Pilar and sebaceous neoplasms
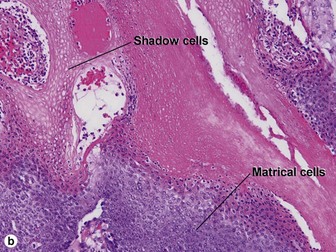
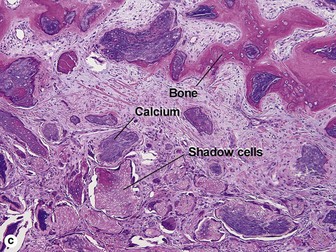
Pilar neoplasms
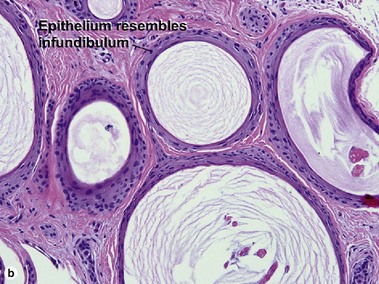
Pilar neoplasms differentiate towards (resemble) various parts of the normal hair follicle. They are named according to what they resemble. Before reading this chapter, review the discussion of hair anatomy in Chapter 1. Blue pilar tumors differentiate towards elements of the inferior segment of the hair follicle. Red pilar tumors differentiate towards the isthmus and infundibulum. Clear cell tumors differentiate towards the glycogenated outer root sheath.
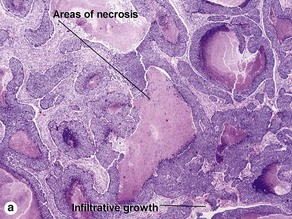
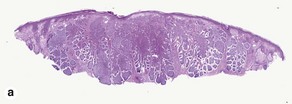
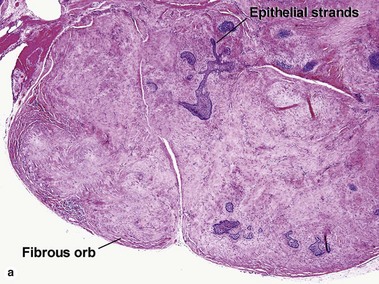
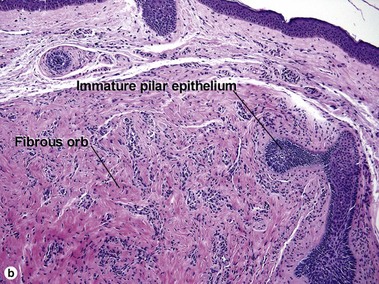
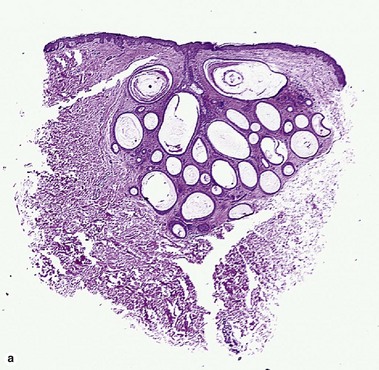
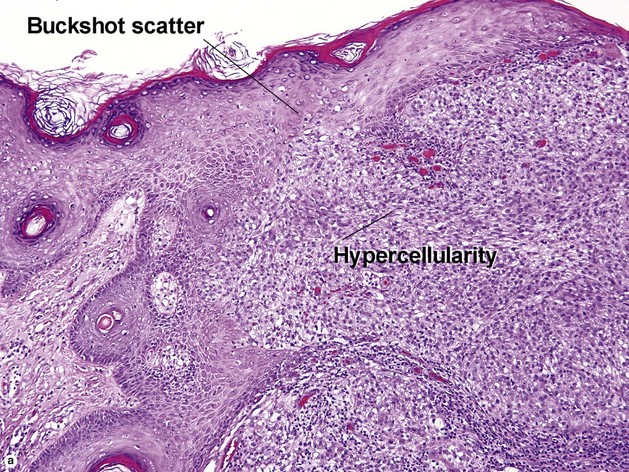
Trichoblastoma
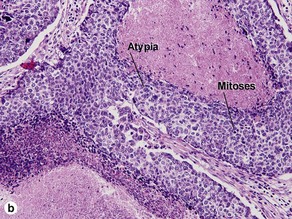
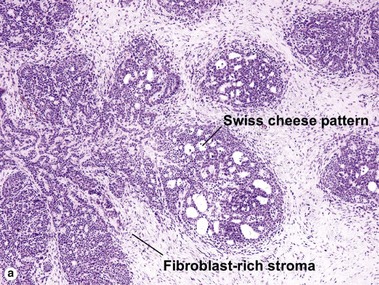
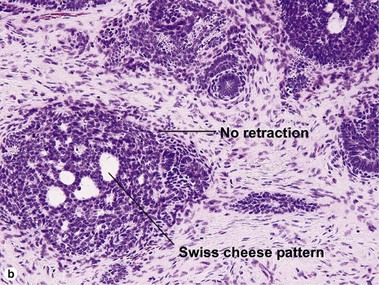
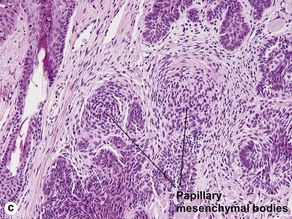
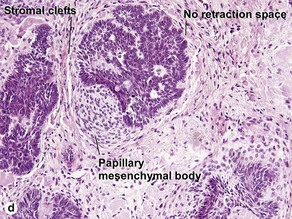
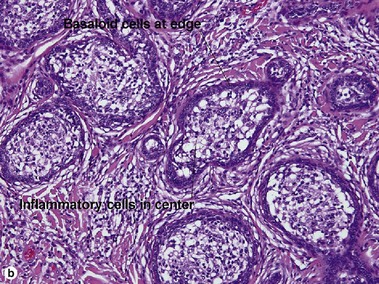
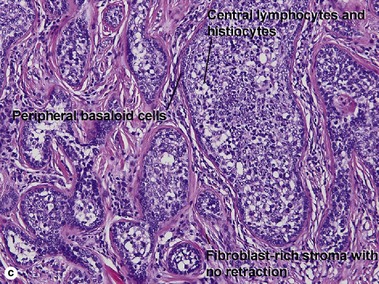
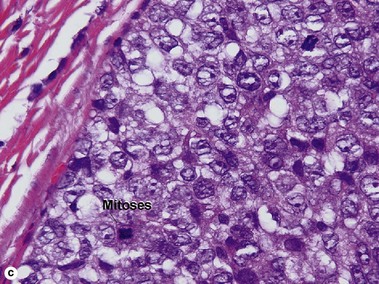
Benign trichoblastomas are large basaloid follicular neoplasms. The tumor islands resemble basal cell carcinoma, but the stroma resembles the normal fibrous sheath of the hair follicle. Trichoepitheliomas and lymphadenomas are distinctive forms of benign trichoblastoma. Trichogerminomas are a type of trichoblastoma with differentiation towards the hair germ. Basal cell carcinoma is the most common malignant counterpart of a benign trichoblastoma. Some trichoblastic carcinomas arising in long-standing trichoblastomas have been very aggressive tumors with metastases.
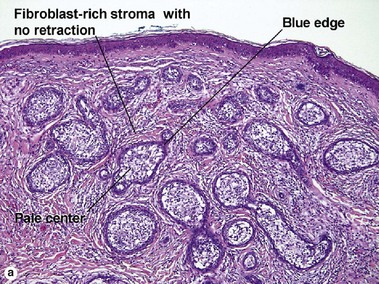
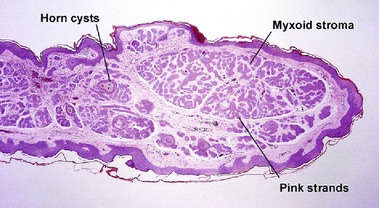
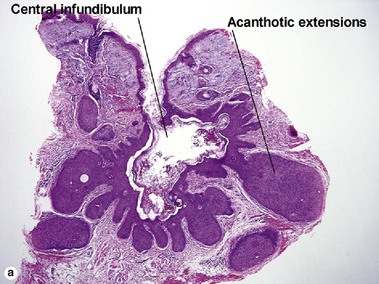
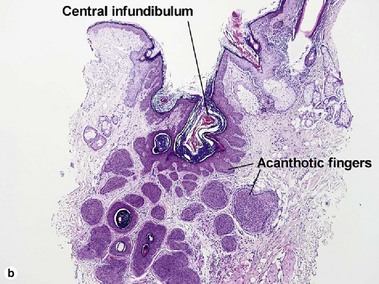
Trichoepithelioma
Table 4-1
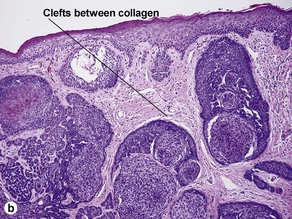
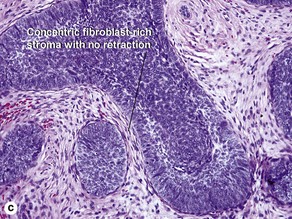
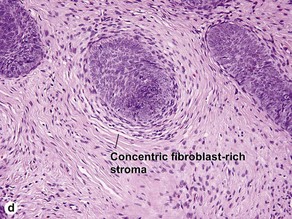
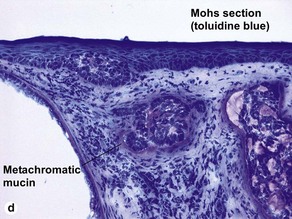
Characteristics of trichoepithelioma versus basal cell carcinoma
| Characteristic | Trichoepithelioma | Basal cell carcinoma |
| Basaloid cells | Yes | Yes |
| Peripheral palisading | Yes | Yes |
| Finger-like and cribriform | Yes | Sometimes |
| Stroma | Concentric, fibroblast-rich | Myxoid |
| Mucin | In tumor islands only, none in stroma | Metachromatic mucin in stroma |
| Papillary mesenchymal bodies | Common | Rare |
| Horn cysts | Common | Rare |
| Calcification | Common | Rare |
| Clefts | Between collagen fibers within stroma | Between epithelium and stroma |
| CD34 staining | Strong staining in stroma | +/− |
| BCL-2 staining | Periphery of islands | Strong, diffuse |
| CK20+ Merkel cells | Present in tumoral islands | Absent in tumoral islands |
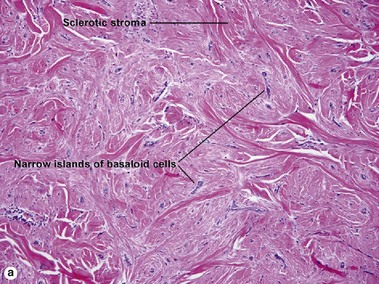
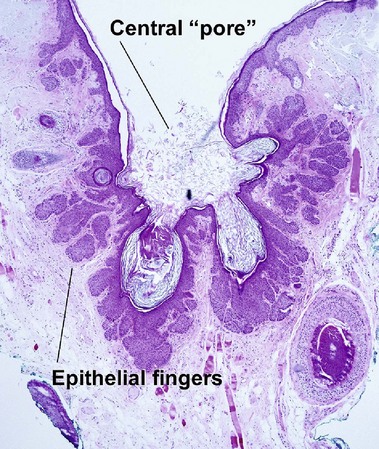
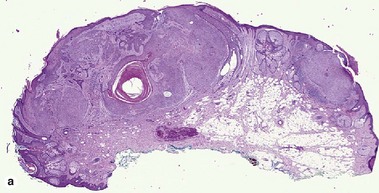
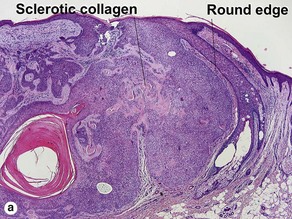
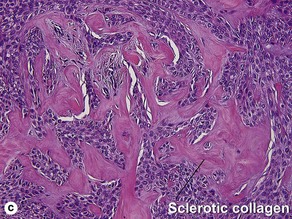
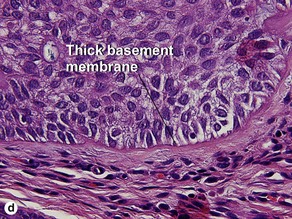
Desmoplastic trichoepithelioma
Table 4-2
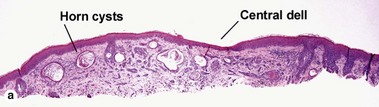
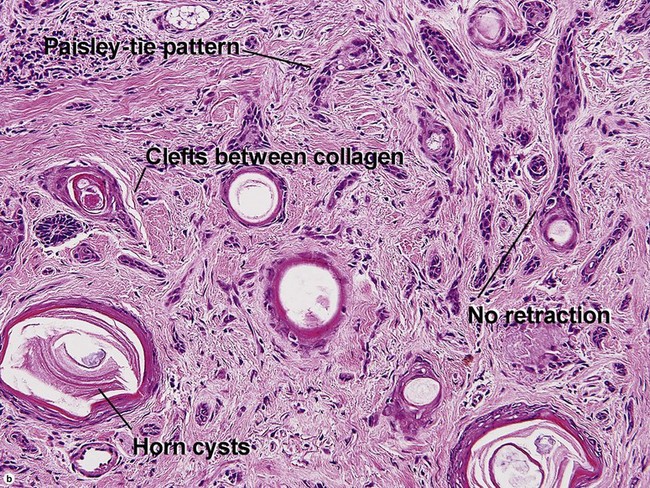
Characteristics of desmoplastic trichoepithelioma versus morpheaform basal cell carcinoma
| Characteristic | Desmoplastic trichoepithelioma | Morpheaform basal cell carcinoma |
| Paisley-tie pattern | Yes | Sometimes superficially |
| Stroma | Red, sclerotic | Red, sclerotic |
| Horn cysts | Common | Occasional |
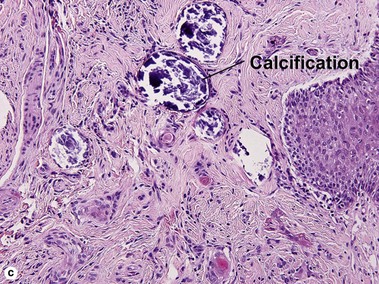
| Calcification | Common | Rare |
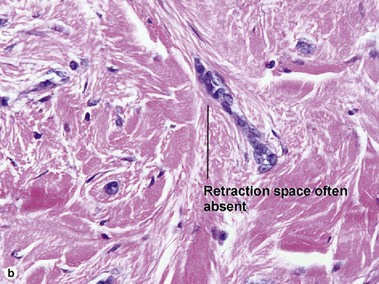
| Clefts | Between collagen fibers within stroma | Between epithelium and stroma |
| Central dell | Yes | No |
| Age | Younger | Older |
| Clinical appearance | Firm doughnut | Scar-like |
Table 4-3
Characteristics of desmoplastic trichoepithelioma versus microcystic adnexal carcinoma
| Characteristic | Desmoplastic trichoepithelioma | Microcystic adnexal carcinoma |
| Paisley-tie pattern | Yes | Yes |
| Stroma | Red, sclerotic | Often red, sclerotic |
| Horn cysts | Common | Common |
| Calcification | Common | Rare |
| Lymphoid aggregates | Rare | Typical |
| Perineural extension | No | Yes |
| Clinical appearance | Firm doughnut | Plaque on upper lip, cheek, chin |
| Central dell | Typical | Absent |
Table 4-4
Characteristics of desmoplastic trichoepithelioma versus syringoma
| Characteristic | Desmoplastic trichoepithelioma | Syringoma |
| Paisley-tie pattern | Yes | Yes |
| Stroma | Red, sclerotic | Red, sclerotic |
| Horn cysts | Common | May occur |
| Calcification | Common | Rare |
| Central dell | Typical | Absent |
| Shape | Broad | Small and round |
| Clinical appearance | Firm doughnut | Small papules |
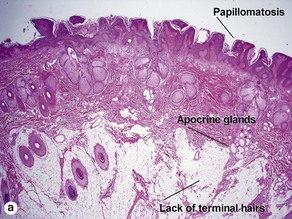
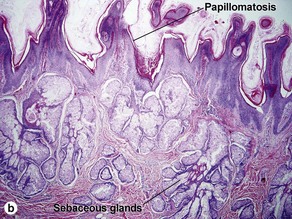
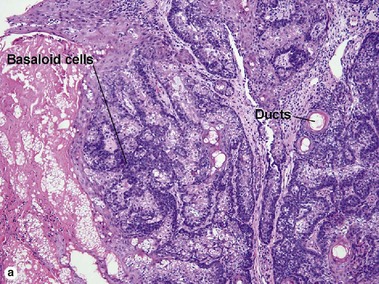
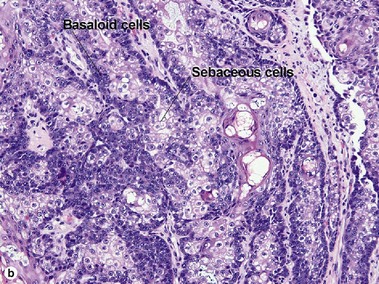
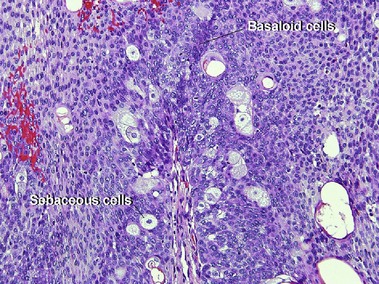
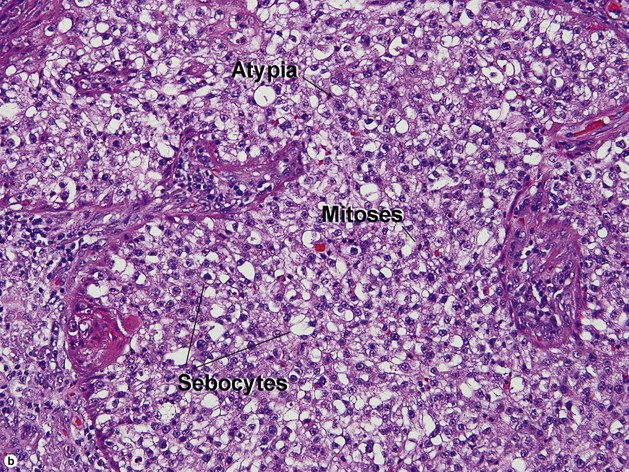
Sebaceous neoplasms
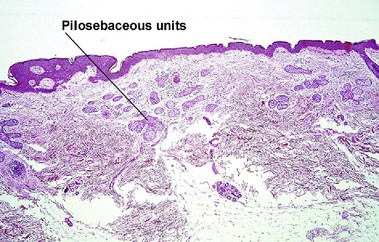
Nevus sebaceus of Jadassohn (organoid nevus)
Ansai, S, Mitsuhashi, Y, Kondo, S, et al. Immunohistochemical differentiation of extra-ocular sebaceous carcinoma from other skin cancers. J Dermatol. 2004; 31(12):998–1008.
Kazakov, DV, Kutzner, H, Rütten, A, et al. Trichogerminoma: a rare cutaneous adnexal tumor with differentiation toward the hair germ epithelium. Dermatology. 2002; 205(4):405–408.
Pereira, PR, Odashiro, AN, Rodrigues-Reyes, AA, et al. Histopathological review of sebaceous carcinoma of the eyelid. J Cutan Pathol. 2005; 32(7):496–501.
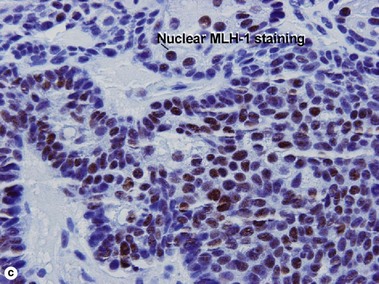
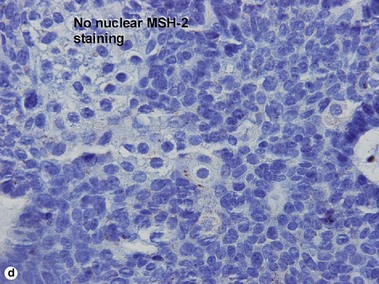
Ponti, G, Longo, C. Microsatellite instability and mismatch repair protein expression in sebaceous tumors, keratocanthoma, and basal cell carcinomas with sebaceous differentiation in Muir–Torre syndrome. J Am Acad Dermatol. 2013; 68(3):509–510.
Sidhu, HK, Patel, RV, Goldenberg, G. Dermatology clinics: what’s new in dermatopathology: news in nonmelanocytic neoplasia. Dermatol Clin. 2012; 30(4):623–641.
Tebcherani, AJ, de Andrade, HF, Jr., Sotto, MN. Diagnostic utility of immunohistochemistry in distinguishing trichoepithelioma and basal cell carcinoma: evaluation using tissue microarray samples. Mod Pathol. 2012; 25(10):1345–1353.
Tse, JY, Nguyen, AT, Le, LP, et al. Microcystic adnexal carcinoma versus desmoplastic trichoepithelioma: a comparative study. Am J Dermatopathol. 2013; 35(1):50–55.
Welsch, MJ, Krunic, A, Medenica, MM. Birt–Hogg–Dube Syndrome. Int J Dermatol. 2005; 44(8):668–673.