Chapter 25 Posterior Approach to the Thoracic Spine
TOTAL EN BLOC SPONDYLECTOMY—THORACIC SPINE
INDICATIONS
En bloc spondylectomy is the treatment of choice for solitary and oligometastatic spinal metastases, with biologically favorable histological findings.1 In appropriately selected patients, neurological outcome, pain control, and oncological control are significantly better after en bloc spondylectomy compared with radiation therapy. Oncological outcomes also exceed those of intralesional techniques. Total en bloc spondylectomy (TES) decreases the rate of local recurrence and can provide long-term survival in selective patients with spinal metastasis.2
SURGICAL TECHNIQUE
Total spondylectomy is performed through the posterior procedure alone or through the anteroposterior combined procedure. The TES technique consists of two steps: en bloc resection of the posterior element and en bloc resection of the anterior column.1,3
En Bloc Resection of the Posterior Element of the Vertebra by Posterior Approach
Exposure
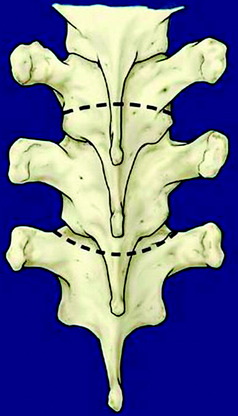
The patient is placed in a prone position over a four-poster frame to prevent compression to the vena cava. A straight, vertical, midline incision is made over the spinous processes and is extended three vertebrae above and below the involved segments. The paraspinal muscles are dissected from the spinous processes and the laminae, and then retracted laterally over the facet joint. After a careful dissection, a large retractor is applied. The surgical field must be wide enough on both sides to allow for dissection under the surface of the transverse processes. In the thoracic spine, the ribs on the affected level are transected 3–4 cm lateral to the costotransverse joint, and the pleura is separated bluntly from the vertebra. To expose the superior articular process of the uppermost vertebra, the spinous and the inferior articular processes of the neighboring vertebra are osteotomized and removed with dissection of the attached soft tissues, including the ligamentum flavum (Fig. 25-1). After the spinous process, lower part of lamina, and inferior facet are removed, the dorsal dura is exposed.3,4
INTRODUCTION OF THE T-SAW GUIDE
Using blunt-tipped dissectors, the soft tissue attached to the inferior aspect of the pars interarticularis is dissected and removed to prevent damage to the corresponding nerve root. A c-curved, malleable, T-saw guide is then introduced through the intervertebral foramen in a cephalocaudal direction.3 In this procedure, the tip of the T-saw guide should be introduced along the medial cortex of the lamina and the pedicle so that the spinal cord and the nerve root are not injured. After the T-saw guide is passed, its tip at the exit of the nerve root canal can be found beneath the inferior border of the pars interarticularis. In the next step, a flexible threadwire saw (0.54 mm in diameter) is passed through the hole in the T-saw guide and is clamped at each end. The T-saw guide is removed, and tension on the threadwire saw is maintained. This procedure also is applied to the contralateral side.
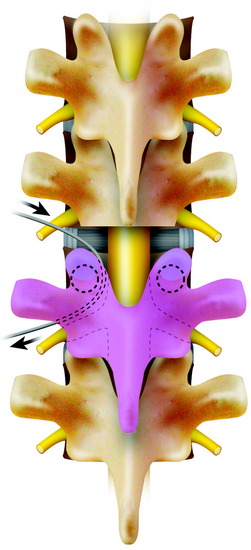
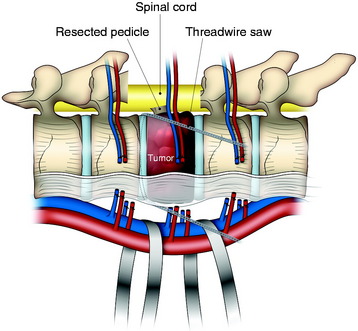
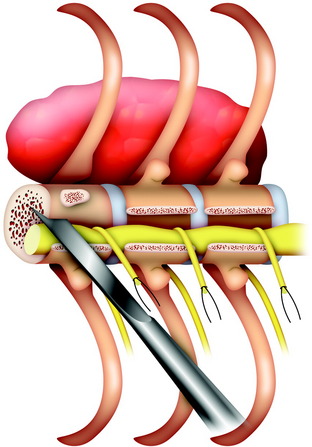
CUTTING THE PEDICLES AND RESECTION OF THE POSTERIOR ELEMENT
While tension is maintained, the threadwire saw is placed beneath the superior articular and transverse processes. With this procedure, the saw placed around the lamina is moved to around the pedicle. With a reciprocating motion of the saw, the pedicles are cut, and then the whole posterior element of the spine (the spinous process, the superior and inferior articular processes, the transverse process, and the pedicle) is removed in one piece (Fig. 25-2). The cut surface of the pedicle is sealed with bone wax to reduce bleeding and to minimize contamination by tumor cells.
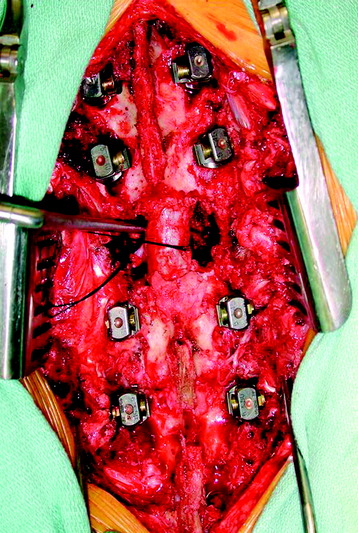
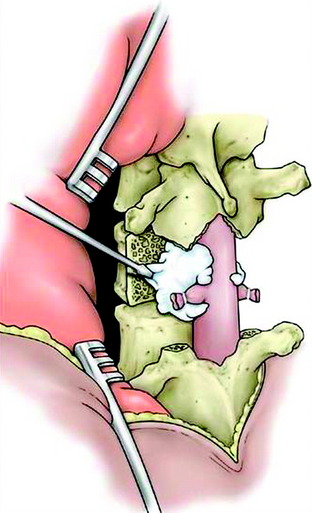
If the unilateral pedicle is affected by the tumor, osteotomy is performed through a healthy lamina, and the cut surface is blocked with bone wax immediately after osteotomy. The threadwire saw is passed under the lamina in a sublaminar fashion after carefully dissecting a passageway for it in the epidural space. If the tumor invades the bilateral pedicles and the pedicle and lamina, an electric cautery knife is inserted into the affected pedicle to coagulate tumor tissue inside the pedicle before pediculotomy to prevent tumor cell contamination. In these cases, the nerve root involved sometimes has to be ligated and included into the tumor mass. If the affected pedicle or vertebral body markedly compresses the nerve root, the more severely affected side is sacrificed. In the thoracic regions, the nerve root can be sacrificed without any functional deficit, except for the T1 nerve root.5 After the posterior bony column is removed, the epidural and foraminal vessels are meticulously coagulated using bipolar coagulator. Before the anterior column is resected, a posterior instrumentation should be performed (Fig. 25-3).
En Bloc Corpectomy By Posterior Approach
POSTERIOR LIGAMENTOUS RELEASE OF THE VERTEBRAL BODY
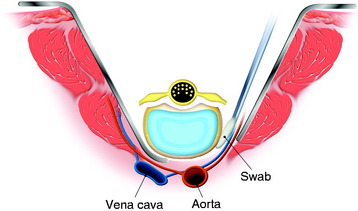
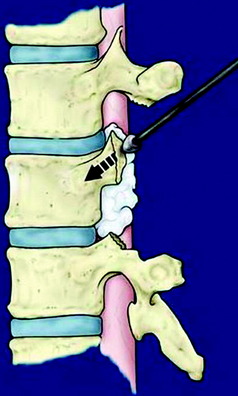
At the beginning of the second step, the segmental arteries must be identified bilaterally. The spinal branch of the segmental artery, which runs along the nerve root, is ligated and divided. This procedure exposes the segmental artery, which appears just lateral to the cut edge of the pedicle. In the thoracic spine, the nerve root is cut on the side from which the affected vertebra is removed. The blunt dissection is performed anteriorly on both sides through the plane between the pleura (or the iliopsoas muscle in lumbar spine) and the vertebral body. Usually, the lateral aspect of the body is dissected easily with a curved vertebral spatula. Then the segmental artery should be dissected from the vertebral body. To aid with retraction of paraspinal structures, cottonoids or rolled gauze pads can be inserted between the vertebra and laterally dissected tissue. By continuing dissection of both lateral sides of the vertebral body anteriorly, the aorta is carefully dissected posteriorly from the anterior aspect of the vertebral body with a spatula and the surgeon’s fingers. After dissection of the lateral surface, the dural sac is freed from the posterior longitudinal ligament (PLL), and the medial portion of the annulus fibrosus is sharply divided with a knife under direct visualization (Fig. 25-4). For the anterior release of great vessels from the anterior longitudinal ligament, blunt finger dissection is applied. After the potential space has undergone finger dissection, a series of spatulas, starting from the smallest size, is inserted sequentially to extend the dissection. A pair of the largest spatulas is kept between the anterior surface of the vertebral body and great vessels to maintain the dissected space and to make the surgical field wide enough for manipulating the anterior column.
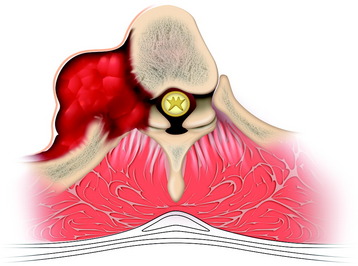
DISSECTION OF THE SPINAL CORD AND REMOVAL OF THE VERTEBRA
Using a cord spatula, the spinal cord is mobilized from the surrounding venous plexus and the ligamentous tissue. The cord protector, which has teeth on both edges to prevent the threadwire saw from slipping, is then applied. The anterior and posterior longitudinal ligaments are cut by the threadwire saw. After cutting the anterior column, the mobility of the vertebra is checked again to ensure a complete corpectomy. The freed anterior column is rotated around the spinal cord and removed carefully. With this procedure, a complete anterior and posterior decompression of the spinal cord (circumferential decompression) and total en bloc resection of the vertebral tumor are achieved (Fig. 25-5).
Corpectomy With Anterior Approach
Anterior column removal can be done with a separate incision after position change.
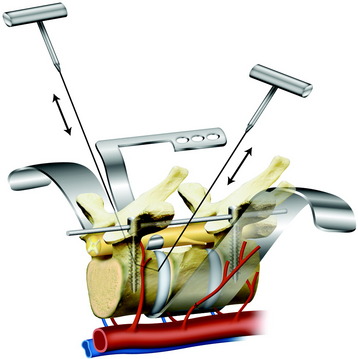
If the posterior ligamentous release procedure is complete, the anterior procedure is easy. The lateral approach is favored. The ipsilateral segmental vessels are identified and dissected off from the vertebral body. The elevation of the segmental vessels makes it easy to dissect the great vessels from the anterior longitudinal ligament. After the great vessels are away from the anterior longitudinal ligament, contralateral segmental vessels are seen. They can be dissected away from the vertebral body surface. All the vascular structures are kept off the vertebral body, which means the vertebral body is freed from the surrounding structures. Proximal and distal discs are removed with a knife or threadwire saw (Fig. 25-6).
THE STAGE OPERATION OF THORACIC SPINE TUMORS WITH INVOLVEMENT OF THE RIBS
INDICATIONS
This approach is indicated in cases of thoracic spinal tumors with rib involvement.6,7
Rib involvement of a thoracic tumor can have several causes (Fig. 25-7). First, a malignant vertebral body tumor, primary or secondary, develops from the bone marrow of the vertebral body and invades the pedicle, breaking the cortical margin. Then adjacent rib head is involved. As a result, tumor spread to the rib bone can form a paraspinal mass.
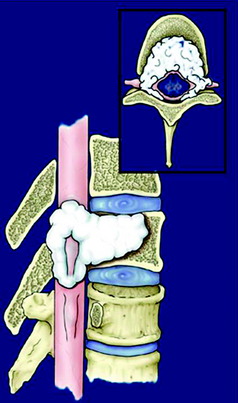
Second, the paraspinal structures, such as a sympathetic ganglion, can be the source of the tumor, such as a paraganglioma. Third, hematogenous malignancy, such as lymphoma, can be the diagnosis of the paraspinal mass. In this case, the tumors invade the spinal canal without destruction of the pedicles (Fig. 25-8). These tumors can be attacked posteriorly only, or from both directions.
INCISION AND POSITIONING
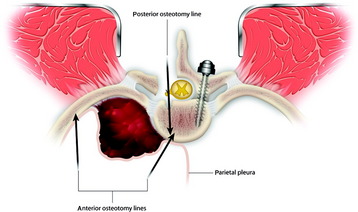
The resection plan for the tumor mass is set from both sides. Anteriorly the vertebral body and proximal rib are included. Posteriorly partial body resection is performed just lateral to the spinal cord (Fig. 25-9).
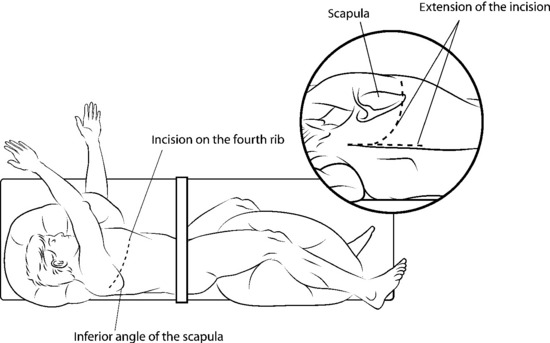
The patient is positioned in the left lateral decubitus position with the right arm elevated.8 If the lesion is located on the T6 and T7 body, a straight incision is made along the fourth rib from just lateral to the paraspinal muscles, and the fourth rib is removed (Fig. 25-10).
The posterior end of the incision is then extended cranially and caudally in a Y-shaped fashion for the posterior approach.8 Posterior spinal elements are exposed subperiosteally from T5 to T8. A laminectomy is performed from T5 to T8, revealing the thecal sac. The T6, T7, and T8 nerve roots are coagulated and severed (Figs. 25-11 and 25-12).
After the roots are retracted, the vertebral body is then penetrated from the posterior cortex to the anterior cortex (Fig. 25-13). The medial aspects of the T6 and T7 pedicles are secured, and the vertebral osteotomy is completed by penetrating posteroanteriorly, while still protecting the spinal cord and the major vessels (see Fig. 25-11).
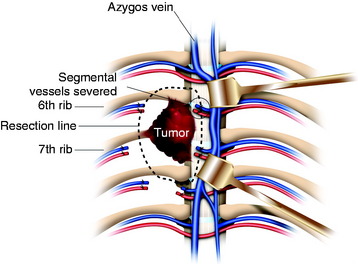
With the anterolateral skin incision, the anterolateral surface of the vertebral body is exposed. Segmental vessels are ligated and severed (Fig. 25-14). The sixth, seventh, and eighth ribs and the intercostal muscles around the tumor covered by the parietal pleura as a barrier are severed with at least a 1-cm margin to the tumor. An anterior osteotomy of T6 and T7 is performed using a chisel with more than 1 cm margin to the tumor.
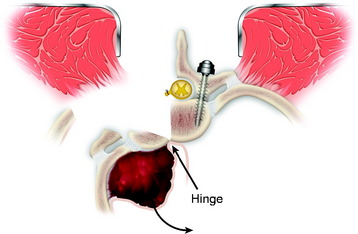
The tumor mass, including parts of the vertebrae, pedicles, transverse processes, and ribs, is removed en bloc by turning it anteriorly, using the anterior margin of the vertebra as a hinge, and avoiding injury to the spinal cord (Fig. 25-15).
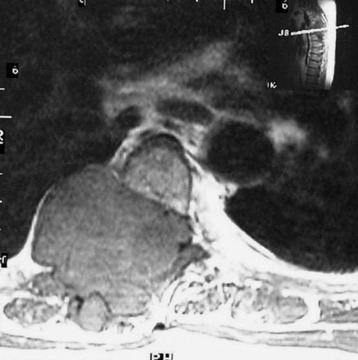
Case I
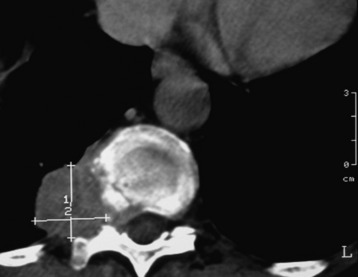
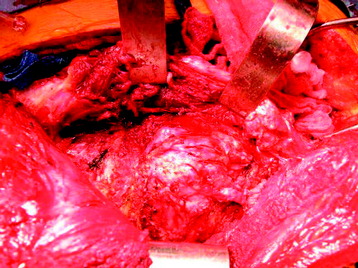
A 48-year-old male patient complained of thoracic back pain with intercostal pain around the right nipple area. The work-up for the patient showed that a right paraspinal mass originated from the right fourth rib and invaded the adjacent pedicle and lamina (Fig. 25-16). The nature of the mass seemed to be bony. Computed tomography (CT) scan showed the hyper-dense lesion. However, the mass did not invade the thoracic cavity. The patient was operated on in the prone position (Fig. 25-17). A T-shaped incision was made. After the muscle incision, the erector spinae muscles were retracted to the medial side (Fig. 25-18). Laminectomy was performed, and the roots were cut and tied (Fig. 25-19). The roots were retracted to the midline, and the facet was removed with partial corpectomy. Rib masses were dissected from surrounding muscles (see Fig. 25-18). The vertebral body was removed with facet and adjacent ribs. After the rib and facet were removed along with the parietal pleura, the lung tissue was exposed (see Fig. 25-19). The mass was removed en bloc (Fig. 25-20). The pathology was osteochondroma.
SINGLE-STAGE POSTEROLATERAL TRANSPEDICULAR APPROACH FOR SPONDYLECTOMY AND EPIDURAL DECOMPRESSION9
The posterior bone work is initiated by removing the spinous processes with a rongeur, then a drill or Kerrison rongeur. The presence of an anterior mass compressing the spinal cord prohibits the use of large Kerrison rongeurs in the spinal canal. The laminectomy includes the bone overlying the disc spaces adjacent to the involved vertebral body segment and a normal dural plane adjacent to the epidural tumor (Fig. 25-21). Bilateral facetectomies and complete pedicle resection to the base of the vertebral body are accomplished with the drill and curettes (Figs. 25-22 and 25-23). In the lumbar spine, a unilateral facetectomy is often sufficient to gain exposure to the vertebral body tumor.
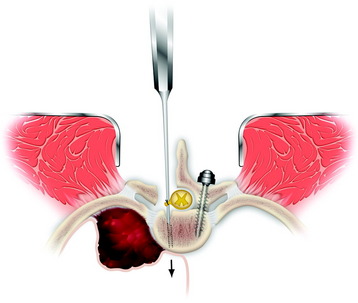
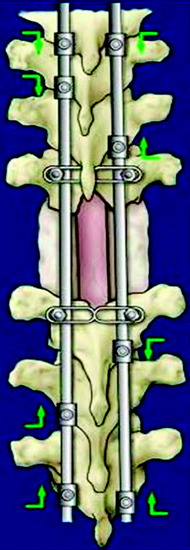
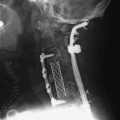
It is rare for a tumor to insinuate between the PLL and the dura. In these cases, the anterior compressive tumor appears bilobed with a hypointense line on magnetic resonance imaging (MRI), representing the PLL, between the vertebral body tumor and the spinal dura. Resection of the intact PLL helps provide a gross resection of tumor at the anterior dura. In the thoracic spine, the plane between the dura and PLL may be difficult to identify, but can be sharply dissected with tenotomy scissors (Fig. 25-24). Curettage or blunt dissection of the ligament may put excessive traction on the spinal dura and should be avoided. Once the anterolateral plane between the dura and PLL has been identified, the PLL often can be dissected along the anterior dura. No significant epidural bleeding has been encountered using this maneuver. Piecemeal resection of the vertebral body then is completed. The drill may be used to create a larger cavity or to resect infiltrated bone. Spinal reconstruction is initiated anteriorly. Right-angle clamps are used to create starting holes in the vertebral body at the proper depth for placement of the Steinmann pins. The pin generally is bent at a 20-degree angle and driven into cranial vertebral body using a needle driver with a gentle rotational movement. The pin then is driven back into the caudal vertebral body. A pin then is placed on the contralateral side. Once radiographic confirmation shows good pin placement, methylmethacrylate (PMMA) mixed with tobramycin is placed into the defect covering the Steinmann pins (Fig. 25-25). The PMMA conforms well to the defect and endplates if allowed to harden slightly before administration and if the area of blood is dried. The PMMA expands slightly just before it hardens, so it should not directly abut the anterior dura. The PMMA should be compressed against the vertebral endplates with a Penfield 3 to prevent gaps from forming at the bone-cement interface. Segmental fixation is then applied to the posterior spine. In the thoracic spine, a claw construct is applied to one side of the spine and a compression construct on the contralateral side (Fig. 25-26). Pedicle screw fixation is used most often in the lumbar spine and for selected thoracic fixation. In cases in which correction of kyphosis is attempted, a single rod is placed before administration of the PMMA. Kyphosis correction may be achieved by underbending the rod and translating the spine into alignment. Cross-links are applied unless they are too prominent. The wound is pulse-irrigated with bacitracin irrigant. Posterolateral bone graft then may be applied to decorticated bone for patients with an expected survival time of at least 1 year.
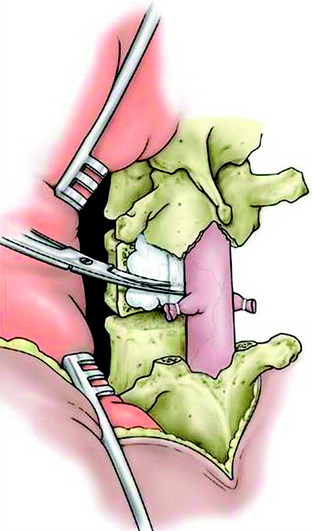
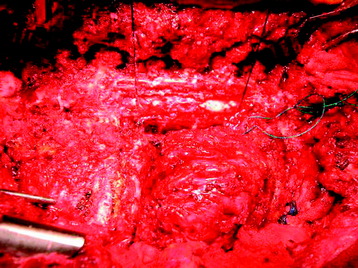
Fig. 25-24 After rhizotomy, the PLL is dissected along the anterior dura and cut with tenotomy scissors.
Case II
This patient showed a tumor mass that involved the posterior element (lamina and facet) and right side proximal rib (Figs. 25-27 and 25-28). For the wide resection margin, the tumor mass was removed with posterior element of one level above and below. The tumor mass originated from the T7 lamina and spinous process. Posterior decompression was performed at T6, T7, and T8. At the T7 level, the pedicle was resected. T6–7 and T7–8 bilateral facets were removed. The right side T7 pedicle-rib complex was drilled out and adjacent parietal pleura was excised (Fig. 25-29). The T7 nerve root was resected bilaterally. Nerve root resection requires wide margin resection. For the wide margin resection, the posterior dura should be resected. If radiation or other adjuvant therapy is planned, the dural resection should not be performed.