Respiratory system
Computed tomography of the thorax
Indications
1. In the assessment of pulmonary masses, chest wall or pleural disease
2. For the staging and follow-up of malignancy in the chest
3. In the assessment (characterisation, quantification and follow-up) of diffuse lung disease
4. Evaluation of known/suspected thoracic vascular assessment (congenital or acquired – pulmonary embolus, aortic dissection, arteriovenous malformation, etc.)
5. In the assessment of airways disease, bronchiectasis and large airway stenosis.
6. Evaluation for thoracic manifestations of known extrathoracic disease
8. Performing CT-guided intervention, e.g. lung, pleura or chest wall mass biopsy, bronchial stent insertion, pleural collection drainage, radiofrequency ablation, etc.
Technique
1. Volume scan – usually performed with intravenous contrast enhancement at a rate of 3–5 ml s–1 with a delay of 25–40 s. However, bolus tracking software can be used to trigger the scan more precisely to coincide with optimal contrast enhancement of specific structures, e.g. mediastinum, aorta in suspected aortic dissection or pulmonary artery in suspected pulmonary embolism. (Delayed imaging at 60 s can be useful in cases of large pleural effusion to assess for underlying soft tissue pleural thickening.)
2. High-resolution scan. Non-contrast scan obtained on full inspiration either:
(a) 1 mm slices at 10 to 20 mm intervals or
(b) Volume acquisition through the lungs with reconstruction of contiguous 1 mm slices:
• Spatial resolution should be maximized using the smallest field of view possible.
• Use a high-resolution (high spatial resolution) ‘bone’ algorithm to reconstruct images.
• A volume acquisition with reconstruction of contiguous slices has the benefit of post-processing capabilities, e.g. multiplanar reformatting can help to illustrate the cranio-caudal distribution of lung changes.
• Additional expiratory images can be performed in suspected air-trapping and airways disease.
• Additional prone images are indicated to differentiate reversible-dependent change from early interstitial fibrosis.
Beigelman-Aubry, C, Hill, C, Brillet, P-Y, Grenier, PA. MDCT of the airways: technique and normal results. Radiol Clin North Am. 2009; 47(2):185–201.
Webb, WR, Muller, NL, Naidich, DP. Technical aspects of high-resolution computed tomography of lung disease. In High-Resolution CT of the Lung, 4th ed, Lippincott Williams and Wilkins; 2008:1–41.
Computed tomography-guided lung biopsy
Indications
1. Investigation of a new or progressing pulmonary opacity when other diagnostic techniques such as bronchoscopy have failed to make a diagnosis.
2. Investigation of a new lung/pleural/chest wall lesion in a patient with known malignancy.
3. To obtain material for culture when other techniques have failed to identify the causative organism in a patient with persistent consolidation.
All biopsies should be planned after case discussion at a multi-disciplinary meeting with a respiratory physician, radiologist, surgeon and oncologist where the balance of benefit versus risk can best be assessed. Central lesions are preferably biopsied transbronchially either by standard bronchoscopy (where there is endobronchial disease) or, if extrabronchial, by transbronchial needle aspiration (TBNA) either ‘blind’ or with endoscopic ultrasound guidance (EBUS).
Contraindications
1. Vascular: bleeding diatheses (including conditions that affect platelet function such as chronic renal failure), patient on anticoagulants, significant pulmonary arterial or venous hypertension.
2. Respiratory: contralateral pneumonectomy (unless the lesion is pleurally based and lung tissue will not be traversed), presence of significant emphysema (particularly bullous disease) or significantly impaired respiratory function such that pneumothorax would not be tolerated. (An FEV1 of <1 l or <35% predicted is often used as lower limit cut-off for biopsy.) Air travel should not be undertaken within 6 weeks following the procedure.
Equipment
• Fine needle aspiration can be performed if there is an on-site cytopathology service. Usually use 20 or 22G needles. Different needles vary by the profile of the needle tip and include Chiba (with a bevelled tip which allows straightforward cytological sample aspiration) and those with modified tips which allow ‘cutting’ to obtain small histological fragments as well as aspiration (suitable for more fibrous lesions), e.g. Franseen® (Cook Medical™) and Westcott® (Becton-Dickinson Medical™).
• Cutting needle biopsy needles are larger gauge (usually 18 or 20G) and obtain a solid core of tissue for histological examination. They usually have adjustable throw of the specimen notch for precise sampling of the lesion. Types include Temno® and Quick-Core® (Cook Medical™). Coaxial needle biopsy systems can be used as these stabilize the cutting needle, allowing resampling without re-puncturing the pleura, aid re-angling of the cutting needle and allow accurate preplanning of depth of passes.
2. Full resuscitation equipment including equipment for pleural aspiration and chest drain insertion.
Staff should be prepared for recognition and treatment of complications of pneumothorax, vasovagal episodes, haemoptysis and (very rarely) air embolus.
Patient preparation
1. Sedative premedication should be avoided if possible as the patient must remain cooperative so that a consistent breathing pattern can be maintained during the procedure.
2. The procedure can routinely be performed on an outpatient basis with observation for 4–6 hours post procedure, but a bed should be available in case of complications. Particularly frail patients, those with frail carers or dependants, or those living alone should be admitted overnight following the procedure.
3. Clotting screen (ideally INR ≤1.4 and platelets > 100 × 109 l–1). There is no clear evidence that aspirin should be discontinued pre-biopsy but consensus suggests clopidogrel should be stopped 5 days prior to procedure.1
Aftercare
1. Close observation post procedure for at least 1 h in a supervised ward or recovery area, with the patient lying in puncture-site-down position (which should be possible for all but anterior approach interventions). (A limited CT at the end of the procedure will have determined if a pneumothorax or parenchymal bleed is present.)
2. Departmental PA chest X-ray at approximately 1–4 h post procedure. If a pneumothorax has developed (or progressed) then the further management will depend on the size of the pneumothorax and clinical condition of the patient. Small pneumothoraces in asymptomatic patients may be observed; larger pneumothoraces in symptomatic patients will require aspiration or chest drain insertion.
3. High-risk and frail patients, particularly those with pre-existing impairment of respiratory function, are best routinely admitted overnight.
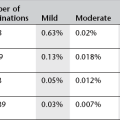
Complications2–4
Usually occur early following the procedure:
1. Pneumothorax in 20%. However, chest drain insertion is necessary in only a small minority (about 3%). The incidence of pneumothorax is increased if:
• the operator is inexperienced
• a larger gauge needle is used
• there is an increased number of needle passes made
• there is a greater pleura to lesion depth
• smaller lesions are biopsied
• the needle traverses a fissure
• the patient is coughing (precipitated by haemorrhage/haemoptysis).
2. Local pulmonary haemorrhage (10%)
4. Other complications, such as haemothorax, implantation of malignant cells along the needle track, spread of infection and air embolism, are all extremely rare
References
1. Malloy, PC, Grassi, CJ, Kundu, A, et al. Consensus guidelines for periprocedural management of coagulation status and hemostasis risk in percutaneous image-guided interventions. J Vasc Interv Radiol. 2009; 20(7):240–249.
2. Gohari, A, Haramati, LB. Complications of CT scan-guided lung biopsy: lesion size and depth matter. Chest. 2004; 126(3):666–668.
3. Yeow, K-M, Su, I-HI-Hao, Pan, K-T, et al. Risk factors of pneumothorax and bleeding: multivariate analysis of 660 CT-guided coaxial cutting needle lung biopsies. Chest. 2004; 126(3):748–754.
4. Manhire, A, Charig, M, Clelland, C, et al. BTS Guidelines: Guidelines for radiologically guided lung biopsy. Thorax. 2003; 58(11):920–936.
Anderson, JM, Murchison, J, Patel, D. CT-guided lung biopsy: factors influencing diagnostic yield and complication rate. Clin Radiol. 2003; 58(10):791–797.
Birchard, KR. Transthoracic needle biopsy. Semin Intervent Radiol. 2011; 28(1):87–97.
Aviram, G, Schwartz, DS, Meirsdorf, S, et al. Transthoracic needle biopsy of lung masses: a survey of techniques. Clin Radiol. 2005; 60(3):370–374.
Richardson, CM, Pointon, KS, Manhire, AR, et al. Percutaneous lung biopsies: a survey of UK practice based on 5444 biopsies. Br J Radiol. 2002; 75(897):731–735.
Methods of imaging pulmonary embolism
1. Plain film chest radiograph. The initial chest radiograph is often normal. Various signs have been described in association with pulmonary embolism but, overall, the chest radiograph is neither specific nor sensitive. It may, however, usefully identify other pathology producing the clinical picture including infection, pneumothorax and rib fracture.
2. Ventilation/perfusion (V/Q) radionuclide scanning. The technique is described later in this chapter. Interpretation of V/Q images is not straightforward and there are a number of causes for the typical V/Q mismatch. Interpretive criteria divide results into normal, very-low and low-probability, intermediate (or indeterminate) probability and high probability groups. Specificity and sensitivity are such that pulmonary embolism is virtually excluded in the ‘normal’ group and is very likely (85–90%) in the high probability group. A significant proportion of patients, however, are placed in the indeterminate/intermediate risk group where specificity is poor and further imaging with CTPA is usually required.
3. Doppler ultrasound of pelvic and leg veins to detect deep vein thrombosis.
4. Multidetector CT pulmonary angiography (CTPA) to diagnose pulmonary emboli down to subsegmental level. Will also assess for presence of secondary right heart strain and for presence of other pathology in the chest. Can be complemented with a CT venography sequence performed at the same examination as CTPA.1
5. Pulmonary arteriography was traditionally the ‘gold standard’ and will detect most pulmonary emboli but has been superseded by multidetector CTPA.
6. MR angiography has yet to find a role in the routine investigation of suspected PE but clearly may be of great benefit in patients where ionizing radiation exposure or the use of iodinated contrast media is relatively contraindicated.
Radionuclide lung ventilation/perfusion (V/Q) imaging
Indications
1. Suspected pulmonary embolism
2. Assessment of perfusion and ventilation abnormalities, e.g. in congenital cardiac or pulmonary disease, e.g. cardiac shunts, pulmonary arterial stenosis, arteriovenous malformations, etc.
3. Quantitative assessment of right-to-left shunting (perfusion only)
4. Quantitative assessment of differential perfusion and ventilation before lung cancer, lung transplant or lung volume reduction surgery1,2
5. Evaluate causes of pulmonary hypertension (to exclude chronic thromboembolism).
Contraindications (to perfusion imaging)
Neither of these are absolute contraindications (indeed, perfusion imaging can be used for assessment of shunts), and it may be considered acceptable to reduce the number of particles administered in these cases.
Radiopharmaceuticals
Ventilation
1. 81mKr (krypton) gas, 6000 MBq max (0.2 mSv ED). Ideal generator-produced agent with a short T1/2 of 13 s and a γ-energy of 190 keV. Simultaneous dual isotope ventilation and perfusion imaging is possible because of different γ-energy to 99mTc. Wash-in and wash-out studies are not possible. Expensive and limited availability
2. 99mTc-Technegas, 40 MBq max (0.6 mSv ED).3 Ultrafine Tc labelled carbon particles, 5–20 nm in size. No simultaneous ventilation and perfusion imaging. Longer residence time in lungs than aerosols, so SPECT and respiration-gated studies possible. Similar diagnostic efficacy to krypton. Expensive dispensing system
3. 99mTc-DTPA, aerosol, 80 MBq max (0.4 mSv ED). Simultaneous ventilation and perfusion imaging not possible. Cheap and readily available alternative to krypton, but less suitable in patients with chronic obstructive airways disease or chronic asthma because clumping of aerosol particles is likely
4. 133Xe (xenon) gas, 400 MBq max (0.4 mSv ED) diluted in 10 l and re-breathed for 5 min. Long T1/2 of 5.25 days and a γ-energy of 81 keV. Ventilation must precede perfusion study because low γ-energy would be swamped by scatter from 99mTc. Wash-in and wash-out studies are possible. Poor-quality images and rarely used.
Technique
Perfusion
1. The injection may be given in the supine, semirecumbent or sitting position (N.B. MAA particle uptake is affected by gravity)
2. The syringe is shaken to prevent particles settling
3. A slow i.v. injection is given directly into a vein (particles will stick to a plastic cannula) over about 10 s. Avoid drawing blood into the syringe as this can cause clumping
4. The patient must remain in position for 2–3 min while the particles become fixed in the lungs
5. Imaging may begin immediately, preferably in the sitting position.
Ventilation
99mTc-DTPA aerosol
1. A DTPA kit is made up with approx. 600 MBq 99mTc ml–1
2. 99mTc-DTPA is drawn into a 5 ml syringe with 2 ml air, then injected into the nebulizer and flushed through with air
3. The patient is positioned initially with their back to the camera, sitting if possible
4. The nose-clip is placed on the patient who is asked to breathe normally through the mouthpiece. The air supply is turned on to deliver a rate of 10 l min–1
5. After reaching a sufficient count rate the air supply is turned off. The patient should continue to breathe through the mouthpiece for a further 15 s
6. The nose-clip is removed and the patient is given a mouth wash and then imaging is commenced.
Computed tomography in the diagnosis of pulmonary emboli
Technique
The technique will depend on individual CT scanner technology. Individual CT manufacturers will recommend specific scanning protocols including delivery of i.v. contrast medium. CT will not only identify the presence of thrombus but allow assessment of secondary right heart strain.1
Computed tomography pulmonary angiography – enhanced scan of pulmonary arterial system1
1. Volume of contrast medium – 100–150 ml or when dual phase injector is used, 60–80 ml of contrast medium followed by saline chase of 30–50 ml
(b) Bolus tracking. A ROI (region of interest) is positioned over the pulmonary artery at the level of the carina. After commencing the injection a ‘tracker scan’ monitors the contrast density within the pulmonary artery and the scan is then triggered when the density at the ROI reaches a preset value – usually 100–120 HU.
3. Rate of injection – 4 ml s–1:
4. Scan from lowest hemidiaphragm to lung apex. Caudocranial scanning may reduce respiratory motion artifact at the lung bases though this is less of an issue with faster multislice scanners
5. Image review and post-processing2 – images should be reviewed at three settings:
Multiplanar reformatted images through the longitudinal axis of a vessel can be helpful to overcome difficulties encountered on axial sections of obliquely oriented arteries, aiding confidence in diagnosis or exclusion of thrombus. If there is no evidence of pulmonary embolism, then need to carefully determine presence of other possible causes of patient’s clinical picture.
Pulmonary arteriography
Indications
1. Demonstration of pulmonary emboli and other peripheral abnormalities, e.g. arteriovenous malformations, when less invasive investigations have been non-diagnostic.
2. Planning and performing therapeutic procedures such as catheter-directed thrombolysis or catheter embolectomy (in patients who cannot receive systemic thrombolysis due to bleeding risk and where surgical embolectomy is contraindicated).
Contraindications1
1. Elevated right ventricular end-diastolic pressure (>20 mmHg) and/or elevated pulmonary artery pressure (>70 mmHg) – where the mortality rate is increased to 2–3% (compared to a documented mortality rate of 0.2–0.5% where pressures are not elevated). Selective arteriography is advised if the results of arteriography are essential to patient management.
2. Left bundle branch block – right heart catheterization may induce complete heart block. Insertion of temporary pacemaker may be indicated prior to the procedure.
Contrast medium
Low osmolar contrast material (LOCM) 370 mg I ml–1; 0.75 ml kg–1 at 20–25 ml s–1 (max. 40 ml).
Additional techniques
1. If the entire chest cannot be accommodated on one field of view, the examination can be repeated by examining each lung. The catheter is advanced to lie in each main pulmonary artery in turn. For the right lung the patient, or the tube, is turned 10° RAO and for the left lung 10° LAO.
2. 40° caudal-cranial view: this view is optimal for the visualization of the bifurcation of the right and left pulmonary arteries, the pulmonary valve, annulus and trunk. With this manoeuvre the pulmonary trunk is no longer foreshortened and is not superimposed over its bifurcation.
Magnetic resonance of pulmonary emboli
A combination of real-time MR (SSFPS – steady-state free precession sequences), MR perfusion imaging (fat 3D gradient-echo sequences) and contrast-enhanced MR angiography (CE-MRA) can be used to detect pulmonary emboli.1 Single-centre studies have shown CE-MRA detecting PE with sensitivities of 77–100% and specificities of 95–100%; there is, however, significant variation in results with high levels of technically inadequate scans and sensitivities as low as 45% in some institutions. The place of MR imaging in diagnosing PE is still evolving but, with the additional benefit of performing lower-limb MR-venography during the same examination, may produce a highly sensitive combined investigation for thromboembolic disease.2
References
Methods of Imaging Pulmonary Embolism
1. Krishan, S, Panditaratne, N, Verma, R, et al. Incremental value of CT venography combined with pulmonary CT angiography for the detection of thromboembolic disease: systematic review and meta-analysis. Am J Roent. 2011; 196(5):1065–1072.
1. Beckles, MA, Spiro, S, Colis, G, Rudd, R. The physiologic evaluation of patients with lung cancer being considered for resectional surgery. Chest. 2003; 123(suppl):105S–114S.
2. Wang, SC, Fischer, KC, Slone, RM, et al. Perfusion scintigraphy in the evaluation for lung volume reduction surgery: correlation with clinical outcome. Radiology. 1997; 205(1):243–248.
3. Win, T, Tasker, AD, Groves, AM, et al. Ventilation-perfusion scintigraphy to predict postoperative pulmonary function in lung cancer patients undergoing pneumonectomy. Am J Roent. 2006; 187(5):1260–1265.
4. Howarth, DM, Lan, L, Thomas, PA, et al. 99mTc Technegas ventilation and perfusion lung scintigraphy for the diagnosis of pulmonary embolus. J Nucl Med. 1999; 40(4):579–584.
5. Freitas, JE, Sarosi, MG, Nagle, CC, et al. Modified PIOPED criteria used in clinical practice. J Nucl Med. 1995; 36(9):1573–1578.
Computed Tomography Pulmonary Angiography – Enhanced Scan of Pulmonary Arterial System
1. Furlan, A, Aghayev, A, Chang, C-CH, et al. Short-term mortality in acute pulmonary embolism: clot burden and signs of right heart dysfunction at CT pulmonary angiography. Radiology. 2012; 265(1):283–293.
2. Wittram, C. How I do it: CT pulmonary angiography. Am J Roent. 2007; 188(5):1255–1261.
1. Gotway, MB, Reddy, GP, Dawn, SK. Pulmonary thromboembolic disease. In: Webb WR, Higgins CB, eds. Thoracic Imaging: Pulmonary and Cardiovascular Radiology. Philadelphia: Lippincott Williams & Wilkins; 2005:609–629.
Magnetic Resonance of Pulmonary Emboli
1. Kluge, A, Luboldt, W, Bachmann, G. Acute pulmonary embolism to the subsegmental level: diagnostic accuracy of three MRI techniques compared with 16-MDCT. Am J Roent. 2006; 187(1):W7–W14.
2. Stein, PD, Chenevert, TL, Fowler, SE. Gadolinium-enhanced magnetic resonance angiography for pulmonary embolism: a multicenter prospective study (PIOPED III). Ann Intern Med. 2010; 152(7):434–443.
Methods of Imaging Pulmonary Embolism
Roy, PM, Colombet, I, Durieux, P, et al. Systematic review and meta-analysis of strategies for the diagnosis of suspected pulmonary embolism. Br Med J. 2005; 331(7511):259.
Stein, PD, Woodard, PK, Weg, JG, et al. Diagnostic pathways in acute pulmonary embolism: recommendations of the PIOPED II investigators. Radiology. 2007; 242(1):15–21.
Parker, JA, Coleman, RE, Grady, E, et al. SNM Practice Guideline for Lung Scintigraphy 4. 0. J Nucl Med Technol. 2012; 40(1):57–65.
Sostman, HD, Stein, PD, Gottschalk, A, et al. Acute pulmonary embolism: sensitivity and specificity of ventilation-perfusion scintigraphy in PIOPED II study. Radiology. 2008; 246(3):941–946.
Computed Tomography Pulmonary Angiography – Enhanced Scan of Pulmonary Arterial System
Remy-Jardin, M, Pistolesi, M, Goodman, LR, et al. Management of suspected acute pulmonary embolism in the era of CT angiography: a statement from the Fleischner Society. Radiology. 2007; 245(2):315–329.
Schoepf, UJ, Costello, P. CT angiography for diagnosis of pulmonary embolism: state of the art. Radiology. 2004; 230(2):329–337.
Stein, PD, Fowler, SE, Goodman, LR, et al. Contrast enhanced multidetector spiral CT of the chest and lower extremities in suspected acute pulmonary embolism: results of the Prospective Investigation of Pulmonary Embolism Diagnosis II (PIOPED II). N Engl J Med. 2006; 354:2317–2327.
Wittram, C, Maher, MM, Yoo, AJ, et al. CT angiography of pulmonary embolism: diagnostic criteria and causes of misdiagnosis. RadioGraphics. 2004; 24(5):1219–1238.
PET and PET-CT of the respiratory system
In recent years, FDG-PET has become an essential part of lung-cancer imaging, adding metabolic information to the morphological information provided by CT. A PET scan is currently recommended for the investigation of lung cancer where the lesion is greater than 1 cm in size and plays an important role in loco-regional and distant staging of non-small cell lung cancer (NSCLC). The scan can be performed either on a dedicated PET scanner or an integrated PET-CT scanner and should be considered in all patients in whom curative-intent treatment is contemplated. Patient preparation and the technique are fully described in Chapter 11.
De Wever, W, Stroobants, S, Coolen, J, Verschakelen, JA. Integrated PET/CT in the staging of non-small cell lung cancer: technical aspects and clinical integration. Eur Respir J. 2009; 33:201–212.
Erasmus, JJ, Rohren, E, Swisher, SG. Prognosis and reevaluation of lung cancer by positron emission tomography imaging. Proc Am Thorac Soc. 2009; 6:171–179.
Paul, NS, Ley, S, Metser, U. Optimal imaging protocols for lung cancer staging: CT, PET, MR imaging, and the role of imaging. Radiol Clin North Am. 2012; 50(5):935–949.
Vansteenkiste, JF, Stroobants, SS. PET scan in lung cancer: current recommendations and innovation. J Thorac Oncol. 2006; 1(1):71–73.
Weber, WA. Assessing tumor response to therapy. J Nucl Med. 2009; 50(5):1S–10S.