Chapter 23 Restless Legs Syndrome and Pregnancy
Epidemiology
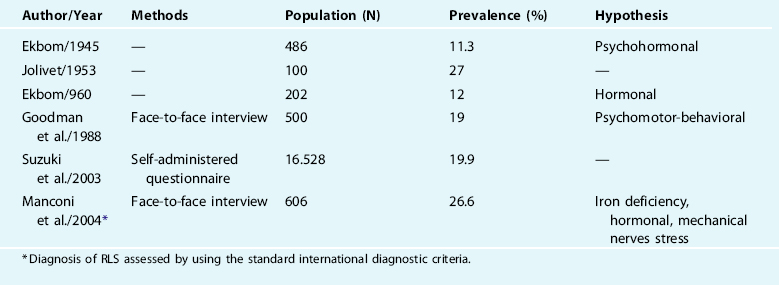
A possible relation between restless legs syndrome (RLS) and pregnancy was noted by Mussio-Fournier and Rawak in 1940.1 They reported the occurrence of a symptoms characterized by “pruritus, urticaria and paresthesias” of the lower limbs, appearing during rest, in three subjects belonging to the same family. The authors focused on one member of the family, who presented with a typical worsening of the symptoms during pregnancy. In 1945, Ekbom2 performed the first structured epidemiologic study on this topic, finding a prevalence of RLS of 11.3% among 486 pregnant women. A few years later, Jolivet,3 in his degree thesis in medicine, reviewed a population of 100 pregnant women and observed 27 cases of RLS. The same topic was further investigated by only a few other epidemiologic studies (Table 23-1), which found an RLS prevalence during pregnancy ranging from 11% to 27%.2–7 The high variability of these rates could be related to several differences in methodology between the studies. Standardized formal criteria8,9 for making the diagnosis of the RLS were used in only one of these studies. The diagnosis was assessed either by self-administered questionnaire or by face-to-face medical interview. The minimal frequency of RLS symptoms required to define “affected” women varied between studies or was not even stated in the methods. The studies have been performed in different geographic areas and on different racial populations. Finally, the time during the pregnancy at which the presence or absence of symptoms was evaluated also varied between studies. Because the prevalence of RLS appears to increase for the duration of the pregnancy,10 this sampling method would clearly bias the prevalence rates that were reported. When the prevalence rate is ascertained by applying the standard diagnostic criteria through a structured medical interview, on a wide and homogeneous population of women, and during the entire course of pregnancy, the frequency is about 26%.7 Another study found that, even excluding those with preexisting RLS, the prevalence of RLS was 26% when examined in late pregnancy.7a This prevalence rate is much higher than that reported for the general population and includes women who had RLS before the pregnancy, as well as those who developed RLS during pregnancy. The percentage of women with preexisting RLS ranges between 5% and 10%. In most cases, however, these women reported a significant worsening of the symptoms during the pregnancy.7
Course and Prognosis
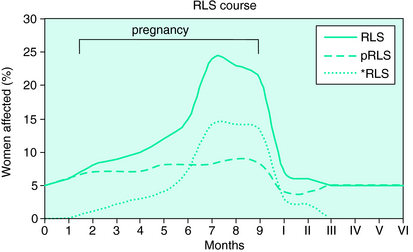
The RLS prevalence is not uniform during pregnancy; it increases progressively starting from the third and four months of gestation and reaches a peak during the third trimester, especially in the eighth month, in which the highest rate is observed. After that it rapidly declines during the ninth month, to disappear around the time of delivery. During the puerperium, the prevalence is about that found during the prepregnancy period5,7 (Fig. 23-1). In women not previously affected by RLS, the mean duration of symptoms during pregnancy usually is 3 to 5 months. Unfortunately, longitudinal data do not yet exist regarding the risk of developing RLS in the future for those who had symptoms only during pregnancy.
Multiparous women often reported having RLS symptoms during the previous pregnancies.5,7 The quality of RLS symptoms, including its anatomic distribution, circadian nature, and relief with motor activity, are not different during pregnancy than those reported by those with idiopathic RLS.7 Familiar RLS history is a common finding, especially for women affected by a preexisting form of RLS.
Sleep Impact
The consequences of the symptoms on the pregnant women sleep are usually not dramatic. Some women with RLS report higher sleep latency, excessive daytime sleepiness, lower total sleep time, and, more frequently insomnia, compared with unaffected pregnant subjects.7 In a few cases the symptoms became very disagreeable, making it impossible for those so affected to relax in the evening or to fall asleep.11 Pregnancy itself, particularly during the third trimester, is frequently associated with sleep loss often secondary to many factors (nocturia, fetal movements, gastroesophageal reflux, snoring, sleep apnea, forced body position, and anxiety about the delivery).12 Therefore, it is difficult to parcel out the real impact of the RLS symptoms alone on sleep during pregnancy. The polysomnographic pattern of pregnant women with RLS has never been systematically studied; however, periodic legs movements during pregnancy have been described.13
Therapy
Many women who develop RLS symptoms during their pregnancy are often more concerned about the fetus and its well-being than about their personal discomfort. Because these women often do not receive an adequate explanation of the symptoms, the first approach should be to reassure the woman that the development and health of the fetus are not at risk and that the symptoms are likely to disappear at the end of the pregnancy.7 Women with RLS should be evaluated for possible iron or folate deficiency and, if present, then appropriately treated. Renal and neurologic dysfunctions or other possible causes of RLS should be excluded. Several behavioral approaches that may help include the avoidance of smoking, caffeine, prolonged erect posture, and excessive daytime motor activity. If symptoms become severe and disrupt sleep or trigger depression, then drug therapy could be useful.
McParland and Pearce11 reported on two women with severe cases of RLS in pregnancy who were successfully treated with carbamazepine, after no improvement was seen with benzodiazepines (temazepam and diazepam) and phenobarbitone. Low evening doses (0.5 mg) of clonazepam, used on an as-needed basis, has been reported to improve symptoms.23 Dopaminergic drugs, which are considered the first choice of treatment for RLS under nonpregnant conditions, could theoretically interfere with the process of lactogenesis, because of their inhibition of prolactin secretion. Unfortunately, there are no controlled studies on the treatment of pregnancy-related RLS.23,24 Most of the drugs used to treat RLS are (with very few exceptions) classified as Pregnancy Category C as defined by the U.S. Food and Drug Administration and may therefore be of some risk to the fetus (see RLSF pamphlet25 or patient book26 for categorization of medications). If treatment is unavoidable, then it should be used only during the third trimester and at the lowest efficacious dosage.
Etiopathogenetic Hypotheses
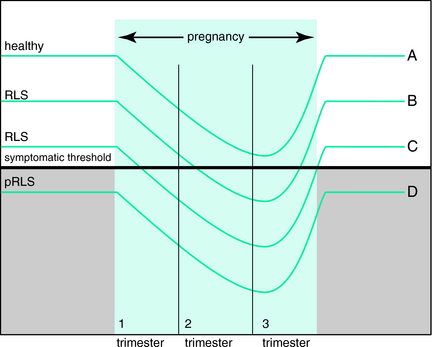
The close temporal overlapping between the symptoms and the third trimester of pregnancy suggests that, during this period, one or more pregnancy-related factors could facilitate the RLS appearance or worsening. How and which pregnancy-related factors could induce the RLS is until now unclear. These disowned factors could be present only in women who develop the RLS during pregnancy (∼25%) but absent in the rest of the women, or they could involve all women, being correlated in general to the pregnant condition itself, but they induce RLS only in the women predisposed to the syndrome. The first hypothesis is less sustainable, because if this possible pathogenetic process involved only approximately one quarter of the women, we would expect that it involved similarly about one quarter of the women already affected by RLS before the pregnancy, causing in them a worsening of the symptoms. In truth, the great majority of preexisting RLS, experience a significant increase of symptom severity during late pregnancy. As outlined in Figure 23-2, a more plausible pathogenetic model is one in which one or more unknown factors, associated with the pregnant condition, reduce the RLS symptomatic threshold during late pregnancy in all women, but provoke RLS only in subjects with preexisting risk factors that determine a low individual symptomatic threshold. In other words, the presence and the duration of the RLS would depend mainly on the individual predisposition. A woman without risk factors, either genetic or environmental (e.g., iron stores) will move closer to the symptomatic threshold during pregnancy, but never reach it and so will not experience the RLS during the pregnancy. A woman with no RLS history, but having sufficient risk factors, will cross the symptomatic line and become affected during pregnancy and, on the basis of her degree of predisposition, she will experience the symptoms only during late pregnancy or for a longer time. The majority of women previously affected by RLS, suffering the same pregnancy influence, will experience a worsening of the symptoms during the pregnancy period.
The nature of these hypothetical risk factors has not been yet identified. New genetic discoveries may begin to provide an understanding of genetic risk factors.27–29 The only environmental risk factors supported by some evidences are represented by iron or folate deficiencies.7,7a,14 During late pregnancy, iron and folic acid levels normally decrease because of the hemodilution and of the increased fetal needs. Compared with non-RLS subjects, women who develop the symptoms during pregnancy seem to have lower, but in normal range, iron and folate values just before the pregnancy onset, and to have lower iron and iron storage indicators at the end of the pregnancy.7,15 This theory is at variance with two findings: women who receive folate and iron oral supplementation during pregnancy develop RLS at the same rate as women without a supplemented diet. In other words, iron or folate supplementation seems to not prevent RLS. Secondly, the RLS symptoms disappear before the delivery, although the main blood and iron loss is due to delivery, and it needs some months to be restored.5,7 Although the impact of iron and folate deficiencies on pregnancy related RLS is probable, it needs to be further evaluated before it can be accepted without reservations.
Other recognized risk factors for RLS in pregnancy are age, the higher the mother’s weight, previous experiences of RLS in pregnancy, and familiar history for RLS.7
The trend of RLS prevalence, and of the symptom severity throughout the pregnancy, is quite similar to that of the main sexual hormones. In fact, estrogens, prolactin, and progesterone increase significantly in the third trimester of pregnancy and drop after delivery, except for the prolactin that continues to assume a pulsatile secretion. This likeness suggested a possible hormonal influence in RLS appearance.7a Because dopamine strongly inhibits the hypothalamic secretion of prolactin releasing factor, increased prolactin during pregnancy could be associated with reduced dopamine levels, which might lower the RLS symptomatic threshold.7,16 On the other hand, it has been demonstrated that estrogens exert an antidopaminergic effect on the basal ganglia and concomitantly increase motor activity in animals.17–21 As a further complication, the excitability of several nervous centers may be raised by progesterone.22
1. Mussio-Fournier JD, Rawak F. Familiäres auftreten von pruritus, urtikaria und parästhetischer hyperkinese der unteren extremitäten. Confin Neurol. 1940;3:110-114.
2. Ekbom KA. Restless legs syndrome. Acta Med Scand. 1945;158(suppl):4-12.
3. Jolivet B. Paresthésies agitantes nocturnes des membres inférieurs, impatiences. Thése de Paris, 1953.
4. Ekbom K. Akroparestesier och restless legs under graviditet. Lakartidningen. 1960;57:2597-2603.
5. Goodman JDS, Brodie C, Ayida GA. Restless leg syndrome in pregnancy. BMJ. 1988;297:1101-1102.
6. Suzuki K, Ohida T, Sone T, et al. The prevalence of restless legs syndrome among pregnant women in Japan and relationship between restless legs syndrome and sleep problems. Sleep. 2003;26:673-677.
7. Manconi M, Govini V, De Vito A, et al. Restless legs syndrome and pregnancy. Neurology. 2004;63:1065-1069.
7a. Manconi M, Govoni V, De Vito A, et al. Pregnancy as a risk factor for restless legs syndrome. Sleep Med. 2004;5:305-308.
8. Tunc T, Karadag YS, Dogulu F, et al. Predisposing factors of restless legs syndrome in pregnancy. Mov Disord. 2007;22:627-631.
9. Walters AS. Toward a better definition of the restless legs syndrome. The International Restless Legs Syndrome Study Group. Mov Disord. 1995;10:634-642.
10. Allen RP, Picchietti D, Hening WA, et al. Restless legs syndrome: Diagnostic criteria, special considerations, and epidemiology. A report from the Restless Legs Syndrome Diagnosis and Epidemiology Workshop at the National Institutes of Health. Sleep Med. 2002:4101-4119.
11. Manconi M, Ferini-Strambi L. Restless legs syndrome among pregnant women. Sleep. 2004;27:350.
12. McPharland P, Pearce JM. Restless legs syndrome in pregnancy. Case reports. Clin Exp. Obstet Gynecol. 1990;17:5-6.
13. Santiago JR, Nolledo MS, Kinzler W, et al. Sleep and sleep disorders in pregnancy. Ann Intern Med. 2001;134:396-408.
14. Nikkola E, Ekblad U, Ekholm E, et al. Sleep in multiple pregnancy: Breathing patterns, oxygenation, and periodic leg movements. Am J Obstet Gynecol. 1996;174:1622-1625.
15. Boetz MI, Lambert B. Folate deficiency and restless legs syndrome in pregnancy. N Engl J Med. 1977;297:670.
16. Lee KA, Zaffke ME, Baratte-Beebe K. Restless legs syndrome and sleep disturbance during pregnancy: The role of folate and iron. J Women’s Health Gen Med. 2001;10:335-341.
17. Wetter TC, Collado-Seidel V, Oertel H, et al. Endocrine rhythms in patients with restless legs syndrome. J Neurol. 2002;249:146-151.
18. Euvrard C, Oberlander C, Boissier JR. Antidopaminergic effect of estrogens at the striatal level. J Pharmacol Exp Ther. 1980;214:179-185.
19. Ogawa S, Chan J, Gustafsson JA, et al. Estrogen increases locomotor activity in mice through estrogen receptor alpha: Specificity for the type of activity. Endocrinology. 2003;144:230-239.
20. Morgan MA, Pfaff DW. Estrogen’s effects on activity, anxiety and fear in two mouse strains. Behav Brain Res. 2002;132:85-93.
21. Becker JB, Beer ME. The influence of estrogen on nigrostriatal dopamine activity: Behavioral and neurochemical evidence for both pre- and postsynaptic components. Behav Brain Res. 1986;19:27-33.
22. Bedard PJ, Malouin F, Dipaolo T, et al. TRH and striatal dopaminergic mechanisms. Prog Neuropsychopharmacol Biol Psychiatry. 1982;6:555-561.
23. Roberts JM. Pregnancy related hypertension. In: Creasy RK, Resnik R, et al, editors. Maternal-Fetal Medicine: Principle and Practice. 2. Philadelphia, WB: Saunders; 1989:783-808.
24. Manconi M, Govoni V, De Vito A, et al. Pregnancy as a risk factor for restless legs syndrome. Sleep Med. 2004;5:305-308.
25. Briggs GG, Freeman RK, Yaffe SJ. Drugs in Pregnancy and Lactation, 5. Baltimore: Williams and Wilkins, 1998.
26. RLS Foundation. Pregnancy and RLS. Available at: www.rls.org.
27. Buchfuhrer MJ, Hening WA, Kushida CA. The Restless Legs Syndrome. New York: Demos, 2006.
28. Winkelmann J, Schormair B, Lichtner P, et al. Genome-wide association study of restless legs syndrome identifies common variants in three genomic regions. Nat Genet. 2007. Epub Jul 18
29. Stefansson H, Rye DB, Hicks A, et al. A genetic risk factor for periodic limb movements in sleep. N Engl J Med. 2007. Epub Jul 18