CHAPTER 1 Preoperative and Intraoperative Care
PREOPERATIVE CARE
Preoperative Evaluation
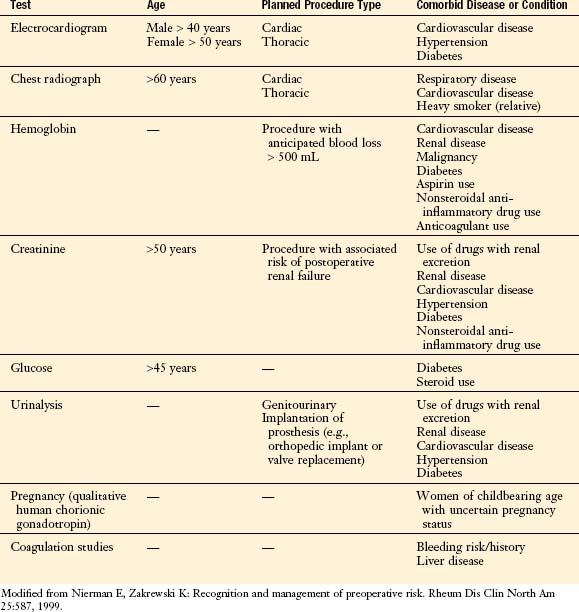
All patients undergo a general evaluation before elective surgery, the primary aim of which is to identify and quantify comorbidities that may influence surgical outcomes. The scope of this evaluation is dictated by a number of factors, including patient age and medical history and the risks associated with the planned procedure. Frequently ordered preoperative tests include: an ECG; a chest radiograph; hemoglobin, creatinine, and glucose levels; a urinalysis; a pregnancy test; and coagulation studies. Not all of these are essential in all cases and some recommendations regarding their use are detailed in Table 1-1.
Additional Considerations
Preparation for Surgery
| Category | Definition | Risk of Infection |
|---|---|---|
| Clean (class I) | Respiratory, gastrointestinal, or genitourinary tract not entered | 1%–3% |
| Clean-contaminated (class II) | Gastrointestinal or respiratory tract entered without significant spillage | 5%–8% |
| Contaminated (class III) | Spillage from gastrointestinal tract or entrance into genitourinary or biliary tract in the presence of infected urine or bile Fresh traumatic wound |
20%–25% |
| Dirty (class IV) | Acute bacterial infection encountered, delayed treatment of a traumatic wound Traumatic wound with retained devitalized tissue, foreign body, or fecal contamination |
30%–40% |
INTRAOPERATIVE CONSIDERATIONS
Anesthesia
Airway
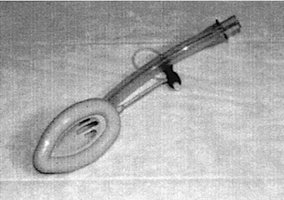
Airway management is a critical component of all anesthetic approaches. Deep sedation and the use of paralytics in conjunction with general anesthesia require ventilatory support. Endotracheal (ET) intubation is the most common method of securing the airway. ET tubes are inserted beyond the vocal cords and are equipped with a distal cuff. Inflation of the cuff protects against aspiration of gastrointestinal secretions and provides a seal to allow for ventilation. In contrast, laryngeal mask airways (LMAs) are equipped with a cuff that fits over the glottic opening (Fig. 1-2). LMAs are an alternative to ET tubes and are particularly useful for shorter procedures involving deep sedation. Because LMAs are more easily displaced and provide less protection against aspiration than do ET tubes, they should not be used for long procedures in which ventilatory support is necessary.
Fleisher LA, Beckman JA, Brown KA, et al. ACC/AHA 2007 Guidelines on Perioperative Cardiovascular Evaluation and Care for Noncardiac Surgery: A Report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines [[Writing Committee to Revise the 2002 Guidelines on Perioperative Cardiovascular Evaluation for Noncardiac Surgery]. Circulation. 2007;116:e418-e499.
Marino PL. The ICU Book, 3rd ed. Philadelphia: Lippincott Williams & Wilkins; 2007.
Nierman E, Zakrewski K. Recognition and management of preoperative risk. Rheum Dis Clin North Am. 1999;25:587.
Weintraub SL, Wang Y, Hunt JP, O’Leary JP. Principles of preoperative and operative surgery. In: Townsend CM, editor. Sabiston Textbook of Surgery: The Biologic Basis of Modern Surgical Practice. 17th ed. Philadelphia: Saunders; 2004:221-241.