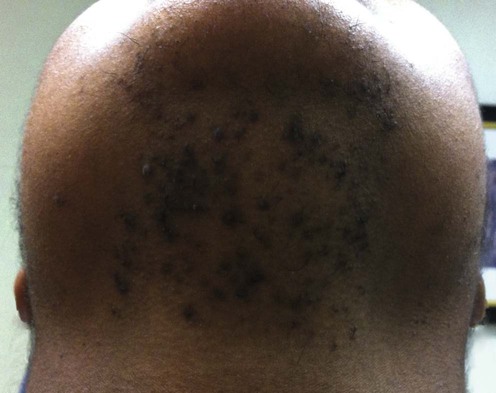
Pseudofolliculitis barbae
Management strategy
Specific investigations
An unusual Ala12Thr polymorphism in the 1A alpha-helical segment of the companion layer-specific keratin K6hf: evidence for a risk factor in the etiology of the common hair disorder pseudofolliculitis barbae.
The authors somehow conclude that this gene represents a significant genetic risk factor for PFB.
First-line therapies
Second-line therapies






 Beard growth
Beard growth Razor shaving technique
Razor shaving technique Hair clippers
Hair clippers Chemical depilatories
Chemical depilatories Adjunctive hair extraction
Adjunctive hair extraction Retinoic acid
Retinoic acid Glycolic acid
Glycolic acid Topical clindamycin
Topical clindamycin Laser depilation
Laser depilation Surgical depilation
Surgical depilation