165 Potassium
• Insulin enhances the activity of the sodium-potassium adenosine triphosphate pump, with a resultant decrease in extracellular potassium. Patients with diabetes mellitus are predisposed to hyperkalemia because of impaired insulin feedback and subsequently poor intracellular transfer of potassium.
• Asthmatic patients treated with bronchodilator therapy or epinephrine are predisposed to hypokalemia.
• Renal failure is responsible for the majority of cases of critical hyperkalemia seen in the emergency department.
• Calcium normalizes electrocardiographic manifestations of hyperkalemia within minutes of administration; however, the clinical effects are generally short-lived. Doses may need to be repeated within 30 minutes.
• Regular (short-acting) insulin administered as a 10-unit intravenous bolus will begin to lower serum potassium concentrations within 10 to 20 minutes, and the clinical effect lasts several hours. An ampule of 50% dextrose in water should be given concurrently to prevent hypoglycemia.
• Nebulized albuterol in 10- to 20-mg continuous treatments will transiently decrease serum potassium by 1 mEq/L over a 1- to 2-hour period.
• Definitive treatment of hyperkalemia is elimination of potassium. Hemodialysis is indicated for severe cases of hyperkalemia; when potassium-free dialysate is used, hemodialysis can reduce serum potassium by 1.5 mEq/hr.
Perspective
Potassium is the major intracellular cation and is closely regulated by the sodium-potassium adenosine triphosphatase (Na+,K+-ATPase) pump. Hypokalemia and hyperkalemia are electrolyte abnormalities common to both hospitalized and emergency department (ED) patients.1
Hypokalemia is observed more frequently than hyperkalemia and affects a broader range of patients; diuretic therapy accounts for as much as 80% of clinically significant cases seen in the ED.2 Hypokalemia is defined as a serum potassium level lower than 3.5 mEq/L. It is further classified as mild (3 to 3.5 mEq/L), moderate (2.5 to 2.9 mEq/L), and severe (<2.5 mEq/L).
Hyperkalemia, a disorder that affects patients with underlying renal insufficiency almost exclusively,1 is defined as a potassium level higher than 5.0 mEq/L. Hyperkalemia is further classified as mild (5 to 6 mEq/L), moderate (6.1 to 7 mEq/L), and severe (>7 mEq/L).
Both disorders can result in cardiac dysfunction, arrhythmia, and death.
Pathophysiology
Total body potassium (K+) is approximately 50 mEq/kg, or 3500 to 4000 mEq, in a normal-sized adult. For conversion purposes, 1 mEq of potassium is equivalent to 39.09 mg. Potassium is the major intracellular cation, and more than 98% of total body potassium is stored in the intracellular space. Intracellular fluid concentrations of potassium range from 150 to 160 mEq/L, with the highest amounts sequestered either in muscle (75%) or in bones and cartilage (8% to 10%).2
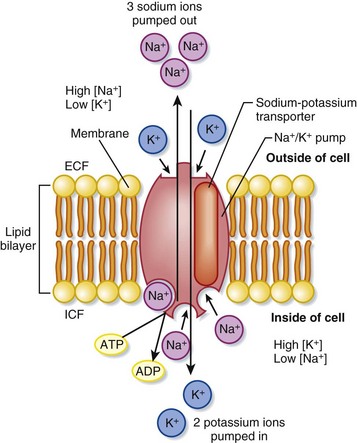
Extracellular potassium makes up less than 2% of total body stores, only two thirds of which is measurable in serum sampling. The normal range of plasma concentrations reported by most laboratory testing is 3.5 to 5 mEq/L; this small fraction is not reflective of total body potassium. Strict regulation of the ratio of intracellular to extracellular potassium (150 to 4 mEq/L) maintains a critical voltage gradient across cell membranes and plays a crucial role in establishing membrane potentials in cardiac and neuromuscular cells.1 The Na+,K+-ATPase transmembrane pump continuously maintains this gradient by actively transporting potassium into and sodium (Na+) out of cells1 (Fig. 165.1). Large changes in the intracellular potassium concentration have little effect on the ratio of intracellular to extracellular potassium. Conversely, even small changes in the extracellular concentration significantly affect this ratio, the transmembrane potential gradient, and the function of cardiac and neuromuscular tissue.1
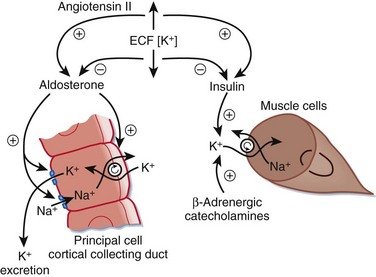
All potassium disorders result from one of three disturbances3: impaired potassium intake, impaired distribution of potassium between the intracellular and extracellular spaces, and impaired renal excretion of potassium (Fig. 165.2).
Clinical Presentation
Hypokalemia
Approximately 20% of hospitalized patients are found to have subtherapeutic serum potassium levels.1 Despite this disease prevalence, most patients are asymptomatic, and only 5% of these patients have clinically significant hypokalemia.
In the outpatient setting, roughly 18% of patients have mild hypokalemia, which is generally asymptomatic. The vast majority of these cases (80%) are caused by potassium-wasting diuretic medications.2 Men and women are affected equally.
Box 165.1 summarizes the clinical findings of hypokalemia.
Box 165.1
Clinical Findings in Hypokalemia
Modified from Zull DN. Disorders of potassium metabolism. Emerg Med Clin North Am 1989;7:771–94.
Moderate Hypokalemia (2.5 to 2.9 mEq/L)
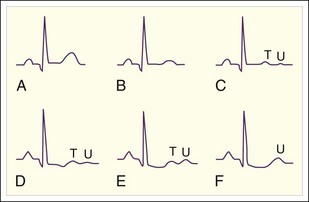
Muscular symptoms become more pronounced as the degree of hypokalemia worsens; the weakness is generalized, but proximal and lower extremity muscle groups are typically affected to a greater degree.2 Cardiac manifestations may include palpitations, non–life-threatening dysrhythmias (premature atrial contractions, premature ventricular contractions), and atrial fibrillation. Electrocardiographic (ECG) changes occur but do not correlate with the degree of hypokalemia (Box 165.2; Fig. 165.3).
Box 165.2
Electrocardiographic Abnormalities in Mild to Moderate Hypokalemia
Low, flattened, or inverted T waves
Potassium concentration usually less than 3.5 mEq/L
Adapted from Cohn JN, Kowey PR, Whelton PK, et al. New guidelines for potassium replacement in clinical practice. Arch Intern Med 2000;160:2429–46; and Zull DN. Disorders of potassium metabolism. Emerg Med Clin North Am 1989;7:771–94.
Hypokalemia may precipitate or worsen encephalopathy in patients with severe liver disease. Potassium depletion increases renal production of ammonia, which readily crosses the blood-brain barrier in the setting of alkalosis.2 Hypokalemia also inhibits the release of insulin and may cause hyperglycemia in patients with preexisting glucose intolerance or non–insulin-dependent diabetes mellitus. The renal complications of moderate hypokalemia reflect vasopressin resistance to the tubular reabsorption of water; symptoms include nocturia, polydipsia, and polyuria.2
Severe Hypokalemia (<2.5 mEq/L)
Alcoholics have the greatest risk for severe hypokalemia. Musculoskeletal symptoms include pronounced fasciculations, tetany, and rhabdomyolysis. Myolysis may cause a transient release of intracellular potassium that can mask the inciting hypokalemic state. In rare cases, life-threatening ascending paralysis and loss of deep tendon reflexes can result in quadriplegia.2
Cardiac manifestations of severe hypokalemia worsen the previously mentioned ECG abnormalities. Of great concern is the development of potentially life-threatening ventricular arrhythmias in patients with preexisting cardiac disease. Ventricular ectopy ranges from premature ventricular contractions to couplets, bigeminy, trigeminy, and episodes of ventricular tachycardia, torsades de pointes, and ventricular fibrillation. In the setting of myocardial infarction or digitalis toxicity, hypokalemia-induced ventricular dysrhythmias are directly proportional to the degree of potassium depletion.2
Hyperkalemia
Moderate Hyperkalemia (6.1 to 7 mEq/L)
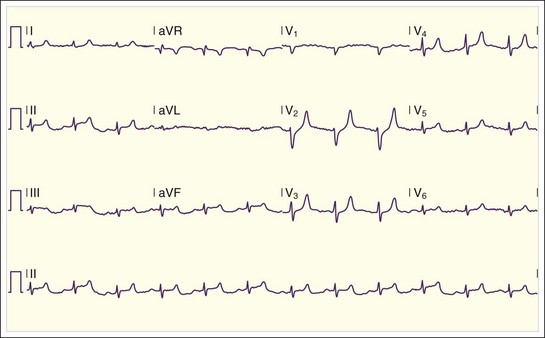
Patients with moderate hyperkalemia may exhibit ECG abnormalities, including peaked T waves and prolongation of the PR interval and QRS complex4 (Figs. 165.4 to 165.7; Box 165.3).
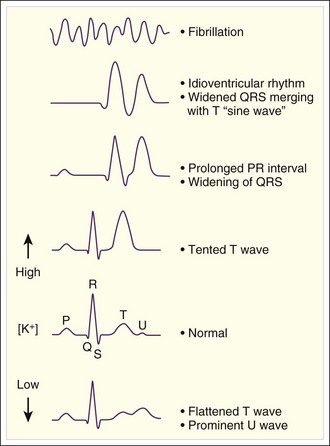
Fig. 165.4 Electrocardiographic findings in hyperkalemia.
(Adapted from Gennari FJ. Disorders of potassium homeostasis: hypokalemia and hyperkalemia. Crit Care Clin 2002;18:273–88.)
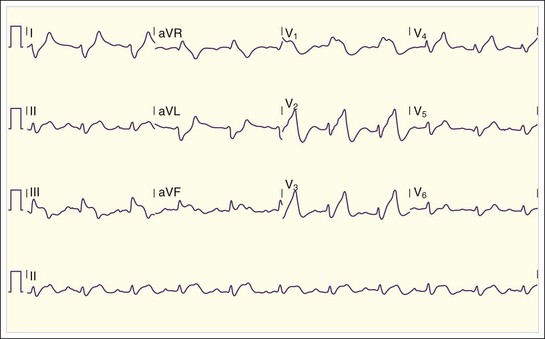
Fig. 165.6 Patient with severe hyperkalemia on arrival at the emergency department (K+ = 8.3 mmol/L).
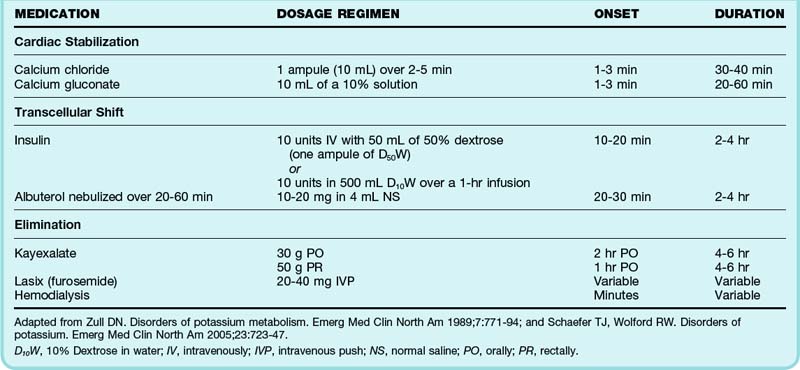
Treatment (Table 165.1)
Hypokalemia
Patients with Cardiovascular Disease
Optimal goals for serum potassium repletion are predicated on the underlying pathology. Patients with a history of congestive heart failure, coronary artery disease, or dysrhythmias and hypertensive patients being treated with diuretic medications should have a serum potassium level of at least 4 mEq/L. These patients require oral supplementation for even mild, asymptomatic hypokalemia with potassium chloride tablets (20 to 40 mEq daily).5 If the patient is taking a potassium-sparing diuretic, the dose should be decreased.
| FORMULATION | DOSAGE REGIMEN | INDICATION |
|---|---|---|
| Oral KCl | 20-80 mEq/day divided 2-3 times per day | Non-urgent correction and/or maintenance therapy with diuretic use |
| Oral KCl liquid (recheck serum K+ in 24-72 hr) | 40-60 mEq per dose | Rapid elevation in patients requiring urgent, but not emergency correction |
| Intravenous KCl | 10-20 mEq/hr (recheck serum K+ after giving 60 mEq) | For patients with severe symptoms or inability to tolerate oral therapy |
Adapted from Zull DN. Disorders of potassium metabolism. Emerg Med Clin North Am 1989;7:771–94; and Schaefer TJ, Wolford RW. Disorders of potassium. Emerg Med Clin North Am 2005;23:723–47.
Asymptomatic Mild Hypokalemia
Healthy patients with asymptomatic, mild hypokalemia (3 to 3.5 mEq/L) do not require pharmacologic potassium supplementation. Treatment should be focused on minimizing further potassium loss and increasing oral intake. Patients should be encouraged to eat a diet rich in potassium (Box 165.4). Potassium-wasting diuretics should be decreased or eliminated, as blood pressure allows. Use of substances that contain glycyrrhizic acid (e.g., licorice, chewing tobacco, laxatives) should be avoided.1,6
Symptomatic Mild and Moderate Hypokalemia
Potassium supplementation is required for patients with symptomatic mild or moderate (<3 mEq/L) hypokalemia. Potassium supplements are available in several forms: potassium chloride, potassium phosphate, potassium citrate, potassium acetate, potassium gluconate, and potassium bicarbonate. Potassium chloride is the preferred formulation for most ED cases of hypokalemia. Potassium phosphate may be beneficial in certain cases of diabetic ketoacidosis.6 Oral potassium supplements are available as tablets, powder, or elixir.
Dosing ranges from 20 to 80 mEq/day; doses greater than 40 mEq should be divided and given either two or three times per day. Oral therapy should be monitored daily because serum potassium levels will rise within 48 to 72 hours.6 Healthy patients who require daily oral supplementation can be discharged from the ED safely if repeated serum potassium measurements can be monitored by the primary care physician for 1 to 2 days. Patients who are elderly, have significant comorbid conditions, or have poor access to follow-up should be admitted to the hospital for a 24-hour observation period.
Magnesium deficiency should be suspected in patients who fail to respond to oral potassium therapy within 96 hours. Magnesium promotes activity of the Na+,K+-ATPase pump, which will replenish intracellular fluid concentrations in the first days of potassium supplementation.6
Severe Hypokalemia
Intravenous (IV) potassium replacement is indicated for patients with severe hypokalemia (<2.5 mEq/L) or moderate hypokalemia accompanied by cardiac arrhythmias, familial periodic paralysis, or severe myopathy.6
IV potassium supplementation can cause excruciating phlebitis and cardiac arrest if directly injected into a vessel—potassium should never be administered as an IV push. Peripheral IV lines can be used for rates of 10 to 20 mEq/hr or less. In cases of moderate hypokalemia, potassium infusions should remain at 10 mEq/hr. To minimize the risk for phlebitis, a central line is necessary for infusion rates greater than 20 mEq/hr (see earlier indications). There is a theoretic concern for cardiac arrest when potassium is administered via central venous access—splitting the potassium infusion rate over two peripheral lines may be preferable.2
Unstable ventricular arrhythmias resulting from severe hypokalemia should be managed according to standard practice guidelines. Severe neuromuscular manifestations may endanger adequate respiratory effort and therefore mandate aggressive airway stabilization. Any volume depletion should be corrected, and coexisting medical conditions that may exacerbate the effects of hypokalemia should be addressed.1
Hyperkalemia
Management of hyperkalemia focuses on three goals of care: cardiac stabilization, transcellular shift of potassium from extracellular fluid to intracellular fluid, and elimination of excess potassium (Table 165.2). Only potassium excretion is a definitive treatment step—other actions serve to temporarily stabilize the cell membrane in an effort to prevent hemodynamic collapse.
Cardiac Stabilization: Calcium
IV calcium rapidly antagonizes the adverse effects of moderate to severe hyperkalemia on cell membrane potential in cardiac myocytes. Calcium can be administered as IV calcium chloride or calcium gluconate, even in patients who are normocalcemic. IV preparations of calcium chloride contain three times more calcium per ampule than do calcium gluconate formulations. Calcium chloride is more likely than calcium gluconate to cause tissue necrosis if it extravasates.7 Calcium normalizes ECG manifestations of hyperkalemia within minutes of administration; however, the clinical effects are generally short-lived. Doses may need to be repeated within 30 minutes or if no effects are observed within 5 to 10 minutes of the initial dose. Calcium should be administered to patients with hyperkalemia-induced ECG changes, and caution should be exercised in patients taking digoxin.
![]() Red Flags
Red Flags
Calcium Supplementation
Calcium chloride may cause significant skin necrosis if extravasated.
Calcium should not be administered with solutions that contain sodium bicarbonate because calcium carbonate (CaCO3) will precipitate.
Intravenous calcium boluses should be avoided in hyperkalemic patients with suspected digoxin toxicity because of the risk for cardiac tetany or fatal arrhythmia. Slow calcium infusions (over a 30-minute period) require close monitoring of these patients.
Transcellular Shift: Insulin and Albuterol
Albuterol is the most readily available β2-agonist used to treat hyperkalemia in the ED. Nebulized albuterol in 10- to 20-mg continuous treatments will decrease serum potassium by 1 mEq/L over a 1- to 2-hour period.8 Though not approved for use in the United States, IV administration of albuterol shifts potassium into the intracellular fluid compartment even more rapidly. Once routinely used for treatment of hyperkalemia, the use of sodium bicarbonate has been challenged. Recent studies have demonstrated that sodium bicarbonate may only enhance urinary elimination of potassium and does not function at a cellular level. It may especially have a deleterious effect on anuric patients and worsen the degree of intracellular acidosis.9
Elimination: Resin Exchange (Kayexalate) and Dialysis
Sodium polystyrene sulfonate (Kayexalate) is an inert resin that exchanges sodium for potassium in the intestinal tract. One gram of Kayexalate removes approximately 0.5 to 1 mEq of potassium in exchange for 2 to 3 mEq of sodium.8 The usual dose of Kayexalate is 30 to 60 g given orally or rectally. Oral Kayexalate begins to reduce total body potassium within several hours of administration, and the clinical effect lasts 4 to 6 hours. Rectal Kayexalate has a shorter time to onset than the oral formulation but is less efficacious.
Emerging literature questions the efficacy and safety of Kayexalate. Although Kayexalate reliably decreases serum potassium when administered over a period of several days, recent literature reviews suggest that the acute effects of the resin may not be as significant as once thought.10 Colonic necrosis, ischemic colitis, colonic bleeding, and perforation have been reported when Kayexalate is combined with 70% sorbitol.9 Kayexalate is often premixed with 33% sorbitol to prevent resin-induced constipation, and there is little evidence to suggest that Kayexalate with 33% sorbitol causes significant colonic pathology at standard doses.11 Very rare instances of colonic injury have been observed when 33% sorbitol is coadministered with Kayexalate as an enema to patients after recent colon surgery.10,11 High-dose Kayexalate precipitates pulmonary edema by increasing extracellular sodium in fluid-overloaded patients.
1 Schaefer TJ, Wolford RW. Disorders of potassium. Emerg Med Clin North Am. 2005;23:723–747.
2 Zull DN. Disorders of potassium metabolism. Emerg Med Clin North Am. 1989;7:771–794.
3 Gaffar M. Diagnosis and treatment of hyperkalemia. Resid Staff Physician. 2003;49:18–22.
4 Mattu A, Brady WJ, Robinson DA. Electrocardiographic manifestations of hyperkalemia. Am J Emerg Med. 2000;18:721–729.
5 Cohn JN, Kowey PR, Whelton PK, et al. New guidelines for potassium replacement in clinical practice. Arch Intern Med. 2000;160:2429–2436.
6 Mandal AK. Hypokalemia and hyperkalemia. Med Clin North Am. 1997;81:611–639.
7 Weisberg LS. Management of severe hyperkalemia. Crit Care Med. 2008;36:3247–3251.
8 Weiner ID, Wingo CS. Hyperkalemia: a potential silent killer. J Am Soc Nephrol. 1998;9:1535–1543.
9 Rachoin JS, Cerceo EA. Four nephrology myths debunked. J Hosp Med. 2011;6(5):E1–E5.
10 Sterns RH, Rojas M, Bernstein P, et al. Ion-exchange resins for the treatment of hyperkalemia: are they safe and effective? J Am Soc Nephrol. 2010;21:733–735.
11 Watson M, Abbott KC, Yuan CM. Damned if you do, damned if you don’t: potassium-binding resins in hyperkalemia. Clin J Am Soc Nephrol. 2010;5:1723–1726.