Podiatric Procedures
Normal daily activities cannot easily be accomplished without walking, so patients with painful or infectious conditions of the feet often seek medical attention. This chapter focuses on procedures performed for common maladies of the foot. Other procedures on the foot are described elsewhere in this text, including anesthesia of the foot and ankle (see Chapters 29 and 31), management of nail bed injuries (see Chapters 35 and 37), incision and drainage of paronychia (see Chapter 37), joint fluid analysis (see Chapter 53), management of common dislocations of the foot (see Chapter 49), and splinting (see Chapter 50).
Common Nontraumatic Conditions of the Foot
Footpad Use
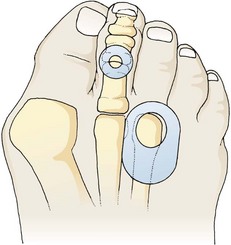
Footpads redistribute pressure over an inflamed, tender area of the foot. The particular type of footpad and its placement depend on the condition being treated (Fig. 51-1). Commercially available aperture footpads are recommended for the temporary relief of warts, corns, hyperkeratoses, and bunions. Verruca virus introduced into the plantar surface of the foot may produce a painful hyperkeratotic lesion, commonly referred to as a “plantar wart,” on the sole of the foot. A simple callus may be painful and result in the formation of a “hard corn” when formed over the bony prominence of a digit. Once recognized and after other conditions are ruled out, definitive care of these lesions is rarely indicated in the ED.
A bunion develops when unbalanced forces applied to the first metatarsal cause lateral displacement of the distal end of the hallux. Bunions typically form in women wearing heeled shoes with narrow toe boxes. The patient may complain of numbness over the distal, medial aspect of the first toe as a result of compression of the terminal branch of the medial dorsal cutaneous nerve. The mechanical forces that precipitate bunion formation may also cause other painful conditions, including intermetatarsal neuromas, hammertoes, ingrown toenails, corns, and calluses. Bursitis may develop over the medial bony prominence of the first metatarsophalangeal (MTP) joint. Self-adherent bunion pads placed over the first MTP joint may provide temporary relief (Fig. 51-2). In the ED, treat patients suffering from these common disorders with analgesics and footpads followed by referral for definitive care. Recommend that the patient avoid wearing the offending shoes. Consider gout when evaluating pain over the first MTP joint, particularly in the presence of other signs of inflammation (e.g., redness, swelling, warmth).
Heel Pain Syndromes
Heel spur pain can be quite bothersome and chronic or recurrent. This condition is not easily remedied in the ED, and after other conditions are ruled out, minimal intervention with podiatric referral is often the best course of action. Patients typically have pain over the medial border of the plantar aspect of the calcaneus. The pain gradually worsens over a period of months. A bony prominence that begins as periostitis extends from the medial aspect of the calcaneal tuberosity into the central plantar fascia and may be seen on radiographs. Radiographs of the calcaneus that do not demonstrate a bony spur suggest plantar fasciitis (see the section “Painful Conditions of the Plantar Surface of the Foot” later in this chapter), even though many patients with plantar fasciitis have plantar calcaneal and Achilles spurs. Plantar calcaneal heel spurs are found in nearly 15% of the population, only 30% of whom have heel pain. Although many persons with heel spurs are asymptomatic, 75% of patients with heel pain have heel spurs.1 However, radiographs have little value in evaluating nontraumatic heel pain because they rarely demonstrate radiographic abnormalities that prompt additional treatment.2
Shoe supports with a heel pad or cup or a doughnut-shaped orthotic often help reduce the discomfort by redistributing weight. Few randomized, controlled trials have evaluated steroid therapy; those that have do not provide substantial evidence supporting its long-term efficacy.3,4 Treatment of the painful site is done with 10 to 20 mg of methylprednisolone injected from the medial aspect of the foot while avoiding the sensitive plantar surface. Some evidence suggests that injecting 25 mg of prednisolone acetate into the medial aspect of the heel provides partial pain relief at 1 month in comparison to lidocaine only, but no advantage can be detected at 3 months.5 A short-leg walking cast may be effective in some patients with recalcitrant heel pain.6 There is little evidence to suggest that specific interventions aimed at reducing heel pain are superior to conservative, supportive treatment alone.
Retrocalcaneal Bursitis, Achilles Tendinopathy, and Calcaneal Apophysitis
Although retrocalcaneal bursitis and Achilles tendinopathy, formerly referred to as Achilles tendinitis, are anatomically distinct, the clinical findings are similar. Pain at the insertion of the Achilles tendon is worsened with prolonged standing or walking and is aggravated by passive or active range of motion in both conditions. Directed palpation can distinguish one entity from the other, but both are treated similarly. Tenderness of the Achilles tendon suggests tendinopathy, whereas tenderness between the tendon and the calcaneus suggests retrocalcaneal bursitis. Achilles tendinopathy has been noted to develop spontaneously after the use of quinolone antibiotics, occasionally with rupture. The condition may occur during quinolone use or a few weeks after therapy and prompts immediate discontinuation of use of the drug if recognized. Rest, elevation, ice, NSAIDs, heel pads, and an open-backed shoe provide relief in the majority of patients. A corticosteroid injection is not usually performed, but it may provide some relief, although its superiority over conservative measures is unproved. Repeated steroid injection is associated with Achilles tendon rupture.7 Injection of platelet-rich plasma (PRP) as treatment of Achilles tendinopathy has gained some support among sports medicine physicians, but recently published studies have failed to demonstrate short- or long-term improvement in pain or function when PRP injection is compared with placebo.8,9 Osteochondrosis of the posterior calcaneal apophysis may cause pain worsened by activity in children between 7 and 10 years of age. It is thought to represent an overuse syndrome in an athletically active child with tenderness in the posterior heel region.7,10 Treat this self-limited condition with rest, ice, and heel pads. Radiographs are not indicated unless other diagnoses are suspected.11 Activity is resumed when the pain abates.
Painful Conditions of the Plantar Surface of the Foot
Repeated microtrauma to the plantar aponeurosis causes pain on the plantar surface of the foot (Fig. 51-3A). Plantar fasciitis is typically unilateral and found in women who wear high-heeled shoes. The pain is maximally severe in the morning or after prolonged sitting and improves after walking, often referred to as “first-step pain.” Some patients with plantar fasciitis may also have a calcaneal heel spur, but the presence or absence of this radiographic finding is clinically irrelevant. Pain is elicited with palpation (see Fig. 51-3B), toe walking, or passive stretching of the plantar aponeurosis. Frequently, this annoying condition resolves spontaneously, but resolution is slow, with as long as 6 to 18 months being needed. Conservative therapy, including rest, elevation, ice, and NSAIDs, results in a satisfactory outcome after 6 to 8 weeks in 90% of patients.12 The pain improves over time in most patients with or without NSAIDs, although the addition of NSAIDs appears to increase pain relief when compared with conservative treatments alone.13 The emergency clinician can do little to treat this chronic, distressing condition. Stretching exercises each morning and evening can be suggested (see Fig. 51-3D). Night splinting to keep the foot dorsiflexed and custom orthoses made from the patient’s foot impression can be very helpful but usually require referral to podiatry for proper fitting (see Fig. 51-3C). Corticosteroid injection is used by some clinicians; its benefit remains unproved, however. A single injection may be warranted as supplemental therapy in resistant cases. Repeated injections of corticosteroids should be avoided and have been associated with rupture of the plantar fascia and fat pad atrophy.14 In a recent study, 50 units of botulinum toxic type A injected into the plantar fascia decreased pain in comparison to placebo but did not cure the disease.15
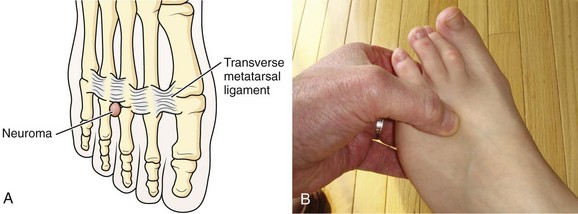
Forefoot Neuroma
A forefoot neuroma, also known as Morton’s neuroma, is a painful condition of the plantar surface of the foot. It most commonly affects women who wear high-heeled shoes. The neuroma forms after chronic irritation to the digital sensory nerve between the metatarsals. A neuroma frequently occurs in the third interspace but may be found in the second space (Fig. 51-4A). Patients report the sensation of a lump or cord in the interspace and describe paresthesia or numbness in the third or fourth toes. Direct compression plus release of the forefoot causes pain and often a “click” (the Mulder sign) (see Fig. 51-4B). Rest, elevation, ice, and NSAIDs may result in some improvement, but surgical excision is often required.16,17 Few data support the use of corticosteroid injections. In one study, less than 50% of patients with a foot neuroma had any benefit from injected corticosteroids.16 Another study demonstrated complete or partial relief in 80% of patients injected with corticosteroids.18 Although this study demonstrated a trend toward improved outcome when injected corticosteroids were compared with footwear modifications, corticosteroid injection therapy alone was not statistically better than footwear modification at 1 year.18
Ganglion Cyst of the Foot
A ganglion cyst is histologically similar to the synovial sheath and contains synovial fluid. The diagnosis is easy to make when the cyst is located over a tendon on the dorsum of the foot (Fig. 51-5) but may be difficult when located among the compact structures of the plantar forefoot. A ganglion cyst usually causes edema along the involved tendon sheath. The mass should roll under the examiner’s finger; a painless, immovable mass suggests a soft tissue neoplasm. Painful ganglion cysts are treated by aspiration with or without injection of a corticosteroid (see Chapter 52). After local or regional anesthesia (see Chapters 29 and 31), insert a 20-gauge needle into the cyst and withdraw yellow, thick, synovial fluid. Manually express any remaining synovial fluid after the needle is withdrawn. Corticosteroid injection is often advocated for ganglion cysts, but recurrence is common after aspiration and corticosteroid injection—as high as 57% in one study.19 Recurrence, chronic pain, neuritis, stiffness, and infection are not uncommon even after surgical excision in many studies.20 Other authors report improved functional outcome, a 9% occurrence of paresthesia, and only a 5.7% recurrence rate after excision.21
Traumatic Conditions of the Foot
Toe Fractures and Fractures of the Sesamoid Bones
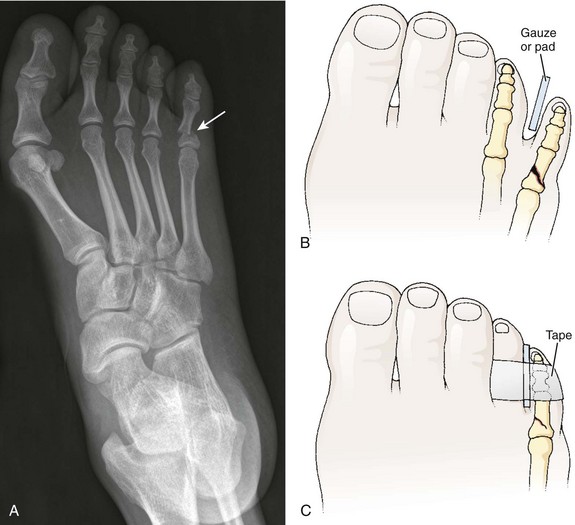
Emergency clinicians often treat toe fractures and can intervene to relieve the pain and encourage healing. As with any other fracture, pay attention to the possibility of disrupted joint cartilage, hypermobility of the fracture segments, and malposition or malunion of the fracture fragments. Fracture displacement greater than 2 mm is uncommon; reduction is rarely needed for most toe fractures.22 However, aggressive reduction is indicated for fractures of the proximal phalanx of the great toe because it represents the main propulsive segment of the forefoot (Fig. 51-6). A plaster cast alone without anatomic reduction is insufficient treatment. Displacement suggests axial rotation or abnormal biomechanical interaction between the hallux and its own interphalangeal or MTP joint.
Treat closed, lesser phalangeal fractures with “immobilization” for 6 weeks. After the fracture is reduced, splint the injured toe against an adjacent noninjured toe. Place a soft corn pad or other suitable material between the toes to prevent skin maceration, and hold the toes together with adhesive tape or a self-adherent wrap such as Coban (Fig. 51-7). Demonstrate the procedure to the patient or family and dispense or prescribe enough material so that the splint can be changed every 2 to 3 days at home. Have the patient wear a less restrictive, stiff-soled shoe (Fig. 51-8). A postoperative shoe (or similar footwear) may be a comfortable alternative for the first several days.
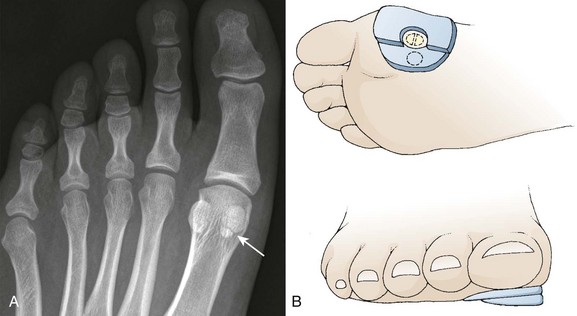
Jumping from a height can result in a fracture of the first MTP joint sesamoid bone (Fig. 51-9A). The great toe sesamoid bones lie in grooves on the bottom of the metatarsal head. Each bone lies within the tendon of its respective flexor hallucis brevis muscle belly. Localized pain on the plantar aspect of the first metatarsal head accompanies a sesamoid bone fracture. Bipartite sesamoids (tibial more frequently than fibular) are common. Comparison radiographs clarify whether the radiographic abnormality represents a fracture.
For a tibial sesamoid injury, an aperture bunion-type pad, reinforced medially with 0.5- to 0.75-cm-thick felt, protects the sesamoid and transfers weight bearing to the surrounding structures (see Fig. 51-9B). A hard-soled shoe and NSAIDs are also helpful. Subsequent radiographs rarely show bony consolidation, but the fracture interface appears smoother.
Stress Fractures
A metatarsal stress fracture, commonly of the distal second and third metatarsals, can develop in runners, military recruits, or those with repetitive trauma to the foot (Fig. 51-10). Other risk factors are listed in Box 51-1.23 There is pain on walking but minimal to no external findings. A bone scan or magnetic resonance imaging (MRI) may detect the subtle fracture that often eludes a plain radiograph. Occasionally, an occult foreign body (FB) of the foot is the culprit and can mimic a stress fracture. Women are more prone than men to stress fractures. Treatment is usually rest and alleviation of the precipitant causes.
Plantar Puncture Wounds
Although nails produce many such wounds, various other objects may cause them, including other metal objects, wood, and glass. Patient response to the injury depends on the penetrating material, location and circumstances of the wound, depth of penetration, footwear, time from injury until initial evaluation, and underlying health. Since superficial puncture wounds generally do well, depth of penetration may be a primary determinant of outcome.24 Because one’s reflexes are not fast enough to pull back when stepping on a sharp object, the clinician should assume that the entire length of a protruding nail has entered the foot (minus the thickness of the footwear). Stepping on an unknown object in a field or while walking in a stream requires a more cautious approach than does a simple puncture from a known object, such as a protruding nail.
The vast majority of patients who step on a nail suffer nothing more than transient pain and never seek medical attention. Because most minor puncture wounds are not seen in the ED, the true risk for infection, including osteomyelitis, is unknown. Consequently, reported infection rates vastly overstate the actual incidence. Probably no more than 2% to 8% of puncture wounds become infected, and in only a small percentage of these wounds does osteomyelitis develop.24,25 A prospective series suggested that only the presence of symptoms (e.g., redness, tenderness, increased swelling) at 48 hours is associated with risk for infection or a potential retained FB.26 Retained foreign material (e.g., a portion of a tennis shoe sole) in the wound is an important factor in persistent infection. Because no single test detects all possible FBs, tailor the evaluation of a suspected FB to the suspected object.
Evaluation
The approach to the patient depends on several factors, including the time from injury to evaluation, suspicion of an FB, and the presence of infection. The extent to which an FB is pursued depends on the history and findings on physical examination. When the patient clearly states that a needle, pin, or nail was removed intact, radiographs or local wound exploration for a retained metallic FB is not needed. Stepping on an identified intact nail does not always require a radiograph, but if there is any debate regarding a retained metallic object, plain radiographs readily demonstrate their presence. Plain radiographs also demonstrate other radiopaque objects such as glass, gravel, bone, and teeth (Fig. 51-11). Rubber or pieces of a sock will not be visible on a radiograph. If the patient steps on an unknown object, a radiograph is usually indicated unless the entire depth of the wound can be ascertained and inspected. Ultrasonography is noninvasive and does not use radiation, thus making it potentially useful for radiolucent FBs, but soft tissue air or calcifications may suggest a retained FB when none is present. Bedside ultrasound has been used to localize radiolucent FBs for removal.27,28 Computed tomography (CT) can demonstrate radiopaque and radiolucent objects, but its expense and greater radiation exposure than with plain films make it unsuitable as an initial screening tool. Use CT scanning when other screening tools fail to demonstrate a suspected FB, when infection is present, or when joint penetration is suspected. Fluoroscopy may be used to help localize metallic or radiopaque FBs during exploration and removal. It may be particularly useful for long metallic objects such as needles and pins. MRI provides no additional benefit and cannot be used when metallic objects are retained. Diabetics with unexplained foot pain or infection warrant investigation for a retained FB; diabetic neuropathy may mask the initial puncture injury.
Treatment
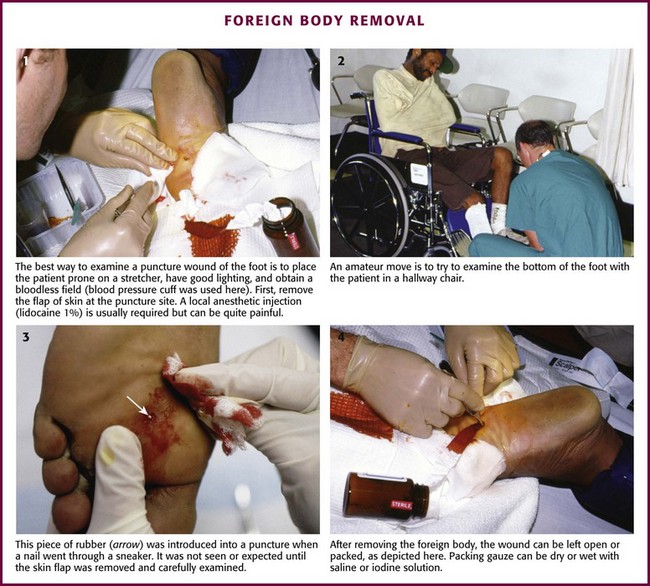
As a general rule, the plantar surface of the foot should be examined under good lighting and in a bloodless field. This is best accomplished with the patient in a prone position, not in a chair (Fig. 51-12). Plantar puncture wounds explored for persistent infection often have foreign material in them. Because persistent infection does not develop in most patients, initial deep exploration in the absence of evidence or strong suspicion of retained material cannot be advocated.24 Routine initial deep wound exploration, including coring of the wound, is not supported by scientific research and is not recommended for simple, noninfected puncture wounds.24 However, selected wounds may benefit from exploration to facilitate a search for FBs and to promote irrigation, cleansing, and drainage. When the wound is large and retained organic material is suspected, local wound exploration may be warranted. Patients wearing rubber-soled shoes during plantar puncture wounds may retain a portion of the shoe in the wound. Exploration of the wound is most productive after local anesthesia or a regional anesthetic block and excision of the epidermal flap. An incision may be required to facilitate removal of the FB when known, but extensive removal of surrounding tissue has not been proved to increase successful removal of retained material.24
Some clinicians favor a coring technique when an FB is found or suspected. Although this may be too aggressive for many wounds, it may be the best way to remove particulate matter as a block (Fig. 51-13). To accomplish coring, advance a No. 11 blade to the hilt and excise a 2- to 3-mm core. Use a hemostat to grab the cutout core or to open the tract to better visualize the wound. Alternatively, use a 2- to 3-mm punch biopsy instrument to core out the tract. The tract can be packed with gauze for a few days or be left open. There is no evidence that coring a plantar puncture wound produces better outcomes than conservative or expectant treatment does, and it should be reserved for selected cases. Occasionally, blunt probes may facilitate exploration of the wound. It is generally impossible and probably counterproductive to attempt to probe or visualize the entire length of the puncture tract. Patients initially seen within 24 hours and without signs of infection generally require only simple topical wound care. Although irrigation of all exposed dermal tissue is recommended, high-pressure irrigation of deep tissues with distention of soft tissues is unlikely to be helpful and is not recommended. Schwab and Powers described a case series of uncomplicated puncture wounds in healthy individuals who underwent conservative treatment with cleansing and crutches.26 Radiographs were obtained at the discretion of the treating clinician, and antibiotics were not given. At the 6-month follow-up, 88% of all patients healed without complication. In the remaining 12% complications developed, including wound infection from retained FBs. No findings on initial evaluation predicted a subsequent infection. Initial antibiotic therapy remains controversial, but there is no evidence to suggest that prophylactic antibiotics reduce the already low rate of infection. In fact, some cases of Pseudomonas osteomyelitis develop despite initial treatment with anti-Pseudomonas antibiotics. The author does not suggest routine prophylactic antibiotics for uncomplicated puncture wounds, and such treatment may theoretically select out resistant organisms.
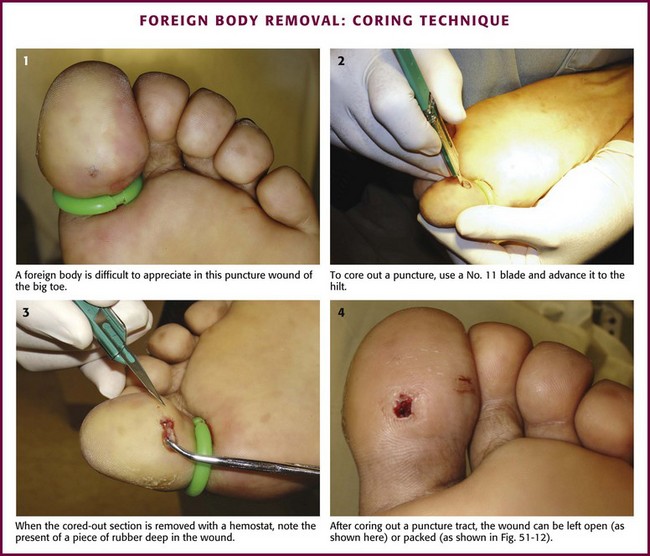
Figure 51-13 Foreign body removal: coring technique.
Patients with obvious signs of infection within a few days of a puncture wound usually have a simple cellulitis (with or without an FB) with a gram-positive organism (Fig. 51-14). In a patient with persistent pain or swelling days to weeks after a puncture wound, the presence or absence of a deep soft tissue infection or low-grade osteomyelitis cannot be ruled in or ruled out by physical examination, plain radiographs, or laboratory tests (such as a sedimentation rate, complete blood count, or wound cultures). A high index of suspicion, coupled with additional investigation, is the prudent approach to patients with minimal findings on physical examination, normal laboratory test results, and continued pain or swelling after a seemingly simple puncture wound in the bottom of the foot. This usually entails CT, bone scan, or MRI. A study of 80 children with plantar puncture wounds and signs of infection found simple cellulitis in 59, retained FBs in 11, and osteomyelitis or septic arthritis in 10 children. Because a significant number of children in this study had retained FBs or bony infections, a cautious approach is warranted.29
Plantar puncture wounds complicated by Pseudomonas osteomyelitis and osteochondritis are clinically clandestine and particularly devastating. They have been described for nearly 40 years. Some investigators have cultured Pseudomonas from the soles of tennis shoes, thus suggesting that puncture wounds made through athletic footwear may be inoculated with Pseudomonas (Fig. 51-15).30 No evidence suggests that prescribing prophylactic anti-Pseudomonas antibiotics on initial evaluation of an uncomplicated wound will prevent infection in patients with subsequent deep space or bone infections.30 Some argue that prophylactic antibiotics, at the time of puncture, may select out resistant organisms.30 Surgical débridement and prolonged intravenous antibiotics are often required for established infections.
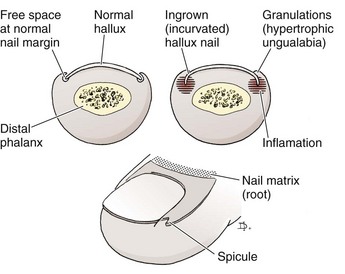
Ingrown Toenail
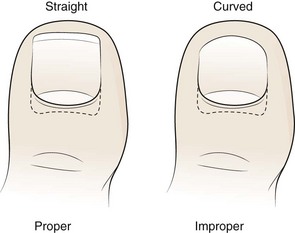
An ingrown toenail is characterized by progressive curving or excessive widening of the lateral margin of the toenail and impingement of the nail into the periungual soft tissue (Fig. 51-16). The toenail normally grows distally in an unimpeded manner, thereby allowing the nail to pass beyond the lateral nail fold. Nail deformity, tight-fitting shoes, and rotational deformity of the toes increase the friction between the nail and the nail fold (Fig. 51-17). Toenails that have been trimmed in a curve increase the likelihood that the lateral nail margin will impinge on the lateral nail fold. The resulting soft tissue injury may lead to hyperkeratosis, edema, and erythema of the nail fold or frank infection (Fig. 51-18). Although an ingrown toenail can be found on any toe, the majority occur on the great toe.

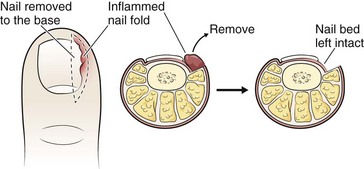
Figure 51-18 An ingrown toenail of this degree requires removal of a portion of the nail and débridement of inflamed tissue.
Treatment
Because the toe is exquisitely tender, additional treatment will usually require digital block anesthesia. The decision to treat and what course of action to take in the ED depend on the patient’s degree of discomfort. Two general courses of action are often suggested: removal of the offending nail spicule or removal of the spicule and some portion of the nail. Any degree of nail removal is usually followed by ablation of the nail bed.31 Nail-splinting techniques may also be effective and are less invasive than nail removal techniques.
Removal of the Nail Spicule and Débridement of Hyperkeratosis for Minor Ingrown Toenails
When the amount of inflammation and pain and the degree of nail deformity are both minimal, such as involvement of only the distal toenail area, simple removal of the impacted nail spicule is indicated and usually curative. If the condition is advanced, complete removal of a portion of the nail may be required. All procedures are best done with a tourniquet to produce a bloodless field. After a digital block and thorough cleansing, remove an oblique segment of the nail about one third to one half the way to the proximal nail fold (Fig. 51-19). The ideal instrument is an English anvil nail splitter, which is designed to cut the nail while minimizing trauma to the underlying nail matrix (Fig. 51-20). Sharp, pointed scissors may be substituted if care is taken to minimize injury to the nail bed by maintaining upward pressure while cutting the nail. Some clinicians use a disposable electric cautery device to cut the nail after softening it by soaking in warm soapy water.

Figure 51-20 English nail anvil used to divide the nail. (Courtesy of Gill Podiatry Supply Company, Middleburg Heights, OH.)
After cutting the nail spicule free from the bulk of the nail, grasp the free edge of the nail with forceps or hemostats and remove it to expose the irritated area. The nail fold typically contains impacted debris that must be removed after the nail fold has been gently retracted away from the nail. Remove debris until the epidermis or dermis is uncovered while taking care to avoid aggressive débridement that causes bleeding. A silver nitrate stick applied to the débrided area may be used to control bleeding. Dress the area with antibiotic ointment and a nonadherent dressing. Soaking the toe in warm water two or three times a day, with home redressing, is explained. Harsh chemicals are avoided in the soaking regimen. The wound should be reinspected for signs of infection at 48 to 72 hours. If the problem has resolved, no further therapy is necessary. If the problem is persistent or recurrent, referral for definitive podiatric care is reasonable. Instruct patients to wear less constricting shoes and to trim the nail straight across. Like most FB reactions, removal of the nail spicule resolves the inflammation and infection. Antibiotics given without removal of the nail spicule will not ensure a satisfactory result or add benefit after removal of the spicule.32 Topical antibiotics (avoid those containing neomycin) are reasonable, but systemic antibiotics are not required. Diabetics and those with peripheral vascular disease require closer follow-up. When the ingrown toenail is caused by a nail deformity, a podiatrist or primary clinician can perform definitive removal during follow-up evaluation.
Toenail Removal for Complex or Extensive Ingrown Toenails
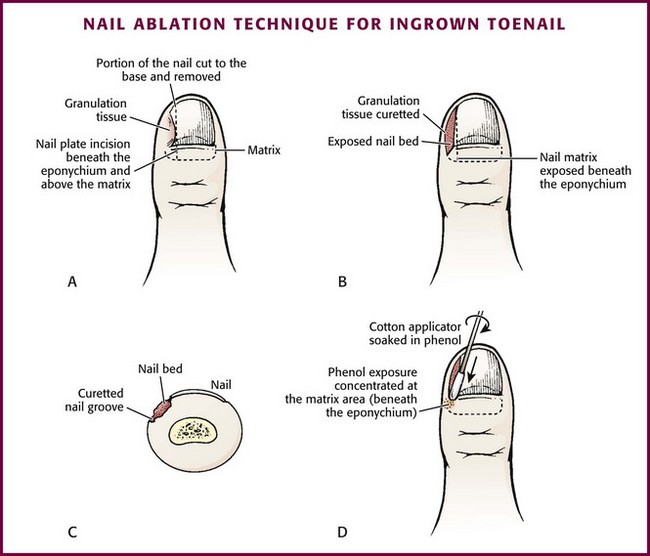
When irritation, infection, or both are more widespread or include the entire toe, removal of a portion of the nail and débridement of the inflamed tissue may be required (Figs. 51-21 and 51-22). Toenail removal may be total or partial. Total nail removal is rarely needed but may be done when both lateral nail folds are infected, particularly if the condition has been present for more than a month. Consider partial removal of the toenail when ingrown toenails are associated with chronic inflammation, infection, or severe pain. Partial nail removal accomplishes two things: removal of the offending portion of nail and destruction of the underlying nail matrix to prevent regrowth of the nail. Phenol, the most commonly applied chemical, causes neurolysis of the nerve endings and necrosis of the nail matrix in a procedure called matricectomy. Several studies have demonstrated that 10% sodium hydroxide solution is as effective as phenol and may be associated with less postprocedure pain and faster recovery.33–35 Since most EDs do not stock phenol or sodium hydroxide solution, nail bed ablation is usually not pursued on the initial visit.
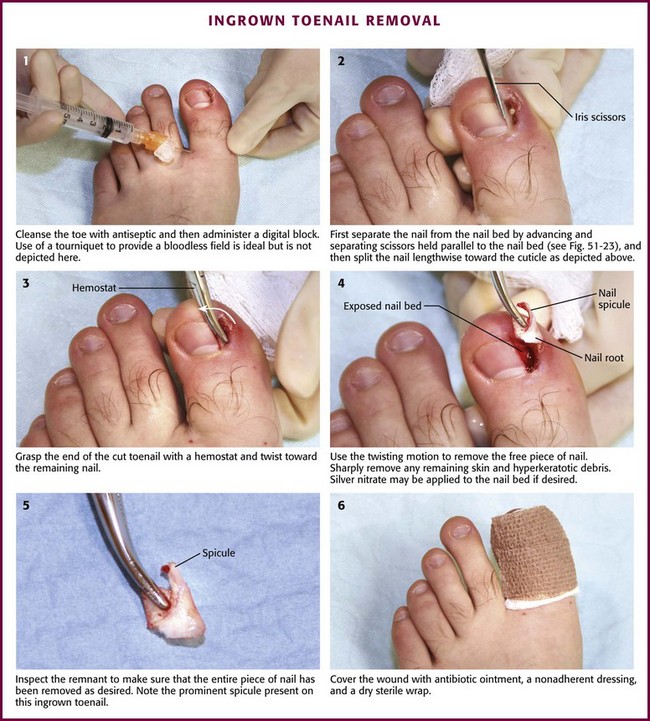
Figure 51-22 Removal of an ingrown toenail.
After a digital block, exsanguinate the toe by squeezing or wrapping, and apply a tourniquet at the base of the toe. Stabilize the toe with the nondominant hand. Separate the lateral third of the nail from the nail bed by advancing and separating scissors held parallel to the nail bed (Fig. 51-23). Split the nail lengthwise toward the cuticle. An English anvil nail splitter is desirable to begin the procedure, but sharp scissors or a No. 11 blade also work. Take care to perform a controlled division along the longitudinal lines of the nail for several millimeters past the proximal nail fold (cuticle). Grasp the end of the cut toenail with a hemostat or forceps. Remove the free piece of nail by twisting it toward the remaining nail. This will pull the nail root out from under the cuticle. Inspect the remnant to be certain that the entire piece of nail has been removed as desired. Sharply remove any remaining or swollen/heaped-up skin and all hyperkeratotic debris. After removal of the nail, most clinicians apply a silver nitrate stick to the nail bed and to granulation tissue for 2 to 3 minutes.36 When finished, the nail bed is open and the heaped-up tissue is now flat.
As an option and if phenol or other ablating solutions are available, the following is suggested to permanently ablate the nail bed so that a new nail will not grow (Fig. 51-24). Apply a 10% sodium hydroxide solution to the nail bed with a cotton-tipped applicator for 1 to 2 minutes to provide effective ablation of the nail matrix.33–35 Alternatively, apply a 1% solution of aqueous phenol to the nail matrix beneath the involved area of the lateral nail groove and proximal nail fold with cotton-tipped applicators. A 1% phenol solution can be prepared by diluting a 70% to 90% aqueous phenol solution in an 80 : 1 ratio (e.g., 8 mL distilled water to 0.1 mL phenol). Remove some of the cotton if the applicator is too bulky to concentrate the solution beneath the proximal nail fold and lateral nail groove. Apply thoroughly moistened (but not saturated) applicators for three 30-second applications. Avoid forcing phenol under the remaining nail by rolling the applicator so that it rolls over the matrix and over the nail surface rather than against the split edge of the nail. Although it is necessary to cover the lateral aspect of the nail bed and lateral nail fold, do not allow excess phenol to contact the exposed nail bed or surrounding healthy tissue. After the third application, the cauterized tissue appears brown tinged or gray. Alternatively, a 1% phenol solution can be applied for 5 minutes. Thoroughly irrigate the cauterized nail bed with water and rub the area with a gloved finger to remove all traces of phenol. Snip away any remaining debris or dead skin with scissors.
Apply antibiotic ointment (not containing neomycin) and a nonadherent dressing to the wound, followed by a dry sterile wrap. Do not forget to remove the tourniquet after the dressing has been applied. Instruct the patient to wash the wound twice daily followed by dry dressing changes. Systemic antibiotics do not hasten wound healing and are not necessary in most cases.31,32 Soaking the open wound in warm water twice a day is soothing and allows the patient to view the healing process. The wound will heal in 2 to 4 weeks and may be accompanied by serous drainage for 2 weeks. The patient should be informed of this possibility. Complications include nail regrowth, infection, growth of an inclusion cyst, or delayed healing. If the condition returns, podiatric referral is recommended for more extensive ablation of the nail bed.
Nail-Splinting Technique
Splinting of the nail spicule at the lateral edge of the affected nail may allow the toenail to grow out without affecting the inflamed soft tissue. This technique provides time for the periungual tissue to heal while the nail continues to grow until it can be trimmed straight across. No portion of the nail is removed when the nail is initially splinted. When the degree of inflammation is minimal, elevation of the nail spicule is easily accomplished with forceps or a hemostat. A cotton pledget inserted under the lateral edge to maintain elevation is often sufficient in minor cases. Alternatively, a wound closure strip can be used to elevate the corner of the offending nail.37 After cleansing the edge of the nail and providing drainage if an abscess is present, insert a wound closure strip obliquely under the corner of the nail with a to-and-fro sawing motion until the corner is sufficiently elevated. Secure the tape closure around the toe (Fig. 51-25A). Instruct the patient to soak the toe in warm water daily, remove the tape closure, and reinsert a new tape strip. This procedure is repeated until the corner of the nail or the nail spicule has grown out and cleared the periungual soft tissue, at which time it can be cut straight across. When the degree of inflammation is moderate, nail splinting is accomplished by using the flexible tube procedure.38,39 Obtain a surgical drain used to perform percutaneous drainage procedures that is 2 to 3 mm in diameter or the small tubing in venipuncture kits. Split a 1-cm piece of the drainage tube lengthwise. Perform a digital block and elevate the lateral edge of the nail with forceps or a hemostat. Insert the split drainage tube along the lateral edge of the nail so that it completely encircles the nail spicule and push it proximately until as much of the lateral nail and nail spicule as possible are covered (see Fig. 51-25B). Some authors suggest that the tube be secured with 2-0 suture passed through the nail,38 but securing the tube with wound closure strips is more easily accomplished.39 Instruct the patient to wash the affected area daily and replace loosened tape strips when needed. When the inflammation and granulation tissue have subsided and the nail spicule has grown sufficiently to not impinge on the periungual soft tissue, the tube splint is removed by the patient and the nail is cut straight across.
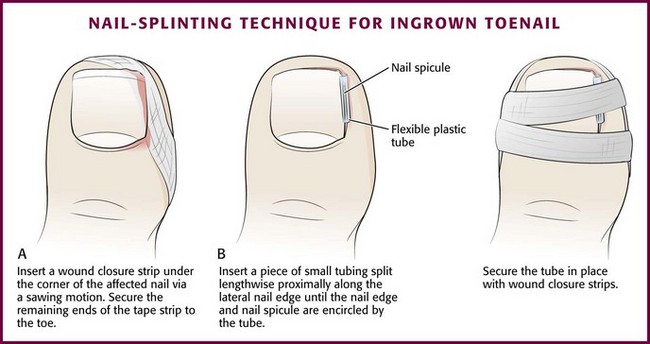
Figure 51-25 Splinting techniques for ingrown toenails.
References
1. Shama, SS, Kominsky, SJ, Lemont, H. Prevalence of non-painful heel spur and its relation to postural foot position. J Am Podiatr Assoc. 1983;24:490–493.
2. Levy, JC, Mizel, MS, Clifford, PD, et al. Value of radiographs in the initial evaluation of non-traumatic adult heel pain. Foot Ankle Int. 2006;27:427.
3. Atkins, D, Crawford, F, Edwards, J, et al. A systematic review of treatments for the painful heel. Rheumatology (Oxford). 1999;38:968.
4. Crawford, F, Atkins, D, Edwards, J. Interventions for treating plantar heel pain. Cochrane Database Syst Rev. (3):2003. [CD000416].
5. Crawford, F, Atkins, D, Young, P, et al. Steroid effectiveness for heel pain: evidence of short-term effectiveness. A randomized controlled trial. Rheumatology (Oxford). 1999;38:974.
6. Tisdel, CL, Harper, MC. Chronic plantar heel pain: treatment with a short leg walking cast. Foot Ankle Int. 1996;17:41.
7. Myerson, MS, eds. Foot and Ankle Disorders, Vol 2. Philadelphia: Saunders, 2000.
8. de Vos, RJ, Weir, A, van Schie, HTM, et al. Platelet-rich plasma injection for chronic Achilles tendonopathy. JAMA. 2010;303:144–149.
9. de Jonge, S, de Vos, RJ, Weir, A, et al. One year follow-up of platelet-rich plasma treatment in chronic Achilles tendonopathy. Am J Sports Med. 2011;39:1623–1629.
10. Micheli, LJ, Ireland, ML. Prevention and management of calcaneal apophysitis in children: an overuse syndrome. J Pediatr Orthop. 1997;7:34.
11. Kose, O. Do we really need radiographic assessment for the diagnosis of non-specific heel pain (calcaneal apophysitis) in children? Skeletal Radiol. 2010;39:359–361.
12. DellaCorte, MP. The heel subtalar complex and ankle. In: Birrer RB, DellaCorte MP, Grisafi PJ, eds. Common Foot Problems in Primary Care. 2nd ed. Philadelphia: Hanley & Belfus; 1998:76.
13. Donley, BG, Moore, T, Sferra, J, et al. The efficacy of oral nonsteroidal anti-inflammatory medication (NSAID) in the treatment of plantar fasciitis: a randomized, prospective, placebo-controlled study. Foot Ankle Int. 2007;28:20.
14. Acevedo, JI, Beskin, JL. Complications of plantar fascia rupture associated with corticosteroid injection. Foot Ankle Int. 1998;19:91.
15. Huang, YC, Wei, SH, Wang, HK, et al. Ultrasonographic guided botulinum toxin type A for plantar fasciitis: an outcome-based investigation for treating pain and gait changes. J Rehabil Med. 2010;42:136–140.
16. Rasmussen, MR, Kitaoka, HB, Patzer, GL. Nonoperative treatment of plantar interdigital neuroma with a single corticosteroid injection. Clin Orthop Relat Res. 1996;326:188.
17. Wu, KK. Morton’s interdigital neuroma: a clinical review of its etiology, treatment and results. J Foot Ankle Surg. 1996;35:112.
18. Saygi, B, Yildirim, Y, Saygi, EK, et al. Morton’s neuroma: comparative results of two conservative methods. Foot Ankle Int. 2005;26:556.
19. Pontious, J, Good, J, Maxian, SH. Ganglions of the foot and ankle: a retrospective analysis of 63 procedures. J Am Podiatr Med Assoc. 1999;89:163.
20. Rozbruch, SR, Chang, V, Bohne, WH, et al. Ganglion cysts of the lower extremity: an analysis of 54 cases and review of the literature. Orthopedics. 1998;21:141.
21. Ahn, JH, Choy, WS, Kim, HY. Operative treatment for ganglion cysts of the foot and ankle. J Foot Ankle Surg. 2010;49:442–445.
22. Van Vleit-Koppert, ST, Cakir, H, Van Lieshout, MM. Demographics and functional outcome of toe fractures. J Foot Ankle Surg. 2011;50:307–310.
23. Sanderlin, BW, Raspa, RF. Common stress fractures. Am Fam Physician. 2003;68:1527.
24. Chisholm, CD, Schlesser, JF. Plantar puncture wounds: controversies and treatment recommendations. Ann Emerg Med. 1989;18:1352.
25. Weber, EJ. Plantar puncture wounds: a survey to determine the incidence of infection. J Accid Emerg Med. 1996;13:274.
26. Schwab, RA, Powers, RD. Conservative therapy of plantar puncture wounds. J Emerg Med. 1995;13:291.
27. Dean, AJ, Gronczewski, CA, Costanino, TG. Technique for emergency medicine bedside ultrasound identification of a radiolucent foreign body. J Emerg Med. 2003;24:303.
28. Imoisili, MA, Bonwit, AM, Bulas, DI. Toothpick puncture injuries of the foot in children. Pediatr Infect Dis J. 2004;23:80.
29. Eidelman, M, Bialak, V, Miller, Y, et al. Plantar puncture wounds in children: analysis of 80 hospitalized patients and late sequelae. Isr Med Assoc J. 2003;5:268.
30. Inaba, AS, Zukin, DD, Perro, M. An update on the evaluation and management of plantar puncture wounds and Pseudomonas infection. Pediatr Emerg Med. 1992;8:38.
31. Fulton, GJ, O’Donohoe, MK, Reynolds, JV. Wedge resection alone or combined with segmental phenolization for the treatment of ingrowing toenail. Br J Surg. 1994;81:1074.
32. Reyzelman, AM, Trombello, KA, Vayser, DJ, et al. Are antibiotics necessary in the treatment of locally infected ingrown toenails? Arch Fam Med. 2000;9:930.
33. Bostanci, S, Kocyigit, P, Gürgey, E. Comparison of phenol and sodium hydroxide chemical matricectomies for the treatment of ingrowing toenails. Dermatol Surg. 2007;33:680–685.
34. Ozdemir, E, Bostanci, S, Ekmekci, P, et al. Chemical matricectomy with 10% sodium hydroxide for the treatment of ingrowing toenails. Dermatol Surg. 2004;30:26.
35. Kocyigit, P, Bostanci, S, Ozdemir, E, et al. Sodium hydroxide chemical matricectomy for the treatment of ingrown toenails: a comparison of three different application periods. Dermatol Surg. 2005;31:744.
36. Erdogan, FG. A simple, pain free treatment for ingrown toenails complicated with granulation tissue. Dermatol Surg. 2006;32:1388.
37. Lazar, L, Erez, I, Katz, S. A conservative treatment for ingrown toenails in children. Pediatr Surg Int. 1999;15:121.
38. Abby, NS, Roni, P, Amnon, B, et al. Modified sleeve method treatment of ingrown toenail. Dermatol Surg. 2002;28:852.
39. Salasche, SJ, Schulte, KW, Neumann, NJ, et al. Surgical pearl: nail splinting by flexible tube—a new noninvasive treatment for ingrown toenails. J Am Acad Dermatol. 1998;39:629.