CHAPTER 66 Revision of Failed Total Elbow Arthroplasty with Osseous Deficiency
INTRODUCTION
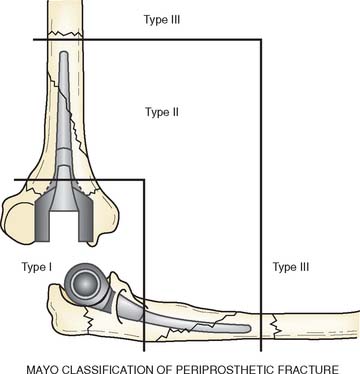
There are several expressions of osseous deficiency. These include (1) deficient length, resulting from absent distal humerus or proximal ulna; (2) compromised bone quality secondary to osteolysis characterized by ballooning of an intact cortex; and (3) periprosthetic fracture. We have classified the periprosthetic fracture as proximal (I) (metaphyseal), with stem involvement (II), or past the stem (III) (Fig. 66-1). From a revision standpoint, the type II fracture involving the stem or a type III fracture proximal or distal to the tip of the stem are of greatest significance. Because the rationale and technique of revision have been covered in detail in Chapter 65, herein we describe three techniques that are used for reimplanation revision following failed total elbow arthroplasty in the face of osseous deficiency. These techniques include impaction grafting, allograft strut grafting, and allograft prosthetic composite. Obviously, impaction grafting and strut grafting can be used in conjunction with these other techniques as well. Implant selection is an important issue. Some have employed unlinked devices in some cases of revision with osseous compromise.4 Others have employed custom designs for such problems.5 We believe that these problems require a linked implant with multiple sizing options.
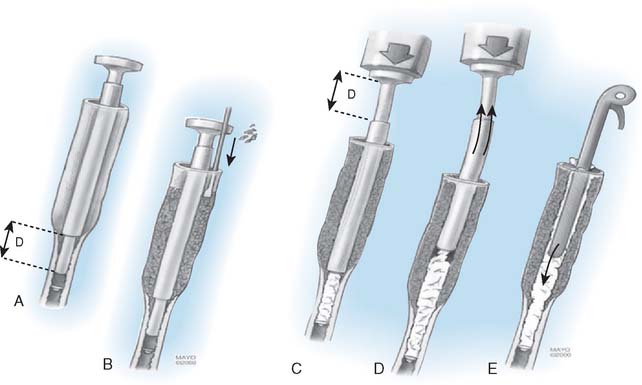
IMPACTION GRAFTING
SURGICAL TECHNIQUE
Bone preparation follows the same basic steps:
Note: The radial nerve is vulnerable in those with osteolysis extending to the spiral groove and may be injured when removing the membrane.14
RESULTS
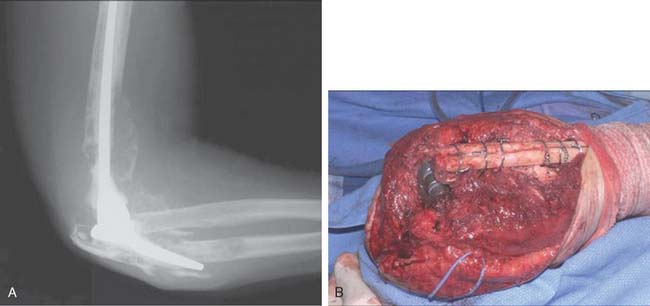
The value of impaction grafting was described originally for acetabular deficiencies by Schreurs et al.13 A 20-year experience with impaction grafting and cemented acetabular component revealed excellent long-term results as well as biopsy evidence of viability and incorporation of the impacted graft. This provides a rationale and a basis for the application at the elbow. We have recently reviewed our experience with 12 patients undergoing revision elbow arthroplasty using an impaction grafting technique between the years 1993 and 1997.9 The average surveillance period was 6 years, with a minimum 2-year follow-up. Recognizing that this represents a salvage-type revision, at the time of last follow-up, eight were intact after the index procedure (Fig. 66-3). In addition, two other patients underwent revision because of loosening and a third required revision due to a subsequent failure of the unrevised ulnar component. One patient developed an infection. Of the eight remaining patients, marked radiographic improvement was observed. At the final follow-up after the additional revision in three patients, five were excellent and four were good with three fair results. This suggests that impaction grafting is a viable option as a salvage for the difficult revision with poor bone quality due to osteolysis.
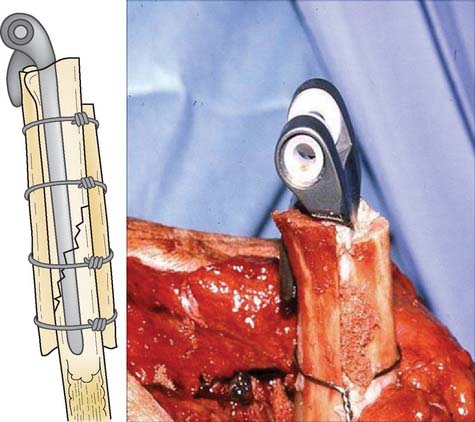
BONE STRUTS
We have adopted the excellent experience of strut reconstruction about the hip, as popularized by Gross,6 for application at the elbow. The results have been gratifying.
TECHNICAL NOTES
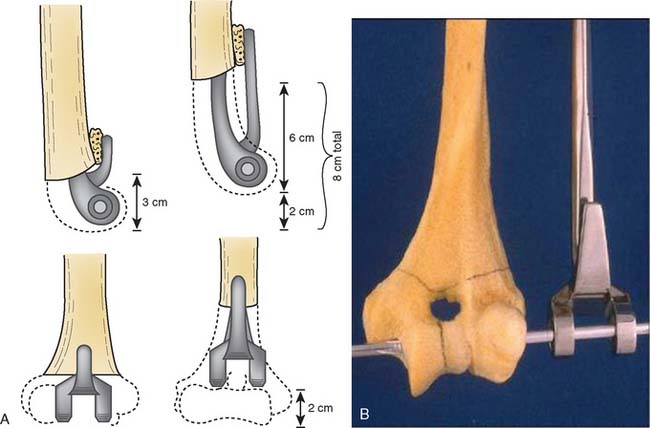
Pearl.
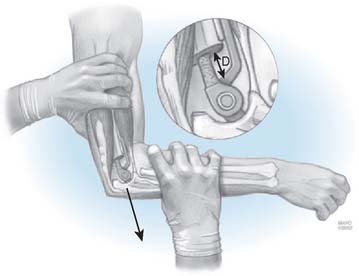
The depth of insertion of the humerus is determined by the “Shuck” test. The trial implant is inserted and with the elbow at 90 degrees the ulna is separated as much as allowed by the soft tissue. This position determines the correct depth of insertion (Fig. 66-6).
RESULTS
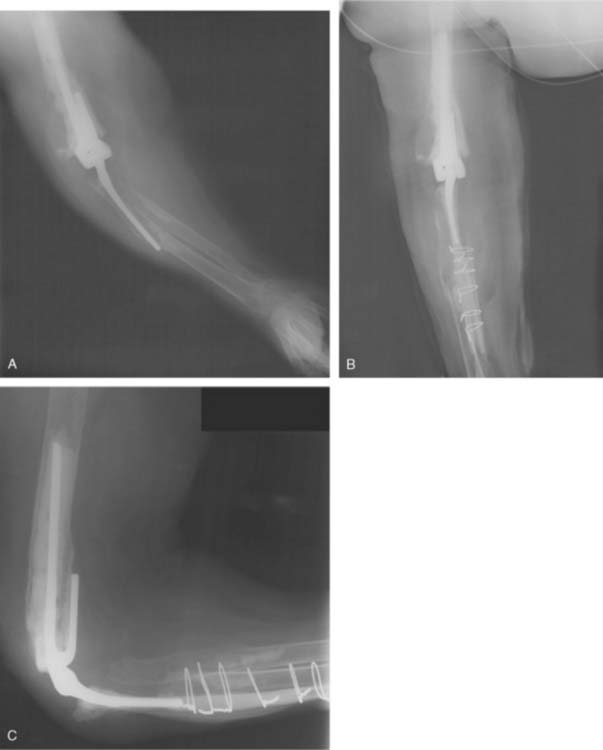
Some employ bone grafting techniques to reconstruct the distal condylar portion of the humerus, if this bone is required by the implant design.7 Experience using strut grafts at the elbow is relatively limited. The Mayo experience with these strut grafts for periprosthetic fractures of the humerus was reported by Sanchez-Sotelo in 2002.12 Between 1991 and 1999 at the Mayo Clinic, 11 periprosthetic fractures with a loose humeral component were managed by two parallel strut grafts, as described earlier (see Fig. 66-4).
The average follow-up was 3 years but ranged from 0.75 years to 8 years. At the time of final assessment, there were no implant failures. Seven of eight patients with an intact reconstruction had a functional arc and no sign of pain (Fig. 66-7). One patient did have limited motion and moderate pain. The complications included one additional undisplaced humeral periprosthetic fracture that failed to heal with closed treatment, one olecranon fracture, one ulnar nerve palsy, and one case of triceps insufficiency. It was concluded that the use of a strut graft can be an effective means of reconstructing the patients with a type II or III periprosthetic fracture.
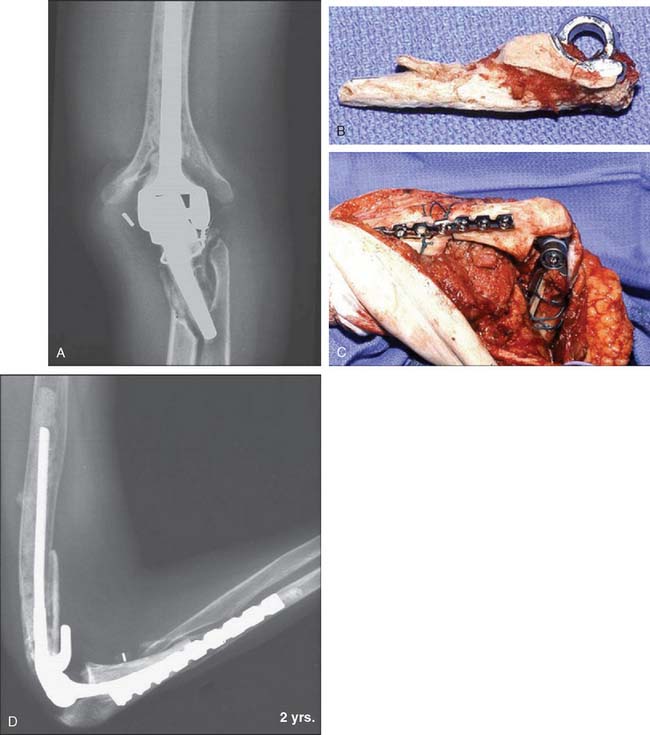
At the ulna, Kamineni et al8 documented the outcome of 22 patients so treated (Fig. 66-8). For the most part, these series represented a salvage procedure because they had an average of two and one-half prior procedures involving the elbow joint. Among 22 patients, the Mayo Elbow Performance score improved from 34 to 79 points. Overall some incorporation of the strut graft occurred in 91%, which reflects the approximate 90% satisfactory rate with the procedure.
ALLOGRAFT PROSTHTETIC COMPOSITE
The use of structure allografts is limited at the elbow since the outcomes are considered unreliable.1–3 On the other hand, the allograft prosthetic composite is a well-recognized technique for massive reconstruction of hip and knee deficiencies often associated with tumor resections.10 At the elbow, the technique of allograft prosthetic composite has changed dramatically. Initially we performed procedures similar to those described for the hip and knee, with a step-cut type of interface between the allograft and the host bone. This experience was reported by Mansat et al11 and is considered our early-phase experience.
INITIAL MAYO EXPERIENCE
Thirteen patients were reviewed who underwent allograft prosthetic composite.11 With an average of 42 months’ follow-up, the Mayo Elbow Performance score was excellent for four, good for three, fair for one, and poor for five (Fig. 66-9). Nine of the 13 patients had minimal pain. The mean arc of flexion was 97 degrees. There were seven complications affecting seven elbows. Five of the seven, however, required revision procedures. Deep infection was the most serious complication, occurring in four elbows. There were two nonunions occurring at the allograft-humeral junction.
CURRENT MAYO TECHNIQUE
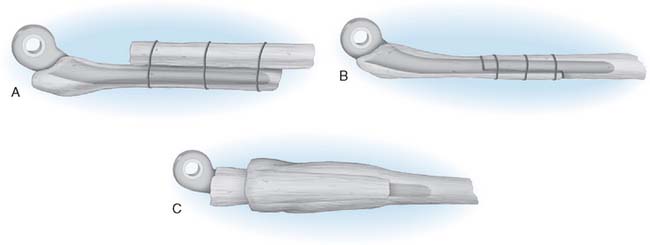
The difficulty and the time consumption of precise step-cuts prompted the concept of a “side-to-side” application. With this logic, the entire circumferential allograft is applied to the host bone and secured with cerclage wires. This approach has been used effectively in those individuals with marked bone loss and in whom the above-mentioned techniques would not be adequate (Fig. 66-10). Several variations have been developed (Fig. 66-11). One modification of this technique has been developed by employing the circumferential allograft to stabilize the implant, but the distal or proximal extension is modified as a continuation of a strut type graft (Fig. 66-12). There is some concern as to the strength of the interface between the allograft and the host bone but there is a high likelihood of healing of the strut graft. A third and final version of fixation is to telescope the circumferential allograft into the expanded host bone (Fig. 66-13).

FIGURE 66-12 A and B, Patient with loss of distal humerus and proximal ulna. The problem was resolved with strut grafting on the humerus (C and D). A type II allograft prosthetic composite was employed in which the extended ulnar component traverses the circumferential allograft and then enters the host bone. The allograft continues distally as a strut (see Fig. 66-11B).
SUMMARY
The three methods described earlier do provide a reasonably reliable set of options for difficult salvage situations. However, it should be emphasized that these do not represent routine revisions but salvage-type procedures, and their high complication rates and potential for failure must be appreciated.
1 Breen T., Gelberman R.H., Leffert R., Botte M. Massive allograft. Surgery. 1988;13A:900.
2 Dean G.S., Holliger E.H., Urbaniak J.R. Elbow allograft for reconstruction of the elbow with massive bone loss. Long term results. Clin. Orthop. Relat. Res. 1997;341:12.
3 Dee R. Reconstructive surgery following total elbow endoprosthesis. Clin. Orthop. Relat. Res. 1982;170:196.
4 Ehrendorfer S. Elbow revision arthroplasty in the situation of bone loss using an unlinked long-stem prosthesis. J. Hand Surg. 1999;24A:1337.
5 Figgie H.E., Inglis A.E., Mow C. Total elbow arthroplasty in the face of significant bone stock or soft tissue losses: preliminary results of custom-fit arthroplasty. J. Arthroplasty. 1986;1:71.
6 Gross A.E., Wong P.K., Hutchison C.R., King A.E. Onlay cortical strut grafting in revision arthroplasty of the hip. J. Arthroplasty. 2003;18(3 suppl 1):104.
7 Gschwend N. Salvage procedure in failed elbow prosthesis. Arch. Orthop. Trauma Surg. 1983;101:95.
8 Kamineni S., Morrey B.F. Proximal ulnar reconstruction with strut allograft in revision total elbow arthroplasty. J. Bone Joint Surg. Am. 2004;86A:1223.
9 Loebenberg M.I., Adams R.A., O’Driscoll S.W., Morrey B.F. Impaction grafting in revision total elbow arthroplasty. J. Bone Joint Surg. 2005;87A:99.
10 Mankin H.J., Doppelt S., Tomford W. Clinical experience with allograft implantation: the first ten years. Clin. Orthop. Relat. Res. 1983;174:69.
11 Mansat P., Adams R.A., Morrey B.F. Allograft-prosthesis composite for revision of catastrophic failure of total elbow arthroplasty. J. Bone Joint Surg. 2004;86A:724.
12 Sanchez-Sotelo J., O’Driscoll S., Morrey B.F. Periprosthetic humeral fractures after total elbow arthroplasty: Treatment with implant revision and strut allograft augmentation. J. Bone Joint Surg. 2002;84A:1642.
13 Schreurs B.W., Sloof T.J., Gardeniers J.W.M., Buma P. Acetabular reconstruction with bone impaction grafting and a cemented cup: 20 years’ experience. Clin. Orthop. Relat. Res. 2001;393:202.
14 Zook J., Ward W.G.Sr. Intraosseous radial nerve entrapment complicating total elbow revision. J. Arthroplasty. 2001;16:919.