Radiation in Pregnancy and Clinical Issues of Radiocontrast Agents
The Joint Commission on Accreditation of Healthcare Organizations (JCAHO) published a sentinel alert1 in August 2011 highlighting the radiation risks of diagnostic imaging in all patients, not just pregnant patients. This alert underscores the fact that x-rays are officially considered a carcinogen. Over the past 2 decades, total exposure to ionizing radiation has nearly doubled. Published reports estimate that the incidence of cancer secondary to radiation is 0.02% to 0.04%.
In utero exposure of the embryo or fetus to radiation generally causes great, but largely unnecessary anxiety in patients, their families, and the clinician. Much of this anxiety is secondary to a general misconception that any exposure to radiation is harmful and will result in an anomalous fetus. More often than not, clinicians themselves add to the confusion and fear by providing exposed women with erroneous information. Many clinicians, nurses, and even radiologists are ignorant of the qualitative and quantitative effects of ionizing radiation.2 Multiple surveys in the literature reveal clinicians’ dearth of knowledge about radiation exposure. This misinformation could lead to inappropriate abortions and litigation. For example, in Greece after the Chernobyl disaster, 23% of pregnancies were terminated because of unsubstantiated fears of teratogenicity.3 A better understanding of the true risk estimates may help alleviate this fear.
It is widely held and published that concerns about the possible effects of exposure to ionizing radiation should not prevent medically indicated diagnostic procedures from being performed on the mother. It is not standard of care to withhold necessary radiologic studies because of fear of fetal injury from diagnostic studies. According to the American College of Radiology, “No single diagnostic x-ray procedure results in radiation exposure to the degree that would threaten the well being of the preembryo, embryo, or fetus.”4–6 This remarkable statement helps put into perspective the effects of diagnostic radiation exposure on pregnancy. Standard diagnostic radiologic procedures performed in the ED are not associated with significant proven fetal risks. A clear understanding of these risks enables clinicians to make an informed decision and knowingly counsel patients that radiologic procedures provide more benefit than harm.
Evaluation of a pregnant patient exposed to radiation should involve consideration of the type of radiation, types of examinations performed, gestational age, and radiation dose to determine an estimation of risk. The radiation dose of interest is the dose absorbed by the embryo or fetus and not by the mother. However, recent articles7,8 have raised concern about exposure of maternal breast tissue to radiation and postulate a relationship to breast cancer decades later. The main goals of this chapter are to review the basic issues of pregnancy and radiation exposure and to provide a practical approach for clinicians in choosing a technique that entails the least risk and in counseling patients who have undergone or will undergo an emergency diagnostic procedure.
Units of Radiation
The dose equivalent, expressed in rem or sievert (Sv), is used to quantify the degree of biologic effect (1 Sv = 100 rem). This unit reflects the biologic response and can be used to compare the effects of different types of radiation. The dose equivalent is the product of the absorbed dose times a quality factor. The quality factor depends on the mass and charge of the radiated particle and is approximately 20 for an α-particle and 1 for x-rays and γ-rays. Therefore, for diagnostic radiographs, CT scans, and 99Tc nuclear studies, the absorbed dose is equal to the dose equivalent; that is, an absorbed dose of 1 rad yields a dose equivalent of 1 rem (1 Gy = 1 Sv) (Table 72-1). All reference data have been converted into rad units for uniformity and comparison throughout the chapter.
Timing of Radiation during Pregnancy and Its Effects
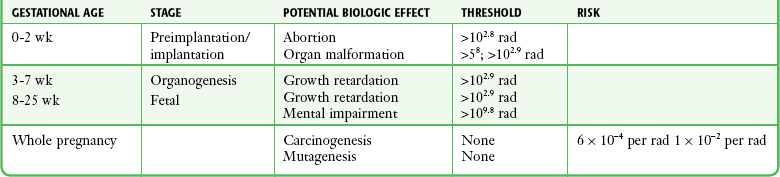
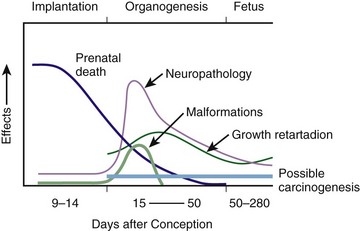
The effects of exposure to radiation on the conceptus depend on the gestational age and the amount of absorbed dose. The relationship between radiation-induced effects and stage of pregnancy is shown in Figure 72-1.9 The harmful effects of ionizing radiation have the following principal biologic effects: intrauterine death, organ malformation, mental impairment, fetal growth retardation, cancer, and genetic mutation.2
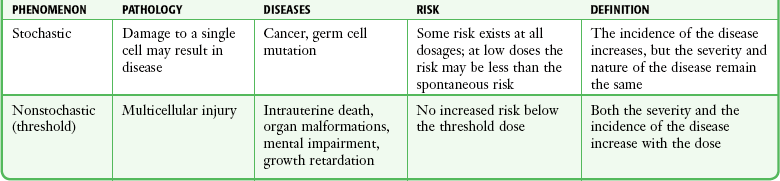
Radiation-induced health effects are divided into two broad categories, stochastic and nonstochastic (Table 72-2). Stochastic effects, such as cancer or genetic mutation, can result from alterations produced in a single cell and are presumed to exist even at low exposure.2 The probability of such an effect occurring increases with dose, and there is no identifiable threshold dose below which the chance is known to be zero. It is important to recognize that at low doses of radiation, the risks are far below the spontaneous incidence of carcinogenesis10 or mutagenesis.11
TABLE 72-2
Stochastic and Nonstochastic (Threshold) Comparison
Modified from Brent RL. Utilization of developmental basic science principles: the evaluation of reproductive risks from pre- and postconception environmental radiation exposures. Teratology. 1999;54:182.
The remaining harmful biologic effects mentioned earlier are nonstochastic effects. Nonstochastic effects require multicellular injury and have a threshold dose below which deleterious effects do not occur.2 It is important to emphasize that the vast majority of embryopathologic effects are believed to be threshold phenomena; therefore, a dose of ionizing radiation below the threshold will not produce these effects.
Stages of Fetal Development
Preimplantation and Implantation Phase
During the preimplantation and implantation phase, the principal radiation-induced health effect is abortion.12 When the number of cells in the conceptus is small and their nature not yet specialized, the effect of damage to these cells is most likely to take the form of failure to implant or undeterminable death of the conceptus.10 The no-effect threshold of an absorbed dose is quite high, estimated at 10 to 15 rad,12 and not likely to be approached by diagnostic ED radiographs or radionuclide testing. By the time that the pregnancy is at term, the threshold for causing intrauterine mortality has risen to about 100 rad.12 These estimates have been extrapolated from animal data. This period has been referred to as the “all-or-none period” because radiation is more likely to kill the embryo than result in a live malformed newborn.
Few human epidemiologic data are available for this period of gestation. Because many women are certainly unknowingly exposed to diagnostic radiation during this period, the lack of such data suggests no association between diagnostic radiation exposure and embryo death. Data from the Japanese atomic bomb experience have been cited for reference, but such a correlation is difficult to justify scientifically. Nonetheless, these data show a decrease in the number of offspring who retrospectively would have been 0 to 3 weeks’ postconceptional age at the time of this significant radiation exposure, thus suggesting increased fetal loss caused by irradiation during preimplantation.13 This decrease in the birth rate is probably multifactorial because stress, disease, and malnutrition were coexistent during this traumatic time. Importantly, fetal loss from exposure to an atomic bomb cannot be scientifically extrapolated to exposure to diagnostic radiation.
Any discussion concerning the potential adverse effects from diagnostic radiation must take into account the natural incidence of spontaneous abortion. Because the main effect of exposure to radiation during the first few weeks after fertilization is abortion as a result of death of the embryo, it is paramount to note that the normal incidence of spontaneous abortion in humans not exposed to radiation is in the 30% to 50% range.2 Exposure to less than 10 rad yields no statistical change in the rate of preimplantation and early postimplantation spontaneous abortion from the expected baseline (Table 72-3).
TABLE 72-3
Risks and Threshold Doses of the Main Effects of Prenatal Irradiation
Modified from Fattibene P, Mazzei F, Nuccetelli C, et al. Prenatal exposure to ionizing radiation: sources, effects, and regulatory aspects. Acta Paediatr. 1999;88:693.
Organogenesis
Exposure to very high-dose radiation, far greater than could be delivered by even aggressive diagnostic radiographs and radionuclide procedures, has been reported to result in teratogenesis. Such information is gleaned from women who were exposed to therapeutic radiation (in the range of 250 rad) during early pregnancy for conditions such as pelvic malignancies. Organ malformations are the main consequence of exposure to radiation during the organogenesis period (3 to 8 weeks). Abnormalities result from killing of cells during the active phase of proliferation and differentiation. Because the embryo is unable to completely replace damaged cells, malformations occur. The most common effects of exposure during organogenesis are malformations in the organs under development at the time of exposure and a reduction in skeletal development. Growth retardation and microcephaly are the predominant effects.10,12,13 These effects have a reported threshold dose range of 5 to 20 rad or higher but are not generally observed unless the exposure is several orders of magnitude or higher.10,12 This dose range is significantly higher than that attained in diagnostic radiology or diagnostic nuclear medicine procedures. Even though ocular abnormalities, developmental facial abnormalities, genital abnormalities, and physical deformities of the extremities have been reported after exposure of the embryo to very high doses, such abnormalities have not been linked to the amount of radiation that would be delivered from even multiple diagnostic radiographic procedures. Importantly, there are no reports of external radiation inducing morphologic malformations in humans unless the offspring also exhibited either growth retardation or a central nervous system (CNS) abnormality. Simply stated, isolated structural abnormalities will not develop in a fetus exposed to radiation. The fear of extra toes, cleft palate, or heart or kidney malformations from exposure to diagnostic radiation during pregnancy is simply unfounded, yet often believed by the general public.
Temporary growth retardation is likely with doses in the range of 10 to 25 rad.13 Infants with low birth weight and length may recover fully and attain normal adult stature. The natural incidence of a live birth having a developmental anomaly is 2% to 4%,9 and the incidence of intrauterine growth retardation is 2% to 3%.9 Again, it is important to emphasize that exposure to less than 5 rad yields no change in the risk for occurrence of organ malformations or growth retardation13 (see Table 72-3).
Fetal Period
Mental Impairment: From the 8th to the 15th week, there is a rapid increase in the number of neurons that migrate to their ultimate sites and lose their capacity to divide. At 15 to 25 weeks, there is more differentiation and architectural definition.9 These embryologic changes make the fetus susceptible to damage to the CNS during the early fetal and midfetal periods.
In utero atomic bomb survivor data indicate that the risk for SMR per rad was higher if exposed during the early fetal versus the midfetal period.13 In children exposed to greater than 50 rad between 8 and 15 weeks after conception, a drop in IQ score of 0.3 point per rad was estimated.13 There is no documented increased risk for mental retardation in humans at a gestational age of less than 8 weeks or greater than 25 weeks when evaluated with doses of less than 50 rad.14 The highest risk for SMR occurs during the early fetal period with fetal doses in the range of 100 rad. All clinical observations on significant reductions in IQ and SMR relate to fetal doses of about 50 rad and higher.10 This dose range greatly exceeds the dosages used for diagnostic imaging.
It is important to relate the magnitude of radiation effects to abnormalities that occur spontaneously in the population. Multiple causes of mental retardation have been identified, including malnutrition, lead poisoning, rubella infection during pregnancy, and maternal alcoholism. Current prevalence figures indicate that the normal incidence of a person having an IQ below 70 is approximately 3%.10 At fetal doses of 10 rad, the spontaneous incidence of mental retardation is much larger than any potential radiation effect on IQ reduction.10 Regardless of the time of gestation, reduction in IQ cannot be clinically identified with fetal doses of less than 10 rad (see Table 72-3).10
Growth Retardation: The human data for Hiroshima and Nagasaki reveal that the major congenital anomaly observed was microencephaly.13 Studies have not demonstrated any increased risk for microencephaly in the population exposed to less than 150 rad in Nagasaki; however, an increased risk in the Hiroshima population exposed to doses as low as 10 to 19 rad has been reported.14 It is possible that the difference between the two cities is secondary to causes (e.g., trauma, stress, malnutrition) other than radiation. In experimental animal data, a dose of 10 to 20 rad did not increase the incidence of microencephaly.15 The dose threshold for microencephaly, as well as other congenital anomalies, is generally accepted to be in the range of a few rad. Permanent growth retardation is not typically seen unless doses exceed 50 rad.13 Irradiation of the human fetus at doses below 10 rad has not been observed to cause congenital malformations or growth retardation (see Table 72-3).2,4,9
Carcinogenesis
The magnitude of risk for carcinogenesis after low-dose radiation exposure and whether the risk changes throughout gestation have been the subject of many publications,16–18 yet interpretation of the data remains open to date. Numerous studies19–22 indicate a 1.3- to 3.0-fold higher incidence of leukemia in children exposed to diagnostic radiation in utero, although some studies fail to substantiate this association.15,23 Excess cancer as a result of in utero exposure has not been clearly demonstrated in Japanese atomic bomb survivor studies even though the population has been monitored for about 50 years, but the number exposed is not large.10 Identification and control of confounding factors make interpretation of radiation carcinogenesis studies difficult, if not impossible to interpret. Brent and coworkers15 noted that most investigators agree that low doses of radiation present a carcinogenic risk to the embryo; however, findings of increased risk for cancer in children exposed in utero to low-dose diagnostic radiation must be reconciled with the fact that high-dose animal and human studies have not found a marked increase in the incidence of cancer.
Risk can be expressed in several ways, including relative risk and absolute risk. In relative risk, the risk is expressed as a function of the “background” risk. For example, a relative risk of 1.0 indicates that there is no effect of irradiation, whereas a relative risk of 1.5 for a given dose indicates that the radiation is associated with a 50% increase in cancer above background rates. The absolute risk estimate simply indicates the excess number of cancer cases expected in a population because of a certain radiation dose.10
The International Commission on Radiological Protection Publication 8410 noted that a recent analysis of many of the epidemiologic studies conducted on prenatal x-ray exposure and childhood cancer are consistent with a relative risk of 1.4 (a 40% increase over the background risk) following a fetal dose of about 1 rad. The best methodologic studies, however, suggest that the risk is probably lower than this. Even if the relative risk were as high as 1.4, the individual probability of childhood cancer after in utero irradiation would be very low (≈0.3% to 0.4%) because the background incidence of childhood cancer is so low (≈0.2% to 0.3%). Absolute risk estimates for cancer from ages 0 to 15 after in utero irradiation have been estimated to be in the range of 600 per 10,000 persons each exposed to 100 rad, or 0.06%/rad.10,12 If a fetus is exposed to 0.1 rad, the increased risk for carcinogenesis is 0.006%, or 3 in 50,000, as compared with the background incidence of 0.2% to 0.3%, or 100 to 150 per 50,000. The increased carcinogenic risk from exposure to 0.1 rad is approximately 50 times smaller than the already low natural incidence of cancer.
Mutagenesis
Investigating possible radiation-induced alterations in the human genome is exceedingly difficult. The geneticists who studied the irradiated populations in Japan are convinced that there were radiation-induced mutations. However, the calculated and confirmed risks were so small that the investigators were unable to demonstrate statistically significant genetic effects.24
The risk for radiation-induced hereditary disease in humans is reported to be around 1% per 100 rad.13,15 If a fetus is exposed to 0.1 rad, the increased risk is approximately 0.001%, or 1 in 100,000. The natural frequency of genetic disease manifesting at birth is approximately 3%,11 or 3000 per 100,000. For 0.1 rad, the increased genetic risk is minute in comparison to the natural incidence of genetic disease.
Radiation Exposure from Diagnostic Radiographs
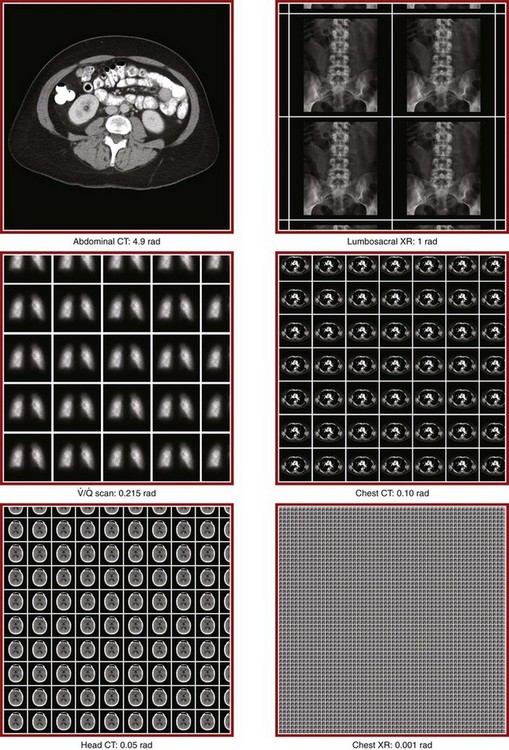
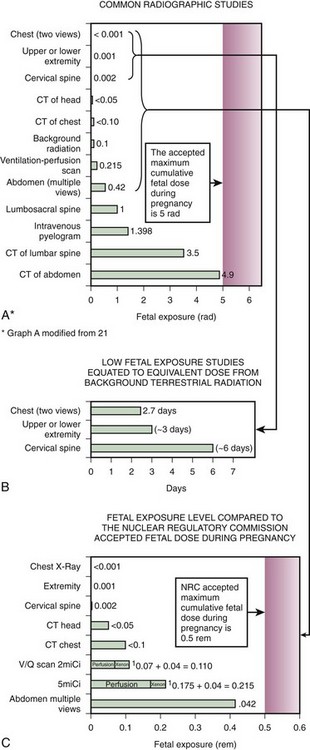
Table 72-4 lists estimated fetal exposure for various diagnostic imaging modalities.25–27 Multiple sources of estimated fetal exposure were reviewed, and the highest reported exposure from these sources is listed. The number of examinations required to reach a cumulative dose of 5 rad is calculated in the second column to underscore the order-of-magnitude difference between the dose considered to have negligible risk (5 rad) and the actual exposed fetal dose. For example, one would require 5000 radiographs of an upper or lower extremity, 12 pelvic radiographs, or more than 5000 two-view chest radiographs before the 5-rad limit is reached. This information is represented graphically in Figure 72-2.
TABLE 72-4
Estimated Fetal Exposure from Various Diagnostic Imaging Methods
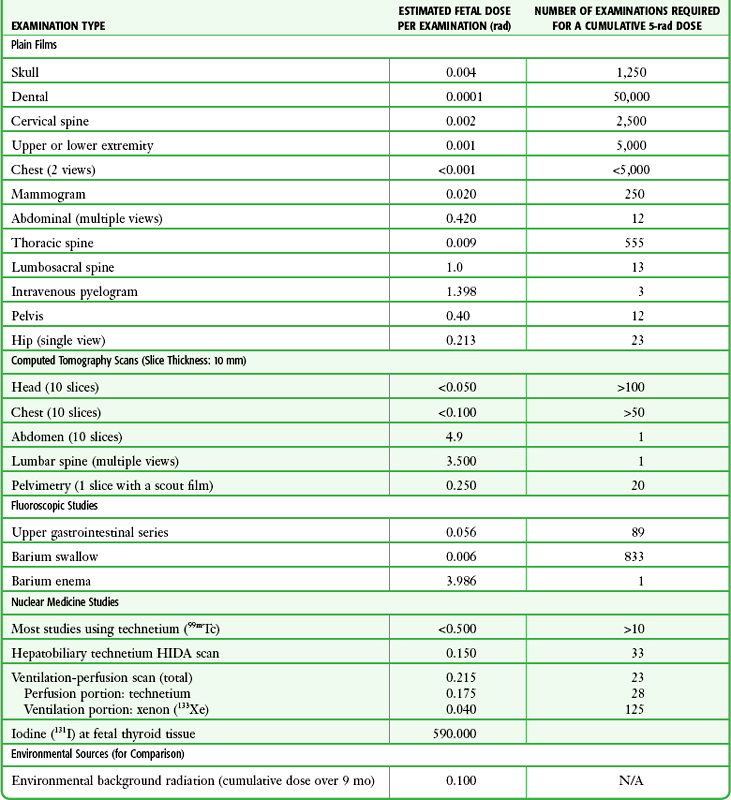
HIDA, hepatobiliary iminodiacetic acid; rad, unit of absorbed radiation.
Reproduced from Toppenberg KS, Hill DA, Miller DP. Safety of radiographic imaging during pregnancy. Am Fam Physician. 1999;59:1813.
Radiation Exposure from CT Scans
Many variables affect calculation of the fetal radiation dose from CT scans, especially slice thickness, number of cuts, distance of the target organ from the fetus, and gestational age. Table 72-4 summarizes the estimated maximal fetal radiation doses from CT scans. It should be noted that CT of the lumbar spine delivers radiation to the fetus that approaches the safe cutoff range. A CT scan of the abdomen exposes the fetus to less radiation than the 5-rad cutoff, but alternative methods of investigation such as US or MRI should be considered in early pregnancy if the clinical condition warrants.
Head CT is the most commonly requested CT scan in pregnancy. The expected fetal absorbed dose is less than 50 millirad (mrad), which is 100 times less than the dose with negligible risk. The estimated radiation dose to the fetus for CT of the chest is less than 0.100 rad. Spiral CT is commonplace in radiology departments and is a popular diagnostic tool used for suspected pulmonary embolism (PE) in pregnant patients. The dose with spiral CT of the chest is less because the duration of the procedure is much shorter.28 Van der Molen29 reported that using 16-slice versus 4-slice CT can equate to a reduction in radiation dose of 20% to 30%.
Ordering CT scans of the head, chest, abdomen, and pelvis is a daily occurrence for emergency medicine clinicians. With that in mind, it is sobering to realize that the seventh National Academy of Science report on the Biological Effects of Ionizing Radiation (BEIR VII) indicated that a 10-rad dose is associated with a lifetime attributable risk for development of a solid cancer or leukemia of 1 in 1000.30,31 As data on the effects of ionized radiation accumulate and the technology of nonionizing techniques improves, our use of ionization-based modalities will diminish.
The American College of Radiology notes that iodinated low-osmolality contrast media (LOCM), most of which are nonionic agents, have been shown to be associated with less discomfort and a lower incidence of minor (1% versus 5% for high-osmolality contrast media [HOCM]) and severe reactions (0.015% versus 0.1% for HOCM). Many radiology departments routinely use LOCM.32 Although authors have expressed concern over the possibility that iodinated contrast media may suppress fetal or neonatal thyroid function for a short period,7 the added benefit of using nonionic contrast agents is that intravascular use of such agents has been reported to have no effect on neonatal thyroid function.33 Postnatal screening for hypothyroidism is done routinely in the United States. The combination of increased use of iodinated contrast agents in pregnant women to rule out PE and the dearth of literature reporting increased fetal hypothyroidism in the United States supports the report that use of iodinated contrast agents does not affect fetal thyroid function.
Nuclear Medicine Studies
A common nuclear medicine procedure ordered from the ED is a ventilation-perfusion ( ) scan. The perfusion portion of the scan is performed by injecting a radioisotope intravenously. The isotope emits radiation and is detected by sensitive cameras. This requires that a radioisotope (e.g., 99Tc) be tagged to a substrate, most commonly albumin. The albumin-technetium aggregate is temporarily trapped in arterioles and capillaries in the lung and its distribution can be identified. The principal photon that is useful for detection and imaging with technetium studies is the γ-ray.34 When the radiotagged substrate is excreted into the maternal bladder, the fetus will receive additional radiation exposure because of the proximity of the maternal bladder. Patient hydration and frequent voiding or bladder catheterization after a
) scan. The perfusion portion of the scan is performed by injecting a radioisotope intravenously. The isotope emits radiation and is detected by sensitive cameras. This requires that a radioisotope (e.g., 99Tc) be tagged to a substrate, most commonly albumin. The albumin-technetium aggregate is temporarily trapped in arterioles and capillaries in the lung and its distribution can be identified. The principal photon that is useful for detection and imaging with technetium studies is the γ-ray.34 When the radiotagged substrate is excreted into the maternal bladder, the fetus will receive additional radiation exposure because of the proximity of the maternal bladder. Patient hydration and frequent voiding or bladder catheterization after a  scan will lessen exposure of the fetus to radiation.
scan will lessen exposure of the fetus to radiation.
Depending on the radioisotope and substrate used, average fetal exposures can be calculated. Commonly used radiopharmaceuticals and estimated fetal doses for  scans and other radionuclide studies are presented in Table 72-5.14 A 5-mCi 99Tc-albumin scan results in 175 mrad of fetal exposure. Reducing the dose to 2 mCi results in 70-mrad fetal exposure. 99Tc-albumin is contraindicated in patients with severe pulmonary hypertension and is pregnancy category C.
scans and other radionuclide studies are presented in Table 72-5.14 A 5-mCi 99Tc-albumin scan results in 175 mrad of fetal exposure. Reducing the dose to 2 mCi results in 70-mrad fetal exposure. 99Tc-albumin is contraindicated in patients with severe pulmonary hypertension and is pregnancy category C.
TABLE 72-5
Radiopharmaceuticals Used in Nuclear Medicine Studies
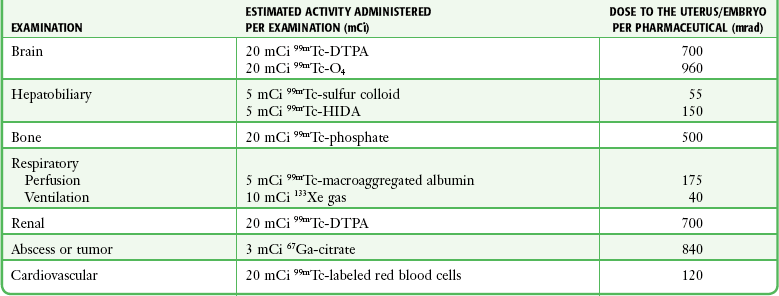
Reproduced from Cunningham GF, ed. Williams Obstetrics. 21st ed. New York: McGraw-Hill; 2001.
Diagnosis of PE
The reported incidence of PE associated with pregnancy is equivalent to roughly 1 in every 2000 pregnancies.7 The mortality rate of untreated acute PE is about 30%, as opposed to 2% to 10% with timely diagnosis and treatment.35 Therefore, the potential morbidity of PE and the attendant risk associated with anticoagulant therapy in pregnant patients necessitate definitive diagnosis.
The radiologic modalities of choice for definitive diagnosis are  scanning versus CT pulmonary angiography. Although conventional pulmonary angiography was long considered the “gold standard” against which other imaging techniques were compared, it is now thought to be no more accurate than well-performed CT pulmonary angiography.7
scanning versus CT pulmonary angiography. Although conventional pulmonary angiography was long considered the “gold standard” against which other imaging techniques were compared, it is now thought to be no more accurate than well-performed CT pulmonary angiography.7
The calculated radiation exposure of the fetus from both  scanning and CT of the chest confers minimal and essentially only theoretical fetal risk.28 Fetal exposure from CT of the chest is less than 0.100 rad. Fetal exposure from CT has been reported to be as low as 0.026 rad with single–detector row helical CT and 0.013 rad for multidetector-row helical CT.7 A 5-mCi 99Tc perfusion scan and a 10-mCi 133Xe ventilation scan summate to 0.225 rad.25 The dose of fetal radiation from the perfusion scan can be altered and is often lowered in the evaluation of pregnant patients (Box 72-1). Lowering the dose by 60%, a level that will usually produce a suitable study, results in lowering fetal exposure to 0.110 rad. Recent articles state that the radiation dose to the fetus from CT angiography of the maternal chest is similar to or lower than that from a
scanning and CT of the chest confers minimal and essentially only theoretical fetal risk.28 Fetal exposure from CT of the chest is less than 0.100 rad. Fetal exposure from CT has been reported to be as low as 0.026 rad with single–detector row helical CT and 0.013 rad for multidetector-row helical CT.7 A 5-mCi 99Tc perfusion scan and a 10-mCi 133Xe ventilation scan summate to 0.225 rad.25 The dose of fetal radiation from the perfusion scan can be altered and is often lowered in the evaluation of pregnant patients (Box 72-1). Lowering the dose by 60%, a level that will usually produce a suitable study, results in lowering fetal exposure to 0.110 rad. Recent articles state that the radiation dose to the fetus from CT angiography of the maternal chest is similar to or lower than that from a  scan.36 Pulmonary angiography results in an estimated fetal exposure of 0.22 to 0.37 rad when done via the femoral route, but it can be lowered to less than 0.05 rad by using the brachial route.28
scan.36 Pulmonary angiography results in an estimated fetal exposure of 0.22 to 0.37 rad when done via the femoral route, but it can be lowered to less than 0.05 rad by using the brachial route.28
CT has supplanted  scanning as the standard diagnostic test in ruling out PE. Because the perfusion scan is being done on a relatively young healthy subset of the population, one would suspect that the percentage of nondiagnostic studies (low or intermediate probability) would be low. However, Chan and colleagues37 reported that
scanning as the standard diagnostic test in ruling out PE. Because the perfusion scan is being done on a relatively young healthy subset of the population, one would suspect that the percentage of nondiagnostic studies (low or intermediate probability) would be low. However, Chan and colleagues37 reported that  scintigraphy is nondiagnostic in 25% of patients, with 73.5% of scans being read as normal and only 1.8% being read as high probability (113 patients in the study). Interestingly, 86% (24 of 28) of the patients who had a nondiagnostic finding did not receive anticoagulant therapy and were found to be free of a thromboembolic event for the following 20.6 months.
scintigraphy is nondiagnostic in 25% of patients, with 73.5% of scans being read as normal and only 1.8% being read as high probability (113 patients in the study). Interestingly, 86% (24 of 28) of the patients who had a nondiagnostic finding did not receive anticoagulant therapy and were found to be free of a thromboembolic event for the following 20.6 months.
Recognizably, the utility of a test that does not answer your question 25% of the time is concerning but should be tempered by the fact that there is a 75% chance of getting a definitive diagnosis, along with published concerns that exposure of childbearing women’s breasts to the higher level of radiation from CT may cause cancer decades later.7,8 Remy-Jardin and Remy38 and Scarsbrook and coworkers7 reported that an exposure of 1 rad to the breasts of a woman aged 35 years increases her risk for breast cancer by approximately 14% over the background rate for the general population. Some authors39 advocate that the breast radiation issue justifies the use of  scanning rather than CT angiography as the primary examination in a pregnant patient.
scanning rather than CT angiography as the primary examination in a pregnant patient.
So which study does one order? Both modalities expose a fetus to low levels of radiation of similar magnitude (CT less than  ) with very low theoretical fetal risk. The advantages of CT pulmonary angiography include the speed with which one can obtain the study and the capability of delineating alternative causes of the symptoms. Scarsbrook and coworkers7 presented an algorithm mindful of the radiation exposure to both the fetus and mother and provided convincing evidence for their recommendation (Fig. 72-3). They suggested that an echocardiogram is a good first step in critically ill pregnant patients in whom PE is being considered. All others should start with a chest radiograph with shielding of the fetus. If findings on the radiograph are normal, proceed with US of the lower extremities to evaluate for deep venous thrombosis. Although the combination may have lower diagnostic yield, it exposes the mother and fetus to minimal risk. If deep venous thrombosis is present, treatment can be instituted. If US is negative, proceed to a half-dose lung perfusion scan if the patient does not have a history of obstructive lung disease. The literature reports that findings in up to 75% of these scans are normal in the pregnant population. An important stipulation for using this algorithm is that one’s hospital radiology team should have experience in reporting normal scans as opposed to low-probability ones, with the understanding that all nondiagnostic tests would lead to consideration of CT pulmonary angiography. The authors note that using this algorithm allows a definitive diagnosis in the vast majority of cases while minimizing risk to both the mother and fetus.
) with very low theoretical fetal risk. The advantages of CT pulmonary angiography include the speed with which one can obtain the study and the capability of delineating alternative causes of the symptoms. Scarsbrook and coworkers7 presented an algorithm mindful of the radiation exposure to both the fetus and mother and provided convincing evidence for their recommendation (Fig. 72-3). They suggested that an echocardiogram is a good first step in critically ill pregnant patients in whom PE is being considered. All others should start with a chest radiograph with shielding of the fetus. If findings on the radiograph are normal, proceed with US of the lower extremities to evaluate for deep venous thrombosis. Although the combination may have lower diagnostic yield, it exposes the mother and fetus to minimal risk. If deep venous thrombosis is present, treatment can be instituted. If US is negative, proceed to a half-dose lung perfusion scan if the patient does not have a history of obstructive lung disease. The literature reports that findings in up to 75% of these scans are normal in the pregnant population. An important stipulation for using this algorithm is that one’s hospital radiology team should have experience in reporting normal scans as opposed to low-probability ones, with the understanding that all nondiagnostic tests would lead to consideration of CT pulmonary angiography. The authors note that using this algorithm allows a definitive diagnosis in the vast majority of cases while minimizing risk to both the mother and fetus.
Scarsbrook and coworkers7 recommended several dose reduction methods when using CT pulmonary angiography on pregnant patients. Although these methods do not fall into the realm of emergency medicine, it is worthwhile to raise these points with radiologists when developing a protocol to lower the radiation exposure to your patients (Box 72-2).
The role of D-dimer levels in the diagnosis of PE is evolving.40,41 During pregnancy D-dimer levels increase, and such increases should be considered physiologic. D-dimer levels are similar to those in nonpregnant patients up to around 20 weeks and then are noted to increase throughout pregnancy to three times higher than the mean in a healthy nonpregnant patient.42
Recently, attempts have been made to establish a range of normal D-dimer values throughout pregnancy, which may be of great value, but as of yet have not been tested in clinical practice.7
Diagnosis of Appendicitis
Acute appendicitis is the most common nonobstetric emergency requiring surgery during pregnancy. Appendicitis is associated with premature labor, fetal morbidity and mortality, and an increased rate of perforation. Concern for appendicitis in a pregnant patient warrants early surgical consultation and discussion of the need and type of imaging. Patel and coauthors36 published an algorithm that uses US and MRI techniques before exposing patients to ionizing radiation. They recommended the use of graded-compression US followed by abdominal/pelvic US to search for other pathology if needed. If the US studies are negative, the authors recommend MRI of the abdomen and pelvis (Fig. 72-4). Notably, some authors43 have found that using a nonionic oral contrast agent (a mixture of ferumoxsil [category B] and barium sulfate) improved sensitivity and specificity in detecting appendicitis in pregnancy. The authors noted that US imaging of the appendix was more easily done during the first and early second trimester and that the left lateral decubitus position assisted in visualization of the appendix in third-trimester patients. Finally, if US and MRI are still inconclusive, CT of the abdomen and pelvis may be considered. Definitive surgical exploration should be discussed with a general surgeon before proceeding to ionizing radiation. If CT is required, the authors reported an estimate of about one cancer per 500 fetuses exposed to 3 rad.
Diagnosis of Pregnancy and Consent
If exposure to less than 5 rad does not measurably affect the exposed embryo, why should the clinician determine the pregnancy status of the patient? Brent2 reported sound reasoning for diagnosing pregnancy before a radiographic study. The principle of informed consent must remain paramount. It is beneficial and ethically more sound to have the patient informed of her pregnancy status before imaging. An informative discussion about the risk-benefit aspects of the test before the study conveys concern for the patient and fetus. Discussing the risk-benefit aspects of imaging after the study may be misconstrued as “backpedaling” and make the patient upset. Many lawsuits are stimulated by the factor of surprise. Frank discussion before imaging may prevent misguided litigation. More importantly, having patients both understand the problem (imaging in pregnancy) and take part in the management discussion can help them become more empowered and potentially reduce the anxiety associated with their condition and with their pregnancy.
Patient Counseling
When a pregnant patient requires an imaging study, be prepared to discuss the risk associated with the test. Counseling can be done after attempting to estimate the dose received by the conceptus from the procedure and comparing the radiation risk with other risks of pregnancy. It is important to use terminology that is easily understood by the patient. Figure 72-5 depicts three different strategies to inform the patient about the level of exposure from her study and established limits. Table 72-6 compares the level of exposure with established background risks.
TABLE 72-6
Probability of Bearing Healthy Children as a Function of Radiation Dose
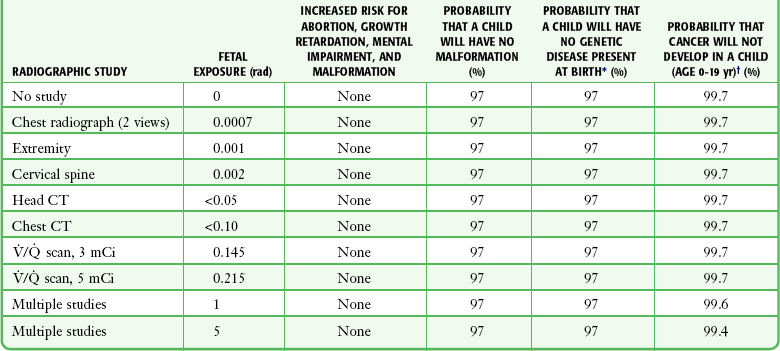
*Rounded values. The radiation risk for genetic mutation is assumed to be 0.01%/rad fetal dose with a linear dose-response relationship. The background rate for genetic mutation is estimated to be 3%. From Osie IK. Fetal doses from radiological examinations. Br J Radiol. 1999;72:773.
†Rounded values. The radiation risk for fatal cancer is assumed to be 0.06%/rad fetal dose with a linear dose-response relationship. Many epidemiologic studies suggest that the risk may be lower than that assumed here. The background risk for childhood cancer is calculated from NCI-SEER. Surveillance, Epidemiology and End Results Cancer Statistics Review 1973-1991: Tables and Graphs. Bethesda, MD: National Cancer Institute; 1994.
Modified from International Commission on Radiological Protection. Publication 84: Pregnancy and medical radiation. Ann ICRP. 2000;30:iii, 1.
The main bar graph (A) in Figure 72-5 compares the fetal exposure level for various radiographic studies with the maximum accepted fetal dose during pregnancy (5 rad). A patient’s particular study may be plotted on this graph to show the clear margin of safety that exists for all single diagnostic tests.
The middle graph (B) equates the exposure from low-level diagnostic studies to the number of hours needed to accumulate a similar exposure dose from background terrestrial radiation. One of the most commonly ordered studies in pregnancy is a chest radiograph. The potential risk to the fetus can be put into perspective for the patient by comparing the absorbed dose for the chest radiograph with the natural background radiation exposure. The environmental background radiation over a 9-month period results in a cumulative dose of 100 mrad,44 or 0.015 mrad/hr. The fetal dose exposure for a chest radiograph (two views) is estimated to be less than 1 mrad. Therefore, the exposure dose to the fetus from a chest radiograph is equivalent to the same amount of naturally occurring background radiation to which the patient was exposed in the previous 2.7 days.
The lower graph (C) depicts the upper limit of the Nuclear Regulatory Commission (NRC) for cumulative gestational dose versus various diagnostic studies. The NRC has established occupational radiation dose limits for pregnancy. Its recommendation is that the dose to the fetus not be allowed to exceed 0.5 rem during gestation. Brent2 noted that this factor-of-10 lowering of the widely accepted threshold is “extremely conservative.” One can explain to the patient that the level of exposure from her radiograph is below the conservative cumulative acceptable dose for a pregnant employee at a nuclear facility in the United States.
Another useful approach is to indicate to the patient the probability of not having a child with either a malformation or cancer and how that probability is affected by radiation. Table 72-6 depicts the probability of bearing healthy children as a function of radiation dose. This discussion should be coupled with the fact that a nonexposed fetus has a baseline incidence of spontaneous abortion, multiple developmental abnormalities, and subsequent childhood cancer.
Numerous organizations have declared fetal exposure to less than 5 rad as being safe. Box 72-3 presents various conclusions from key organizations on the use of radiation and pregnancy. The International Commission on Radiological Protection concluded that fetal doses below 10 rad should not be considered a reason for terminating a pregnancy.10 If a patient still has considerable concern or has possibly received greater than 5 rad, referral to a radiation physicist or genetic specialist for further counseling is reasonable.
Nonionizing Radiation: MRI and US
MRI
MRI is currently not approved by the U.S. Food and Drug Administration (FDA) for use in pregnant patients.45 However, a body of data in this population is developing. MRI is becoming a valuable complement to US when additional information is needed to make treatment decisions during pregnancy (see Fig. 72-4).46,47 Recent advances in fast MRI techniques have helped eliminate previous obstacles of slow imaging times and fetal movement. Possible indications for the use of MRI in a pregnant patient include further evaluation for adnexal masses, placental status, hydronephrosis, pelvic vein thrombosis, appendicitis, and small bowel obstruction.48
Magnetic resonance direct thrombus imaging (MR-DTI) is a technique that allows direct visualization of PE and simultaneous imaging of the legs without the need for intravenous contrast media. Early data suggest that it is highly accurate in the detection of PE.7 As more studies are conducted and the availability of MRI improves, MRI may replace ionizing techniques for the diagnosis of thromboembolism.
The Safety Committee of the Society for Magnetic Resonance Imaging has stated that MRI procedures are indicated for use in pregnant women when other nonionizing diagnostic imaging methods are inadequate or when the examination will provide important information that would otherwise require exposure to ionizing radiation.49 It is required that pregnant patients be informed that although to date there is no indication that the use of clinical MRI procedures during pregnancy produces deleterious effects, according to the FDA the safety of MRI procedures during pregnancy has not been definitively proved. It is advisable to obtain informed consent for MRI of a pregnant patient. In addition, because of limited data, most facilities avoid imaging patients in their first trimester. With inadvertent exposure in a wanted pregnancy, however, the present accumulated data would not warrant interruption of the pregnancy (Box 72-4).
Generally during pregnancy, non–contrast-enhanced MRI is performed. Fortunately, most maternal pelvic and fetal MRI does not require contrast media. Although no direct adverse effects on the fetus have been documented, gadolinium-based contrast material is not recommended for use in pregnant patients.48,50 Gadolinium-based contrast material has been shown to cross the placenta and appear within the fetal bladder moments after intravenous administration.51 It is then excreted into amniotic fluid and potentially reabsorbed from the gastrointestinal tract.51 Because it is reabsorbed in the fetal gastrointestinal tract, the half-life of gadolinium-based contrast material in the fetal circulation is not known. Gadolinium is a class C drug.
US
US continues to be the screening modality of choice for evaluation of the maternal pelvis and the fetus because of its safety profile, relatively low cost, and real-time capability. Obstetric and gynecologic US accounts for more than half of the US imaging volume in the United States.52 In the 40 years since its introduction into clinical practice, US has not been shown to convey any significant health risk to the fetus or mother,53 although most safety data were collected before 1992, when the permissible power output of scanners was significantly lower than the power used in contemporary scanners.54 Generally, the increasing power output raises concern for thermal and mechanical effects on developing tissue. These issues are small with standard B-mode imaging and more concerning with use of the Doppler modality. US societies have developed unitless output display standards, namely, a thermal index and mechanical index, to allow the operator to determine whether the study exceeds a generally accepted safe range.55 The radiologic principle known as ALARA is generally supported and promotes a balance between obtaining the necessary medical information while using minimal settings and examination time. Human data accumulated over a 25-year period have revealed no consistent adverse effects from prenatal diagnostic US examination.56,57 US in pregnancy is considered a safe procedure.
The American College of Obstetricians and Gynecologists has reviewed the effects of radiography, US, and MRI during pregnancy and suggested guidelines for radiographic examination during pregnancy (Box 72-5).6
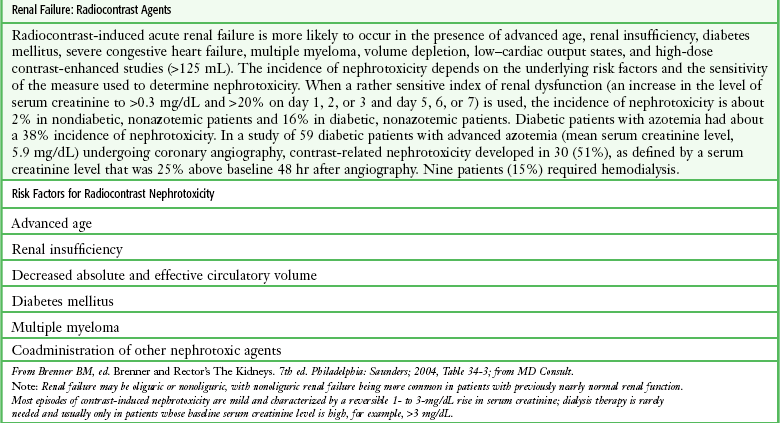
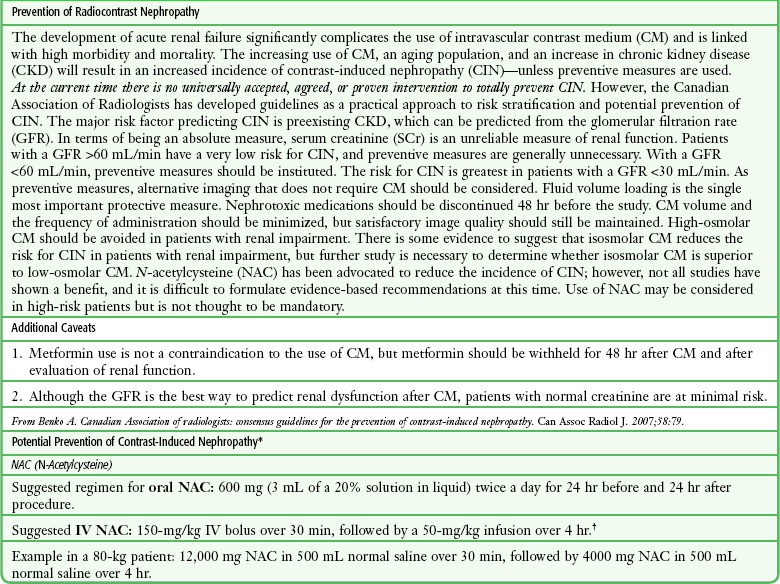
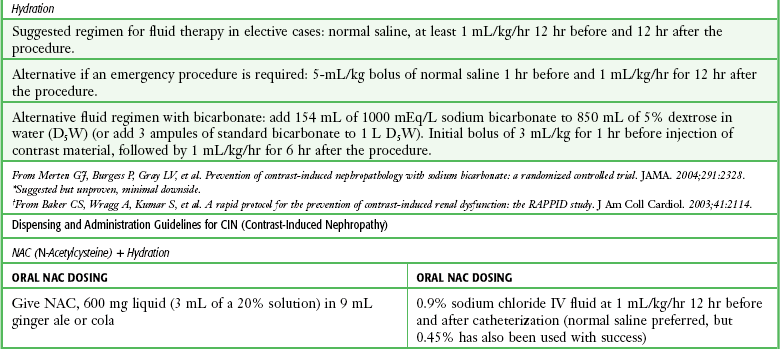
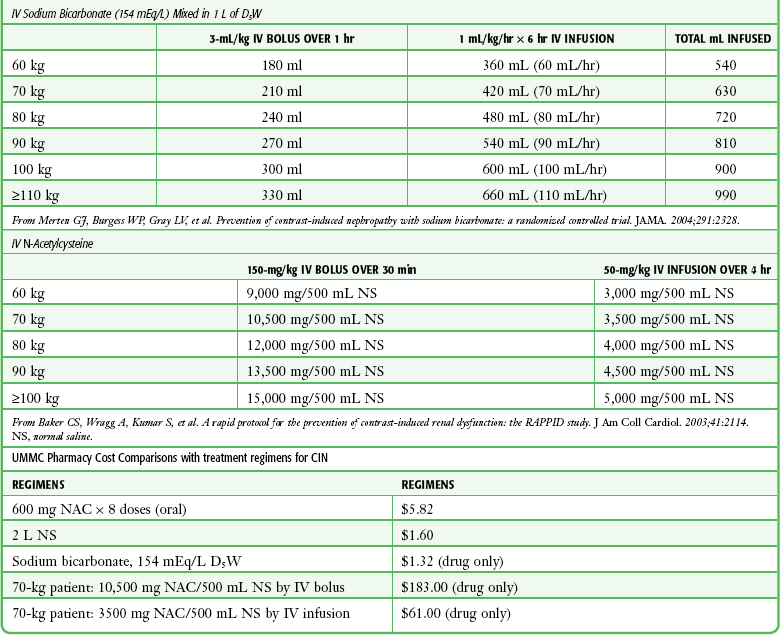
Clinical Use of Radiocontrast Material
Emergency clinicians must frequently initiate studies with the use of radiocontrast material. A full discussion of these procedures is not within the scope of this chapter, but basic issues of contrast material–induced nephropathy, the possible prevention thereof, and recent concern over the use of gadolinium for MRI studies have been included for completeness and ready reference (Table 72-7 and Box 72-6).
References
1. Issue 47, August 24. The Joint Commission Sentinel Event Alert. Radiation risks of diagnostic imaging, 2011.
2. Brent, RL. The effect of embryonic and fetal exposure to x-ray, microwaves, and ultrasound: counseling the pregnant and nonpregnant patient about these risks. Semin Oncol. 1989;16:347.
3. Bentur, Y, Horlatsch, N, Kiren, G. Exposure to ionizing radiation during pregnancy: perception of teratogenic risk and outcome. Teratology. 1991;43:109.
4. American College of Obstetricians and Gynecologists (ACOG). Committee on Obstetric Practice: Guidelines for Diagnostic Imaging During Pregnancy (ACOG Committee Opinion No. 158). Washington, DC: ACOG; 1995.
5. Gray, JE. Safety (Risk) of Diagnostic Radiology Exposure. Radiation Risk: A Primer. Reston, VA: American College of Radiology; 1996.
6. American College of Obstetricians and Gynecologists (ACOG). Committee on Obstetric Practice: Guidelines for Diagnostic Imaging During Pregnancy (ACOG Committee Opinion No. 299). Washington, DC: ACOG; 2004.
7. Scarsbrook, AF, Evans, AL, Owen, AR, et al. Diagnosis of suspected venous thromboembolic disease in pregnancy. Clin Radiol. 2006;61:1.
8. Cook, JV, Kyriou, J. Radiation from CT and perfusion scanning in pregnancy. BMJ. 2005;331:6.
9. Mettler FA, Jr., Upton A, eds. Medical Effects of Ionizing Radiation, 2nd ed, Philadelphia: Saunders, 1995.
10. International Commission on Radiological Protection. Pregnancy and medical radiation. Ann ICRP. 2000;30(iii):1.
11. Osie, IK. Fetal doses from radiological examinations. Br J Radiol. 1999;72:773.
12. Fattibene, P, Mazzei, F, Nuccetelli, C, et al. Prenatal exposure to ionizing radiation: sources, effects and regulatory aspects. Acta Paediatr. 1999;88:693.
13. Greskovich, JF, Jr., Macklis, RM. Radiation therapy in pregnancy: risk calculation and risk minimization. Semin Oncol. 2000;27:633.
14. , Williams Obstetrics. Cunningham, FG. 20th ed, New York, McGraw-Hill, 1997:1053.
15. Ionizing and nonionizing radiations. In: Brent R, Meistrich M, Paul M, eds. Occupation and Environmental Reproductive Hazards: A Guide for Clinicians. Baltimore: Williams & Wilkins; 1993:165.
16. Stewart, A, Webb, D, Hewitt, D. A survey of childhood malignancies. BMJ. 1958;1:1495.
17. Kneale, GW, Stewart, AM. Prenatal x-rays and cancers: further tests of data from the Oxford survey of childhood cancers. Health Phys. 1986;51:369.
18. Gilman, EA, Kneale, GW, Knox, EG, et al. Pregnancy x-rays and childhood cancers: effects of exposure age and radiation dose. J Radiol Prot. 1988;8:3.
19. Lilienfield, AM. Epidemiological studies of the leukemogenic effects of radiation. Yale J Biol Med. 1966;39:143.
20. Diamond, EL, Schmerler, H, Lilienfield, AM. The relationship of intrauterine radiation to subsequent mortality and development of leukemia in children: a prospective study. Am J Epidemiol. 1973;97:283.
21. Monson, RR, MacMahon, B. Prenatal x-ray exposure and cancer in children. In: Boice JD, Jr., Fraumeni JF, Jr., eds. Radiation Carcinogenesis: Epidemiology and Biological Significance. New York: Raven; 1984:97.
22. Harvey, EB, Boice, JD, Jr., Honeyman, M, et al. Prenatal x-ray exposure and childhood cancer in twins. N Engl J Med. 1985;312:541.
23. Tabuchi, A. Fetal disorders due to ionizing radiation. Hiroshima J Med Sci. 1964;13:125.
24. Brent, RL. Utilization of developmental basic science principles: the evaluation of reproductive risks from pre- and postconception environmental radiation exposures. Teratology. 1999;59:182.
25. Toppenberg, KS, Hill, DA, Miller, DP. Safety of radiographic imaging during pregnancy. Am Fam Physician. 1999;59:1813.
26. Brent, R. The pulmonologist’s role in caring for pregnant women with regard to the reproductive risks of diagnostic radiological studies or radiation therapy. Clin Chest Med. 2011;32:33–42.
27. Jain, VD, Chelmow, D. Psychosocial and environmental pregnancy risks. Available at http://emedicine.medscape.com/article/259346-overview#aw2aab6b3.
28. Sellman, JS, Holman, RL. Thromboembolism during pregnancy: risks, challenges, and recommendations. Postgrad Med. 2000;108:71.
29. Van der Molen AJ. Considerable reductions in radiation exposure possible with 16-MDCT scanner on body applications. Presented at an American Roentgen Ray Society meeting, Miami, May 2004.
30. Grammaticos, P, Fountos, G. The physician should benefit, not harm the patient. Hell J Nucl Med. 2006;9:82.
31. Committee to Assess the Health Risks from Exposure to Low Levels of Ionizing Radiation. BEIR VII: Health Risks from Exposure to Low Levels of Ionizing Radiation. Available at http://www.nap.edu/reportbreif/11340/11340rb2005.
32. Manual on Contrast Media. Version 5.0. American College of Radiology; 2004.
33. Bona, G, Zaffaroni, M, Defilippi, C, et al. Effects of iopamidol on neonatal thyroid function. Eur J Radiol. 1992;12:22–25.
34. Mallinckrodt. Product insert for TechneScan MAA Kit for the preparation of technetium Tc 99m albumin aggregated, 093 (Form No. A09310). St. Louis: Mallinckrodt; 2000.
35. Nikolaou, K, Thieme, S, Sommer, W, et al. Diagnosing pulmonary embolism: new computed tomography applications. J Thorac Imaging. 2010;25:151–160.
36. Patel, SJ, Reede, DL, Katz, DS, et al. Imaging the pregnant patient for nonobstetric conditions: algorithms and radiation dose considerations. Radiographics. 2007;27:1705–1722.
37. Chan, WS, Ray, JG, Murray, S, et al. Suspected pulmonary embolism in pregnancy: clinical presentation, results of lung scanning, and subsequent maternal and pediatric outcomes. Arch Intern Med. 2002;162:1170.
38. Remy-Jardin, M, Remy, J. Spiral CT angiograph of the pulmonary circulation. Radiology. 1999;212:615.
39. Freeman, LM, Stein, EG, Sprayregen, S, et al. The current and continuing important role of ventilation-perfusion scintigraphy in evaluating patient with suspected pulmonary embolism. Semin Nucl Med. 2008;38:432–440.
40. Tardy, B, Tardy-Poncet, B, Viallon, A, et al. Evaluation of d-dimer ELISA test in elderly patients with suspected pulmonary embolism. Thromb Haemost. 1998;79:38.
41. Perrier, A, Desmarais, A, Goehring, C, et al. d-Dimer testing for suspected pulmonary embolism in outpatients. Am J Respir Crit Care Med. 1997;156:492.
42. Francalanci, I, Comeglio, P, Liotta, AA, et al. d-Dimer concentrations during normal pregnancy, as measured by ELISA. Thromb Res. 1995;78:399.
43. Pedrosa, I, Levine, D, Eyvazzadeh, A, et al. MR imaging evaluation of acute appendicitis in pregnancy. Radiology. 2006;238:891–899.
44. Deluca, SA, Castronovo, FP, Jr. Radiation exposure in diagnostic studies. Am Fam Physician. 1987;36:101.
45. U.S. Food and Drug Administration. Guidance for Content and Review of a Magnetic Resonance Diagnostic Device 510(k) Application. Washington, DC: U.S. Food and Drug Administration; 1988.
46. Curtis, M, Hopkins, MP, Zarlingo, T, et al. Magnetic resonance imaging to avoid laparotomy in pregnancy. Obstet Gynecol. 1993;82:833.
47. Kier, R, McCarthy, SM, Scoutt, LM, et al. Pelvic masses in pregnancy: MR imaging. Radiology. 1990;176:709.
48. Levine, D, Barnes, PD, Edelman, RR. Obstetric MR imaging. Radiology. 1999;211:609.
49. Shellock, FG, Kanal, E. Policies, guidelines, and recommendations for MR imaging safety and patient management: SMRI safety committee. J Magn Reson Imaging. 1991;1:97.
50. Levine, D. Obstetric MRI. J Magn Reson Imaging. 2006;24:1–15.
51. Shellock, FG, Kanal, E. Bioeffects and safety of MR procedures. In Edelman RR, Hesselink JR, Zlatkin MB, eds.: Clinical Magnetic Resonance Imaging, 2nd ed, Philadelphia: Saunders, 1996.
52. Johnson, JL, Abernathy, DL. Diagnostic imaging procedure volume in the United States. Radiology. 1983;146:851.
53. Miller, DL. Safety assurance in obstetrical ultrasound. Semin Ultrasound CT MR. 2008;28:156–164.
54. Miller, MW, Brayman, AA, Abramowicz, JS. Obstetric ultrasonography: a biophysical consideration of patient safety—the “rules” have changed. Am J Obstet Gynecol. 1998;179:241–254.
55. Houston, LE, Odibo, AO, Macones, GA. The safety of obstetrical ultrasound: a review. Prenat Diagn. 2009;29:1204–1212.
56. Reece, EA, Assimakapoulos, E, Xue-Zhong, Z, et al. The safety of obstetric ultrasonography: concern for the fetus. Obstet Gynecol. 1990;76:139.
57. Ziskin, MC, Petitti, DB. Epidemiology of human exposure to ultrasound: a critical review. Ultrasound Med Biol. 1988;14:91.


 scan is 1 to 5 mCi of 99Tc. Reduced doses, as low as 1 mCi, are often used in pregnancy.
scan is 1 to 5 mCi of 99Tc. Reduced doses, as low as 1 mCi, are often used in pregnancy. scan. 133Xe has a short half-life and results in 40-mrad fetal exposure. Normal findings on the perfusion scan may obviate the need for the ventilation scan, and some centers routinely perform only the perfusion portion because most pregnant women have normal ventilation.
scan. 133Xe has a short half-life and results in 40-mrad fetal exposure. Normal findings on the perfusion scan may obviate the need for the ventilation scan, and some centers routinely perform only the perfusion portion because most pregnant women have normal ventilation. ) Scanning
) Scanning scan in pregnancy to limit the total radiation exposure.
scan in pregnancy to limit the total radiation exposure. scan.
scan. scan is 0.04 rad.
scan is 0.04 rad. ventilation-perfusion.
ventilation-perfusion.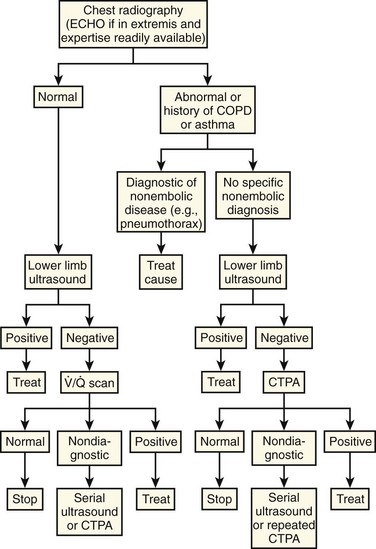
 scan, ventilation-perfusion scan.
scan, ventilation-perfusion scan. 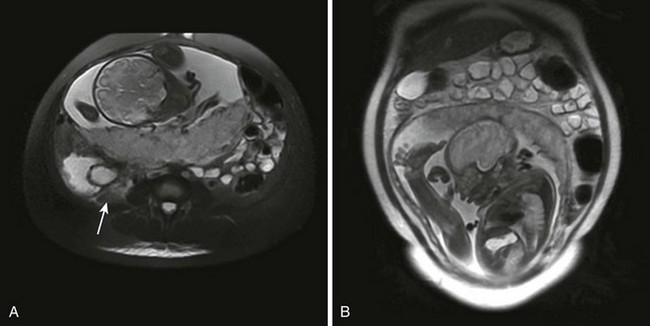
 scan, ventilation-perfusion scan.
scan, ventilation-perfusion scan.