3. Perinatal Transport and Levels of Care*
Mario A. Rojas, Kelly Shirley and Margaret G. Rush
Perinatal transport is the timely and appropriate transfer of high-risk pregnant mothers to health care facilities in which expertise and resources for optimal care are available to improve mortality and morbidity of both the mother and her fetus. If transfer of the mother is not possible because of risk outweighing potential benefit, the objective then shifts to optimizing delivery and birth of the high-risk infant. In the latter situation, it is necessary to have adequately trained professionals to resuscitate and stabilize the infant before his or her transfer to a medical center that has the appropriate expertise and resources.
For perinatal transport to effectively support high-risk mothers and their fetuses, as well as sick newborn infants, each country, state, or region must identify its perinatal resources with respect to physical and human capabilities. This review should include classification of levels of care and expertise, as well as mapping of resources as they exist within specific geographic areas. Classification of perinatal resources according to the different levels of care as recommended by the American Academy of Pediatrics and the American College of Obstetricians and Gynecologists in their Guidelines for Perinatal Care4 will direct organization, identification of resources and roles of patient referral and retrieval centers, as well as reveal the natural elevation of care within the geographic area of question (Table 3-1). Historically, regionalization has been recommended as the most effective and cost-efficient use of perinatal resources. 8,11,12,36,45 The implementation of this important strategy is subject to qualitative variance depending on the characteristics of the health care system and resources where it is applied. In countries in which universal health care is the norm, regionalization is more easily implemented, whereas in market-driven health care systems in which de-regionalization is predominant, these provisions for care become more challenging. * Whatever the circumstances, perinatal providers must use innovative strategies to maintain high-quality perinatal transport systems. 19,22
| BPP, Biophysical profile; NCPAP, nasal continuous positive airway pressure; NRP, Neonatal Resuscitation Program; PGE1, prostaglandin E 1; S.T.A.B.L.E., S.T.A.B.L.E. program. | ||||
| Maternal | Neonatal | |||
|---|---|---|---|---|
| Risk-Oriented Prenatal Care | Basic Neonatal Care | Patient Characteristics | Personnel | |
| Level 1 |
Medical screening examination/ Patient triage
Initial treatment and stabilization
Maternal-fetal monitoring/prenatal ultrasound/BPP
Non-stress test/stress test
30-minute response time for cesarean section
24-hour clinical laboratory services
24-hour radiology services
24-hour blood bank services
|
Resuscitation and stabilization (NRP; S.T.A.B.L.E.):
Initiation of respiratory support (nasal cannula, oxygen hood, NCPAP, and Neopuff™)
Surfactant administration
Peripheral IV access/IV fluids
Initiation of antibiotics
Initiation of PGE 1 when a congenital heart defect is suspected
|
Uncomplicated maternity and neonatal care
Emergency management of unexpected complications
Healthy term infants
Stable late-preterm infants 35-37 weeks’ gestation
|
Obstetrician
Pediatrician
Family physicians
Certified nurse midwife
Pediatric nurse practitioner
24-hour anesthesia availability
|
| Level 2 A |
15-minute response time for cesarean section
Complicated cases not requiring intensive care
|
Level 1 care AND
Special care nursery
|
Complete maternity and neonatal care for uncomplicated and most high-risk patients (infants >32 weeks and >1500 g) |
Neonatologist
Pediatric neonatal hospitalist
24-hour in-house anesthesia for obstetrics
|
| Level 2 B | Capability to provide mechanical ventilation for up to 24 hours or continuous positive airway pressure | Neonatologist | ||
| Level 3 |
Provision of comprehensive perinatal health care services for women and neonates of all risk categories
Complicated cases requiring intensive care
Labor <34 weeks’ gestation
|
Provision of comprehensive perinatal health care services for women and neonates of all risk categories |
Intensive care patients
Anticipated need for neonatal surgery
|
Maternal-fetal specialist
Neonatologist
Obstetrician
|
| Level 3 A |
Provide comprehensive care for infants >28 weeks’ gestation and weighing >1000 g
Sustained mechanical ventilation
|
Pediatric surgeon for minor surgical procedures | ||
| Level 3 B |
Provide comprehensive care for infants ≤28 weeks’ gestation and weighing <1000 g
Sustained mechanical ventilation
High-frequency ventilation
Inhaled nitric oxide
|
Full range of pediatric medical and surgical subspecialties | ||
| Level 3 C |
Provision of comprehensive perinatal health care services at and above those of subspecialty care facilities
Responsibility for regional perinatal health care service organization and coordination
|
Extracorporeal life support
Open heart surgery for congenital cardiac malformations
|
Pediatric cardiothoracic surgeon | |
Because all hospitals cannot provide all levels of perinatal care, interhospital transport of pregnant women and neonates is an essential component of any regional perinatal effort. Women who are at risk for complications and pose significant risk for adverse outcomes or whose neonates are likely to require intensive care support should be considered candidates for referral during the antepartum period. 25 Similarly, it is accepted medical practice to transfer a neonate to a hospital that can provide the services needed or anticipated to be needed if the birth hospital cannot provide that level of service. †
Once resources are identified and classified, a model for integration of perinatal services may be constructed. Strategic planning at this level will direct the design of the organizational structure of the perinatal transport system, including identification of leadership functions, the different member nurseries/units and their roles, and the definition and process for perinatal elevation of care. This integration will then allow for the creation of a system for continuous data collection and analysis, facilitating a systems approach to problem solving and the implementation of quality improvement strategies within the system. 27
REGIONAL PERINATAL REFERRAL AND TRANSPORT SYSTEM
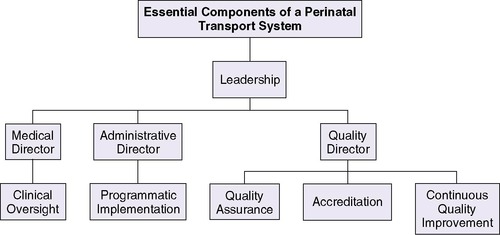
Independent of the health care system with which one identifies (universal versus market driven), the referral system must identify a subspecialty care regional perinatal center, for which the responsibility of coordinating interfacility perinatal transfer lies. Although many different models provide clinical care in transport, the transport system should include the minimal components of (1) leadership (both medical and administrative), (2) communication, and (3) quality assurance (Figure 3-1).
Leadership
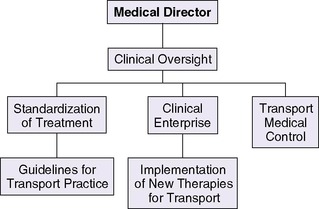
One proposed model is the implementation of a leadership team that comprises a medical director, administrative director, and quality director. This team approach enables collaborative and timely oversight of the transport system with potential for growth and quality improvement. The medical director should be a physician with expertise in transport medicine. The medical director’s role includes overseeing the following37 (Figure 3-2):
 |
| FIGURE 3-2 |
• Development, implementation, and monitoring of patient care and transport standards
• Scope of practice of team members
• Team selection
• Training and continuing education
• Support of perinatal partnerships and advocacy
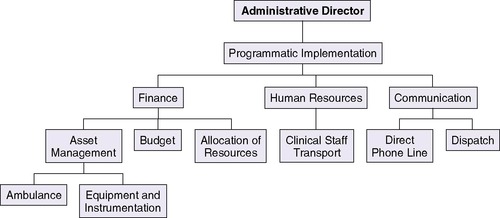
The administrative director working in conjunction with the medical director oversees the budget and day-to-day management of the transport process, including maintenance of equipment. The administrative director should possess clinical transport knowledge paired with strong administrative qualities, because this role includes oversight of finance, human resources, and communication operations (Figure 3-3). 37 The quality director should be a health care provider with a professional background in continuous quality improvement, process analysis, and management. In association with the medical director and administrator, the quality director is responsible for the development and maintenance of a transport database for operational management, quality assurance, and analysis. This administrator should also be able to apply the basic concepts of quality improvement and management to implement novel interventions aimed at improving the perinatal transport system (Figure 3-4). 27
 |
| FIGURE 3-3 |
 |
| FIGURE 3-4 |
Communication
As indicated in Table 3-1, a regional subspecialty perinatal care center should be responsible for coordination of perinatal transport (level 3C). Integral to the regional transport system is the creation of a centralized communication center with a perinatal regional hotline. 20 The communication center is responsible for coordinating maternal and neonatal transports within the different levels of care. Roles within this center include referring physician, dispatcher, bed locator, and transport medical control officer (obstetrician and neonatologist). The inclusion of specialized personnel in the initial communication process may support rendering institutions appropriate treatment strategies while decreasing diagnostic discordance. 46
For purposes of basic communication, a central dedicated telephone line is recommended to provide direct, easy, and immediate access to the regional system. This access should be staffed 24 hours per day, 7 days per week and should be unencumbered. This model also includes the transfer of the referral call to the transport medical control officer, thereby greatly simplifying the process for the referral-consultation. The ability to support communication among the referring physician, the dispatcher, and the medical control officer simultaneously can speed up decision making and the initiation of transport. Once in transport, communication among the transport team, the referring physician, and the medical control officer becomes integral to the care provided (Figure 3-5). Changes in patient status, bed status, equipment needs, and weather need to be communicated in a timely manner. This information may demand a review of the transport plan and is best facilitated through a central communication center. 20,37 The organization of a perinatal regional hotline has been shown to increase significantly both in utero and neonatal transports, allowing for safe, 24-hour, on-call management of perinatal transports and the collection of epidemiologic indicators relative to perinatal transfers. 20
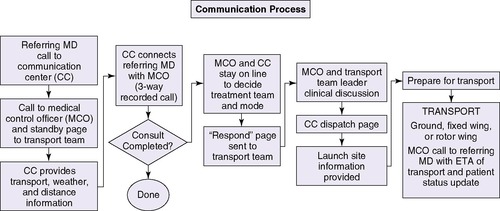 |
| FIGURE 3-5
(Contributed by S. Brodtrick, D. Quinn, and M. Cortez.)
|
The rapidly advancing field of telecommunications offers a wide variety of opportunities for transmitting medical information, subject to proper consideration of privacy and confidentiality requirements. This medium permits the use of satellite technology and video-conferencing equipment to conduct a real-time consultation between medical specialists in two geographically different areas. Store-and-forward telemedicine involves acquiring medical data (e.g., medical images, biosignals) and then transmitting this data to a medical specialist for assessment offline. It does not require the presence of both parties at the same time. These technologies may facilitate appropriate referral of patients according to complexity and may decrease incidence of inappropriate transfer or diagnostic discordance, allowing for optimal use of resources. 45,52 Furthermore, these innovative strategies have the potential to overcome de-regionalization of services by creating virtual regional networks for perinatal transport.
Quality
The regional subspecialty perinatal care center, as noted in Table 3-1, is responsible for regional outreach support, education, and continuous quality oversight. Traditionally, quality improvement was assigned to the medical director. However, in light of current health care complexities and regulatory specifications surrounding the quality and safety of patient care, it is recommended that this role be assigned to an individual with the expertise to effectively evaluate programmatic performance at all levels of the organizational structure. This continuous evaluation of the process will facilitate modification of the transport system when potential problems are identified. 27
The leadership team should oversee overall transport performance. The systematic collection and analysis of carefully selected performance indicators such as patient demographics, management and outcome, safety, logistics, equipment malfunction, and cost will drive quality initiatives. A quality review of individual transports, incidence reports, and occurrence debriefs will enhance this process. 37,55 Using a transport validated physiologic score (e.g., the transport risk index of physiologic stability [TRIPS]) to evaluate patient status before, during, and after transport can assist team and transport performance. 34,37
In addition, quality assurance may be implemented through continuing education both internally and externally. Transport programs must create individualized internal training programs that effectively provide current and continuous education to ensure maintenance of appropriate skills for high-quality perinatal transport. A similar program must be adapted to provide educational resources to the referring hospital where training in pre-transport resuscitation and stabilization is imperative. Ensuring competence in these areas has the potential to improve short-term and long-term morbidity of sick infants, offsetting the negative effects of de-regionalization and distance between interhospital transfer facilities. 7,37
High-Risk Maternal Referral
The most effective method to decrease mortality and morbidity during the perinatal and neonatal period is the timely and appropriate referral of mothers with high-risk pregnancies to medical centers in which both the human and technical resources are available to address complications. 14,20In situations in which the risk to the mother outweighs the benefit of her transfer during active labor, the timely dispatch of the neonatal transport team from the regional perinatal center for resuscitation and stabilization of the high-risk neonate may be considered the optimal approach to delivery of care.
Adequate referral of high-risk perinatal patients begins with high-quality antepartum surveillance.48 Indications for referral to a regional center are shown in Box 3-1. Early identification of factors that can affect pregnancy outcome is important in developing appropriate diagnostic and treatment plans. Optimal perinatal care implies having well-trained and up-to-date obstetricians at all levels of care during both the antepartum and intrapartum period. These physicians should be experts in identifying maternal-fetal risk factors and complications through their knowledge, clinical skills, and expertise in prenatal ultrasound and fetal monitoring. 1,17,40,42 In situations in which this level of expertise is not available, medical and nursing personnel should be specifically trained to identify high-risk pregnancies with the objective of pursuing early referral. Consultation and referral decisions for the high-risk mother should be based on the results of a thorough evaluation of each patient and specific guidelines. Communication between the referral center and the regional perinatal center may be facilitated through the use of video-medicine technology. 18
BOX 3-1
A. Prenatal Ultrasound Diagnosis
1. Complex fetal genetic or congenital anomalies
2. Severe intrauterine growth restriction44
3. Hydrops fetalis
4. Severe oligohydramnios and polyhydramnios
5. Fetal airway anomalies
B. Maternal Medical Complications
1. Advanced or uncontrolled diabetes mellitus
2. Severe organic heart or lung disease
3. Severe renal disease
4. Maternal infection that can affect the fetus
5. Thyrotoxicosis
C. Maternal Surgical Complications
1. Acute abdominal emergency
2. Trauma requiring intensive care
3. Thoracic emergency requiring intensive care
D. Obstetric Complications
1. Premature onset of labor
2. Premature rupture of membranes
3. Third trimester bleeding
4. Severe preeclampsia or hypertension
5. Multiple gestations
6. Rh isoimmunization
Neonatal Referral
Despite efforts to identify high-risk perinatal patients during the antepartum period, as many as 30% to 50% of infants who ultimately require additional neonatal care may not be recognized until the late intrapartum or early neonatal period. 33 For this reason, all hospitals that provide obstetric services must be prepared for the birth, resuscitation, stabilization, and treatment of premature or term sick infants. The Neonatal Resuscitation Program (NRP) 3,6,42 sponsored by the American Heart Association and the American Academy of Pediatrics is an excellent resource for training individuals and maintaining resuscitation skills in both a regional program and an individual hospital setting. Certification (and renewal) of NRP training should be a universal standard for all delivery room and nursery staff. Beyond the immediate delivery room setting, supportive care should be offered and maintained until the transport team has arrived and assumed care (Box 3-2). This continuance of care is well standardized within the S.T.A.B.L.E. program. 28,51 This program is the only neonatal continuing education program to focus exclusively on the post-resuscitation and/or pre-transport stabilization care of neonates.
BOX 3-2
Sugar and safe care
Temperature
Airway
Blood pressure
Lab work
Emotional support for the family
Modified from Karlsen K: The S.T.A.B.L.E Program: post-resuscitation/pre-transport stabilization care of sick infants—guidelines for neonatal healthcare providers, ed 5, Park City Utah, 2006, S.T.A.B.L.E., Inc.
NEONATAL TRANSPORT
Stabilization of patients and preparation for transport should begin before the transport team arrives. In consultation, the referring center (physician) and transport medical control officer (MCO) may address additional areas of attention based on specific patient clinical assessment and presumptive diagnosis. Although the reasons for neonatal referral may be quite diverse and based on needs of infants relative to the capabilities of the referring center, the most common indications include respiratory distress, prematurity, congenital anomalies (surgical and nonsurgical), and suspected congenital heart disease. Stabilization and support of these infants may require frequent interhospital communication (referring physician and transport medical control officer) to identify specific medical interventions. The importance of this form of continuing dialogue with respect to accuracy in diagnosis, management, and changes in patient status cannot be stressed enough. Again, the use of video-telemedicine may facilitate the accuracy of these interactions. 7,18
When the transport team arrives, the receiving hospital generally assumes control of the infant’s care, although a certain degree of flexibility and cooperation with the referring staff are maintained. In the event that a community EMS service is used for transport, the referring physician retains medical control until the patient reaches the regional referral center.
Team Configuration
Transport teams may be composed of a variety of medical personnel, including neonatologists, neonatal nurse practitioners, registered nurses, respiratory therapists, paramedics, and emergency medical technicians. 34,35The two general categories of transport teams are dedicated and non-dedicated, with a third hybrid model now emerging in many institutions. Dedicated teams are those whose members perform neonatal transport on a full-time basis. They generally are not assigned to any other major clinical responsibilities. Non-dedicated teams are composed of members who, although available for transport, are primarily involved with other clinical duties. The hybrid model takes advantage of the well-trained pool of neonatal intensive care unit (NICU) staff, as in the case of the non-dedicated team, but allows for a timely response to transport, as in the dedicated team model. The decision about which type of team to use depends largely on institutional factors. These factors often include the acuity of care level managed in the unit, annual volume of transports, financial support, and national, state, or local laws regulating the expanded role of nurses and respiratory therapists in health care. 23 Regardless of the team composition, the team must have the cumulative expertise to resuscitate, stabilize, and provide critical care throughout the transport.
Dedicated transport teams originated in the 1980s when large metropolitan hospitals began to experience an increase in the demand for neonatal transports. These teams often are composed of a nurse designated as team leader and a second nurse or a respiratory therapist as a partner, with a physician or nurse practitioner added to the team when a neonate is critically ill and more advanced procedures may be anticipated. 16,17,30,35 Nurse-led teams have been shown (1) to provide better continuity of care, improved documentation, better maintenance of transport equipment, improved team availability, and stronger liaisons with referring hospitals and (2) to reduce overall operating costs. 37 The principal advantage to dedicated teams includes their immediate around-the-clock availability and their advanced training in neonatal resuscitation and stabilization procedures. However, the additional personnel necessary for dedicated teams may make these teams expensive to maintain.
Non-dedicated teams usually are made up of staff nurses and respiratory therapists within the NICU. 16,35 The advantage to having a unit-based, non-dedicated transport team is the large pool of trained personnel available around the clock. Qualifications of team members can be based on their daily bedside critical care experience and supplemental education, such as certification as a neonatal resuscitation provider. The primary disadvantage to this team design is that the transport nurse’s patient assignments must be absorbed by the unit nursing staff until he or she returns. However, unit-based teams usually are very cost effective because critical care skills are maintained during regular patient care, advanced skill training may be more focused, and administrative oversight duties are diminished. 35
The hybrid model recognizes the advantage of pulling the transport team from bedside providers while ensuring immediate, around-the-clock availability. Using this model, transport team members are identified through an interview process and receive additional training for transport care. The personnel then rotate service between bedside care and transport service based on schedule, allowing for a dedicated transport team 24 hours per day, 7 days per week. This model allows for timely dispatch, with no change in patient assignments at the bedside. In addition, this model takes advantage of ongoing bedside critical care training and provides for appropriate skill maintenance. These teams may be nurse-led or may integrate respiratory therapy, physician, or nurse practitioner leadership, based on patient acuity.
Transport Education
A minimum of 2 years of level III neonatal critical care staff experience is a basic requirement for the nursing and respiratory therapy components of most neonatal transport services. Nurses and respiratory therapists who specialize in neonatal transport should have a basic understanding of neonatal pathophysiology, resuscitation and stabilization techniques, ventilatory management, and radiographic interpretation. In the event of a critically ill patient, a nurse practitioner or physician may serve as team leader with respect to high-level procedures and patient management. 29,30
Most transport programs will develop training programs individualized to local needs, with the level of training dependant on whether the providers are nurse-led or physician-led. The scope of practice and curriculum is overseen by the medical director. Although no standard curriculum for transport providers exists, guidelines have been published by the American Academy of Pediatric Taskforce on Interhospital Transport. 2,37 Programs using air transport should ensure that all providers, including physicians who may be involved occasionally, have education on air safety, survival methods, and flight physiology (including air transport effects of barometric pressure, g-force, humidity change, potential temperature loss, noise, and vibration). In addition, the program must ensure continuing education for all aspects of transport to include updates on care management, maintenance of skills, reviewing of practice standards, and new management strategies. 37,49
Mode of Transport
When initiating a neonatal transport program, the first step should be to identify the geographic catchment area, total number and location of perinatal resources, distance in miles/kilometers, and duration of transport time (ground versus air) between the different levels of care. An important factor is the particular characteristics of the topography of the catchment area, which will help determine the ratio of ground-to-air transport resources required. In areas with good roads and low traffic volume, ground transport may be the only transport system required. 14,26,37,50 Selecting the proper mode of transport (ambulance, helicopter, or fixed-wing aircraft) depends on many variables including environmental conditions. Severity of disease and clinical status of the patient should guide the overall plan for mode of transport. In general, when transport time exceeds 2 hours, air transport is more appropriate. 37 However, local ground transport capabilities to-from a referring hospital and airport must be known when fixed-wing air transport is used.
Equipment and Medications
The equipment and medications necessary for neonatal transport are similar to those used in the NICU. Equipment must be light, compact, durable, and motion and g-force tolerant. All electronic equipment should have its own independent power supply (AC/DC capability), adequate visual and audio alarms, and lack of electromagnetic interference. 14,37Table 3-2 provides a list of common transport equipment and medications.
| CPAP, Continuous positive airway pressure; NS, normal saline; PGE, prostaglandin E; UAC, umbilical artery catheter; T-PICU, T-piece infant care unit. | ||||||
| *( ) designates numbers of pieces of equipment to be carried in transport kit. |
||||||
| Physiologic Monitoring and Safety | Airway and Suction Equipment | Respiratory Equipment | Procedure Equipment | Iv Fluid and Access | Medications | Refrigerated Medication |
|---|---|---|---|---|---|---|
| BP cuffs, #2-#4 (2 each) Electrodes (2 of each available size) Pulse oximeter probes (2) Dispensable thermometers (2) Skin temperature probes (8) Rectal probe (1) Warming pad portable: chemical (2) 4×4 gauze pads (2) Nonstick gauze pads (2) Bowel bag (1) Sterile rolled gauze (2) Ear protectors (2) Hats (2) Flashlight (2) Tape measures (2) |
Laryngoscope (2) Laryngoscope blades (2 of each size) Laryngoscope light bulbs (3) AA batteries (4) Endotracheal tubes (3 of each size) Stylettes (4) CO 2 detector (2 self-contained, sterile) Closed suction catheter (2 of each size) Meconium aspiration device (2) Bulb suction (2) Suction catheters (2 of each size) Saline bullets (4) Replogle (2 of each size) Orogastric tubes (2 of each size) |
Anesthesia bags (2 per T-PICU infant resuscitator) Self-inflating bag (2) Oxygen mask (2) Facemasks (2 of each size) Infant nasal cannula (2) CPAP prongs (2 of each size)Neonatal flow sensor (2) CPAP circuit (1) Ventilator circuit (1) Point-of-care blood gas equipment (1-2) |
Sterile towels (1) UAC tray (1) Single-lumen umbilical catheters (2 of each size) Double-lumen umbilical catheters (2 of each size) Umbilical tape (2) Povidone iodine (3) Scalpels #11 and #15 (1 each) 4.0 silk suture (4) Dressing for umbilical line (2) Needle aspiration/chest tube kit (2) Transducer (2) Chest tubes, 10 Fr/12 Fr (2 of each size) Heimlich valve (2) Sterile gloves (5 of each size) |
D 5W 50 mL (2) NS 250 mL (1) D 10W 500 mL (1) D 50W 50 mL (1) Heparin sodium 1000 mcg/mL vial (3) Syringes, 3 mL/1 mL (6 each) IV catheter, #22 and #24 gauge (5 each) Access kit, including dressing, tourniquet (2) Butterfly needle (3 of each size) Arm board (2) Heel warmers (2) Lancets (2 of infant and preemie size) Syringes (5 of each size) |
Epinephrine 1:10,000 (2) Naloxone 1 mg/ 1 mL (2)4.2% sodium bicarbonate (2) Dopamine (2) Dobutamine (2) Acyclovir (1) Ampicillin (2) Gentamicin (2) Vitamin K for injection (1) Eye ointment (2) Lidocaine HCl (1) Adenosine (1) Vecuronium (1) Sterile saline for injection (2) Abboject needle (2) Fentanyl (2) Midazolam (2) Phenobarbital (2) |
Exogenous surfactant (1) PGE (2) |
Novel Interventions
Because the objective of the perinatal transport team is to bring the intensive care environment to the newborn infant, it is fundamental that initial resuscitation and stabilization be performed by skilled practitioners in order for the team to successfully continue to offer appropriate high-quality intensive care during the transport of the baby. Level I and level II centers should be equipped with surfactant, nasal continuous positive airway pressure (NCPAP) systems, and oxygen-air blenders to give prompt and effective respiratory support while maintaining blood saturation levels within acceptable limits awaiting the arrival of the transport team. Adequate management of the premature infant with surfactant deficiency will include supporting adequate recruitment of the lung and minimizing barotrauma. Acquiring the requisite skills to intubate and administer surfactant appropriately and to administer early NCPAP has the potential to improve patient survival, decrease the need for mechanical ventilation,15,47,48,53,54and decrease morbidity in situations in which duration of transport may be prolonged for hours because of unforeseen delays. Although the use of NCPAP in the delivery room is not a novel intervention, 56 its use as an early intervention in the delivery room for infants with respiratory failure is accepted as a common approach for the management of premature infants with respiratory distress syndrome (RDS) and term infants with mild to moderate respiratory failure. Because surfactant is an expensive medication, level I and level II centers can maintain 1 or 2 ampules in their pharmacy to be restocked by the perinatal transport team before transport. The use of NCPAP during transport has also been evaluated recently and has been shown to be a safe and efficacious intervention for respiratory support. 39
The use of a resuscitation device such as the T-piece infant resuscitator (Neopuff™ Infant Resuscitator, Fisher & Paykel Healthcare) may help decrease the variability of pressures administered to the neonate during resuscitation, stabilization, or administration of surfactant. This device also has the potential to minimize lung damage while supporting lung recruitment with the use of positive end-expiratory pressure (PEEP). 9,43 This system can also temporarily replace the need for mechanical ventilation if NCPAP is unsuccessful in maintaining respiratory stability.
Another important intervention for perinatal transport is the administration of prostaglandin E 1 (PGE 1) in patients in whom a suspicion of congenital heart diseases is supported with a positive hyperoxia test. Adequate knowledge of dosing and preparation is fundamental to the successful use of this medication that can prevent patients with ductal dependent lesions from becoming clinically unstable and developing severe hypoxemia and metabolic acidosis before the arrival of the transport team. The need for intubation and ventilator support to prevent apnea varies depending on the anticipated length of transfer and the dose of PGE 1 necessary to maintain the infant asymptomatic. 10,21 Knowledge by the referring physician of the performance and interpretation of the hyperoxia test will facilitate the decision to start PGE 1 and should be part of the maintenance-of-skills program. We recommend that both level I and level II nurseries maintain in stock a vial of PGE 1.
In recent years, inhaled nitric oxide (iNO) has been used on transport to support term and near-term infants with hypoxemic respiratory failure that does not respond to conventional mechanical ventilation. 31 The use of this therapeutic gas can be lifesaving and may decrease associated morbidities. Its use during transport will require certain adaptations for both ground and air transport in order to use this gas safely and effectively. Another novel intervention is the use of whole-body cooling or head cooling during transport to minimize brain damage from severe hypoxic ischemic encephalopathy. The use of passive and active cooling before and during transport as a therapy for neonatal encephalopathy has been reported in the literature, but more studies are required to determine the safety and efficacy of this intervention. 5
Patients managed during transport with other more-complex interventions such as high-frequency jet ventilation (HFJV) and extracorporeal membrane oxygenation (ECMO) have been reported in the literature. Their use for routine transport cannot be recommended because of the complexity of training, equipment, and logistics required to administer these interventions. 13,38 Every country and regional perinatal center must determine its priorities for transport based on epidemiologic studies conducted in its catchment area to support the demand with appropriate resources for adequate perinatal transport.
FAMILY-CENTERED CARE FOR TRANSPORT
Separation of the infant and mother (parents) is often the consequence of neonatal transport. This physical separation affects both bonding and attachment, increasing the stress surrounding the delivery of an ill infant.28,32,51 Creative ways to minimize the negative impacts of this separation must be incorporated into the transport process.
Before departure from the referring facility, the transport team should meet with the parents of the infant, communicating the plan for transport, providing information with regard to the receiving hospital (to include phone numbers, directions, and unit-specific guidelines), and answering any questions the parents may have. The transport team should identify a phone number that may be used to communicate with the parents once the infant is transported. In addition, the transport team should enable the parents to see and touch the infant before departure and should provide the parents with a photograph of their infant.37
Upon arrival at the receiving medical center, a transport team member should call the parents to update them on the condition and the safe arrival of their baby in the receiving facility. At this time, the transport team should give the parents the names of those who will be responsible for the care of the infant. Once the infant is admitted into the receiving unit, the receiving physician should communicate directly with the parents and referring physician. Engaging the parents in the caregiving process as soon as possible empowers parents and assists the health care team in devising a care plan that will be mutually acceptable and in the best interest of the infant.
Facilitation of communication with parents may be improved with the use of video-telemedicine.24 This technology would enable the parents to see their infant in the receiving center and speak directly with the nurses or physicians caring for their infant.
FUTURE OF NEONATAL TRANSPORT
Research, innovation, and maintenance of regionalization represent the future for perinatal transport. The mandate for highly motivated leadership able to apply epidemiologic, research, and quality-improvement methodology to the area of perinatal transport is essential for progress. The development and evaluation of new interventions, as well as the evaluation of what we consider “standard therapies,” are imperative to better outcomes. The inclusion of continuous quality improvement at the top leadership level of the organizational structure of the perinatal transport system and the systematic collection of relevant data within an identified perinatal region represents the backbone for research in standing and new technologies. Special attention must be centered toward the community in order to improve resuscitation and stabilization efforts. In addition, benchmarking with regard to morbidity and mortality outcomes for transported patients will provide clarity for evaluation of the transport experience. The ultimate focus of this effort is to improve maternal and neonatal outcomes. Ultimate success will depend on the level of multidisciplinary participation of government, community, and private industry stakeholders.
REFERENCES
1. Abbrescia, K.; Sheridan, B., Complications of second and third trimester pregnancies, Emerg Med Clin N Am 21 (2003) 695.
2. American Academy of Pediatrics, Task Force on Interhospital Transport, In: (Editors: MacDonald, MG.; Ginzburg, HM.) Guidelines for air and ground transport of neonatal and pediatric patientsed 2 ( 1999)The Academy, Elk Grove Village, Ill.
3. American Academy of Pediatrics, American Heart Association, In: (Editor: Kattwinkel, J.) Textbook of neonatal resuscitationed 5 ( 2006)The Academy, Elk Grove Village, Ill.
4. American Academy of Pediatrics, American College of Obstetricians and Gynecologists, Interhospital care of the perinatal patient, In: Guidelines for perinatal careed 6 ( 2007)The Academy, Elk Grove Village, Ill.
5. Anderson, M.E.; Longhofer, T.A.; Phillips, W.; et al., Passive cooling to initiate hypothermia for transported encephalopathic newborns, J Perinatol 27 (2007) 592.
6. Annibale, D.J.; Cahill, J.B.; Tuttle, D.S.; et al., Preparation of the critically ill neonate for transport, J South Carolina Med Assoc 98 (2002) 129.
7. Arad, I.; Gofin, R.; Baras, M.; et al., Neonatal outcome of inborn and transported very-low-birth-weight infants: relevance of perinatal factors, Eur J Obstet Gynecol Reprod Biol 83 (1999) 151.
8. Bartels, D.B.; Wypij, D.; Wenzlaff, P.; et al., Hospital volume and neonatal mortality among very low birth weight infants, Pediatrics 117 (2006) 2206.
9. Bennett, S.; Finer, N.N.; Rich, W.; et al., A comparison of three neonatal resuscitation devices, Resuscitation 67 (2005) 113.
10. Browing-Carmo, K.A.; Barr, P.; West, M.; et al., Transporting newborn infants with suspected duct dependent congenital heart disease on low-dose prostaglandin E 1 without routine mechanical ventilation, Arch Dis Child Fetal Neonatal Ed 92 (2007) F117.
11. Chien, L.Y.; Whyte, R.; Aziz, K.; et al., Improved outcome of preterm infants when delivered in tertiary care centers, Obstet Gynecol 98 (2001) 247.
12. Cifuentes, J.; Bronstein, J.; Phibbs, C.S.; et al., Mortality in low birth weight infants according to level of neonatal care at hospital of birth, Pediatrics 109 (2002) 745.
13. Coppola, C.P.; Tyree, M.; Larry, K.; et al., A 22-year experience in global transport extracorporeal membrane oxygenation, J Pediatr Surg 43 (2007) 46.
14. Cornette, L., Contemporary neonatal transport: problems and solutions, Arch Dis Child Fetal Neonatal Ed 89 (2004) F212.
15. Dani, C.; Bertini, G.; Pezzati, M.; et al., Early extubation and nasal continuous positive airway pressure after surfactant treatment for respiratory distress syndrome among preterm infants < 30 weeks gestation, Pediatrics 113 (2004) e560.
16. Danzig, D., Neonatal transport teams: a survey of functions and roles, Neonatal Netw 3 (1984) 41.
17. Devoe, L.D., Antenatal fetal assessment: contraction stress test, nonstress test, vibroacoustic stimulation, amniotic fluid volume, biophysical profile, and modified biophysical profile—an overview, Semin Perinatol 32 (2008) 247.
18. Di Lieto, A.; De Falco, M.; Campanile, M.; et al., Regional and international prenatal telemedicine network for computerized antepartum cardiotocography, Telemed J E Health 14 (2008) 49.
19. Dobrez, D.; Gerber, S.; Budetti, P., Trends in perinatal regionalization and the role of managed care, Obstet Gynecol 108 (2006) 839.
20. Dupuis, O.; Gaucherand, P.; Mellier, G., et le Comité de pilotage de la cellule des transferts périnatals: Perinatal regional hotline organisation and rate of perinatal transfer: results from 2003 and 2004 in the French Rhône-alps area—a two year study of 4079 transfers, J Gynecol Obstet Biol Reprod 35 (2006) 702.
21. Ferrarese, P.; Marra, A.; Doglioni, N.; et al., Routine mechanical ventilation for transferred neonates with duct-dependent congenital heart disease, Arch Dis Child Fetal Neonatal Ed 92 (2007) F422.
22. Gerber, S.E.; Dobrez, D.G.; Budetti, P., Managed care and perinatal regionalization in Washington State, Obstet Gynecol 98 (2001) 139.
23. Gomez, M., Hiring, staffing, and team composition, In: (Editors: McClosky, K.; Orr, R.) Pediatric transport medicine ( 1995)Mosby, St Louis.
24. Gray, J.E.; Safran, C.; Davis, R.B.; et al., Baby CareLink: using the Internet and telemedicine to improve care for high-risk infants, Pediatrics 106 (2000) 1318.
25. Heller, G.; Richardson, D.K.; Schnell, R.; et al., Are we regionalized enough? Early-neonatal deaths in low-risk births by the size of delivery units in Hesse, Germany 1990–1999, Int J Epidemiol 31 (2002) 1061.
26. Hon, K.-L.E.; Olsen, H.; Leung, T.-F., Air versus ground transportation of artificially ventilated neonates: comparative differences in selected cardiopulmonary parameters, Pediatr Emerg Care 22 (2006) 107.
27. Kaluzny, A.D.; McLaughlin, C.P., Continuous quality improvement in health care: theory, implementation, and applications. ( 1994)Aspen Publishers, Gaithersburg, Md.
28. Karlsen, K., The S.T.A.B.L.E. Program: post-resuscitation/pre-transport stabilization care of sick infants—guidelines for neonatal healthcare providers. ed 5 ( 2006)S.T.A.B.L.E., Inc, Park City Utah.
29. King, B.R.; Foster, R.L.; Woodward, G.A.; et al., Procedures performed by pediatric nurses: how “advanced” is the practice?Pediatr Emerg Care 17 (2001) 410.
30. King, B.R.; King, T.M.; Foster, R.L.; et al., Pediatric and neonatal transport teams with and without a physician, Pediatr Emerg Care 23 (2007) 77.
31. Kinsella, J.P.; Schmidt, J.M.; Griebel, J.; et al., Inhaled nitric oxide treatment for stabilization and emergency medical transport of critically ill newborns and infants, Pediatrics 95 (1995) 773.
32. Klaus, M.H.; Kennell, J.H., Maternal-infant bonding: the impact of early separation or loss on family development. ( 1976)Mosby, St Louis.
33. Ledger, W.J., Identification of the high risk mother and fetus: does it work?Clin Perinatol 6 (1980) 125.
34. Lee, S.K.; Zupanic, J.AF.; Pendray, M.R.; et al., Transport risk index of physiologic stability: a practical system for assessing infant transport care, J Pediatr 139 (2001) 220.
35. Lee, S.K.; Zupancic, J.AF.; Sale, J.; et al., Cost-effectiveness and choice of infant transport systems, Med Care 40 (2002) 705.
36. Lui, K.; Abdel-Latif, M.E.; Allgood, C.L.; et al., The New South Wales and Australian Capital Territory Neonatal Intensive Care Unit Study Group: Improved outcomes of extremely premature outborn infants: effects of strategic changes in perinatal and retrieval services, Pediatrics 118 (2006) 2076.
37. Lupton, B.A.; Pendray, M.R., Regionalized neonatal emergency transport, Semin Neonatol 9 (2004) 125.
38. Mainali, E.S.; Greene, C.; Rozycki, H.J.; et al., Safety and efficacy of high-frequency jet ventilation in neonatal transport, J Perinatol 27 (2007) 609.
39. Murray, P.G.; Stewart, M.J., Use of nasal continuous positive airway pressure during retrieval of neonates with acute respiratory distress, Pediatrics e754 (2008) 121.
40. Nabhan, A.F.; Abdelmoula, Y.A., Amniotic fluid index versus single deepest vertical pocket as a screening test for preventing adverse pregnancy outcome, Cochrane Database Syst Rev 3 (2008); CD006593, DOI:10.1002/14651858.CD006593.pub2.
41. Neto, M.T., Perinatal care in Portugal: effects of 15 years of a regionalized system, Acta Paediatr 95 (2006) 1349.
42. Niermeyer, S.; , the contributors and reviewers for the Neonatal Resuscitation Guidelines, International guidelines for neonatal resuscitation: and excerpt from the guidelines 2000 for cardiopulmonary resuscitation and emergency cardiovascular care— international consensus on science, Pediatrics 106 (2000) e29; Accessed July 11, 2009, fromwww.pediatrics.org/cgi/content/full/106/3/e29.
43. Oddie, S.; Wyllie, J.; Scally, A., Use of self-inflating bags for neonatal resuscitation, Resuscitation 67 (2005) 109.
44. Pedersen, N.G.; Figueras, F.; Wojdemann, K.R.; et al., Early fetal size and growth as predictors of adverse outcome, Obstet Gynecol 112 (2008) 765.
45. Phibbs, C.S.; Baker, L.C.; Caughey, A.B.; et al., Level and volume of neonatal intensive care and mortality in very-low-birth-weight infants, N Engl J Med 356 (2007) 2165.
46. Philpot, C.; Day, S.; Marcdante, K.; et al., Pediatric interhospital transport: diagnostic discordance and hospital mortality, Pediatr Crit Care Med 9 (2008) 15.
47. Reininger, A.; Khalak, R.; Kendig, J.W.; et al., Surfactant administration by transient intubation in infants 29 to 35 weeks’ gestation with respiratory distress syndrome decreases the likelihood of later mechanical ventilation: a randomized control trial, J Perinatol 25 (2005) 703.
48. Rojas, M.A.; Lozano, J.M.; Rojas, M.X.; et al., For the Colombian Neonatal Research Network: Very early surfactant without mandatory ventilation in premature infants treated with early continuous positive airway pressure: a randomized control trial, Pediatrics 123 (2009) 137.
49. Skeoch, C.H.; Jackson, L.; Wilson, A.M.; et al., Fit to fly: practical challenges in neonatal transfers by air, Arch Dis Child Fetal Neonatal Ed 90 (2005) F456.
50. Svenson, J.E.; O’Connor, J.E.; Lindsay, B., Is air transport faster? A comparison of air versus ground transport times for interfacility transfers in a regional referral system, Air Med J 24 (2003) 170.
51. Taylor, R.M.; Price-Douglas, W., The S.T.A.B.L.E. Program post-resuscitation/pretransport stabilization care of sick infants, J Perinat Neonat Nurs 22 (2008) 159.
52. Tsai, S.H.; Kraus, J.; Wu, H.-R.; et al., The effectiveness of video-telemedicine for screening of patients requesting emergency air medical transport (EAMT), J Trauma 62 (2007) 504.
53. Verder, H.; Albertsen, P.; Ebbeson, F.; et al., Nasal continuous positive airway pressure and early surfactant therapy for respiratory distress syndrome in newborns of less than 30 weeks’ gestation, Pediatrics 103 (1999) e24.
54. Verder, H.; Robertson, B.; Greisen, G.; et al., Surfactant therapy and nasal continuous positive airway pressure for newborns with respiratory distress syndrome, N Engl J Med 331 (1994) 1051.
55. Woodward, W.GA.; Insoft, R.M.; Pearson-Shaver, A.L.; et al., The state of pediatric interfacility transport: consensus of the second national pediatric and neonatal interfacility transport medicine leadership conference, Pediatr Emerg Care 18 (2002) 38.
56. Wung, J.T.; Driscol Jr, J.M.; Epstein, R.A.; et al., A new device for CPAP by nasal route, Crit Care Med 3 (1975) 76.
57. Yu, V.Y.; Doyle, L.W., Regionalized long-term follow-up, Semin Neonatol 9 (2004) 135.