2. Prenatal Environment
Effect on Neonatal Outcome *
*Please note that the PURPLE type in each chapter is intended to make it easier to identify clinically applicable material.
Priscilla M. Nodine, Jaime Arruda and Marie Hastings-Tolsma
The human fetus develops within a complex maternal environment. Structurally defined by the intrauterine/intraamniotic compartment, the character of the prenatal environment is determined largely by maternal variables. The fetus depends totally on the maternal host for respiratory and nutritive support and is significantly influenced by maternal metabolic, cardiovascular, and environmental factors. In addition, the fetus is limited in its ability to adapt to stress or modify its surroundings. This creates a situation in which the prenatal environment exerts a tremendous influence on fetal development and well-being. This influence lasts well beyond the period of gestation, often affecting the newborn in ways that have profound significance for both immediate and long-term outcome.
There is great utility in identifying maternal factors that adversely affect the condition of the fetus. Providers of obstetric care have long used this information to identify the “at-risk” population and design interventions that prevent or reduce the occurrence of fetal and neonatal complications. It is equally important that neonatal care providers obtain a clear picture of the prenatal environment and use this information before birth to anticipate the newborn’s immediate needs and make appropriate preparations for resuscitation and initial nursery care. After birth, an awareness of the likely sequelae of environmental compromise helps focus ongoing assessment and aids in clinical problem solving.
The purpose of this chapter is to help neonatal care providers evaluate maternal influences on the prenatal environment, identify significant environmental risk factors, and anticipate the associated neonatal problems. Information on the assessment and treatment of specific neonatal problems is provided throughout this text and is not repeated here. For a more extensive discussion of perinatal physiology and complicated pregnancies, refer to the references cited at the end of this chapter.
PHYSIOLOGY
Two variables have a critical influence on fetal well-being throughout gestation: utero-placental functioning and inherent maternal resources. The interplay of these factors is a major determinant of fetal oxygenation, metabolism, and growth. Alterations in the development and function of the placenta also influence fetal growth and development. The fetus may be affected to the point that survival is threatened. Likewise, extrauterine well-being may be compromised.
The placenta has a dual role in providing nutrients and metabolic fuels to the fetus. First, placental secretion of endocrine hormones, chiefly human chorionic somatomammotropin (HCS), increases throughout pregnancy, causing progressive changes in maternal metabolism. The net effect of these changes is an increase in maternal glucose and amino acids available to the fetus, especially in the second half of pregnancy. Second, the placenta is instrumental in the transfer of these (and other) essential nutrients from the maternal to the fetal circulation and, conversely, of metabolic wastes from the fetal to the maternal system. Adequate maternal and fetal blood flow through the placenta is essential throughout the entire pregnancy.
Fetal respiration also depends on adequate placental function. Respiratory gases (oxygen and carbon dioxide) readily cross the placental membrane by simple diffusion, with the rate of diffusion determined by the P o2 (or P co2) differential between maternal and fetal blood.
Although the placenta mediates the transport of respiratory gases, carbohydrates, lipids, vitamins, minerals, and amino acids, the maternal reservoir is their source. Maternal-fetal transfer depends on the characteristics and absolute content of substances within the maternal circulation, the relative efficiency of the maternal cardiovascular system in perfusing the placenta, and the function of the placenta itself. 155 The fetal environment can be disrupted by inappropriate types or amounts of substances (e.g., ethanol) in the maternal circulation, decreases or interruptions in placental blood flow (e.g., placental abruption), or abnormalities in placental function (e.g., small placenta). Maternal nutrition, exercise, and disease can impair placental uptake and transfer of substances across the placenta to the fetus.
COMPROMISED FETAL ENVIRONMENT
Maternal Disease
DIABETES
The prevalence of diabetes mellitus and gestational diabetes mellitus (GDM) is increasing worldwide. Diabetes is the most common endocrine disorder affecting pregnancy, and approximately 2% to 7% of pregnant women in the United States are diagnosed with GDM annually. 32 Despite major reductions in mortality over the past several decades, the infant of a diabetic mother (IDM) continues to have a considerable perinatal disadvantage. The physiologic changes in maternal glucose use that accompany pregnancy, coupled with either a preexisting hyperglycemia (as found in types 1 and 2 diabetes) or an inability to mount an appropriate insulin response (as seen in patients with gestational diabetes) result in a significantly abnormal fetal environment. This is because of the increased level of maternal glucose, often in concert with episodic hypoglycemia and ketone exposure. Early in pregnancy, this environment may have a teratogenic effect on the embryo, accounting for the dramatic increase in spontaneous abortions and congenital malformations in the offspring of diabetic women with poor metabolic control. 8 During the second and third trimesters, the mechanics of placental transport dictate that fetal glucose levels depend on, but are slightly less than, maternal levels. 126 Assuming adequate placental function and perfusion, elevations in maternal glucose lead to fetal hyperglycemia and increased fetal insulin production. Repeated or continued elevations in blood glucose result in fetal hyperinsulinism, alterations in the use of glucose and other nutrients, and altered patterns of growth and development. 8,126
Fetal macrosomia (greater than the 90th percentile for weight) occurs in 25% to 42% of diabetic pregnancies because of hyperinsulinemia. These macrosomic infants suffer increased morbidity and mortality from unexplained death in utero, birth trauma, hypertrophic cardiomyopathy, vascular thrombosis, neonatal hypoglycemia, hyperbilirubinemia, erythrocytosis, and respiratory distress. 93 Macrosomic infants have double the risk for shoulder dystocia during vaginal birth and are at greater risk for death during the last 4 to 6 weeks of gestation. 170 Brachial plexus injury and facial nerve palsy also can result from shoulder dystocia. 72 Finally, macrosomic infants are at higher risk for dysfunctional labor patterns and operative vaginal deliveries, which can also contribute to their higher rate of birth trauma.
In addition to the basic metabolic disturbances, diabetes predisposes the pregnant woman to several other complications, including gestational hypertension, preeclampsia, renal disease, and vascular disease. 8 As a consequence, the fetus may be compromised further by chronic hypoxia and other insults, which can lead to intrauterine demise, prematurity, growth restriction, cardiovascular problems, respiratory distress syndrome (RDS), and long-term neurologic problems. 37 In terms of predicting perinatal morbidity and mortality, the “prognostically bad signs of pregnancy,” first identified by Pedersen in the 1960s, are especially significant. The occurrence of any of these signs, which include diabetic ketoacidosis, hypertension, pyelonephritis, and maternal noncompliance, continue to be useful predictors of increased fetal and neonatal risk. 46
In preparing for the delivery of an IDM, the neonatal team should consider the classification of maternal diabetes (type 1 or 2, or gestational). In addition, the quality of metabolic control throughout the pregnancy and labor, maternal complications, and the duration of the pregnancy should be considered, along with indicators of fetal growth and well-being. In cases in which the newer generation sulfonylurea (i.e., glyburide) has been used, an increased incidence of neonatal jaundice may be anticipated.77
THYROID DISEASE
Thyroid disorders are the second most common endocrine disorder seen in pregnancy. 9 The thyroid hormones triiodothyronine (T 3) and thyroxine (T 4) cross the placenta in small amounts, though the significance of the transfer has not been well elucidated. The fetus depends on maternal T 4 in the first trimester of pregnancy. At 8 to 10 weeks’ gestation, the fetal thyroid begins to concentrate iodine and produce T 4. During the second and third trimester, the fetus is independent of maternal status. At approximately 24 weeks, thyroid-stimulating immunoglobulins (TSIs) or thyroid-stimulating hormone (TSH) receptor Abs, which are classes of immunoglobulin G (IgG), cross the placenta and stimulate fetal thyroid. Iodine is readily transferred from mother to fetus. The fetal thyroid gland concentrates iodine and synthesizes its own hormones as early as 10 to 12 weeks’ gestation; this is independent of maternal thyroid function. Maternal thyroid hormones are believed to be important for fetal neurologic development in the first trimester. 3 Significant decreases in intelligence quotient (IQ) of offspring of mothers with untreated hypothyroidism in early gestation have been shown in some studies. 70,96 Whereas subclinical hypothyroidism does not need to be treated, 26 severe maternal hypothyroidism may result in increased neurodevelopmental delay in offspring, pregnancy loss, prematurity, preeclampsia, low birth weight, and abruptio placenta. 25 Treatment with replacement hormone during pregnancy is well tolerated by the fetus and reduces these risks. 3
Maternal hyperthyroidism presents a different situation. Thyroid-stimulating antibodies, commonly found in patients with Graves’ disease, as well as many of the drugs used to treat hyperthyroidism, cross the placenta and can have a significant effect on the fetus. Antibodies, including long-acting thyroid stimulant (LATS) and TSI, can increase fetal thyroid hormone production. High levels are associated with fetal and neonatal hyperthyroidism. Untreated maternal thyrotoxicosis has been linked to preterm delivery, intrauterine growth restriction (IUGR), low birth weight, and stillbirth. In rare cases, the offspring of women with Graves’ disease may themselves have this condition. In fetuses and newborns, this is evidenced by elevations in heart rate, growth restriction, prematurity, goiter, and congestive heart failure. The perinatal mortality rate is high. 26 Administration of antithyroid medication to the mother can decrease thyroid hormone production in both the mother and the fetus but may result in fetal hypothyroidism and goiter. 1
Another maternal antibody, TSH-binding inhibitor immunoglobulin, also crosses the placenta and can prevent the expected fetal thyroid response to TSH. The result is a transient fetal and neonatal hypothyroidism. Iodine deficiency in the mother is another cause of fetal and neonatal hypothyroidism and, in its severe form, leads to cretinism because of the fetus’s dependence on maternal iodine reserves. 1
PHENYLKETONURIA
Phenylketonuria (PKU) is an inherited disorder in which an enzymatic defect precludes conversion of the essential amino acid phenylalanine to tyrosine. This metabolic derangement is evidenced by an accumulation of excessive amounts of phenylalanine and alternative pathway by-products in the blood, and these are toxic to the central nervous system. Historically, PKU resulted in virtually certain mental retardation; affected individuals often were institutionalized and rarely reproduced. With the advent of universal neonatal screening in the United States since the 1960s and effective dietary treatment to prevent hyperphenylalaninemia during infancy and early childhood, genetically affected persons may avoid the devastating effects of this disease, have relatively normal development, and become pregnant. For women who do conceive, PKU poses a significant environmental risk for their developing fetus. The care of these women and their infants presents a unique perinatal challenge.
An estimated 3000 healthy young women of childbearing age with successfully treated PKU are in the United States. 104 However, most discontinued their special diet in childhood because, at the time, most doctors believed it was safe to do so. Unfortunately, their blood phenylalanine levels are very high when they become pregnant if they are eating a normal diet. In up to 90% of such cases, the offspring will be microcephalic and/or have mental retardation. These babies also have an increased incidence of low birth weight, cardiac defects, and characteristic facial features regardless of whether they are themselves affected with PKU. 97,98 They cannot be helped by the PKU diet, or they suffer from brain damage caused entirely by their mothers’ high phenylalanine levels during pregnancy. To prevent such damage, these women should resume their special PKU diets during preconception. Studies have identified improved long-term outcomes when desirable phenylalanine levels (2 to 8 mg/dL) are achieved at least 3 months before pregnancy and maintained throughout gestation. 102 Phenylalanine levels drop quickly once dietary restrictions are instituted, and there is a strong correlation between maternal blood levels and neonatal outcome. 102
About 1 baby in 14,000 inherits PKU when both parents have the PKU gene and both pass it on to their baby. Neonatal blood screening will identify these PKU babies. If this screening is performed within the first 24 hours of life, the American Academy of Pediatrics recommends re-screening at 1 to 2 weeks of age to avoid missed cases of PKU. Once identified, PKU babies should be fed a special formula that contains protein but no phenylalanine, started within the first 7 to 10 days of life, and they must remain on an individualized, restricted diet throughout childhood/adolescence, and generally for life. In some instances, breastfeeding may be possible. 88 When treatment is discontinued too soon, risks include blindness, learning disabilities, behavioral disturbances, and a decrease in IQ. When no treatment is instituted at all, phenylalanine accumulates in the bloodstream and causes brain damage and mental retardation.
RENAL DISEASE
Maternal adaptation to pregnancy involves major changes in renal function and structure. Renal hemodynamic changes begin early in pregnancy and before significant expansion of plasma volume. Renal blood flow increases in the first trimester by 35% to 60% and then decreases from the second trimester to term. Additional changes include an increase in the glomerular filtration rate (GFR) and effective renal plasma flow, a decrease in renal vascular resistance, an activation of the renin-angiotensin-aldosterone system, and increased retention of sodium and water. These changes place unique demands on the renal system. Women with preexisting renal disease may have a successful pregnancy outcome with proper prenatal care; however, some women do experience fetal loss and deterioration in renal function. Furthermore, moderate or severe renal dysfunction complicates pregnancy and increases maternal and fetal risks and adverse outcomes. 16
Renal disease in pregnancy may occur as a result of urinary tract infections, glomerular disease, or severe hypertension or as a complication of systemic diseases including diabetes and systemic lupus erythematosus. 84 Regardless of the underlying etiologic factors, pregnancy outcome relates most closely to these factors: the presence of hypertension and the degree of renal insufficiency before and during pregnancy. 84 Many women with renal disorders are hypertensive before pregnancy, and they often develop a superimposed pregnancy-induced hypertension leading to preeclampsia. 83 Even those with previously normal blood pressures run an increased risk for developing hypertension during pregnancy. The presence of hypertension in these pregnancies represents a significant risk to the fetus and is strongly associated with IUGR, preterm delivery, and perinatal loss.
Drug therapy to control chronic hypertension has been shown to have a beneficial effect on fetal outcome and generally is continued throughout pregnancy. Renal insufficiency, as measured by creatinine clearance or serum creatinine level, also has implications for fetal outcome. Mild to moderate renal insufficiency (serum creatinine less than 1.5 mg/dL) is associated with a generally favorable outcome, whereas severe insufficiency (serum creatinine greater than 1.6 mg/dL) often carries an increased risk for perinatal death. Persistent proteinuria also may increase fetal loss, and a urinary protein excretion rate higher than 0.5 g/24 hr may be an independent predictor of fetal outcome. 112 As a rule, the number of preterm deliveries and growth-restricted infants increases with increasing blood pressure and decreasing renal function.
Bacteriuria occurs in 2% to 7% of pregnancies. If untreated, asymptomatic bacteriuria may lead to pyelonephritis or acute cystitis. Risks for the fetus are preterm birth and IUGR. Fetal death is an additional risk with pyelonephritis. Prophylactic antibiotics (suppressive therapy) should be given to women with persistent or frequent recurrence of bacteriuria or a history of pyelonephritis in pregnancy. 147
Two special circumstances are dialysis during pregnancy and pregnancy after renal transplant. Women undergoing dialysis rarely become pregnant. When pregnancy does occur, it is associated with significant perinatal morbidity and mortality, with spontaneous abortions reaching 50%. Hemodialysis also is associated with numerous complications, including placental abruption, polyhydramnios, IUGR, preterm labor, and pregnancy loss. 56,106 The risk may be lower with ambulatory peritoneal dialysis. 56 Pregnancy after transplantation is more common and has a better prognosis than pregnancy managed by dialysis. 84 A long interval from transplantation to conception and use of a low dose of prednisone are predictive of successful outcome. 16Infants born after maternal transplantation are commonly preterm. A wide range of perinatal problems have been noted, thus requiring specialized care at a tertiary center. Other complications may include growth restriction, RDS, congenital anomalies, adrenocortical insufficiency, hyperviscosity, seizures, and neonatal sepsis.66 Concerns persist about neonatal complications if exposure to immunosuppressive therapy occurred while in utero. The criteria used to predict fetal outcome with other renal patients (i.e., hypertension, renal insufficiency) also have predictive value in post-transplantation pregnancies. Acute renal failure in pregnancy is associated with a maternal mortality rate of 20% and an increased fetal mortality rate. 80
NEUROLOGIC DISORDERS
The risks that accompany pregnancies complicated by maternal neurologic disorders vary according to the individual disease entity and pertain to both the course of the mother’s disease and pregnancy outcome. The physiologic and hormonal changes of pregnancy can influence the course of chronic neuromuscular disorders, such as epilepsy, multiple sclerosis, and myasthenia gravis. The medications used to control these disorders can be particularly problematic for the fetus.
The prevalence of maternal seizure disorders is about 4 in every 1000 pregnancies, and most are treated with antiepileptic drugs (AEDs). The disorders and/or the AEDs have been associated with increased fetal and neonatal risks, including spontaneous abortion, prematurity, small for gestational age, congenital defects, intrauterine demise, neonatal depression, and hemorrhage. Significant numbers of epileptic women experience an increase in seizure activity during pregnancy. This is probably because of decreased compliance with medication regimens, physiologic changes associated with pregnancy, and gestational changes in plasma levels of anticonvulsant drugs. 91,108 There is evidence that maternal seizures may compromise fetal oxygenation, possibly because of diminished placental blood flow or maternal hypoxemia resulting from post-seizure apnea. For these reasons, control of maternal seizure activity with anticonvulsants is one of the primary goals of prenatal care.
Placental transport of anticonvulsants does occur, resulting in fetal levels that approximate or, in some cases, exceed maternal levels. 21 Although the majority of infants born to women with epilepsy are normal, these infants are at increased risk for poor outcomes. 153Many studies have demonstrated an increased incidence of congenital defects in the offspring of epileptic women treated with anticonvulsants. Estimates of risks vary, but studies report a 21/2-fold increased risk over the general population when AED monotherapy is used and a 5-fold increased risk when multiple AEDs are used during pregnancy.108,110 The teratogenic potential of most individual AEDs remains unclear, but valproate seems to be consistently associated with the highest rates of congenital malformations and the use of other AEDs is recommended if possible during pregnancy. 20,160 Although many newer AEDs are listed as class B medications in pregnancy, reports of teratogenicity are just now surfacing, so caution should be used with all anticonvulsants. 53,75The most common major congenital malformations associated with AEDs are neural tube defects (e.g., spina bifida), orofacial defects (e.g., cleft lip, cleft palate), heart malformations (e.g., ventricular septal defect), urogenital defects (e.g., hypospadias), and skeletal abnormalities (e.g., radial ray defects, phalangeal hypoplasias).107 The influence of the seizure disorder itself, as well as genetic makeup, cannot be ignored. Maternal folic acid supplementation has been shown to improve pregnancy outcomes for women taking AEDs. 130,160
Infants born to mothers treated with anticonvulsants, especially barbiturates, may exhibit signs of generalized depression, including decreased respiratory effort, poor muscle tone, and feeding difficulties. They also may have symptoms indicative of drug withdrawal (seeChapter 11). These symptoms are usually present in the first week of life and include tremors, restlessness, hypertonia, and hyperventilation.21In addition, abnormal clotting and hemorrhage in the offspring of women treated with phenytoin, phenobarbital, and primidone have been reported. This appears to be caused by a decrease in vitamin K–dependent clotting factors. Hemorrhage usually starts within the first 24 hours, is often severe, and may result in death. Infants born to these mothers should have cord blood clotting studies done, vitamin K prophylaxis on admission to the nursery, and close observation. Reports of long-term sequelae for the infants of epileptic mothers with AED use during pregnancy, especially the third trimester, include possible cognitive and behavioral deficiencies. 107
Multiple sclerosis (MS) frequently strikes women during their reproductive years. The onset of MS usually is insidious; the course is marked by a seemingly capricious cycle of exacerbation and remission. A wide range of sensory, motor, and functional changes is associated with this disease; the type and severity of symptoms vary dramatically from one individual to another and in any one patient over time. The disease is a T-cell–mediated autoimmune disease of the central nervous system triggered by unknown exogenous agents in individuals with specific genetics. 73 Pregnancy usually is well tolerated and may be associated with MS stability or improvement. The reported effects of the disease on pregnancy outcomes, including risk for malformations, cesarean section rates, newborn birth weight, and rate of preterm delivery, are inconsistent. Some report no increase in adverse pregnancy outcomes, 114,169 whereas other groups report a higher cesarean rate as well as a greater number of low-birth-weight infants in mothers with MS. 45 Alterations in neural function, fatigue, and general weakness may play a role in pregnancy outcomes. During the postpartum period, a higher-than-expected relapse rate has been identified and is associated with hormonal changes. 52,163 However, in women with MS, the disease process itself is not a threat to fetal or neonatal well-being. The priority for neonatal care providers is to determine the extent of the mother’s disability, including her level of fatigue and her ability to care for her infant. The availability of appropriate support systems, both personal and professional, should be assessed, and needed follow-up and referrals should be made.
Even though the prognosis for these infants is excellent, some factors associated with MS are potentially problematic. Bladder dysfunction, common in women with MS, often results in urinary tract infections during pregnancy. Associated fetal and neonatal problems include preterm delivery and sepsis. Early identification and prompt treatment with appropriate antibiotics should minimize these risks. An additional area of concern is the variety of drugs administered to MS patients. Immunosuppressants are frequently used during severe exacerbations. The placental transport and fetal risk vary with the individual agent used. Prednisone and intravenous steroids generally are considered safe for use in pregnancy. 73 Azathioprine also is generally considered safe because the fetal liver lacks the enzyme that converts azathioprine to its active metabolites, thus protecting the fetus from any teratogenic effects from this drug. However, neonatal hematologic and immune impairment have been reported in some exposed infants. 60 Cyclophosphamide has been associated with skeletal defects, growth retardation, and preterm labor19 and is best avoided during pregnancy. Cyclosporine is not teratogenic; however, it may be associated with prematurity and growth restriction. Early in-utero exposure to interferon beta is controversial. 124 Other drug therapies should be evaluated carefully before use because definitive knowledge about safety in pregnancy may be lacking. 60 A final consideration is a long-term one: the incidence of MS in the offspring of a parent with the disease is 4%, compared with 0.1% in the general population. 73
Myasthenia gravis (MG) is a chronic autoimmune disease that causes neuromuscular dysfunction and is encountered rarely in pregnancy; only 1 in 20,000 pregnancies is complicated by MG. 81 Cells of the immune system make proteins called antibodies that block nerve impulses to the muscles. Antibodies to acetylcholine receptor (AchR) have been found in most affected persons. Distinguishing features include generalized weakness and muscle fatigue with activity. Persons with MG also may experience respiratory compromise and difficulty swallowing. 81 The course of MG during pregnancy is unpredictable and may vary in different pregnancies in the same woman. 59 Exacerbations occur in approximately 40% of pregnancies and remission in 30%, with the remaining 30% experiencing no change. During the first trimester and the first month postpartum, exacerbations are more likely. 81 Corticosteroids can be used to maintain the remissions of MG and should be continued on the lowest possible doses throughout the pregnancy and postpartum period. Immunosuppressive agents like methotrexate, cyclophosphamide, and mycophenolate mofetil are contraindicated in pregnancy, but azathioprine and cyclosporine A are sometimes used and plasmapheresis and intravenous immunoglobulins can be effective in the treatment of myasthenic crises during pregnancy. Instrumental delivery may be needed in the second stage as MG mothers are more likely to become exhausted. 81
Infants born to myasthenic mothers may be affected by the drug therapy and the underlying immunologic dysfunction. Increased rates of premature rupture of membranes (PROM), preterm delivery, and cesarean birth have been reported. 59An additional risk stems from transplacentally acquired antiacetylcholine receptor antibodies, which cause approximately 12% of these newborns to experience a transient, self-limited course of MG. It is difficult to predict which pregnancies will result in an affected infant, although infants born to women with very high AChR antibody titers may be at highest risk. 81Affected infants usually present at birth or within the first 24 hours of life with generalized weakness, a feeble cry, diminished suck and swallow, and a decreased respiratory effort that may require mechanical support.59Therefore plans should be made in advance for delivery of the mother with MG, and intensive care facilities for the newborn should be available immediately. Symptoms from neonatal MG generally subside within a few weeks after birth and do not recur.
MG is not a contraindication to pregnancy and can usually be managed well with relatively safe and effective therapies, including maternal rest. Standard therapies for some obstetric complications, such as preeclampsia and preterm labor, may need to be altered in women with MG. 81 Vaginal delivery is recommended if possible. Breast feeding is not contraindicated but depends on maternal medications and infant and maternal health postpartum.
SYSTEMIC LUPUS ERYTHEMATOSUS
Systemic lupus erythematosus (SLE) is an autoimmune disease that presents primarily in women of childbearing age. The pathogenesis involves the production of autoantibodies and immune complexes. The clinical effects of lupus range from mild or subclinical disease to serious illness affecting multiple organ systems. The leading causes of death are infections and renal failure. In pregnancy, SLE is associated with an increased incidence of preeclampsia, thrombotic events, spontaneous abortion, preterm delivery, IUGR, and stillbirths. 113,152 Outcome is best when infections, renal disease, and hypertension do not complicate pregnancy and when pregnancy occurs with prolonged disease remission. 49,137 Reported frequency of SLE flares in pregnancy is 15% to 60%. 2 When necessary, treatments used with pregnancies complicated by SLE include anti-inflammatory, antimalarial, immunosuppressive, and biological drugs and/or anticoagulants. 49
The neonatal manifestations of SLE are rare and are attributed to the placental transfer of maternal antibodies to the fetus. Usual findings of neonatal lupus include a transient lupus-like rash (erythematous lesions of the face, scalp, and upper thorax), thrombocytopenia, and hemolysis.2 These findings generally are transient and clear within a few months. A strong association has been established between maternal antibodies to the anti-Ro/SS-A and anti-La/SS-B antigens and congenital heart block, a rare manifestation of neonatal lupus syndrome.2 The fetal heart block may be detected with antenatal testing; some authors believe that antenatal fetal surveillance with nonstress tests should begin at 28 weeks’ gestation. Infants are treated with cardiac pacemakers after delivery; however, about one third of affected infants die within 3 years.164
HEART DISEASE
Significant changes in cardiovascular function accompany normal pregnancy. Plasma and red blood cell volumes rise, heart rate and cardiac output increase, and peripheral vascular resistance falls. These changes facilitate increased uterine blood flow, placental perfusion, and fetal oxygenation and growth. They also increase maternal oxygen consumption and cardiovascular workload and can further compromise the cardiovascular status of women with preexisting serious heart disease. Approximately 2% to 4% of childbearing-age women have concomitant heart disease. 86 Pregnancy creates a risk for maternal cardiovascular complications, but especially for those with underlying heart disease, and includes an increased incidence of thromboembolism and sudden death. 85,146 In some cases, such as Eisenmenger’s syndrome and primary pulmonary hypertension, the risk to maternal survival is so great that pregnancy is contraindicated. In general, how well the woman with heart disease tolerates pregnancy depends on the specific disease process and the degree to which her cardiac status is compromised. 123
Maternal heart disease also affects the fetus. Fetal risks are the result of genetic factors, alterations in placental perfusion and exchange, and the effect of maternally administered drugs. The genetic risk is demonstrated by the increased incidence of congenital heart defects that occur in the offspring of parents who have such a defect. The exact risk depends on the specific parental lesion, mode of inheritance, and exposure to environmental triggers. 23
Alterations in placental perfusion and gas exchange occur when the mother’s condition involves chronic hypoxemia or a significant decrease in cardiac output. These factors increase the threat to the fetus, with fetal risk increasing as maternal cardiac status declines. Chronic maternal hypoxemia results in a decrease in oxygen available to the fetus and is associated with fetal loss, prematurity, and IUGR. 168 Significant reductions in maternal cardiac output create decreased uterine blood flow and diminished placental perfusion with a resulting impairment in the exchange of nutrients, oxygen, and metabolic wastes. Possible fetal and neonatal consequences include spontaneous abortion, IUGR, neonatal asphyxia, central nervous system (CNS) damage, and intrauterine, intrapartum, or neonatal death. 85
A wide variety of drugs are used in the management of maternal cardiovascular disease. Although sometimes it is difficult to differentiate drug effects from the effects of the underlying disease, some associations between drug administration and fetal outcomes can be made. Anticoagulants are used to decrease the risk for thromboembolism, especially in women with artificial valves, a history of thrombophlebitis, or rheumatic heart disease. Oral anticoagulants, specifically warfarin sodium (Coumadin), have been associated with fetal malformations, including nasal hypoplasia and epiphyseal stippling, when administered during the first trimester. They also have been associated with eye and CNS abnormalities when administered later in pregnancy. The incidence of warfarin embryopathy is estimated to be 15% to 25%. Warfarin also is associated with maternal and fetal hemorrhage. Because of these risks, warfarin is contraindicated in pregnancy except in special circumstances such as pregnancy in women with prosthetic heart valves. 38 Heparin is considered the preferred agent for anticoagulation therapy during pregnancy. Heparin does not cross the placenta; therefore it does not result in fetal anticoagulation or neonatal hemorrhage (although maternal hemorrhage still may occur), nor has it been associated with congenital defects. Low-molecular-weight heparin is another alternative for anticoagulation during pregnancy. 51 In general, patients being treated with low-molecular-weight heparin during pregnancy are converted to unfractionated heparin during the final weeks of pregnancy because of the ease of rapid reversal of anticoagulation for labor and delivery. Some studies, however, did not demonstrate any difference in bleeding complications for gravidas continued on low-molecular-weight heparin versus those who were converted to unfractionated heparin. 89
Antiarrhythmic medications and cardiac glycosides used during pregnancy cross the placenta to varying degrees. They have not been implicated in fetal malformations and, although several have been associated with minor complications, generally are considered safe for use in pregnancy. 136 Reported complications include uterine contractions (quinidine, disopyramide), decreased birth weight (digoxin, disopyramide), and maternal hypotension with a sudden decrease in placental perfusion (verapamil).
Antihypertensives and diuretics also have been used in the treatment of cardiovascular disease during pregnancy. Labetalol and methyldopa are commonly used in pregnant women with chronic hypertension. These medications have been studied in prospective trials that revealed no adverse fetal or maternal outcomes. 58,157 Their use in the first trimester has also demonstrated safety. Atenolol has been associated with fetal growth restriction and abnormal placental growth. 24,54 Calcium channel blockers, such as nifedipine, are also safely used during pregnancy without an increase in major birth defects or adverse neonatal outcomes. 143 Diuretic use in pregnancy remains an area of some controversy. Fetal and neonatal compromise can result from diuretic-induced electrolyte and glucose imbalance and decreased placental perfusion caused by maternal hypovolemia. The use of thiazide diuretics has been linked to neonatal liver damage and thrombocytopenia. In general, diuretic use is restricted to women with pulmonary edema or acute cardiac or renal failure. Antihypertensive medications are not clearly shown to reduce the risk for preeclampsia in the hypertensive patient. 143
Although a great number of complications are possible, remember that, with few exceptions, most of the drugs used in the treatment of maternal heart disease can be used in pregnancy if the maternal condition warrants it. Angiotensin-converting enzyme inhibitors are contraindicated in pregnancy because of an association with fetal injury (renal dysfunction, fetal oliguria, oligohydramnios, fetal skull hypoplasia) and fetal death.
RESPIRATORY DISEASE
Respiratory function is altered even in normal pregnancy. Changes include a decrease in lung volume and increases in oxygen consumption, tidal volume, and minute ventilation. Significant decreases in maternal respiratory function and oxygenation can result in fetal growth restriction and fetal hypoxia with negative outcomes, but careful management of respiratory disease during pregnancy generally results in a favorable outcome.
Asthma is the most common respiratory disease in pregnancy, occurring in 3% to 12% of women, and the prevalence among pregnant women is rising. 115 For about two thirds of pregnant women, the course of asthma changes. 140 Infants born to women whose asthma is well controlled usually do well; unstable or worsening disease, especially status asthmaticus, increases fetal risk. 14 Commonly used asthma medications (e.g., long-acting beta agonists, inhaled corticosteroids, oral corticosteroids, other bronchodilators, and cromones) are generally considered safe for use in pregnancy. However, limited studies have associated maternal bronchodilator use and cromone exposure with an elevated risk for fetal gastroschisis99and a slight increase in fetal musculoskeletal malformation,150respectively. Additional research is needed to help determine whether a real risk exists and to guide asthma treatment during pregnancy. Presently, clinical evidence supports pharmacologic asthma control because the fetus is at greater risk from inadequate control of asthma than from asthma medications. 14
Fetal risks related to maternal asthma depend on the severity of the condition. Controlled asthma carries few risks for the fetus. However, severe or uncontrolled asthma increases the risk for infant death and the incidence of low birth weight, IUGR, preterm birth (possibly influenced by steroid use), and the need for cesarean delivery.82 Risks are higher in poorly controlled asthma patients. 15 Noncompliance with treatment, respiratory tract infections, allergens and irritants, smoking, gastroesophageal reflux, and exercise can lead to asthma exacerbations. 115
Cystic fibrosis (CF) was once considered a lethal childhood disease, but the life expectancy of a person with CF has increased, and is currently at about 35 years. 127 With careful planning and appropriate medical care, women with CF of childbearing age may conceive and have successful pregnancies with good neonatal outcomes, especially if their nutritional state and lung function remain good. 67 Women with severe disease may be cautioned to avoid conception because there is a risk for significant deterioration during gestation. Women who are positive for Burkholderia cepacia in sputum also have a worse prognosis. 67 Pregnancy in women with CF is likely to be associated with increased health care utilization and more antibiotic use compared with that of non-pregnant women with CF; high rate of gestational diabetes (12%) compared with non-CF pregnancies; and aggressive interventions to ensure weight gain, including the use of total parenteral nutrition for some. 33,119,154 Women with CF may experience pulmonary infections, which should be treated promptly and vigorously with antibiotics, fluids, and respiratory therapy. Fetal risks related to CF include prematurity, IUGR, and perinatal death, caused primarily by maternal hypoxemia and infection. Because all infants born to mothers with CF will be heterozygous carriers for CF (at least), genetic counseling and carrier testing of the father are important components of preconceptual care and early prenatal care. 154
Maternal Behavior
Maternal health behavior is an important component of neonatal and childhood health and may even be the single most important factor for the overall health of a child. 120 Health behaviors evaluated here are smoking, substance abuse, and nutrition, but other maternal behaviors also influence pregnancy outcomes, such as sleep patterns and exercise. Appropriate preconceptual and prenatal counseling regarding maternal health behaviors can help optimize neonatal health. 71,128
SMOKING
From 16% to 25% of women in the United States smoke during pregnancy, 125,158 with approximately 60% of smokers continuing to smoke through pregnancy. Of those who quit during pregnancy, half resume smoking by 6 months postpartum, 101 putting children at risk for second-hand smoke. It is well established that maternal smoking is a risk factor for stillbirths, IUGR, placental abruption, placental previa, PROM, and preterm labor. 158 Long-term effects include childhood obstructive airway disease, sudden infant death syndrome (SIDS), neurodevelopmental abnormalities, and childhood cancer, 158 and concerns about exposure to second-hand smoke continue to escalate. The exact mechanism by which fetal growth is restricted or fetal health is compromised is not entirely clear; reduced uterine artery blood flow, reduced placental blood flow resulting from vasoconstriction or smaller fetal capillaries in the placental capillary bed, elevated nicotine and carbon monoxide levels, and chronic fetal hypoxia all may play a role. 71,94 Fetal risk increases with the number of cigarettes smoked, maternal anemia, and poor nutrition. 69The babies of smokers may undergo withdrawal-like symptoms manifested by jittery movements and may be more difficult to soothe.95
Eliminating or reducing smoking, especially by the end of the first trimester, can improve fetal growth and health. Smoking cessation programs consistently implemented during prenatal visits have been shown to significantly improve smoking cessation rates. 109 The use of nicotine patches to facilitate smoking cessation during pregnancy is controversial. 125 Smoking cessation during pregnancy must be a major priority in counseling women preconceptually and prenatally because these are times when women may be most receptive to quitting because of a strong desire for a healthy pregnancy and baby. 109
SUBSTANCE ABUSE
Prenatal substance abuse rates vary greatly; however, it is estimated that about 11% of childbearing women have used illegal substances. 17 Use of drugs and alcohol by the mother places the fetus and newborn at risk for a plethora of structural, functional, and developmental problems. Perinatal morbidity is related to the direct effects of the abused substance on the developing fetus, its sudden withdrawal, the interactions of multiple abused substances, the nutritional effects of addiction on the mother, and the social and health care implications of substance abuse. 13,44,159
Alcohol is one of the most commonly abused substances during pregnancy. Although known to be a teratogen since the 1970s, about 40% of women in the United States drink some alcohol during pregnancy and about 3% to 5% drink heavily throughout pregnancy. 62 Alcohol in the maternal circulation crosses the placenta, resulting in direct fetal exposure to alcohol and its metabolites. 22There may be a wide range of effects on the exposed fetus; these include developmental and behavioral abnormalities, spontaneous abortion, stillbirth, craniofacial malformations, growth restriction, preterm birth, CNS dysfunction, and organ or joint abnormalities.13,22,55 The mechanism of fetal injury is not entirely clear but is likely related to three main factors: a teratogenic effect, hypoxia as a result of increased oxygen consumption, and a diminished ability to use amino acids in protein synthesis. 22 The expression of fetal alcohol effects ranges from subtle to extreme and depends on the timing of exposure, the dose, and the genetic response of the mother and fetus to the effects of alcohol. Secondary factors such as maternal age, nutritional status, general health, and the effects of other abused substances also may influence outcome. 141,166 When the more severe effects are exhibited, the condition is known as fetal alcohol syndrome (FAS). FAS is characterized by growth restriction, physical dysmorphic features including facial anomalies (small palpebral fissures, low nasal bridge, indistinct philtrum, thin upper lip, shortened lower jaw), and neurologic dysfunction, including mental retardation and neurodevelopmental deficits.134Other physical abnormalities involve the heart, skeletal system, and ears. “Fetal alcohol spectrum disorders (FASD)” is an umbrella term for FAS and other less physically noticeable yet long-term effects of alcohol exposure on the fetus.22Infants with FASD also may exhibit problems with suck, tremors, irritability, and hypertonus related to alcohol withdrawal. Continued abnormalities in motor, behavioral, and intellectual development often persist into childhood. Safe levels of alcohol intake have not been established; therefore women should be advised to avoid alcohol intake during pregnancy.
Chemical dependency in pregnancy is a complex problem and creates a high-risk patient. The mother’s reporting of drug use often is unreliable; frequently, more than one substance is involved, and there may be a cycle of drug use and periodic abstinence during pregnancy. In addition, a host of medical and social problems are associated with maternal drug abuse. Substance abusers generally have poor health; infectious diseases such as pneumonia, sexually transmitted disease (including human immunodeficiency virus [HIV] infection and acquired immunodeficiency syndrome [AIDS]), urinary tract infections, and hepatitis are common. 13,34 Nutrition and prenatal care often are inadequate; anemia frequently is seen. These factors contribute to a poor pregnancy outcome and make it difficult to isolate the effects of any one drug on the fetus. However, several generalizations can be made. The majority of drugs used by the mother, including opiates (e.g., methadone, heroin), barbiturates, and sedative-hypnotic drugs, cross the placenta and affect the fetus. Fetal risks include growth restriction, malformations, intrauterine demise, prematurity, asphyxia, CNS dysfunction, and neurobehavioral abnormalities. Fetal drug dependence does occur and is associated with neonatal abstinence syndrome (NAS), which is manifested by CNS irritability and gastrointestinal dysfunction17,34 (see Chapter 11).
Cocaine use by the mother merits special attention. Cocaine is a CNS stimulant that produces vasoconstriction, tachycardia, and hypertension in both the mother and the fetus. Its use during pregnancy has been linked to growth restriction, smaller head circumference, genitourinary tract anomalies, placental abruption, stillbirths, RDS, congenital infection, NAS, and cerebral infarcts, as well as impaired performance as measured with the Brazelton behavioral assessment tool.13,121
All prenatal care providers should thoroughly assess pregnant women for alcohol and substance abuse at each prenatal visit, and treatment interventions should be initiated when abuse is identified. Toxicology screening of maternal blood or urine can verify suspicions of abuse; however, universal screening is not currently recommended. Neonatal urine or meconium screening can provide an accurate indication of exposure when there are clinical indications of drug effect. Laws in some states consider prenatal drug exposure to be a form of child abuse; thus the practitioner may be required to report positive drug tests in pregnant women or their newborns. (See Chapter 11 for a more complete discussion of complications in drug-exposed neonates.)
MATERNAL NUTRITION, MALNUTRITION, AND OBESITY
Maternal nutritional status and placental function during pregnancy can significantly influence the growth, development, and health of the fetus and newborn. Nutritional problems that interfere with fetal cell division (increases in cell number) can have permanent consequences. If the fetus is at a stage in which cells are only enlarging (increases in cell size), then nutritional deficits may be reversed if a healthy maternal dietary intake is resumed soon enough in the pregnancy. All women presenting for prenatal care should be questioned about their usual dietary intake and should have their weight and height assessed so that body mass index (BMI) can be determined and appropriate nutrition counseling initiated. BMI can be calculated by dividing a woman’s prepregnancy weight in kilograms by her height in meters squared; it is the most frequently used single tool in determining obesity. If a woman’s prepregnancy weight is unknown, the value obtained at the first prenatal visit should be used. Although the BMI values for classification vary, the Institute of Medicine (IOM) employs the relative weight classification and prepregnancy BMI values as follows117:
• Underweight: less than 19.8
• Healthy weight: 19.8 to 26
• Overweight: 26.1 to 29
• Obese: greater than 29
Optimal ranges for weight gain in singleton pregnancies are also based on the IOM recommendations. As a general rule, weight gain should be as follows: underweight women should gain 28 to 40 lb; normal-weight women, 25 to 35 lb; overweight women, 15 to 25 lb; obese women, up to 15 lb. The optimal weight gain for women carrying twins is 35 to 45 lb. 117 The IOM guidelines are continually being evaluated, but at least one study confirms that following these guidelines can improve pregnancy outcomes. 78 However, fewer than half of women gain the recommended weight during pregnancy, 165 with 43.3% of women gaining above the IOM guidelines. 149
Prenatal nutrition involves more than appropriate weight gain; a variety of healthy foods should be consumed, providing essential nutrients. The dietary reference intakes (DRIs) increase for most nutrients during pregnancy. Protein, iron, vitamin A, and iodine requirements nearly double, yet some nutrient requirements do not change much. 156 Other maternal factors that should be considered when counseling women on nutrition include age, parity, preconceptual nutritional status, preexisting medical conditions, current medical conditions complicating the pregnancy, food likes and dislikes, and cultural influences. Each woman’s counseling should be individualized, and referral to a nutrition specialist and other medical specialists may be indicated. 39
Malnourished and underweight mothers have more perinatal losses and preterm births, and their newborns have lower Apgar scores and more frequently are of low birth weight (less than 2500 g). This is especially true of significantly underweight women (low BMI) and women with eating disorders, such as anorexia and bulimia, who fail to gain adequate weight during pregnancy.165 Small-for-gestational-age (SGA) newborns, defined as below the tenth percentile birth weight for gestational age, have higher mortality rates in the perinatal period and are at risk for later problems such as insulin resistance and poor school performance. 165 However, it may be difficult to draw direct correlations between inadequate maternal diet and fetal growth unless the nutritional disturbances are severe. Many fetuses grow well despite suboptimal maternal nutrition, in part because of the complexities of placental transport and the ability of the fetus to be preferentially supplied with some nutrients.
Although reduced birth weight is associated with inadequate carbohydrate, protein, and total caloric intake, inappropriate amounts of other nutrients may also affect the fetus. Vitamin and mineral deficiencies have been linked to miscarriage and stillbirth, congestive heart failure (thiamine), megaloblastic anemia (folic acid, B 12), congenital anomalies including neural tube defects (folic acid, zinc, copper), and skeletal abnormalities (vitamin D, calcium). 90,161 Vitamin overdosage, especially of the fat-soluble vitamins, also has been implicated in fetal abnormalities. Vitamin A overdose has been associated with kidney malformations, neural or cranial defects, and hydrocephalus; vitamin D overdose has been linked with cardiac, neurologic, and renal defects. 39
Obesity has become an epidemic in the United States and other developed countries. Obstetricians and gynecologists now cite obesity as the leading health problem confronting women today. It is a complex problem resulting from a combination of genetic, cultural, behavioral, socioeconomic, and environmental influences. Obesity affects all organ systems and contributes to a multitude of physiologic complications such as cardiovascular disease, gestational diabetes, infections, preeclampsia, and other adverse perinatal outcomes. 27,29
Overweight, obese, and morbidly obese women (BMI greater than 40) are at risk for chorioamnionitis, preeclampsia, stillbirth, cesarean delivery, instrumental delivery, postpartum hemorrhage, perineal lacerations, and prolonged hospital stay. Their offspring may suffer macrosomia, shoulder dystocia, meconium aspiration, fetal distress, early neonatal death, complications from cesarean birth, and birth defects.47 A 1% decrease in the number of obese pregnant women in the United States would result in 16,000 fewer cesarean births per year. 35
In addition, obese women may be struggling with associated psychosocial problems such as poor self-esteem, guilt about weight, depression, and ridicule from family and others. Some may not seek prenatal care until pregnancy is well into the second or third trimester. Thus obese women should be considered at high risk for childbearing complications, and these women and their fetus/newborn should be monitored closely throughout gestation and the perinatal period. When problems are identified, individualized intervention strategies should be implemented in an attempt to promote normal birth weight (appropriate for gestational age [AGA]) and improve perinatal outcomes. In conclusion, maternal health behavior, including smoking, nutrition, and drug use, before and during pregnancy is associated with adverse outcomes for the newborn and also long-term health risks of the newborn well into adulthood. Supportive, informed prenatal care for pregnant women at risk is essential to improved newborn health. 28
Obstetric Complications
ANTEPARTUM BLEEDING
Maternal cardiovascular support is crucial to fetal well-being. Chronic blood loss can lead to maternal anemia and a related decrease in oxygen-carrying capacity. Uncompensated acute bleeding results in diminished blood volume, decreased systolic pressure, decreased cardiac output, and ultimately decreased placental perfusion. The net effect on the fetus is decreased oxygenation and impaired nutrient delivery.
Gestational bleeding in the first or second trimester of pregnancy has been linked to increased risks of preterm labor, preterm birth, PROM, and low birth weight. 36 The most common causes of hemorrhage late in pregnancy include placental abruption and placenta previa. In an abruption, a normally implanted placenta separates from the uterine wall before the time of delivery, resulting in maternal bleeding and a functional decrease in uteroplacental size. A relationship between hypertensive disorders, cocaine use, and cigarette smoking and an increased incidence of abruptions has been reported. 12,61 The risk for abruption was four times higher in women with preterm PROM. In the presence of an intrauterine infection, the relative risk increased ninefold. 11 The separation may be partial or complete, involving peripheral and/or central portions of the placenta. Fetal compromise relates to the extent of the separation and to the frequent need for preterm delivery. When the abruption is small and bleeding is minimal, the pregnancy may continue without significant fetal compromise; however, remember that the decrease in uteroplacental surface area is irreversible and reduces the absolute placental capability. As the fetus grows or experiences additional stressors, its ability to tolerate the abruption may change. Extensive abruptions are poorly tolerated by both fetus and mother; the resulting maternal hemorrhage and decreased placental function lead to fetal asphyxia and, without immediate intervention, to intrauterine demise. 36,41
A placenta previa exists when the placenta lies abnormally low in the uterus and to some extent covers or encroaches on the internal cervical os. In the latter part of pregnancy, the normal elongation of the lower uterine segment and changes in the cervix disrupt the attachment of the overlying placenta. 116 This generally presents as episodic, painless maternal bleeding, often accompanied by preterm labor. To avoid active labor with resulting maternal hemorrhage, fetal lung maturity is assessed at 35 to 37 weeks. If the lungs are sufficiently mature, a cesarean section is scheduled before the onset of labor. Fetal compromise relates to the extent of the previa, severity of maternal hemorrhage, degree of the resulting fetal hypoxia, and gestational age at delivery. 145
Other placental abnormalities leading to antepartum bleeding include velamentous insertion and vasa previa. A vasa previa occurs when naked fetal vessels traverse the cervical os below the level of the fetal presenting part; it is associated with a high perinatal mortality rate. A velamentous insertion is defined as the insertion of the umbilical cord into the chorioamnionic membranes rather than the mass of the placenta. 131
HYPERTENSIVE DISORDERS OF PREGNANCY
Chronic hypertension in pregnancy, defined as hypertension diagnosed before pregnancy or before 20 weeks’ gestation, complicates 1% to 6% of births in the United States each year. Chronic hypertension is associated with IUGR, preterm birth, placental abruption, and stillbirth.58 The degree of fetal compromise is related to the degree and control of maternal hypertension. Women with chronic hypertension have a 25% risk for developing superimposed preeclampsia. 133
Gestational hypertension was defined by the Working Group on Research on Hypertension in Pregnancy as hypertension arising after 20 weeks in the absence of proteinuria. 133
Preeclampsia, a type of pregnancy-induced hypertension, is a condition in which hypertension, accompanied by proteinuria and edema, develops during the second half of pregnancy in women with or without preexisting hypertensive disease. It is most common in primigravidae in obese women, in women with multiple gestations and molar pregnancies, in women with a family history of this disorder, and those with a history of pregestational diabetes mellitus. 144 As a perinatal complication, preeclampsia is significant because of its high toll in terms of both maternal and fetal well-being.
Pregnancy is normally associated with vasodilation and decreased peripheral vascular resistance. The net effect is that, even though there is a significant increase in blood volume, maternal blood pressure does not increase during pregnancy. In contrast, pregnancy-induced hypertension is associated with vasoconstriction and an increase in peripheral vascular resistance and arterial pressure. The result is a reduction in blood flow to the vital organs, including the kidney, liver, brain, and uterus; reduced maternal blood volume; and a host of maternal hepatic, CNS, and coagulation abnormalities. The major effect on the intrauterine environment is placental insufficiency caused by significant reductions in uteroplacental blood flow and the development of placental vascular abnormalities. Associated fetal and neonatal risks include IUGR, prematurity with all of its attendant problems, perinatal asphyxia, and perinatal death. The risk to the infant increases with earlier onset and increasingly severe maternal disease, such as chronic hypertension with superimposed preeclampsia. 144Maternal seizures (eclampsia) further compromise the fetus by promoting hypoxemia and acidosis, which can result in intrauterine demise.
HELLP syndrome, a severe form of pregnancy-induced hypertension manifested by hemolysis, elevated liver enzymes, low platelets, and renal function abnormalities, carries a high risk for fetal and maternal death. In mild cases of HELLP syndrome, conservative management may facilitate improvement in the condition before delivery, but the risk for IUGR remains. In many cases of HELLP syndrome, immediate delivery is indicated regardless of the gestational age of the fetus. 142 The use of steroids in HELLP has been shown to improve maternal oliguria, mean arterial pressure, mean increase in platelet count, mean increase in urinary output, and liver enzyme elevations. However, no evidence suggests an improvement in maternal and perinatal mortality or morbidity with the use of maternal steroids except with regard to improvement in fetal lung maturity. 105
Drugs commonly used to treat pregnancy-induced hypertension include magnesium sulfate, hydralazine, labetalol, nifedipine, and other antihypertensive agents. Magnesium sulfate is the most commonly used agent in the United States for the prevention of maternal seizures and has been shown to be more effective than phenytoin (Dilantin). 57
Hypotonia and CNS depression have been reported as neonatal side effects, yet no correlation has been found between neonatal magnesium level and Apgar score.132These effects are more likely the result of coexisting complications, such as prematurity and asphyxia.139 Hydralazine and other antihypertensives are used in the treatment of severe maternal hypertension; actions include relaxation of the arterial bed, decreased vascular resistance, and decreased blood pressure. Maternal response to antihypertensives must be monitored carefully, because precipitous decreases in blood pressure reduce placental perfusion and further compromise the fetus.
INFECTION
Group B streptococcus (GBS) is a major cause of sepsis, meningitis, and death among newborn infants. It is estimated that 10% to 30% of all pregnant women are colonized with GBS in the vagina or rectum. The American College of Obstetricians and Gynecologists (ACOG) Committee on Obstetric Practice now recommends “vaginal or rectal group B streptococci screening cultures at 35 to 37 weeks of gestation for all pregnant women.” Treatment for women with a positive culture, GBS bacteriuria in the current pregnancy, or a previously GBS-infected infant is usually penicillin. 30
PRETERM LABOR
Preterm birth, defined as any birth before 37 weeks’ gestation, poses an unparalleled threat to neonatal survival and well-being. Its cost, both human and economic, is staggering, and its prevention is a primary focus of modern obstetric care. Prevention is best accomplished through an aggressive effort to identify women at risk and close follow-up to achieve early recognition and appropriate intervention should preterm labor occur. 10 Unfortunately, many women continue to receive inadequate prenatal care or no care at all. Even women who obtain early and ongoing care often fail to recognize the signs of preterm labor and delay reporting symptoms until intervention becomes difficult if not impossible. 42
Risk assessment markers in clinical use today include measurements of cervical length and the biochemical marker fetal fibronectin. Fetal fibronectin is a glycoprotein secreted by fetal membranes. Its presence in cervical-vaginal secretions between 22 and 35 weeks’ gestation has been associated with an increased risk for preterm labor and delivery. Its absence (high negative predictive value) can be used to identify patients who are at low risk for preterm delivery. 10Cervical length is assessed by three consecutive measurements using transvaginal ultrasound. The average length of the cervix varies with gestational change but is approximately 4 cm in length from 26 weeks. The length of the cervix has been inversely correlated to the risk for preterm birth. 76 Thus a combination of fetal fibronectin and cervical length may be used to assess the risk for preterm delivery for a given patient. 118
Although in many specific instances, a definitive cause cannot be identified, it is possible to identify several factors that generally are associated with preterm labor and delivery. 10When preterm labor cannot be halted, it culminates in the delivery of a physiologically immature infant. The result is a host of neonatal problems that relate largely to the degree of immaturity and also to compounding problems such as infant anomalies or maternal disease and to the events that led to the preterm delivery (e.g., asphyxia resulting from a bleeding placenta previa). Problems commonly encountered in preterm infants include respiratory distress, asphyxia, hyperbilirubinemia, metabolic disturbances, fluid and electrolyte imbalance, neurologic and behavioral problems, infection, nutritional deficits and feeding problems, ineffective thermoregulation, cardiovascular disturbances, chronic respiratory disease, and hematologic disturbances.
Although hydration often is used as a first-line measure for preterm uterine activity, the data do not support the efficacy of hydration as a treatment for preterm labor. 148
Beta-sympathomimetic agents, such as ritodrine hydrochloride and terbutaline sulfate, are commonly used as a means of interrupting preterm labor. They achieve their tocolytic action by maximizing the beta 2-adrenergic effects on the uterus, with a resulting decrease in uterine smooth muscle contractility. 42 Although these drugs are effective in prolonging gestation, they are associated also with maternal, fetal, and neonatal complications. 10 Mothers may experience tachycardia and dysrhythmias, hyperglycemia, hypokalemia, anxiety, nausea, and vomiting. Myocardial ischemia and pulmonary edema are rare but serious maternal side effects. The fetus also may develop tachycardia and hyperglycemia. Neonates born after beta-sympathomimetic therapy may develop a rebound hypoglycemia in response to in utero hyperglycemia and overproduction of insulin. Beta-sympathomimetic tocolytic agents increase fetal aortic blood flow and fetal cardiac output that might increase fetal systolic pressure and cerebral blood flow, which can lead to an increased incidence of intracranial bleeding in immature fetal brains. 122
Magnesium sulfate has also been employed as a tocolytic. Magnesium sulfate decreases muscle contractility, thereby inhibiting uterine activity and effectively interrupting preterm labor. Neonatal consequences of maternal magnesium administration include decreased muscle tone and drowsiness, as well as decreases in serum calcium level.42 A recent double-blind randomized control trial has suggested that magnesium sulfate given to preterm babies may decrease rates of gross motor dysfunction. 43
Prostaglandins play an important role in the onset of labor. Prostaglandin synthetase inhibitors, such as indomethacin, are a class of pharmacologic agents that interfere with the body’s synthesis of prostaglandin, thereby inhibiting prostaglandin-mediated uterine contractions. These drugs have been used to treat preterm labor. They can cause in utero constriction, or closure, of the ductus arteriosus with resulting development of fetal pulmonary hypertension and congestive heart failure. They also may lead to oligohydramnios and must be used with caution, especially late in the third trimester. Other neonatal risks include decreased platelet activity and gastrointestinal irritation. 18 The use of selective cyclooxygenase (COX-2) inhibitors in preterm labor treatment is being investigated. 100
Calcium channel blockers, such as nifedipine, also have a demonstrated ability to interfere with the labor process. Uterine contractility is directly related to the presence of free calcium. Increased calcium concentration enhances muscle contractility, whereas decreased calcium levels inhibit contractility. 42 Calcium antagonists block the entry of calcium into cells and inhibit uterine muscle contraction. In animal studies, these drugs have been associated with fetal acidosis. 50 However, lower umbilical artery pH values or lower Apgar scores have not been associated with nifedipine. 87
The use of progesterone suppositories in preterm labor prevention was recently investigated by daFonseca et al. 44a The study involved 142 women with high-risk singleton pregnancies treated with either 100 mg progesterone or placebo vaginal suppository. The study found statistically significant differences in the frequency of uterine activity and rate of preterm delivery in women treated with progesterone. 10 Intramuscular progesterone injection has also been studied in the prevention of recurrent preterm birth. In women with a history of preterm birth, there appears to be a beneficial effect of intramuscular progesterone to prevent recurrent preterm birth. No evidence supports the use of progesterone as a prophylactic agent in other women at risk for preterm birth such as women with short cervix or twin gestation. 48
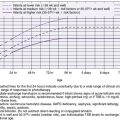
Corticosteroid treatment of pregnant women who deliver prematurely was first introduced in 1972 to enhance fetal lung maturity. In 1994, the National Institutes of Health (NIH) sponsored a Consensus Development Conference on the Effect of Corticosteroids for Fetal Maturation on Perinatal Outcomes. The consensus panel concluded that giving a single course of corticosteroids to pregnant women at risk for preterm birth reduced the risk for death, RDS, and intraventricular hemorrhage in preterm infants. The 1994 panel noted that the optimal benefit of antenatal corticosteroid therapy lasts 7 days. Since then, the use of repeated courses of antenatal corticosteroids became widespread in the United States, England, and Australia. In 2000, the NIH reconvened to present research of repeated courses of antenatal corticosteroid therapy. In studies in preterm animals, multiple doses of antenatal corticosteroids improved lung function when compared with a single dose. Human studies suggested possible benefits in reduction of the incidence and severity of RDS and the incidence of patent ductus arteriosus. Little or no evidence supported a reduction in mortality rate or reductions in the incidence of intraventricular hemorrhage, chronic lung disease, sepsis, necrotizing enterocolitis, or retinopathy of prematurity with repeated antenatal corticosteroid therapy. Some of the suggested fetal risks of repeated antenatal corticosteroid therapy include decreased somatic and brain growth, adrenal suppression, neonatal sepsis, chronic lung disease, and death. The current clinical recommendations based on the 2000 NIH Consensus Statement are as follows6:
• All pregnant women between 24 and 34 weeks’ gestation who are at risk for preterm delivery within 7 days should be considered candidates for antenatal treatment with a single course of corticosteroids.
• Treatment consists of two doses of 12 mg of betamethasone given intramuscularly 24 hours apart or four doses of 6 mg of dexamethasone given intramuscularly 12 hours apart.
• Repeated courses of corticosteroids should not be used routinely. In general, it should be reserved for patients enrolled in randomized controlled trials.
ENVIRONMENTAL EFFECTS OF LABOR ON THE FETUS
Effects of Contractions
During labor, the dynamics of uterine contractions alter the intrauterine environment and influence the fetus. A “healthy” fetus is equipped to withstand the challenge of labor, but when the fetus is compromised or the labor is dysfunctional, the fetus can be taxed beyond its capacity, placing it at risk for further compromise, asphyxia, or intrauterine death.
Strong uterine contractions are characterized by decreased blood flow through the intervillous spaces in the placenta. As blood flow decreases, a corresponding decline in placental gas exchange occurs and the fetus must depend on its existing reserves to maintain oxygenation until placental blood flow is reestablished. The net effect is that fetal Pa o2 decreases as the consequence of uterine contraction. In the fetus with adequate reserves, the fall in Pa o2 is not drastic; the fetus remains adequately oxygenated and so can tolerate the stress of labor.
Fetal Reserve
The factors that influence fetal reserve fall into two general categories: those that diminish reserves and those that exhaust reserves. When fetal oxygen reserves are diminished, the fetus has less-than-optimal oxygenation at the onset of a contraction. This may occur as a consequence of any condition that decreases placental exchange, including reduced placental surface area caused by abruption, placenta previa, an abnormally small placenta, decreased placental perfusion caused by maternal hypotension or hypertension, or maternal hypoxemia. Oxygen reserves can be diminished also as a result of a reduction in fetal oxygen-carrying capacity, as in severe anemia or acute fetal hemorrhage. 79
A fetal reserve that is adequate at the onset of labor can be exhausted by factors that place unusual demands on the fetus. Exhaustion of reserves occurs with contractions that last for a prolonged period, are of extremely high intensity, or occur with increased frequency and without an adequate recovery period between individual contractions. 79 This is often a consequence of the use of oxytocic agents to induce or augment labor.
Determination of cord gases at delivery can be used to determine the timing of a hypoxic or neurologic event. A base excess of equal to or less than 12 mmol/L generally is defined as the threshold that may be associated with hypoxic injury. 135 Fetal pulse oximetry may also be used. Decreased fetal pulse oximetry values, especially prolonged and recurrent recordings less than 30%, are correlated with abnormal fetal heart rate patterns, indicating an association with fetal compromise and metabolic acidosis. 151
Fetal Response to Contraction-Induced Hypoxia
When the fetal oxygen reserve is diminished or exhausted, uterine contractions can precipitate a significant fall in Pa o2. The fetus is quite limited in its ability to compensate for this hypoxemia. The adult mechanism, which involves increasing total cardiac output by increasing heart rate, does not play a major role in the fetal response. Instead, the fetus responds with a redistribution of cardiac output as a means of maintaining critical function; blood flow to the brain and heart increases, whereas perfusion of less critical organs is reduced. 7 This mechanism enables the fetus to survive brief episodes of hypoxia, but severe and prolonged hypoxic episodes are poorly tolerated.
Acute hypoxemia leads to the development of acidosis and also produces a reflex bradycardia as a result of vagal stimulation, both of which further compromise fetal oxygenation. In addition, myocardial hypoxia has a direct bradycardic effect. 7 These mechanisms give rise to one of the classic signs of fetal distress, the late deceleration, in which the peak of uterine pressure, which also represents the nadir of intervillous blood flow and the onset of fetal hypoxemia, is followed by a decline in fetal heart rate. Late decelerations are significant in that they help identify the fetus that cannot tolerate labor because of inadequate oxygen reserves and they allow for the implementation of measures to enhance fetal reserve, improve placental perfusion, or interrupt labor. 167
Late decelerations are particularly ominous when accompanied by loss of fetal heart rate variability and/or fetal baseline tachycardia, because these findings are indicative of fetal acidosis. In the preterm infant, the findings of decreased variability and tachycardia, with or without late decelerations, correlate highly with acidosis, depression, and low Apgar scores. 167
Other Factors That Evoke a Fetal Response During Labor
HEAD COMPRESSION
Pressure on the fetal head during labor, especially with pushing efforts in the second stage, also produces a vagal response and a reflex slowing of the fetal heart rate. In general, this does not indicate hypoxia or fetal compromise and often is seen in a healthy fetus. The deceleration that accompanies head compression, also called an early deceleration, is differentiated from the late deceleration of fetal asphyxia by its timing in relation to a contraction. In early deceleration, the heart rate begins to fall as a contraction builds, reaching its lowest point as the contraction peaks. As the contraction subsides, the heart rate returns to baseline. The result is a uniformly shaped dip that mirrors the shape of the contraction. In comparison, a late deceleration also has a uniform shape but lags behind the contraction, with the fall in heart rate beginning at or slightly after the contraction peak and continuing to fall as the contraction subsides. With a late deceleration, the heart rate does not return to baseline until well after the contraction has ended.
CORD COMPRESSION
Compression of the umbilical cord occurs when the cord is looped around fetal body parts, when it is knotted or prolapses, or when amniotic fluid is scant (oligohydramnios). During labor, cord compression may be exacerbated by contractions and descent of the fetus, resulting in varying degrees of occlusion of the umbilical vessels and diminution of blood flow. Partial venous occlusion may be manifested by fetal heart rate acceleration, whereas significant occlusion precipitates a rapid fall in heart rate, caused at least in part by vagal reflex. Variable decelerations can be spontaneous, occurring at any time, or periodic, occurring with contractions. They typically have an abrupt descent in heart rate and may be V, U, or W shaped—hence the term variable deceleration. Periodic variable decelerations are identified by a decline in heart rate that generally begins before the contraction peaks but, unlike early decelerations, falls rapidly and does not mirror the shape of the contraction. Typically, recovery of the heart rate also is rapid. However, when the occlusion is severe or of long duration or if the fetus has diminished oxygen reserves, recovery may be slow, indicating fetal hypoxia and, in essence, incorporating a component of late deceleration within the variable deceleration. 167
When variable decelerations are persistent and worsening during labor in the presence of oligohydramnios, intrapartum amnioinfusions have significantly decreased fetal heart rate abnormalities, acidemia at birth, and rates of cesarean birth. 129 An amnioinfusion involves infusion of fluid into the uterine cavity via an intrauterine pressure catheter (IUPC). This fluid provides cushioning of the umbilical cord, which may reduce the frequency and severity of the cord compression. Amnioinfusions have also been used when thick meconium is present in amniotic fluid to provide a diluting effect that can reduce the amount of meconium present in the infant’s trachea. However, a recent study showed no benefit of amnioinfusion on moderate to severe meconium aspiration syndrome or perinatal death. 64
MATERNAL PAIN MEDICATION
Maternal anesthesia and/or analgesia has the potential to affect the infant, either during labor and delivery or in the newborn period. The risk is increased if the fetus is preterm or is otherwise compromised. This is not to say that there is no place for these drugs in obstetric care—only that they must be used judiciously and with a clear understanding of the risks and benefits involved. Table 2-1 summarizes the effects of commonly used analgesic and anesthetic agents on the fetus and newborn. 4,68
| CNS, Central nervous system. | |
| Drug | Possible Fetal and Neonatal Side Effects |
|---|---|
| Narcotics |
Fetal and neonatal effects are related to the dose, route, and timing of maternal administration and may be reversed by the administration of a narcotic antagonist (naloxone):
CNS depression
Fetal bradycardia
Depressed respiratory effort
Decreased muscle tone and reflexes
Decreased responsiveness
|
| Paracervical block | Fetal bradycardia and asphyxia related to decreased uterine blood flow and direct fetal myocardial depression |
| Epidural and spinal block |
Fetal bradycardia and asphyxia related to maternal hypotension
Fetal/neonatal toxicity
Neonatal respiratory depression after epidural containing fentanyl
|
| General (inhalation) anesthesia |
Fetal and newborn effects related to the duration and depth of maternal anesthesia include the following:
CNS depression
Respiratory depression
Decreased responsiveness
|
ASSESSMENT OF FETAL WELL-BEING
Over the past 20 to 30 years, the capability to assess fetal well-being has advanced from simple auscultation of the fetal heart to direct physiologic and biochemical measurement of fetal status. With these advances, an appreciation of the similarities between the fetus and newborn, as well as a more complete understanding of the unique features of fetal life, has been gained. This knowledge reinforces the importance of viewing fetal physiology as a precursor of neonatal function and especially as a significant influence on the success with which the fetus will complete the adaptations required by the birth process.
The goal of antepartum fetal surveillance is to answer the following questions: What is the safest environment for a fetus at the gestational age at which the testing is taking place? Is the fetus more likely to survive in utero for the week after testing, or does the fetus have a significant risk for in utero death based on the degree of environmental or intrinsic intolerance demonstrated through testing? In the case of preterm infants, this may mean delivery at a gestational age at which there is a high likelihood for respiratory, neurologic, cardiac, gastrointestinal, and immunologic immaturity that will require neonatal intensive care.
The obstetric practitioner has several tools available to help answer the preceding questions. First and foremost is the identification of maternal conditions that may predispose the fetus to in utero compromise. Examples of such conditions include type 1 diabetes mellitus, chronic hypertension, collagen vascular disease, antiphospholipid antibody disease, maternal cardiac or pulmonary disease, preeclampsia, blood group isoimmunization, in utero infection, PROM, and maternal substance abuse. This list is not all-inclusive but demonstrates several commonly encountered conditions for which antepartum fetal surveillance is warranted.
Once the decision is made to assess fetal well-being, four modalities are available in general practice to help the practitioner and patient answer questions about the optimal environment for the fetus at any given time—fetal movement counts, the contraction stress test, the nonstress test, and the fetal biophysical profile. Two additional tools often used by maternal-fetal medicine specialists in certain clinical situations are Doppler flow studies and percutaneous umbilical cord blood sampling (PUBS). None of these tools is used as the sole determinant for delivery; rather, each is used in conjunction with the entire clinical picture. The choice of testing method also is clinically driven; each method is useful in certain clinical settings, but no one method is the correct choice in all situations.
Although most of the procedures used to monitor fetal well-being are decidedly high-tech, the simple “kick count,” or fetal movement survey, is a low-tech, low-cost screening tool. Many women with an intrauterine fetal demise have no identifiable risk factors that would place them in a fetal testing protocol. Fetal motor activity reflects the fetal condition in utero, and a decrease in or absence of fetal movements often presages fetal death. This is one reason that many institutions ask their patients to begin a fetal movement counting protocol at 26 to 32 weeks of gestation. Although there are continuing study results, some centers have demonstrated a significant decrease in the incidence of fetal mortality after the institution of a fetal movement counting protocol.
There are several different approaches to fetal movement counting. None has been shown to be superior. 7 One approach is to have the patient choose a certain time every day to rest in the lateral position and count fetal movements. The perception of 10 distinct fetal movements within 2 hours constitutes a reassuring session. The most important aspect of this type of testing is to emphasize to the patient the importance of notifying her practitioner immediately if the fetal movement counting has not met the established criteria. A system must be in place in which patients have immediate access to health care personnel 24 hours per day.
The contraction stress test (CST) is used in an attempt to evaluate fetal response to uterine contractions. 74 The principle behind the CST is that uterine contractions cause a transient interruption in uteroplacental perfusion. With normal fetal reserve, this intermittent interruption is well tolerated. With inadequate or exhausted reserve, late fetal heart rate decelerations appear. Because late decelerations during labor had been associated with fetal hypoxia and acidosis, it was reasoned that similar interpretations could be applied to contractions induced in the antepartum patient. Thus the CST is considered a test of uteroplacental reserve.
During a CST, uterine contraction activity is evoked with either the use of maternal nipple stimulation or an intravenous infusion of oxytocin. The fetal heart rate is charted using graph paper attached to a monitor that uses a continuous wave ultrasound transducer placed on the maternal abdomen over the uterus. The minimum number of spontaneous or evoked contractions necessary for adequate testing is three contractions of 40 seconds’ duration in a 10-minute period. The results are interpreted as follows:
• A negative CST result is one in which no late fetal heart rate decelerations occur during the examination.
• In a positive CST result, late decelerations occur after 50% or more of the contractions, even if contraction frequency is fewer than three in 10 minutes.
• A suspicious or equivocal finding is one in which intermittent late or significant variable decelerations occur.
• A CST result is considered unsatisfactory if fewer than three contractions occur per 10 minutes or a poor-quality tracing is obtained.
In many clinical situations, a positive CST warrants delivery of the fetus because of suspected in utero hypoxemia during periods of uterine contraction. However, there are numerous exceptions to this rule. For example, if a positive CST is noted in the presence of maternal diabetic ketoacidosis, a correction of the underlying metabolic process may reverse the fetal acidosis and a negative CST may be obtained subsequently. Thus the delivery of a neonate who has metabolic acidosis and is preterm can be avoided.
The nonstress test (NST) is a tool used to indirectly assess the integrity of the fetal autonomic nervous system. The fetal heart is under the dual influences of the sympathetic and parasympathetic nervous systems. By approximately 28 weeks’ gestation, 85% of fetuses demonstrate fetal heart rate accelerations in response to fetal movement. Lack of these intermittent fetal heart rate accelerations usually indicates a fetal sleep cycle. However, many other intrinsic and extrinsic factors, including fetal acidosis, may lead to an absence of these intermittent accelerations in heart rate. Examples include but are not limited to medication exposure, maternal smoking, uteroplacental insufficiency, and fetal structural or chromosomal anomaly. Factors leading to maternal acidosis (severe anemia, congenital heart disease, and sepsis) also can result in fetal acidosis and nonreactive NST.
The NST is performed with the patient in a semi-Fowler’s or lateral tilt position. As in the CST, the fetal heart rate is monitored with an external transducer. NSTs are interpreted as either reactive or nonreactive. An accepted definition of a reactive NST is an increase in fetal heart rate of 15 beats/min for 15 seconds above the baseline heart rate occurring twice in a 20-minute period. 7 Some centers may require that the fetal heart rate accelerations be associated with fetal movements, as well as perceived by the maternal patient. A nonreactive test is defined as lacking the necessary fetal heart rate accelerations during a 40-minute period. The following may be candidates for nonstress testing:
• Women who have diabetes that must be controlled with insulin
• Women who have pregnancy-induced hypertension or intrinsic renal disease
• Women in whom fetal IUGR or postdate pregnancy has been determined
• Women who have reported decreased fetal movement
The NST has certain advantages over the CST. It does not entail the production of uterine contractions, and so there are fewer potential problems or contraindications to the NST. Because the NST is quicker and easier to conduct, it is often the first-line screening test of fetal well-being. Its disadvantages are that it does not evaluate uteroplacental reserve and that it has a higher false-positive rate than the CST.
When the NST is nonreactive, an option that is often used in lieu of the CST or delivery of the fetus is the biophysical profile (Table 2-2). This test combines the NST with real-time ultrasound evaluation of the fetus. Although there are several different biophysical profile (BPP) scoring systems, the one most generally accepted assigns a numerical score of 0 or 2 for the absence or presence, respectively, of five different parameters. These include fetal movement, tone, “breathing” movements, amniotic fluid volume, and the NST. One advantage to evaluation of several different fetal biophysical variables is enhanced specificity of testing with a diminished incidence of delivery for false-positive results. The presence or absence of acute markers (movement, tone, breathing, and NST) helps reflect fetal status at the time of testing. Evaluation of amniotic fluid volume as a marker is indirect evidence that the portions of the fetal CNS that control that activity are intact and functioning and therefore not acidotic. However, the absence of a given marker may be difficult to interpret, because it may simply reflect normal periodicity.
| Biophysical Variable | Normal (2) | Abnormal (0) |
|---|---|---|
| Fetal breathing—At least one episode of at least 30 seconds during a 30-minute observation | Present | Absent |
| Gross body movement—At least three body or limb movements during a 30-minute observation | ≥3 | ≤2 |
| Fetal tone—One episode of extension or flexion of limbs or trunk during a 30-minute observation | Present | Absent |
| Reactive nonstress test—At least two episodes of 15 beats/min fetal heart rate accelerations during 30-minute observation | Yes | No |
| Amniotic fluid volume—At least one pocket of at least 1 cm × 1 cm in two directions | Present | Absent |
| Normal Score: 8-10 |
The biophysical activities that mature first in fetal development disappear last as acidosis worsens. Fetal tone (flexion and extension) is present at 71/2 to 81/2 weeks after the last menstrual period. This activity, as well as gross body movement, is mediated in the cortex and nuclei of the CNS. Fetal movement is present by 9 weeks. Fetal breathing movements (i.e., rhythmic breathing movements of 35 seconds or more) are generally seen by 20 weeks’ gestation. The CNS center responsible for control of this activity is the ventral surface of the fourth ventricle. The final acute marker to mature is fetal heart rate acceleration in response to movement (reactive NST) seen in the later second trimester. The posterior hypothalamus and medulla control this activity. Given that the first marker to appear in development is the last to disappear with worsening fetal acidosis, the absence of fetal tone has been found to be associated with high perinatal morbidity and mortality. 162 Chronic sustained fetal hypoxia or acidosis may produce a protective redistribution of cardiac output away from less vital fetal organs (e.g., kidney, lung) toward the essential organs (e.g., brain, heart, adrenal glands). Redistribution of fetal blood flow may be so profound that renal perfusion decreases to the point that oligohydramnios is established. When the largest vertical amniotic fluid pocket within the uterus is less than 1 cm, the perinatal mortality rate is as high as 110/1000. 31
A BPP score of 8 or 10 is normal; a score of 6 is equivocal, and the profile should be repeated in 12 to 24 hours. A score of 4 or less is abnormal. Management in the presence of an abnormal BPP depends on the gestational age and the maternal and/or fetal factors contributing to the altered state.
The BPP employs the advantages of real-time ultrasonography to observe fetal behavior. 103 One of its major advantages is as an intermediate step in the evaluation of a fetus with a nonreactive NST before a time-consuming CST is performed. It is also a useful tool for patients with contraindications to the CST, such as premature labor, premature rupture of membranes, unexplained vaginal bleeding, or multiple gestations. The modified BPP, which combines an acute marker (NST) with the chronic marker of fetal well-being (amniotic fluid index [AFI]), has been shown by some centers to be as predictive of fetal well-being as the full BPP. Because evaluation of the AFI is less time consuming and requires less technical skill, this may be an acceptable alternative for many centers. Finally, it should be noted that though widely used, there is insufficient evidence from randomized trials to support the use of BPP as a test of fetal well-being in high-risk pregnancies. 92
No matter which of these testing modalities is used, the patient should be counseled as to the predictive value of a “normal” test. The incidence of stillbirth within 1 week of a reactive NST is 1.9/1000; for a negative CST, it is 0.3/1000; and for a normal BPP, it is 0.8/1000. 7 Although some investigators have reported a decreased incidence of fetal mortality after initiation of a fetal movement counting program for “low-risk” patients, enough data are not yet available to apply these numbers to the general population. 111
The role of Doppler flow assessment of the fetal arterial and venous systems in the prediction of in utero well-being is increasingly accepted. Measurement of umbilical artery velocity is used as a method of fetal surveillance for growth-restricted fetuses. Specifically, decreased or absent end-diastolic flow may appear days before conventional antenatal tests become abnormal. In cases such as these, at a minimum, intensive fetal surveillance is advised. 63 Reversal of diastolic flow is highly predictive of in utero fetal demise within 24 hours and warrants immediate intense investigation or delivery. No role for Doppler velocimetry in conditions other than in growth restriction has been demonstrated. 7
The dramatic improvement in ultrasound image quality over the past 15 years also has made it possible to directly sample fetal blood and tissue. The technique of percutaneous umbilical blood sampling (PUBS) has given the obstetrician access to the fetal circulation with relative safety for both the fetus and mother. In this procedure, real-time ultrasonography is used to guide the insertion of a needle into the umbilical vein or artery. Samples of fetal blood can be obtained, or, as in the case of red cell isoimmunization, transfusions can be carried out. The fetal loss rate is generally quoted as 1% to 2%. 5,138
REFERENCES
1. Abalovich, M.; Amino, N.; Barbour, L.A.; et al., Management of thyroid dysfunction during pregnancy and postpartum: an Endocrine Society Clinical Practice Guideline, J Clin Endocrinol Metab 92 (Suppl 8) ( 2007) S1.
2. Adams-Waldorf, K.M.; Nelson, J.L., Autoimmune disease during pregnancy and the microchimerism legacy of pregnancy, Immunol Invest 37 (2008) 631.
3. Alexander, E.K., Timing and magnitude of increases in levothyroxine requirements during pregnancy in women with hypothyroidism, N Engl J Med 351 (2004) 241.
4. American Academy of Pediatrics, American College of Obstetricians and Gynecologists, and March of Dimes Birth Defects Foundation, Guidelines for perinatal care. ed 6 ( 2007)The Academy, Elk Grove Village, Ill.
5. American College of Obstetricians and Gynecologists (ACOG) Committee Opinion, Fetal pulse oximetry, Obstet Gynecol 98 (2001) 523.
6. American College of Obstetricians and Gynecologists (ACOG) Committee Opinion, Antenatal corticosteroid therapy for fetal maturation, Int J Gynaecol Obstet 78 (2002) 95.
7. American College of Obstetricians and Gynecologists (ACOG) Practice Bulletin, Antepartum fetal surveillance, Int J Gynaecol Obstet 68 (2000) 175.
8. American College of Obstetricians and Gynecologists (ACOG) Practice Bulletin, Gestational diabetes, Obstet Gynecol 98 (3) ( 2001) 525.
9. American College of Obstetricians and Gynecologists (ACOG) Practice Bulletin, Thyroid disease in pregnancy, Obstet Gynecol 100 (2) ( 2002) 387.
10. American College of Obstetricians and Gynecologists (ACOG) Practice Bulletin, Management of preterm labor, Obstet Gynecol 101 (2003) 1039.
11. Ananth, C.V.; Oyelese, Y.; Srinivas, N.; et al., Preterm premature rupture of membranes, intrauterine infection, and oligohydramnios: risk factors for placental abruption, Obstet Gynecol 104 (2004) 71.
12. Ananth, C.V.; Smulian, J.C.; Vintzileos, A.M., Incidence of placental abruption in relation to cigarette smoking and hypertensive disorder during pregnancy: a meta-analysis of observational studies, Obstet Gynecol 93 (1999) 622.
13. Araojo, R.; McCure, S.; Feibus, K., Substance abuse in pregnant women: making improved detection and good clinical outcome, Clin Pharmacol Ther 83 (2008) 521.
14. Asthma and Pregnancy—update 2004, National Asthma Education Prevention Program Working Group on Managing Asthma During Pregnancy, Recommendations for pharmacologic treatment—update 2004, In: NIH U.S. Department of Health and Human Services, National Heart, Lung and Blood Institute, ( 2004); NIH Publication No. 05-3279.
15. Bakhireva, L.N.; Schatz, M.; Jones, K.L.; et al., Organization of Teratology Information Specialists Collaborative Research Group: Asthma control during pregnancy and the risk of preterm delivery or impaired fetal growth, Ann Allergy Asthma Immunol 101 (2008) 137.
16. Bar, J.; Ben-Rafael, Z.; Padoa, A.; et al., Prediction of pregnancy outcome in subgroups of women with renal disease, Clin Nephrol 53 (2000) 437.
17. Bell, J.; Harvey-Dodds, L., Pregnancy and injecting drug use, Br Med J 336 (2008) 1303.
18. Besinger, R.; Niebyl, J.R.; Keyes, W.G.; et al., Randomized comparative trial of indomethacin for the long term treatment of preterm labor, Am J Obstet Gynecol 164 (1991) 981.
19. Briggs, G.; Freeman, R.K.; Yaffe, S.J., Drugs in pregnancy and lactation: a reference guide to fetal and neonatal risk. ed 7 ( 2005)Lippincott Williams & Wilkins, Baltimore.
20. Bromfield, E.B.; Dworetzky, B.A.; Wyszynski, D.F.; et al., Valproate teratogenicity and epilepsy syndrome, Epilepsia ( 2008); Epub ahead of print, PMID:18557775,.
21. Buehler, B.A.; Stempel, L.E., Anticonvulsant therapy during pregnancy, In: (Editors: Rayburn, W.F.; Zuspan, F.P.) Drug therapy in obstetrics and gynecologyed 3 ( 1992)Mosby, St Louis.
22. Burd, L.; Roberts, D.; Olson, M.; et al., Ethanol and the placenta: a review, J Matern Fetal Neonatal Med 20 (2007) 361.
23. Burns, J., Congenital heart disease: risk to offspring, Arch Dis Child 58 (1983) 947.
24. Butters, L.; Kennedy, S.; Rubin, P.C., Atenolol in essential hypertension during pregnancy, Br Med J 301 (1990) 1103.
25. Casey, B.M.; Dashe, J.S.; Wells, C.E.; et al., Subclinical hypothyroidism and pregnancy outcomes, Obstet Gynecol 105 (2005) 239.
26. Casey, B.M.; Dashe, J.S.; Wells, C.E.; et al., Subclinical hyperthyroidism and pregnancy outcomes, Obstet Gynecol 107 (2006) 337.
27. Castro, L.C.; Avina, R.L., Maternal obesity and pregnancy outcomes, Curr Opin Obstet Gynecol 14 (2002) 601.
28. Catalano, P.M., Management of obesity in pregnancy, Obstet Gynecol 109 (2007) 419.
29. Catalano, P.M.; Ehrenberg, H.M., The short- and long-term implications of maternal obesity on the mother and her offspring, Br J Obstet Gynaecol 113 (2006) 1126.
30. Centers for Disease Control and Prevention, Perinatal group B streptococcal disease after universal screening recommendations—United States, 2003-2005, MMWR 56 (2007) 701.
31. Chamberlain, P.F.D.; Manning, F.A.; Morrison, I.; et al., Ultrasound evaluation of amniotic fluid volumes. I. The relationship of marginal and decreased amniotic fluid volumes to perinatal outcome, Am J Obstet Gynecol 150 (1984) 250.
32. Cheng, Y.W.; Caughey, A.B., Gestational diabetes: diagnosis and management, J Perinatol ( 2008); Epub ahead of print, PMID:18633419.
33. Cheng, E.Y.; Goss, C.H.; McKone, E.F.; et al., Aggressive prenatal care results in successful fetal outcomes in CF women, J Cyst Fibros 5 (2006) 85.
34. Christensen, C., Management of chemical dependence in pregnancy, Clin Obstet Gynecol 51 (2008) 445.
35. Chu, S.Y.; Kim, S.Y.; Schmid, C.H.; et al., Maternal obesity and risk of cesarean delivery: a meta-analysis, Obes Rev 8 (2007) 385.
36. Clark, S.L., Placenta previa and abruptio placentae, In: (Editors: Creasy, R.K.; Resnik, R.) Maternal-fetal medicineed 4 ( 1999)Saunders, Philadelphia.
37. Coetzee, E.J.; Levitt, N.S., Maternal diabetes and neonatal outcome, Semin Neonatal 5 (2000) 221.
38. Cotrufo, M.; De Feo, M.; De Santo, L.S.; et al., Risk of warfarin during pregnancy with mechanical valve prostheses, Obstet Gynecol 100 (5 Pt 1) ( 2002) 1040.
39. Cox, J.T.; Phelan, S.T., Nutrition during pregnancy, Obstet Gynecol Clin North Am 35 (2008) 369.
40. Reference deleted in proofs
41. Crane, J.M.; van der Hof, M.C.; Dodds, L.; et al., Neonatal outcomes with placenta previa, Obstet Gynecol 93 (1999) 541.
42. Creasy, R.K.; Iams, J.D., Preterm labor and delivery, In: (Editors: Creasy, R.K.; Resnik, R.) Maternal-fetal medicineed 4 ( 1999)Saunders, Philadelphia.
43. Crowther, C.A.; Hiller, J.E.; Doyle, L.W.; et al., Effect of magnesium sulfate given for neuroprotection before preterm birth: a randomized controlled trial, JAMA 290 (2003) 2669.
44. Curet, L.B.; Hsi, A.C., Drug abuse during pregnancy, Clin Obstet Gynecol 45 (2002) 73.
44a. daFonseca, E.B.; Bittar, R.E.; Carvalho, M.H.; Zugaib, M., Prophylactic administration of progesterone by vaginal suppository to reduce the incidence of spontaneous preterm birth in women at increased risk: A randomized placebo-controlled double-blind study, Am J Obstet Gynecol 188 (2003) 419.
45. Dahl, J.; Myhr, K.M.; Daltveit, A.K.; et al., Pregnancy, delivery, and birth outcome in women with multiple sclerosis, Neurology 65 (2005) 1961.
46. Diamond, M.P.; Salyer, S.L.; Vaughn, W.K.; et al., Reassessment of White’s classification and Pedersen’s prognostically bad signs of diabetic pregnancies in insulin-dependent diabetic pregnancies, Am J Obstet Gynecol 156 (1987) 599.
47. Dietl, J., Maternal obesity and complications during pregnancy, J Perinat Med 33 (2005) 100.
48. Dodd, A.; Flenady, V.J.; Cincotta, R.; et al., Progesterone for the prevention of preterm birth: a systematic review, Obstet Gynecol 112 (2008) 127.
49. Doria, A.; Tincani, A.; Lockshin, M., Challenges of lupus pregnancies, Rheumatology 47 (2008) iii9.
50. Ducsay, C.A.; Thompson, J.S.; Wu, A.T.; et al., Effects of calcium entry blocker (nicardipine) tocolysis in rhesus macaques: fetal plasma concentrations and cardiorespiratory changes, Am J Obstet Gynecol 157 (1987) 1482.
51. Dulitzki, M.; Pauzner, R.; Langevitz, P.; et al., Low-molecular-weight heparin during pregnancy and delivery: preliminary experience with 41 pregnancies, Obstet Gynecol 87 (1996) 380.
52. Dwosh, E.; Guimond, C.; Duquette, P.; et al., The interaction of MS and pregnancy: a critical review, Int MS J 10 (2003) 38.
53. Eadie, M.J., Antiepileptic drugs as human teratogens, Expert Opin Drug Saf 7 (2008) 195.
54. Easterling, T.R.; Brateng, D.; Schmucker, B.; et al., Prevention of preeclampsia: a randomized trial of atenolol in hyperdynamic patients before onset of hypertension, Obstet Gynecol 93 (1999) 725.
55. Elloit, E.J.; Bower, C., Alcohol and pregnancy: the pivotal role of the obstetrician, Aust NZ J Obstet Gynaecol 48 (2008) 227.
56. Elliott, J.P.; O’Keefe, D.F.; Schon, D.A.; et al., Dialysis in pregnancy: a critical review, Obstet Gynecol Surv 46 (1991) 319.
57. Evidence from the Collaborative Eclampsia Trial, Which anticonvulsant for women with eclampsia?Lancet 345 (1995) 1455.
58. Ferrer, R.L.; Sibai, B.M.; Mulrow, C.D.; et al., Management of mild chronic hypertension during pregnancy: a review, Obstet Gynecol 96 (2000) 849.
59. Ferrero, S.; Pretta, S.; Nicolette, A.; et al., Myasthenia gravis: management issues during pregnancy, Eur J Obstet Gynecol Reprod Biol 121 (2005) 128.
60. Ferrero, S.; Pretta, S.; Ragni, N., Multiple sclerosis: management issues during pregnancy, Eur J Obstet Gynecol Reprod Biol 115 (2004) 3.
61. Fleming, A.D., Abruptio placentae, Crit Care Clin 7 (1991) 865.
62. Floyd, R.L.; Sidhu, J.S., Monitoring prenatal alcohol exposure, Am J Med Genet C Semin Med Genet 127C (1) ( 2004) 3.
63. Forouzan, I., Absence of end-diastolic flow velocity in the umbilical artery: a review, Obstet Gynecol Surv 50 (1995) 219.
64. Fraser, W.; Hotmeyr, J.; Lede, R.; et al., Amnioinfusion for the prevention of the meconium aspiration syndrome, N Engl J Med 353 (2005) 946.
65. Reference deleted in proofs.
66. Ghafari, A.; Sanadgol, H., Pregnancy after renal transplantation: ten-year-center experience, Transplant Proc 40 (2008) 251.
67. Gilljam, M.; Antoniou, M.; Shin, J.; et al., Pregnancy in cystic fibrosis: fetal and maternal outcomes, Chest 118 (2000) 85.
68. Goetzl, L.M., ACOG Practice Bulletin. Clinical management guidelines for obstetrician-gynecologists: obstetric analgesia and anesthesia, Obstet Gynecol 100 (2002) 177.
69. Gruslin, A.; Perkins, S.L.; Manchanda, R.; et al., Maternal smoking and fetal erythropoietin levels, Obstet Gynecol 95 (2003) 561.
70. Haddow, J.E.; Palomaki, G.; Allan, W.; et al., Maternal thyroid deficiency during pregnancy and subsequent neurophysiological development of the child, N Engl J Med 341 (1999) 549.
71. Haslam, C.; Lawrence, W., Health-related behavior and beliefs of pregnant smokers, Health Psychol 23 (2004) 486.
72. Henriksen, T., The macrosomic infant: a challenge in current obstetrics, Acta Obstet Gynecol Scand 87 (2008) 134.
73. Houtchens, M.K., Pregnancy and multiple sclerosis, Semin Neurol 27 (2007) 434.
74. Huddleston, J., Continued utility of the contraction stress test?Clin Obstet Gynecol 45 (2002) 1005.
75. Hunt, S.; Russell, A.; Smithson, W.H.; et al., Topiramate in pregnancy: preliminary experience from the UK Epilepsy and Pregnancy Register, Neurology 71 (2008) 272.
76. Iams, J.D.; Goldenberg, R.L.; Meis, P.J.; et al., The length of the cervix and the risk of spontaneous premature delivery, N Engl J Med 334 (1996) 567.
77. Jacobson, G.F.; Ramos, G.A.; Ching, J.Y.; et al., Comparison of glyburide and insulin for the management of gestational diabetes in a large managed care organization, Am J Obstet Gynecol 93 (2005) 118.
78. Jain, N.J.; Denk, C.E.; Kruse, L.K.; et al., Maternal obesity: can pregnancy weight gain modify risk of selected pregnancy outcomes?Am J Perinatol 24 (2007) 291.
79. James, D.K.; Steer, P.J.; Weiner, C.P.; et al., High risk pregnancy: management options. ed 3 ( 2006)Saunders, Philadelphia.
80. Jones, D.C.; Hayslett, J.P., Outcome of pregnancy in women with moderate or severe renal insufficiency, N Engl J Med 335 (1996) 226.
81. Kalidindi, M.; Ganpot, S.; Tahmesebi, T.; et al., Myasthenia gravis and pregnancy, J Obstet Gynecol 27 (2007) 30.
82. Karima, M.; Davar, R.; Mirzaei, M.; et al., Pregnancy outcomes in asthmatic women, Iran J Allergy Asthma Immunol 7 (2008) 105.
83. Karmon, A.; Sheiner, E., The relationship between urinary tract infection during pregnancy and preeclampsia: causal, confounded or spurious?Arch Gynecol Obstet 277 (2008) 479.
84. Kashanizadeh, N.; Nemati, E.; Sharifi-Bonab, M.; et al., Impact of pregnancy on the outcome of kidney transplantation, Transplant Proc 39 (2007) 1136.
85. Khairy, P.; Ouyang, D.W.; Fernandes, S.M.; et al., Pregnancy outcomes in women with congenital heart disease, Circulation 113 (2006) 517.
86. Khandelwal, M.; Rasanen, J.; Ludormirski, A.; et al., Evaluation of fetal and uterine hemodynamics during maternal cardiopulmonary bypass, Obstet Gynecol 88 (1996) 667.
87. King, J.F.; Flenady, V.; Papatsonis, D.; et al., Calcium channel blockers for inhibiting preterm labour: a systematic review of the evidence and a protocol for administration of nifedipine, Aust NZ J Obstet Gynaecol 43 (2003) 192.
88. Kirby, R., Maternal phenylketonuria: a new cause for concern, J Obstet Gynecol Neonatal Nurs 28 (1999) 227.
89. Kominiarek, M.A.; Angelopoulos, S.M.; Shapiro, N.L.; et al., Low-molecular-weight heparin in pregnancy: peripartum bleeding complications, J Perinatol 27 (2007) 329.
90. Kovacs, C., Vitamin D in pregnancy and lactation: maternal, fetal, and neonatal outcomes from human and animal studies, Am J Clin Nutr 520S (2008) 88.
91. Krishnamurthy, K.B., Pregnancy and epilepsy: update on pregnancy registries, Curr Treat Options Neurol 10 (2008) 246.
92. Lalor, J.G.; Fawole, B.; Alfirevic, Z.; et al., Biophysical profile for fetal assessment in high risk pregnancies, Cochrane Database Syst Rev 23 (1) ( 2008); CD000038.
93. Langer, O.; Yogev, Y.; Most, O.; et al., Gestational diabetes: the consequences of not treating, Am J Obstet Gynecol 192 (2005) 989.
94. Larsen, L.G.; Clausen, H.V.; Jansson, L., Stereologic examination of placentas from mothers who smoke during pregnancy, Am J Obstet Gynecol 186 (2002) 531.
95. Law, K.L.; Stroud, L.; LaGasse, L.; et al., Smoking during pregnancy and newborn neurobehavior, Pediatrics 111 (2003) 1318.
96. Lazarus, J.H.; Kokandi, A., Thyroid disease in relation to pregnancy: a decade of change, Clin Endocrinol 46 (2000) 381.
97. Lenke, R.R.; Levy, H.L., Maternal phenylketonuria and hyperphenylalaninemia: an international survey of the outcome of untreated and treated pregnancies, N Engl J Med 303 (1980) 1202.
98. Lenke, R.R.; Levy, H.L., Maternal phenylketonuria: results of dietary therapy, Am J Obstet Gynecol 142 (1982) 548.
99. Lin, S.; Munsie, J.P.; Herdt-Losavio, M.L.; et al., Maternal asthma medication use and the risk of gastrochisis, Am J Epidemiol 168 (2008) 73.
100. Loudon, J.A.; Groom, K.M.; Bennett, P.R., Prostaglandin inhibitors in preterm labour, Best Pract Res Clin Obstet Gynaecol 17 (2003) 731.
101. Ma, Y.; Goins, K.V.; Pbert, L.; et al., Predictors of smoking cessation in pregnancy and maintenance postpartum in low-income women, Matern Child Health J 9 (2005) 393.
102. Maillot, F.; Lilburn, M.; Baudin, J.; et al., Factors influencing outcomes in the offspring of mothers with phenylketonuria during pregnancy: the importance of variation in maternal blood phenylalanine, Am J Clin Nutr 88 (2008) 700.
103. Manning, F.A.; Morrison, I.; Lange, I.R.; et al., Fetal assessment based on fetal biophysical profile scoring: experience in 12,620 referred high risk pregnancies. I. Perinatal mortality by frequency and etiology, Am J Obstet Gynecol 151 (1985) 343.
104. March of Dimes Birth Defects Foundation. ( 2004) ; www.marchofdimes.com.
105. Matchaba, P.; Moodley, J., Corticosteroids for HELLP syndrome in pregnancy, Cochrane Database Syst Rev 1 (2004); CD002076.
106. Maurer, G.; Ambriola, D., Pregnancy following renal transplant, J Perinat Neonat Nurs 8 (1994) 28.
107. Meador, K.J.; Pennell, P.B.; Harden, C.L.; et al., Hope Work Group: Pregnancy registries in epilepsy: a consensus statement on health outcomes, Neurology 71 (2008) 1109.
108. Meador, K.J.; Reynolds, M.W.; Crean, S.; et al., Pregnancy outcomes in women with epilepsy: a systematic review and meta-analysis of the published pregnancy registries and cohorts, Epilepsy Res 81 (2008) 1.
109. Melvin, C.; Dolan, M.P.; Windsor, R.A.; et al., Recommended cessation counseling for pregnant women who smoke: a review of evidence, Tob Control 9 (2000) 1.
110. Montouris, G., Importance of monotherapy in women across the reproductive cycle, Neurology 69 (2007) S10.
111. Moore, T.R.; Piacquadio, K., A prospective evaluation of fetal movement screening to reduce the incidences of antepartum fetal death, Am J Obstet Gynecol 160 (1989) 1075.
112. Moroni, G.; Pontincelli, C., The risk of pregnancy in patients with lupus nephritis, J Nephrol 16 (2003) 161.
113. Motta, M.; Tincani, A.; Meroni, P.; et al., Follow-up of children exposed antenatally to immunosuppressive drugs, Rheumatology 47 (2008) iii32.
114. Mueller, B.A.; Zhang, J.; Critchlow, C.W., Birth outcomes and need for hospitalization after delivery among women with multiple sclerosis, Am J Obstet Gynecol 186 (2002) 446.
115. Murphy, V.E.; Clifton, V.L.; Gibson, P.G., Asthma exacerbations during pregnancy: incidence and association with adverse pregnancy outcomes, Thorax 61 (2006) 169.
116. Mustafa, S.A.; Brizot, M.L.; Carvalho, M.H.; et al., Transvaginal ultrasonography in predicting placenta previa at delivery: a longitudinal study, Ultrasound Obstet Gynecol 20 (2002) 356.
117. National Academy of Science, Nutrition during Pregnancy. I. Weight Gain. II. Nutritional Supplements, In: I.O.M. National Academy of Science, Food and Nutrition Board, Committee on Nutrition Status During Pregnancy ( 1990)National Academy Press, Washington DC.
118. Ness, A.; Visintine, J.; Ricci, E.; et al., Use of fetal fibronectin and transvaginal ultrasound cervical length to triage women with suspected preterm labor: a randomized trial, Am J Obstet Gynecol 195 (2006) 567.
119. Odegaard, I.; Stray-Pederson, B.; Hallberg, K.; et al., Maternal and fetal morbidity in pregnancies of Norwegian and Swedish women with cystic fibrosis, Acta Obstet Gynecol Scand 81 (2002) 698.
120. Odent, M., The rise of preconceptual counseling vs the decline of medicalized care in pregnancy, Birth Psychology ( 2002); Accessed September 13, 2006, fromhttp://birthpsychology.com/primalhealth/primal10.html.
121. Ogunyemi, D.; Hernandez-Loera, G.E., The impact of antenatal cocaine use on maternal characteristics and neonatal outcomes, J Matern Fetal Neonatal Med 15 (2004) 253.
122. Papatsonis, D.N.M.; Kok, J.H.; van Geijn, H.P.; et al., Neonatal effects of nifedipine and ritodrine for preterm labor, Obstet Gynecol 95 (2000) 477.
123. Patel, A.; Asopa, S.; Tang, A.T.; et al., Cardiac surgery during pregnancy, Tex Heart Inst J 35 (2008) 307.
124. Patti, F.; Cavallaro, T.; Lo Fermo, S.; et al., Is in utero early-exposure to interferon beta a risk factor for pregnancy outcomes in multiple sclerosis?J Neurol ( 2008); Epub ahead of print, PMID: 18677640.
125. Pauly, J.R.; Slokin, T.A., Maternal tobacco smoking, nicotine replacement and neurobehavioral development, Acta Paediatr 97 (2008) 1331.
126. Pedersen, J., The pregnant diabetic and her newborn. ed 2 ( 1977)Williams & Wilkins, Baltimore.
127. Pinkerton, K., Cystic fibrosis life expectancy: 2006. ( 2008) ; Accessed September 14,http://ezinearticles.com/?Cystic-Fibrosis-Life-Expectancy&id=353570; from.
128. Pirie, P.L.; Lando, H.; Curry, S.J.; et al., Tobacco, alcohol, and caffeine use and cessation in early pregnancy, Am J Prev Med 18 (2000) 54.
129. Pitt, C.; Sanchez-Ramos, L.; Kaunitz, A.M.; et al., Prophylactic amnioinfusion for intrapartum oligohydramnios: a meta-analysis of randomized controlled trials, Obstet Gynecol 96 (2000) 861.
130. Pittschieler, S.; Brezinka, C.; Jahn, B.; et al., Spontaneous abortion and the prophylactic effect of folic acid supplementation in epileptic women undergoing antiepileptic therapy, J Neurol ( 2008); Epub ahead of print, PMID:18677647.
131. Quintero, R.; Sepulveda, W.; Romero, R.; et al., Cord: Velamentous insertion, In: Fetal echocardiography 2009: An intense review course ( 2009); Accessed July 11,www.thefetus.net/1999; from.
132. Roberts, J., Pregnancy-related hypertension, In: (Editors: Creasy, R.K.; Resnick, R.) Maternal fetal medicineed 4 ( 1999)Saunders, Philadelphia.
133. Roberts, J.M.; Pearson, G.D.; Cutler, J.A.; et al., Summary of the NHLBI Working Group on Research on Hypertension During Pregnancy, Hypertens Pregnancy 22 (2003) 109.
134. Rosen, T.S.; Bateman, D.A., Infants of addicted mothers, In: (Editors: Fanoroff, A.A.; Martin, R.L.) Neonatal-perinatal medicineed 7 ( 2001)Mosby, St Louis.
135. Ross, M.G.; Gala, R., Use of umbilical artery base excess: algorithm for the timing of hypoxic injury, Am J Obstet Gynecol 187 (2002) 1.
136. Rotmensch, H.H.; Elkayam, U.; Frishman, W., Anti-arrhythmic drug therapy during pregnancy, Ann Intern Med 98 (1993) 487.
137. Ruiz-Irastorza, G.; Khamashta, M.A., Lupus and pregnancy: ten questions and some answers, Lupus 17 (2008) 416.
138. Sarno, A.P.; Wilson, R.D., Fetal cardiocentesis: a review of indications, risks, applications and technique, Fetal Diagn Ther 23 (2008) 237.
139. Scardo, J.A.; Hogg, B.B.; Newman, R.B.; et al., Favorable hemodynamic effects of magnesium sulfate in preeclampsia, Am J Obstet Gynecol 174 (1995) 1249.
140. Schatz, M.; Dombrowski, M.P.; Wise, R.; et al., Asthma morbidity during pregnancy can be predicted by severity classification, J Allergy Clin Immunol 112 (2003) 283.
141. Shankar, K.; Ronis, M.J.; Badger, T.M., Effects of pregnancy and nutritional status on alcohol metabolism, Alcohol Res Health 30 (2007) 55.
142. Sibai, B.M., The HELLP syndrome (hemolysis, elevated liver enzymes, and low platelets): much ado about nothing?Am J Obstet Gynecol 162 (1990) 311.
143. Sibai, B.M., Chronic hypertension in pregnancy, Obstet Gynecol 100 (2002) 1358.
144. Sibai, B.M., Diagnosis and management of gestational hypertension and preeclampsia, Obstet Gynecol 102 (2003) 181.
145. Sinha, P.; Kuruba, N., Ante-partum haemorrhage: an update, J Obstet Gynaecology 28 (2008) 377.
146. Siu, S.C.; Sermer, M.; Colman, J.M.; et al., Prospective multicenter study of pregnancy outcomes in women with heart disease, Circulation 104 (2001) 515.
147. Smaill, F.; Vasuez, J.C., Treatment of asymptomatic bacteriuria in pregnancy, Cochrane Database Syst Rev 18 (2) ( 2007); CD00490.
148. Stan, C.; Boulvain, M.; Hirsbrunner-Amagbaly, P.; et al., Hydration for treatment of preterm labour, Cochrane Database Syst Rev 2 (2002); CD003096.
149. Stotand, N.E.; Cheng, Y.W.; Hopkins, L.M.; et al., Gestational weight gain and adverse neonatal outcomes among term infants, Obstet Gynecol 108 (2006) 635.
150. Tata, L.J.; Lewis, S.A.; McKeever, T.M.; et al., Effect of maternal asthma, exacerbations and asthma medication use on congenital malformations in offspring: a UK population-based study, Thorax 63 (2008) 981.
151. Tekin, A.; Ozkan, S.; Caliskan, E.; et al., Fetal pulse oximetry: correlation with intrapartum fetal heart rate patterns and neonatal outcome, J Obstet Gynaecol Res 34 (2008) 824.
152. Tincani, A.; Bazzani, C.; Zingarelli, S.; et al., Lupus and the antiphospholipid syndrome in pregnancy and obstetrics: clinical characteristics, diagnosis, pathogenesis, and treatment, Semin Thromb Hemost 34 (2008) 267.
153. Tomson, T.; Perucca, E.; Battino, D., Navigating toward fetal and maternal health: the challenge of treating epilepsy in pregnancy, Epilepsia 45 (2004) 1171.
154. Tonelli, M.R.; Aitken, M.L., Pregnancy in cystic fibrosis, Curr Opin Pulm Med 13 (2007) 537.
155. Tropper, P.J.; Petrie, R.H., Placental exchange, In: (Editor: Lavery, J.P.) The human placenta: clinical perspectives ( 1987)Aspen Publications, Rockville, Md.
156. Trumbo, P.; Schlicker, S.; Yates, A.A.; et al., Dietary reference intakes for energy, carbohydrates, fiber, fat, fatty acids, cholesterol, protein and amino acids, J Am Diet Assoc 102 (2002) 1621.
157. Umans, J.G.; Lindheimer, M.D., Antihypertensive treatment, In: (Editors: Lindheimer, M.D.; Roberts, J.M.; Cunningham, F.G.) Chesley’s hypertensive disorders in pregnancyed 2 ( 1998)Appleton & Lange, Norwalk, Conn.
158. U.S. Department of Health and Human Services, The health consequences of smoking: a report of the Surgeon General: 2004, In: Centers for Disease Control and Prevention Office on Smoking and Health editor: ( 2008); Accessed, November 13,www.cdc.gov/tobacco/data_statistics/sgr/sgr_2004/index.htm#full; from.
159. U.S. Department of Health and Human Services, National survey on drug use and health: 2006. ( 2008) ; Accessed, November 12,www.oas.samhsa.gov/NSDUH/2k6NSDUH/2k6Results.pdf; from.
160. Vajda, F.J., Treatment options for pregnant women with epilepsy, Expert Opin Pharmacother 9 (2008) 1859.
161. Van Mieghem, T.; Van Schoubroeck, D.; Depiere, M.; et al., Fetal cerebral hemorrhage caused by vitamin K deficiency after complicated bariatric surgery, Obstet Gynecol 112 (2008) 434.
162. Vintzileos, A.M.; Campbell, W.A.; Rodes, J.F., Fetal biophysical profile scoring: current status, Clin Perinatol 16 (1989) 661.
163. Vukusic, S.; Hutchinson, M.; Hours, M.; et al., Pregnancy and multiple sclerosis (the PRIMS study): clinical predictors of post-partum relapse, Brain 127 (2004) 1353.
164. Waltuck, J.; Buyon, J.P., Autoantibody associated congenital heart block: outcome in mothers and children, Ann Intern Med 120 (1994) 544.
165. Wells, C.S.; Schwalberg, R.; Noonan, G.; et al., Factors influencing inadequate and excessive weight gain in pregnancy: Colorado 2000-2002, Matern Child Health J 10 (2006) 55.
166. West, J.R.; Blake, C.A., Fetal alcohol syndrome: an assessment of the field, Exp Biol Med 230 (2005) 354.
167. Westgate, J.A.; Wibbens, B.; Bennet, L.; et al., The intrapartum deceleration in center stage: a physiologic approach to the interpretation of fetal heart rate changes in labor, Am J Obstet Gynecol 197 (2007) 236.
168. Whittemore, R., Congenital heart disease: its impact on pregnancy, Hosp Pract 18 (1983) 65.
169. Worthington, J.; Jones, R.; Crawford, M.; et al., Pregnancy and multiple sclerosis: a three-year prospective study, J Neurol 241 (1994) 228.
170. Zhang, X.; Decker, A.; Platt, R.W.; et al., How big is too big? The perinatal consequence of fetal macrosomia, Am J Obstet Gynecol 198 (2008) 517.e1.