CHAPTER 36 Proximal Femoral Osteotomy in the Skeletally Immature Patient With Deformity
Indications
Surgical technique
Surgical Technique for the Lateral Approach to the Proximal Femur
As the vastus lateralis is retracted medially, the periosteum of the femur is visualized. The lateral periosteum is incised, and the femur is subperiosteally exposed just distal to the lesser trochanter. A curved retractor is carefully placed subperiosteally around the anterior shaft of the femur. Posteriorly, the periosteum and the soft tissues are more securely attached to the bone; they are best elevated off of the bone with the electrocautery and the elevator. With blunt dissection, the subperiosteal exposure can be extended distally. With an adequate exposure, the femur should be visible and accessible from the proximal aspect of the greater trochanter to a point distal to the lesser trochanter, which is sufficient for the application of the fixation plate (Box 36-1).
Surgical Technique for Correcting Proximal Femoral Valgus Deformity in Young Children
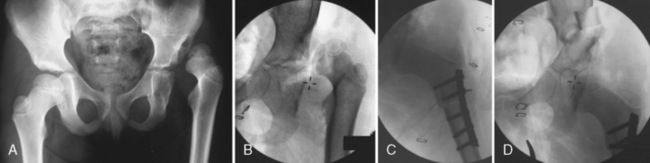
For children who are less than 5 years old, a small fragment, a semi-tubular straight plate, a Wagner forked plate (Aesculap, San Francisco, CA), or a small blade plate (Synthes, Paoli, PA) can be used for fixation. The appropriate implant is temporarily inserted into the incision to assess the adequacy of the exposure. If necessary, the skin and fascial incisions are extended distally to facilitate the insertion of the plate. C-arm imaging is used to confirm the optimum position of hip abduction, flexion, and internal rotation needed to reduce or satisfactorily position the femoral head into the acetabulum. A four- or five-hole small-fragment straight semi-tubular plate is the best choice for a femoral shortening osteotomy in conjunction with the open reduction of a developmentally dislocated hip. The anterior iliofemoral approach and open reduction are performed first through an oblique incision that parallels the lateral edge of the iliac crest. For the shortening osteotomy, the lateral proximal femur is approached as previously described. The osteotomy (Figure 36-1) is performed just distal to the lesser trochanter. The plate is placed just distal to the inferior edge of the greater trochanter physis as assessed with the C-arm. The plate is provisionally fixed by inserting a screw in the most proximal screw hole. A drill hole is also made in the bone that corresponds with the second most proximal hole. The proximal screw is loosened, and the plate is rotated anteriorly. The femoral osteotomy is performed just distal to the predrilled second proximal hole.
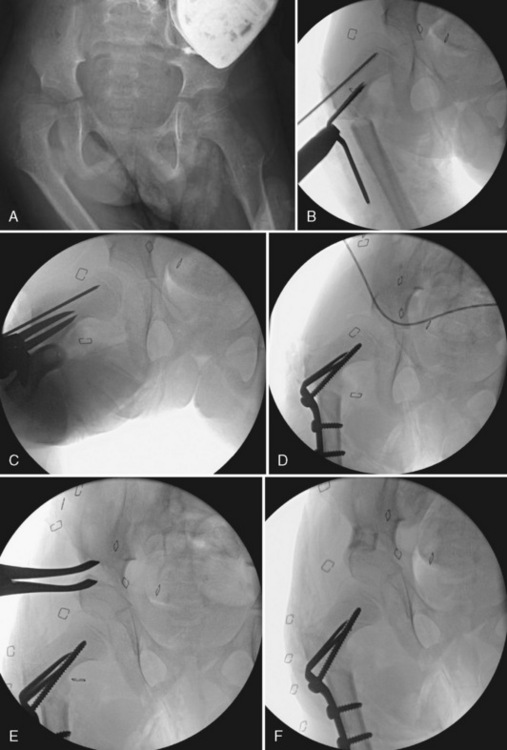
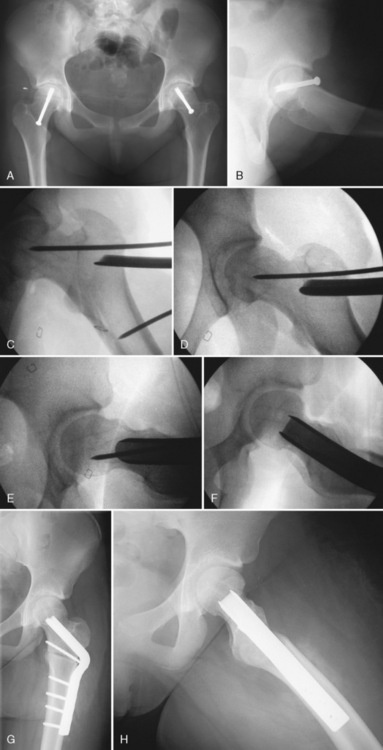
A Wagner forked plate works well for younger, smaller patients as fixation if angular correction is desired beyond shortening or rotation, as in a varus osteotomy to correct coxa valga associated with residual DDH or with static encephalopathy. If the Wagner plate is to be used, a smooth K-wire is inserted just proximal to the intended site of plate insertion (Figure 36-2). The K-wire is inserted from lateral to medial and placed superiorly in the neck on the anteroposterior view to provide enough space for the subsequent insertion of the Wagner plate. It is centered in the femoral neck on the lateral view. Subperiosteal retractors are circumferentially placed around the femur to protect the soft tissues. A femoral osteotomy is performed at the midpoint of the lesser trochanter, and this is confirmed with the use of C-arm imaging. The femur is transversely cut with an oscillating power saw under direct vision. After completing the osteotomy, consideration should be given to shortening the distal fragment 1 cm to 2 cm, because growth stimulation and secondary limb-length discrepancy often occur in these young patients. A Wagner forked plate of appropriate size is inserted into the proximal femoral fragment with the use of the previously inserted K-wire as a guide. The forked tips of the plate are inserted through the distal lateral cortex and carefully advanced medially and proximally into the femoral neck; the correct position is confirmed with the C-arm. After the prongs of the plate are fully inserted, the distal femoral fragment is reduced and secured to the proximal fragment with a self-centering bone-holding clamp. When performing a varus-producing osteotomy, the distal fragment should be slightly medialized relative to the proximal fragment. The proportion of medialization will vary slightly, depending on the entry point of the plate in the proximal fragment. Excessive medialization can produce an unstable construct as a result of a loss of contact between the fragments.
The final neck shaft angle, the plate fixation, and the hip reduction should be evaluated using the C-arm. A deep suction drain is placed, and the wound is closed in separate fascial layers. For young children (i.e., those less than 6 years old), a 1½ hip spica cast holding the thigh in a slightly abducted and flexed position is applied for 5 to 6 weeks (Box 36-2).
BOX 36–2 Technical Pearls: Correcting Proximal Femoral Valgus Deformity in Young Children
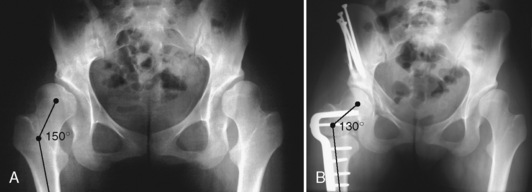
Surgical Technique for Correcting Femoral Valgus Deformity in Older Children, Preadolescents, and Adolescents
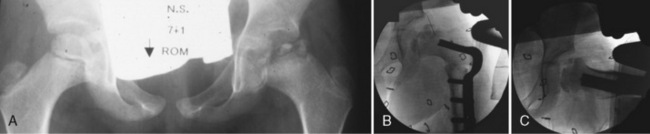
After the optimal correction has been achieved, the side plate is secured to the distal fragment with three bicortical screws with the use of the standard compression plating technique. After osteotomy fixation, hip range of motion is assessed to ensure that adequate flexion and extension, abduction and adduction, and approximately equal internal and external rotation have been obtained. Final C-arm images are taken to assess that both an appropriate redirection of the proximal femur and a stable osteotomy construct have been achieved (Figure 36-3). If the PFO is performed in conjunction with a pelvic osteotomy for the treatment of residual DDH, the pelvic osteotomy is performed first, followed by the PFO. If these procedures are performed in conjunction with a pelvic osteotomy to treat severe neuromuscular hip dysplasia, the PFO and any accompanying soft-tissue releases are done first, followed by the pelvic osteotomy. A deep suction drain is inserted into the fascial layers. The fascia of the vastus lateralis and the tensor fascia lata are repaired separately.
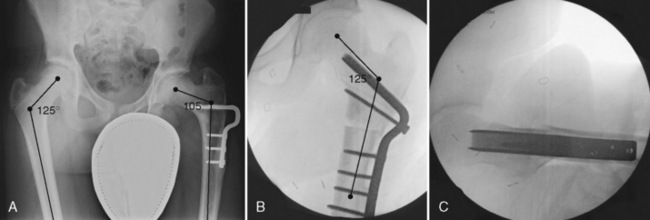
A proximal femoral varus-producing osteotomy is similarly performed for both preadolescents and adolescents. The same lateral approach and subperiosteal femoral exposure as described previously are used. The osteotomy site is typically located just proximal to the lesser trochanter in the intertrochanteric region. The osteotomy is fixated with either an adolescent-size (i.e., 90-degree angled, 40-mm blade length, and 10-mm offset) or an adult-size (i.e., 90-degree angled, 40-mm blade plate, and 10-mm offset) blade plate (Synthes, Paoli, PA). The radiographically monitored techniques for chisel and plate insertion are the same as those that were previously described. However, it is often considerably more difficult to insert both the chisel and the blade plate into the relatively denser bone of the adolescent. The chisel is gradually driven into the femur to a depth that is equal to the length of the blade plate that has been selected during preoperative planning (Figure 36-4).
Postoperatively, older patients are mobilized with protective weight bearing equal to the weight of the lower extremity for 6 weeks. When early bone consolidation callus formation appears on plain radiographs, progressive weight bearing is allowed. Most patients can perform full weight bearing without crutch protection by 8 to 10 weeks. Elective hardware removal is advised before excessive lateral bone overgrowth (Box 36-3).
Surgical Technique for Correcting Proximal Femoral Varus Deformity
When the osteotomy is complete, the distal fragment is mobilized and secured to the side plate with a bone clamp. If additional lengthening of the extremity is not desired, then one or both osteotomy fragments should be appropriately shortened to avoid the overlengthening of the extremity. After the blade plate has been inserted, a more normal neck shaft angle will be noted when the varus deformity is corrected as assessed with the C-arm (Figure 36-5). If necessary, it is possible to alter the relative degree of varus and valgus by changing to a different angle blade plate or bending the blade plate with a plate bender. Passive hip abduction will be notably increased. Patients with the coxa vara deformity often have inherent shortening of the adductor muscles. If after the correction of the varus deformity it appears that the shortening of the adductor muscle is limiting passive abduction, an adductor tenotomy should be performed, typically of the adductor longus tendon. Internal and external hip rotation is assessed. It may be necessary to internally rotate the distal fragment to correct an out-toeing gait deformity. The medial and lateral relationship of the two fragments is assessed. The fixation screws are inserted into the distal fragment with the use of a compression technique. Final C-arm images are taken to confirm that the desired correction has been achieved.
Very severe varus deformities can occur among younger children as a result of either congenital (developmental) coxa vara or coxa vara that occurs as a result of the treatment of DDH. The trochanter in these patients is often very high riding, the femoral neck is shortened, and the neck shaft angle is less than 90 degrees. When correcting this severe deformity, consideration must be given to restoring a more normal neck shaft angle, distal and lateral repositioning of the greater trochanter, and restoring a more normal femoral neck length. Both Wagner and Morscher have used a three-part osteotomy when attempting to correct all aspects of this often severe deformity. When performing either of these two relatively complex femoral osteotomies, the surgeon should be aware of the circulatory pathways of the medial femoral circumflex artery as it courses into the femoral capital epiphysis. There is an inherent risk of injury to the critical terminal branches of the medial circumflex artery as well as a risk for the subsequent occurrence of femoral capital epiphysis avascular necrosis that occurs with any osteotomy that cuts through the lateral femoral base of the trochanter or the femoral neck. Similarly, Cech and colleagues reported about the use of a two-part osteotomy to obtain correction, specifically of the typically severe coxa vara deformity that can occur after marked growth disturbance associated with the closed treatment of DDH. The 100-degree blade plate is inserted directly through the lateral aspect of the trochanter, and the osteotomy cut is a two-part triangle that is centered along the newly elongated inferior neck of the proximal femur. This osteotomy is theoretically less likely to injure the circulation of the proximal femur than the Wagner and Morscher osteotomies. When correcting relatively severe coxa vara deformities with any of the previously described valgus osteotomies, the trochanter is moved distally. This places the abductor muscles under increased tension, and a relative abductor contracture may be noted intraoperatively. With time, the functional abduction muscle tightness will resolve (Box 36-4).
BOX 36–4 Technical Pearls: Correcting Proximal Femoral Varus Deformity
Surgical Technique for Proximal Femoral Osteotomy for Slipped Capital Femoral Epiphysis
The intertrochanteric osteotomy can be fixed with either a 120-degree or a 90-degree angled blade plate. The 120-degree blade plate is inserted through the lateral cortex of the femur beginning at the level of the greater trochanter and is directed proximally into the femoral neck, whereas the 90-degree blade plate is inserted through the lateral femoral cortex and transversely across the proximal femur at the base of the femoral neck and is perpendicular to the femoral shaft (Figure 36-6).
Patients ambulate on postoperative day 1 or 2, as previously described. Large corrections have often been made at the osteotomy site. Weight bearing should not be progressed until there is radiologic evidence of progressive consolidation, which may take several weeks. With this approach, bone overgrowth on the implant often occurs. Implant removal is advised within 1 to 1.5 years (Box 36-5).
BOX 36–5 Technical Pearls: Proximal Femoral Osteotomy for Slipped Capital Femoral Epiphysis
Annotated references and suggested readings
Abraham E., Gonzalez M.H., Pratap S., Amirouche F., Atluri P., Simon P. Clinical implications of anatomic wear characteristics in slipped capital femoral epiphysis and primary osteoarthritis. J Pediatr Orthop. 2007;27:788-795.
Axer A. Subtrochanteric osteotomy in the treatment of Perthes’ disease. J Bone Joint Surg. 1965;47B:489.
Bucholz R.W., Ogden J.A. Patterns of ischemic necrosis of the proximal femur in nonoperatively treated congenital hip disease. In: The Hip. Proceeding of the sixth open scientific meeting of the Hip Society. St. Louis: CV Mosby; 1978:44-63.
Cech O., Vavra J., Zidka M. Management of ischemic deformity after the treatment of developmental dsyplasia of the hip. J Pediatr Orthop. 2005;25:687-694.
Crawford A.H. The role of osteotomy in the treatment of slipped capital femoral epiphysis. In: Barr S.J., editor. Instructional course lectures. Park Ridge: American Academy of Orthopaedic Surgeons; 1989:273-279.
Diab M., Hresko M.T., Millis M.B. Intertrochanteric versus subcapital osteotomy in slipped capital femoral epiphysis. Clin Orthop Relat Res. (427); 2004:204-212.
Galpin R.D., Roach J.W., Wenger D.R., Herring J.A., Birch J.G. One-stage treatment of congenital dislocation of the hip in older children, including femoral shortening. J Bone Joint Surg Am.. 1989;71(5):734-741.
Ganz R., Gill T.J., Gautier E., Ganz K., Krugel N., Berlemann U. Surgical dislocation of the adult hip a technique with full access to the femoral head and acetabulum without the risk of avascular necrosis. J Bone Joint Surg. 2001;83B:1119-1124.
Gautier E., Ganz K., Krugel N., Gill T., Ganz R. Anatomy of the medial femoral circumflex artery and its surgical implications. J Bone Joint Surg Br.. 2000;82(5):679-683.
Gordon J.E., Capelli A.M., Delgado E.D., Schoenecker P.L. Pemberton pelvic osteotomy and varus rotational osteotomy in the treatment of acetabular dysplasia in patients who have static encephalopathy. J Bone Joint Surg. 1996;78A:1863-1871.
Gordon J.E., Hughes M.S., Shepherd K., Szymanski D.A., Schoenecker P.L., Parker L., Uong E.C. Obstructive sleep apnoea syndrome in morbidly obese children with tibia vara. J Bone Joint Surg. 2006;88B:100-103.
Kalamchi A., MacEwen G.D. Avascular necrosis following treatment of congenital dislocation of the hip. J Bone Joint Surg Am.. 1980;62(6):876-888.
Describes the pattern of AVN in the femoral head following treatment for DDH..
Karadimas J.E., Holloway G.M., Waugh W. Growth of the proximal femur after varus-derotation osteotomy in the treatment of congenital dislocation of the hip. Clin Orthop Relat Res. (162); 1982:61-68.
Kasser J.R., Bowen J.R., MacEwen G.D. Varus derotation osteotomy in the treatment of persistent dysplasia in congenital dislocation of the hip. J Bone Joint Surg. 1985;67A:195-202.
Leunig M., Casillas M.M., Hamlet M., Hersche O., Notzli H., Slongo T., Ganz R. Slipped capital femoral epiphysis: early mechanical damage to the acetabular cartilage by a prominent femoral metaphysis. Acta Orthop Scand. 2000;71:370-375.
Leunig M., Slongo T., Kleinschmidt M., Ganz R. Subcapital correction osteotomy in slipped capital femoral epiphysis by means of surgical hip dislocation. Oper Orthop Trauma. 2007;19:389-410.
McNerney N.P., Mubarak S.J., Wenger D.R. One-stage correction of the dysplastic hip in cerebral palsy with the San Diego acetabuloplasty: results and complications. J Pediatr Orthop. 2000;20:93-103.
Morscher E. Osteotomy to lengthen the femur neck with distal adjustment of the trochanter major in coxa vara after hip dislocation. Orthopade. 1988;17:485.
Oh C.W., Guille J.T., Kumar S.J., Lipton G.E., MacEwen G.D. Operative treatment for type II avascular necrosis in developmental dysplasia of the hip. Clin Orthop Relat Res. (434); 2005:86-91.
Paley D.R. Hip joint considerations. In: Paley D.R., Herzenberg J.E., editors. Principles of deformity correction. Berlin: Springer-Verlag; 2002:650-653.
Schoenecker P.L., Anderson D.J., Capelli A.M. The acetabular response to proximal femoral varus rotational osteotomy. Results after failure of post-reduction abduction splinting in patients who had congenital dislocation of the hip. J Bone Joint Surg. 1995;77A:990-997.
Schoenecker P.L., Strecker W.B. Congenital dislocation of the hip in children. Comparison of the effects of femoral shortening and of skeletal traction in treatment. J Bone Joint Surg. 1984;66A:21-27.
Spencer S., Millis M.B., Kim Y.-J. Early results of treatment of hip impingement syndrome in slipped capital femoral epiphysis and pistol grip deformity of the femoral head-neck junction using the surgical dislocation technique. J Pediatr Orthop. 2006;26:281-285.
Tonnis D. Femoral osteotomies to improve the hip joint. In: Tonnis D., editor. Congenital dysplasia and dislocation of the hip in children and adults. Berlin: Springer-Verlag; 1987:336-355.
Wagner H., editor. The hip: Proceedings of the 4th open scientific meeting of the hip society. St. Louis: CV Mosby; 1976.
Weiner S.D., Weiner D.S., Riley P.M. Pitfalls in treatment of Legg-Calve-Perthes disease using proximal femoral varus osteotomy. J Pediatr Orthop.. 1991;11(1):20-24.
Whiteside L.A., Schoenecker P.L. Combined valgus derotation osteotomy and cervical osteoplasty for severely slipped capital femoral epiphysis: mechanical analysis and report preliminary results using compression screw fixation and early weight bearing. Clin Orthop Rel Res. 1978;132:88-97.