CHAPTER 18 Proximal Ulnar Fractures in Children
INTRODUCTION
Proximal ulnar fractures in children and adolescents are uncommon, accounting for between 4% and 7% of pediatric and adolescent elbow fractures.1,2,6,8 As a result, (1) they are often completely missed, (2) the variation in growth centers makes the radiographic interpretation confusing, (3) the precise fracture line is often not appreciated, and (4) the potential for a poor outcome occurs if the displacement is not appreciated. In this chapter, we review fractures of the physis, metaphysis, and coronoid (Table 18-1).
TABLE 18-1 Types of Proximal Ulnar Fracture in the Pediatric Age Group
| Type | Incidence |
|---|---|
| Apophyseal (physeal, epiphyseal) | Very rare |
| Metaphyseal | 5% of elbow fractures |
| Coronoid | Less than 1% of elbow fractures |
GROWTH AND DEVELOPMENT
As noted in Chapter 1, at birth none of the articular elements of the ulna, including the coronoid and olecranon, are ossified. At age 9, the secondary center of ossification appears at the olecranon (Fig. 18-1). The ossification center may be bipartite and eccentric, and as the proximal ulna grows, the growth plate orientation alters from transverse to oblique. Closure of the physis begins at the articular surface and progresses toward the extensor surface of the bone. Just before fusion of the growth plate, the metaphyseal bone develops a sclerotic margin and may be widely separated from the apophysis, resembling a fracture. These vagaries can make it difficult to recognize a fracture of the olecranon in a child, and comparative views of the opposite side are often valuable.2 Although a secondary center may appear in the olecranon tip, there is no secondary ossification center of the coronoid. This helps explain the fracture pattern observed in the proximal ulna of the various age groups (Fig. 18-2).
APOPHYSEAL FRACTURE
Apophyseal fractures are extremely rare. Reviewing his experience and that of the literature up to 1991, Wilkins17 identified only 16 such cases. As a matter of fact, a review of the literature of the less rare olecranon or proximal ulnar fracture resulted in the identification of 192 cases but no mention of a fracture of the apophysis.17
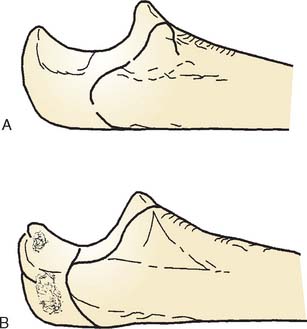
The fracture may or may not include the coronoid as the fracture line passes between the growth center and the proximal ulna (see Fig. 18-2). This is because the coronoid does not develop from a separate growth center; thus, the fracture line in this rarest of fractures may be rather variable (Fig. 18-3).
METAPHYSEAL FRACTURE
Metaphyseal fractures, although more common than fracture of the apophysis, still account for only approximately 5% of elbow injuries.3,11,15 Wilkins17 identified only 230 cases among 4,684 proximal ulnar fractures reported in the child before 1991. It appears that there is a biphasic frequency by age, with the greatest early frequency occurring between 5 and 6 years12 and a second incidence observed in the adolescent. The first peak probably relates to the growth and development of the bone. The second peak relates to the growth and development of the individual participating in activity with increasing propensity for injury.
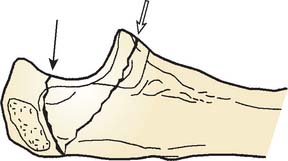
The mechanism of injury is similar to that described for many injuries about the elbow, including supracondylar, condylar fractures, and dislocations. Although proximal ulna fractures may be caused by direct impact, a more common mechanism is a fall onto an outstretched hand with transmission of the force proximally to the elbow. Differences in injury pattern probably relate to the precise degree of elbow flexion, possibly the rotation of the forearm, and the manner in which the muscles contracted at the time of impact. With fracture of the metaphysis, a varus or valgus force often occurs, causing additional fractures about the elbow. In four large series of proximal ulnar fractures, 20% had a documented associated fracture.17 In some reports, as many as 50% to 70% had an additional injury, most commonly involving the radial head with a valgus stress at the time of impact (Fig. 18-4).2,14,16
CLASSIFICATION
In 1981, Matthews10 offered a classification based on radiographic appearance, degree of displacement, and associated injury (±4 mm being the limit). Wilkins17 considered these by the mechanism of the fracture: (A) flexion; (B) extension; (1) valgus; (2) varus; and (C) shear injury. More recently, Graves and Canale7 classified the fracture according to (1) displacement greater or less than 5 mm and (2) presence of compounding. This classification was subsequently modified by Gaddy and coworkers,3 with a type I fracture being less than 3 mm and a type II greater than 3 mm. Evans and Graham2 have proposed a classification system based on anatomic site, fracture configuration, intra-articular displacement, and associated injuries, with approximately 18 subtypes. Thus, this fracture has the interesting characteristic of having almost as many classifications as episodes of occurrence.
Although metaphyseal fractures are extremely uncommon, as noted, they are more frequent than the physeal injury is, and they account for approximately 5% of all elbow injuries. Of these, only 10% to 20% require surgical management. Rarely, proximal ulna fractures may be associated with ipsilateral fractures in the distal humerus,9 ulnar shaft,13 or radial head.4
TREATMENT
As implied from the above-mentioned classification, the approach to treatment is based primarily on fracture displacement. Fortunately, approximately 80% of these fractures are minimally displaced, requiring open reduction and internal fixation in only 15% to 20% of individuals.2
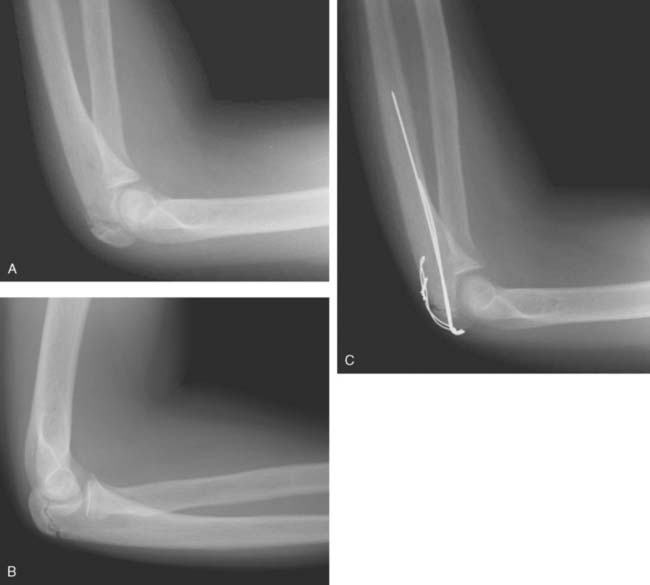
For those fractures that are minimally displaced, simple immobilization for approximately 3 weeks appears to be adequate and is the universal recommendation. For displacement of greater than 3 mm, depending on the classification, surgical treatment is indicated. It is uncommon to have greater than 4 mm displacement in patients under the age of 10 years; thus, open reduction and internal fixation are generally observed in the older age group. Several authors have noted that displacement found intraoperatively is often significantly greater than displacement appreciated on plain radiographs.3,7 Typically, the AO technique with smooth K-wire with circumferential tension band wire is adequate (Fig. 18-5). Recently, there have been several reports successfully using heavy absorbable suture in tension band technique instead of wire.2,5 Absorbable suture was prominent, less likely than wire to become symptomatic and did not need to be removed. Metal internal fixation is typically removed 6 to 12 months postoperatively to ensure that premature closure of the proximal ulnar physis does not occur, and to relieve symptoms of proximal hardware. There have been no reported cases of premature proximal ulnar physeal closure using this internal fixation technique.
RESULTS
Graves and Canale7 reported the results of 39 fractures treated over 30 years at the Campbell Clinic. Twenty-eight of 30 patients treated nonoperatively were classified as satisfactory after closed treatment. Of the nine treated by open reduction and internal fixation, seven (78%) developed a satisfactory result. Gaddy and colleagues3 reported 35 fractures occurring in patients ranging from 2 months to 15 years. Of these, all 23 treated nonoperatively were considered satisfactory. The criterion for nonoperative treatment was displacement of less than 3 mm. Furthermore, 10 of 10 patients with greater than 3 mm of displacement underwent open reduction and internal fixation, and all developed a satisfactory outcome.
Evans and Graham2 reported the results of 40 proximal ulna fractures treated surgically. In the text of their article a detailed treatment algorithm is provided, outlining their indications for surgical treatment. In summary, fractures greater than 4 mm were always treated surgically, fractures with less than 2 mm of displacement were never treated surgically, and treatment of fractures with displacement between 2 and 4 mm was determined by anatomic site, fracture configuration, and associated injuries. Thirty-six of 40 fractures were managed by tension band technique; 28 using wire and eight using absorbable suture.
COMPLICATIONS
As implied by the above-mentioned comments, the complications are uncommon; thus, approximately a 95% satisfactory outcome is observed whether the fracture is managed operatively or nonoperatively. The most common sequela of the fracture is slight limitation of extension. Ectopic bone does not appear to be a problem.
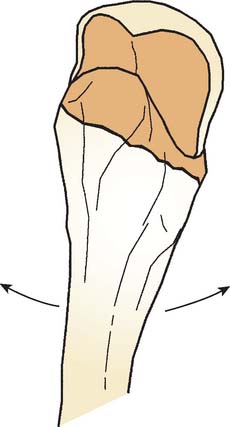
FRACTURE OF THE CORONOID
Because there is no secondary center of ossification, fracture of the coronoid as an isolated fracture is rare. As in the adult, injury to this structure is seen primarily with severe trauma or elbow dislocation. When a coronoid fracture is observed, a high level of suspicion should be aroused that a concurrent elbow dislocation has occurred.15 We have also seen in consultation a stress fracture of the coronoid in a 17-year-old gymnast (Fig. 18-6). Treatment is predicated on the integrity of the ulnohumeral joint; thus, the elbow is reduced and stability is ensured (see Chapters 27 and 29). The coronoid fracture in the child is then treated as a secondary consideration and frequently nothing need be done if the elbow is stable. We have not seen nor reported a large coronoid fracture as an isolated injury requiring open reduction and internal fixation in the child.
1 Dormans J., Rang M. Fractures of the olecranon and radial neck in children. Orthop. Clin. North Am. 1990;21:257.
2 Evans M.C., Graham K. Olecranon fractures in children, part I: a clinical review. Part II: a new classification and management algorithm. J. Pediatr. Orthop. 1999;19:559.
3 Gaddy B.C., Strecker W.B., Schoenecker P.L. Surgical treatment of displaced olecranon fractures in children. J. Pediatr. Orthop. 1997;17:321.
4 Gicquel P.H., De Billy B., Carger C.S., Clavert J.M. Olecranon fractures in 26 children with mean follow-up of 59 months. J. Pediatr. Orthop. 2001;21:141.
5 Gortzak Y., Mercado E., Atar D., Weisel Y. Pediatric olecranon fractures: open reduction and internal fixation with removable Kirschner wires and absorbable sutures. J. Pediatr. Orthop. 2006;26:39.
6 Grantham S.A., Kiernan H.A. Displaced olecranon fracture in children. J. Trauma. 1975;15:197.
7 Graves S., Canale T. Fractures of the olecranon in children. Long-term follow-up. J. Pediatr. Orthop. 1993;13:239.
8 Henrikson B. Supracondylar fracture of the humerus in children. Acta Chir. Scand. 1966;369:1.
9 James P., Heinrich S.D. Ipsilateral proximal metaphyseal and flexion supracondylar humerus fractures with an associated olecranon avulsion fracture. Orthopedics. 1991;14:713.
10 Matthews J.G. Fractures of the olecranon in children. Injury. 1981;12:207.
11 Maylahn D.J., Fahey J.J. Fractures of the elbow in children. J. A. M. A. 1958;166:220.
12 Newell R.L.M. Olecranon fractures in children. Injury. 1975;7:33.
13 Olney B.W., Menelaus M.B. Monteggia and equivalent lesions in childhood. J. Pediatr. Orthop. 1989;9:219.
14 Papavasilou V.A., Beslikas T.A., Nenopoulos S. Isolated fractures of the olecranon in children. Injury. 1987;18:100.
15 Regan W., Morrey B.F. Fractures of the coronoid process of the ulna. J. Bone Joint Surg. 1989;71A:1348.
16 Theodorou S.D. Dislocation of the head of the radius associated with fracture of the upper end of the ulna in children. J. Bone Joint Surg. 1969;51B:700.
17 Wilkins K.E. Fractures involving the proximal apophysis of the olecranon. In: Rockwood C.A., Wilkins K.E., King R.E., editors. Fractures in Children. Philadelphia: J. B. Lippincott; 1991:751.