CHAPTER 30 Refractive surgery with phakic IOLs
Fundamental principles
Phakic IOLs have several advantages over other types of refractive surgery in high ametropias. Unlike laser corneal surgery, they are not associated with regression (no wound healing) and do not change the normal shape of the cornea (better quality of vision)1. Also phakic IOLs do not interfere with accommodation, presenting in young patients important advantages over lens surgery.
Indications for surgery, anatomical considerations, and preoperative assessment
The general indications for phakic IOLs are:
Although these are general indications for phakic IOLs, in some special circumstances these criteria can be slightly adapted to a particular case. In myopia, phakic IOLs may be the procedure of choice in lower degrees if the cornea is too thin (less than 480 µm) or some form of ectacic disorder (even subclinical) is present. Very steep corneas are not suitable for laser treatment in hyperopia and may be more correctly addressed with intraocular surgery. Concerning age, phakic IOLs may be also eventually used in anisometropia in children2. Above the age of 50, as accommodation is waning, the use of phakic IOLs is generally discontinued. Intraocular pathology like diabetic retinopathy, uncontrolled glaucoma, and any form of uveitis are considered contraindications to the implantation of phakic IOLs. On the other hand, corneal ectactic disorders may be (if stable) a good indication.
Anterior chamber depth is very important for the safety of implantation of all types of phakic IOLs. It must be measured from the endothelium to the anterior surface of the natural lens and the minimum is 2.80 mm. Recent studies even show that a 3.00 mm depth improves the safety3. The anterior chamber depth may be determined with different devices. The most common are the Orbscan (B&L), Pentacam (Oculus), IOL Master (Zeiss), and the OCT (Zeiss or Heidelberg Engineering). Ultrasonic biometers are not suitable as they include the thickness of the cornea in the AC depth measurement. If implantation of a phakic IOL is done in a shallow anterior chamber, the risk of endothelial cell loss and eventually corneal decompensation is too high.
Anterior and posterior chamber sizes are very important for the implantation of some phakic IOLs. Angle-supported anterior chamber phakic IOLs need to match exactly with anterior chamber dimensions. If they do not, important complications like rotation and decentration of IOL (IOL too small) or pupil distortion and iris atrophy (IOL too large) may occur. Likewise the sulcus fixated posterior chamber phakic IOLs need adequate size to avoid touching the natural lens, causing cataracts (small IOL), or pushing the iris forward closing the angle (IOL too large). Concerning this problem, iris-fixated phakic IOLs have a great advantage as ‘one size fits all’. Classically to determine the angle-to-angle and sulcus-to-sulcus distances the white-to-white measurement (W/W) was done with a calliper or with instruments such as Orbscan, Pentacam, or IOL Master. However, this measurement does not always correlate with the intraocular measurements leading to errors in IOL size4. Nowadays, at least for angle-supported anterior chamber phakic IOLs, the OCT does a precise ‘in vivo’ measurement of the angle-to-angle distance. Unfortunately, there is still no device allowing us a perfect measurement of sulcus-to-sulcus distance.
Once all the above criteria are met, to implant a phakic IOL, we need to determine its power. To do that, the most used formula is the one developed by Van der Hejde5, which takes into account the spherical equivalent (cycloplegic for hyperopia), anterior chamber depth, and keratometry.
Goals of surgery
The goal of surgery is to correct the ametropia in a permanent and stable way.
Phakic Acrysof Caché
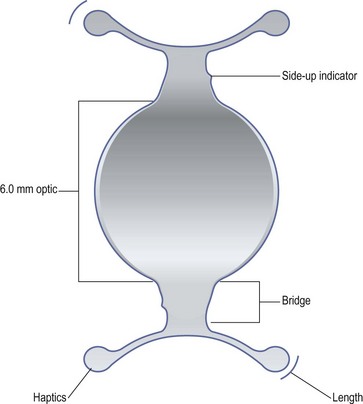
The Phakic Acrysof is an anterior chamber angle-supported phakic IOL (Fig. 30.1) made of hydrophobic acrylic with an optic of 6.0 mm and four haptics to ensure the angle fixation. It is available only for myopia (−6.00/−16.00) and has four different sizes in order to fit perfectly in the anterior chamber (12.5, 13, 13.5, and 14 mm).
Artiflex
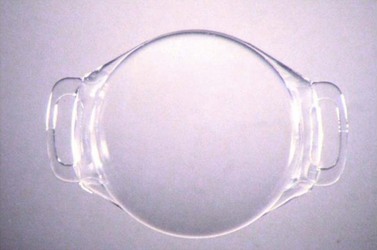
The Artiflex is an anterior chamber iris-fixated phakic IOL (Fig. 30.2) with a design similar to the Artisan. It is has a 6.0 mm optic made of polisyloxane (silicone) and two haptics (claws) made of PMMA. The overall diameter is also 8.5 mm and ‘one size fits all’. It is available for myopia (−2.00/−14.50) and astigmatism (myopic up to −7.50).
ICL
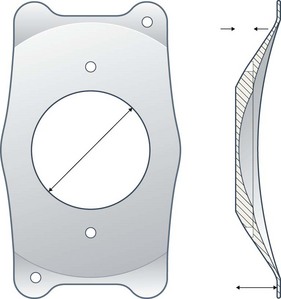
The ICL is a posterior chamber phakic IOL designed to fit in the ciliary sulcus (Fig. 30.3). It is of a plate haptic shape made of ‘collamer’ and has an optic diameter from 4.65 to 5.50 mm (myopia, according to power) or 5.50 mm (hyperopia) and four haptics to ensure the fixation in the ciliary sulcus. It is available for myopia (−3.00/−23.00), hyperopia (+3.00/+21.50), and astigmatism (myopic up to −6.00).To ensure a perfect fit in the ciliary sulcus, the ICL comes in four different sizes for myopia and astigmatism (11.5, 12, 12,5, and 13 mm) as well as for hyperopia (11, 115, 12, and 12.5 mm).
Anesthesia
All phakic IOLs can be implanted in topical, peribulbar, or general anesthesia. This should be a patient and surgeon choice. In Artisan, as a large incision is used (see Operation techniques), we recommend the use of general anesthesia in the learning curve.
Operation techniques
Intraoperative complications
Postoperative care
Postoperative complications
1 Waring G. Comparison of refractive corneal surgery and phakic IOLs. J Refract Surg. 1998;14:277-279.
2 Lesueur LC, Arne JL. Phakic intraocular lens to correct high myopic amblyopia in children. J Refract Surg. 2002;18(5):519-523.
3 Doors M, Cals D, Berendshot T, et al. Influence of anterior chamber morphometrics on endothelial cell changes after phakic intraocular lens implantation. J Cataract Refract Surg. 2008;34:2110-2118.
4 Werner L, Izak A, Pandey S, et al. Correlation between different measurements within the eye relative to phakic intraocular lens implantation. J Cataract Refract Surg. 2004;30:1982-1988.
5 Heijde GL. Some optical aspects of implantation of an IOL in a myopic eye. Eur J Implant Refract Surg. 1989;1:245-248.
6 Budo C, Hessloehl JC, Izak M, et al. Multicenter study of the Artisan phakic intraocular lens. J Cataract Refract Surg. 2000;26:1163-1171.
7 Marinho A. Complications of iris-supported phakic IOLs. In: Alio J, Azar D, editors. Management of Complications of Refractive Surgery. Berlin: Springer; 2008:238-244.
8 Sanders D. Anterior subcapsular opacities and cataracts 5 years after surgery in the Visian implantable collamer lens FDA trial. J Refract Surg. 2008;24:566-570.
9 Lovisolo C, Mazzolani F. Complications of iris-supported phakic IOLs. In: Alio J, Azar D, editors. Management of Complications of Refractive Surgery. Berlin: Springer; 2008:245-264.