79
Perforating Disorders
Classically, a group of disorders in which there is transepidermal elimination (‘perforation’) of components of the dermis, in particular collagen and/or elastic fibers (Table 79.1). Etiologies are multiple, including inheritance as an isolated cutaneous disease or in association with genetic disorders that affect connective tissue (e.g. Ehlers–Danlos syndrome). Most commonly, however, the perforating disorder is acquired and is related to the cutaneous trauma that results from scratching pruritic skin, especially in the setting of chronic kidney disease. A number of other cutaneous diseases occasionally undergo perforation, e.g. granuloma annulare, calcinosis cutis, chondrodermatitis nodularis helicis.
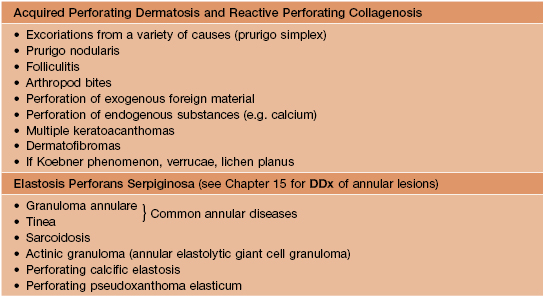
Table 79.1
Major perforating disorders.
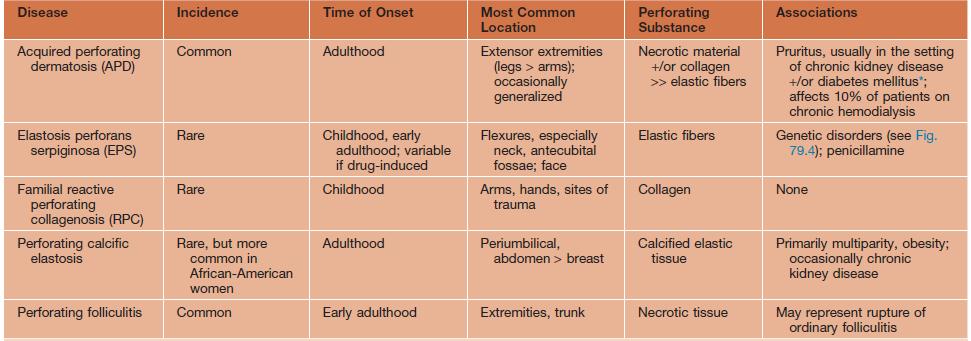
* Occasionally affects patients with pruritus due to other disorders, e.g. Hodgkin disease, biliary cirrhosis.
Courtesy, Ronald Rapini, MD.
Acquired Perforating Dermatosis (APD)
• The most commonly observed perforating disorder (see Table 79.1); it is an acquired disease that affects primarily adults; the term APD encompasses several overlapping entities including acquired reactive perforating collagenosis (RPC), Kyrle’s disease, and perforating folliculitis.
• Erythematous, skin-colored or hyperpigmented papules and papulonodules with a central keratotic core that favor the extensor surfaces of the extremities (Figs. 79.1 and 79.2); the central core is a reflection of the transepidermal elimination of collagen and/or elastic fibers as well as hyperkeratosis associated with epidermal hyperplasia.

Fig. 79.1 Acquired perforating dermatosis. Numerous papules and papulonodules on the legs in a patient with diabetes mellitus and chronic kidney disease. Courtesy, Ronald Rapini, MD.
Elastosis Perforans Serpiginosa (EPS)
• Annular or serpiginous plaques composed of keratotic papules that are usually skin-colored (Fig. 79.3); lesions favor flexural sites, in particular the neck and antecubital fossae, and can be several centimeters in diameter.


Fig. 79.3 Elastosis perforans serpiginosa. A Multiple annular plaques favoring the antecubital fossae, a flexural site. B Closer view with foci of hyperkeratosis at sites of transepidermal elimination. The patient had received penicillamine.
• Occurs in patients with inherited disorders that affect connective tissue (~40% of cases of EPS; Fig. 79.4) or as a consequence of medications that disrupt elastin formation, e.g. penicillamine; in the former group, the onset is during childhood or early adulthood; there is also a skin-limited childhood form that may be inherited.
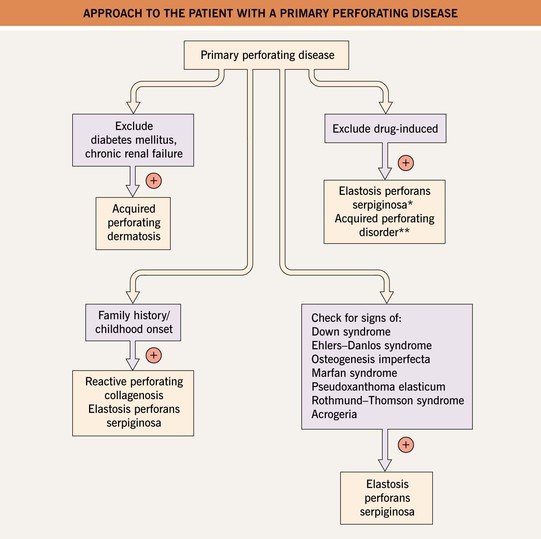
Fig. 79.4 Approach to the patient with a primary perforating disease. *Penicillamine. **Tumor necrosis factor-alpha inhibitors, bevacizumab, sirolimus, indinavir.
• Elastic fibers are surrounded by a hyperplastic epidermis and then eliminated transepidermally.
Familial Reactive Perforating Collagenosis (RPC)
Perforating Calcific Elastosis
• Most common site of involvement is periumbilical (Fig. 79.5); may be seen on the breast in the setting of chronic kidney disease.

Fig. 79.5 Perforating calcific elastosis. When a biopsy was performed from the elevated edge of this supraumbilical plaque in a multiparous African-American woman, resistance was felt, as well as a grinding sound.
• The periumbilical form favors obese, middle-aged, multiparous black women.
For further information see Ch. 96. From Dermatology, Third Edition.