Chapter 6 Clinical Science of Restless Legs Syndrome
The masterful description of restless legs syndrome (RLS) in a monograph written over half a century ago by Ekbom,1 even giving clues as to the pathophysiology, remains a classic in RLS literature. Perusal of the literature reveals that the great English physician Thomas Willis,2 in the late 17th century, gave a tantalizing account of what appears to be the first description of RLS. What Willis described as “wherefore to some, when being a Bed, they betake themselves to sleep presently in the Arms and Legs, Leapings, and Contractions of the Tendons, and so great a Restlessness and Tossings of their Members ensue, that the diseased are no more able to sleep, than if they were in a place of the greatest Torture” seems to accurately reflect the description of an RLS patient as mentioned in the contemporary literature. The scientific community waited nearly two centuries before Wittmaack3 described RLS-like symptoms under the heading of “anxietias tibiarum.” Later, Beard4 in 1918 and Oppenheim5 in 1923 used the term neurasthenia for what appeared to be RLS-like symptoms. The description of leg movements caused by paresthesia during rest by Mussio-Fournier and Rawak6 in 1940 and of “leg jitters” by Allison7 in 1943 heralded the introduction of the term irritable legs by Ekbom in 1944,8 and finally restless legs in 1945.1 Ekbom put RLS on firm footing as an organic neurological disorder and dispelled the myth of the past that RLS is of psychogenic origin. It took another 50 years to refine the diagnostic criteria9 for RLS with a later revision10 (four essential criteria and supportive and associated features), which were clearly enumerated by Ekbom in his classic clinical description. Clinicians and researchers are still groping for clues to understanding the pathophysiology, including the site(s) of origin of the sensorimotor components of RLS.11,12 An important reason for this intellectual failure is that there is no single diagnostic test for RLS. Clinical trials, epidemiological surveys, and studies to uncover the pathophysiology of RLS are hampered by the lack of a clear diagnostic test for the condition, although attempts have been made to find one by performing an overnight polysomnographic study (PSG), suggested immobilization test (SIT), and actigraphy. Clinicians and researchers have to depend on a purely clinical description, which can be extremely difficult, if not impossible in some cases, particularly in those with an atypical or uncommon presentation. There are certain conditions that may closely mimic RLS and certain conditions associated with RLS (symptomatic or comorbid), which must be recognized by clinical clues and in some cases by appropriate laboratory tests (see Chapter 18). The second reason is that RLS is almost certainly not a single disease. The heterogeneity of RLS is exemplified by phenotypical variation, linkage to different chromosomal localization, varying prevalence findings in European and North American compared with Asian epidemiological studies, differing electrophysiological and neuroimaging findings, and varying therapeutic responses to different classes of medications (e.g., dopaminergic drugs, anticonvulsants, opioids, and benzodiazepines), including iron treatment.
Phenotypical Variation
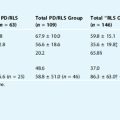
There are indications for two phenotypes for RLS:13 early onset (EO) (before the age of 45 years) and late onset (LO) (after the age of 45 years). But exceptions clearly occur, and for some genetic epidemiological investigations, earlier cutoffs may be meaningful. EO-RLS is more consistently associated with a possible family history, more slowly progressive course, and longer duration of the disease than LO-RLS. The latter progresses relatively rapidly, and generally patients seek medical advice within 5 years of onset of symptoms. LO-RLS is frequently secondary or symptomatic, whereas EO-RLS is primary or idiopathic. The other difference between these two phenotypes is that cerebrospinal fluid (CSF) ferritin levels are lower in EO-RLS than in LO-RLS.14 Another finding differentiating the two types is greater deficiency in brain iron in EO-RLS than in LO-RLS.15
Genetic Heterogeneity
An increased incidence of RLS (as high as 70%) has been noted in the first-degree relatives of idiopathic or primary cases.16,17 A high concordance in monozygotic twins18 and complex segregation analysis19,20 suggest an autosomal dominant mode of inheritance. Linkage and association analyses have now documented significant RLS-associated variations in seven different chromosomes (see Chapter 8). Recently, four predispositive allelic variations in different genes have been found. One is the neuronal nitric oxide gene located near the 12q area that was first implicated in RLS.21,22 The other identified genes (on chromosomes 2p. 6p, and 15q) are related to development and suggest that the basis for RLS may lie in the original elaboration of the nervous system.23,24
Dilemma With the Iron Deficiency Theory of Restless Legs Syndrome
The current hot topic of scientific research in RLS is the iron–dopamine connection,11,25 with clear evidence for the role of iron, and indirectly, for the role of dopamine in idiopathic RLS (see Chapter 11), at least in one major subgroup. Nordlander26 first demonstrated improvement of symptoms with intravenous iron treatment. O’Keefe and associates27 first reported low iron levels as measured by serum levels of ferritin, the primary storage protein for iron. The question of iron deficiency is important as such a deficiency may reduce the effective activity of the dopamine system. Various ways in which iron might influence dopamine have been suggested. Iron is needed as a cofactor for tyrosine hydroxylase, the rate-limited enzyme for dopamine synthesis, and therefore iron deficiency may impair the normal production of dopamine. Dopamine D2 receptor is an iron-containing protein, and hence the hypofunction of D2 receptor may be caused by iron deficiency. Both iron and dopamine show a circadian rhythm, with the lowest levels occurring at night when RLS symptoms are worse and exacerbated. The question of iron deficiency is particularly relevant in elderly patients who have low iron stores as measured by serum ferritin. RLS symptoms are often relieved by both iron and dopamine, whereas dopamine antagonists worsen RLS symptoms. Certain conditions (e.g., iron deficiency anemia, pregnancy, and end-stage renal disease) predisposing to RLS often have low iron stores. Further support for the role of iron in RLS includes the inverse correlation of body iron stores to the severity of RLS, improvement of RLS symptoms after both oral and intravenous iron treatment,28,29 and CSF14,30 and special neuroimaging findings31 showing decreased brain iron in RLS patients. Transcranial Doppler study32 showing hypoechogenicity in the substantia nigra (SN) also suggests reduced iron in the SN in RLS patients. The pharmacological facts complement imaging studies showing striatal dopamine abnormalities (see later). Finally, limited postmortem findings in seven cases of RLS showing no morphological abnormalities in the basal ganglia but a problem with iron acquisition and storage in the SN firmly established the role of brain iron deficiency in RLS symptomatology.33 There are, however, some inexplicable contradictions in two different autopsy findings from the same group. The initial finding of increased transferrin receptor concentration in the SN could not be corroborated in the second quantitative autopsy study.34 The second study found decreased activity of iron regulatory protein 1 (IRP1) controlling synthesis of transferrin receptors. Brain iron storage problems are not always reflected in the blood iron and ferritin levels; herein lies the dilemma. Not all iron-deficient states are associated with RLS and not all RLS patients show iron deficiency, either by laboratory techniques or by therapeutic response. There is a single report of a randomized double-blind placebo-controlled trial of oral iron supplementation failing to show any significant difference in RLS symptoms with treatment.35 Should we, therefore, label the group of RLS with decreased iron or ferritin primary or comorbid (symptomatic) RLS or a special phenotypical variant of primary RLS, suggesting RLS heterogeneity? Another unanswered question is the reason for brain iron storage problems. Is it simply an epiphenomenon, a triggering factor, an incidental finding unrelated to RLS symptoms, or secondary to sleep deprivation or fragmentation disturbing iron metabolism?
Controversy Regarding the Dopamine Deficiency Theory of Restless Legs Syndrome
The dopaminergic theory of RLS is popularized predominantly on the basis of the therapeutic response noted in every patient, at least initially, and supplemented by neuroimaging findings that have been inconsistent. There is compelling indirect, but not direct, evidence that there is a dopamine deficiency in RLS. The first clue to the current popular dopaminergic deficiency theory of RLS came from Akpinar’s letter to the editor in 198236 showing improvement of RLS symptoms after levodopa ingestion. This brief report opened therapeutic avenues for alleviating RLS symptoms. Subsequent reports show that even a low dose of dopamine nearly always relieves RLS symptoms; this is the basis of a diagnostic test using L-dopa and looking for a response in reduced symptoms.37 Several open-label and double-blind clinical trials demonstrated the efficacy of dopaminergic treatment in RLS,38,39 whereas dopamine antagonist worsened the RLS symptoms. Exacerbation of RLS symptoms in the evening when dopamine activity in the body is at its lowest level; exacerbation of RLS symptoms with iron deficiency, which may reduce the production of dopamine, and increasing frequency of RLS symptoms with increasing age when dopaminergic neurons show age-related depletion may be cited as indirect evidence in support of dopaminergic theory in the pathophysiology of RLS. CSF studies from the Johns Hopkins University group40 show no significant differences in homovanillic acid (HVA) and 5-hydroxyindoleacetic acid (5-HIAA), which are dopamine metabolites between RLS patients and control subjects, but did show increased CSF tetrahydrobiopterin, whereas Stiasny-Kolster and colleagues41 found no significant differences for HVA, tetrahydrobiopterin (BH4), and several other dopamine-related metabolites between 22 RLS patients (CSF samples obtained in the evening) and 11 control subjects. A comparative study of evening and morning samples showed that the RLS subjects showed an increased circadian difference between day and night in these values, with higher concentrations found in the morning.42
The pharmacological facts complement some neuroimaging studies showing evidence of presynaptic or postsynaptic dopamine deficiency, but other studies have not confirmed these conclusions (see later). Therefore, besides the therapeutic response to dopaminergic medication, the rest of the studies involving the dopamine system, including neuroimaging studies, CSF analysis of dopamine metabolites, and limited autopsy studies do not provide convincing evidence of a primary dopaminergic deficiency syndrome. Certainly, RLS is not Parkinson’s disease (PD), an example of a clear nigrostriatal dopamine deficiency (dopaminergic A9 cell degeneration) syndrome. Does this mean that RLS is due to a defect (functional or structural) in the diencephalospinal dopaminergic (A11 neurons) pathways? It is possible, but at present, this is pure speculation. What is needed is an animal model of RLS, but this is currently lacking. Ondo and associates43 attempted to produce an animal model by injecting 6-hydroxy-dopamine into the A11 dopaminergic neurons in rats. There are two problems with this model: the behavior of the animals lacks phenomenological similarity to human RLS patients, and it is not clear whether the lesion was localized to A11 neurons only, without also involving nigrostriatal (A9) dopaminergic neurons. Another animal model tried to explain dopamine contribution in RLS in a dopamine D3 receptor knockout mouse model.43a Finally, the prevalence of RLS in PD may be higher than in the general population, but this is an area of controversy.44 There are certainly no population-based reports of increased prevalence of PD in RLS patients.
Heterogeneity of Neuroimaging Findings in Restless Legs Syndrome
Based on the assumption of dopamine deficiency in RLS, the neuroimaging studies thus far have focused on the nigrostriatal dopaminergic system (see Chapter 12). Studies including positron emission tomography (PET) and single-photon emission computed tomography (SPECT) investigated postsynaptic or presynaptic dopamine receptor binding. The results have been inconsistent. This contradiction could be due to the heterogeneity of the disease, methodological difference, or timing of the study (asymptomatic periods and different circadian phases). The iodobenzamide-SPECT (IBZM-SPECT) study by Staedt and colleagues45 and Michaud and associates46 as well as the [11C]raclopride PET study by Turjanski and coworkers47 showed a mild reduction in the postsynaptic D2 receptor binding. Turjanski and colleagues suggested that this reduced D2 receptor binding indicated either an increase in endogenous dopamine (increased dopamine release or turnover) or a decrease in central dopaminergic transmission. In contrast, Eisenseher48 and Tribl49 and their colleagues using IBZM-SPECT found normal postsynaptic dopamine D2 receptor function. Eisenseher and colleagues cautioned that age-matched controls are needed in all studies, because there is an inverse correlation between D2 receptor binding and age in PD patients.
Presynaptic dopamine system function can be measured using iodopropen-carbomethoxy-tropane (IPT) or beta-carbomethoxy-iodophenyl- tropane (β-CIT) (IPT-SPECT and β-CIT-SPECT), which are cocaine analogues with high affinity to dopamine transporters in the presynaptic terminals of the dopaminergic neurons. [18F]Fluorodopa PET study also detects striatal presynaptic binding. [18F]Fluorodopa PET studies by Turjanski and colleagues47 and Ruottinen and associates50 revealed a mild reduction of the mean uptake in putamen and caudate of RLS patients compared with control subjects. In contrast, [18F]fluorodopa PET by Trenkwalder and coworkers,51 IPT-SPECT studies by Eisensehr and colleagues,48 and a β-CIT SPECT study by Michaud and colleagues46 found normal presynaptic dopamine function. A more recent study found surprisingly that D2 receptors were increased in RLS, supporting a presynaptic deficit.52
Heterogeneity in the Neurophysiological Findings in Restless Legs Syndrome
Some electrophysiological and functional magnetic resonance imaging (MRI) studies have suggested a possible site of abnormality in the brainstem, but contradictory observations in blink reflex excitability studies speak against this conclusion.53 The inconsistent electrophysiological findings may be related to the following factors: methodological problems, time of the day of the study (most of the studies have been performed during asymptomatic periods), and the different subtypes of RLS with differing loci or generators (e.g., cortical, brainstem, spinal, and peripheral regions or a combination of different locations) for the origin of RLS symptoms, including motor components (e.g., myoclonus in relaxed awake patients, periodic limb movements in wakefulness [PLMW] and in sleep [PLMS]). Several electrophysiological studies have suggested the brainstem or spinal cord as the site of origin for PLMS and RLS. The absence of cortical prepotentials on back-averaging, normal electroencephalogram, and the absence of high-amplitude cortical potentials in somatosensory evoked response argue against these movements being of cortical origin. Some studies of patients with RLS or PLMS, however, have found support for the presence of hyperexcitable brainstem reflexes. Briellmann and colleagues,54 and Wechsler and associates,55 for example, found enhanced excitability of the late component of the blink reflex. In contrast, Bucher and coworkers,56 (also unpublished personal observation) found no abnormalities of the blink reflex in such patients. Transcranial magnetic stimulation studies in RLS patients show altered cortical excitability, but normal motor threshold and conduction velocity suggest that the motor pathways are generally intact and the altered cortical excitability is secondary to subcortical mechanism. Tergau and colleagues,57 studied intracortical inhibition in 18 RLS patients and 17 age-matched control subjects by using paired transcranial magnetic stimulation technique. They found a significant reduction of intracortical inhibition in RLS, suggesting motor cortex disinhibition. Studies by Entezari-Taher and associates58 and Stiasny-Kolster and coworkers59 also suggested impairment of the cortical inhibition by showing significant shortening of the cortical silent period. These findings suggest an altered cortical excitability as a result of subcortical inputs. Transcranial magnetic stimulation findings, therefore, lend support to enhanced blink reflex excitability found by some investigators indicating the site of generator in RLS at the brainstem level. Functional MRI studies also pointed to midbrain and thalamic or cerebellar loci and not the cortex.60 A finding of increased volume of the pulvinar in the voxel-based MRI morphometric analysis of the thalamus also suggests a role for the thalamus61 in the pathogenesis of RLS. The possibility, however, remains that some motor components in RLS, including PLMS, may be of spinal origin. The presence of PLMS in patients with spinal cord lesions, including thoracic transection and transient RLS after spinal anesthesia, provides support for the spinal cord as the site of generator for PLMS in RLS patients. That such generators may exist in the isolated spinal cord for a number of different cyclical motor behaviors has been shown experimentally by Grillner.62 Thus, a suprasegmental spinal cord lesion may disinhibit the lumbosacral spinal cord generator to produce PLMS. Studies of the spinal flexor reflex in both idiopathic63 and comorbid RLS associated with chronic renal failure64 showed a low-threshold, more easily elicitable and widely distributed response than controls. Additionally, RLS patients showed enhancement of flexor reflex components during sleep, indicating state dependence of the reflex response in RLS patients. These findings indicate pronounced excitability of the spinal cord mechanism, possibly facilitated by the loss of supraspinal inhibition. Neurophysiological studies, including nerve conduction velocities and somatosensory evoked response recordings, in RLS patients revealed no abnormalities. Polymyographic studies in RLS in one study65 suggested a possible propriospinal mechanism for the pattern and recruitment of the movements, but this has been contradicted by studies66,67 showing no such pattern. Polymyographic studies showing periodic limb movements in sleep in different limbs occurring asynchronously in different periods, as well as their occurrence in the cranially innervated muscles (unpublished observations), suggest multiple oscillators responsible for involuntary movements in RLS.
Heterogeneity in the Epidemiological Study
RLS may be the most common movement disorder, but it has been much less commonly diagnosed. Frequent misdiagnosis and poor recognition have hampered epidemiological studies in RLS. A case in point is the survey from Europe and the United States showing the correct diagnosis of RLS by general physicians to be less than 7% of those diagnosed (based on validated diagnostic questions) with distressing RLS symptoms occurring at least two times a week.68 The estimated prevalence rates vary widely from 1% to 15%, but contemporary studies from North America and Europe have given an approximate prevalence rate of 5% to 10% (see Chapter 7). In contrast, studies from the East (e.g., Singapore, Japan, and India) generally report low prevalence rates (less than 1% to 5%, with the exception of Korea). This variation in worldwide prevalence of RLS may be related to methodological issues, heterogeneity of RLS, and ethnic, racial, or other environmental factors.
Future Directions in Restless Legs Syndrome Research
Many questions remain unresolved, including the most exciting iron–dopamine deficiency theory in RLS. A better understanding of the iron–dopamine connection may provide a key to designing new treatment for RLS. Future research should, therefore, be directed to developing new treatment options and an understanding of the pathophysiology and molecular neurobiology of RLS. Efforts should be directed toward development of a potential animal model for RLS-PLMS. Such models could include spinal cord transection or brainstem preparations, as well as models created through iron deficiency. Investigations to develop a valid laboratory diagnostic test for RLS will enhance the diagnostic capabilities and therefore be important for clinical trials and epidemiological surveys. Better treatment options should be directed toward development of the drugs with consistent results without “wearing-off” effects (rebound), augmentation, or serious adverse side effects. Future investigations should also explore the recent advances in neuroimaging techniques and should include dopamine transport ligands to test the presynaptic dopamine system, as well as regional imaging techniques to study brain circuitry (cortical and subcortical) to see changes during RLS sensorimotor symptoms. These studies should be performed during symptomatic and asymptomatic periods and should include brain regions outside the striatum. We need population-based epidemiological studies in different ethnic and racial populations in different continents and subcontinents. Further investigations should be directed toward a better understanding of the sleep–wake patterns in RLS patients and particularly the role of sleep deprivation and fragmentation in RLS morbidity and pathophysiology. One important aspect is impaired cognitive performance in RLS and whether this is a primary finding in RLS or a result of sleep deprivation. Other lines of research should include the role of the metabolic syndrome and alterations of immune functions in RLS symptomatology and morbidity. RLS research took a new and exciting direction in the latter part of the last century. Let us hope that research will proceed at a faster speed in the 21st century to find the cause and a cure for this very common but uncommonly diagnosed condition with considerable morbidity. Advances in the clinical neuroscience of RLS are described in detail in the following chapters of this section.
1. Ekbom KA. Restless legs: A clinical study. Acta Med Scand Suppl. 1945;158:1-23.
2. Willis T. The London Practice of Physick. London: Bassett and Crooke, 1685.
3. Wittmaack T. Lehrbuch des Nervenkrankheiten Pathologie and Therapie des sensibilitat: Neurosen. In Leipzig. Germany: E. Schafer; 1861.
4. Beard GM. A Practical Treatise on Nervous Exhaustion, 2. New York: William Wood and Co, 1880.
5. Oppenheim H. Lehrbuch des Nervenkrankheiten, 7. Berlin: S. Karger, 1923.
6. Mussio-Fournier JD, Rawak F. Familiares Auftreten von Pnuritus, Urticaria and Parasthetischer Hyperkinesie des unteren extremitaten. Confin Neurol (Basel). 1940;3:110-114.
7. Allison FG. Obscure pains in the chest, back or limbs. Canad Med Assoc J. 1943;48:36-38.
8. Ekbom KA. Restless legs syndrome. Neurology. 1960;10:868-873.
9. Walters AS. Toward a better definition of the restless legs syndrome. The International Restless Legs Syndrome Study Group. Mov Disord. 1995;10:634-642.
10. Allen RP, Picchietti D, Hening WA, et al. Restless legs syndrome: Diagnostic criteria, special considerations, and epidemiology. A report from the Restless Legs Syndrome Diagnosis and Epidemiology Workshop at the National Institutes of Health. Sleep Med. 2003;4:101-119.
11. Allen RP, Earley CJ. Restless legs syndrome: A review of clinical and pathophysiologic features. J Clin Neurophysiol. 2001;18:128-147.
12. Earley CJ. Clinical practice. Restless legs syndrome. N Engl J Med. 2003;348:2103-2109.
13. Allen RP, Earley CJ. Defining the phenotype of the restless legs syndrome (RLS) using age-of-symptom-onset. Sleep Med. 2000;1:11-19.
14. Earley CJ, Connor JR, Beard JL, et al. Ferritin levels in the cerebrospinal fluid and restless legs syndrome: Effects of different clinical phenotypes. Sleep. 2005;28:1069-1075.
15. Early CJ, Barker PB, Horska A, et al. MRI-determined regional brain iron concentrations in early and late-onset restless legs syndrome. Sleep Med. 2006;7:458-461.
16. Allen RP, La Buda MC, Becker P, et al. Family history study of the restless legs syndrome. Sleep Med. 2002;3(suppl):S3-S7.
17. Walters AS, Hickey K, Maltzman J, et al. A questionnaire study of 138 patients with restless legs syndrome: The ‘Night-Walkers’ survey. Neurology. 1996;46:92-95.
18. Ondo WG, Vuong KD, Wang Q. Restless legs syndrome in monozygotic twins: Clinical correlates. Neurology. 2000;55:1404-1406.
19. Winkelmann J, Muller-Myhsok B, Wittchen HU, et al. Complex segregation analysis of restless legs syndrome provides evidence for an autosomal dominant mode of inheritance in early age at onset families. Ann Neurol. 2002;52:297-302.
20. Mathias RA, Hening W, Washburn M, et al. Segregation analysis of restless legs syndrome: Possible evidence for a major gene in a family study using blinded diagnoses. Hum Hered. 2006;62:157-164.
21. Desautels A, Turecki G, Montplaisir J, et al. Identification of a major susceptibility locus for restless legs syndrome on chromosome 12q. Am J Hum Genet. 2001;69:1266-1270.
22. Winkelmann J, Lichtner P, Schormair B, et al. Variants in the neuronal nitric oxide synthase (nNOS, NOS1) gene are associated with restless legs syndrome (abstract). Mov Disord. 2007:8.
23. Winkelmann J, Schormair B, Lichtner P, et al. Genome-wide association study of restless legs syndrome identifies common variants in three genomic regions. Nat Genet. 2007;39:1000-1006.
24. Stefansson H, Rye DB, Hicks A, et al. A genetic risk factor for periodic limb movements in sleep. N Engl J Med. 2007;357:639-647.
25. Allen R. Dopamine and iron in the pathophysiology of restless legs syndrome (RLS). Sleep Med. 2004;5:385-391.
26. Nordlander NB. Therapy in restless legs. Aeta Med Scand. 1953;145:453-457.
27. O’Keeffe ST, Gavin K, Lavan JN. Iron status and restless legs syndrome in the elderly. Age Ageing. 1994;23:200-203.
28. Earley CJ, Heckler D, Allen RP. The treatment of restless legs syndrome with intravenous iron dextran. Sleep Med. 2004;5:231-235.
29. Earley CJ, Heckler D, Allen RP. Repeated IV doses of iron provides effective supplemental treatment of restless legs syndrome. Sleep Med. 2005;6:301-305.
30. Mizuno S, Mihara T, Miyaoka T, et al. CSF iron, ferritin and transferrin levels in restless legs syndrome. J Sleep Res. 2005;14:43-47.
31. Allen RP, Barker PB, Wehrl F, et al. MRI measurement of brain iron in patients with restless legs syndrome. Neurology. 2001;56:263-265.
32. Schmidauer C, Sojer M, Seppi K, et al. Transcranial ultrasound shows nigral hypoechogenicity in restless legs syndrome. Ann Neurol. 2005.
33. Connor JR, Boyer PJ, Menzies SL, et al. Neuropathological examination suggests impaired brain iron acquisition in restless legs syndrome. Neurology. 2003;61:304-309.
34. Connor JR, Wang XS, Patton SM, et al. Decreased transferrin receptor expression by neuromelanin cells in restless legs syndrome. Neurology. 2004;62:1563-1567.
35. Davis BJ, Rajput A, Rajput ML, et al. A randomized double-blind placebo-controlled trial of iron in restless legs syndrome. Eur Neurol. 2000;43:70-75.
36. Akpinar S. Treatment of restless legs syndrome with levodopa plus benserazide. Arch Neurol. 1982;39:739.
37. Stiasny-Kolster K, Kohnen R, Carsten Moller J, et al. Validation of the “L-DOPA test” for diagnosis of restless legs syndrome. Mov Disord. 2006;21:1333-1339.
38. Littner MR, Kushida C, Anderson WM, et al. Practice parameters for the dopaminergic treatment of restless legs syndrome and periodic limb movement disorder. Sleep. 2004;27:557-559.
39. Chesson AL Jr, Wise M, Davila D, et al. Practice parameters for the treatment of restless legs syndrome and periodic limb movement disorder. An American Academy of Sleep Medicine report. Standards of Practice Committee of the American Academy of Sleep Medicine. Sleep. 1999;22:961-968.
40. Earley CJ, Hyland K, Allen RP. CSF dopamine, serotonin and biopterin metaboites in patients with restless legs syndrome. Mov Disord. 2001;16:144-149.
41. Stiasny-Kolster K, Moller JC, Zschocke J, et al. Normal dopaminergic and serotonergic metabolites in cerebrospinal fluid and blood of restless legs syndrome patients. Mov Disord. 2004;19:192-196.
42. Earley CJ, Hyland K, Allen RP. Circadian changes in CSF dopaminergic measures in restless legs syndrome. Sleep Med. 2006;7:263-268.
43. Ondo WG, He Y, Rajasekaran S, Lee WD. Clinical correlates of 6-hydroxydopamine injections into A11 dopaminergic neurons in rats: A possible model for restless legs syndrome. Mov Disord. 2000;15:154-158.
43a. Clemens S, Rye D, Hochman S. Restless legs syndrome: revisiting the dopamine hypothesis from the spinal cord perspective. Neurology. 2006;67:125-130.
44. Ondo WG, Vuong KD, Jankovic J. Exploring the relationship between Parkinson disease and restless legs syndrome. Arch Neurol. 2002;59:421-424.
45. Staedt J, Stoppe G, Kogler A, et al. Nocturnal myoclonus syndrome (periodic movements in sleep) related to central dopamine D2-receptor alteration. Eur Arch Psychiatry Clin Neurosci. 1995;245:8-10.
46. Michaud M, Soucy JP, Chabli A, et al. SPECT imaging of striatal pre-and postsynaptic dopaminergic status in restless legs syndrome with periodic leg movements in sleep. J Neurol. 2002;249:164-170.
47. Turjanski N, Lees AJ, Brooks DJ. Striatal dopaminergic function in restless legs syndrome: 18F-dopa and 11C-raclopride PET studies. Neurology. 1999;52:932-937.
48. Eisensehr I, Wetter TC, Linke R, et al. Normal IPT and IBZM SPECT in drug-naïve and levodopa-treated idiopathic restless legs syndrome. Neurology. 2001;57:1304-1309.
49. Tribl GG, Asenbaum S, Happe S, et al. Normal striatal D2 receptor binding in idiopathic restless legs syndrome with periodic leg movements in sleep. Nucl Med Commun. 2004;25:55-60.
50. Ruottinen HM, Partinen M, Hublin C, et al. An FDOPA PET study in patients with periodic limb movement disorder and restless legs syndrome. Neurology. 2000;54:502-504.
51. Trenkwalder C, Walters AS, Hening WA, et al. Positron emission tomographic studies in restless legs syndrome. Mov Disord. 1999;14:141-145.
52. Cervenka S, Palhagen SE, Comley RA, et al. Support for dopaminergic hypoactivity in restless legs syndrome: A PET study on D2-receptor binding. Brain. 2006;129:2017-2028.
53. Chokroverty S, Jankovic J. Restless legs syndrome: A disease in search of identity. Neurology. 1999;52:907-910.
54. Briellmann RS, Rosler KM, Hess CW. Blink reflex excitability is abnormal in patients with periodic leg movements in sleep. Mov Disord. 1996;11:710-714.
55. Wechster LR, Stakes JW, Shahani BT, et al. Periodic leg movements of sleep (nocturnal myoclonus): An electrophysiological study. Ann Neurol. 19, 1986. 168-117
56. Bucher SF, Trenkwalder C, Oertel WH. Reflex studies and MRI in the restless legs syndrome. Acta Neurol Scand. 1996;94:145-150.
57. Tergau F, Wischer S, Paulus W. Motor system excitability in patients with restless legs syndrome. Neurology. 1999;52:1060-1063.
58. Entezari-Taher M, Singleton JR, Jones CR, et al. Changes in excitability of motor cortical circuitry in primary restless legs syndrome. Neurology. 1999;53:1201-1205.
59. Stiasny-Kolster K, Haeske H, Tergau F, et al. Cortical silent period is shortened in restless legs syndrome independently from circadian rhythm. Suppl Clin Neurophysiol. 2003;56:381-389.
60. Bucher SF, Seelos KC, Oertel WH, et al. Cerebral generators involved in the pathogenesis of the restless legs syndrome. Ann Neurol. 1997;41:639-645.
61. Etgen T, Draganski B, Ilg C, et al. Bilateral thalamic gray matter changes in patients with restless legs syndrome. Neuroimage. 2005;24:1242-1247.
62. Grillner S. Ion channels and locomotion. Science. 1997;278:1087-1088.
63. Bara-Jimenez W, Aksu M, Graham B, et al. Periodic limb movements in sleep: state-dependent excitability of the spinal flexor reflex. Neurology. 2000;54:1609-1616.
64. Aksu M, Bara-Jimenez W. State dependent excitability changes of spinal flexor reflex in patients with restless legs syndrome secondary to chronic renal failure. Sleep Med. 2002;1:37-42.
65. Trenkwalder C, Bucher SF, Oertel WH. Electrophysiological pattern involuntary limb movements in the restless legs syndrome. Muscle Nerve. 1996;19:155-162.
66. Provini F, Vertrugno R, Meletti S, et al. Motor pattern of periodic limb movements during sleep. Neurology. 2001;57:300-304.
67. de Weerd AW, Rijsman RM, Brinkley A. Activity patterns of leg muscles in periodic limb movement disorder. J Neurol Neurosurg Psychiatry. 2004;75:317-319.
68. Allen RP, Walter AS, Montplaisir J, et al. Restless legs syndrome prevalence and impact: REST general population study. Arch Intern Med. 2005;165:1286-1292.