Chapter 29 Performance of Rigid Bronchoscopy
I Historical Background
Rigid bronchoscopy is an invasive surgical technique that is used to visualize the oropharynx, larynx, vocal cords, trachea, and proximal pulmonary branches. The origins of rigid bronchoscopy, like many aspects of modern medicine, can be traced back to Hippocrates (460-370 BC), who advised introducing a pipe into the larynx in a suffocating patient to assess the airways.1 Because of limitations with lighting, the field was largely dormant until the 1800s, when incandescent light bulbs were invented. The development of local anesthesia in 1880 also made bronchoscopy more tolerable. In March of 1897, Gustave Killian passed an endoscope through the larynx and removed a piece of pork bone from the right main stem bronchus using cocaine anesthesia.1 Chevalier Jackson further advanced the field of rigid endoscopy by developing improved lighting, auxiliary instrumentation for removal of foreign objects, and rigid bronchoscopy training programs.2 He is recognized as the father of contemporary rigid endoscopy.3 Since Jackson’s time, many changes have been made to the bronchoscope, so that current rigid instrumentation and ventilation systems allow for more precise and accurate assessment of the aerodigestive tract.3 H. H. Hopkins of England invented the first conventional lens system by using glass rods instead of small lenses, which produced a significantly brighter image, occupied less space, and allowed for greater visualization of an object in a single field.1 This provided the basis for fiberoptic and modern rigid bronchoscopy.
II Indications and Contraindications
The tracheobronchial tree can be directly observed with either rigid or flexible bronchoscopy. Although the advent of flexible bronchoscopy has given physicians improved access to more distal portions of the tracheobronchial tree with a more rapid learning curve and less patient discomfort compared with rigid bronchoscopy,2 there are still several situations in which rigid bronchoscopy is more appropriate. The larger working port and rigid structure make rigid bronchoscopy useful for surgical interventions within the airway, such as the removal of foreign bodies or polyps (see “Foreign Body Removal”).4 At the same time, the bronchoscope can be used in establishing and maintaining airway control in patients with difficult ventilation, such as those with an acute airway obstruction or massive hemoptysis.4 The major advantage of the rigid bronchoscope compared to the flexible one is that it has a ventilation port that can be directly connected to the anesthesia ventilator, allowing for maintenance of an airway and external ventilation while airway procedures are performed. In fact, the latest practice guidelines for the management of a difficult airway (DA) include the use of rigid bronchoscopy because it “reduces airway-related adverse outcomes.”5
Other instances in which rigid bronchoscopy is indicated include deeper diagnostic biopsies when a fiberoptic specimen would be inadequate; dilatation of strictures; bronchial stenting; fracture reduction; application of laser therapy or cryotherapy; tumor removal; and diagnosis of vascular rings. Some of the indications for pediatric rigid bronchoscopy are listed in Box 29-1.
Box 29-1
Indications for Rigid Bronchoscopy
Foreign body evaluation and management
Interval evaluation after laryngotracheal reconstruction
Management of severe laryngotracheal infections
Assessment of toxic inhalation or aspiration
Evaluation of laryngeal pathology
Management of mass lesions of the airway, including recurrent respiratory papillomatosis
Adapted from Hartnick CJ, Cotton RT: Stridor and airway obstruction. In Bluestone CD, Stool DE, Alper CM, et al (eds): Pediatric otolaryngology, ed 4, Philadelphia, 2003, Elsevier.
There are few contraindications to rigid bronchoscopy. In practice, most of the factors limiting rigid bronchoscopy are related to the general anesthesia used, such as an unstable cardiovascular or respiratory status.6 One absolute contraindication to rigid bronchoscopy is an unstable cervical spine, because of the hyperextension of the head required during the procedure. In this instance, flexible bronchoscopy is indicated to avoid any further spinal injury during bronchoscopy. Other contraindications include laryngeal stenosis that prevents passage of the bronchoscope; limited range of motion of the mandible; severe kyphoscoliosis; uncontrolled coagulopathy; and extreme ventilatory/oxygenation demands.7,8
III Instrumentation
The Storz endoscope with the Hopkins rod-lens optical system, introduced in 1966, is the most widely used rigid bronchoscope and has largely replaced the Jackson and Holinger endoscopes.9 As described earlier, the rod-lens system provides better illumination, greater visualization, and angled views. The bronchoscope is a hollow, rigid metal tube that is tapered and beveled on the distal end and has a series of different-sized ports on the proximal end that serve different purposes. There are side holes at the end of the bronchoscope to allow for ventilation proximal to the tip.10 The beveled edge of the tip is used to facilitate introduction of the bronchoscope into the airway and for resection of tumors. The inferior port is usually the ventilating port connected to the anesthesia circuit. The superior port connects to the prismatic light deflector and the light source (Figs. 29-1 and 29-2). The main port is the working channel for aspiration and for insertion of instruments such as telescopes, biopsy forceps, laser fibers, balloon devices, cryotherapy probes, and stents. The port can be left open to allow room air into the system or it can be closed to prevent leakage of air or anesthetic gases, depending on the ventilation and type of anesthesia being used.
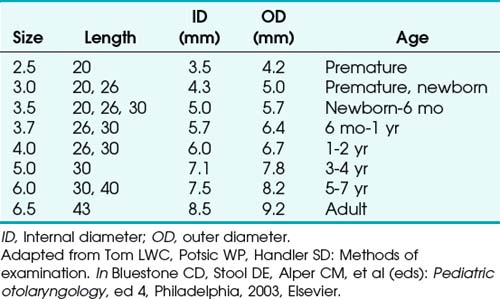
Bronchoscopes vary in size, in length, and in internal and external diameter. Table 29-1 depicts the different sizes of Storz bronchoscopes used by patient age, although this choice needs to be tailored to the individual patient. The size chosen should maximize the surgeon’s view while causing the least trauma to the airway.9 Telescopes with different angles (0, 30, and 70 degrees), lengths, and diameters can be inserted through the main working port to visualize areas that are difficult to see with the rigid bronchoscope alone, namely the right and left upper bronchial orifices and the right middle bronchial orifice.9 Illumination can be provided either through a light carrier rod that goes down a channel in older endoscopes, through the telescope, or by means of a port that attaches to a prismatic light deflector which subsequently attaches to a light source in newer endoscopes (Figs. 29-3 and 29-4). The last configuration has the advantage that it provides both proximal and distal illumination.
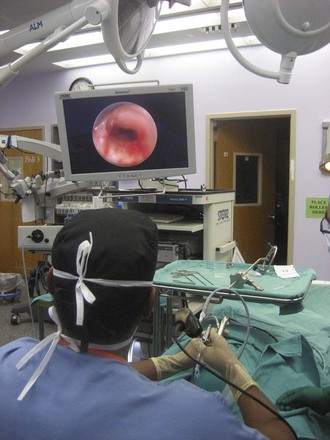
Rigid bronchoscopy should be performed either in an operating room (OR) or an endoscopy suite. As with all procedures that require general anesthesia, the room should be equipped with equipment for oxygen (O2) saturation monitoring, carbon dioxide (CO2) monitoring, blood pressure monitoring, and electrocardiography. A full set of ventilating bronchoscopes (see Table 29-1 for sizes) and a backup light source should be available. The standard adult size rigid bronchoscopy is 8 mm in diameter and 40 cm long. Other instruments such as graspers, biopsy forceps, optical forceps, and suction devices should also be available to the surgeon (Fig. 29-5). Optional items include a flexible bronchoscope that can be passed through the rigid bronchoscope for further examination of the lower tracheobronchial tree. Video capability is also desirable but not required (Fig. 29-6).
IV Preoperative Considerations
A thorough history should be taken to assess previous cardiac disease, such as a recent myocardial infarction or any documented dysrhythmias, or pulmonary disease (e.g., asthma) that may require bronchodilators before bronchoscopy.4 To minimize the risk of bleeding, the patient should have a normal platelet count, prothrombin time, and partial thromboplastin time. Unless a bleeding history is known, a preoperative coagulation workup is not necessary. Because patients with uremia have qualitative platelet abnormalities that can predispose to excessive bleeding, creatinine and blood urea nitrogen values should be relatively normal.4 Patients should also be questioned about aspirin or anticoagulant use and timing of the last intravenous dose. Additional laboratory studies and tests may be ordered depending on the history.
Pulmonary function tests are no longer indicated as routine preoperative assessment of respiratory disease but may be useful for determining the postoperative plan.11 For example, patients with a forced vital capacity (FVC) of less than 20 mL/kg is at an increased risk for pulmonary complications postoperatively and may benefit from extended postoperative monitoring.10 Also, patients with forced expiratory volumes of less than 50% are at risk for hypercarbia and hypoxia.12 The clinical predictors of cardiac complications perioperatively or postoperatively with major risk are unstable or severe angina, decompensated congestive heart failure, significant dysrhythmias, and severe valvular disease.13 Cardiac conditions should be evaluated and the medical therapies optimized before the surgery. Perhaps the simplest way to assess the patient’s overall cardiopulmonary status is to inquire about exercise tolerance.
Often, rigid bronchoscopy is performed emergently with limited preoperative evaluation or testing in order to secure an airway, and knowledge and assessment of risk factors for cardiopulmonary mortality, difficult intubation (DI), and difficult mask ventilation (DMV) may be of importance for perioperative and postoperative management. DI may be predicted by weight, head and neck movement, jaw movement, receding mandible, “buck” teeth, Mallampati classification, thyromental distance, sternomental distance, and a history of DI.5,14,15 There are five independent risk factors for DMV: age greater than 55 years, body mass index greater than 26 kg/m2, presence of a beard, lack of teeth, and a history of snoring.14 A careful evaluation of the patient’s jaw and neck mobility should be made, because severe cervical spine disease is a contraindication to rigid bronchoscopy.
V Anesthesia for Bronchoscopy
Traditionally in the pediatric population, inhalational anesthesia with spontaneous respiration has been used during rigid bronchoscopy, often with switching to a total intravenous anesthetic technique after induction. Disadvantages of inhalational anesthesia with spontaneous respiration include difficulty in maintaining an adequate plane of anesthetic depth and the anesthetic pollution of the surgical environment from a gas leak around the bronchoscope.16 Malherbe and colleagues proposed total intravenous anesthesia with propofol and remifentanil and spontaneous respiration as a reasonable alternative to deep inhalational anesthesia that carries no major complications.16 In the spontaneous respiration technique, the patient is not given an NMB agent and is allowed to breathe spontaneously. The ventilating port of the bronchoscope is attached to the anesthesia circuit with 100% O2 flow (see Fig. 29-1). The advantage of spontaneous ventilation is that it allows for continuous ventilation during the procedure; the main disadvantage is that the depth of anesthesia required for the procedure itself may suppress both cardiac output and the respiratory drive, making spontaneous respirations difficult.17 Another potential disadvantage is that the instrumentation required for the procedure itself provides increased airway resistance and may reduce the efficacy of spontaneous respirations.18
When PPV is used, it is typically achieved by first relaxing the patient with an NMB agent and subsequently connecting the ventilating port of the bronchoscope to the anesthesia circuit. Positive pressure is administered by squeezing the bag or by using the anesthesia ventilator, forcing gas pressure through the rigid bronchoscope.19 Advantages include the prevention of atelectasis, improved oxygenation, and the ability to overcome the increased airway resistance caused by the instrumentation within the rigid bronchoscope.18 A disadvantage to PPV is that a proximal eyepiece must be in place, which hinders the use of suction or other instrumentation during ventilation.20 There is also usually some gas leak during PPV due to the absence of a tight seal, decreasing efficiency. Finally, the size of the bronchoscope and the presence of a telescope in the lumen increases resistance to airflow and increases dead space ventilation, making ventilation more difficult.
In apneic oxygenation, there are periods of time when the anesthesiologist withholds ventilation during which the surgeon works. The patient is first hyperventilated to produce a profound hypocarbia. Under direct visualization, a catheter is then passed to the carina, and the flow rate of O2 is set. The period of time in which the surgeon can work is determined by the rise in CO2, after which the patient is allowed an equivalent amount of time during the next ventilation cycle to return to baseline. The partial pressure of CO2 (PCO2) is expected to rise continuously at a rate of 3 mm Hg per minute.10 This technique is risky when it is used in patients who have a history of CO2 retention (e.g., COPD), and intraprocedural awareness is also reported more frequently with this technique.
Jet ventilation is usually used during laser procedures, and it is provided by use of a jet-ventilator with a jet injection cannula (JIC), also known as a Saunders injector.21 This technique is used to overcome the hypoventilation caused by air leaks during PPV.22 The cannula has three lumens, two of which open proximally and deliver the jet ventilation; a distal lumen measures airway pressure.21 The JIC is 3 mm in diameter, can have various lengths, and is made of stainless steel and therefore has a lower risk of endotracheal ignition.21,22 The JIC is usually introduced distal to the lesion being accessed to provide optimal ventilation. High-pressure O2 (50 psi) is delivered to the airway at high velocities, creating a negative pressure and causing a Venturi effect.16 The negative pressure caused by the high velocity of air entering the airways induces a column of air from outside the injector to flow into the airways and expand the lungs. Exhalation is passive and relies on the collapse of the airway once the pressure is removed. Sufficient time must be allotted for air egress during this technique to prevent stacked breaths and progressive hyperinflation. This method is contraindicated during foreign body removal, because the high-flow air may dislodge the foreign body and cause a complete obstruction.18 Of note, jet ventilation does not prevent acidemia or hypercarbia and may increase the risk of air embolism, pneumothorax, and particle dissemination into the lungs and distal airways.20 Also, in patients with poor lung compliance, ventilation may be inadequate with this technique.10
NPV, compared with spontaneous assisted ventilation, reduces the administration of opioids, shortens recovery time from anesthesia, and prevents hypercarbia.20 It can be accomplished by a poncho-wrap connected to a negative-pressure ventilator, with a 2-L/min O2 flow, negative pressure of −25 hectopascals (hPa), a respiratory rate of 15 breaths/min, and an inspiration/expiration ratio of 1 : 1. NPV may be safer in patients with poor tolerance to hypercarbia, such as patients with myocardial ischemia.20
Intravenous and topical medications can be used provided the patient’s history reveals no prior adverse reactions or if the potential benefit outweighs the expected risks. Opioids are often used for analgesia, for sedation, and to decrease the cough reflex. However, because they depress the respiratory drive, they should be withheld from patients who have signs of airway obstruction or a foreign body. A recent study by Yoon and colleagues comparing propofol sedation to a combination of both propofol and alfentanil showed that the propofol-only group had a higher average oxygen saturation as measured by pulse oximetry (SpO2; 97.8 ± 1.6 versus 96.4 ± 1.1, P < 0.01). The degree of cough (measured using a 100 mm visual analogue scale), however, was not different between the groups (73.4 ± 22.7 versus 72.2 ± 18.5, respectively). This may be partially attributed to the intrinsic antitussive properties of propofol. Therefore, narcotics may not be required if the patient is being induced with propofol.23
Anticholinergics are often used to reduce airway secretions and have been shown to enhance the absorption and prolong the analgesic action of topical analgesics such as lidocaine which are administered to the airways to reduce reactivity, prevent bronchospasm, and dampen the systemic reaction to airway manipulation.24 Intravenous anticholinergics are also commonly used to prevent the parasympathetic-mediated bradycardia and hypotension that can occur during rigid bronchoscopy.11 Their routine use remains debated.25 A steroid such as dexamethasone can be used to decrease intraoperative and postoperative edema that can result from airway instrumentation.
For emergence from anesthesia, all anesthetic gases are turned off, NMB agents are reversed, and the patient is ventilated until spontaneous respirations resume. Topical lidocaine may again be administered to prevent laryngospasm and diminish coughing.12
VI Surgical Technique
The surgeon should ensure that the necessary instrumentation is available before rigid bronchoscopy is initiated. In pediatric bronchoscopy, the size of the bronchoscope needed can be approximated by the patient’s age, or by size of an appropriate endotracheal tube (see Table 29-1). In all patients, bronchoscopes one or two sizes smaller than the preselected one should be available in case the airway encountered is smaller than anticipated.9 The surgeon should also select the appropriate size of instruments that will be used during the procedure, such as laryngoscopes, telescopes, endotracheal tubes, forceps, and suctions, and ensure that they are functioning properly. Teeth should be protected with rubber guards or with damp gauze, and the eyes should be protected with lubricant and tape.4,12
After informed consent for the procedure is obtained, the patient is taken to the OR or endoscopy suite. In pediatric bronchoscopy, the child should be positioned with the neck flexed on the body and the head extended at the neck.9 This position is sometimes called the “sniffing” position, and is used to position the trachea anteriorly.4 A shoulder roll to elevate the shoulders and a foam donut to stabilize the head are usually placed in older children; in younger children, a small donut for the head is sufficient. The goal is to align the oral, pharyngeal, and tracheal axes to facilitate insertion of the bronchoscope.
The anesthesiologist may induce anesthesia with either mask ventilation or intravenous agents, after which the surgeon begins the endoscopy by examining the oral cavity, oropharynx, and supraglottic larynx.12 The vocal cords are identified and may at this point be sprayed with a topical agent such as lidocaine to diminish airway reactivity and laryngospasm. In pediatric bronchoscopy, especially in cases of airway obstruction due to a foreign object, a slotted laryngoscope can be used in combination with a telescope to examine the larynx and the airway before the rigid bronchoscope is inserted, because there is a possibility of dislodging the foreign object and causing a complete obstruction during the introduction of instruments.12 O2 can also be insufflated via a flexible large-bore catheter into the laryngeal inlet during the preliminary examination to allow the surgeon additional time to work in the airway (Fig. 29-7).12
Whereas in older children and adults the bronchoscope may be advanced directly into the trachea without laryngoscopic assistance, in younger children it is easiest and safest to use a laryngoscope to guide the rigid bronchoscope.9 The laryngoscope is introduced in the usual fashion into the vallecula until the glottis is in the field of vision. The rigid bronchoscope is then introduced within or adjacent to the lumen of the laryngoscope down to the level of the true vocal cords.9 If the vocal cords are not open, then the patient is not sufficiently relaxed, and additional intravenous anesthetic or NMB agent should be given.3 The rigid bronchoscope is then rotated 90 degrees to align the leading edge with the axis of the vocal cords as the bronchoscope passes through the glottic opening into the subglottis. This provides the path of least resistance and minimizes the risk of glottic damage.7 A simple twisting motion may be required to advance the bronchoscope into the subglottic area.9 Once it is distal to the glottis, it can be rotated back 90 degrees to its original orientation. Although the beveled tip of the rigid bronchoscope is conventionally directed anteriorly, some surgeons advocate placing the tip along the posterior wall of the trachea to prevent damage to the membranous trachea.8
In older children, adolescents, and adults, laryngoscopy is not always required. The patient’s maxilla is grasped with the left hand while at the same time support is provided for the rigid bronchoscope, and the dentition is protected by the thumb of the surgeon’s nondominant hand.4,9 The bronchoscope is passed into the oral cavity in a plane perpendicular to that of the patient, and the posterior pharynx can be visualized. The bronchoscope is then rotated to a plane parallel with the airway axis. After visualization of the epiglottis, the tip of the bronchoscope is used to displace the epiglottis and tongue anteriorly. This maneuver requires gentle rocking of the bronchoscope on the thumb (not on the teeth) and brings the vocal cords into the field of vision.4 Once the vocal cords are in view, the glottis can be approached and the subglottis may be entered, as previously described.9
For the intubated patient, the rigid bronchoscope may be advanced alongside the tube and then passed through the glottic opening as the tube is removed under direct visualization. If the patient has had the larynx surgically removed or closed, the rigid bronchoscope should be placed only through the laryngostoma.8
Once the bronchoscope has been successfully introduced into the trachea, the “sniffing” position can be converted to cervical hyperextension by removing the supporting pillow and donut from under the head and by lowering the headboard to extend the neck.4,26 This maneuver is typically used in adults. The nondominant hand then holds the bronchoscope while the dominant hand is used for instrumentation of the airway for the duration of the procedure.4 If any resistance is felt during the procedure, the surgeon should always reevaluate the patient’s head and positioning, jaw opening, and bronchoscope size as well as ensuring that the patient’s lips are not caught. At this point, the anesthesia circuit can be attached to the bronchoscope through the side port, and the catheter with O2 flow can be removed (Fig. 29-8). Unless total intravenous anesthesia is being used, the lens cap to the main working port should be on to prevent leakage of anesthetic gas through the proximal end of the bronchoscope.
Before any intervention, an initial examination of the airway is performed. The subglottis and trachea are examined, and any masses or mucosal discolorations should be thoroughly investigated.9 Even after premedication with an anticholinergic agent, secretions are frequently encountered during the bronchoscopy and can be suctioned by introducing a rigid or flexible suction cannula into the main working port. This or any other rigid instrumentation of the airway allows for escape of anesthetic gases into the OR environment and results in a loss of the closed anesthesia circuit. Flexible suction catheters can be used through a smaller side port to prevent the loss of the closed anesthesia circuit.12
Care must be taken not to suction the airways excessively, because this may lead to mucosal edema and inflammation and worsen the respiratory status of the patient. This effect can be mitigated by premedicating the patient with a steroid such as dexamethasone. The bronchoscope is then advanced to the level of the carina. The appearance and movement of the carina are noted during respirations. Decreased movement of the carina can be an indicator of hilar lymphadenopathy.9 In order to advance the rigid bronchoscope to the main stem bronchus, the head should be slightly turned to the side opposite the intended bronchus. The distal airways may be evaluated by inserting different-angled telescopes to view the tracheobronchial tree. The 30- and 90-degree telescopes are especially useful to examine the segmental orifices of the upper lobes, in particular the right upper lobe, which is in a difficult location.3,7 The distal tracheobronchial tree can also be examined by inserting the flexible bronchoscope through the rigid bronchoscope.7
After the preliminary evaluation of the airway is completed, the planned procedure is performed (see later discussion). For diagnostic bronchoscopy, the bronchial brushings, washings, and biopsies are performed, in that order.3 If any bleeding is encountered, it can be controlled with electrocautery or local application of epinephrine, oxymetazoline, or phenylephrine.3 Phenylephrine may result in pulmonary edema or cardiac depression and should be used very cautiously. This emphasizes the need for constant communication between the anesthesiologist and the surgeon during rigid bronchoscopy. The procedure must be paused periodically and the working port sealed to minimize leakage of anesthetic gases into the OR environment and to allow for adequate ventilation. After the procedure is completed, the secretions should be thoroughly suctioned to prevent atelectasis.12 Once the anesthesiologist has prepared for postbronchoscopy ventilation, the bronchoscope can be removed under direct vision if O2 saturation is greater than 90%.3,12 Bronchospasm and temporary hypoxia are not uncommon after withdrawal of the bronchoscope, and the anesthesiologist must be ready to support ventilation via mask ventilation or endotracheal intubation until spontaneous ventilation resumes.3,12
VII Complications
The complications that may occur during or after rigid bronchoscopy can often be avoided by a thorough preoperative evaluation and proper technique.3 These include damage to dentition, arytenoid dislocation, respiratory depression, laryngospasm, bronchospasm, subglottic edema, hypoxia, dysrhythmias, mucosal or parenchymal bleeding, perforation, pneumothorax, pneumomediastinum, and death.3,9,27 In pediatric rigid bronchoscopy, the complication rates range from 1.9% to 4%.27 In adults, Lukomsky and associates reported a complication rate of 5%,28 whereas Drummond and coworkers reported a rate of 13.4%.29 Patients with an increased preoperative risk, neoplastic disease, presence of a foreign body, or carinal involvement should be monitored closely, because these conditions are particularly associated with an increased complication rate in adults.29 The three risk factors identified by Hoeve and colleagues for an increased complication rate in children are a history of tetralogy of Fallot, need for biopsy or drainage of a lesion during bronchoscopy, and a history of foreign body aspiration.27
It is imperative that patients be evaluated pre-operatively for poor dentition, because loose teeth are at risk for damage or dislodgement during the procedure. If cervical spine disease with a contracted neck is present, rigid bronchoscopy may not be safely performed; a limited range of cervical motion precludes safe advancement of the scope into the airway, resulting in complications ranging from dental injury to perforation of the posterior pharynx, membranous trachea, or distal airway.26 Such perforation of the airway may result in pneumomediastinum or pneumothorax but can be avoided by choosing an alternative method for examining the airway (e.g., flexible bronchoscopy) in susceptible patients.16
Hemorrhage can occur during bronchoscopy, especially during deep tissue biopsies. It may be controlled by use of the bronchoscope to apply pressure to the bleeding site, thorough suction, local application of epinephrine, or intravenous vasopressin. The patient’s greatest danger when this occurs is aspiration rather than hemorrhagic shock.27
Bronchospasm and laryngospasm occasionally occur intraoperatively. Their incidence can be reduced by maintaining an adequate anesthetic plane and by the topical application of a local anesthetic, such as lidocaine. Other agents, including opioids and beta-blockers, can be used to blunt the hemodynamic response to airway stimulation.16
Late complications include airway edema, pneumothorax, and atelectasis.12 Laryngeal edema is usually more serious in children, because their airway lumen is smaller and resistance increases exponentially with any airway swelling.12 This condition can be improved with the administration of humidified O2, racemic epinephrine, and steroids. If the patient does not respond to medical management, endotracheal intubation may be necessary. Laryngeal edema may be reduced by premedicating the patient with intravenous steroids.16 In cases of Venturi ventilation or high ventilation pressures, pneumothorax may result from barotrauma.10,12
Rigid bronchoscopy requires excellent communication between the anesthesiologist and the surgeon. Failure to communicate may lead to inadequate control of the airway and can result in hypercarbia, hypoxemia, or death, especially in patients with impending complete airway obstruction.26 This can be prevented by having all parties involved in the surgery familiarize themselves with the procedure before starting. A contingency plan must be in place in the event the airway is lost. This may entail preparation for tracheostomy or ventilatory bypass in an absolute emergency.
VIII Foreign Body Removal
The removal of aspirated foreign bodies remains one of the main indications for rigid bronchoscopy, especially in children, in whom the use of flexible bronchoscopy is comparatively risky. In 2006, the total number of deaths caused by aspiration or ingestion of foreign objects, including food, totaled 3981.30 Most deaths resulting from foreign body aspiration occur before hospital arrival.31 The incidence of foreign body aspiration peaks in older infants and toddlers, with 74% of cases occurring in children younger than 3 years of age.32 The male-to-female ratio is about 2 : 1 in children.32 In adults, the peak incidence occurs in the sixth decade of life.33
The clinical progression of foreign body aspiration occurs in three stages. The initial stage is usually characterized by a choking episode followed by coughing, gagging, and even obstruction of the airway.32 In a series of 100 cases published by Barrios and coworkers, the history of a choking crisis was the clinical parameter with the highest sensitivity (97%) and also had a fair specificity (63%).34 Chest radiographs may appear normal, and symptoms can be minimal.31,34 In cases of suspected foreign body aspiration, rigid bronchoscopy remains the gold standard for both diagnosis and treatment. Whereas atelectasis is more common in adults, air trapping is more common in children.33 The location of the foreign object also differs between adults (right bronchial tree) and pediatric patients (central airway). The second stage is usually asymptomatic, because the initial symptoms resolve due to a fatigued cough reflex.32 As many as 50% of initial presentations of foreign body aspiration go undiagnosed for longer than 7 days,29 and this is more likely to occur in an adult.33 The third stage indicates a complicated foreign body aspiration, which can be associated with pneumonia, hemoptysis, bronchiectasis, chronic cough, lung abscess, fever, or malaise.32
Radiographic evaluation includes anteroposterior and lateral views of the extended neck and chest. It is imperative that both inspiratory and expiratory views be obtained whenever possible to evaluate for unilateral air trapping.32 The four main types of obstruction at a bronchial orifice are bypass valve obstruction, check valve obstruction, stop valve obstruction, and ball valve obstruction.32 In bypass valve obstruction, the obstruction is incomplete and will result in a normal radiographic evaluation. In check valve obstruction, commonly seen acutely, the foreign body permits air flow into the lung segment but blocks the air flow out of the lung segment. This results in a mediastinal shift away from the obstruction on an expiratory film. Stop valve obstruction is seen when a foreign body has been present for an extended period; it is characterized by no airflow into, and subsequent collapse of, the affected lung segment. The rarest type of obstruction, the ball valve type, permits airflow out of the lung segment but not into it. This phenomenon results in atelectasis and a mediastinal shift toward the obstructed segment on an expiratory film. Other studies (e.g., fluoroscopy, videofluoroscopy) have been used when the diagnosis is uncertain.31,32
The management of an aspirated foreign body depends on the clinical picture. If an acute complete obstruction is suspected, rigid bronchoscopy must be performed promptly. More frequently, however, the patient presents in the second or third stage, when there is adequate time to plan a successful and safe bronchoscopy. If possible, the procedure should be scheduled when experienced personnel are available, the instruments have been appropriately selected, and the child is fasted appropriately to prevent aspiration of gastric contents.19,32 Advanced planning for the procedure includes determining the nature of the foreign object to guide the selection of instruments for its retrieval.
Controversy remains regarding the anesthetic approach during bronchoscopy for foreign body aspiration. Those who advocate spontaneous ventilation argue that PPV may precipitate an acute obstruction with clinical deterioration,18,32 whereas others advocate controlled ventilation with NMB to prevent the patient from moving and decrease the probability of airway trauma. A retrospective series of 94 cases showed no difference in adverse events with either ventilatory management approach,18 whereas a prospective study by Chen and colleagues consisting of 384 children found that patients managed with total intravenous anesthesia and spontaneous ventilation had increased intraoperative body movement, longer duration of emergence from anesthesia, lower percentage of successful foreign body removal, and more postoperative laryngospasm.35 Chen’s study also identified five risk factors for intraoperative hypoxemia (SpO2 ≤ 90%): younger age, plant seed as the type of foreign body, longer operative time, presence of pneumonia before procedure, and spontaneous ventilation. Manual jet ventilation was found to decrease the risk of intraoperative hypoxemia. The factors associated with postoperative hypoxemia were plant seed as the foreign object and prolonged emergence from anesthesia. Patients with these characteristics should be closely monitored after the procedure.
If the foreign body is small enough, it can be removed through the lumen of the main working port. However, the objects are usually larger and need to be removed with the bronchoscope as a unit. Once the object is within the forceps, it is dislodged from the airway and the bronchoscope is advanced to cover the foreign object, preventing it being stripped off the forceps during withdrawal.32 Removal of the bronchoscope may compromise the airway, so, again, communication during withdrawal is critical. Vegetable foreign bodies should be grasped lightly to avoid fragmentation of the foreign body into the distal airways.32 After removal of the object, bronchoscopy should be repeated to ensure that no residual foreign body is left and to assess the patency of the airway distal to the previous obstruction. Bleeding is usually controlled with thorough suctioning and vasoactive agents. If residual granulation tissue is present and is the source of bleeding or residual obstruction, it may be resected at the repeat endoscopy.32
IX Conclusions
The risk for complications increases significantly with inexperienced personnel, and the American College of Chest Physicians recommends that trainees perform at least 20 procedures under supervision to obtain basic competency and at least 10 procedures per year to maintain competency.7 The importance of communication between the bronchoscopist and the anesthesiologist cannot be overstated. When applied appropriately, rigid bronchoscopy can be a life-saving intervention in airway management.
X Clinical Pearls
• Open communication between the surgeon and the anesthetist is of highest importance during rigid bronchoscopy.
• Inspect the equipment prior to the patient’s arrival; ensure that the bronchoscopes, light sources, light carriers and connectors are all in working order.
• Check that instruments (suctions, graspers, telescopes) are appropriate length for the selected bronchoscope.
• Have a backup set that is a size smaller than what you plan to use.
• For pediatric patients, calculate the safe maximum dose of each topical medication (e.g., lidocaine), and restrict their presence in the operative field.
• Place dental/gingival protection, and never leave the bronchoscope on the teeth.
• Advance the scope only when there is an identifiable lumen.
All references can be found online at expertconsult.com.
5 Caplan RA, Benumof JL, Berry FA, et al. Practice guidelines for management of the difficult airway. Anesthesiology. 2003;98:1269–1277.
6 Beamis JF. Modern use of rigid bronchoscopy. In: Bollinger CT, Mathur PN. Interventional bronchoscopy. Basel: Karger; 2000:22–30.
12 Pereira KD, Hessel AC. Performance of rigid bronchoscopy. Haber CA, ed. Benumof’s airway management, ed 2, Philadelphia: Mosby Elsevier, 2007. Chapter 27
13 Eagle KA, Berger PB, Calkins H, et al. ACC/AHA guideline update for perioperative cardiovascular evaluation for noncardiac surgery: Executive summary. A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee to Update the 1996 Guidelines on Perioperative Cardiovascular Evaluation for Noncardiac Surgery). J Am Coll Cardiol. 2002;39:542–553.
14 Langeron O, Masso E, Huraux C, et al. Prediction of difficult mask ventilation. Anesthesiology. 2000;92:1229–1236.
20 Natalini G, Cavaliere S, Vitacca M, et al. Negative pressure ventilation vs. spontaneous assisted ventilation during rigid bronchoscopy. Acta Anaesthesiol Scand. 1998;42:1063–1069.
27 Hoeve LJ, Rombout J, Meursing AE. Complications of rigid laryngobronchoscopy in children. Int J Pediatr Otorhinolaryngol. 1993;26:47–56.
31 Reilly J, Thompson J, MacArthur C, et al. Pediatric aerodigestive foreign body injuries are complications related to timeliness of diagnosis. Laryngoscope. 1997;107:17–20.
32 Darrow DH, Holinger LD. Foreign bodies of the larynx, trachea, and bronchi. In: Bluestone CD, Stool SE, Alper CM, et al. Pediatric otolaryngology. ed 4. Philadelphia: Saunders; 2003:1543–1547.
33 Baharloo F, Veyckemans F, Francis C, et al. Tracheobronchial foreign bodies: Presentation and management in children and adults. Chest. 1999;115:1357–1362.
1 Marsh BR. Historic development of bronchoesophagology. Otolaryngol Head Neck Surg. 1996;114:689–716.
2 Hass AR, Vachani A, Sterman DH. Advances in diagnostic bronchoscopy. Am J Respir Crit Care Med. 2010;182:589–597.
3 Miller JI. Rigid bronchoscopy. Chest Surg Clin North Am. 1996;6:161–167.
4 Mentzer SJ. Bronchoscopy, rigid and flexible. In: Sugarbaker DJ, Bueno R, Krasna MJ. Adult chest surgery. New York: McGraw-Hill, 2009. Chapter 52
5 Caplan RA, Benumof JL, Berry FA, et al. Practice guidelines for management of the difficult airway. Anesthesiology. 2003;98:1269–1277.
6 Beamis JF. Modern use of rigid bronchoscopy. In: Bollinger CT, Mathur PN. Interventional bronchoscopy. Basel: Karger; 2000:22–30.
7 Ernst A, Silvestri GA, Johnstone D. Interventional pulmonary procedures: Guidelines from the American College of Chest Physicians. Chest. 2003;123:1693–1717.
8 Shepherd RW, Beamis JF. Understanding the basics of rigid bronchoscopy. J Respir Dis. 2006;27:100–113.
9 Casselbrant ML, Alper CM. Methods of examination. In: Bluestone CD, Stool SE, Alper CM, et al. Pediatric otolaryngology. ed 4. Philadelphia: Saunders; 2003:1379–1394.
10 Neustein SM, Eisenkraft JB. Thoracic procedures. In: Silverstein JH, Rooke GA, Reves JG, et al. Geriatric anesthesiology. ed 2. New York: Springer; 2008:378–389.
11 Studer W, Bolliger CT, Biro P. Anesthesia for interventional bronchoscopy. In: Bollinger CT, Mathur PN. Interventional bronchoscopy. Basel: Karger; 2000:44–54.
12 Pereira KD, Hessel AC. Performance of rigid bronchoscopy. Haber CA, ed. Benumof’s airway management, ed 2, Philadelphia: Mosby Elsevier, 2007. Chapter 27
13 Eagle KA, Berger PB, Calkins H, et al. ACC/AHA guideline update for perioperative cardiovascular evaluation for noncardiac surgery: Executive summary. A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee to Update the 1996 Guidelines on Perioperative Cardiovascular Evaluation for Noncardiac Surgery). J Am Coll Cardiol. 2002;39:542–553.
14 Langeron O, Masso E, Huraux C, et al. Prediction of difficult mask ventilation. Anesthesiology. 2000;92:1229–1236.
15 Wilson ME, Spiegelhalter D, Roberston JA, et al. Predicting difficult intubation. Br J Anaesth. 1988;61:211–216.
16 Malherbe S, Whyte S, Singh P, et al. Total intravenous anesthesia and spontaneous respiration for airway endoscopy in children: A prospective evaluation. Paediatr Anaesth. 2010;20:434–438.
17 Litman RS, Ponnuri J, Trogan I. Anesthesia for tracheal or bronchial foreign body removal in children: An analysis of ninety-four cases. Anesth Analg. 2000;91:1389–1391.
18 Farrell PT. Rigid bronchoscopy for foreign body removal: Anaesthesia and ventilation. Paediatr Anaesth. 2004;14:84–89.
19 Banoub M, Kraenzler EJ. Anesthesia for pulmonary and mediastinal surgery. In: Estafanous FG, Barash PG, Reves JG. Cardiac anesthesia: Principles and clinical practice. ed 2. Philadelphia: Lippincott Williams & Wilkins; 2001:703–766.
20 Natalini G, Cavaliere S, Vitacca M, et al. Negative pressure ventilation vs. spontaneous assisted ventilation during rigid bronchoscopy. Acta Anaesthesiol Scand. 1998;42:1063–1069.
21 Sen MK, Suri JC. Therapeutic bronchoscopy. Indian J Chest Dis Allied Sci. 2000;42:167–179.
22 Mehta AC, Lee FY, Cordasco EM, et al. Concentric tracheal and subglottic stenosis: Management using the Nd-YAG laser for mucosal sparing followed by gentle dilatation. Chest. 1993;104:673–677.
23 Yoon HI, Kim JH, Lee JH, et al. Comparison of propofol and the combination of propofol and alfentanil during bronchoscopy: A randomized study. Acta Anaesthesiol Scand. 2011;55:104–109.
24 Watanabe H, Lindgren L, Rosenberg P, et al. Glycopyrronium prolongs topical anaesthesia of oral mucosa and enhances absorption of lignocaine. Br J Anaesth. 1993;70:94–95.
25 Jöhr M. Is it time to question the routine use of anticholinergic agents in paediatric anaesthesia? Paediatr Anaesth. 1999;9:99–101.
26 Kucharczuk JC. Bronchoscopy: Flexible and rigid. In: Evans SR, ed. Surgical pitfalls: Prevention and management. Philadelphia: Saunders; 2009:657–659.
27 Hoeve LJ, Rombout J, Meursing AE. Complications of rigid laryngobronchoscopy in children. Int J Pediatr Otorhinolaryngol. 1993;26:47–56.
28 Lukomsky GI, Ovchinnikov AA, Bilal A. Complications of bronchoscopy: Comparison of rigid bronchoscopy under general anesthesia and flexible fiberoptic bronchoscopy under topical anesthesia. Chest. 1981;79:316–321.
29 Drummond M, Magalhaes A, Hespanhol V, et al. Rigid bronchoscopy: Complications in a university hospital. J Bronchol; 2003;10.
30 National Safety Council. Odds of death due to injury. United States http://www.nsc.org/news_resources/injury_and_death_statistics/Documents/Odds%20of%20Dying.pdf, 2006. Available at (accessed February 2012)
31 Reilly J, Thompson J, MacArthur C, et al. Pediatric aerodigestive foreign body injuries are complications related to timeliness of diagnosis. Laryngoscope. 1997;107:17–20.
32 Darrow DH, Holinger LD. Foreign bodies of the larynx, trachea, and bronchi. In: Bluestone CD, Stool SE, Alper CM, et al. Pediatric otolaryngology. ed 4. Philadelphia: Saunders; 2003:1543–1547.
33 Baharloo F, Veyckemans F, Francis C, et al. Tracheobronchial foreign bodies: Presentation and management in children and adults. Chest. 1999;115:1357–1362.
34 Barrios JE, Gutierrez C, Lluna J, et al. Bronchial foreign body: Should bronchoscopy be performed in all patients with a choking crisis? Pediatr Surg Int. 1997;12:118–120.
35 Chen L, Zhang X, Li S, et al. The risk factors for hypoxemia in children younger than 5 years old undergoing rigid bronchoscopy for foreign body removal. Anesth Analg. 2009;109:1079–1084.