Chapter 22 Posterior Approach to the Cervicothoracic Junction (Pancoast Tumor Surgery)
INTRODUCTION
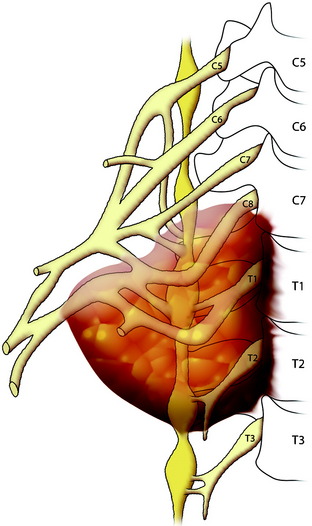
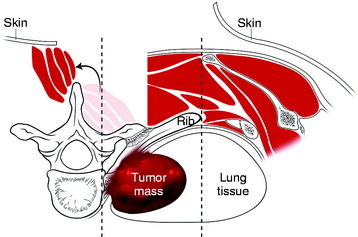
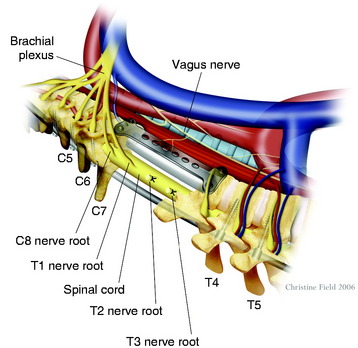
Primary carcinomas arising in the apex of the lung (Pancoast tumors) can extend into the chest wall and the brachial plexus, causing the characteristic Pancoast syndrome (Fig. 22-1). The classic Pancoast syndrome of rib erosion, shoulder pain radiating down the arm, and Horner’s syndrome results from destruction of the first rib extending typically to involve the T1 nerve root and stellate ganglion of the brachial plexus (Fig. 22-2).1
Factors that affect local tumor control and survival are the completeness of tumor resection, TNM (tumor size, node status, metastatic disease) status, and possibly the extent of lung resection.2–4 The completeness of tumor resection is often limited by the degree of spinal and brachial plexus involvement. In the past, spinal involvement was not a surgical indication. However, advanced surgical techniques and magnetic resonance imaging (MRI) for spine and brachial plexus tumors have led to a reassessment of their respectability. Recently, induction chemoradiation protocols have resulted in an improved ability to achieve pathologically complete histological tumor responses, which may ultimately improve the rates of complete resection and long-term survival.
PREOPERATIVE EVALUATION
NEUROLOGICAL EVALUATION
It is important to clinically distinguish T1 nerve root involvement from that of C8 or the lower trunk of the brachial plexus. Pain extending along the ulnar aspect of the forearm to the wrist suggests isolated involvement of the T1 nerve root. These patients do not present with hand intrinsic weakness, and resection does not generally result in significant weakness. Conversely, pain radiating into the hand, especially the fourth and fifth digits, is indicative of involvement of the C8 nerve root or lower trunk of the brachial plexus, and these patients often present with substantial hand intrinsic weakness.5 Resection may result in a flail hand. Both computed tomography (CT) and MRI demonstrate the brachial plexus well, but they often fail to reveal enough anatomical detail to distinguish T1 from C8 or lower trunk involvement. The physical examination is as important as electrodiagnostic tests.
RADIOLOGICAL EVALUATION
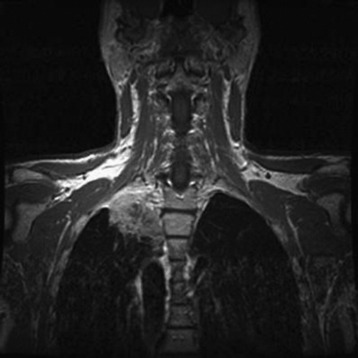
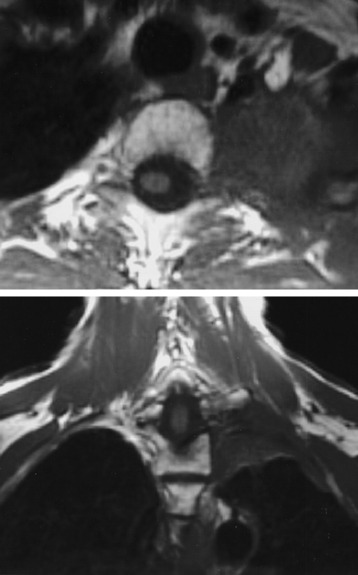
A preoperative MRI classification scheme was devised to assess the degree of spinal element involvement and the type and extent of operation required for tumor resection. MRI findings are divided into four classes based on the degree of involvement of the spinal column and neural structures (Table 22-1).5 Class A tumors involve the vertebral body (VB) periosteum only, and Class B tumors involve the proximal rib head and distal neural foramen without epidural involvement (Fig. 22-3). Class C and D tumors often are not amenable to en bloc resection in which gross-total resection can be achieved. Class C tumors extend through the neural foramen with minimal or no vertebral body involvement but with unilateral epidural compression. Class D tumors involve the vertebral column (vertebral body and/or lamina) with or without epidural compression (Fig. 22-4).
| Magnetic Resonance Imaging Staging System | |
| Class | Description |
| A | Vertebral body periosteum only |
| B | Extension of tumor into distal neural foramen |
| C | Extension of tumor into proximal neural foramen and/or epidural space |
| D | Vertebral body or posterior element infiltration with our without epidural tumor |
SURGICAL TECHNIQUE
CLASS A AND B LESIONS
Position and Incision
The patient is placed in a lateral decubitus position with the right upper arm abducted.
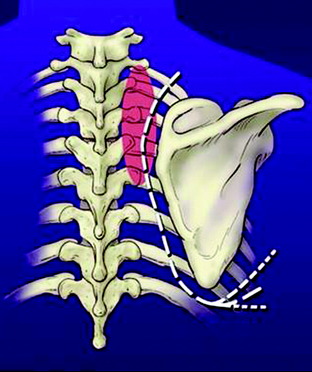
An extended standard posterolateral thoracotomy incision for thoracotomy and posterior midline vertical incision for laminectomy are made (Fig. 22-5). The incision is made midway between the spinous process and medial border of the scapula and extends over the inferior border.
Skin Flap Exposure and Paraspinal Muscle Dissection
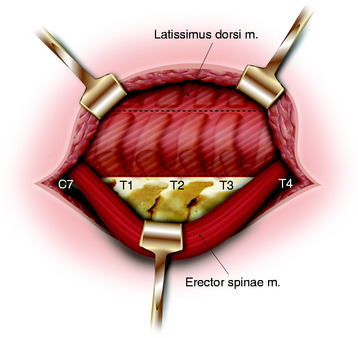
After the skin incision is made, the subcutaneous tissue is dissected. The trapezius muscle is incised and reflected along the edge of the subcutaneous tissue. The erector spinae muscle is dissected from the lamina and facet bilaterally from C4 to T8. The dissection plane is made between the spinalis muscle and longissimus muscle in the side the tumor is located. The bilateral erector spinae muscle is retracted to the side that does not involve the tumor (Fig. 22-6). The paraspinal muscles are dissected from the posterior elements of the spine by using a Bovie cautery to expose the transverse processes, pars interarticularis, and unilateral laminae.
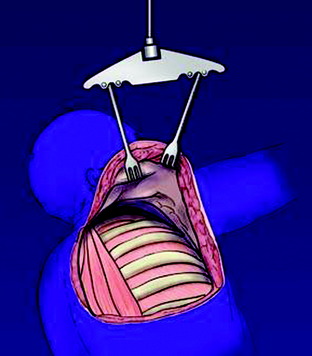
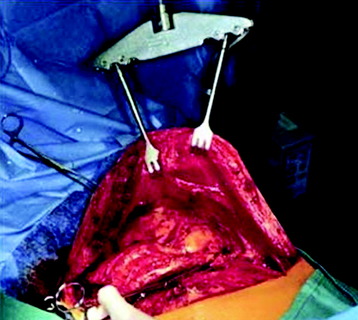
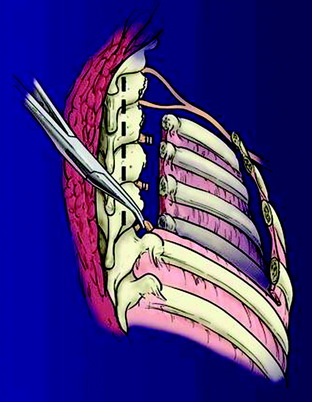
The scapula is elevated from the chest wall by cutting the rhomboid and levator scapulae muscles and is secured with an internal mammary retractor (Figs. 22-7 and 22-8). The chest wall is cut distal to the tumor, most often involving the first through fourth ribs. The chest contents are explored for pulmonary nodes and mediastinal involvement that may preclude resection.
Rib Removal with Disarticulation, Combined with Removal of Lung Apex Mass
Using an osteotome or drill, the base of the transverse process is sectioned distal to the level of the neural foramen and fractured through the costovertebral junction by using forward traction (Figs. 22-9 and 22-10). Tenotomy scissors are used to dissect the intercostal muscles and identify the nerve roots at the level of the neural foramen. Rhizotomy is accomplished by double ligation of the nerve roots by using small vascular clips and sectioning. Proximal nerve roots should be sent for an evaluation of margins and resected more proximally if found to be pathologically positive. The vertebral body periosteum is dissected using a Bovie cautery starting from a normal plane, and segmental feeding vessels are ligated using vascular clips or No. 2-0 silk ligatures. Placement of spinal instrumentation is not required in Class A and B lesions because the pars interarticularis and facet joints remain intact.
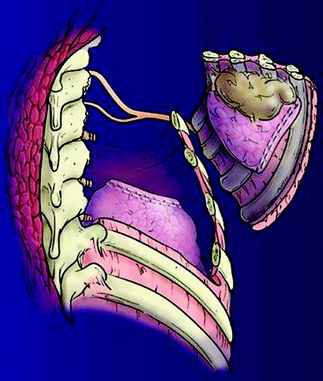
The chest wall is then pushed forward, and the nerve roots are ligated at the distal neural foramen. En bloc chest wall and tumor resection is accomplished (Figs. 22-11 and 22-12).
CLASS C LESIONS
The tumor may extend through the neural foramen to compress the epidural space without bone infiltration. Using a drill, the laminae and facet joints are cut proximal to the facet joint, transverse process, and pars interarticularis, and the pedicles are drilled to the base of the vertebral body (Fig. 22-13). This provides exposure of the proximal neural foramen and lateral dura. The tumor is dissected from the dura by using tenotomy scissors, and a rhizotomy is performed as previously described. Unilateral single-level facet resection is generally tolerated without instrumentation, but multilevel resection may result in scoliosis if fusion is not performed. Although instrumentation has been used in patients treated in the lateral position, a second posterior approach is favored to ensure coronal- and sagittal-plane alignment.
CORPECTOMY AND ANTERIOR COLUMN RECONSTRUCTION
After the thoracotomy, by separating the pleura from the T1–4 vertebral bodies, the aorta and vena cava can be mobilized to the left side with the pleura, presenting an ample surgical field.6 Segmental vessels of T2 and T3 are ligated and separated. VBs are dissected from the surrounding esophagus and trachea. Adjacent lung tissue is removed with the rib-muscle complex. The corpectomy is completed using the high-speed drill. After the corpectomy, polymethylmethacrylate (PMMA) and Steinmann pins or an autologous rib or an iliac crest bone graft are used for anterior vertebral body reconstruction. The PMMA in chest tube can be used for vertebral body reconstruction. Stabilization is augmented by the placement of an anterior plate (Fig. 22-14). With the patient in the prone position, anterior plating may be difficult depending on lung dissection from the vertebral body. In cases of insufficient exposure of the lateral surface of the vertebral body, anterior plating should be performed via the anterior approach.
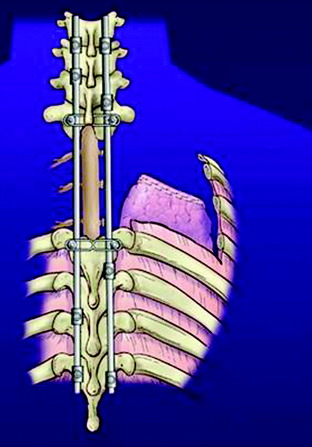
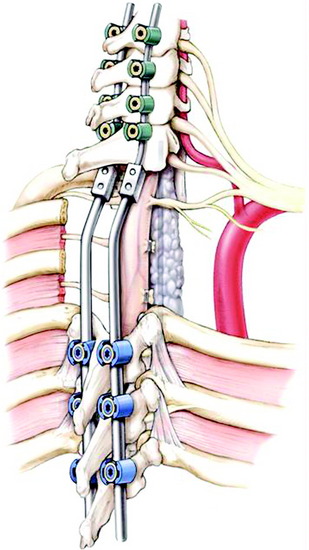
POSTERIOR STABILIZATION
In the old days, posterior segmental fixation was conducted with sublaminar hooks in the cervical spine and hooks or pedicle screws in the thoracic spine. Recently, the use of hybrid lateral mass-pedicle screw fixation systems is advocated to help avoid placement of sublaminar hooks in the cervical spine (Figs. 22-15 and 22-16).7,8 All instrumentation is placed before the chest wall and intrathoracic dissection to provide a protective barrier around the spinal cord. Posterior segmental fixation is undertaken with the patient in a position that is aligned in both the sagittal and coronal planes.
CASE ILLUSTRATION I
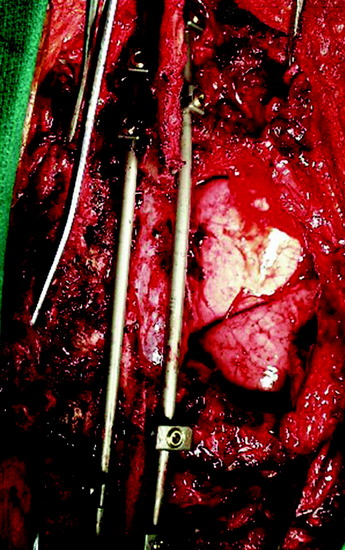
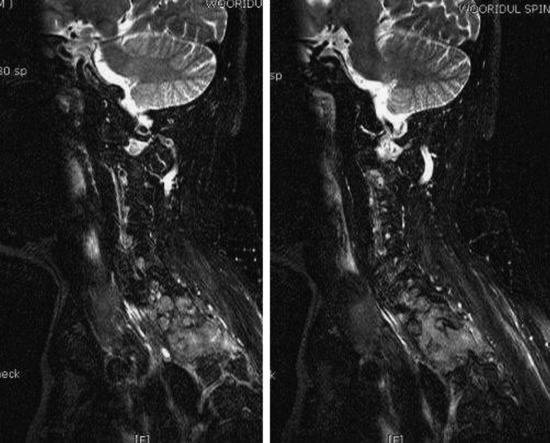
A lung cancer patient complained of posterior neck pain with tingling pain in the right hand. The MRI showed a larger superior sulcus mass with T1 body invasion (Figs. 22-17 and 22-18). The surgeon attempted to resect the T1 vertebral body through the posterior route. With the patient in the prone position, a midline vertical incision was made from C5 to T7 and another perpendicular incision along the rib was added. The laminae, bilateral pedicles, facet joints, and pars interarticularis were resected using a high-speed drill. The epidural mass was removed from the dorsal and lateral side of the spinal cord. The vertebral body mass was removed via the transpedicular approach. Anterior column reconstruction was performed using Steinmann pins and PMMA. A hybrid lateral mass-pedicle screw fixation system was used for posterior stabilization (Figs. 22-19 and 22-20).
CASE ILLUSTRATION II
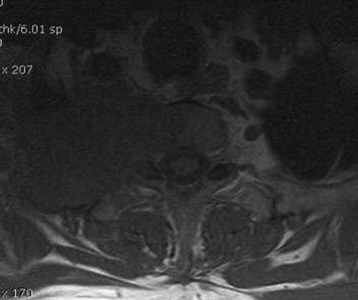
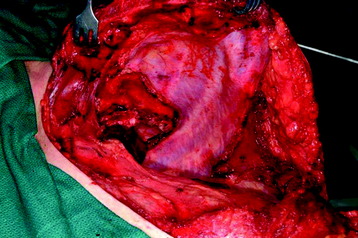
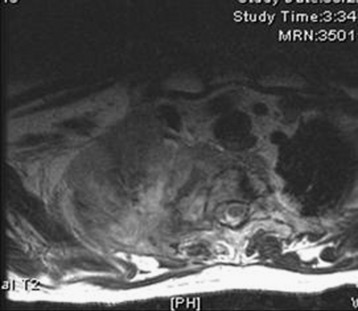
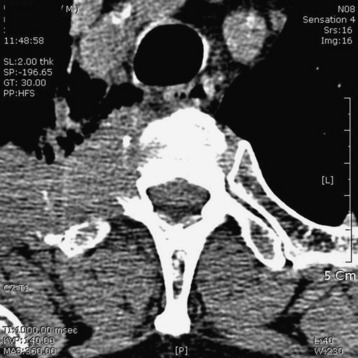
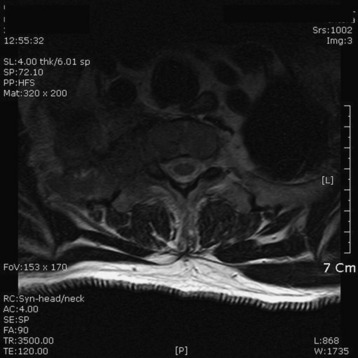
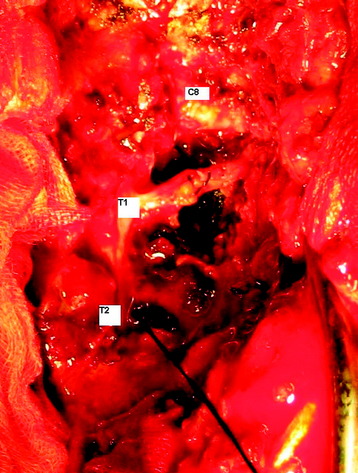
A 56-year-old male patient complained of right shoulder pain and right arm paresthesia for 2 months. Physical examination revealed hypesthesia on his right fourth and fifth fingers. Flexion and abduction of the fourth and fifth fingers were moderately impaired. Shoulder MRI was checked initially, but no abnormal finding was found. Then C-spine CT and MRI were taken. On CT scan, a low density mass was shown in the right thoracic cavity with the mass invading the right neural foramen (T1–2) and T1 vertebral body (Fig. 22-21). On MR sagittal view, signal change was seen at the right pedicles of the T1 and T2 vertebral bodies. In addition, foraminal masses were seen at the C7–T1 and T1–2 intervertebral foramen (Fig. 22-22). On MR axial view, the right half of the T1 vertebral body was infiltrated with tumor mass. An operation was performed with the posterior approach (Fig. 22-23). Multiple ribs (first, second, and third ribs) were resected, and total laminectomy was performed from T1 to T3. Additional facet removal was performed at the right C7–T1, T1–2, and T2–3. C8 and T1 root decompression was achieved after epidural mass removal. The T2 root was resected, including a dorsal root ganglion (Fig. 22-24). Posterior stabilization was performed with a lateral mass-pedicle screw fixation system.