Postoperative nausea and vomiting
Postoperative nausea and vomiting (PONV) is the most frequent side effect that occurs after exposure to anesthetic agents, occurring in 20% to 30% of the general surgical population and up to 80% in high-risk patients. Although PONV is self-limiting, it increases patients’ dissatisfaction and can be associated with significant morbidity (Box 109-1). PONV also results in higher costs from treatment, delayed discharge from the postanesthesia care unit or the hospital, and unplanned hospitalization.
Physiology
The vomiting center of the brain, in the reticular formation, receives input from the chemotactic trigger zone, gastrointestinal tract, vestibular portion of the eighth cranial nerve, and pharynx. Important neurotransmitter receptor sites documented, or suspected, to be associated with PONV include serotonin, dopamine, histamine, neurokinin-1, opioid, acetylcholine, and muscarinic receptor sites (see Chapter 98).
Risk factors
Identification of independent risk factors for PONV is complicated because of limitations in study designs and the wide array of variables influencing PONV, including patient-related, surgery-related, and anesthesia-related factors. Some risk factors appear to be well established (Box 109-2). Other factors may be associated with PONV, but confirmation of these factors will require additional investigation. Factors that are unlikely to increase the incidence of PONV include obesity, higher intraoperative inspired fraction of O2 (50%-80% vs. 30%), and early stage of the menstrual cycle (Figure 109-1).
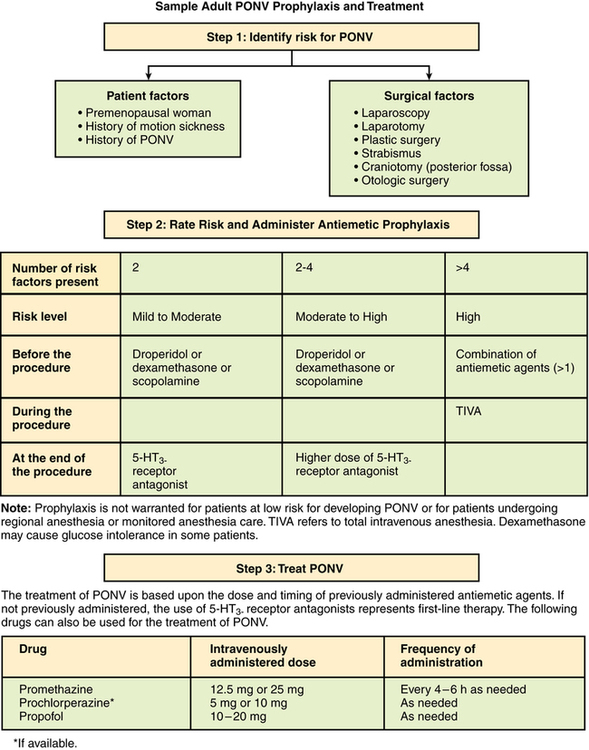
Several risk-scoring systems have been developed; they combine various established risk factors in an attempt to simplify and predict the likelihood of PONV occurring (see Box 109-2). Identification of high-risk patients will allow a more effective and cost-efficient prophylactic treatment program to be established, whereas low-risk patients (i.e., most general surgical patients) would be spared the added expense and possible side effects of treatment.
Treatment
The next steps in preventing PONV are to identify high-risk patients and administer an effective prophylactic program to them. Next, any underlying causes of hypotension or cerebral hypoxia should be identified and corrected. For patients who develop PONV, treatment options include nonpharmacologic measures, such as acupuncture, acupressure, and transcutaneous electrical nerve stimulation, and the administration of antiemetic agents, either individually or in combination from the various classes (see Chapter 98).




