Chapter 106 Prevention of Retinal Detachment
Introduction
Rhegmatogenous retinal detachment continues to be an important cause of reduced visual acuity and blindness. In consecutive series, initial surgical attempts to reattach the retina currently fail in approximately 10–20% of cases, and reoperations are unsuccessful in as many as 5% of cases.1–3 Anatomical success is significantly less common in consecutive series of eyes with features suggesting an increased risk of proliferative vitreoretinopathy (PVR).4 Following anatomically successful surgery, visual acuity returns to 20/50 or better in only approximately 50% of cases.5 Thus, the prevention of retinal detachment is a worthy goal, and a variety of prophylactic methods have been investigated since Jules Gonin, in 1920, first identified the pathogenesis and treatment of this previously incurable disorder. However, despite a long-standing interest in the ophthalmologic community regarding prophylactic therapy, there have been no optimal clinical trials to test the legitimate value of any form of preventive treatment.6–8
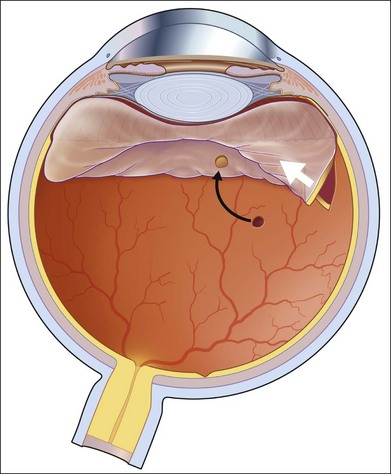
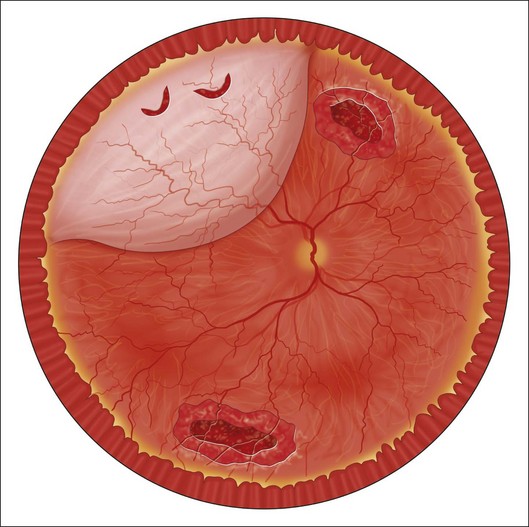
Vitreous liquefaction and a retinal break are prerequisites for rhegmatogenous retinal detachment, and the usual pathologic sequence is vitreous liquefaction followed by some degree of posterior vitreous detachment (PVD). This results in vitreoretinal traction at the site of a vitreoretinal adhesion and in the production of a retinal tear (Fig. 106.1). Alternatively, traction may be exerted upon areas of lattice degeneration containing atrophic retinal holes. Continued vitreoretinal traction near retinal breaks appears to be necessary to cause the vast majority of clinical retinal detachments. Thus, retinal detachment might be avoided by: (1) preventing vitreous liquefaction and associated PVD; (2) relieving vitreoretinal traction; or (3) creating a chorioretinal adhesion around vitreoretinal adhesions and retinal breaks.
No means are available to prevent vitreous liquefaction and later PVD in most eyes, although maintaining an intact posterior lens capsule after extracapsular cataract surgery may reduce or delay these changes.9,10 Vitreoretinal traction can be relieved by vitrectomy or by scleral buckling. However, prophylactic vitrectomy is not performed because there are technical difficulties in completely removing the peripheral vitreous gel, and it is relatively hazardous. Scleral buckling is only rarely employed, such as in particularly high-risk cases in which a nontraumatic giant retinal tear has already occurred in a fellow eye11 or in cases of posterior segment open globe injuries.12 Thus, the primary method of preventing retinal detachment involves the use of laser photocoagulation or cryotherapy to create a chorioretinal adhesion around both visible sites of vitreoretinal adhesion and retinal breaks. Although this is frequently successful in sealing the treated lesion and preventing it from causing a clinical retinal detachment, the genuine value of such therapy related to simple observation remains unclear in most situations, since most visible asymptomatic retinal breaks and vitreoretinal degenerative lesions do not cause retinal detachments. Instead, breaks causing detachment usually occur in regions of the peripheral retina that appear normal before PVD.6,7 In addition, relatively extensive prophylactic therapy may cause vitreous changes that actually increase the chances of subsequent vitreoretinal traction and retinal detachment.6,13
Risk factors for retinal detachment
In any eye with visible retinal breaks or vitreoretinal adhesive lesions that predispose to retinal detachment, a number of additional factors are considered to be associated with a relatively high risk of subsequent retinal detachment (Table 106.1). Symptoms and signs of acute PVD place an eye at particularly high risk. Additional factors include a variety of hereditary, congenital, acquired, and iatrogenic problems.
Table 106.1 Risk factors for rhegmatogenous retinal detachment
| Hereditary/congenital/developmental/degenerative
Prior ocular surgery Prior ocular trauma Inflammatory Other Fellow-eye nontraumatic retinal detachment |
In evaluating the natural history or risk of retinal detachment in these cases, particular attention must be paid to the way in which both natural history and postoperative data, regarding a variety of retinal lesions, have been collected. The risk of retinal detachment is substantially different among subgroups of eyes, a fact that influences interpretation of both natural history data and treatment results. For example, since an acute PVD is the primary cause of most retinal detachments, and since most retinal tears occur during or soon after PVD, it is likely that eyes without a PVD have a higher risk of later retinal detachment than eyes with a history of prior PVD and no subsequent retinal breaks, regardless of additional risk factors.14 Similarly, vitreous liquefaction and PVD occur with greater frequency in older patients and in myopic and nonphakic eyes.15 Thus, data regarding lesions in otherwise normal, young, nonmyopic eyes are not comparable with data from cases with other risk factors that greatly increase the likelihood of PVD. Since more than one factor is often present, data analysis is difficult if all features are not recorded. For example, myopic aphakic eyes with lattice degeneration and with a history of retinal detachment in the fellow eye have a substantially greater risk of retinal detachment than otherwise normal eyes with lattice degeneration. No prospective randomized trials of therapy to prevent retinal detachment have been performed.6–8 The few published studies of treated and untreated comparable eyes have been retrospective, and most reports regarding prophylactic therapy have simply described results of a treatment series.
This chapter briefly discusses published outcomes regarding both the natural course of lesions that predispose an eye to retinal detachment and results of prophylactic therapy for these retinal breaks and vitreoretinal adhesive lesions. The topic of “subclinical retinal detachment” (for definition, see Fig. 106.4) will not be discussed as a separate entity because of the nonspecific nature of the term. This chapter distinguishes symptomatic from asymptomatic cases and is organized according to the type of retinal break or vitreoretinal adhesive disorder and also according to the presence of other high-risk factors. A brief discussion of treatment methods precedes the review of treatment results and complications.
Symptomatic eyes
Patients are considered symptomatic if they describe photopsia and/or increased vitreous floaters associated with an acute posterior vitreous detachment. Approximately 15% of eyes with a symptomatic PVD develop retinal tears of various types.16–18 The risk of retinal tears is directly related to the amount of vitreous hemorrhage associated with symptoms, and the finding of pigmented cells in the vitreous is a sign associated with a particularly high chance of associated retinal tear(s).19 In symptomatic eyes, retinal tears associated with persistent vitreoretinal traction are especially likely to cause retinal detachment, and the likelihood is even higher in cases with additional high-risk factors.
Retinal tears resulting from a symptomatic PVD should be distinguished from pre-existing retinal breaks detected after the PVD but not caused by it. Thus, atrophic retinal holes within areas of lattice degeneration are not considered “symptomatic,” even if they were first observed during an examination prompted by symptoms of an acute PVD. Symptomatic retinal tears are subdivided into those with persistent vitreoretinal traction and those in which all traction in the region of the retinal defect has disappeared (Fig. 106.1).
Tears with persistent vitreoretinal traction
Most symptomatic tears with persistent vitreoretinal traction are horseshoe-shaped and have a high risk of causing clinical retinal detachment. Rarely, a retinal tear with a free operculum may have persistent vitreoretinal traction as a result of a residual vitreoretinal adhesion near the retinal break, most frequently at the location of a retinal blood vessel (Fig. 106.2).
Horseshoe-shaped tears
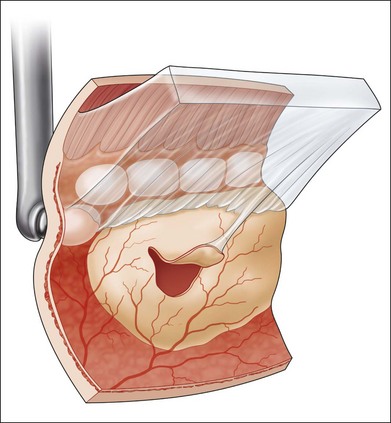
Untreated symptomatic retinal tears with persistent vitreoretinal traction have been reported to cause retinal detachment in 33–55% of cases (Table 106.2). Treatment of this type of break substantially reduces the risk of retinal detachment (Table 106.2),20 and immediate therapy for these lesions is indicated to prevent an accumulation of subretinal fluid.7,26 A chorioretinal adhesion is created in flat retina immediately adjacent to localized subretinal fluid (Fig. 106.3). Reviews of treatment techniques have been provided elsewhere in the literature,27 and these are briefly discussed later in this chapter.
Round tears
The percentage of operculated retinal tears that are associated with persistent vitreoretinal traction in the vicinity of the retinal break is unknown, but it is quite low. Only two symptomatic operculated retinal breaks have been reported to progress to retinal detachment, and both were associated with persistent vitreoretinal traction on a nearby retinal vessel.23,25 In unusual cases in which an operculated retinal hole is the only retinal break associated with a clinical retinal detachment, it is presumed that anomalous persistent vitreoretinal adhesions are located in the vicinity of the retinal tear (Fig. 106.2). Failures following treatment of operculated retinal holes have not been reported (Table 106.1).
Tears unassociated with persistent vitreoretinal traction
Symptomatic operculated retinal tears unassociated with persistent vitreoretinal traction in the vicinity of the retinal break have not been reported to progress to clinical retinal detachment (Table 106.1). Similarly, although large numbers of these breaks have been treated prophylactically, there are no reports in the literature of a treatment failure (Table 106.1). Treatment of this type of retinal break appears to be unnecessary unless the possibility of persistent vitreoretinal traction cannot be excluded.
Retinal holes and precursors of retinal detachment
Eyes with symptoms and signs of acute PVD frequently contain atrophic retinal breaks that are not due to acute vitreoretinal traction. For the purposes of this discussion, these lesions are considered to be pre-existing and not symptomatic.17 Similarly, precursors of retinal detachment, including lattice degeneration, cystic retinal tufts, and age-related retinoschisis, are managed as if they were originally discovered in asymptomatic eyes.
Asymptomatic eyes without high-risk factors
Vitreoretinal precursors of retinal breaks
Lattice degeneration
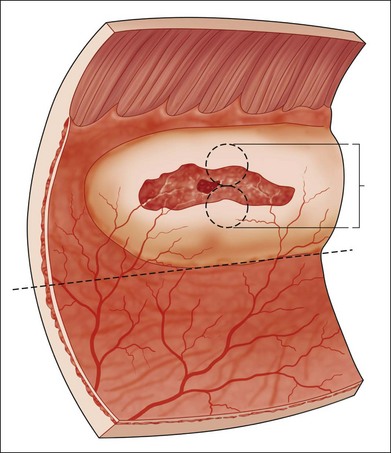
Lattice degeneration is present in approximately 30% of retinal detachments, and approximately 94% of these detachments occur in primary (nonfellow) eyes.6 Because lattice lesions are visible and occur in approximately 8% of the population, they have commonly been considered as candidates for prophylactic therapy. However, Byer’s natural history study of 276 patients and 423 involved eyes, followed an average of almost 11 years, indicated that lattice lesions in phakic nonfellow eyes were not particularly dangerous.28 At the end of the follow-up period, atrophic retinal holes were present in 150 (35%) eyes. Subclinical retinal detachments, defined as subretinal fluid extending more than one disc diameter (DD) from the break but not posterior to the equator (Fig. 106.4), were observed in ten of the eyes with holes. In six of these eyes, the subclinical detachment developed during the observation period, whereas four eyes exhibited the changes at the initial examination. Only one subclinical detachment was considered in need of treatment after a small asymptomatic posterior extension of subretinal fluid.
Four asymptomatic tractional retinal tears were observed in three of these 423 eyes at the initial examination, and symptomatic tractional tears without clinical detachment developed in five additional eyes during follow-up periods of 1.5–18 years.28 Three of five symptomatic and all asymptomatic breaks occurred adjacent to lattice lesions. All symptomatic breaks were successfully treated; no asymptomatic tractional tears were treated, and none changed over follow-up periods of 7, 10, and 15 years.
Clinical retinal detachments developed in three of the 423 eyes.28 Two were due to round retinal holes in lattice lesions of patients in their mid-20s, and one was due to a symptomatic tractional tear. These figures clearly indicate that patients with lattice degeneration in a phakic nonfellow eye should not be treated prophylactically unless symptoms occur. However, retinal detachments associated with vitreoretinal traction upon lattice lesions containing atrophic retinal holes are relatively common in eyes with significant amounts of myopia.29,30 A discussion regarding self-examination of peripheral visual fields and periodic follow-up examinations are in order in myopic patients to reduce chances of macular involvement by slowly progressive detachments resulting from round holes in lattice lesions.
Cystic retinal tufts
Retinal tears at sites of cystic retinal tufts may be responsible for as many as 10% of clinical retinal detachments associated with posterior vitreous detachment,31 and they are also associated with asymptomatic small horseshoe-shaped tears and minimal subretinal fluid in the absence of PVD.32 Byer31 calculated the chances of clinical retinal detachment in eyes with cystic retinal tufts to be one in 357, and these lesions are not worthy of prophylactic therapy in otherwise normal eyes.
Degenerative retinoschisis
Clinical retinal detachments occur in association with degenerative retinoschisis in up to 6% of consecutive detachment cases,33 and the presence of retinoschisis and outer layer breaks has sometimes been considered an indication for prophylactic therapy.34 However, a natural course study of 218 eyes in 123 patients demonstrated no clinical retinal detachments during a follow-up period averaging 9.1 years.33 The vast majority of small subclinical detachments that develop in association with outer layer breaks remain small, and prophylactic therapy is indicated only in the presence of obvious significant progression of subretinal fluid posterior to the equator.
Asymptomatic retinal breaks
In phakic nonfellow eyes, asymptomatic retinal breaks that are routinely discovered during an evaluation of the peripheral retina are extremely unlikely to lead to clinical retinal detachment, even if they are flap tears and even if posterior vitreous detachment occurs.35 During a follow-up period averaging 11 years, asymptomatic retinal breaks in 235 eyes of 196 patients were studied, and horseshoe-shaped tears were present in 45 cases. Acute PVD occurred in nine eyes without adversely affecting the pre-existing breaks, although new horseshoe-shaped tears developed in three cases, and these were promptly treated. Subclinical retinal detachments were observed in 19 (8%) eyes. Modest extension of subretinal fluid required therapy in two of these cases, and in a third case, a peripheral clinical retinal detachment slowly developed after 14 years of observation.
Prophylactic therapy for asymptomatic retinal breaks in phakic nonfellow eyes is usually not recommended. An occasionally observed exception to this rule is an inferior retinal dialysis. These breaks can cause slowly progressive retinal detachments that frequently become symptomatic only after macular involvement.36
Asymptomatic nonfellow eyes with high-risk factors
Myopic nonfellow eyes
Myopia is obviously associated with an increased risk of retinal detachment, and there is a direct correlation between amount of myopia and rate of retinal detachment.37 Lattice degeneration associated with retinal holes did not correlate with degree of myopia in the natural course study of Byer,28 although most slowly progressive clinical retinal detachments associated with lattice degeneration and an absence of extensive posterior vitreous detachment occur in young myopic patients,29,30 as noted above. There appears to be no increased value for treatment of myopic eyes with lattice degeneration in nonfellow eyes, and it is noteworthy that the small favorable effect of preventive treatment of lattice lesions in phakic fellow eyes could not be demonstrated if the degree of myopia exceeded 6 diopters.38
Asymptomatic retinal breaks are more common in myopic eyes than in emmetropic or hyperopic cases.5 However, clinical retinal detachments in these cases are rare in the absence of new symptoms, and prophylactic treatment is usually not advised in nonfellow eyes.
Aphakic and pseudophakic nonfellow eyes
Removal of the crystalline lens is associated with a substantial increase in the rate of later retinal tears and detachments,39 regardless of the method of cataract surgery, and this probably is due to vitreous changes in the nonphakic eye. An intact posterior lens capsule appears to be associated with a reduced rate of retinal detachment following cataract surgery, whereas Nd:YAG capsulotomy is clearly associated with an increased risk of subsequent detachment.9,10
Asymptomatic retinal breaks in nonfellow nonphakic eyes or eyes undergoing cataract surgery have sometimes been regarded as an indication for prophylactic therapy. However, Friedman et al.40 followed 18 retinal breaks in nonmyopic aphakic eyes for 3–7 years, and none detached. Hyams et al.41 studied 103 myopic aphakic eyes and discovered 25 asymptomatic retinal breaks in 19 eyes. Although six of the 25 were horseshoe-shaped tears, later retinal detachment occurred in no cases. More thorough reviews of the literature regarding the natural course of asymptomatic nonphakic retinal breaks and therapy for them have been published elsewhere,6,27 and there are not sufficient data to provide firm guidelines for management of asymptomatic retinal breaks in nonfellow eyes that are nonphakic or scheduled for cataract surgery. Treatment of horseshoe-shaped tears in these cases appears to be frequently recommended despite the lack of appropriate information in the literature.7,26
Asymptomatic patients with retinal detachment in the fellow eye
Pathologic vitreoretinal changes often occur bilaterally, and patients with retinal detachment in one eye have a significantly increased risk of retinal detachment in the other eye. This risk has been estimated as ranging from as low as 9% to as high as 40%.27 Thus attempts to prevent retinal detachment in the second eye have received considerable attention. Prospective randomized studies have not been performed, but retrospective data regarding precursors of retinal detachments and asymptomatic retinal breaks have been published. These can be further categorized as phakic and nonphakic fellow eyes.
Asymptomatic phakic fellow eyes
Precursors of retinal breaks
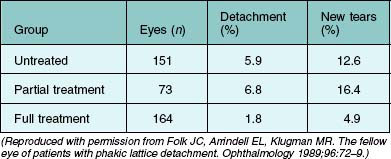
Lattice degeneration is three times more common in eyes in which a retinal detachment associated with lattice degeneration has occurred in the fellow eye than it is in the general population.6 Lattice degeneration has been the most frequently studied indication for prophylactic therapy in fellow eyes. The widely quoted study of Folk et al.38 retrospectively studied 388 consecutive cases, in which phakic retinal detachment associated with lattice degeneration occurred in one eye and lattice degeneration was present in the second eye. During an average follow-up period of over 7 years, new retinal breaks or detachments occurred in 31 (20%) untreated eyes (Table 106.3). New tears with retinal detachment developed in nine eyes (5.1%), and new tears without detachment developed in ten cases. In ten eyes, new holes developed within areas of lattice degeneration, and atrophic retinal breaks occurred in areas distant from lattice lesions in the remaining two cases.
Folk et al.38 reported a reduction in the incidence of new retinal tears and detachments in eyes receiving prophylactic therapy for all lattice lesions (Table 106.3). New tears without detachment occurred in five (3.0%) of these fully treated eyes. Retinal detachment occurred in three additional eyes (1.8%), compared with 5.1% in the 151 untreated phakic fellow eyes. The small beneficial effect of treating all lattice lesions was apparent when follow-up periods of 3, 5, and 7 years were analyzed separately. The beneficial effect was statistically significant for all patient subgroups, except in eyes with myopia of 6 diopters or more and in eyes with both high myopia and more than 6 clock-hours of lattice degeneration. Importantly, in these subgroups, treatment did not reduce the risk of retinal tears or detachment. Conversely, no detachments occurred after full treatment in eyes with less than 6 clock-hours of lattice degeneration or with less than 1.25 diopters of myopia.
In a subsequent evaluation of the same data, Folk et al.42 reported that new horseshoe-shaped tears developed in areas unassociated with lattice degeneration in approximately 30% of treated cases, and Byer6 has estimated that as many as 58% of retinal detachments in eyes with lattice degeneration arise in areas that exhibit no visible vitreoretinal abnormalities (Fig. 106.5). Because of this reality, some surgeons have recommended prophylactic therapy featuring the production of laser or cryotherapy burns over 360° of the peripheral retina (Fig. 106.6).6,27 However, the precise indications, intraocular findings, long-term results, and complications of this form of therapy have not been thoroughly described, and remarkably different success rates have been reported. Haut et al.43 described 109 phakic fellow eyes followed for a minimum of 5 years, and only one retinal detachment and two additional tears occurred posterior to the circumferential chorioretinal adhesion. However, in another study,44 retinal detachment occurred in five of 10 cases of Stickler syndrome within 15 months of 360° prophylactic therapy. Byer6 has tabulated and reviewed data from 15 reports advocating such treatment, and he concluded that this form of treatment appeared to be both ineffective in preventing subsequent detachment and dangerous in apparently aggravating vitreoretinal traction. The value of this form of therapy to prevent giant retinal tears and tears following vitrectomy and other procedures will be discussed in a separate section below.
Studies of prophylactic therapy of lattice degeneration, with and without holes, in phakic fellow eyes have been of limited value because they have not been prospective and because important information has been missing from available retrospective analyses. In particular, the outcomes have not been studied as a function of the presence of a posterior vitreous detachment. Davis25 demonstrated that retinal detachments were unusual in phakic fellow eyes if a PVD was present at the time of the initial examination. Retinal detachments occurred in none of 33 such cases. However, if a PVD was not present, retinal detachment subsequently developed in 14 (13%) of 112 phakic fellow eyes with lattice lesions.
Degenerative retinoschisis is an unusual cause of progressive retinal detachment, but retinoschisis is both common and frequently bilateral. Thus, patients with both retinal detachment and retinoschisis in one eye frequently have retinoschisis in the fellow eye. An evaluation of the literature regarding prophylactic therapy for retinoschisis in phakic fellow eyes is very difficult because of a lack of complete information regarding the cases.27 In the unusual case in which outer layer retinal breaks have been responsible for retinal detachment in the first eye, and outer layer breaks and retinoschisis are present in the fellow eye, prophylactic therapy is frequently recommended.
Retinal breaks
Asymptomatic retinal breaks in phakic second eyes of patients with previous retinal detachment are frequently cited as an indication for prophylactic therapy.27 Flap tears appear to be much more likely to cause retinal detachment than round or operculated retinal holes (Fig. 106.1).25,45 Merin et al.45 discovered retinal breaks in 186 (19%) of 966 fellow eyes, 28 of which (15%) later developed retinal detachment. Horseshoe-shaped tears were the cause of the detachment in 20 (71%) of the 28 eyes, whereas only 19% of breaks were flap tears in the 158 eyes that did not progress to retinal detachment. However, Hyams et al.41 followed ten untreated asymptomatic horseshoe-shaped tears in phakic fellow eyes, and no retinal detachments occurred. Deficiencies in prior reports have made it difficult to assess both the natural course of asymptomatic retinal breaks that are discovered on an examination of a fellow eye and the results of treatment of these lesions. Most of these breaks are round and located within areas of lattice degeneration, and these cases were discussed earlier. Data regarding therapy for asymptomatic horseshoe-shaped tears in fellow eyes suffer from a lack of details, including the status of the vitreous gel and the relationship between the original retinal break and the cause of subsequent retinal detachment. An aggressive national program of routine treatment of all retinal breaks in fellow eyes did not reduce the prevalence of retinal detachment in Israel.46 Still, treatment of horseshoe-shaped tears that are discovered in asymptomatic fellow eyes is sometimes recommended despite the absence of optimal supportive data.
Giant retinal tears
Prophylactic treatment is frequently recommended in phakic fellow eyes in which a nontraumatic giant retinal tear has occurred in the first eye. Freeman11 followed 321 cases for 12 months to 29 years. New giant retinal tears occurred in 14 (4.4%) untreated eyes, 13 of which were highly myopic and had developed “high-risk features” of increased vitreous liquefaction, and “white-with-pressure” that increased in extent. In a report by Wolfensberger et al.,47 48 patients were evaluated following repair of a giant retinal tear in one eye and 360° cryotherapy of the second eye for a mean of 84 months. During the follow-up period, retinal detachment developed in three patients, and a retinal tear alone was observed in a fourth.
Ang et al.48 subsequently described 360° cryotherapy to prevent giant retinal tear in Type 1 Stickler syndrome in a retrospective study. Most of the cases were phakic, and the results indicated that such treatment significantly reduced the risk of later retinal detachment. However, the results of this study were subsequently criticized49 because of methodology issues, and the ultimate answers regarding the value of this form of therapy will require more optimal studies.50
Asymptomatic aphakic and pseudophakic fellow eyes
All eyes have an increased risk of retinal detachment after cataract extraction, and the risk for fellow eyes in patients with previous retinal detachment in the first eye has been estimated to be 14–41%.27 The chances of detachment would be expected to be higher if secondary YAG capsulotomy were required.9,10 Thus, prophylactic therapy has frequently been recommended for vitreoretinal lesions in fellow eyes that are nonphakic or that are scheduled to undergo cataract extraction.
Precursors of retinal breaks
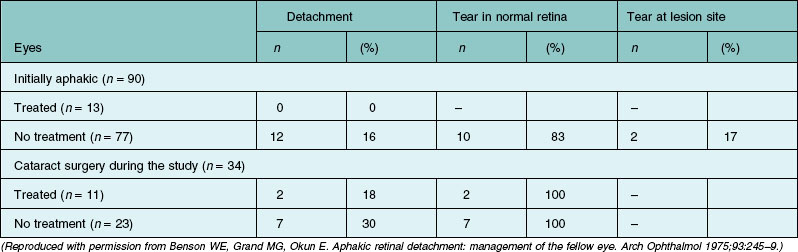
Of the precursors of retinal tears that have been considered for prophylactic therapy before or after cataract extraction, only lattice degeneration has been extensively studied, and reviews of the literature have been published.6,27 However, no prospective randomized studies have compared the natural course in these cases with outcomes following preventive treatment.7 As is true of phakic fellow eyes, a major problem in treating only visible pathology is the frequency of new retinal tears that develop in areas of the peripheral retina that appear normal (Table 106.4, Fig. 106.5). Although treatment of visible lesions appears to reduce the chances of retinal tears occurring at the treated site, the retinal detachments that frequently develop in these fellow eyes are not prevented by this focal therapy.51–53
Studies of prophylactic treatment of lattice degeneration in fellow nonphakic eyes have not been stratified on the basis of posterior vitreous detachment. Hovland14 demonstrated the critical importance of this variable by studying aphakic eyes of patients with aphakic retinal detachment in the primary eye. Retinal detachment subsequently occurred in one (2.3%) of 43 eyes with a PVD in the fellow eye. In the 40 eyes without a previous PVD, retinal detachment later occurred in eight eyes (21%). Similarly, Davis25 reported that retinal detachments occurred in five (24%) of 21 aphakic fellow eyes without an apparent PVD (absence of Weiss ring or clearly visible posterior cortical vitreous surface) at the initial examination, but detachments did not occur in 15 additional cases in which a PVD was initially present.
However, as noted earlier, the risk–benefit ratio of this form of treatment in unoperated eyes remains unknown. Treatment of lattice lesions in nonphakic fellow eyes is frequently recommended,26 despite the lack of supportive data. In eyes in which a PVD has previously occurred, it is doubtful if therapy is particularly effective or necessary. The value of various forms of prophylactic treatment in eyes without PVD will remain debatable until appropriate trials are conducted.
Retinal breaks
Retinal breaks in nonphakic eyes of patients with a previous retinal detachment in the other eye appear to have a higher rate of detachment.27 Davis25 described asymptomatic retinal breaks in ten aphakic fellow eyes. Subsequent retinal detachments occurred in five of these cases. Four of the five breaks causing retinal detachment were horseshoe-shaped tears, and the type of the fifth break was not reported. The literature regarding the value of treating round holes unassociated with lattice lesions is not clear. Treatment can be expected to prevent retinal detachment resulting from the identified break but not detachment resulting from breaks in other areas of the retina. Treatment of asymptomatic horseshoe-shaped tears in aphakic fellow eyes and in fellow eyes scheduled to undergo cataract extraction is recommended despite the absence of supportive data.26
Giant retinal tears
Aphakic fellow eyes in nontraumatic giant retinal tear cases have a high risk of retinal detachment. Prophylactic therapy has been recommended for fellow eyes of these patients if significant vitreous liquefaction and progressive “white-with-pressure” are observed10 or, alternatively, in all such cases.
Prophylactic therapy in eyes undergoing vitreoretinal surgery
As noted previously, because of the tendency for new retinal breaks to develop in areas of the retina that appear normal, 360° treatment (Fig. 106.6) has been advocated during various forms of vitreoretinal surgery.
During silicone oil removal in previously operated eyes
In a nonrandomized retrospective study of eyes following vitrectomy and silicone oil installation, 360° laser therapy appeared to be of value following removal of the oil,54 a more recent prospective study55 demonstrated similar results in apparently comparable eyes following oil removal.
During primary vitrectomy for nonretinal detachment
In a study of eyes undergoing primary vitrectomy for macular disorders, Koh and coworkers56 evaluated a consecutive series of 220 eyes in a retrospective analysis. Peripheral laser therapy had been applied in 115 cases, and they were compared with 105 allegedly comparable eyes that had not received laser retinopexy. Postoperative retinal detachment subsequently developed in 11.4% of the nontreated cases and in 3.5% of those that were treated. However, the eyes were not stratified on the basis of a pre-existing vitreous detachment, and 56 cases were lost to follow-up before 6 months.
During pneumatic retinopexy
Tornambe57 has advocated 360° laser therapy to prevent later retinal detachment in cases undergoing primary pneumatic retinopexy for retinal detachment, and other authors have described this technique at meetings and in non-peer-reviewed publications. Treated cases have had a lower incidence of subsequent retinal detachments due to new breaks. Still, optimal prospective studies have not been performed.
Treatment methods
The three methods currently available for creating chorioretinal adhesions are diathermy, photocoagulation, and cryotherapy. Diathermy is best applied with scleral dissection, a surgical technique that currently is very rarely employed to prevent retinal detachment. However, it can be used to treat localized subclinical detachments when combined with scleral buckling. Thus, treatment to prevent retinal detachment usually entails a choice between cryotherapy and laser photocoagulation. Photocoagulation was first performed using a xenon arc light source, but this has been replaced by laser photocoagulation. Cryotherapy and laser photocoagulation cause chorioretinal adhesions that seem equally effective in preventing retinal detachment, and choice of a treatment method depends on individual features of the case. Sometimes both methods are used in the same eye, because parts of one or more lesions can be treated best with one modality and other parts are treated best with the other (see Fig. 106.3).
Surgical techniques
Cryotherapy
Some retinal lesions can be treated with a single application, whereas others require multiple applications. Large retinal breaks are surrounded by contiguous applications while avoiding freezing of the exposed pigment epithelium within the open break, thus preventing further dispersion of pigment epithelial cells into the vitreous cavity. Areas of lattice degeneration are also surrounded by multiple applications, with each application straddling the posterior and lateral margins of the lattice lesions where acute retinal tears are most likely. The area anterior to all retinal breaks with persistent vitreous traction is also treated, since progressive traction may cause anterior extension of the break (see Fig. 106.3).
Results and complications of prophylactic therapy
As noted in previous sections, no prospective randomized clinical trial has been performed to evaluate treatment of precursors of retinal tears and retinal breaks, and interpretation of existing treatment results is difficult because the natural course of the respective lesions is uncertain.7,26 In addition, available studies have not appropriately stratified important variables for comparison of subgroups. However, the most thorough natural course studies of lattice degeneration,28 degenerative retinoschisis,33 and asymptomatic retinal breaks6 demonstrate that these conditions rarely cause acute retinal detachment in patients without a previous retinal detachment in the fellow eye.
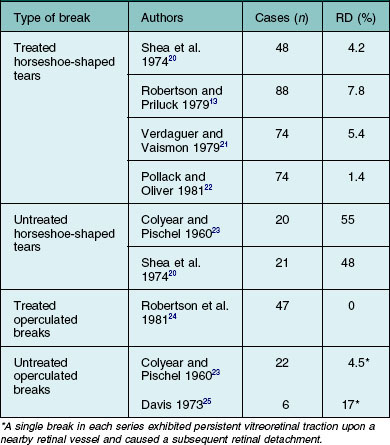
Results of prophylactic therapy
Results of treatment to prevent retinal detachment are presented in Tables 106.2–106.4. The studies are all somewhat incomplete, as most do not describe information about important variables, including the refractive error, the status of the crystalline lens, the status of the posterior vitreous surface, the type of retinal breaks, and whether there had been a detachment in the fellow eye. In addition, longer-term (e.g., 5–10 years) follow-up information is lacking in most reports. In a 1991 study, Smiddy et al.58 demonstrated that new retinal breaks continued to occur long after initial prophylactic therapy. In symptomatic eyes that were treated, new retinal breaks were observed in 13%, 3 months after therapy and in 21%, 2 years postoperatively. The outcomes in this report were not stratified as a function of the type of initial retinal break, so the data are not included in the tables. Another study demonstrated that most detachments that occurred after prophylactic therapy were associated with progression of an incomplete initial PVD.59
Flap tears
Horseshoe-shaped tears are mostly responsible for clinical retinal detachment. Symptomatic horseshoe-shaped tears are much more likely to cause retinal detachment than are asymptomatic tears, but many studies have not distinguished between these groups. However, failure of treatment is more common following therapy of symptomatic cases.58 Early failures are usually due to vitreoretinal traction forces that cause an accumulation of subretinal fluid before establishment of an adequate chorioretinal adhesion or to incomplete or inadequate therapy. Treatment should be placed in flat retina immediately adjacent to the location of subretinal fluid, and treatment should extend well anterior to the “horns” of the tear and into the vitreous base (Fig. 106.3).26 However, even optimal therapy may be unsuccessful because of extension of subretinal fluid before an effective chorioretinal adhesion develops. This may be more common following cryotherapy than after laser photocoagulation, because the adhesion forms more quickly after application of the latter method.60
Lattice degeneration
There are many difficulties in analyzing results of treatment of lattice degeneration, as mentioned earlier. Results of one study of fellow eyes are listed in Table 106.3. Most new tears following therapy occur in areas not previously treated.
Patients with previous retinal detachment in the fellow eye
Fellow eyes of patients with retinal detachment in a first eye have a substantial risk of retinal detachment, and the risk is even higher after cataract extraction. Smiddy et al.58 demonstrated that aphakia and pseudophakia are statistically significant risk factors for failure after prophylactic therapy for retinal breaks. Results of treatment of aphakic fellow eyes in one report are listed in Table 106.4. It is important to note that treatment of the visible lesions in untreated eyes would have prevented few retinal detachments.51
Complications of prophylactic treatment
Complications of preventive therapy include failure to prevent retinal detachment, iatrogenic problems increasing the risk of retinal detachment, and other problems caused by treatment, and they have been reviewed in detail elsewhere.27 Retinal detachments that occur despite prophylactic therapy are a result of either an inadequate adhesion around a retinal break or a new retinal break. Extension of the detachment is considered a complication of therapy if the treatment is inadequate in extent or intensity, and a particularly common cause of failure in treating horseshoe-shaped tears is an absence of an adequate chorioretinal adhesion surrounding the anterior margins of the break, where vitreoretinal traction persists.26 New retinal breaks are a complication of prophylactic therapy if the treatment causes excessive damage to the retina, resulting in a break at that location, or if it aggravates vitreous degenerative changes and vitreoretinal traction, causing a tear elsewhere.
Epiretinal proliferation that causes macular pucker has been considered an important complication of prophylactic therapy, but the association between treatment and membrane formation is uncertain. Symptomatic retinal tears are almost always due to a posterior vitreous detachment, and a PVD is present in more than 90% of eyes with idiopathic epimacular proliferation.15 Also, when vitreoretinal traction causes a retinal tear, pigment epithelial cells are usually liberated into the vitreous cavity, and these may be a source of subsequent epimacular proliferation. The method of creating a chorioretinal adhesion appears to be unrelated to the incidence of postoperative macular pucker.61
1 Comer MB, Newman DK, George ND, et al. Who should manage primary retinal detachments? Eye. 2000;14:572–578.
2 Minihan M, Tanner V, Williamson TH. Primary retinal detachment: 20 years of change. Br J Ophthalmol. 2001;85:546–548.
3 Thompson JA, Snead MP, Billington BM, et al. National audit of the outcome of primary surgery for rhegmatogenous retinal detachment. II. Clinical outcomes. Eye. 2002;16:771–777.
4 Asaria RH, Gregor ZJ. Simple retinal detachments: identifying the at-risk case. Eye. 2002;16:404–410.
5 Wilkinson CP, Rice TA. Michels retinal detachment, 2nd ed. St Louis: Mosby; 1997. p. 935–77
6 Byer NE. Rethinking prophylactic therapy of retinal detachment. In: Stirpe M, ed. Advances in vitreoretinal surgery. New York: Ophthalmic Communications Society; 1992:399–411.
7 Wilkinson CP. Interventions for asymptomatic retinal breaks and lattice degeneration for preventing retinal detachment. Cochrane Database Syst Rev. 1, 2005. CD003170
8 Kreis AJ, Aylward GW, Wolfensberger TJ. Prophylaxis for retinal detachment. Evidence or eminence based? Retina. 2007;27:466–472.
9 Javitt JC, Tielsch JM, Canner JK, et al. National outcomes of cataract extraction: increased risk of retinal complications associated with Nd:YAG laser capsulotomy. Ophthalmology. 1992;99:1487–1498.
10 Tielsch JM, Legro MW, Cassard SD, et al. Risk factors for retinal detachment after cataract surgery: a population-based case-control study. Ophthalmology. 1996;103:1537–1545.
11 Freeman HM. Fellow eye of nontraumatic giant retinal tears. In: Lewis H, Ryan SJ. Medical and surgical retina. St Louis: Mosby; 1994:222–225.
12 Arroyo JG, Postel EA, Stone T, et al. A matched study of primary buckle placement during repair of posterior segment open globe injuries. Br J Ophthalmol. 2003;87:75–78.
13 Robertson DM, Priluck IA. 360-degree prophylactic cryo-retinopexy: a clinical and experimental study. Arch Ophthalmol. 1979;97:2130–2134.
14 Hovland KR. Vitreous findings in fellow eyes of aphakic retinal detachment. Am J Ophthalmol. 1978;86:350–353.
15 Sebag J. Myopia effects upon vitreous-significance in retinal detachments. In: Stirpe M, ed. Anterior and posterior segment surgery: mutual problems and common interests. New York: Ophthalmic Communications Society, 1998.
16 Brod RD, Lightman DA, Packer AJ, et al. Correlation between vitreous pigment granules and retinal breaks in eyes with acute posterior vitreous detachment. Ophthalmology. 1991;98:1366–1369.
17 Byer NE. Natural history of posterior vitreous detachment with early management as the premier line of defense against retinal detachment. Ophthalmology. 1994;101:1503–1513.
18 Tasman WS. Posterior vitreous detachment and peripheral retinal breaks. Trans Am Acad Ophthalmol Otolaryngol. 1968;72:217–224.
19 Tanner V, Harle D, Tan J, et al. Acute posterior vitreous detachment: the predictive value of vitreous pigment and symptomatology. Br J Ophthalmol. 2000;84:1264–1268.
20 Shea M, Davis MD, Kamel I. Retinal breaks without detachment, treated and untreated. Mod Probl Ophthalmol. 1974;12:97–102.
21 Verdaguer JT, Vaismon M. Treatment of symptomatic retinal breaks. Am J Ophthalmol. 1979;87:783–788.
22 Pollack A, Oliver M. Argon photocoagulation of symptomatic flap tears and retinal breaks of fellow eyes. Br J Ophthalmol. 1981;65:469–472.
23 Colyear BH, Pischel DK. Preventative treatment of retinal detachment by means of light coagulation. Trans Pac Coast Oto-Ophthalmol Soc. 1960;41:193–215.
24 Robertson DM, Norton EWD. Long-term follow-up of treated retinal breaks. Am J Ophthalmol. 1973;75:393–404.
25 Davis MD. The natural history of retinal breaks without detachment. Trans Am Ophthalmol Soc. 1973;71:343–372.
26 American Academy of Ophthalmology. Management of posterior vitreous detachment, retinal breaks, and lattice degeneration. Preferred practice pattern. San Francisco: American Academy of Ophthalmology; 1998.
27 Wilkinson CP, Rice TA. Michels retinal detachment, 2nd ed. St Louis: Mosby; 1997. p. 1081–133
28 Byer NE. Long-term natural history of lattice degeneration of the retina. Ophthalmology. 1989;96:1396–1401.
29 Burton TC. The influence of refractive error and lattice degeneration on the incidence of retinal detachment. Trans Am Ophthalmol Soc. 1989;87:143–155.
30 Stirpe M, Heimann K. Vitreous changes and retinal detachment in highly myopic eyes. Eur J Ophthalmol. 1996;6:50–58.
31 Byer NE. Cystic retinal tufts and their relationship to retinal detachment. Arch Ophthalmol. 1981;99:1788–1790.
32 Byer NE. Posterior vitreous detachment as a risk factor for retinal detachment. Ophthalmology. 1995;102:528–532.
33 Byer NE. Long-term natural history study of senile retinoschisis with implications for management. Ophthalmology. 1986;93:1127–1137.
34 Hagler WS, Waldoff HS. Retinal detachment in relation to senile retinoschisis. Trans Am Acad Ophthalmol Otolaryngol. 1973;77:99–111.
35 Byer NE. What happens to untreated asymptomatic retinal breaks and are they affected by posterior vitreous detachment? Ophthalmology. 1998;105:1045–1049.
36 Sigelman J. Vitreous base classification of retinal tears: clinical application. Surv Ophthalmol. 1980;25:59–74.
37 The Eye Disease Case–Control Study Group. Risk factors for idiopathic rhegmatogenous retinal detachment. Am J Epidemiol. 1993;137:749–757.
38 Folk JC, Arrindell EL, Klugman MR. The fellow eye of patients with phakic lattice retinal detachment. Ophthalmology. 1989;96:72–79.
39 Norregaard JC, Thoning H, Andersen TF, et al. Risk of retinal detachment following cataract extraction: results from the International Cataract Surgery Outcomes Study. Br J Ophthalmol. 1996;80:689–693.
40 Friedman Z, Neumann E, Hyams SW. Vitreous and peripheral retina in aphakia: a study of 200 non-myopic aphakic eyes. Br J Ophthalmol. 1973;57:52–57.
41 Hyams SW, Neumann E, Friedman Z. Myopia-aphakia. II. Vitreous and peripheral retina. Br J Ophthalmol. 1975;59:483–485.
42 Folk JC, Bennet SR, Klugman MR, et al. Prophylactic treatment to the fellow eye of patients with phakic lattice retinal detachment: analysis of failures and risks of treatment. Retina. 1990;10:165–169.
43 Haut J, Ladjimi A, Van Effenterre G, et al. Preventative treatment of retinal detachment of the contralateral eye: results of 5 years of follow-up of 109 eyes. J Fr Ophtalmol. 1991;14:397–404.
44 Monin C, Van Effenterre G, Andre-Sereys P, et al. Prevention of retinal detachment in Wagner-Stickler disease: comparative study of different methods. J Fr Ophtalmol. 1994;17:167–174.
45 Merin S, Feiler V, Hyams S, et al. The fate of the fellow eye in retinal detachment. Am J Ophthalmol. 1971;71:477–481.
46 Michaelson IC, Stein R, Neumann E, et al. A national cooperative study in the prevention of retinal detachment. In: Pruett RC, Regan CD. Retina congress. New York: Appleton-Century-Crofts, 1974.
47 Wolfensberger TJ, Aylward GW, Leaver PK. Prophylactic 360 degree cryotherapy in fellow eyes of patients with spontaneous giant retinal tears. Ophthalmology. 2003;110:1175–1177.
48 Ang A, Poulsob AV, Goodburn SF, et al. Retinal detachment and prophylaxis in type 1 Stickler syndrome. Ophthalmology. 2008;115:164–168.
49 Aylward GW, daCruz L, Sullivan P, et al. Stickler syndrome. Ophthalmology. 2008;115:1636–1637.
50 Ang GS, Townsend J, Lois N. Interventions for prevention of giant retinal tear in the fellow eye. Cochrane Database Syst Rev. 2, 2009. CD006909
51 Benson WE, Grand MG, Okun E. Aphakic retinal detachment: management of the fellow eye. Arch Ophthalmol. 1975;93:245–249.
52 Le Mesurier R, Chignell AH. Prophylaxis of aphakic retinal detachment. Trans Ophthalmol Soc UK. 1981;101:212–213.
53 Hudson JR, Kanski JJ. Prevention of aphakic retinal detachment by circumferential cryotherapy. Mod Probl Ophthalmol. 1977;18:530–537.
54 Laidlaw DA, Karia N, Bunce C, et al. Is prophylactic 360-degree laser retinopexy protective? Risk factors for retinal detachment after removal of silicone oil. Ophthalmology. 2002;109:153–158.
55 Avitabile T, Longo A, Lentmig G, et al. Retinal detachment after silicone oil removal is prevented by 360 degrees laser treatment. Br J Ophthalmol. 2008;92:1479–1482.
56 Koh HK, Cheng L, Kosobucki B, et al. Prophylactic intraoperative 360 degree laser retinopexy for prevention of retinal detachment. Retina. 2007;27:744–749.
57 Tornambe PE. Pneumatic retinopexy: the evolution of case selection and surgical technique. A twelve-year study of 302 eyes. Trans Am Ophthalmol Soc. 1997;95:551–578.
58 Smiddy WE, Flynn HW, Nicholson DH, et al. Results and complications in treated retinal breaks. Am J Ophthalmol. 1991;112:623–631.
59 Mastropasqua L, Carpineto P, Ciancaglini M, et al. Treatment of retinal tears and lattice degeneration in fellow eyes in high risk patients suffering retinal detachment: a prospective study. Br J Ophthalmol. 1999;83:1046–1049.
60 Folk JC, Sneed SR, Folberg R, et al. Early retinal adhesion from laser photocoagulation. Ophthalmology. 1989;96:1523–1525.
61 Saran BR, Brucker AJ. Macular epiretinal membrane formation and treated retinal breaks. Am J Ophthalmol. 1995;120:480–485.