CHAPTER 19 Adrenalectomy
Case Study
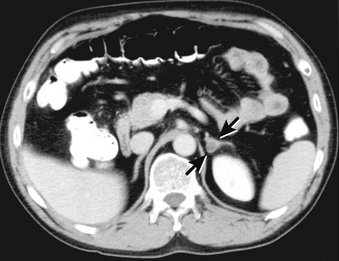
She undergoes laboratory testing, which reveals a serum potassium level of 3.1 mEq/L, a serum renin level of 1.31 ng/mL/hr (normal range, 0.15–3.39 ng/mL/hr), and a serum aldosterone level of 82 ng/dL (normal range, 1–16 ng/dL). A computed tomography (CT) scan of the abdomen shows a 2-cm left adrenal mass and a normal-appearing right adrenal gland (Fig. 19-1).
BACKGROUND
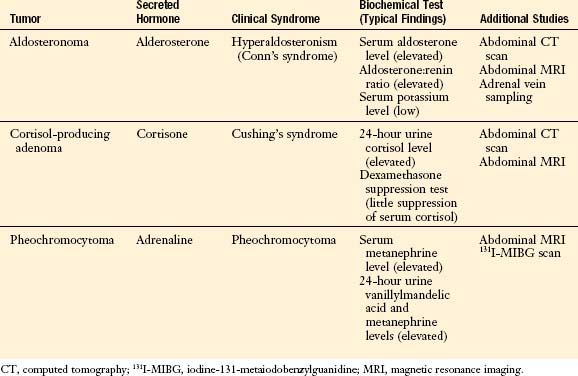
Tumors arising within the adrenal gland are broadly categorized as either functioning or nonfunctioning. The former secrete one of a number of hormones (Table 19-1). The indications for adrenalectomy, the subject of this chapter, include the treatment of functioning adrenal tumors, suspected primary adrenal malignancies, and in select cases, isolated metastases from extra-adrenal malignancies.
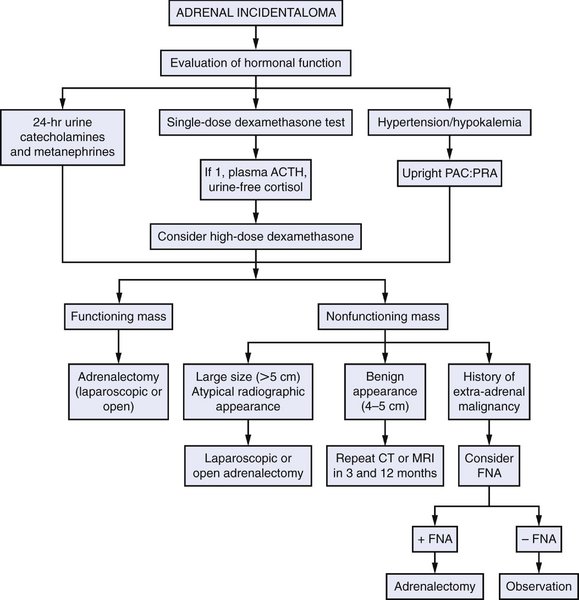
INDICATIONS FOR ADRENALECTOMY
PREOPERATIVE EVALUATION
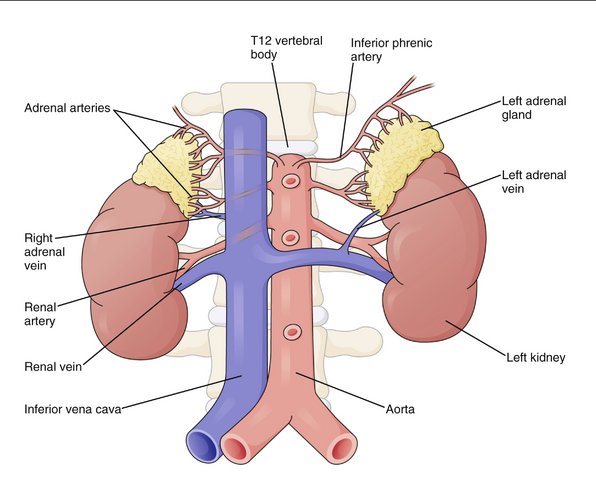
COMPONENTS OF THE PROCEDURE AND APPLIED ANATOMY
Preoperative Considerations
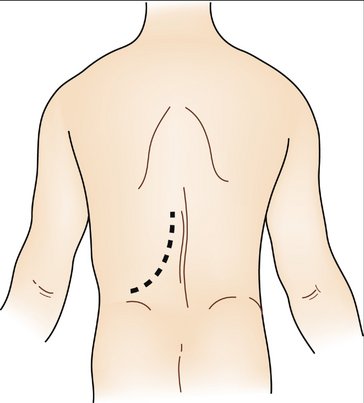
Patient Positioning and Preparation
Port Placement
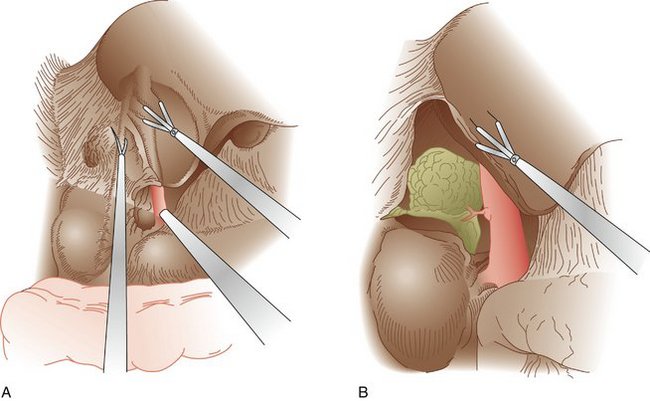
Right Adrenalectomy
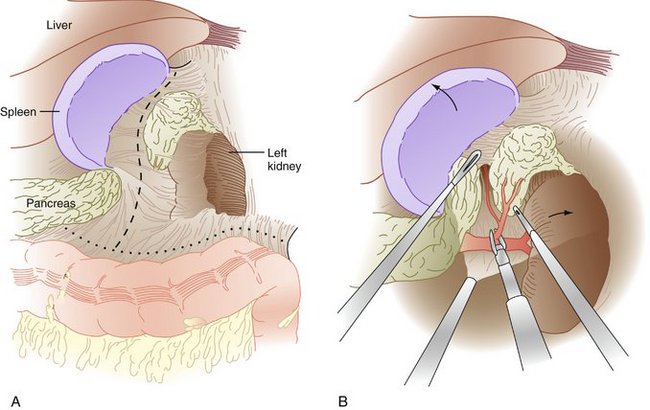
Left Adrenalectomy
Other Operative Approaches
Additional Operative Considerations
NORMAL POSTOPERATIVE COURSE
Additional Postoperative Considerations
Complications
Brunt LM. Minimal access adrenal surgery. Surg Endosc. 2006;20:351-361.
Cobb WS, Kercher KW, Sing RF, Heniford BT. Laparoscopic adrenalectomy for malignancy. Am J Surg. 2005;189:405-411.
Gumbs AA, Gagner M. Laparoscopic adrenalectomy. Best Pract Res Clin Endocrinol Metab. 2006;20:483-499.
Mitchell IC, Nwariaku FE. Adrenal masses in the cancer patient: surveillance or excision. Oncologist. 2007;12:168-174.