CHAPTER 16 Physeal Fractures of the Elbow
ANATOMY AND GROWTH
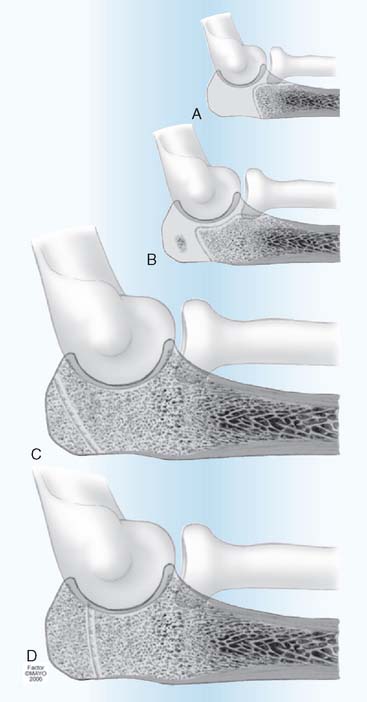
The elbow joint consists of the articulating surfaces of three epiphyses: the distal humerus, the proximal ulna, and the proximal radius. At birth, each epiphysis is one mass of cartilage, each with its own epiphyseal growth plate (the physis). With growth, the distal humerus develops four ossification centers1,2,4; the proximal ulna, two5; and the proximal radius, one.3 The lateral three distal humeral ossification centers eventually unite into one bony epiphysis; the fourth, the medial epicondyle, gradually separates from the others, becomes an apophysis, and no longer participates in longitudinal growth or joint articulation (Fig. 16-1). The two proximal ulna ossification centers unite to form one articulating epiphysis; its physis provides longitudinal growth, thereby qualifying it as a true epiphysis. Knowledge of the timing and pattern of ossification of these epiphyses, particularly the distal humerus, is essential in treating fractures of the elbow in children.
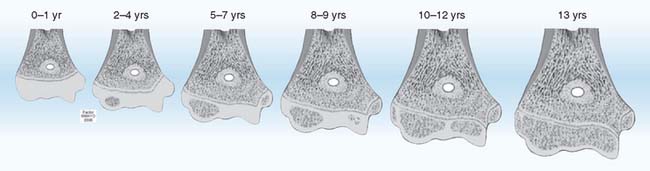
FIGURE 16-1 Distal humerus epiphysis growth centers at various ages. At birth, the physis is transverse and the epiphysis is one cartilaginous mass. By age 2 years, the capitellar ossification center is usually present.1 The physis still is relatively linear and transverse. At ages 5 to 7 years, there is mild obliquity of the epiphyseal growth plate to the longitudinal axis of humerus and beginning ossification of the medial epicondyle.4 Trochlear ossification begins at 8 to 9 years, is irregular with indistinct margins, and often appears as multiple fragments. At ages 10 to 12 years, a projection of metaphyseal bone separates the medial epicondyle from the major distal epiphysis, which now contains three ossification centers—capitellum, trochlea, and lateral epicondyle.2 These three ossification centers unite with each other in the 13th year and to the humeral epiphysis by the 16th year, earlier in girls. There is wide variation of ages of these occurrences between genders and among children, but the sequence is constant.
(From Peterson, H. A.: Epiphyseal Growth Plate Fractures. Heidelberg, Springer, 2007, used with permission of Mayo Foundation for Medical Education and Research.)
EPIDEMIOLOGY
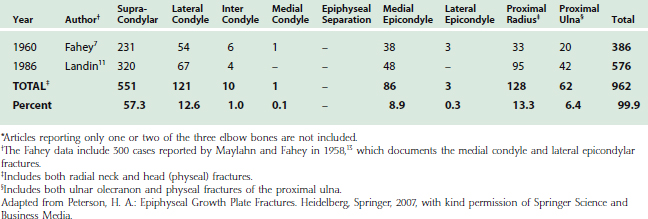
The incidence of fracture of physes of the elbow is unknown. Of all elbow fractures in children, slightly more than half are supracondylar fractures (Table 16-1). The vast majority of the remaining half are physeal fractures. When studying physeal fractures at all sites, the relative frequency of elbow fractures varies widely in different series.8,9,12,15–20 The only data available from a population-based study were gathered in Olmsted County, Minnesota, from 1979 to 1988.20 This study reported 951 cases of physeal fracture; 47 (5%) were in the elbow. Of these, 37 (3.9%) were in the distal humerus, 6 (0.6%) in the proximal radius, and 4 (0.4%) in the proximal ulna. Because elbow fractures in children are often referred to tertiary treatment centers, these percentages will be higher in nonpopulation-based studies.
Analyzing data of elbow fractures is further complicated by difficulties in separating supracondylar fractures from physeal fractures of the distal humerus; by the vagaries of ossification of the multiple secondary centers of ossification of the distal humerus1,2,4; by the inclusion or exclusion of fractures of the medial epicondyle, which is an apophysis rather than an epiphysis; by imprecise definition between olecranon and physeal fractures of the proximal ulna, and by the difficulty in distinguishing radial neck fractures from those that involve the radial physis.
When physeal fractures of the elbow are considered as a separate category (excluding supracondylar fractures), 60 percent occur in the distal humerus. In one series,9 fracture of the distal humeral lateral condyle was 26%; followed by radial head, 23%; medial epicondyle, 22%; proximal ulna, 17%; T-intercondyle, 4%; medial condyle, 3%; lateral epicondyle, 3%; and separation of the entire distal humeral epiphysis (typically occurring only in infants and young children), 2%.
CLASSIFICATION
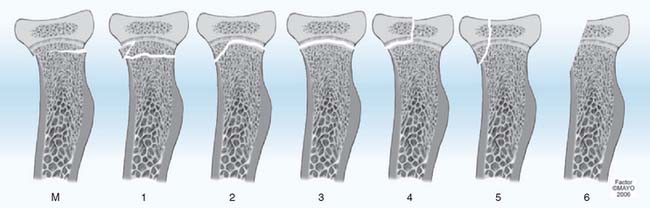
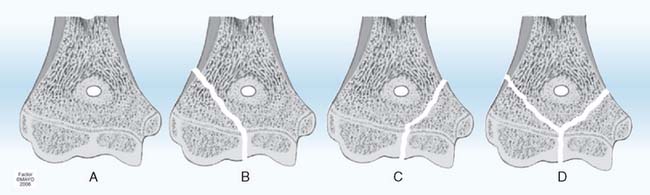
Many classifications of physeal fractures have been proposed.18,22 The classification of Salter-Harris24 has been the most frequently used over the past four decades. There have been no case reports of acute physeal compression injury (Salter-Harris type V) of the distal humerus, proximal radius, or proximal ulna recorded in the literature. Speculation suggests that acute compression injury (type V) of any physis is unlikely and may not exist.23 Supracondylar fractures of the distal humerus often have fracture lines extending distally into the physis, making them type 1 Peterson physeal fractures (Fig. 16-2).18,88 Fractures of the proximal radius metaphysis (neck) (see Fig. 16-7M), and of the olecranon (see Fig. 16-8), frequently extend proximally into the physis,18,184 also making them Peterson type 1 fractures. Therefore, the Peterson classification18,22 is used in the remainder of this chapter.
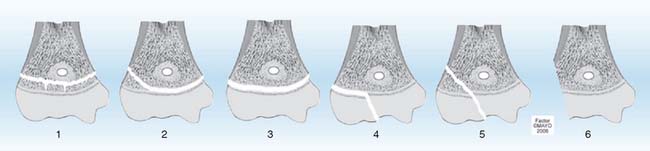
FIGURE 16-2 Peterson classification of distal humeral physeal fractures in children.
(From Peterson, H. A.: Epiphyseal Growth Plate Fractures. Heidelberg, Springer, 2007, used with permission of Mayo Foundation for Medical Education and Research.)
EVALUATION
Any recent abnormality or change in a child’s elbow, with or without a history of injury, deserves careful physical examination, including vascular and neurolo-gic evaluation.49–51 This will avoid the uncomfortable situation of finding a postreduction vascular or neurologic deficit without knowing the prereduction status.
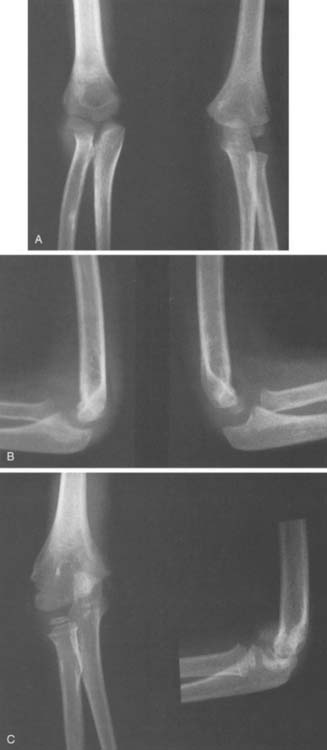
Imaging possibilities of cartilage and osseous structures are numerous. True anteroposterior and lateral roentgenographs of good quality are essential for evaluation of the injured pediatric elbow. Soft tissue as well as osseous structures must be clearly discernible. An intra-articular hematoma may displace the posterior fat pad of the distal humerus (the fat pad sign), which may be the only demonstrable change in an undisplaced or spontaneously reduced intra-articular fracture.26,47,94 Symmetric views of the contralateral elbow provide a valuable basis for comparison in assessing injury.48 This is particularly true in the pediatric elbow because of the wide variance in the ages at which the multiple ossification centers appear. Anteroposterior varus and valgus stress views,35,81,143 and oblique views of the injured or of both elbows are also helpful.48
In younger children in whom the cartilaginous proportion of the epiphysis is high, arthrography,25,26,28,36,40,42,52,143 ultrasonography,29,31,32,44,53 and magnetic resonance imaging (MRI)33,34,41,44,46,119 play important roles in defining the injury. In older children, with predominantly osseous epiphyses, tomography37 and computed tomography (CT)27,30 may be of value.
Chapters 6 and 12 of this textbook also review imaging techniques that aid in evaluating anatomy, development, and pathology of children’s elbows.
DISTAL HUMERUS
EPIDEMIOLOGY
Fractures of the distal humeral physes have two peculiarities when compared with injuries to other physes.17 The age distribution for all physeal fractures is a bell-shaped curve, with the peak at age 11 to 12 years for girls and age 14 years in boys.17,20 The distal humerus has a bimodal age distribution, with a larger peak occurring at 2 to 7 years and a second smaller peak occurring at 11 to 15 years (Table 16-2). This bimodal age distribution may be related to the preponderance of sup-racondylar (actually transcondylar) fractures, which are predominant at ages 5 to 10 years.
TABLE 16-2 Physeal Fractures of the Distal Humerus by Age and Gender in Olmsted County, Minnesota, 1979-198820
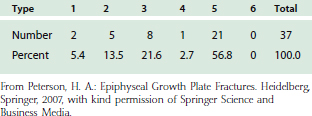
The second departure from other physes is the type of fracture. At most other sites, type 2 is the most common fracture. In the distal humerus, more than 50% of physeal fractures of the distal humerus are type 5 (Table 16-3), most likely associated with the preponderance of lateral condyle fractures (see Table 16-1).
TABLE 16-3 Physeal Fractures of the Distal Humerus by Type in Olmsted County, Minnesota, 1979-198820 (Peterson Classification)
The changing anatomy of the distal humeral physis during growth (see Fig. 16-1) predisposes it to specific fractures at different ages.19 Although any fracture type can occur at any age, from birth to age 2 years, the most common fracture is epiphyseal separation (type 3). From age 2 to age 6 years, type 3 fractures become less common and types 2, 4, and 5 become more common. By age 6 to 10 years, shear type 2 and 3 fractures are rare and type 5 fractures, particularly of the lateral condyle, predominate. During ages 10 years to maturity, type 5 fractures and avulsion fractures of the medial epicondyle are the most common. These patterns provide a basis for presenting the fractures by age.19
NEWBORN TO 2 YEARS
The epiphysis of the distal end of the humerus is one large cartilaginous mass during the first 2 years of life (see Fig. 16-1). Its interface with the metaphysis is smooth and transverse. Therefore, transverse, shear-type fractures totally within the physis are the most common fracture in the newborn,39,54,55,57,59,61,62,64,67–69,72,74–78 and in infants.36,56,60,63,66,70,73,79 These fractures tend to be reported separately and not in case series (see Table 16-1). They are typically types 2 and 3 (see Fig. 16-2).70 The entire epiphysis usually is displaced posteromedially60,61,67 but may be displaced medially,63,64,75,79 anteriorly,9,65 posteriorly, or laterally, depending on the mechanism of the injury. Rotatory malalignment may accompany displacement or occur alone. This can predispose to cubitus varus.59 Injuries of types 4 and 5 are theoretically possible, but at this age, they are more difficult to diagnose because the epiphysis is primarily cartilaginous in very young children. Injury with mild displacement may go undetected in abused children who present late for medical attention.25 Types 2 and 3 fractures frequently are misdiagnosed as elbow dislocations.56,57,60,64,66,71,75,83,85 Arthrography,25,26,28,36,40,42,52,57,63,71,83 ultrasonography,31,32,44,53,74,76 and MRI44,58,69,74,77 in these young children may aid in establishing the correct diagnosis.
Treatment of type 1, 2, and 3 fractures consists of aligning the epiphysis with the metaphysis. Precise anatomic reduction is desirable but not necessary.9 Usually, this can be obtained by closed manipulation or traction.57,64,66,69,75,85 Immobilization with the elbow in 90 degrees of flexion and forearm pronation for 3 weeks is usually adequate.60,66 Because the entire epiphyseal growth plate usually remains with the epiphysis, damage to the growth plate is uncommon, and the potential for resumption of normal growth is good. The prognosis in these cases is favorable; minor malalignment usually corrects itself with normal growth and development, and physeal growth arrest is uncommon. Percutaneous pin fixation or open reduction25,59 is rarely necessary. Only four cases have been reported in which open reduction and internal fixation were performed late because of severe malalignment or interposition of soft tissue.55,71,86
AGES 2 TO 6 YEARS
In early childhood, the growth plate gradually becomes more oblique distally and medially, from the lateral to the medial epicondyle (see Fig. 16-1). This obliquity of the epiphyseal line may account in part for the frequent lateral displacement of the epiphysis and the difficulty of maintaining accurate reduction. The ossification center of the capitellum may appear as early as 6 months and always by 2 years of age (see Fig. 16-1).1,83 This ossification center is initially oval and provides valuable orientation for alignment of the radial diaphysis. In the normal elbow roentgenograph, a line drawn through the radial diaphysis always passes through the capitellar ossification center in any projection. This aids in differentiating elbow dislocation from fracture. In a distal humeral epiphyseal separation, the capitellar ossification is aligned with the radius, regardless of degree of displacement, but is not properly positioned on the humerus. If the radius does not align with the capitellar ossification, there is radiohumeral subluxation or dislocation. Type 2 and 3 fractures are common.80 As age increases, type 2 and 3 fractures are progressively less common, presumably due to a more irregular and stable physis.
Type 4 fractures are not common at this age but are a source of frequent complication, usually nonunion. They may occur on the medial condyle, which when not ossified makes diagnosis by routine roentgenographs very difficult (Fig. 16-3). When there is significant swelling medially and normal osseous contour, supplemental imaging is necessary. Soft tissue enhancement techniques and stress views are valuable, but if they are not diagnostic, ultrasonography, arthrography, or MRI should be considered.
Type 5 fractures are common at this age, and their differentiation from type 2 fractures is difficult and important because displaced type 5 fractures frequently develop nonunion if left untreated (Fig. 16-4).71,75,78,102,107,110,112,123,130,137 Supplemental imaging, such as arthrography, ultrasonography, or MRI, should be considered. A coronal plane transcondylar fracture pattern has been described.98 All displaced type 5 fractures require anatomic reduction and maintenance of reduction. Attempts to accomplish this with immobilization in a cast frequently lead to subsequent displacement of even nondisplaced or minimally displaced fractures of the lateral condyle. This contributes to significant complications. Because so much of the distal humerus is still only cartilage, closed reduction with percutaneous pinning is also not advised. The bone and pins can be visualized roentgenographically, whereas the cartilage cannot. Open reduction and internal fixation (usually smooth wires) should be considered for any displaced fracture at this age.
An occasional complication of any distal humeral fracture at this age is the fishtail deformity.43,60,84,87 This occurs most commonly after supracondylar, medial, or lateral condylar fractures and consists of an L-shaped distal humeral articular surface. It is caused by premature arrest of the central portion of the physis, which may be due to central longitudinal malunion, avascular necrosis, or central physeal arrest without malunion or avascular necrosis. The deformity is often mild, with no functional impairment, but at this age can be marked with significant consequences.18,84
AGES 6 TO 10 YEARS
By 6 years of age, the epiphyseal growth plate begins to become irregular and obliquity increases (see Fig. 16-1). A projection of metaphyseal bone begins to separate the medial epicondyle from the trochlea, adding greater stability to the physis. Therefore, shear-type injuries, such as types 2 and 3 fractures, become less common.96
On transverse section, the physis remains irregularly oval, whereas that of the metaphysis becomes elongated in the coronal plane and thin in the sagittal plane. Thus, the strength of the physis is, at this age, greater than the strength of the metaphysis. Most injuries in this age group are, therefore, supracondylar fractures. The decreased area and elongated contour of bone contact in supracondylar fractures make possible rotation and subsequent tilting of the distal fragment (cubitus varus). Because the area of fracture contact is greater with physeal fractures, rotation, tilt, and subsequent cubitus varus are less likely than for supracondylar fractures.60
LATERAL CONDYLE
Fractures of the lateral condyle are relatively common, constituting approximately 10% to 15% of all fractures in the region of the elbow (see Table 16-1). They are the most common physeal fracture of the elbow. They occur in children between the ages of 2 and 16 years104 but are most common between 6 and 10 years of age.90,103,117,133,139,142 The mechanism of injury is usually a varus stress with the elbow in extension.122 The lateral condyle may fracture during elbow dislocation.143 Less commonly, pre-existing cubitus varus may predispose to fracture of the lateral condyle.106
Because this fracture involves both the articular surface and the physis, anatomic reduction is necessary and must be maintained until the fracture has united. If the fracture is undisplaced and stable, external immobilization by a long arm cast with the elbow in 90 degrees of flexion for 4 weeks will suffice.104,105 Frequent roentgenographic follow-up to assess maintenance of reduction is essential. If there is displacement, reduction and internal fixation will prevent redisplacement. If the fracture can be reduced or closed, pins inserted per-cutaneously may be used for fixation to prevent redisplacement.92,105 Some authors129 recommend arthrography to ensure a congruent joint surface before proceeding with percutaneous pinning. In most instances, however, open reduction and accurate replacement by direct vision is necessary. The reduction must be held by firm internal fixation, preferably metal rather than suture.89,110,113 Smooth pins, small in diameter, are the standard.101,105,115,142 Screws are preferred by some authors126,136 and biodegradable pins by others.93 Insertion of fixation devices from metaphysis to metaphysis and from epiphysis to epiphysis is preferred. However, because the trochlear cartilage is not ossified and not visible on roentgenographs, the pins may necessarily pass from epiphysis to metaphysis, crossing the physis obliquely. These pins should be removed within 3 weeks to prevent premature partial growth arrest. Pins not crossing the physis should remain in situ until there is some roentgenographic evidence of fracture healing, which occurred after approximately 6 weeks in one study.105 Fractures with early pin removal can be protected with additional long arm cast.105 Threaded pins predispose to premature partial physeal arrest and should not be used across a physis. Skeletal traction for elbow physeal fractures should be used only temporarily in children with multiple injuries.
In one series of 33 lateral condylar fractures, four untreated cases all developed nonunion, 12 treated by closed reduction and immobilization had six with “poor results,” and 17 treated by open reduction and nailing had three with poor results.14
Untreated and inadequately treated cases are frequently complicated by malunion and nonunion, and these cause deformity, loss of motion, degenerative arthrosis, and tardy ulnar neuro-pathy.10,14,90,95,99–102,110,116,126,128,131,140,144,147,156,162 There is no agreement on the management of these complications, although many authors recommend osteosynthesis, combined with corrective osteotomy for significant deformity.89,98,99,108,112,121,125,128,134,145
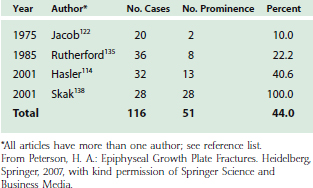
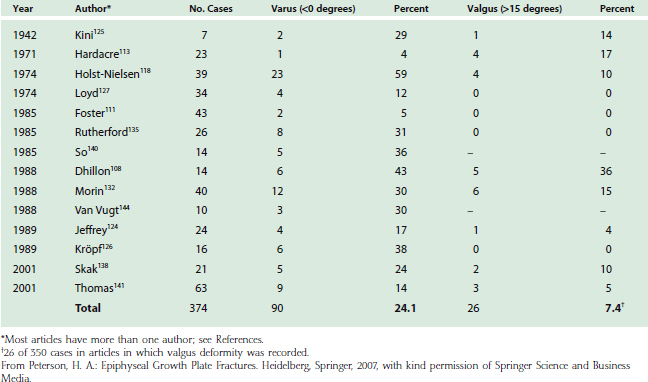
Lateral prominence of the elbow is common after lateral condyle fracture (Table 16-4). This rarely is trou blesome or requires treatment. Varus or valgus deformity is also common (Table 16-5) and may be due to malposition of the fragment or to true overgrowth of the capitellum and its physis. Overgrowth is an interesting phenomenon and occasionally occurs even fol-lowing successful management of a lateral condyle fracture.97,118,146,147 Although this may produce measurable cubitus varus, functional impairment is rare, and treatment is often for cosmetic improvement.
Premature physeal closure113,146 has been noted in up to 20% of lateral humeral fractures. The premature fusion is more often complete than partial. Complete physeal closure causes no angular deformity, and the cessation of growth results in only minor relative shortening compared with the contralateral humerus. This usually results in no functional or cosmetic impairment. Premature partial lateral closure sufficient to cause progressive cubitus valgus is uncommon. Partial closure of the center of the physis, where a fracture crossed the physis and epiphysis, leads to a disturbance of growth referred to as a fishtail deformity.10,84,101,126,142
MEDIAL CONDYLE
Fractures of the medial condyle83,84,86,87,102,108,109,148–156 are much less frequent (see Table 16-1) perhaps because of normal cubitus valgus and because of the projection of metaphyseal bone between the trochlea and medial epicondyle. They occur in children of all ages, with the peak age between 6 and 10 years in most series. Fractures of the medial condyle may result from a fall on the apex of the flexed elbow or from an avulsion valgus stress injury on an extended elbow.67,153 Marked swelling on the medial side of the elbow is usually present (see Fig. 16-3). Some occur before the trochlea is ossified. Therefore, the displaced fragment consists of a portion of bone from the medial side of the lower humeral metaphysis, along with the cartilaginous trochlea and the ossified medial epicondyle. The unossified portion of the trochlea is not seen on the roentgenograph. Thus, if the fracture occurs before ossification of the trochlea, it may be mistaken for a fracture of the medial epicondyle. If the diagnosis is not made and the injury is treated nonoperatively as an avulsion fracture of the medial epicondyle, a poor functional result can be anticipated.82,151
In addition to the factors of articular congruity and growth plate alignment, fractures of the medial condyle are important because of its proximity to the ulnar nerve. Anatomic reduction, therefore, is mandatory to avoid tardy ulnar palsy as well as nonunion or malunion. These fractures usually require open reduction and rigid internal fixation. Only if the fracture is undisplaced may this fracture be treated by cast immobilization alone.150 The complication rate is high.155
Fractures may involve both condyles, with a split through the center of the articular surface (Fig. 16-5D).161 These fractures are analogous to the adult T-intercondylar fracture, are frequently comminuted, and fortunately, are not common. They are often the result of direct force and therefore may be open fractures. This is an unstable situation that requires open reduction and internal fixation.9
AGE 10 TO MATURITY
The growth plate obliquity and irregularity continue to increase (see Fig. 16-1). The medial epicondyle and the trochlea are completely separated by a projection of metaphyseal bone. The medial epicondyle does not articulate with the ulna or contribute to the longitudinal length of the humerus. All four ossification centers are now visible roentgenographically. Trochlear ossification is frequently irregular and fragmented, simulating fracture. The trochlea, capitellum, and lateral epicondyle fuse to each other in approximately the 13th year (earlier in girls) before uniting with the humerus.1 Transverse shear-type type 2 and 3 physeal fractures are now virtually impossible (only one case has been illustrated in the literature18), except for the medial epicondyle. This conjoined epiphysis later fuses with the shaft, usually by the 16th year. Once fused, growth ceases and growth alteration following fracture is no longer possible.
Injuries involving the conjoined epiphysis at this age are nearly always type 5. Lateral and medial condylar fractures both occur in this age group120 (see Fig. 16-5B and C). Medial condylar fractures129,163 are more common than they are at younger ages but are still less common than lateral condylar fractures. Both require open anatomic reduction and internal fixation. The T- or Y-type fracture (see Fig. 16-5D)131,159 is more frequent than at younger ages and usually requires open reduction and internal fixation. A minimally displaced fracture may be treated by reduction and percutaneous screw fixation.157 A posterior surgical approach gives excellent visualization and an opportunity for reduction and fixation of the multiple fragments.158
The triplane fracture is a type 5 fracture variation, usually found in the distal tibia. It has been reported in the distal humerus,160 and, because it involves both articular and physeal cartilage, it should be treated by anatomic reduction and maintenance of reduction.
MEDIAL EPICONDYLE
The medial epicondylar apophysis is extra-articular and is usually roentgenographically present (ossified) by age 5 years (see Fig. 16-1). Multicentric ossification centers have been demonstrated and give a fragmented appearance. Awareness of this normal variant may obviate misdiagnosis. The medial epicondyle matures slowly and is the last of the six epiphyses of the elbow to unite with its adjacent metaphysis; as late as the 19th year in men.4
The medial epicondyle is located slightly posteriorly, rather than strictly medially, which may cause confusion in roentgenographic interpretation.4 Oblique roentgenographs of both elbows are sometimes necessary to determine whether the epicondyle on the injured side is in an abnormal position.
Fractures of the medial epicondyle constitute nearly 10% of all fractures of the elbow region (see Table 16-1),47 and usually occur between 9 and 15 years of age.6,165,166,173 The injury is unusual in younger children. The mechanism of injury is usually a valgus stress of the joint, which produces traction on the medial epicondyle through the flexor muscles. Arm wrestling is not a common activity among children but may result in this fracture.172,173 The fracture is usually type 3, although types 2, 4, and 5 have been noted.6,9 The epicondyle is always displaced distally because of the pull of the flexor muscle mass origin. It may be dislocated into and entrapped in the elbow joint, associated with opening of the joint by valgus stress. The entrapped epicondyle must be extracted from the joint and reduced. This is best done by open surgery, because manipulative maneuvers are unlikely to remove it from the joint, reduce it, and render it stable. About half of the cases are associated with partial or complete dislocation of the elbow,164,169,170,175 usually posterolateral dislocation.
Nowhere in the discussion of physeal injuries of the elbow is there a greater divergence of opinion concerning treatment than in medial epicondylar fractures. Recommendations range from performing open reduction in virtually all cases, to no surgical treatment for any case (other than for intra-articular epicondyle entrapment). The fear of painful pseudarthrosis following nonoperative treatment has been cited for using open reduction and internal fixation in nearly every case, even with minimal (1-mm) separation.9 Conversely, cases treated nonoperatively are reported to do relatively well for many years, despite a high rate of nonunion.168,171
Any hypesthesia, paresthesia, or paralysis in the ulnar nerve distribution is an adequate reason for exploration, inspection of the nerve, and replacement of the fragment. If the ulnar nerve is found to be constricted or contused, it may be transposed anterior to the medial condyle.85,91 This is rarely necessary.153,167
In North America, 2 mm of displacement seems to be a commonly used criterion to determine treatment of physeal fractures in general. If the medial epicondyle is displaced 2 mm or less, the elbow may be immobilized for 3 weeks in a long arm cast, with the elbow in moderate flexion and the forearm in pronation. Oblique roentgenographs or comparison roentgenographs of the normal opposite elbow may be helpful in determining the degree of displacement. If the medial epicondyle is displaced more than 2 mm or rotated, or if the elbow joint is unstable on application of valgus stress, open reduction and internal fixation are indicated. The gravity stress test is a useful diagnostic test for acute medial instability.179 Displaced fractures of the medial epicondyle, if left untreated, frequently progress to malunion or nonunion (Fig. 16-6). Tardy ulnar palsy is a common late problem despite relatively good elbow motion and freedom from symptoms for several years.171
The medial epicondyle can sometimes be reduced by closed means but cannot be held reduced. Percutaneous pinning is hazardous because of the proximity of the ulnar nerve. Therefore, open reduction and internal fixation with two smooth Kirschner wires, one screw, or absorbable rods and screws, is frequently performed.168,174,178 It is usually not necessary to mobilize the ulnar nerve, although if the epicondyle is markedly displaced, this maneuver may be helpful in gaining exposure. Kirschner wires should be removed after 3 weeks and active motion begun. Potential complications after pinning, however, include pseudarthrosis, an ulnar sulcus, a double-contoured epicondyle, hypoplasia, or hyperplasia.176
The physis of the epicondyle often closes after fracture, but because it does not contribute to longitudinal length4 and because the epiphysis does not articulate with the ulna, problems due to growth arrest are rare or nonexistent. This is particularly true because most of these children are near maturity and the other physes about the elbow have already closed.
Because of the proximity of the ulnar collateral ligament, elbow stability should be examined after fracture healing. Severe chronic medial instability, and even recurrent elbow dislocation, although rare, may occur after fibrous union of a displaced fracture.177,179 Treatment options include osteosynthesis of the fragment to the condyle or excision of the fragment.
LATERAL EPICONDYLE
The ossification center of the lateral epicondyle appears at about age 10 years (see Figs. 16-1 and 16-8A) and fuses with the lateral condyle at 14 years of age.2 Its ossification characteristics are prone to misinterpretation as an avulsion or chip fracture of the lateral metaphysis because (1) it ossifies as a smooth, thin, curved sliver of bone; (2) it is well separated from the humerus; and (3) the distal part usually fuses with the capitellum before the proximal part unites with the adjacent humeral shaft. As the epiphysis matures, its outline usually becomes smooth and well defined, but it may be irregular.2
Fracture of the lateral epicondyle is uncommon (see Table 16-1), and is usually associated with other elbow injuries. Separation fracture may accompany elbow dislocation.180 Isolated fracture of the lateral epicondyle is rare.9,65 In most cases, there is relatively little displacement of the fragment. Immobilization of the elbow for 3 to 4 weeks usually is sufficient. Open reduction and internal fixation are usually unnecessary because these injuries tend to occur only in children approaching the age of skeletal maturity. The risk of associated growth arrest is minimal or nonexistent. Tardy ulnar nerve palsy has been reported.91
PROXIMAL RADIUS
The epiphysis of the radial head begins to ossify at about the age of 5 years. Although it may appear first as a sphere, ossification soon advances into one or two ovoid, flat, or wedge-shaped nuclei, which may be eccentrically located on the radial metaphysis45 and misinterpreted as an avulsion fracture of the epiphysis. Notches and clefts in the proximal radial metaphysis may closely resemble post-traumatic appearances.3
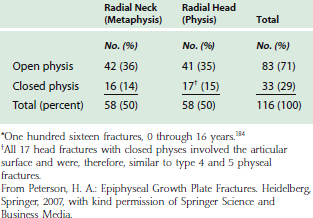
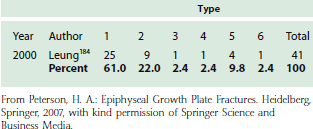
By definition, radial head fractures in children (age 0 through 16 years) are those that include the physis (Fig. 16-7). If these fractures appear in older children in whom physis is closed, they include the articular surface.18,184 Radial neck fractures are metaphyseal, entirely distal to the physis. Physeal fractures 1, 2, 5, and 6 also involve the metaphysis, but because the major problem is physeal or articular cartilage involvement, they all qualify as fractures of the head. Of all pediatric elbow fractures, 10% to 15% involve the radial head and neck (see Table 16-1).18,191 Of these head and neck fractures, approximately 50% involve the head and 50% the neck (Table 16-6).18 Proximal radial physeal fractures account for only 0.6% of all physeal fractures.18,20
The normal valgus carrying angle of the elbow causes compression laterally during a fall on the outstretched arm. This drives the capitellum against the outer side of the head of the radius, tilting it and displacing it outward. The fracture may be, therefore, type 1, 2, 3, 4, or 5 (see Fig. 16-7), with type 1 being most common (Table 16-7). A second mechanism of injury is associated with posterior dislocation of the elbow with simultaneous compression of the capitellum on the anterior portion of the head of the radius.187 This has the potential to produce the more serious type 4 and 5 fractures.
The joint capsule is attached to the radius in continuity with the annular ligament. Because the radial neck lies outside the joint capsule, fracture of the neck may not cause joint effusion or fat pad displacement. Fracture of the radial head, however, usually produces elbow effusion and a positive fat pad sign.3
Differentiating fractures that involve only the neck of the radius (metaphysis) from those that also involve the physis (head) can be difficult. Oblique roentgenographs and occasionally MRI can be helpful in making this differentiation.
The type 1 fracture is common (see Table 16-7), but may be difficult to diagnose. It is usually incorrectly called a neck fracture or type 2 fracture (Fig. 16-8). It is distinguished by a transmetaphyseal fracture with fracture extension to the physis. The transmetaphyseal fracture is often only a compression fracture that may not be visible on the initial roentgenographs. Transmetaphyseal sclerosis, however, is always present 3 to 6 weeks after fracture and verifies the compression component. The fracture line extending to the physis is also frequently difficult to visualize on routine anteroposterior and lateral views and is often best seen on oblique views. This may be only a fracture line, but often there is a displaced corner of metaphysis that may be called a “chip” fracture. Most importantly, however, is that there is no fracture transversely within the physis and the epiphysis is not displaced. Therefore, this is not a type 2 fracture. These fractures need only temporary external immobilization and invariably heal without sequelae.
If a type 2 or 3 fracture is minimally displaced or can be manually reduced, immobilization for 3 to 4 weeks will suffice.183 A wire or a hook inserted percutaneously can be used to manipulate a mildly or moderately displaced head into position.9,181 Occasionally, with a type 3 fracture, the entire epiphysis will be inverted or even displaced through the joint capsule, and closed reduction is not possible. In this instance, open reduction is necessary. After surgical reduction, the fracture is often stable, and no internal fixation is necessary.9,189 Immobilization, with the elbow in 90 degrees of flexion and the forearm in neutral rotation, is satisfactory.
If the surgical reduction is unstable, internal fixation with two crossed Kirschner wires188 or with one longitudinal wire through the capitellum ossification center extending across the radiocapitellar joint into the intramedullary cavity of the radial diaphysis can be considered.9,186,189 Each method of internal fixation should be supplemented with a long arm cast. The wires may be removed in 3 weeks and gentle protected motion using a collar and cuff begun. If a single longitudinal wire is used, it should be stout enough to avoid wire breakage at the joint level.9 If this occurs, removal of the portion of wire embedded in the radius can be difficult, and it may be less damaging to leave the wire permanently in the radius.
Type 4 and 5 injuries require precise anatomic reduction to restore articular congruity. Open reduction and internal fixation with tiny transverse or oblique Kirschner wires will help prevent displacement of the fragments during healing. Premature closure of the physis nearly always occurs,184,187,190 but because the proximal radius accounts for only 20% of the growth of the radius and because type 4 and 5 injuries often occur in older children, problems from growth arrest are rare.182 Functional impairment, however, particularly limited forearm rotation, is common after type 4 and 5 injuries.184 The presence of associated fractures in the humerus and ulna reduces the chance of a favorable outcome.185
Type 6 fracture (a part missing) (see Fig. 16-7) is always an open injury and usually results in functional impairment.18,21 Regardless of how little physis is lost, the remaining physis always stops growing. Late reconstructive surgery is usually necessary.
Most radial head physeal fractures result in premature complete physeal closure and eccentric enlargement of the radial head.185 Abnormal cam motion may occur during forearm rotation, and this may be painful. Excision of the radial head in a growing child will result in distal radial-ulnar length variance and should be avoided. After the patient reaches maturity and has joint pain or limited motion, the radial head may be excised with little risk of development of wrist deformity.85 However, excision of the head rarely restores motion. Thus, the primary indication for excision of the radial head is pain.
PROXIMAL ULNA
The proximal ulnar growth apparatus has features of both an epiphysis and an apophysis.195 Because the proximal ulnar physis produces longitudinal growth and has articular involvement, it is included as an epiphysis.
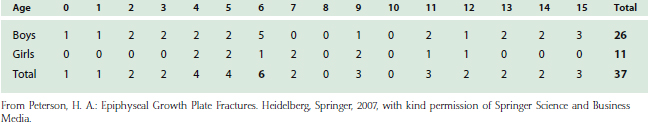
The olecranon is the cartilage/bone projection of the proximal ulna. Its anterior aspect forms the articular surface with the humeral trochlea. As such, the olecranon includes the epiphysis, physis, and most of the metaphysis. Early in life, the physis is L-shaped, extending from the transverse metaphyseal-epiphyseal interface anteriorly and distally as part of the thick subchondral articular surface, to beneath the coracoid process (Fig. 16-9A). With growth, the epiphysis becomes a relatively smaller portion of the olecranon (see Fig. 16-9B, and C). In this sense, the physis “migrates” proximally, and has been called the “wandering physeal line.” The extent of this proximal migration varies among children.47 In the majority of children, the physis continues to migrate proximally and obliquely until it is completely extra-articular (see Fig. 16-9C). This usually occurs by age 12 years. In the minority, the physis remains relatively transverse and closes while its anterior edge is still intra-articular (see Fig. 16-9D).
The secondary center of ossification first appears at age 9 years in girls and 11 years in boys.47 The epiphysis initially often has two, sometimes three, and occasionally several ossification centers.5 The physis is usually closed by the end of the 16th year.195
Fractures of the proximal ulna account for 5% to 10% of children’s elbow fractures (see Table 16-1), and are often accompanied by other elbow fractures. Most fractures of the olecranon primarily involve metaphyseal bone distal to the physis (Fig. 16-10M).85 Fractures of the proximal ulnar physis account for only 0.3% of all physeal fractures.18,20 When the physis is involved, the fracture is usually a type 2 injury (see Fig. 16-10, 2a and 2b), occasionally a type 3 injury (see Fig. 16-10, 3). In type 2 injuries, the fracture line in the metaphysis may be oblique (as shown) or may enter the ulnar shaft more longitudinally. Because the proximal fragment contains articular surface, these fractures require anatomic reduction and maintenance of reduction until the fracture has united. Frequently, this can be accomplished by closed means, immobilizing the elbow in extension. However, if displacement is more than 3 mm, open reduction and internal fixation are advised.193 Fixation may be accomplished by longitudinal Kirschner wire or a wire loop, or in older children, a tension band wire. A longitudinal screw should not be used in a young child if significant growth remains.9 However, growth arrest problems are rare.196,199 Excision of the fragment, which is sometimes performed in adults, should be avoided, particularly in young children. In older children, who subject their upper extremities to excessive stress, delayed physeal closure can simulate a nonunion,197,198 sometimes called a stress or chronic type 3 fracture. Fracture of the coronoid apophysis is rare.192
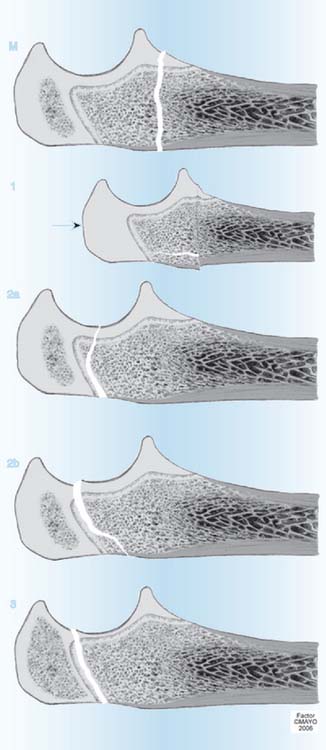
FIGURE 16-10 Peterson classification of proximal ulnar physeal fractures in children.22 M, Fracture of the metaphysis. 1, Type 1 fracture with greenstick or longitudinal split fracture. There is a torus or transmetaphyseal fracture with extension of the fracture proximally to the physis. The arrow suggests compression force originates proximally from the epiphyseal side. However, this has not been proven and distally applied pressure could result in compression if the elbow is in full extension at the moment of impact. This fracture has been noted to occur only before ossification of the epiphysis. 2a, Type 2 fracture with anterior metaphyseal fragment. 2b, Type 2 fracture with posterior metaphyseal fragment. 3, Type 3 fracture.38
(From Peterson, H. A.: Epiphyseal Growth Plate Fractures. Heidelberg, Springer, 2007, used with permission of Mayo Foundation for Medical Education and Research.)
Children with osteogenesis imperfecta are apparently prone to proximal ulnar type 2 anterior fracture-avulsions (see Fig. 16-10, 2a). Internal fixation is commonly used, and although fracture union is the rule, refracture can occur.194,199
GROWTH ARREST
Because each of the three elbow physes contribute only 10% of the entire upper extremity length, complete closure of any or all of these physes rarely, if ever, causes significant arm length discrepancy. Any resulting discrepancy is mild and causes no functional impairment and few, if any, cosmetic or clothes-fitting complaints. Even if complete closure of all physes about the elbow occurred in a young child, surgical lengthening of the involved humerus or forearm bones or surgical arrest of the contralateral elbow physes would rarely, if ever, be indicated.
Premature partial closure of the distal humerus, or proximal radius or ulna, is very rare. Premature partial closure of the medial or lateral humeral condyle theoretically may result in progressive cubitus varus or valgus, respectively. This could be determined only after many months of follow-up. In this rare occurrence, surgical closure of the remaining physis might be considered. Of 178 bar excisions for premature partial closure performed at Mayo Clinic between 1968 and 1997, none involved the elbow.18 Supracondylar osteotomy to correct angular growth is rarely necessary.
Premature closure of the central physis between the medial and lateral humeral condyles occurs occasionally and has been called a fishtail deformity.18,84 The underlying cause of the arrest is multifactorial and may be due to a gap in reduction of an intracondylar fracture, avascular necrosis of the central or trochlear portion of the epiphysis, or central premature physeal arrest (bar formation) without a gap or avascular necrosis. This usually occurs in younger children and causes no pain and only minimal loss of motion. With growth, the deformity can, however, gradually progress to premature degenerative arthrosis and functional disability. The intercondylar notch may also predispose to subsequent intercondylar fracture. Thus, if the fishtail deformity is identified in a young child, surgical closure of the medial and lateral portions of the physis may prevent the deformity from progressing and result in only minimal additional humeral length discrepancy.
1 Silberstein M.J., Brodeur A.E., Graviss E.R. Some vagaries of the capitellum. J. Bone Joint Surg. 1979;61A:244.
2 Silberstein M.J., Brodeur A.E., Graviss E.R. Some vagaries of the lateral epicondyle. J. Bone Joint Surg. 1982;64A:444.
3 Silberstein M.J., Brodeur A.E., Graviss E.R. Some vagaries of the radial head and neck. J. Bone Joint Surg. 1982;64A:1153.
4 Silberstein M.J., Brodeur A.E., Graviss E.R., Luisiri A. Some vagaries of the medial epicondyle. J. Bone Joint Surg. 1981;63A:524.
5 Silberstein M.J., Brodeur A.E., Graviss E.R., Luisiri A. Some vagaries of the olecranon. J. Bone Joint Surg. 1981;63A:722.
6 Cox F.J., Hurley M.T., Compton R.B. Fractures about the elbow in children. Calif. Med. 1952;76:13.
7 Fahey J.J. Fractures of the elbow in children. Instr. Course Lect. 1960;17:13.
8 Hanlon C.R., Estes W.L.Jr. Fractures in children: A statistical analysis. Am. J. Surg. 1954;87:312.
9 Havranek P., Hàjkova H. Treatment of children’s epiphyseal injuries in the elbow region. Acta Univ. Carol. 1985;31:243.
10 Kreusch-Brinker R., Noack W. Injuries of the distal epiphysis of the humerus in the period of growth [German]. Unfallchirurgie. 1986;12:60.
11 Landin L.A., Danielsson L.G. Elbow fractures in children: An epidemiologic analysis of 589 cases. Acta Orthop. Scand. 1986;57:309.
12 Mann D.C., Rajmaira S. Distribution of physeal and nonphyseal fractures in 2650 long-bone fractures in children aged 0-16 years. J. Pediatr. Orthop. 1990;10:713.
13 Maylahn D.J., Fahey J.J. Fractures of the elbow in children. Review of three hundred consecutive cases. J. Am. Med. Assoc. 1958;166:220.
14 McDonnell D.P., Wilson J.C. Fractures of the lower end of the humerus in children. J. Bone Joint Surg. 1948;30A:347.
15 Mizuta T., Benson W.M., Foster B.K., Paterson D.C., Morris L.L. Statistical analysis of the incidence of physeal injuries. J. Pediatr. Orthop. 1987;7:518.
16 Ogden J.A. Injury to the growth mechanisms of the immature skeleton. Skeletal Radiol. 1981;6:237.
17 Peterson C.A., Peterson H.A. Analysis of the incidence of injuries to the epiphyseal growth plate. J. Trauma. 1972;12:275.
18 Peterson H.A. Epiphyseal Growth Plate Fractures. Heidelberg: Springer, 2007.
19 Peterson H.A. Physeal injuries of the distal humerus. Orthopedics. 1992;15:799.
20 Peterson H.A., Madhok R., Benson J.T., Ilstrup D.M., Melton L.J.III. Physeal fractures: Part I. Epidemiology in Olmsted County, Minnesota, 1979-1988. J. Pediatr. Orthop. 1994;14:423.
21 Peterson H.A. Physeal fractures: Part 2. Two previously unclassified types. J. Pediatr. Orthop. 1994;14:431.
22 Peterson H.A. Physeal fractures: Part 3. Classification. J. Pediatr. Orthop. 1994;14:439.
23 Peterson H.A., Burkhart S.S. Compression injury of the epiphyseal growth plate: Fact or fiction? J. Pediatr. Orthop. 1981;1:377.
24 Salter R.B., Harris W.R. Injuries involving the epiphyseal plate. J. Bone Joint Surg. 1963;45A:587.
25 Akbarnia B.A., Silberstein M.J., Rende R.J., Graviss E.R., Luisiri A. Arthrography in the diagnosis of fractures of the distal end of the humerus in infants. J. Bone Joint Surg. 1986;68A:599.
26 Blane C.E., Kling T.F.Jr., Andrews J.C., DiPietro M.A., Hensinger R.N. Arthrography in the post-traumatic elbow in children. Am. J. Roentgenol. 1984;143:17.
27 Blickman J.G., Dunolp R.W., Sanzone C.F. Is CT useful in the traumatized pediatric elbow? Pediatr. Radiol. 1990;20:184.
28 Brodeur A.E., Silberstein M.J., Graviss E.R. Radiology of the Pediatric Elbow. Boston: G K Hall Medical, 1981;234.
29 Brown J., Eustace S. Neonatal transphyseal supracondylar fracture detected by ultrasound. Pediatr. Emerg. Care. 1997;13:410.
30 Chapman V., Grottkau B., Albright M., Elaini A., Halpern E., Jaramillo D. MDCT of the elbow in pediatric patients with posttraumatic elbow effusions. Am. J. Roentgenol. 2006;187:812.
31 Davidson R.S., Markowitz R.I., Dormans J., Drummond D. Ultrasonographic evaluation of the elbow in infants and young children after suspected trauma. J. Bone Joint Surg. 1994;76A:1804.
32 Dias J.J., Lamont A.C., Jones J.M. Ultrasonic diagnosis of neonatal separation of the distal humeral epiphysis. J. Bone Joint Surg. 1988;70B:825.
33 Ecklund K. Magnetic resonance imaging of pediatric musculoskeletal trauma. Top. Magn. Reson. Imaging. 2002;13:203.
34 Griffith J.F., Roebuck D.J., Cheng J.C.Y., Chan Y.L., Raner T.N., Ng B.K.W., Metreweli C. Acute elbow trauma in children: spectrum of injury revealed by MR imaging not apparent on radiographs. Am. J. Roentgenol. 2001;176:53.
35 Grogan D.P., Ogden J.A. Pediatric elbow fracture need not be your nemesis. J. Musculoskeletal Med. 1986;May:64.
36 Hansen P.E., Barnes D.A., Tullos H.S. Arthrographic diagnosis of an injury pattern in the distal humerus of an infant. J. Pediatr. Orthop. 1982;2:569.
37 Hoeffel J.C., Blanquart D., Galloy M.A., Dinia W., Mainard L., Gerber R., Bretagne M.C. Fractures of the lateral condyle of the elbow in children. Radiological aspects [French]. J. Radiol. 1990;71:407.
38 Holland C.T. A radiographic note of injuries to the distal epiphyses of the radius and ulna. Proc. R. Soc. Med. 1929;22:695.
39 Houben J.J., van Elegem P., Godart S., Blaimont P. Slipped epiphysis of the elbow in the young child. Diagnostic aspects. Acta Orthop. Belg. 1983;49:592.
40 Hudson T.M. Elbow arthrography. Radiol. Clin. North Am. 1981;19:227.
41 Kamegaya M., Shinohara Y., Kurokawa M., Ogata S. Assessment of stability in children’s minimally displaced lateral humeral condyle fracture by magnetic resonance imaging. J. Pediatr. Orthop. 1999;19:570.
42 Marzo J.M., d’Amato C., Strong M., Gillespie R. Usefulness and accuracy of arthrography in management of lateral humeral condyle fractures in children. J. Pediatr. Orthop. 1990;10:317.
43 McCarthy S.M., Ogden J.A. Radiology of postnatal skeletal development. VI. Elbow joint, proximal radius, and ulna. Skeletal Radiol. 1982;7:239.
44 Nimkin K., Kleinman P.K., Teeger S., Spevak M.R. Distal humeral physeal injuries in child abuse: MR imaging and ultrasonography findings. Pediatr. Radiol. 1995;25:562.
45 Nussbaum A.J. The off-profile proximal radial epiphysis: Another potential pitfall in the diagnosis of elbow trauma. J. Trauma. 1983;23:40.
46 Pudas T., Hurme T., Mattila K., Svedstrom E. Magnetic resonance imaging in pediatric elbow fractures. Acta Radiol. 2005;46:636.
47 Resnik C.S. Diagnostic imaging of pediatric skeletal trauma. Radiol. Clin. North Am. 1989;27:1013.
48 Rogers L.F. Fractures and dislocations of the elbow. Semin. Roentgenol. 1978;13:97.
49 Skaggs D., Pershad J. Pediatric elbow trauma. Pediatr. Emerg. Care. 1997;13:425.
50 Skaggs D. Elbow fractures in children: diagnosis and treatment. J. Am. Acad. Orthop. Surg. 1997;5:303.
51 Sponseller P.D. Problem elbow fractures in children. Hand Clin. 1994;10:495.
52 Yates C., Sullivan J.A. Arthrographic diagnosis of elbow injuries in children. J. Pediatr. Orthop. 1987;7:54.
53 Ziv N., Litwin A., Katz K., Merlob P., Grunebaum M. Definitive diagnosis of fracture—separation of the distal humeral epiphysis in neonates by ultrasonography. Pediatr. Radiol. 1996;26:493.
54 Barrett W.P., Almquist E.A., Staheli L.T. Fracture separation of the distal humeral physis in the newborn. Case report. J. Pediatr. Orthop. 1984;4:617.
55 Berman J.M., Weiner D.S. Neonatal fracture-separation of the distal humeral chondroepiphysis: a case report. Orthopedics. 1980;3:875.
56 Blanquart D., Hoeffel J.C., Galloy M.A., Mainard L., Bretagne M.C. Separation of the distal humeral epiphysis in young children. Radiologic features. Ann. Pediatr. (Paris). 1990;37:470.
57 Chand K. Epiphyseal separation of distal humeral epiphysis in an infant. A case report and review of the literature. J. Trauma. 1974;14:521.
58 Costa M., Owen-Johnstone S., Tucker J.K., Marshall T. The value of MRI in the assessment of an elbow injury in a neonate. J. Bone Joint Surg. 2001;83B:544.
59 deJager L.T., Hoffman E.B. Fracture-separation of the distal humeral epiphysis. J. Bone Joint Surg. 1991;73B:143.
60 DeLee J.C., Wilkins K.E., Rogers L.F., Rockwood C.A. Fracture-separation of the distal humeral epiphysis. J. Bone Joint Surg. 1980;62A:46.
61 Downs D.M., Wirth C.R. Fracture of the distal humeral chondroepiphysis in the neonate: a case report. Clin. Orthop. 1982;169:155.
62 Haliburton R.A., Barber J.R., Fraser R.L. Pseudodislocation: an unusual birth injury. Can. J. Surg. 1967;10:455.
63 Holda M.E., Manoli A.II, LaMont R.L. Epiphyseal separation of the distal end of the humerus with medial displacement. J. Bone Joint Surg. 1980;62A:52.
64 Kaplan S.S., Reckling F.W. Fracture separation of the lower humeral epiphysis with medial displacement: Review of the literature and report of a case. J. Bone Joint Surg. 1971;53A:1105.
65 Keon-Cohen B.T. Fractures of the elbow. J. Bone Joint Surg. 1966;48A:1623.
66 Marmor L., Bechtol C.O. Fracture separation of the lower humeral epiphysis. Report of a case. J. Bone Joint Surg. 1960;24A:333.
67 McIntyre W.M., Wiley J.J., Charette R.J. Fracture-separation of the distal humeral epiphysis. Clin. Orthop. 1984;188:98.
68 Milton L.P., Port R.B. Separation of the distal humeral epiphysis in a neonate. Am. J. Dis. Child. 1985;139:1203.
69 Moucha C.S., Mason D.E. Distal humeral separation. Am. J. Orthop. 2003;32:497.
70 Oh C., Park B., Ihn J., Kyung H. Fracture-separation of the distal humeral epiphysis in children younger than three years old. J. Pediatr. Orthop. 2000;20:173.
71 Omer G.E.Jr, Simmons J.W. Fractures of the distal humeral growth plate. South. Med. J. 1968;61:651.
72 Paige M.L., Port R.B. Separation of the distal humeral epiphysis in the neonate. Am. J. Dis. Child. 1985;139:1203.
73 Perio A., Mut T., Aracil J., Martos F. Fracture-separation of the lower humeral epiphysis in young children. Acta Orthop. Scand. 1981;52:295.
74 Raupp P., Haas D., Lovasz G. Epiphyseal separation of the distal humerus. J. Perinat. Med. 2002;30:528.
75 Rogers L.F., Rockwood C.A. Separation of the entire distal humeral epiphysis. Radiology. 1973;106:393.
76 Rose R.E.C., Dixon R., Bullock R. Chondro-epiphyseal separation of the distal humerus in the newborn: a case report and review of the literature. West. Indian Med. J. 2002;51:268.
77 Sawant M.R., Narayanan S., O’Neill K., Hudson I. Distal humeral epiphysis fracture separation in neonates-diagnosis using MRI scan. Case report. Injury. 2002;33:179.
78 Siffert R.S. Displacement of the distal humeral epiphysis in the newborn infant. J. Bone Joint Surg. 1963;45A:165.
79 Yngve D.A. Distal humeral epiphyseal separation. Orthopedics. 1985;8:100.
80 Abe M., Ishizu T., Nagaoka T., Onomura T. Epiphyseal separation of the distal humeral epiphysis: a follow-up note. J. Pediatr. Orthop. 1995;15:426.
81 Beghin J.A., Bucholz R.W., Wenger D.R. Intracondylar fractures of the humerus in young children. A report of two cases. J. Bone Joint Surg. 1982;64A:1083.
82 Cothay D.M. Injury of the lower medial epiphysis of the humerus before development of the ossification centre. Report of a case. J. Bone Joint Surg. 1967;49B:766.
83 Mizuno K., Hirohata K., Kashiwagi D. Fracture-separation of the distal humeral epiphysis in young children. J. Bone Joint Surg. 1979;61A:570.
84 Nwakama A.C., Peterson H.A., Shaughnessy W.J. Fishtail deformity following fracture of the distal humerus in children: case presentations, discussion of etiology, and thoughts on treatment. J. Pediatr. Orthop. 2000;9B:309.
85 Smith F.M. Children’s elbow injuries: fractures and dislocations. Clin. Orthop. 1967;50:7.
86 Sutherland D.H., Wrobel L. Displacement of the entire humeral epiphysis. Proceedings of the Western Orthopedic Association (Abstr). J. Bone Joint Surg. 1974;56A:206.
87 Yoo C.I., Suh K.T., Kim Y.J., Kim H.T., Kim Y.H. Avascular necrosis after fracture separation of the distal end of the humerus in children. Orthopedics. 1992;15:959.
88 Abraham E., Gordon A., Abdul-Hadi O. Management of supracondylar fractures of the humerus with condylar involvement in children. J. Pediatr. Orthop. 2005;25:709.
89 Gaur S.C., Vishwakarma D.P., Varma B. An unusual injury of the lower humeral epiphysis in a child: a case report. Injury. 1985;16:625.
90 Gogola G.R. Pediatric humeral condyle fractures. Hand Clin. 2006;22:77.
91 Holmes J.C., Hall J.E. Tardy ulnar nerve palsy in children. Clin. Orthop. 1978;135:128.
92 Jones K.G. Percutaneous pin fixation of fractures of the lower end of the humerus. Clin. Orthop. 1967;50:53.
93 Mäkelä E.A., Böstman O., Kekomäki M., Södergaard J., Vainio J., Törmälä P., Rokkanen P. Biodegradable fixation of distal humeral physeal fractures. Clin. Orthop. 1992;283:237.
94 Micheli L.J., Santori R., Stanitski C.L. Epiphyseal fractures of the elbow in children. Am. Fam. Physician. 1980;22:107.
95 Morrissy R.T., Wilkins K.E. Deformity following distal humeral fracture in childhood. J. Bone Joint Surg. 1984;66A:557.
96 Sen R.K., Bedi G.S., Naji O.N. Fracture epiphyseal separation of the distal humerus. Australasian Radiol. 1998;42:271.
97 Storm S.W., Williams D.P., Khoury J., Lubahn J.D. Elbow deformities after fracture. Hand Clin. 2006;22:121.
98 Stricker S.J., Thomson J.D., Kelly R.A. Coronal-plane transcondylar fracture of the humerus in a child. Clin. Orthop. 1993;294:308.
99 von Laer L., Brunner R., Lampert C. Malunited supracondylar and condylar humeral fractures [German]. Orthopade. 1991;20:331.
100 Wilkins K.E. Residuals of elbow trauma in children. Clin. Orthop. 1990;21:291.
101 Amgwerd M., Sacher P. Treatment of fractures of the radial condyle of the humerus in children [German]. Z. Unfall. Versicherungsmed. 1990;83:49.
102 Attarian D.E. Lateral condyle fractures: Missed diagnoses in pediatric elbow injuries. Mil. Med. 1990;155:433.
103 Badelon O., Bensahel H., Mazda K. Lateral humeral condylar fractures in children: a report of 47 cases. J. Pediatr. Orthop. 1988;8:31.
104 Bast S.C., Hoffer M.M., Aval S. Nonoperative treatment for minimally and nondisplaced lateral humeral condyle fractures in children. J. Pediatr. Orthop. 1998;18:448.
105 Cardona J.I., Riddle E., Kumar S.J. Displaced fractures of the lateral humeral condyle: criteria for implant removal. J. Pediatr. Orthop. 2002;22:194.
106 Davids J.R., Maguire M.F., Mubarek S.J., Wenger D.R. Lateral condylar fracture of the humerus following posttraumatic cubitus varus. J. Pediatr. Orthop. 1994;14:466.
107 DeBoeck H. Surgery for nonunion of the lateral humeral condyle in children. Six cases followed for 1-9 years. Acta Orthop. Scand. 1995;66:401.
108 Dhillon K.S., Sengupta S., Singh B.J. Delayed management of the lateral humeral condyle in children. Acta Orthop. Scand. 1988;59:419.
109 Finnbogason T., Karlsson G., Lindberg L., Mortensson W. Nondisplaced and minimally displaced fractures of the lateral humeral condyle in children: a prospective radiographic investigation of fracture stability. J. Pediatr. Orthop. 1995;15:422.
110 Flynn J.C., Richards J.F. Nonunion of minimally displaced fractures of the lateral condyle of the humerus in children. J. Bone Joint Surg. 1971;53A:1096.
111 Foster D.E., Sullivan J.A., Gross R.H. Lateral humeral condylar fractures in children. J. Pediatr. Orthop. 1985;5:16.
112 Gaur S., Varma A.N., Swarup A. A new surgical technique for old ununited lateral condyle fractures of the humerus in children. J. Trauma. 1993;34:68.
113 Hardacre J.A., Nahigian S.H., Froimson A.I., Brown J.E. Fractures of the lateral condyle of the humerus in children. J. Bone Joint Surg. 1971;53A:1083.
114 Hasler C.C., von Laer L. Prevention of growth disturbances after fractures of the lateral humeral condyle in children. J. Pediatr. Orthop. 2001;10:123.
115 Hennrikus W.L., Millis M.B. The dinner fork technique for treating displaced lateral condylar fractures of the humerus in children. Orthop. Rev. 1993;22:1278.
116 Heyl J.H. Fracture of the external condyle of the humerus in children. Ann. Surg. 1935;101:1069.
117 Holmberg L. Fractures in the distal end of the humerus in children. Acta Chir. Scand. 1945;63(Suppl 103):1.
118 Holst-Nielsen F., Ottsen P. Fractures of the lateral condyle of the humerus in children. Acta Orthop. Scand. 1974;45:518.
119 Horn B.D., Herman M.J., Crisci K., Pizzutillo P.D., MacEwen G.D. Fractures of the lateral humeral condyle: role of the cartilage hinge in facture stability. J. Pediatr. Orthop. 2002;22:8.
120 Ingersol R.E. Fractures of the humeral condyles in children. Clin. Orthop. 1965;41:32.
121 Inoue G., Tamura Y. Osteosynthesis for long-standing nonunion of the lateral humeral condyle. Arch Orthop. Trauma Surg. 1993;112:236.
122 Jakob R., Fowels J.V., Rang M. Observations concerning fractures of the lateral humeral condyle in children. J. Bone Joint Surg. 1975;57B:430.
123 Jeffrey C.C. Nonunion of the epiphysis of the lateral condyle of the humerus. J. Bone Joint Surg. 1958;40B:396.
124 Jeffrey R.S. Injuries of the lateral humeral condyle in children. J. R. Coll. Surg. Edinburg. 1989;34:156.
125 Kini M.G. Fractures of the lateral condyle of the lower end of the humerus with complications. J. Bone Joint Surg. 1942;24:270.
126 Kröpfl A., Genelin F., Obrist J., Zirniter J. Malunions and disturbances of growth after fractures of the lateral humeral condyle in children [German]. Unfallchirurgie. 1989;15:113.
127 Loyd R.D., Miller W.A. Fractures of the lateral humeral condyle in children (abstr). J. Bone Joint Surg. 1984;56A:1301.
128 Masada K., Kawai H., Kawabata H., Masatomi T., Tsuyuguchi Y., Yamamoto K. Osteosynthesis of old, established nonunion of the lateral condylar of the humerus. J. Bone Joint Surg. 1990;72A:32.
129 Mintzer C.M., Waters P.M., Brown D.J., Kasser J.R. Percutaneous pinning in the treatment of displaced lateral condyle fractures. J. Pediatr. Orthop. 1994;14:462.
130 Mirsky E.C., Karas E.H., Weiner L.S. Lateral condyle fractures in children: evaluation of classification and treatment. J. Orthop. Trauma. 1997;11:117.
131 Modrzewski K. Late ulnar nerve paresis in adults after neglected treatment for fracture of the capitellum with part of the trochlea in children [Polish]. Chir. Narzadow Ruchn. Orthop. Pol. 1995;60:9.
132 Morin B.M., Poitras B.P., Labelle H., Fassier F. Fractures of the lateral humeral condyle: Long-term results following early open reduction. In: Uhthoff H.K., Wiley J.J., editors. Behavior of the Growth Plate. New York: Raven Press; 1988:183.
133 Murnahgan J.M., Thompson N.S., Taylor T.C., Cosgrove A.P. Fractured lateral epicondyle with associated elbow dislocation. Int. J. Clin. Pract. 2002;56:475.
134 Roye D.P.Jr, Bini S.A., Infosino A. Late surgical treatment of lateral condylar fractures in children. J. Pediatr. Orthop. 1991;11:195.
135 Rutherford A. Fractures of the lateral humeral condyle in children. J. Bone Joint Surg. 1985;67A:851.
136 Sharma J.C., Arora A., Mathur N.C., Gupta S.P., Biyani A., Mathur R. Lateral condylar fractures of the humerus in children: fixation with partially threaded 4.0 mm AO cancellous screws. J. Trauma. 1995;39:1129.
137 Shimada K., Masada K., Tada K., Yamamoto T. Osteosynthesis for the treatment of nonunion of the lateral condyle in children. J. Bone Joint Surg. 1997;79A:234.
138 Skak S.V., Olsen S.D., Smaabrekke A. Deformity after fracture of the lateral humeral condyle in children. J. Pediatr. Orthop. 2001;10:142.
139 Smith F.J., Joyce J.J.III. Fractures of the lateral condyle of the humerus in children. Am. J. Surg. 1954;87:324.
140 So Y.C., Fang D., Leong J.C.Y., Bong S.C. Varus deformity following lateral humeral condylar fractures in children. J. Pediatr. Orthop. 1985;5:569.
141 Thomas D.P., Howard A.W., Cole W.G., Hedden D.M. Three weeks of Kirschner wire fixation for diaphyseal lateral condylar fractures of the humerus in children. J. Pediatr. Orthop. 2001;21:565.
142 Valdisseri L., Venturi B., Busanelli L. External humeral condyle fracture in children. A long-term review of 30 cases reported. Chir. Organi. Mov. 1993;78:105.
143 van Haaren E.R., van Vugt A.B., Bode P.J. Posterolateral dislocation of the elbow with concomitant fracture of the lateral humeral condyle: case report. J. Trauma. 1994;36:288.
144 van Vugt A.B., Severijnen R.V.S.M., Festen C. Fractures of the lateral humeral condyle in children: late results. Arch. Orthop. Trauma Surg. 1988;107:206.
145 Vathana P., Prosartritha T. Repair of nonunion lateral humeral condyle: a case report. J. Med. Assoc. Thai. 1998;81:146.
146 Wadsworth T.G. Injuries of the capitellar (lateral humeral condyle) epiphysis. Clin. Orthop. 1972;85:127.
147 Wadsworth T.G. Premature epiphyseal fusion after injury to the capitellum. J. Bone Joint Surg. 1964;46B:46.
148 Bede W.B., Lefebvre A.R., Rosman M.A. Fractures of the medial humeral condyle in children. Can. J. Surg. 1975;18:137.
149 Chacha P.B. Fracture of the medial condyle of the humerus with rotational displacement. Report of two cases. J. Bone Joint Surg. 1970;52A:1453.
150 El Ghawabi M.H. Fracture of the medial condyle of the humerus. J. Bone Joint Surg. 1975;57A:677.
151 Fahey J.J., O’Brien E.T. Fracture-separation of the medial humeral condyle in a child confused with fracture of the medial epicondyle. J. Bone Joint Surg. 1971;53A:1102.
152 Fowles J.V., Kassab M.T. Displaced fractures of the medial humeral condyle in children. J. Bone Joint Surg. 1980;62A:1159.
153 Kilfoyle R.M. Fractures of the medial condyle and epicondyle of the elbow in children. Clin. Orthop. 1963;41:43.
154 Kim H.T., Song M.B., Conjares J.V., Yoo C.I. Trochlear deformity occurring after distal humeral fractures: magnetic resonance imaging and its natural progression. J. Pediatr. Orthop. 2002;22:188.
155 Leet A.I., Young C., Hoffer M.M. Medial condyle fractures of the humerus in children. J. Pediatr. Orthop. 2002;22:2.
156 Minami A., Sugawara M. Humeral trochlear hypoplasia secondary to epiphyseal injury as a cause of ulnar nerve palsy. Clin. Orthop. 1988;228:227.
157 Godette G.A., Gruel C.R. Percutaneous screw fixation of intercondylar fracture of the distal humerus. Orthop. Rev. 1993;22:466.
158 Kasser J.R., Richards K., Millis M. The triceps-dividing approach to open reduction of complex distal humeral fractures in adolescents: a Cybex evaluation of triceps function and motion. J. Pediatr. Orthop. 1990;10:93.
159 Papavasiliou V.A., Beslikas T.A. T-Condylar fractures of the distal humeral condyles during childhood: an analysis of six cases. J. Pediatr. Orthop. 1986;6:302.
160 Peterson H.A. Triplane fracture of the distal humeral epiphysis. J. Pediatr. Orthop. 1983;3:81.
161 Re P.R., Waters P.M., Hresko T. T-condylar fractures of the distal humerus in children and adolescents. J. Pediatr Orthop. 1999;19:313.
162 Royle S.G., Burke D. Ulnar neuropathy after elbow injury in children. J. Pediatr. Orthop. 1990;10:495.
163 Saraf S.K., Tuli S.M. Concomitant medial condyle fracture of the humerus in a childhood posterolateral dislocation of the elbow. J. Orthop. Trauma. 1989;3:352.
164 Carlioz H., Abols Y. Posterior dislocation of the elbow in children. J. Pediatr. Orthop. 1981;4:8.
165 Case S.L., Hennrikus W.L. Surgical treatment of displaced medial epicondyle fracture in adolescent athletes. Am. J. Sports Med. 1997;25:682.
166 Chessare J.W., Rogers L.F., White H., Tachdjian M.O. Injuries of the medial epicondylar ossification center of the humerus. Am. J. Roentgenol. 1977;129:49.
167 Collins R., Lavine S.A. Fractures of the medial epicondyle of the humerus with ulnar nerve paralysis. Proc. Child Hosp. DC. 1964;20:274.
168 Dunn P.S., Ravn P., Hansen L.B., Burph B. Osteosynthesis of medial humeral epicondyle fractures in children. 8-Year follow-up of 33 cases. Acta Orthop. Scand. 1994;65:439.
169 Fowles J.V., Slimane N., Kassab M.T. Elbow dislocation with avulsion of the medial humeral epicondyle. J. Bone Joint Surg. 1990;72B:102.
170 Hendel D., Aghasi M., Halperin N. Unusual fracture dislocation of the elbow joint. Arch. Orthop. Trauma Surg. 1985;104:187.
171 Josefsson P.O., Danielson L.G. Epicondylar elbow fracture in children. 35-Year follow-up of 56 unreduced cases. Acta Orthop. Scand. 1986;57:313.
172 Low B.Y., Lim J. Fracture of humerus during arm wrestling: report of 5 cases. Singapore Med. J. 1991;32:47.
173 Ogawa K., Ui M. Fracture-separation of the medial humeral epicondyle caused by arm wrestling. J. Trauma. 1996;41:494.
174 Partio E.K., Hirvensalo E., Bostman O., Rokkanen P. A prospective controlled trial of the fracture of the humeral medial epicondyle—how to treat? Ann. Chir. Gynaecol. 1996;85:67.
175 Pritchett J.W. Entrapment of the medial nerve after dislocation of the elbow: case report. J. Pediatr. Orthop. 1984;4:752.
176 Skak S.V., Grossman E., Wagn P. Deformity after internal fixation of fracture separation of the medial epicondyle of the humerus. J. Bone Joint Surg. 1994;76B:272.
177 Sugita H., Kotani H., Ueo T., Miki T., Senzouku F., Hara T., Nagagawa Y., Sakka A., Nagagawa T., Seki K. Recurrent dislocation of the elbow [Japanese]. Nippon Geka Hokan. 1994;63:181.
178 Szymanska E. Evaluation of AO kit screw fixation of medial condyle and epicondyle distal humeral epiphyseal fractures in children [Polish]. Ann. Acad. Med. Stetin. 1997;43:239.
179 Woods G.W., Tullos H.S. Elbow instability and medial epicondylar fractures. Am. J. Sports. 1977;5:23.
180 Li Y.H., Leong J.C. Fractured lateral epicondyle associated with lateral elbow instability. Injury. 1995;26:267.
181 Chotel F., Sailhan F., Martin J., Filipe G., Pem R., Garnier E., Berard J. A specific closed percutaneous technique for reduction of Jeffrey Type II lesion. J. Pediatr. Orthop. B. 2006;15:376.
182 Gaston S.R., Smith F.M., Baab O.D. Epiphyseal injuries of the radial head and neck. Am. J. Surg. 1953;85:266.
183 Jeffery C.C. Fractures of the head of the radius in children. J. Bone Joint Surg. 1950;32B:314.
184 Leung A.G., Peterson H.A. Fractures of the proximal radial head and neck, with emphasis on those that involve the articular cartilage. J. Pediatr. Orthop. 2000;20:7.
185 Malmvick J., Herbertsson P., Josefsson P.O., Hasserius R., Besjakov J., Karlsson M.K. Fracture of the radial head and neck of Mason types II and III during growth: a 14-25 year follow-up. J. Pediatr. Orthop. B. 2003;12:63.
186 McBride E.E., Monnet J.C. Epiphyseal fractures of the head of the radius in children. Clin. Orthop. 1960;16:264.
187 O’Brien P.I. Fractures involving the proximal radial epiphysis. Clin. Orthop. 1965;41:51.
188 Osada D., Tamai K., Kuramochi T., Saotome K. Three epiphyseal fractures (distal radius and ulna and proximal radius) and a diaphyseal ulnar fracture in a seven-year-old child’s forearm. J. Orthop. Trauma. 2001;15:375.
189 Payne J.F., Earle J.L. Fracture dislocation of the proximal radial epiphysis. Minn. Med. 1969;52:479.
190 Reidy J.A., Van Gorder G.W. Treatment of displacement of proximal radial epiphysis. J. Bone Joint Surg. 1963;45A:1355.
191 Sessa S., Lascombes P., Prevot J., Gagneux E. Fractures of the radial head and associated elbow injuries in children. J. Pediatr. Orthop. 1996;5:200.
192 Bracq H. Fracture of the coronoid apophysis. Rev. Chir. Orthop. 1987;73:472.
193 Burrel C.G., Strecker W.B., Schoenecker P.L. Surgical treatment of displaced olecranon fractures in children. J. Pediatr. Orthop. 1997;17:321.
194 Gwynne-Jones D.P. Displaced olecranon apophyseal fractures in children with osteogenesis imperfecta. J. Pediatr. Orthop. 2005;25:154.
195 Parson F.G. Observations on traction epiphyses. J. Anat. Physiol. 1904;38:248.
196 Rabinovich A., Adili A., Mah J. Outcomes of intramedullary nail fixation through the olecranon apophysis in skeletally immature forearm fractures. J. Pediatr. Orthop. 2005;25:565.
197 Retrum R.K., Wepfer J.F., Olsen D.W., Laney W.H. Case report 355: delayed closure of the right olecranon epiphysis in a right-handed, tournament-class tennis player (post-traumatic). Skeletal Radiol. 1986;15:185.
198 Schweitzer G. Bilateral avulsion fractures of the olecranon apophyses. Arch. Orthop. Trauma Surg. 1988;107:181.
199 Zionts L.E., Moon C.N. Olecranon apophysis fractures in children with osteogenesis imperfecta revisited. J. Pediatr. Orthop. 2002;22:745.