CHAPTER 21 Post-Traumatic Elbow Stiffness in Children
ETIOLOGY
Elbow stiffness can be categorized as either extra-articular or intra-articular in origin. Heterotopic ossification and soft tissue contracture are two common causes of extrinsic contracture. Early aggressive passive range-of-motion (ROM) exercises or repeated forceful manipulation during fracture reduction have been associated with heterotopic ossification and elbow stiffness.25,27 Delayed open reduction and internal fixation have also been shown to increase the risk of developing heterotopic ossification.14 Intra-articular T-condylar fractures are rare in children, but when they occur, they frequently are associated with elbow stiffness.9,23 Soft tissue contracture frequently occurs following immobilization or surgical treatment.29
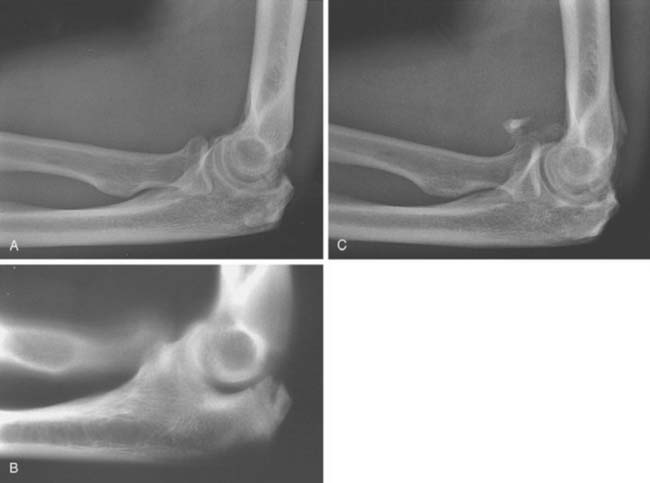
Fracture malunion, callus formation, and degenerative changes are common intra-articular causes of elbow stiffness.30 Anatomic reduction of displaced intra-articular elbow fractures is important to prevent post-traumatic arthritis as well as to maintain the precise anatomic relationships among the three bones that make up the elbow and is required for normal elbow motion.21 If malunion does occur, resulting in articular incongruity or bone impingement, secondary degenerative changes often follow causing intrinsic elbow stiffness (Fig. 21-1).
INCIDENCE
Although it is not common, elbow stiffness may occur following almost any form of elbow trauma. Henrikson6 reported stiffness in 3% to 6% of patients treated for supracondylar humerus fractures. Loss of motion following supracondylar humerus fractures may be due to soft tissue contracture or heterotopic ossification.
Wedge and Roberson29 reported some loss of elbow motion following radial neck fractures in 33% of patients undergoing open reduction, and in 100% of patients when internal fixation was used. Aside from fractures, patients frequently experience loss of extension following elbow dislocation.11
PRESENTATION
Loss of motion accompanied by pain is an infrequent presenting complaint in young patients and was present in only 3 of 28 patients in a series from the Mayo Clinic.26 Symptoms such as catching or locking may be present and suggest the presence of loose bodies within the elbow.
EVALUATION
HISTORY
A detailed history of the injury and subsequent treatment is typically all that is necessary to determine whether the etiology for the stiffness is extrinsic or intrinsic. Important information to gather includes the mechanism and time of the initial injury, the precise nature of the nonoperative or operative treatment, and the length of the period of immobilization. Knowledge of the nature and duration of any physical therapy is helpful. Information regarding any complication such as a wound healing problem or infection is also useful. Factors commonly seen in the child that strongly suggest an extrinsic etiology include extra-articular fracture, especially supracondylar involvement, simple dislocation without associated fracture, and immobilization lasting longer than 4 weeks. Crush injuries and high-energy injuries with local soft tissue damage also predispose the patients to developing extrinsic contracture. Patients with an associated head injury are at risk for developing an extrinsic contracture due to heterotopic ossification.19
Post-traumatic intrinsic stiffness is most common following an intra-articular fracture. Because these more commonly require open reduction, surgical treatment may contribute to intrinsic etiology, especially if associated with malunion, excess callus formation, or retained hardware. Detailed questioning about the length of time elapsed since the injury and the specific treatment received for the elbow stiffness is helpful in determining the likelihood of future improvement.
EXAMINATION
Motion
Accurate measurement of elbow range of motion (ROM) with a goniometer is essential. The functional arc of elbow motion is from 30 to 130 degrees.21 Patients with elbow ROM greater than this arc rarely suffer any functional limitation, but it is reasonable to attempt to restore normal ROM through a trial of nonoperative treatment. We have found that the use of splints is helpful and better tolerated than physical therapy (see Chapter 11). Very seldom is surgical treatment indicated for patients with less than 0 degrees of extension loss or greater than 125 degrees of flexion. Extension is the most common portion of the arc affected. Limitation of pronation and supination is observed almost exclusively after radial head and neck fractures and suggests involvement of the radiocapitellar joint or proximal radioulnar synostosis if no rotational motion is present.
Stability
Varus or valgus instability is classified by the method of Morrey.20 The elbow is stable if there is no varus or valgus laxity. Mild instability exists if varus or valgus laxity is present but is less than 5 degrees in either direction. Elbows were considered moderately unstable if varus or valgus laxity was considered to be 5 to 10 degrees and associated with mild symptoms. Severely unstable elbows had greater than 10 degrees varus and valgus laxity and caused limitations in daily activities. Varus and valgus instability associated with elbow stiffness is uncommon in children unless bone has been resected.
IMAGING STUDIES
Magnetic Resonance Imaging
Recent literature has recommended magnetic resonance imaging (MRI) of the stiff elbow.3 However, MRI does not image osseous anatomy as well as other radiographic techniques. For specific indications, MRI can provide helpful information. Evaluation for possible avascular necrosis, physeal injury, and soft tissue lesions is often facilitated by MRI. In general, as with CT, transverse images are less helpful in assessing elbow contracture.
TREATMENT: INDICATIONS AND CONTRAINDICATIONS
NONOPERATIVE TREATMENT
The amount of time transpiring between the injury and the presence of an established contracture affects treatment. Early and aggressive passive ROM exercises have been demonstrated to cause heterotopic ossification in pediatric patients.25 During the first 1 to 3 months following injury; therefore, active ROM is used primarily. We have found swimming to be a very beneficial activity for the treatment of pediatric elbow stiffness. Although the exact mechanism is not clear, it is easy to imagine how swimming or playing in the water is relaxing, soothing, nonthreatening, and safe for children and adolescents. Therefore, we strongly encourage patients to swim regularly as soon as possible following injury or treatment.
Splinting
Previous authors have described the use of static and dynamic splinting to improve elbow ROM. Green and McCoy5 reported the use of a turnbuckle splint for elbow contracture, whereas others have advocated dynamic splinting.7 Our current practice is to use a static splint primarily at night, with an adjustable hinge that can be fixed in any degree of flexion (see Chapter 11). Each night before retiring, the patient applies the brace to the affected elbow. Preferably this is immediately following a session of stretching. Patients with a primary limitation in extension place the elbow and splint in maximal extension to the point of tolerance and fix the hinge in this position. Conversely, patients with a primary limitation in flexion fix the splint in maximal flexion, again limited by pain. Patients with significant limitation in both planes alternate nights in flexion and extension. This nonoperative regimen of active and passive ROM exercises, NSAIDs, and splinting should be tried for a minimum of 1 and up to 3 months before its effectiveness can be determined.
SURGICAL TREATMENT
Patients whose injuries are more than 6 months old and who have failed an adequate trial of nonoperative treatment as described earlier and who experience significant functional limitation due to elbow stiffness may be considered for operative treatment. Successful surgical treatment addresses all extrinsic and intrinsic pathologic elements contributing to stiffness.22 In the pediatric patient, release of the extrinsic soft tissue contracture is typically performed in a manner similar to the technique described by Husband and Hastings8 or Mansat and Morrey.16 Anterior capsulectomy is performed through a lateral Kocher incision for flexion contracture. If the medial capsule cannot be adequately released through the lateral incision, a medial incision is made through which the anterior capsular release is completed.12
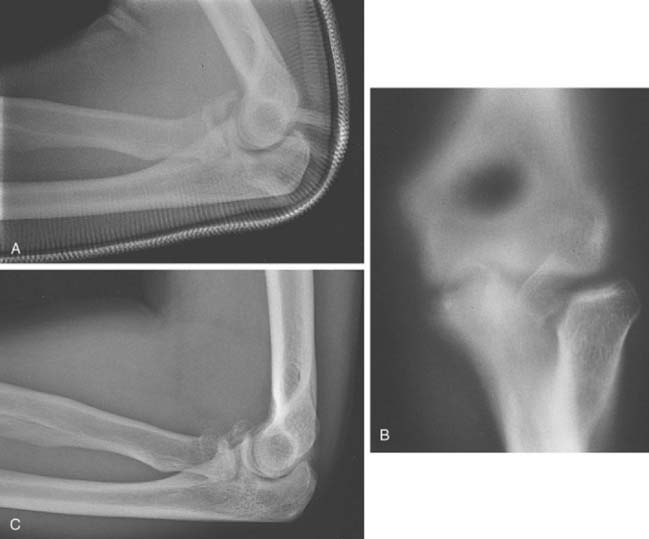
Occasionally, the lateral collateral and medial collateral ligaments must also be released to restore adequate motion. Posterior capsulectomy is performed through the same lateral incision if extension contracture is present, hence the term column procedure.16 Thorough inspection of the joint is also performed, and intra-articular pathology causing limitation of elbow motion is treated. The olecranon tip should be excised if it is impinging on the posterior humerus in extension, and the coronoid tip should be excised if it is impinging within the coronoid fossa in flexion (Fig. 21-2). Lysis of adhesions is performed if necessary and any additional pathologic condition, such as loose bodies, addressed. If marked degenerative changes are present at the radiocapitellar joint, causing restricted ROM, radial head excision may be considered in skeletally mature patients (Fig. 21-3). Occasionally, excessive callus formation or malunion results in a bone block to motion, which may be removed deftly using burr or rongeur. We rarely release muscle/tendon units, because these will stretch out after surgery.
An important lesson learned is that patients undergoing posterior release for limited elbow flexion frequently develop ulnar neuritis postoperatively. To prevent ulnar neuritis, we are increasingly proactive and in many patients performing in situ decompression of the ulnar nerve within the cubital tunnel, or subcutaneous anterior ulnar nerve transposition at the time of contracture release. This is performed through the medial incision used to complete elbow contracture release.
Patients with extensive intra-articular pathology limiting motion, but who have at least 50% of the articular cartilage intact, may benefit from distraction arthroplasty. A recent publication by Mader reported significant elbow motion improvement in 14 pediatric and adolescent patients treated with mechanical distraction.1,15 Patients with intrinsic contracture and less than 50% of the articular cartilage remaining may be considered for fascial interposition arthroplasty.20 It is less common to require these modalities in the pediatric population.
Following closure and application of a soft dressing, the patient is allowed to awaken from anesthesia enough to allow neurovascular assessment. If the patient is neurovascularly intact, an indwelling brachial plexus catheter is inserted and continuous passive motion (CPM) is begun immediately. ROM in the CPM machine is rapidly increased to the amount of motion obtainable intraoperatively (see Chapter 10). The brachial plexus catheter and CPM are continued on an inpatient basis until satisfactory motion is achieved and the patient is able to tolerate continued use of CPM without the brachial plexus catheter. After a total of approximately 3 to 4 days in the hospital, the patient is discharged home with a portable CPM machine to be used for approximately 6 weeks. When not using CPM, the patient typically uses a static adjustable splint. This regimen requires some compliance not readily attainable in the very young patient; as noted earlier, we attempt to defer surgery in those with open physes if possible. If surgery is performed in the younger child, the above-described regimen is modified according to what is attainable by that particular patient.
RESULTS
There is a paucity of literature available on the results of treatment for the stiff elbow in pediatric patients. No published results can be found describing nonoperative results in pediatric patients, and only four papers could be identified describing operative results for the treatment of elbow stiffness in pediatric patients.2,15,18,26 Mih and Wolf18 reported a series of nine pediatric patients treated surgically for elbow stiffness. Six of the nine patients had post-traumatic stiffness, and the remaining three patients had stiffness secondary to juvenile rheumatoid arthritis, hemophilia, or avascular necrosis of the capitellum. Preoperatively, patients had a mean total arc of motion of 55 degrees, which improved to 108 degrees at a mean duration of follow-up of 17 months.
We have reviewed our experience with patients age 21 or younger who underwent surgical treatment for elbow stiffness at the Mayo Clinic since 1979.26 Thirty-nine patients were identified, 28 of whom developed stiffness following trauma. Excluding nontraumatic etiology, eight patients had a complex fracture with associated elbow dislocation, seven sustained an isolated intra-articular elbow fracture, five patients an isolated elbow dislocation, four patients an extra-articular distal humerus fracture, and four patients a soft tissue injury or contusion without an elbow dislocation or fracture. All patients had failed a trial of nonoperative treatment and had functional limitation because of restricted ROM.
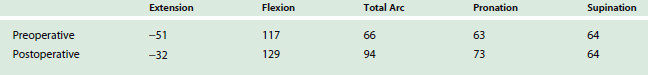
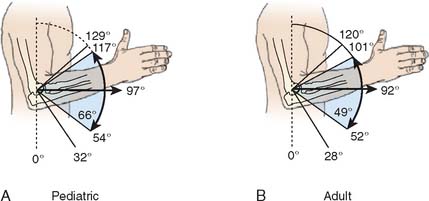
Surgical procedures performed are listed in Table 21-1; as noted, virtually all underwent anterior release. Mean preoperative and postoperative ROMs are displayed in Table 21-2. The mean arc of motion improved from 66 degrees preoperatively to only 94 degrees after surgery. These results suggest that, at least in our experience, pediatric patients tend to regain less motion than adult patients treated for post-traumatic elbow stiffness (Fig. 21-4).4,8,20,28 Also of note is that, unlike in the adult population, three patients regained no motion or even lost motion after surgery.
TABLE 21-1 Surgical Procedures Performed in 28 Pediatric Patients with Elbow Stiffness
| Procedure | Number of Patients |
|---|---|
| Anterior capsulotomy | 26 |
| Posterior capsulotomy | 12 |
| Olecranon tip excision | 9 |
| Radial head excision | 7 |
| Osteophyte/heterotopic bone excision | 6 |
| External fixation | 5 |
| Fascial arthroplasty | 3 |
| Hardware removal | 3 |
| Loose body removal | 3 |
| Coronoid tip excision | 2 |
| Humeral contouring | 2 |
ARTHROSCOPIC RELEASE
Arthroscopic elbow contracture release has gained increasing popularity in the treatment of adult patients with elbow stiffness10,13,24 and has been used with increasing frequency in pediatric and adolescent patientsat the Mayo Clinic.17 Between 1997 and 2004, 45 pediatric and adolescent patients underwent arthroscopic elbow contracture release at the Mayo Clinic. In Table 21-3, motion arc improvement following arthroscopic release in pediatric patients is compared with improvement following open surgical treatment in pediatric patients and following open surgical treatment in adult patients from the same institution. The results of arthroscopic pediatric elbow contracture release appear to be slightly better than open contracture release for pediatric patients but not as successful as open contracture release in adult patients. It is unclear at this time if the improved motion following arthroscopic surgery is a consequence of arthroscopic technique or the result of more consistent use of CPM, static adjustable splinting or other factors.
TABLE 21-3 Comparison Between Open Adult, Open Pediatric, and Arthroscopic Pediatric Elbow Contracture Release
| Motion Arc Improvement | |
|---|---|
| Mansat | 45 |
| Stans | 28 |
| Mclntosh | 38 |
COMPLICATIONS
The combination of previous surgery, extensive dissection, external fixation, and immediate ROM following surgery places surgical patients at risk for complications. In the Mayo series, there was one deep wound infection requiring surgical débridement, one transient radial nerve palsy, one postoperative hematoma that required surgical evacuation, and three patients with persistent contracture without improvement following surgery. Patients undergoing distraction arthroplasty or fascial interposition arthroplasty are at greater risk for complications than patients treated with surgical release without external fixation.20
1 Ayoub K., Gibbons P., Bradish C.F. Compass elbow hinge: Short-term results in five adolescents. J. Pediatr. Orthop. Part B. 2004;13:395.
2 Bae D.S., Waters P.M. Surgical treatment of posttraumatic elbow contracture in adolescents. J. Pediatr. Orthop. 2001;21:580.
3 Fortier M.V., Forster B.B., Pinney S., Regan W. MR assessment of post-traumatic flexion contracture of the elbow. J. Magnet. Res. Imag. 1995;5:473.
4 Gates H.S., Sullivan F.L., Urbaniak J.R. Anterior capsulotomy and continuous passive motion in the treatment of post-traumatic flexion contracture of the elbow. J. Bone Joint Surg. 1992;74A:1229.
5 Green D.P., McCoy H. Turnbuckle orthotic correction of elbow-flexion contractures after acute injuries. J. Bone Joint Surg. 1979;61A:1092.
6 Henrikson B. Supracondylar fracture of the humerus in children. Acta Chir. Scand. 1966;369:1.
7 Hepburn G.R., Crivelli K.J. Use of elbow Dynasplint for reduction of elbow flexion contracture. J. Sports Ther. 1984;5:269.
8 Husband J.B., Hastings H. The later approach for operative release of post-traumatic contracture of the elbow. J. Bone Joint Surg. 1990;72A:1353.
9 Jarvis J.G., D’Astous J.L. The pediatric T-supracondylar fracture. J. Pediatr. Orthop. 1984;4:697.
10 Jones G.S., Savoie F.H. Arthroscopic capsular release of flexion contractures (arthrofibrosis) of the elbow. Arthroscopy. 1993;9:277.
11 Josefsson O., Gentz C., Johnell O. Surgical versus nonsurgical treatment of ligamentous injuries following dislocations of the elbow joint. A prospective randomized study. J. Bone Joint Surg. 1987;69A:605.
12 Jupiter J.B., O’Driscoll S.W., Cohen M.S. The assessment and management of the stiff elbow. Instruc. Course Lect. 2003;52:93.
13 Kim S.J., Shin S.J. Arthroscopic treatment for limitation of motion of the elbow. Clin. Orthop. Rel. Res. 2000;375:140.
14 Lal H.M., Bhan S. Delayed open reduction for supracondylar fractures of the humerus. Int. Orthop. 1991;15:189.
15 Mader K., Koslowsky T.C., Gausepohl T., Pennig D. Mechanical distraction for the treatment of posttraumatic stiffness of the elbow in children and adolescents. Surgical Technique. J. Bone Joint Surg. 2007;89A(Part 1, Suppl 2):26.
16 Mansat P., Morrey B.F. The column procedure: a limited lateral approach for extrinsic contracture of the elbow. J. Bone Joint Surg. 1998;80A:1603.
17 McIntosh, A., and O’Driscoll, S. W.: Arthroscopic treatment of elbow stiffness in pediatric and adolescent patients. Presented at the American Shoulder and Elbow Surgeons Specialty Day, AAOS Annual Meeting, San Diego CA, Feb. 17, 2007.
18 Mih A.D., Wolf F.G. Surgical release of elbow-capsular contracture in pediatric patients. J. Pediatr. Orthop.. 1994;14:458.
19 Mital M.A., Barber J.E., Stinson J.T. Ectopic bone formation in children and adolescent with head injuries: its management. J. Pediatr. Orthop.. 1987;7:83.
20 Morrey B.F. Post-traumatic contracture of the elbow. J. Bone Joint Surg.. 1990;72A:601.
21 Morrey B.F., Askew L.J., An K.N., Chao E.Y. A biomechanical study of normal functional elbow motion. J. Bone Joint Surg.. 1981;63A:872.
22 Papandrea R., Waters P.M.. Posttraumatic reconstruction of the elbow in the pediatric patient. Clin. Orthop., 2000;370:115-126.
23 Papvasilious V.A., Beslikas T.A. T-condylar fractures of the distal humeral condyles during childhood: an analysis of six cases. J. Pediatr. Orthop.. 1986;6:302.
24 Phillips B.B., Strasburger S. Arthroscopic treatment of arthrofibrosis of the elbow joint. Arthroscopy. 1998;14:38.
25 Pirone A.M., Graham H.K., Krajbich J.I. Management of displaced extension-type supracondylar fractures of the humerus in children. J. Bone Joint Surg.. 1988;70A:641.
26 Stans A.A., Maritz N.G.J., O’Driscoll S.W., Morrey B.F. Operative treatment of elbow contracture in patients. 21 years of age or younger. J. Bone Joint Surg.. 2002;84A:382.
27 Thompson H.G., Garcia A. Myositis ossificans: aftermath of elbow injuries. Clin. Orthop. Rel. Res. 1967;50:129.
28 Urbaniak J.R., Hansen P.E., Beissinger S.F., Aitken M. Correction of post-traumatic flexion contracture of the elbow by anterior capsulotomy. J. Bone Joint Surg. 1985;67A:1160.
29 Wedge J.H., Roberson D.E. Displaced fractures of the neck of the radius. J. Bone Joint Surg. 1982;64B:256.
30 Zionts L.E., Mirzayan R. Fracture of the lateral epicondyle of the humerus in a child: A case report. J. Bone Joint Surg. 2002;84A:818.