Positive-pressure mechanical ventilation
In addition to these industry-derived improvements, our understanding of intraoperative changes in respiratory mechanics has also improved so that appropriate MV settings can be used in patients with airflow obstruction or lung or chest wall abnormalities. Recent concern about the risk of developing acute lung injury in previously healthy patients after intraoperative MV is also discussed in this chapter. A list of the abbreviations for terms commonly used in respiratory physiology is provided in Box 223-1.
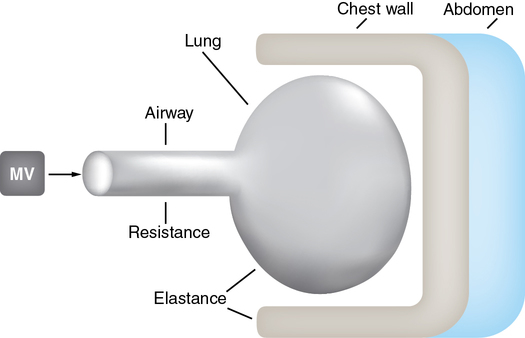
Respiratory mechanics
Two independent patient-related forces have to be overcome to achieve lung inflation by positive-pressure MV (Figure 223-1): (1) resistance to the flow of gases within the airway and (2) compliance and elastance of the lung and chest wall, respectively. The latter concept can be difficult for the anesthesia provider to understand. In an inflated lung, the elastin within the lung is stretched. If you then remove a lung from the thoracic cavity and if the airway is open, the lung will collapse. This does not happen within the thoracic cavity because the parietal pleura is adherent to the thoracic cavity. In an intubated paralyzed patient at end expiration, or when the lungs are at their functional residual capacity, positive pressure must be applied to expand the lungs to deliver a breath. The amount of pressure (plateau pressure [Pplat]) applied to expand the lungs to a known volume is a measure of the compliance of the lung (Compliance = ΔV/ΔP). For example, 5 cm of H2O pressure in a patient with a VT of 500 would equal a compliance of 100. In a patient with a diseased lung (e.g., with severe acute respiratory distress syndrome), the compliance would typically be less than 20.
< ?xml:namespace prefix = "mml" />
Mode of mechanical ventilation
Volume control mechanical ventilation
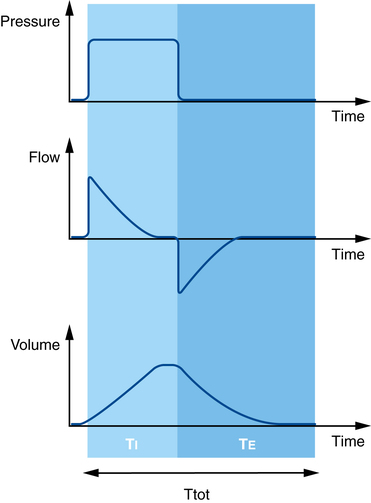
During volume control mode, VT and TI (or respiratory rate and inspiratory: expiratory [I:E] ratio) are set by the clinician and inspiratory flow remains constant (Figure 223-2). In volume control MV, the resistive impedance (transmission of the VT through the airway) and the elastic impedance (compliance of the lung or chest wall) both contribute to the peak airway pressure (Ppeak).
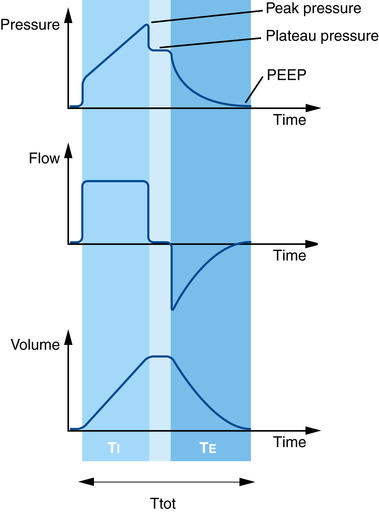
A short end-inspiratory pause may be included in the respiratory cycle in volume control MV so that, after the VT has been fully delivered and just prior to exhalation, airflow is reduced to zero for a fixed proportion of TI. The airway pressure recorded during this end-inspiratory interval is called the plateau (Pplat), pause, or end-inspiratory hold pressure (see Figure 223-2). In many anesthesia ventilators, the default setting in volume control mode may include no end-inspiratory pause so that only Ppeak is recorded. However, it is always possible (and desirable) to include an end-inspiratory pause when using volume control MV so that both Ppeak and Pplat are recorded.
Pressure control mechanical ventilation
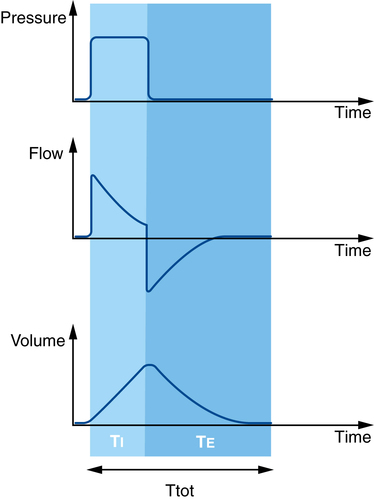
In pressure control MV, inspiratory pressure and TI (or respiratory rate and I:E ratio) are set by the clinician and remain constant, but the delivered VT and inspiratory flow will vary during inspiration (Figure 223-3). In pressure control MV, in which inspiratory pressure remains constant for the duration of TI, no Ppeak or end-inspiratory Pplat is registered (as occurs in volume control mode when an end-inspiratory pause is added into the respiratory cycle). Therefore, the relationship between Ppeak and Pplat that is informative in volume control MV cannot be used in pressure control MV.
Intraoperative mechanical ventilation: Which mode should we use?
Contemporary anesthetic machines now provide modes of ventilatory support similar to those used in critical care ventilators. Use of assisted (rather than control) modes of ventilatory support during a surgical procedure depends on the intraoperative conditions, patient-related factors (there is no difference between control mode and assisted mode if the patient has received a neuromuscular blocking agent and has a train-of-four of zero and therefore cannot initiate any respiratory effort), the airway device used, and the preference of the individual clinician involved. In pressure support mode, the ventilator delivers a constant inspiratory pressure until the ventilator cycles into expiration. The trigger to change from inspiration to expiration is when the inspiratory flow declines to a set proportion of peak inspiratory flow (Figure 223-4).
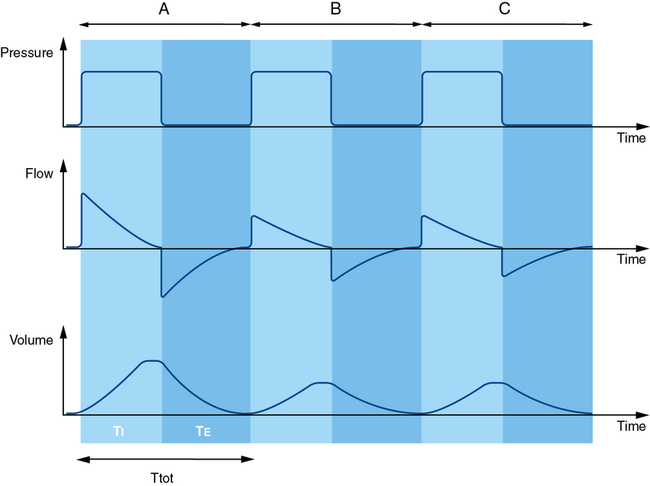
Clinical application of intraoperative mechanical ventilation
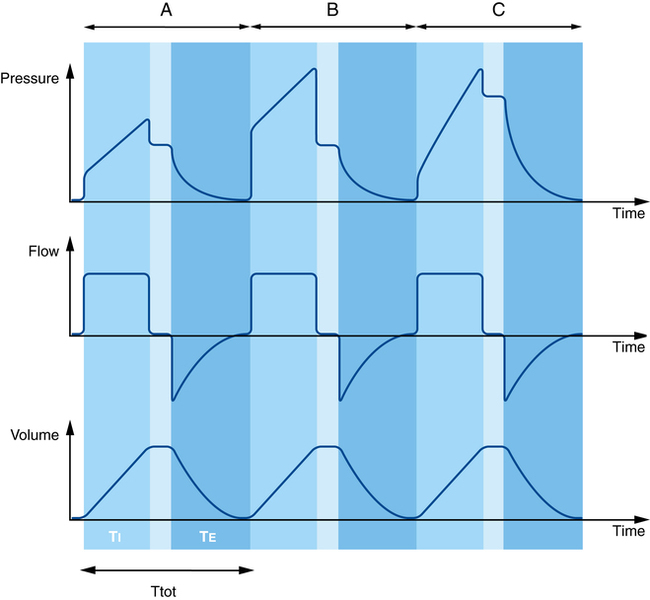
In volume control MV, an increase in respiratory system impedance (either increased resistance or decreased compliance) will lead to the set VT being delivered during the set TI but at the expense of higher airway pressures. Importantly, an increase in airway resistance or decrease in lung compliance can be differentiated by observing the associated changes in Ppeak and Pplat. An increase in airway resistance is reflected by an increase in Ppeak with a relatively unchanged Pplat (Figure 223-5, B) so that the difference between Ppeak and Pplat is increased. In volume control MV, a decrease in lung compliance will increase both Ppeak and Pplat so that the difference between Ppeak and Pplat remains unchanged (Figure 223-5, C).
In pressure control MV (constant inspiratory pressure and TI), any increase in airway resistance or decrease in lung compliance will lead to a decrease in inspiratory flow and delivered VT (Figure 223-6). In contrast to volume control MV, in pressure control MV, there is no way of identifying which factor (airway resistance or lung compliance) is responsible for the decrease in alveolar ventilation.