73
Photodermatoses
Photo Facts
• More than 95% of UVR that reaches the earth’s surface is UVA.
• UVA, but not UVB, can penetrate through glass windows.
• The penetration of UVR into the skin is wavelength-dependent (Fig. 73.1).
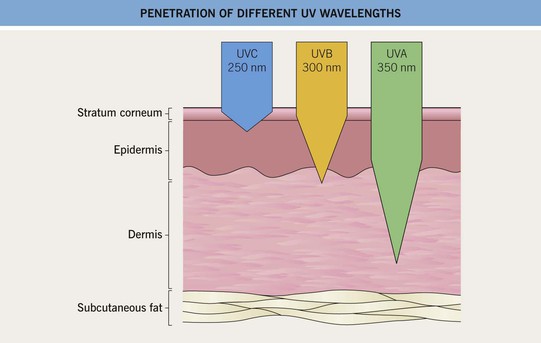
Fig. 73.1 Depth of penetration of different wavelengths of UV light into human skin. Depth of penetration varies greatly with the thickness of the different skin layers and their composition (e.g. melanin content). The beginning of the wedge-shaped portion of the penetration symbol represents a decrease to approximately one-third of the incident energy density, and the tip of the symbol represents a decrease to approximately 1%. Figure not drawn to scale.
• Principles and formulations of sunscreens are discussed in the Appendix.
Cutaneous Effects of UVR Exposure: Acute
• Typically, a UVB-induced sunburn appears within 30 minutes to 8 hours of sufficient exposure, peaks at 12–24 hours, and diminishes over hours to days with desquamation.
• Tanning occurs as a biphasic response to UVR and is wavelength-dependent.
– ‘Delayed tanning’ usually results from UVB exposure and peaks about 3 days after sun exposure.
Cutaneous Effects of UVR Exposure: Chronic
• The visible long-term effects of UVR include photoaging and photocarcinogenesis.
• Cutaneous signs of photoaging are pictured in Fig. 73.2 and also include solar lentigines, sunburn lentigines, and ephelides; in more darkly pigmented skin, small seborrheic keratoses, melasma, and dyspigmentation may be seen.
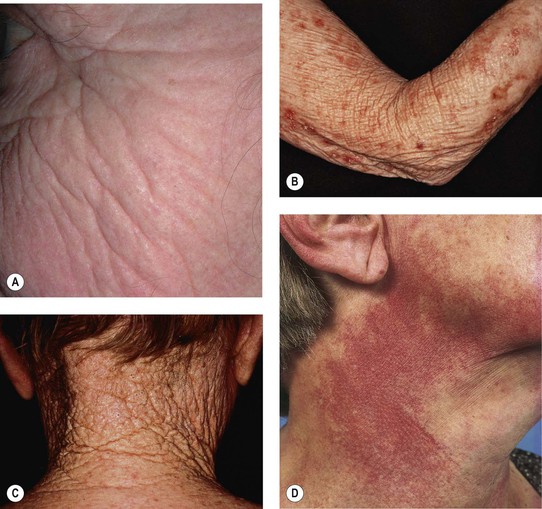

Fig. 73.2 Cutaneous signs of significant photoaging. A, B Solar elastosis of the cheek and arm with the characteristic yellow discoloration and thickening of the skin. C Cutis rhomboidalis nuchae with deep furrowing of the posterior neck. D Poikiloderma of Civatte with sparing of the anterior neck. E Multiple open comedones of the malar region in Favre–Racouchot syndrome. F Brown discoloration of the dorsal hand due to hemosiderin deposits from recurrent solar purpura. G Fragility of atrophic photodamaged skin of the shin. H Erosive pustular dermatosis of the bald scalp. I Photoaging in a 93-year-old African-American woman, demonstrating fine wrinkling and numerous tiny seborrheic keratoses. A, Courtesy, Henry Lim, MD; B, Courtesy, Jean L. Bolognia, MD. E, I, Courtesy, Henry Lim, MD; F, G, Courtesy, Jean L. Bolognia, MD.
• Chronic UVR is responsible for development of actinic keratoses, squamous cell carcinoma, basal cell carcinoma, and cutaneous melanoma (see Chapters 88 and 93).
Photodermatoses
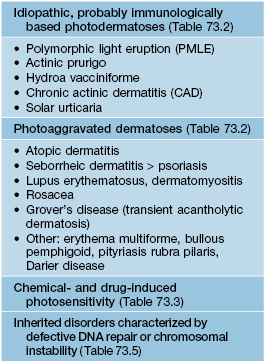
• The photodermatoses are classified into four broad categories (Table 73.1) and are discussed in Tables 73.2 (Figs. 73.3–73.10), Table 73.3 (Fig. 73.11), and Table 73.5 (Fig. 73.12).
Table 73.2
Clinical features of the idiopathic, probably immunologically based, photodermatoses and photoaggravated dermatoses.
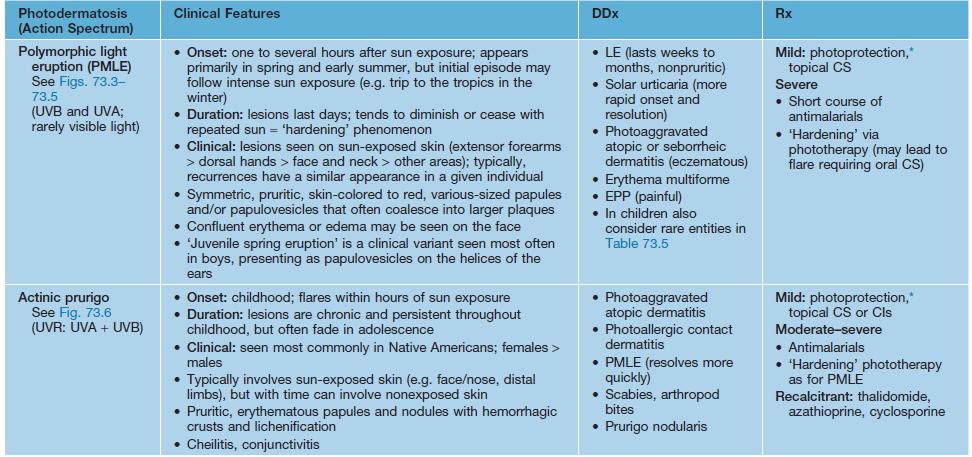
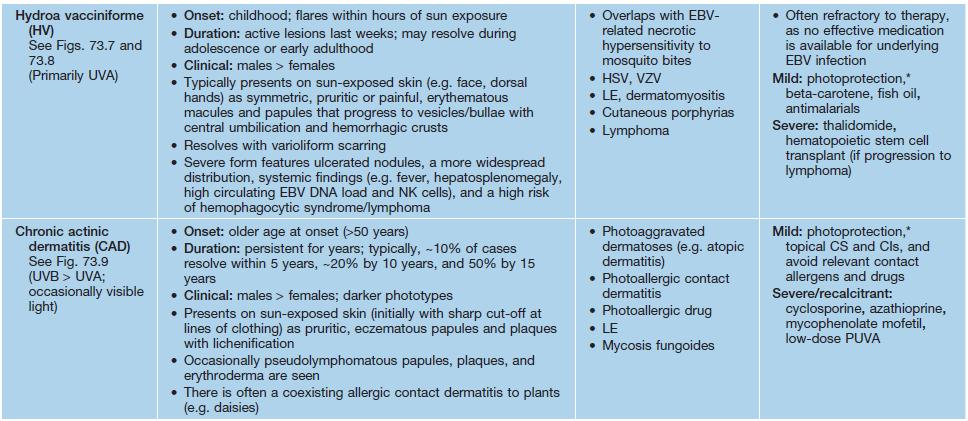
* Photoprotection generally includes avoidance of sun, sun-protective clothing, broad-spectrum sunscreens, hats, sunglasses; for UVA-sensitive disorders, must also caution about protection from UVR received while driving or through glass windows; zinc- and titanium dioxide-based sunscreens are best for visible light-sensitive disorders.
UVA, ultraviolet A; UVB, ultraviolet B; LE, lupus erythematosus; EPP, erythropoietic protoporphyria; CI, calcineurin inhibitor; PUVA, psoralens plus ultraviolet A; UVR, ultraviolet radiation, including both UVA and UVB; HSV, herpes simplex virus; VZV, varicella–zoster virus; EBV, Epstein–Barr virus; PMLE, polymorphic light eruption; CAD, chronic actinic dermatitis.

Fig. 73.3 Polymorphic light eruption (PMLE) of the face. Edematous erythematous plaques on the cheeks of a young child.



Fig. 73.4 Polymorphic light eruption (PMLE) of the upper extremity. Small papules (A), papulovesicles (B), and larger edematous papules and plaques (C).

Fig. 73.5 Polymorphic light eruption (PMLE) of the thigh. Edematous papules becoming confluent into plaques. Courtesy, Jean L. Bolognia, MD.




Fig. 73.6 Actinic prurigo. A The clinical features, including a photodistribution and worsening in the summer, are somewhat suggestive of polymorphic light eruption, but the lesions were persistent and the HLA type was that seen in association with actinic prurigo. Note the involvement of the ears. B The crusted papules are more dense on the distal arms. C This patient with severe actinic prurigo has involvement of the buttocks. D Significant cheilitis that is more severe on the lower lip in a Peruvian man with Native American (as well as European) ancestry. A–C, Courtesy, John L. M. Hawk, MD; D, Courtesy, Jean L. Bolognia, MD.



Fig. 73.7 Hydroa vacciniforme. A There is an early, polymorphic light eruption-like appearance, but with vesicles around the mouth and umbilicated lesions on the nose. B Hemorrhagic crusts are admixed with varioliform scars; the latter are the sequelae of repeated acute attacks. Note the telangiectasias on the nasal tip. C More severe crusting and scarring. A, C, Courtesy, John L. M. Hawk, MD; B, Courtesy, Jean L. Bolognia, MD.

Fig. 73.8 EBV-associated hydroa vacciniforme-like eruption. This Hispanic child had >50 000 copies of EBV DNA/100 000 WBCs as well as EBV RNA within skin lesions by in situ hybridization; he subsequently died of lymphoma. Note the facial edema, erythema, papulovesicles, hemorrhagic crusts, and varioliform scars. Courtesy, Richard Antaya, MD.



Fig. 73.9 Chronic actinic dermatitis (CAD). A Chronic eczematous changes of the posterior neck with lichenification and a sharp cut-off at the collar in a patient with phototype V skin. B Lichenification and hyperpigmentation in sun-exposed sites with areas of depigmentation. Note the sparing of sun-protected areas (i.e. nasolabial fold and shoulder). C Chronic eczematous changes of the dorsal hand and wrist with associated hyperpigmentation and scaling. Note the sharp cut-off at the distal forearm. Courtesy, Henry Lim, MD.

Fig. 73.10 Solar urticaria. Wheal and flare responses within minutes of exposure to UVB irradiation in a patient undergoing phototesting. Courtesy, John L. M. Hawk, MD.
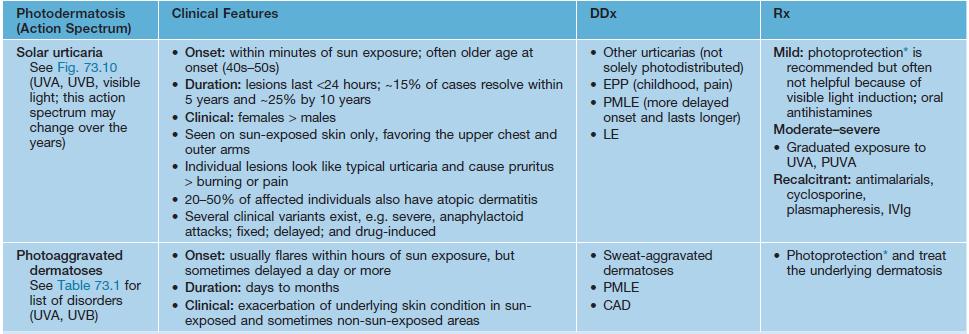
Table 73.3
Chemical- and drug-induced photosensitivity.
Treatment of phototoxic and photoallergic reactions includes discontinuation of the offending agent or medication, photoprotection, symptomatic care, and occasionally topical or oral CS if severe. Photoprotection generally includes avoidance of sun, sun-protective clothing, broad-spectrum sunscreens, hats, and sunglasses; for UVA-sensitive disorders, must also caution about protection from UVR received while driving or through glass windows; zinc- and titanium dioxide-based sunscreens are best for visible light-sensitive disorders.
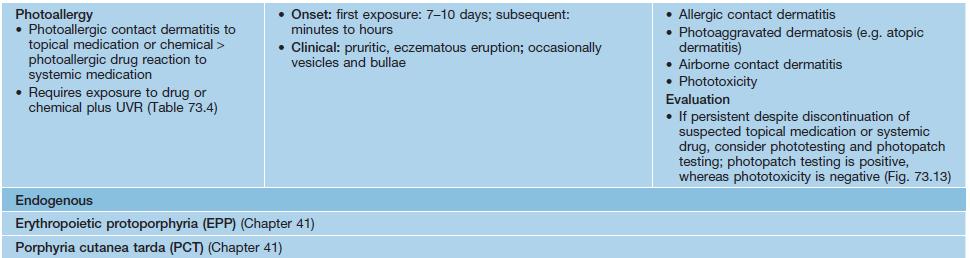
* Lichenoid drug eruptions, including photolichenoid drug eruptions, are discussed in Chapter 9.
UVR, ultraviolet radiation, including both UVA and UVB; UVA, ultraviolet A; UVB, ultraviolet B; PCT, porphyria cutanea tarda; NSAIDs, nonsteroidal anti-inflammatory drugs; EPP, erythropoietic protoporphyria; LE, lupus erythematosus.
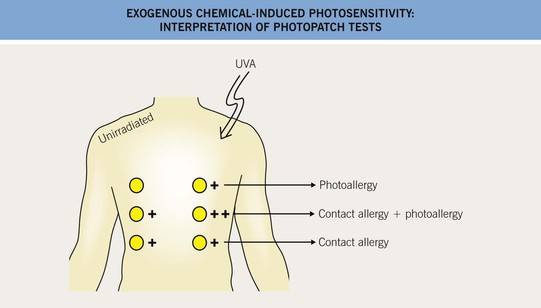
Fig. 73.13 Exogenous chemical-induced photosensitivity: Interpretation of photopatch tests. This schematic demonstrates the interpretation of photopatch tests. The UVA dose is usually the lower of 5 J/cm2, or 50% of the MED to UVA.

Fig. 73.11 Drug-induced photosensitivity and hyperpigmentation. Gray-brown patches involving the sun-exposed skin of a patient receiving diltiazem. Courtesy, Henry Lim, MD.

Fig. 73.12 Xeroderma pigmentosum. A 17-year-old boy with skin phototype V who has hyper- and hypopigmentation admixed with scarring, lentigines, and seborrheic as well as actinic keratoses. Note the squamous cell carcinoma in situ of the lower lip in association with severe actinic cheilitis. Courtesy, Julie V. Schaffer, MD.
• Phototoxicity results from direct tissue and cellular injury following UVR-induced activation of a phototoxic agent; resembles a sunburn (Table 73.4).
Table 73.4
Common phototoxic and photoallergic agents.
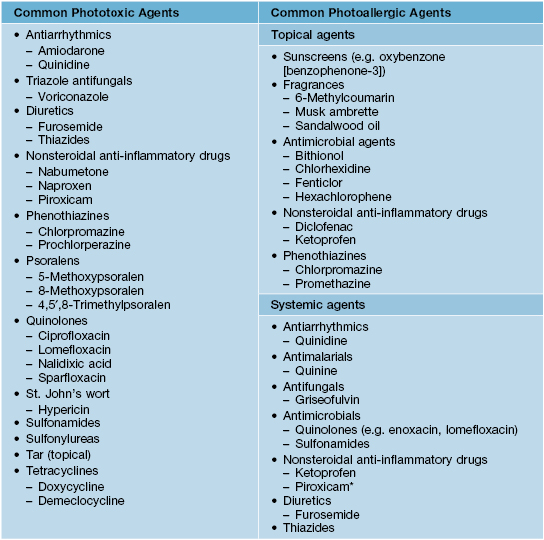
* Often have positive patch test to thimerosol.
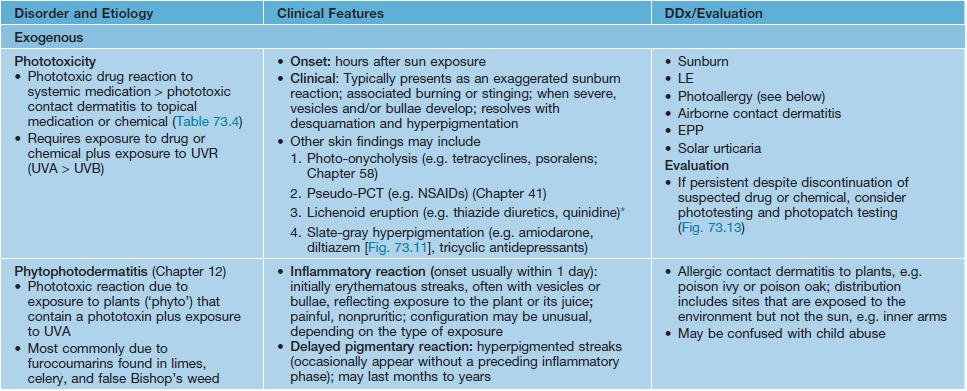
Table 73.5
Clinical features of selected inherited photosensitivity disorders associated with defective DNA nucleotide excision repair or chromosomal instability.
All four listed diseases are rare and inherited in an autosomal recessive fashion, but they are the more common of these disorders.
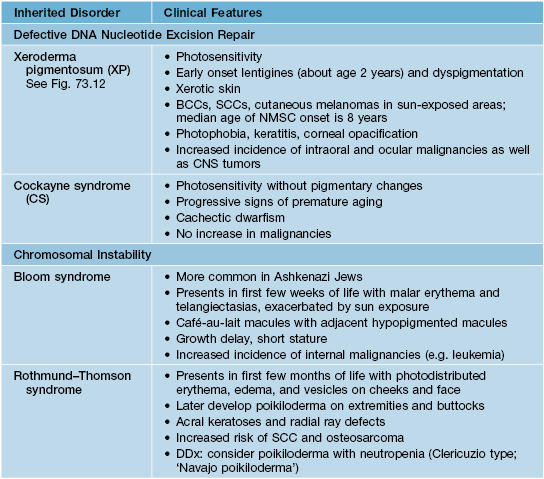
BCC, basal cell carcinoma; SCC, squamous cell carcinoma.
• Photoallergy is a delayed-type hypersensitivity response that requires both a photoallergen (usually topical) and UVR exposure; resembles eczema (Table 73.4).
• It is important to recognize photodistributed versus photoprotected areas on the body; sparing of certain sites, including behind the ears, under the chin, the upper eyelids, and the nasolabial folds, is a clue to a photodistributed eruption (Fig. 73.14).
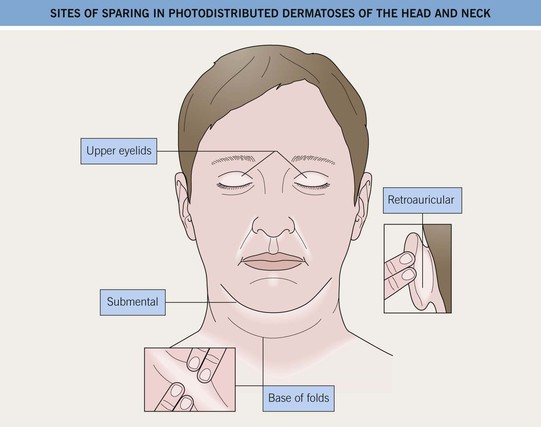
Fig. 73.14 Sites of sparing in photodistributed dermatoses of the head and neck (e.g. chronic actinic dermatitis and photoallergic dermatitis). Relatively sun-protected sites include the upper eyelids, nasolabial folds, retroauricular areas, submental region, and deepest portion of skin furrows. In airborne contact dermatitis, these areas may be involved.
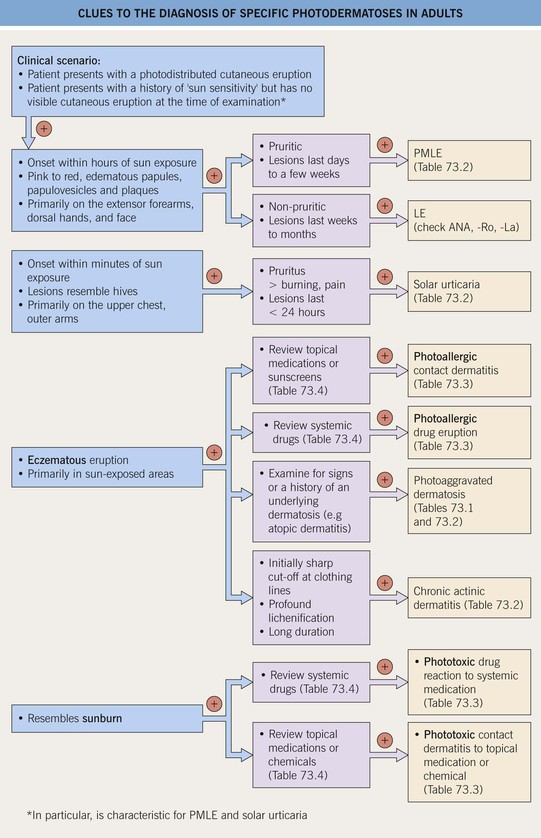
• Clues to the diagnosis of various photodermatoses are outlined in Fig. 73.15.
Grover’s Disease (Transient Acantholytic Dermatosis)
• Occurs primarily in middle-aged males > females as pruritic, often crusted, skin-colored to pink papules and papulovesicles on the trunk, primarily in sun-exposed areas (see Fig. 48.2 and Fig. 73.16).
For further information see Ch. 87. From Dermatology, Third Edition.