Respiratory Care Practice Review
Oxygen Therapy
Patients with cardiovascular and pulmonary impairments frequently need oxygen supplementation.1 Respiratory care practitioners and the nursing staff are generally responsible for administration of this drug under a physician’s order. Therapists have a variety of methods from which to choose to deliver oxygen in the most effective way (individual methods are discussed later in this chapter). Long-term oxygen therapy for patients with chronic obstructive pulmonary disease (COPD) who are hypoxemic has been reported to improve quality of life and life expectancy.2–5 However, even though the benefits of long-term oxygen therapy have been established, U.S. congressional mandates for competitive bidding and caps in rental agreement programs have led to cutbacks. As a consequence, the dose of oxygen and its mode of delivery may need to be modified at rest and during activity.6 This is an issue of significant concern. As practitioners working with patients requiring oxygen, physical therapists need to advocate for their patients to ensure that they receive appropriate oxygen therapy.
The purpose of oxygen therapy is to treat and prevent hypoxemia, excessive work of breathing, and excessive myocardial work.7 Although individual oxygen appliances offer suggested guidelines regarding oxygen administration, the only way to ensure effective delivery from a given device is by blood gas monitoring of PaO2 (partial pressure of oxygen in the arterial blood) or monitoring hemoglobin saturation by oximetry. Medicare and third-party payers have specific indications for oxygen therapy. These indications may differ and physical therapists need to identify these in the practice setting and provide the documentation required for patients to receive the oxygen they need. Initially, a patient may need oxygen only with higher levels of activity or exercise; that needs to be documented by an exercise test that shows desaturation by oximetry. As a patient’s disease progresses, continuous oxygen may be indicated. Careful monitoring of patients will determine when the need for continuous oxygen occurs. Oxygen therapy is usually administered by one of two methods: low-flow or high-flow systems.
Low-Flow Systems
A low-flow oxygen system is one that is not intended to meet the total oxygen requirements of the patient (does not deliver atmospheric oxygen concentration to the patient). For example, using a normal minute ventilation (minute ventilation = tidal volume [TV] × respiratory rate [RR]) of 8 L/min (500 mL × 16 breaths per minute) with a patient receiving 1 L/min of oxygen, the patient is breathing 8 L/min but the device only provides 1 L/min. Thus 7 L/min are contributed from room air. Each time there is a change in the patient’s breathing pattern, tidal volume, and respiratory rate, the fraction of inspired oxygen (FiO2) may also change. Ideally, for efficient use of a nasal cannula, the patient should have a normal tidal volume, respiratory rate, and breathing pattern. This is often not the case, but the cannula is used because it is well tolerated by the patient. This method of oxygen delivery is not used when a specific concentration of oxygen is needed.8
Nasal Cannulas
The nasal cannulas (also called nasal prongs) are one of the most common low-flow devices encountered because of low expense and high patient compliance (Figure 43-1). This device supplies an FiO2 of approximately 24% to 40% oxygen with flow rates from 1 L/min to 6 L/min. Flow rates greater than 6 L/min can cause nasal mucosal irritation and drying. The approximate liter flow and resultant FiO2 values are shown in Table 43-1.
Table 43-1
Approximate Liter Flow and Resultant FiO2 Values
| Flow (L/min) | FiO2 (%) |
| 1 | 24 |
| 2 | 28 |
| 3 | 32 |
| 4 | 36 |
| 5 | 40 |
| 6 | 44 |
Adapted from the American College of Sports Medicine: Guidelines for exercise testing and prescription, ed 6, Philadelphia: Lippincott, Williams & Wilkins, 2000.
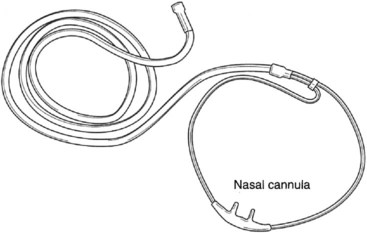
Nasal cannulas deliver 100% oxygen; however, this percentage significantly lessens as the oxygen mixes with inspired air from the room. The amount of oxygen delivered depends on the flow rate and the ventilatory pattern of the patient. A larger minute volume (TV × RR) would dilute the oxygen at any given flow rate and cause a greater decrease in the percentage delivered to the lungs. In other words, the faster and deeper a patient breathes, the more diluted the oxygen becomes. On the other hand, if a patient has a low minute volume, the oxygen percentage delivered increases.7 If precise control of FiO2 is needed, the nasal cannula should not be used.9 In these cases a high-flow system (i.e., a Venturi mask) may be used.
The patient should be encouraged to breathe through the nose to receive maximum benefit from the nasal cannula; however, mouth breathing does not mean the patient will not receive appropriate oxygen.10 Clinically, it is found that some patients who mouth-breathe do so because of nasal polyps, sinus congestion, deviated septum, or other physical issues. If the work of breathing is increased when the patient tries to breathe through the nose, it may be counterproductive.
Simple Mask
The simple mask is another commonly used low-flow oxygen-delivery device. It can deliver from 40% to 60% oxygen, depending on the flow rate and the patient’s ventilatory pattern. This device requires a flow rate of 5 to 6 L/min to prevent rebreathing carbon dioxide and excessive respiratory work.11 As with the nasal cannula, this type of oxygen delivery method should not be used if precise control of oxygen concentration (FiO2) is required because the simply mask is still considered a low-flow oxygen system.
Partial Rebreathing Mask
The partial rebreathing mask is basically a mask with a reservoir bag attached. The oxygen source supplies the bag with 100% oxygen, which then mixes with exhaled anatomical dead-space air that has not taken place in gas exchange. This exhaled air is rich in oxygen. The exhaled air that has taken place in gas exchange and contains CO2 is vented through the open port on each side of the mask. This mask can deliver oxygen concentrations from 70% to more than 80%. It requires flows between 7 and 10 L/min to keep the bag from fully collapsing during inspiration.7
Nonrebreathing Mask
Another low-flow delivery device, the nonrebreathing mask, also contains a bag reservoir, but it can deliver up to 100% oxygen. This mask has valves on the reservoir bag and side vents. This feature prevents ambient air mixing on inspiration and exhaled air mixing on expiration. For this mask to operate effectively, a good seal between the patient’s face and the mask must be achieved. The bag should partially deflate during inspiration (Figure 43-2).
Transtracheal Oxygen Catheter
Another form of low-flow oxygen delivery is the transtracheal oxygen catheter. This has been used for pediatric and adult patients.12,13 It is a cannula that is surgically placed into the trachea via a small incision between the second and third tracheal rings. Generally these devices are used by patients at home who need continuous oxygen therapy. Transtracheal oxygen catheters are more efficient than nasal cannulas, and they have a high patient acceptance rate with low complications.14 Because the oxygen is administered directly into the trachea, 50% less oxygen is needed.7 For people who use portable oxygen systems and for those who require high oxygen flow rates, transtracheal oxygen catheters may be beneficial.15 The catheter can be covered by the patient’s clothing and is therefore cosmetically appealing. Complications such as plugging of the catheter and subcutaneous emphysema have been reported.16,17 These complications may be avoided with proper care of the catheter, good hydration, and maintenance as directed by the patient’s health care team. The transtracheal procedure is not routine in many practice settings; thus if a patient is interested in this form of oxygen therapy, it is wise to find a team that has done the procedure frequently enough to become highly skilled at it.
High-Flow Systems
Venturi Mask
The Venturi mask is a common method of delivering high-flow oxygen concentrations from 24% to 50%. This mask operates via the Venturi principle, which provides for a mixing of 100% oxygen and entrained ambient air. The oxygen flows though a narrow orifice at a high velocity, causing a subatmospheric pressure. This drop in pressure is what causes the ambient air to be entrained through a port. The size of the port determines the amount of air that is entrained, thus the percentage of oxygen delivered. The Venturi mask has a rotating air entrainment port that allows the health care provider to “dial in” the desired FiO2 (Figure 43-3). Flow rates of 40 to 80+ L/min provide minute ventilation at rates that are higher than those the patient could breathe without assistance; consequently, the mask provides the entire inspired atmosphere to the patient. This means that regardless of the patient’s respiratory rate, tidal volume, or breathing pattern, the oxygen delivery (FiO2) will be consistent.
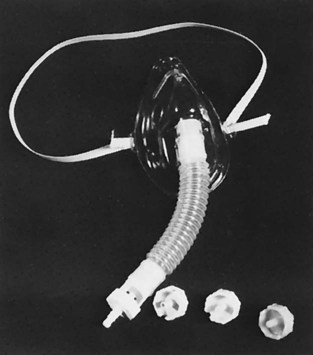
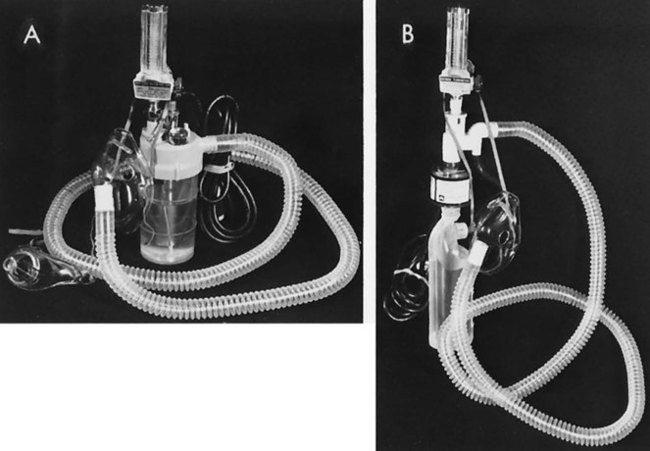
Mechanical aerosol systems also operate via air entrainment, but the mask is connected to the aerosol unit by large-bore tubing to allow a specific FiO2 to be delivered with high humidity (Figure 43-4). Although drainage bags are usually attached to the tubing to collect condensation, the tubing must be monitored for possible pooling of water, which causes flow obstruction to the patient. If partial obstruction occurs, a mild back pressure results in the tubing, causing less air entrainment. This means that a higher concentration of oxygen results and potentially a higher dosage of oxygen than desired may be delivered to the patient.
Portable Oxygen
Home oxygen-delivery systems include high-pressure oxygen cylinders, low-pressure liquid oxygen,18 and oxygen concentrators.8 Additional options include continuous flow versus demand or pulsed oxygen delivery.19–21 There are also a number of oxygen-conserving devices from which to choose.22 When a continuous system is changed to either a demand or pulsed system, or when a new oxygen-conserving device is started, the patient must be monitored carefully. Clinical experience has shown that some patients may not tolerate the same liter flow with a pulsed system, and oximetry and perceived exertion must be evaluated when there is any change in oxygen delivery. The oxygen delivery may not be as effective as a continuous flow device when changing to a pulsed oxygen system. Unfortunately, there is no mandate for clinical testing of the devices before they come to market, so documented effectiveness of one versus another in clinical use is not available.23
Heliox, a combination of 21% oxygen and 79% helium, has been used in acute care for patients who have upper airway obstruction and increased work of breathing (spontaneously breathing patients, as well as those on a ventilator). However, use of heliox has not been widespread because of its cost, which has been estimated to be 13 times that of oxygen. Heliox for portable oxygen and home use has been documented as effective for patients with asthma and COPD. It has been shown to decrease airway resistance and decrease the work of breathing and has also been effective with patients who have increased mucus secretions. Studies have demonstrated an increase in patients’ ability to exercise using heliox; however, it has not been shown to significantly decrease dyspnea.24–26
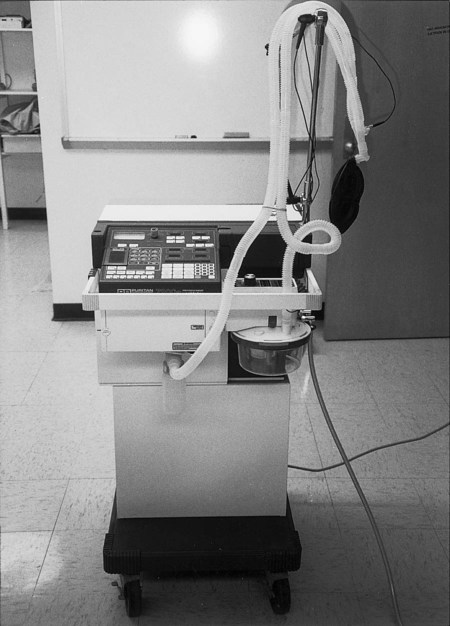
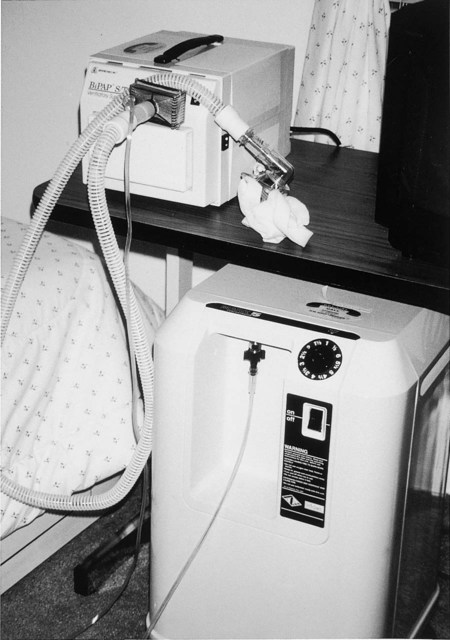
Oxygen concentrators are commonly used in the home health setting, especially because Medicare offers coverage for these devices (Figure 43-5). They are electrically powered and create oxygen by drawing ambient air across a semipermeable membrane, separating oxygen from nitrogen. They generally operate at 2 L/min and provide FiO2 90% oxygen output. Long oxygen tubing, up to 50 feet, allows patients extra mobility. Patients using concentrators should have a back-up device, such as a portable tank, in case of a power outage. In addition, the electrical power company should be notified of any patient who is using oxygen by concentrator so that the patient’s location is designated as a high priority for backup and restoration of power if an outage occurs.
Continuous (Constant) Positive Pressure Breathing
CPAP may be used to improve oxygenation27,28 in patients for whom the usual means of oxygen delivery is not effective or for those with obstructive sleep apnea.29 Sleep apnea and COPD often occur together; recently, recognition of when “overlap syndrome” occurs there is higher mortality than either disease process alone.30 CPAP has also been used to help the transition of weaning patients from mechanical ventilation,31 including infants who have had cardiac surgery. CPAP can help stabilize these infants and normalize their spontaneous breathing pattern.32 It has also been useful in the management of respiratory distress in premature babies and decreases the need for invasive mechanical ventilation.33 Early intervention using CPAP in older patients with cardiogenic pulmonary edema has also been effective.34 Quality-of-life predictors have been shown to be positive a year after initiation of CPAP; improvement was noted at 3 months after initiation of CPAP and continued at 1 year.35,36
Patients who are mouth breathers may have difficulty adjusting to CPAP, thus rendering it less effective in these cases. Those with moderate to severe sleep-disordered breathing have been found to be less adherent to CPAP therapy than are who are nose breathers. This is related to a leak that compromises the CPAP.37
Use of Oxygen to Improve Exercise
Oxygen has been shown to increase exercise performance in patients with COPD who have moderate to severe airflow obstruction and mild hypoxemia at rest.38–40 It has also been shown to benefit patients with COPD who are nonhypoxemic at rest.41,42 Breathlessness is the most common symptom that limits exercise tolerance. Oxygen supplementation will often provide an increased driving pressure of oxygen, which allows the patient to decrease the work of breathing.43 Peripheral muscle weakness has been found in many patients with COPD. Improving exercise tolerance will result in improved muscle strength and endurance. Another consideration, if hyperoxia is not enough, is the use of noninvasive positive pressure (NPPV). This is still somewhat controversial and requires more study, but in this author’s clinical opinion, NPPV can be very beneficial.44 As previously discussed in this chapter, heliox has been shown to improve exercise tolerance in patients with asthma and COPD who have upper airway obstruction, inflammation, and increased mucus secretions.
Noninvasive ventilation will be discussed later in the chapter, but it is interesting to note that in some pulmonary rehabilitation programs it is being used in addition to supplemental oxygen with very positive results. The combination of oxygen and noninvasive ventilation was shown to be better than supplemental oxygen alone.45 The rationale for this improvement when using both oxygen and noninvasive ventilation is that in patients with severe COPD, the ventilatory muscles can be “unloaded” and this may promote higher levels of exercise.46
Additional Respiratory Modalities
Incentive Spirometry
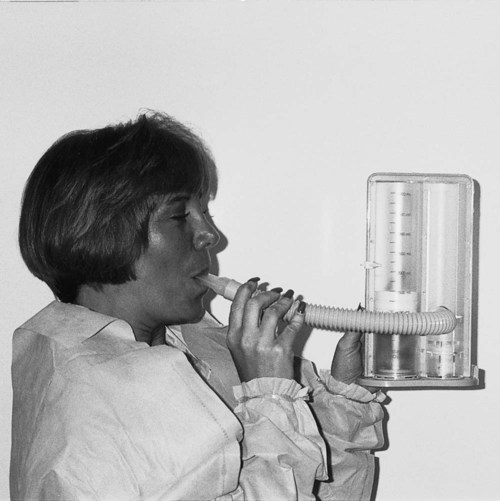
Incentive spirometry (IS), also called sustained maximum inspiration (SMI), is a visual and/or audio feedback device that encourages slow, deep inspiration (Figure 43-6). Generally this treatment is performed frequently, up to every hour, and its purpose is to treat and prevent atelectasis and pneumonia, especially in postoperative patients who are considered a high risk for postoperative complications.47–51 In many acute care settings, IS is done routinely. Several articles challenge the routine use of IS and have found that the addition of IS added no benefit to breathing exercise postoperatively.52–55 In a study of patients scheduled for lung resection, when a combination of inspiratory muscle training and IS was performed before and after lung resection, there were significant lung function improvements in FEV1 that were higher postoperatively than preoperatively.52
Humidity and Aerosol Therapy
Humidity Therapy
Humidification is the addition of water vapor in its molecular form to a gas. When a dry gas is administered to a patient (e.g., via a nasal cannula), some type of humidification appliance is used to prevent unnecessary complications. Flows of 2 L/min or less may not require humidification when using a nasal cannula. Humidification therapy is also indicated in the presence of thick tenacious secretions and when an artificial airway is in place. Artificial airways, such as endotracheal and tracheostomy tubes, bypass the normal humidification system (the upper airway); therefore supplementation is essential.56
There are basically two types of humidifiers. Bubble-through humidifiers are those that are generally used with simple oxygen appliances. The passover type of humidifier is usually found in conjunction with a mechanical ventilator. Both bubble-through and passover humidifiers are available for ventilators,57 and they are usually heated to warm the humidified air to body temperature before it enters the airway.7
Aerosol Therapy
An aerosol is created when a suspension of liquid or solid particles exists in a gas. Two common forms of aerosol medication delivery in the clinical setting are the small-volume nebulizer (SVN) and the metered-dose inhaler (MDI). A bland aerosol is administration of water or saline solution to the patient’s lungs.58
In general the goals of aerosol therapy are to hydrate dried retained secretions, to improve cough efficiency, to restore and maintain function of the mucociliary escalator, to deliver medications, and to humidify gases delivered through artificial airways. The MDI is strictly used for medication delivery (see Chapter 45).
Other forms of aerosol delivery are the spinning disk (such as in a room humidifier or mist ) and the ultrasonic nebulizer. Both of these are electrically powered as opposed to the SVN, which is pneumatically powered (Figure 43-7).59

A key element in aerosol delivery is particle size. The size of the aerosol particle will determine its ability to penetrate the airway before depositing or raining out. The therapeutic range is considered 1 micron, with the smaller range of particles having the greatest penetrating ability. The larger particles deposit sooner. If they are greater than 5 microns, then the chances of entry into the airway are less. The particles may deposit in the nose and proximal airway. The greatest amount of alveolar deposition (95% to 100%) occurs in the 1 to 2 micron range. On the other hand, aerosol particles smaller than 1 micron are so stable that they may not deposit at all.7
Comparisons between the ability of SVNs and MDIs to deliver medications have found that the MDI is either equal in efficacy or outperforms nebulizers. Significant cost savings are also realized by those institutions that recognize MDI usage as an effective means of aerosol medication delivery over SVN.60
To further enhance the efficacy of the MDI treatment, the recommendation is that a spacer or holding chamber may be attached to hold the aerosol particles before inhalation. This device allows greater drug particle deposition to the airways and reduces oropharyngeal deposition.61 Ventilator patients who are receiving drug aerosol therapy also receive greater benefit from an in-line MDI with a holding chamber compared with a jet nebulizer.62
Intermittent Positive Pressure Breathing
Intermittent positive pressure breathing (IPPB) continues to be used in some settings, but there is little evidence to support its efficacy as a treatment modality.58
This particular technology was developed during World War II to assist pilots breathing in unpressurized cabins at high altitudes. IPPB subsequently became a very popular respiratory therapy device in the 1960s and 1970s (Figure 43-8). Its use began to decline in the 1980s. In 1983 the National Heart, Lung, and Blood Institute reported that IPPB has limited therapeutic benefit. This clinical trial is only one of several studies that show IPPB is an outmoded medical technology. Research dating back to the 1950s questions the efficacy of this device.63
Although the use of IPPB is questionable in regard to its clinical efficacy, it may be a beneficial form of treatment in acute asthma or COPD that is refractory to standard therapy, atelectasis that has not responded to simpler therapy, and the prevention of respiratory failure in patients with kyphoscoliosis and neuromuscular disorders.64
Mechanical Ventilation
Many disease states that lead to cardiac and/or respiratory failure will require mechanical ventilation to support the patient’s effort to ventilate and oxygenate (Figure 43-9). Patients receiving mechanical ventilator support can be found in many settings, from the acute care hospital to skilled nursing facilities and home care. Children needing continuous mechanical ventilation who live in the home and community need to be integrated into the school system and community recreational facilities. Patients with acute exacerbations of disorders such as emphysema, COPD, and chronic bronchitis may require mechanical ventilation and are generally seen in hospital intensive care units and weaned before they are discharged home. Patients with disorders requiring long-term ventilation, such as spinal cord injury, brain injury, and certain neuromusculoskeletal diseases, may be found receiving mechanical ventilation in rehabilitation hospitals, the home, or a long-term care facility. According to the American Association for Respiratory Care (AARC), the scope of practice for the respiratory therapist has expanded to include anywhere that patients with respiratory disease present. Therapists currently practice in hospitals, long-term care, pulmonary rehabilitation, patients’ homes, and pulmonary physicians’ offices.
Over the past 20 years there has been an increase in the use of noninvasive mechanical ventilation (NIMV) in patients with respiratory failure to avoid the risks involved with intubation. It is becoming the standard “first line therapy in several situations” in acute care.65
Several other patient populations have also been supported and their health and sleep improved through the use of NIMV, among them patients with end-stage Duchenne muscular dystrophy, cystic fibrosis, and other neuromuscular dysfunction. In patients with Duchenne MD the pulmonary function data are monitored and the patient may be started on NIMV only at night, progressing to continuous ventilation as needed.66 This has also been shown to prolong life and eliminate the need for tracheostomy in these patients needing ventilation.67 In patients with cystic fibrosis, as the disease process progresses, a heavier workload is placed on the respiratory muscles. The patient will often develop a rapid, shallow breathing pattern that results in decreased alveolar ventilation. NIMV may reduce respiratory muscle work of breathing and improve gas exchange. It can decrease oxygen desaturation during exercise and airway clearance and help in patient recovery following an exacerbation. More data are needed to evaluate long-term benefits and criteria for the use of NIMV in people with cystic fibrosis.68
Invasive Versus Noninvasive Mechanical Ventilation
Invasive mechanical ventilation involves the insertion of an artificial airway into the trachea that attaches to ventilator tubing. Noninvasive mechanical ventilation (NIV) is delivered by a nasal or facial mask that attaches to a positive airway pressure BiPAP machine. Patient preferences are observed in an attempt to have them feel comfortable and increase adherence to using NIV. In one study of 60 patients with acute respiratory failure being treated with NIV, no preference between the standard oronasal mask and a total face mask was found.69 Noninvasive mechanical ventilation is growing in use, especially for acute exacerbations of COPD. It has been used primarily for patients with acute hypercapnic ventilatory failure, but its use is now expanding to larger populations. Benefits of NIV include a reduction in the need for intubation, a decrease in complication rate, and a reduced length of hospitalization. One factor in the success of NIV is the early delivery of ventilation in patients with respiratory failure.70
In a study involving medical-surgical intensive care units in North American, South America, Spain, and Portugal, 1638 patients were studied who were receiving mechanical ventilation. The median age of study patients was 61 years. Indications for mechanical ventilation were acute respiratory failure (66%), acute exacerbation of COPD (14%), coma (10%), and neuromuscular disorders (10%). Mechanical ventilation was administered via endotracheal tube in 75%, tracheostomy tube in 24%, and facial mask in 1% of patients. A total of 47% of patients were ventilated on an assist-control mode and 46% were ventilated with synchronized intermittent mandatory ventilation (SIMV), pressure support, or a combination of both modes.71 In North America it seems that, clinically, the trend toward NIV is growing significantly.72–74
Patients with chest wall restriction such as severe kyphoscoliosis also benefit from NIV. Ventilation and oxygenation go hand in hand. If the chest wall is not moving, ventilation is decreased. Just giving oxygen to patients with severe thoracic restriction will not bring them to optimal respiratory function. The NIV provides improved ventilation that will improve patient function and endurance.75
BiPAP is a noninvasive form of ventilation that uses a tightly fitted oronasal mask that delivers positive pressure at two different levels, one for inspiration and another for exhalation, both of which are above atmospheric pressure. It may also be referred to as pressure release ventilation. Indications for BiPAP include signs of respiratory failure or chronic respiratory failure in patients with severe COPD, increased work of breathing, patients with neuromusculoskeletal impairments that limit ventilation and thus oxygenation, and sleep disordered breathing. Use of BIPAP has improved outcomes in terms of less daytime fatigue and improved activity levels. In addition, it may be used as a bridge for patients such as those at the end stage of cystic fibrosis who need lung transplants.76,77
Modes of Mechanical Ventilation for Positive Pressure Ventilation (Invasive Mechanical Ventilation)
Trigger. Variable that causes a breath to be delivered by the ventilator. A patient may inhale, causing the ventilator circuit pressure to drop to a preset number (i.e., less than 1 or 2 cm H2O). This is called a pressure trigger. Some ventilators are volume and flow triggered.
Flow rate. The speed at which the ventilator breath is delivered. This parameter is usually measured in liters per minute.
Frequency. Refers to the number of breaths delivered over time (e.g., 10 breaths per minute).
Spontaneous breath. Breathing through the ventilator circuit without assistance.
The following are descriptions of common current ventilator modes.78
Controlled mechanical ventilation (CMV) or total support of ventilation. The control mode is now a lesser-used method of ventilation and generally requires the patient to be sedated and paralyzed. The ventilator delivers all breaths at a preset frequency, volume or pressure, and flow rate. The patient cannot take spontaneous breaths or trigger the machine. This mode may be used when total control of ventilation is needed (e.g., during surgery, in patients with high-level quadriplegia).
Assist control (AC) or partial support of ventilation. The patient receives a preset pressure or volume, frequency or number of breaths, and flow rate. In between machine-cycled breaths, the patient can trigger the machine to deliver another breath at the preset parameters. All breaths are machine delivered. No spontaneous breathing can occur.
Assisted mechanical ventilation. This mode is similar to AC; however, there is no set frequency. The patient triggers the machine at will to deliver a set pressure or volume at a set flow rate.
Intermittent mandatory ventilation (IMV). As the ventilator delivers a set mandatory frequency and volume or pressure, the patient is allowed to take spontaneous breaths between cycles. The problem with this mode is that the breath is delivered without regard to the patient’s breathing cycle. This has usually been replaced by an improved method, synchronous intermittent mandatory ventilation (SIMV).
SIMV. This mode synchronizes the machine-delivered breaths (IMV) with the patient’s spontaneous breaths. In IMV the machine may cycle a breath before the patient can completely exhale a spontaneous breath. If no inspiratory effort is present, the machine delivers the mandatory breaths. Usually, the preset number of breaths is low, allowing more effort with support on the part of the patient.
CPAP. The patient allows the patient to spontaneously breathe and has a preset level of pressure that is constantly maintained during the whole respiratory cycle. This method of positive pressure support can also be achieved through use of commercially available pneumatically powered units that hook directly into the oxygen wall outlet. A tight-fitting mask is secured around the patient’s mouth and nose, and a preset pressure and oxygen percentage is delivered.
BiPAP. A noninvasive form of mechanical ventilation usually delivered through a tight-fitting oronasal mask. There are different pressures for inspiration and exhalation, which are always above atmospheric levels. Inspiratory pressure is higher than expiratory pressure.
Airway pressure release ventilation (APRV). This may also be called pressure release ventilation. The patient is allowed to spontaneously breathe with a set amount of CPAP. If additional ventilation is required, the CPAP will be dropped periodically, releasing the pressure, causing the patient to exhale. When the exhalation is complete, CPAP is restored. Proponents of this mode claim that by allowing the patient control, patient comfort and compliance are high.
Pressure support ventilation (PSV). When using pressure support, the patient is allowed to breathe spontaneously, triggering a preset amount of inspiratory support until the flow rate reaches a minimal level of preset pressure in the airway. The patient controls the frequency, tidal volume, and inspiratory time. This mode is often used in conjunction with SIMV. This mode is also popular because of high patient compliance. The pressure is set for safe levels, and the volume is variable. When the patient breathes in, the volume continues until the preset pressure is reached. That is the end of inspiration.
Mandatory minute ventilation (MMV). The patient is allowed to breathe spontaneously; however, a minimal level of minute ventilation will be achieved through ventilator-assisted breaths. This is usually accomplished by using PSV.
Volume-assured pressure support (VAPS). This is one of the newest modes of ventilation. It allows the patient to breathe spontaneously in the PSV mode and monitors each breath’s tidal volume. If the breath is not going to reach the set volume, the ventilator will hold the flow rate constant and increase the pressure until the desired volume is reached.
Alarm Management and Precautions
The most common alarms are those that monitor high and low pressure, FiO2, apnea, disconnection, and volume. The high-pressure alarm is the one that sounds most commonly when the patient is receiving physical therapy. This alarm indicates that more than the preset pressure is needed to deliver the volume of ventilation. Generally, if the high-pressure alarm continues to sound, the patient should be checked for secretions. Suctioning can remedy this problem. The ventilator tubing should also be checked for possible occlusion from compression or excessive water buildup (Figure 43-10). High-pressure alarms may also sound in the case of bronchospasm or breath holding. Do not use strong resistance exercise with patients on mechanical ventilation because they may hold their breath and perform a Valsalva maneuver, which will cause increased circuit pressure to deliver the tidal volume to the patient. Low pressure alarm may signify a leak in the ventilator circuitry or a disconnection from the machine. Before turning a patient or performing upper extremity exercise, make sure there is clearance and ease of movement in the ventilator circuit tubing to prevent it from coming off during the interventions. In one case (in an unnamed medical center’s intensive care unit) a patient’s low-pressure alarm sounded and the patient was bagged while the cause was evaluated. The source was a disconnection that occurred when a new employee from the housekeeping department unplugged the ventilator to use the plug for a cleaning machine. When the low-pressure alarm sounds, first consider that the patient is not being ventilated.
Weaning from Mechanical Ventilation
Weaning is generally initiated when the reason for placing the patient on mechanical ventilation is reversed. Several factors need to be evaluated. Is there adequate ventilation and oxygenation? During weaning, the work required by the patient to breathe may increase and oxygen may need to be titrated appropriately. Hemodynamic stability must be monitored. Using CPAP during weaning may provide the bridge necessary to wean with less stress and decreased ventilatory demand. In general in patients who are receiving mechanical ventilation, the ventilator is discontinued and then the artificial airway is evaluated and removed. In some patients with neuromuscular and musculoskeletal issues, however, ventilator weaning by lung expansion with NIV and decannulation will be a better solution.79
Some patients with neuromusculoskeletal concerns may use other mechanical means of ventilation, such as a pneumobelt.80 The pneumobelt is a noninvasive device placed over the abdomen. It has a bladder that inflates and mechanically puts pressure on the abdomen, thereby causing exhalation. When the bladder deflates, the diaphragm descends and inspiration occurs. Another negative pressure device used to help patients with neurological deficits is the chest cuirass, which resembles a turtle shell placed over the chest wall. Negative pressure is applied to the chest wall, which elevates the thorax to provide inspiration and then releases to allow for exhalation. The benefits of these mechanical aids are that the patient does not need an artificial airway and he or she is provided with a more physiological means of ventilation. They are well received by many people with neurological impairments.
Role of the Physical Therapist
The physical therapist can have a significant role in keeping the patient who is mechanically ventilated from having decreased aerobic capacity by helping the patient perform aggressive mobilization (see Chapters 18, 19, and 20), exercise, airway clearance techniques, and breathing strategies and interventions (see Chapters 21, 22, and 23). The physical therapist can also play a role in finding optimal positions to support the patient who is being weaned. Therapists who have been working on breathing strategies can be a source of comfort and encouragement for the patient during the weaning periods. Active mobilization early in the course of mechanical ventilation will result in more successful outcomes.
Evidence now supports the use of early physical and occupational therapy by giving patients sedation breaks and rousing patients to exercise. This has been shown to result in better functional outcomes at discharge, fewer ventilator days, and fewer days of delirium compared with standard ventilator treatment without waking patients for therapy.81,82