6
Psoriasis
Key Points
• Affects up to 2% of the population.
• Koebner phenomenon – elicitation of psoriatic lesions by traumatizing the skin.
– Scalp.
– Nails, hands, feet, trunk (intergluteal fold).
– Most commonly – well-demarcated, erythematous plaques with silvery scale (Fig. 6.1).

Fig. 6.1 Psoriatic plaques. Note the sharp demarcation and silvery scale. Courtesy Julie V. Schaffer, MD.
– Other lesions include sterile pustules, glistening plaques in intertriginous zones.
– Regular acanthosis, confluent parakeratosis with neutrophils, hypogranulosis, dilated blood vessels (see Chapter 1).
• Major systemic association is psoriatic arthritis (see Table 6.1), most commonly presenting as asymmetric oligoarthritis of hands/feet; the metabolic syndrome is also common.
– Genes that have been associated with psoriasis include those encoding caspase recruitment domain family member 14 (CARD14, a regulator of NF-κB signaling) and, for generalized pustular psoriasis, the IL-36 receptor antagonist (a regulator of IL-8 production and IL-1β responses).
Variants
Chronic Plaque Psoriasis
• Typical lesion – well-demarcated, erythematous plaque with silvery scale.
• Often symmetrical lesions on the elbows and knees; additional sites include the scalp, presacrum, hands, feet, intergluteal fold, and umbilicus (Figs. 6.2–6.4).



Fig. 6.3 Palmoplantar psoriasis. Erythematous scaling plaques of the palmar (A) and plantar surfaces (B). Occasionally, there is well-demarcated hyperkeratosis with minimal erythema (C). A, Courtesy, Peter C. M. van de Kerkhof, MD.

Fig. 6.4 Psoriasis of the genitalia. Erythematous plaques with scale on the penis and scrotum. Courtesy, Peter C. M. van de Kerkhof, MD.
Guttate Psoriasis
• Typical lesion – small papule or plaque (3 mm to 1.5 cm) with adherent scale (Fig. 6.6).


Fig. 6.6 Guttate psoriasis. A Small discrete papules and plaques of guttate psoriasis in an adolescent; note the Koebner phenomenon. B Numerous papules due to the Koebner phenomenon after a sunburn. B, Courtesy Ronald P. Rapini, MD.
• Often preceded by an upper respiratory tract infection.
• In children, may have spontaneous remission but often responds well to UVB phototherapy.
• DDx: pityriasis rosea, syphilis, id reaction to tinea pedis, and small plaque parapsoriasis.
Linear Psoriasis
Erythrodermic Psoriasis
• Generalized erythema of the skin, with areas of scaling.
• Nail changes, facial sparing, and a history of typical plaque-type psoriasis may be helpful clues.
• May be seen after abrupt tapering of medications, especially CS.
• DDx: other causes of erythroderma, e.g., pityriasis rubra pilaris, generalized atopic dermatitis, Sézary syndrome (see Table 8.2).
Pustular Psoriasis
• Generalized pustular psoriasis (von Zumbusch pattern).
– Erythema and sterile pustules arising within erythematous, painful skin; lakes of pus characteristic (Fig. 6.7).

Fig. 6.7 Pustular psoriasis. Large areas of erythema with numerous pustules. Confluence of pustules creates lakes of pus. Courtesy, Julie V. Schaffer, MD.
– DDx: acute generalized exanthematous pustulosis (AGEP; pustular drug reaction) (see Chapter 17).
– Sterile pustules on palms/soles (Fig. 6.8).

Fig. 6.8 Pustulosis of the palms and soles. Multiple sterile pustules are admixed with yellow-brown macules on the palm.
– May have no evidence of psoriasis elsewhere.
– Triggering factors – infections, stress.
– May be aggravated by smoking.
– Associated with inflammatory bone lesions (see Chapter 21).
– DDx: includes Sneddon–Wilkinson disease (see below).


Fig. 6.9 Annular pustular psoriasis. Multiple annular inflammatory plaques studded with pustules. As the lesions enlarge, there can be central clearing, dry desquamation (A), and/or moist desquamation that resembles wet cigarette paper (B). B, Courtesy, Peter C. M. van de Kerkhof, MD.
– Significant overlap with AGEP.
• Localized pattern – within plaques, often due to irritants (Fig. 6.10).

Fig. 6.10 ‘Localized’ pattern of pustular psoriasis. The pustules are limited to preexisting plaques of psoriasis.
• Acrodermatitis continua (of Hallopeau).
– Erythema and scale of distal digit with pustules (Fig. 6.11).
Special Sites
Scalp
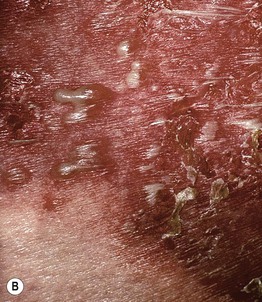
Flexural (Inverse Psoriasis)
• Shiny, pink, well-demarcated thin plaques with minimal scale (Fig. 6.12).

Fig. 6.12 Inverse psoriasis. Shiny erythematous plaques in the axilla that lack scale. Courtesy, Ronald P. Rapini, MD.
• Additional DDx: seborrheic dermatitis, candidiasis, tinea cruris, erythrasma, granular parakeratosis (see Fig. 13.4).
Oral
Nail (See Chapter 58)
• Fingernails > toenails (Fig. 6.13).

Fig. 6.13 Nail psoriasis. Changes include distal onycholysis, pitting, and ‘oil spot’ (salmon patch) phenomenon.
• Associated with psoriatic arthritis.
• Findings include nail pitting, oil spots (salmon patch), onycholysis with proximal red rim, splinter hemorrhages, subungual debris.
Sneddon–Wilkinson Disease (Subcorneal Pustular Dermatosis)
• Often begins in body folds or major intertriginous zones.
• Lesions are annular with superficial pustules on the border.
• Two schools of thought – this disease is (1) a variant of psoriasis vs. (2) a separate entity (Fig. 6.14).
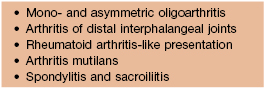
Psoriatic Arthritis (See Table 6.1)
• Seen in 5–30% of patients with cutaneous psoriasis.
• Most commonly is an asymmetric oligoarthritis affecting the distal interphalangeal joints (Fig. 6.15).

Fig. 6.15 Psoriatic arthritis. Asymmetric involvement of the distal interphalangeal (DIP) and proximal interphalangeal (PIP) joints. A ‘sausage’ digit (third digit bilaterally) results from involvement of both the DIP and PIP joints.
• More rarely, but classically, is arthritis of all the interphalangeal joints.
• Occasionally, presentation is rheumatoid arthritis-like, affecting small- and medium-sized joints symmetrically.
• DDx: reactive arthritis (previously referred to as Reiter’s disease).
– Urethritis, arthritis, ocular findings (e.g., conjunctivitis), and oral ulcers in addition to psoriasiform lesions, especially on the soles (keratoderma blennorrhagicum) or genitalia (balanitis circinata) (Fig. 6.16).



Fig. 6.16 Reactive arthritis (formerly Reiter’s disease). A, B Plantar lesions of keratoderma blennorrhagicum. C Papulosquamous lesions of balanitis circinata on the penis. B, Courtesy, Eugene Mirrer, MD.
– Strongly associated with HLA-B27.
– Course is often self-limited.
Treatment
Table 6.2
Indications and contraindications for topical corticosteroids.
Maximal quantities: 50 g/week of a superpotent corticosteroid; 100 g/week of a potent corticosteroid.
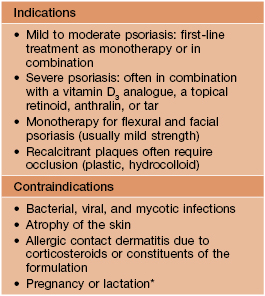
* Relative; can consider limited use of mild- to moderate-strength corticosteroids.
Courtesy, Peter C. M. van de Kerkhof, MD.
• Vitamin D3 analogues (calcipotriene, calcitriol) (Table 6.3).
Table 6.3
Indications and contraindications for vitamin D3 analogues.
If used in conjunction with phototherapy, vitamin D3 preparations need to be applied after UV irradiation or at least several hours prior, because they may reduce UV penetration into the skin.
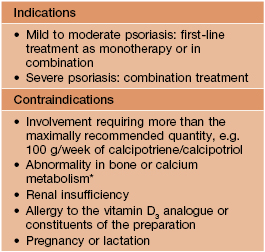
* For example, sarcoidosis and bone metastases.
Courtesy, Peter C. M. van de Kerkhof, MD.
• Calcineurin inhibitors (may be first-line for sensitive areas such as the face or flexures).
• Tars (e.g. liquor carbonis detergens [LCD] 5%).
• Phototherapy and systemic agents.
• Phototherapy – UVB (narrowband or broadband > PUVA) (Table 6.4); if thick keratotic plaques, can combine with oral retinoids.
Table 6.4
Indications and contraindications for phototherapy.
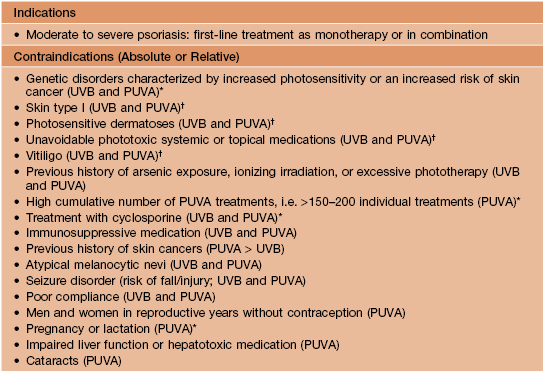
* Absolute contraindication.
† Need to adjust the dose and monitor closely.
PUVA, psoralen + ultraviolet A; UVB, ultraviolet B.
Courtesy, Peter C. M. van de Kerkhof, MD.
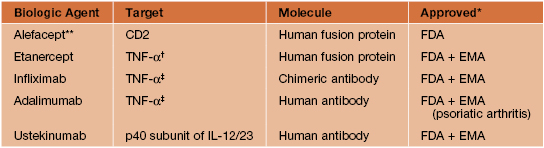
• Methotrexate (oral or intramuscular, occasionally subcutaneous) (Table 6.5).
Table 6.5
Indications and contraindications for methotrexate (MTX).
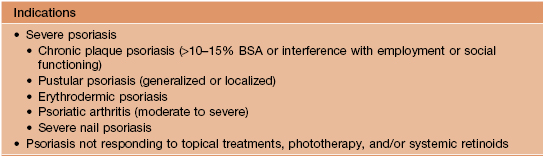
* Absolute contraindication.
† Requires significant reduction in dosage.
‡ Because of possible mutagenic risk and teratogenicity, discontinue MTX 3 months prior to attempts to conceive; continue contraception during these 3 months.
BSA, body surface area.
Courtesy, Peter C. M. van de Kerkhof, MD.
• Oral retinoids (e.g. acitretin, isotretinoin).
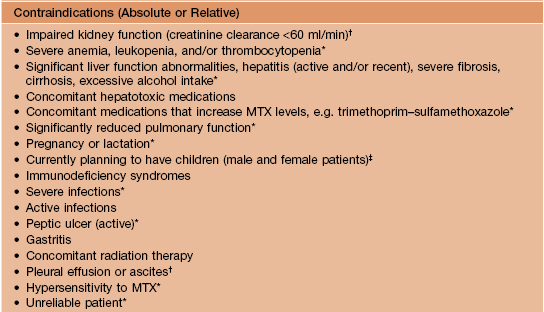
• Targeted immunomodulators (‘biologic’ agents) (Tables 6.6 and 6.7).
Table 6.6
Commercially available biologic agents used for the treatment of psoriasis.
* By registration authorities for the treatment of psoriasis.
** Production of alefacept in the United States was discontinued in 2011.
† Soluble form.
‡ Soluble form and transmembrane TNF receptor.
EMA, European Medicines Agency; FDA, Food and Drug Administration; IL, interleukin; TNF, tumor necrosis factor.
Table 6.7
Indications and contraindications for commercially available targeted immune modulators (‘biologic’ agents).
Administration of live vaccines is contraindicated in patients receiving biologic agents for psoriasis.
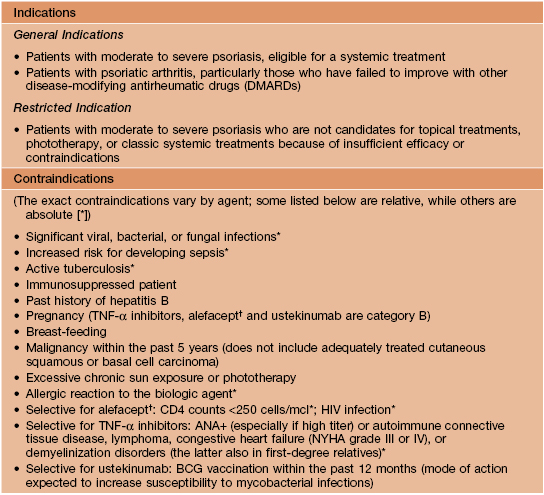
† Production of alefacept in the United States was discontinued in 2011.
BCG, bacillus Calmette–Guérin; NYHA, New York Heart Association.
Courtesy, Peter C. M. van de Kerkhof, MD.
• See Table 6.8 for treatment options in patients with comorbidities or special situations.
Table 6.8
Treatment of the psoriatic patient with comorbidities or special situations.
Targeted immunomodulators (‘biologic’ agents) are contraindicated in patients with active tuberculosis.
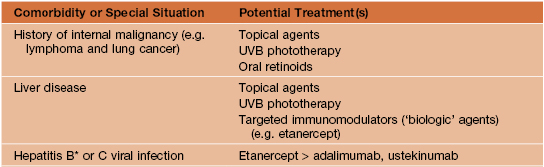
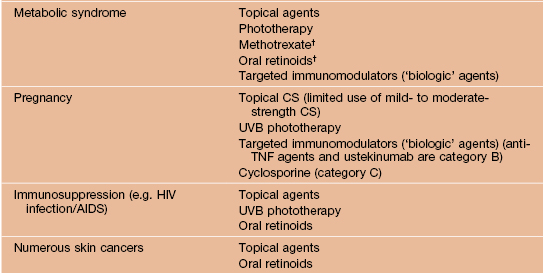
† Caution with use in patients with fatty liver.
*In hepatitis B surface antigen (HBsAg) carriers, either anti-HBV treatment or prophylaxis is required to prevent hepatitis reactivation; others require careful monitoring.
• See Table 6.9 for the recommended laboratory evaluation for patients receiving targeted immunomodulators.
Table 6.9
Recommended laboratory evaluation for patients receiving targeted immunomodulators for psoriasis.
A complete medical history and physical examination should also be performed, with particular attention to history/risk/symptoms/signs of tuberculosis, other chronic infections, malignancy, neurologic disorders and cardiac disease (especially congestive heart failure in patients receiving TNF-α inhibitors).
| Drug | Prior to treatment | During treatment |
| TNF-α inhibitors (e.g. adalimumab, etanercept, infliximab) or ustekinumab | Tuberculin skin test*/interferon-γ release assay** and/or (e.g. if immunosuppression or history of tuberculosis) chest x-ray CBC, CMP Hepatitis B and C virus serologic profiles Consider HIV testing |
Annual tuberculin skin test*/interferon-γ release assay** and/or chest x-ray CBC or CMP every 3-12 months (or as clinically indicated) |
* ≥5 mm of induration should be considered as positive.
** e.g. QuantiFERON® TB Gold or T-SPOT®.TB.
CMP, comprehensive metabolic panel (includes liver function tests); PPD, purified protein derivative.
For further information see Ch. 8. From Dermatology, Third Edition.