of petechial papule or eschar followed by PCR and/or immunohistochemistry (Table 63.3); serologic results are not helpful in the acute setting.
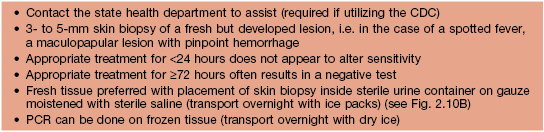
Table 63.3
Evaluation of suspected cutaneous lesion(s) of a spotted fever, including Rocky Mountain spotted fever (RMSF), via real-time PCR.
As recommended by the Centers for Disease Control and Prevention (CDC). www.cdc.gov/rmsf/resources/SkinBiopsyInformation.docx.
• DDx: viral exanthem (e.g. enterovirus, EBV, measles, parvovirus B19, dengue virus; see Fig. 68.1), other rickettsial spotted fevers (similar eruption but more likely to have an inoculation eschar; see Table 63.1), typhus (several forms), ehrlichiosis, morbilliform drug reaction; when severe and purpuric, meningococcemia, vasculitis, hemorrhagic fevers.
• Rx: begun empirically; doxycycline or tetracycline represents first-line therapy, even in children (Table 63.4).
Table 63.4
Treatment of rickettsial diseases.
Empiric treatment with an appropriate agent should be initiated immediately when a diagnosis of Rocky Mountain spotted fever (RMSF), human monocytotropic ehrlichiosis (HME), human granulocytotropic anaplasmosis (HGA), or another potentially severe rickettsiosis is suspected clinically.
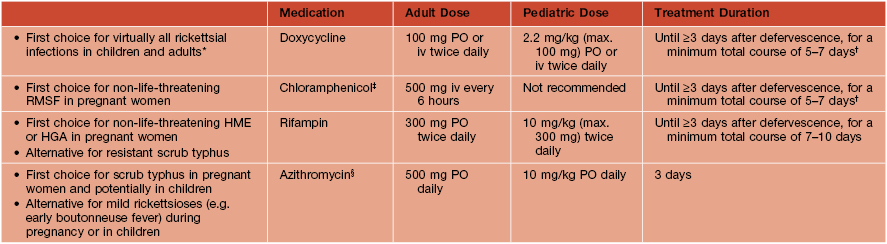
* With the exception of infections in pregnant women, although doxycycline administration during pregnancy can be considered in life-threatening situations when the suspicion of RMSF or other severe rickettsioses is high; other tetracyclines are also effective for rickettsial infections.
† Recommended by the CDC; others recommend a 10-day course.
‡ May be associated with gray baby syndrome when administered late in the third trimester of pregnancy.
§ Clarithromycin may also be considered.
Typhus – Epidemic and Endemic (Murine)
Rickettsialpox
• Most often occurs in urban areas.
• Within 48 hours, a papulovesicle (then eschar) develops at the site of the bite of the mouse mite (Fig. 63.7A); fever, myalgias, and headache appear 1–2 weeks later followed soon thereafter by a cutaneous eruption.


Fig. 63.7 Rickettsialpox. A Eschar at the site of the mite bite. B Scattered papules with central hemorrhagic crusts.
• The eruption has a widespread distribution that includes the face, but the number of lesions is usually limited, i.e. ~20–40; the individual macules and papules develop central vesicles and hemorrhagic crusts (Fig. 63.7B).
Ehrlichiosis
• The primary vector for ehrlichiosis is the lone star tick Amblyomma americanum (Figs. 63.1 and 63.8), with the white-tailed deer serving as a major reservoir.
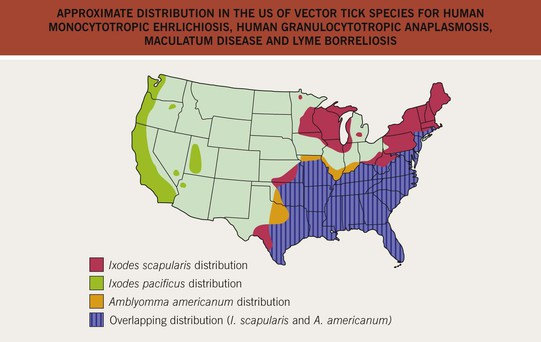
Fig. 63.8 Approximate distribution in the United States of vector tick species for human monocytotropic ehrlichiosis, human granulocytotropic anaplasmosis, maculatum disease, and Lyme borreliosis. It has been postulated that Amblyomma maculatum, which is classically found primarily along the Atlantic and Gulf coasts, has a range as broad as that of Amblyomma americanum. From Chapman, A. S., et al. MMWR Recomm. Rep. 2006;55:1–27.
• Mucocutaneous lesions appear an average of 5 days into the illness of HME and vary from a widespread morbilliform eruption to petechiae favoring the palms and soles to vesicular; occasionally palpable purpura due to small vessel vasculitis can occur.
• DDx: see sections on RMSF and rickettsialpox (if vesicular).
Anaplasmosis (Human Granulocytotropic Anaplasmosis)
• Cutaneous manifestations are rare (<5% of patients), but patients may have concurrent signs and symptoms of Lyme borreliosis and/or babesiosis because all three infections are transmitted by Ixodes ticks, e.g. I. scapularis in the northeastern United States (see Fig. 63.8).
• The illness is usually not as severe as HME and patients may have peripheral neuropathy.
For further information see Ch. 76. From Dermatology, Third Edition.







