Chapter 73 Penetrating Spinal Cord Injuries
Penetrating spine injury is a major cause of spinal cord injury (SCI) in the United States. Gunshot injuries have been reported to be the third leading cause of SCI.1 Stab wounds and other penetrating injuries tend to occur less in the United States than in some other countries. In South Africa, they account for 25% of all SCIs.2
Military versus Civilian Gunshot Injuries
Most experience with the management of penetrating SCIs has been gained during wartime. During World War I, survival was uncommon after a complete myelopathy (72% mortality). Treatment of these injuries consisted of laminectomy for incomplete myelopathy and debridement of the entry and exit wounds for complete myelopathy.3 A high operative mortality rate (62%) added to the dismal outcome.
During World War II, advances were made in trauma resuscitation and therapy. These advances dramatically decreased the mortality from penetrating SCIs.4–6 Some surgeons reported neurologic improvement in patients who were managed surgically.7 During the Korean War, most patients with penetrating SCIs underwent surgical exploration. There were reports of significant improvement.8 Further improvements were made in trauma resuscitation, evacuation, and surgical treatment during Operation Iraqi Freedom and Operation Enduring Freedom.9 The treatment of civilian penetrating SCIs, however, has generated less optimism than previous military reports have.10–14 Despite these findings, some authors have demonstrated benefit with early surgical intervention following civilian gunshot wounds.15 This is likely related to the pathophysiology of this type of injury.
Military weapons fire high-velocity missiles, while civilian weapons (typically handguns) fire low-velocity missiles. The pathophysiology of the SCI differs on the basis of velocity. High-velocity missiles may produce SCI by a concussive effect of the bullet passing close to, but not through, the spinal canal.16 Most SCIs caused by high-velocity missiles fit this pattern. These types of injuries may have a slightly better prognosis. Low-velocity missiles are more likely to injure the spinal cord directly, without a significant concussive effect; therefore, the prognosis for recovery is worse owing to the direct cord injury. This phenomenon may also explain the large percentage of civilian gunshot SCIs that present as complete myelopathies.10,12,17,18
Impalement Pathophysiology
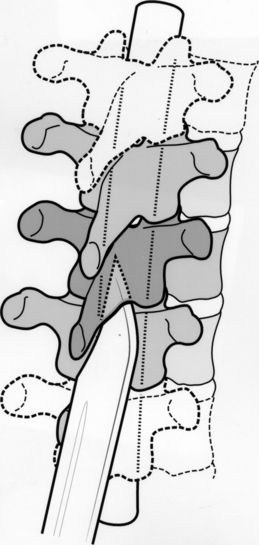
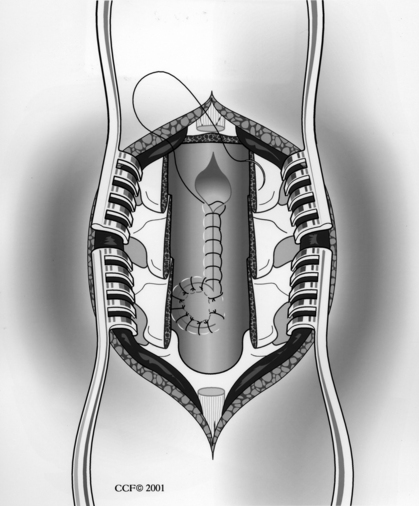
A weapon (knife) that penetrates the spinal canal may damage the spinal cord directly or indirectly. The direct injury may range from a dural tear to a total cord transection. Indirectly, there may be spinal cord contusion from the weapon impacting the cord against the bony spinal canal. The anatomy of the spinal canal may protect the spinal cord from a complete transection (Fig. 73-1). The weapon usually enters the spinal canal in the gutter between the spinous process and transverse process, thus leading to an incomplete SCI. Classically, the Brown-Séquard syndrome or a variant results.19
Resuscitation
The initial management begins with advanced trauma life support measures. The airway should be evaluated and secured. If necessary, endotracheal intubation should be performed. Oral intubation using manual in-line traction has been shown to be both safe and effective in patients with suspected SCI.20 Tracheostomy is indicated if the injury involves the trachea or larynx.21 Chest radiographs and arterial blood gas analysis (if indicated) should be part of the initial evaluation. The incidence of associated visceral injuries may be as high as 25%.22 These injuries, such as pneumothorax or vascular injury, must be sought early, as their treatment takes priority over spinal cord or spinal column injury.
The patient’s early course may be complicated by hypotension, which may be due to blood loss (hypovolemia) or to neurogenic shock from the loss of sympathetic vasomotor tone. Determining the exact cause of the hypotension is often difficult in the acute setting. However, tachycardia and cool extremities are often observed with hypovolemia, while bradycardia is often observed with spinal shock.19 The treatment for either condition is aggressive volume resuscitation. A central venous catheter is often helpful for monitoring the volume resuscitation. If the hypotension persists despite adequate intravascular volume replacement, vasopressor agents such as phenylephrine or dopamine should be employed. Vagolytic agents such as atropine may also be used. An indwelling pulmonary artery catheter may be useful if hypotension persists despite the use of vasopressor agents. Enthusiasm for the use of these catheters has waned lately.23
A Foley catheter should be placed. This allows bladder decompression and assists with gauging of the effectiveness of volume resuscitation. It also decreases the likelihood of subsequent urologic complications.19
Once the patient is stable from a cardiopulmonary standpoint, a more thorough history and physical examination should be performed. Information about the mechanism of injury and the caliber of the weapon should be obtained. The physical examination should note whether the patient has suffered a complete or incomplete myelopathy. If the injury is incomplete, the level of the SCI should be noted. The entry and exit sites should be inspected, and notation of cerebrospinal fluid (CSF) or foreign material should be made.7
Treatment of non-neurologic injuries is of primary importance because such treatment is usually lifesaving (rather than function-preserving).19 Because the course that a penetrating object takes within the torso is unpredictable, there may be an associated visceral injury.19 A trauma surgeon should assist with the evaluation for such potential injuries. Explorations of the neck, chest, and abdomen take precedence over spine surgeries.24
Some clinicians advocate exploration for wounds that penetrate the platysma, whereas others advocate the individualization of surgical planning.19 The two approaches appear equally effective if injuries to the great vessels, upper airway, and upper gastrointestinal tract can be ruled out via angiography, endoscopy, or swallowing studies.25–28
Pharyngeal perforation carries the risk of osteomyelitis.21,28,29 There are divergent views on the appropriate management of pharyngeal perforation. Some authors advocate broad-spectrum antibiotics, debridement of bone and soft tissue, drainage, and immobilization.21 Others have reported a lower infection rate with neural decompression and debridement of the wound.30
Radiographic Evaluation
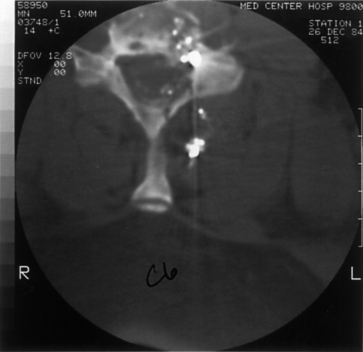
Initial evaluation should begin with routine radiographs. Fractures and bullet fragments may be seen (Fig. 73-2). A CT through the area of involvement should be performed next. This modality is generally superior to plain radiographs for the evaluation of the injury and for localizing the fracture or bullet fragments (Fig. 73-3). Compressive lesions may be identified with routine CT imaging. Bone and/or bullet fragments compressing the thecal sac may be identified. The aforementioned will also give the surgeon a sense of spinal stability or instability. CT myelography may be used to assess or confirm neural compression. This modality may also aid in the evaluation of a CSF fistula. If there is a question of spinal instability, passive flexion/extension radiographs may be used, but only in an awake, alert patient in whom there is no neurologic deficit.
MRI may also be used in the evaluation. There will be artifacts from the bullet fragments, but valuable information, such as the presence of extradural hematoma, disc herniation, or spinal cord contusion, may be gained. There is a risk of fragment migration in the magnetic field, so only patients for whom the information gained would have been difficult to obtain with other imaging modalities should undergo MRI.31
Steroids and Antibiotics
Experience with large patient populations has shown no improvement in outcome from using steroids in patients with penetrating spine injuries.19,32–34 This lack of efficacy and the potential adverse effects on wound healing and infection suggest that steroids have no role in patients with penetrating spine injury.
The rate of infection in penetrating SCI during the Vietnam War was lower in comparison to the rates in prior conflicts. The reason for the lower incidence was predominantly the use of antibiotics.35 Therefore, one may reasonably conclude that prophylactic antibiotics are of benefit in penetrating SCI. At least 7 days of antibiotic treatment for penetrating abdominal wounds with accompanying involvement of the spine have been shown to result in fewer infectious complications than do shorter courses of antibiotic treatment.36 The antibiotic agents should be chosen on the basis of the region of the body injured and local hospital bacterial sensitivities.
There has been some concern regarding infection following associated visceral injury. Roffi et al. reviewed 42 patients with gunshot wounds to the spine involving bullets passing through the alimentary tract.36 The patients were treated with a 2-week course of broad-spectrum antibiotics, and no evidence of late infection or osteomyelitis was found. Waters and Sie confirmed these findings in over 1000 cases of gunshot wounds to the spine.37 It may be concluded from these findings that it is not necessary to debride and remove bullet fragments following civilian gunshot wounds, even in the face of viscus perforation. This is not the case with high-velocity missile injuries, which pose a greater risk of contamination. Debriding the wound and removing the bullet fragments plus giving parenteral antibiotics are recommended.38
Surgical Indications
Missile Injuries
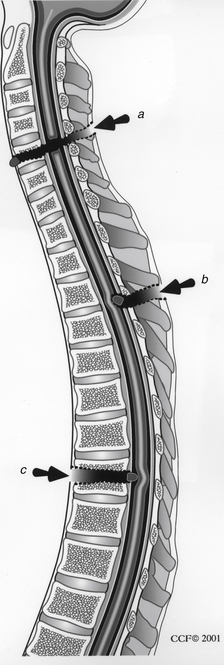
Surgery may be indicated in the following circumstances: (1) cord compression with an incomplete injury, (2) a discrepancy between the clinical examination and the missile trajectory with a complete myelopathy, (3) a migratory missile fragment, (4) spinal instability, (5) associated infection, and (6) persistent CSF leak17–19 (Fig. 73-4). Consideration should be given to surgical exploration of lesions of the cauda equina regardless of neurologic status. Because such injuries involve nerve roots rather than the spinal cord proper, they have a better prognosis.7 Surgery to remove a bullet fragment is not warranted unless compression of the cauda equina exists. Removal of the fragment when associated with a spinal cord–level injury remains controversial. As was noted previously, the type of injury may warrant fragment removal. If the injury was caused by a high-velocity weapon, such as during wartime, debridement and fragment removal may be indicated, especially in the face of viscus injury. If incomplete SCI is noted and the fragment is compressive, removal should be strongly considered. The composition of the bullet fragments has not been shown to adversely affect neurologic function.13,39,40
Impalement Injuries
Indications for surgery include neural element compression by bone or soft tissue fragments, retained fragments, CSF fistula, and infection. In contrast to gunshot injuries, retained foreign material should be removed after a stab wound. Because stab wounds are rarely delivered with enough force to cause spinal instability, this is an uncommon indication for surgery after these types of injuries.
Surgical Technique
Dorsal Approach
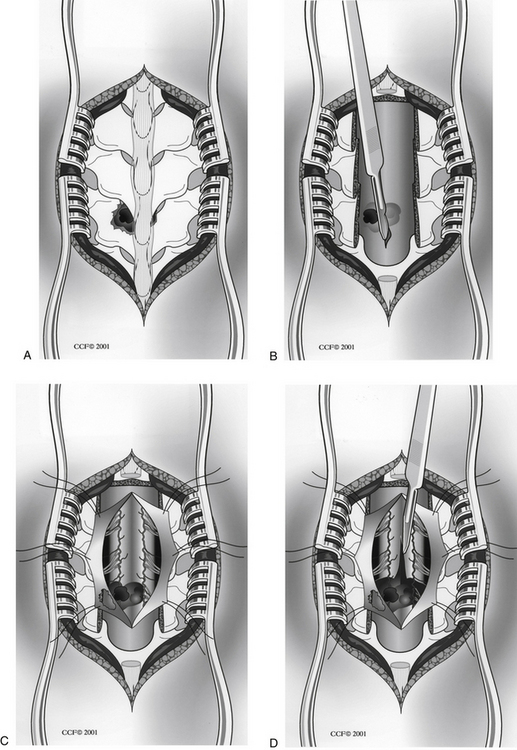
The dorsal approach is used most commonly for treatment of penetrating SCIs.19 A midline incision is made over the area of injury, and a standard subperiosteal dissection is used to gain access to the spine. Laminectomy or laminotomy is performed to expose the area of injury. Care should be taken to remove all compressive elements. Of particular importance is preservation of the facet joints to preserve spinal stability. The dura mater is often opened to expose the injured spinal cord or nerve roots. If an intramedullary mass with associated neurologic deficit is identified, it can be approached via midline myelotomy. Unnecessary injury to the posterior columns can be avoided by strict adherence to the placement of the midline myelotomy, and liquefied clot can be removed from within the spinal cord with gentle irrigation and suction19 (Fig. 73-5).
Dural closure should be pursued aggressively, care being taken not to compromise intradural contents19 (Fig. 73-6). Watertight closure should be performed, either primarily or with patching. Every effort should be made to use autologous material, such as local fascia or fascia lata. Ventral dural tears represent a challenge to repair from the dorsal approach. They may be left alone or may be loosely patched with muscle or other tissue. Fibrin-based tissue sealants are often helpful in treating such dural lacerations. CSF diversion is another useful adjunct.
Dorsolateral and Ventral Approaches
If a compressive lesion is lateral or ventral to the spinal cord, a dorsolateral or ventral approach may be indicated. Options include a transpedicular or costotransversectomy approach or a thoracotomy and lateral extracavitary approach for a more ventral exposure. Because these approaches do not provide wide exposure of the dura, they are rarely indicated.17 If the spine has been judged unstable, appropriate fixation and fusion techniques should be employed.
Prognosis
Prognosis is better after an impalement injury than after a missile injury. Overall, 60% of patients with stab wounds are able to ambulate at follow-up, compared to 24% of those with SCI due to gunshot wounds.41 The prognosis is poor with complete injury in either group.
Complications
CSF fistula may occur at the entrance or exit site. Fistulous connections with the bowel, bladder, and pleural cavity have also been reported.42–44 The initial management should be with subarachnoid drainage. If this fails, surgical exploration is warranted.
With the institution of prophylactic antibiotics, the incidence of infection after gunshot wounds has dramatically decreased.36 The antibiotics should be given for 7 to 14 days and should be tailored to the body site violated and to local hospital sensitivities. The combination of removal of retained foreign material, debridement, and prophylactic antibiotics should achieve a low infection rate after an impalement injury.
Metallic fragments have been reported to migrate in the CNS.45–48 If there has been migration and the patient is asymptomatic, no treatment may be needed, and the patient may simply be followed. If the patient is or becomes symptomatic (e.g., radiculopathy or paresthesias), the fragment should be retrieved.
Lead intoxication after a gunshot injury is rare. Bullets become encapsulated by poorly vascularized fibrous tissue.49 In addition, the lead from a bullet is relatively insoluble. Removal of a bullet for the purpose of decreasing lead intoxication is not warranted.
Penetrating spine injuries often lead to deafferentation pain. This pain is problematic in that it is often refractory to treatment.21 The problem is usually managed medically but often with minimal or no success. Surgery to remove bullet fragments thought to be related to pain has not been shown to provide improvement.41,50,51 Procedures such as spinal cord stimulation may be an option if medical therapy fails.
Bell R.S., Neal C.J., Tingo J., et al. Traumatic brain and spinal column injury: a 5-year study of the impact blast and other military grade weaponry on the central nervous system. J Trauma. 2009;66(4):S104-S111.
Jacobson S.A., Bor E. Spinal cord injury in Vietnamese combat. Paraplegia. 1970;7:263-281.
Kitchel S.H. Current treatment of gunshot wounds to the spine. Clin Orthop Relat Res. 2003;408:115-119.
Turgut M., Ozcan O.E., Gurcay O., Saglam S. Civilian penetrating spinal firearm injuries of the spine. Arch Orthop Trauma Surg. 1994;113:290-293.
Waters R.L., Sie I.H. Spinal cord injuries from gunshot wounds to the spine. Clin Orthop Relat Res. 2003;408:120-125.
1. Young J.S., Burns P.E., Bowen A.M., McCtchen R. Spinal cord injury statistics: experience of the Regional Spinal Cord Injury Systems. Phoenix, AZ, Good Samaritan Medical Center. 1982.
2. Peacock W.J., Shrosbree R.D., Key A.G. A review of 450 stab wounds of the spinal cord. S Afr Med J. 1977;51:961-964.
3. Tinsley M. Compound injuries of the spinal cord. J Neurosurg. 1946;3:306-309.
4. Guttman L. Spinal cord injuries: comprehensive management and research,. Oxford, UK: Blackwell Scientific; 1976.
5. Haynes W.G. Acute war wounds of the spinal cord: analysis of 184 cases. Am J Surg. 1946;72:424-433.
6. Hopkins D.A., Marshall T.K. Firearm injuries. Br J Surg. 1967;54:344-353.
7. David C.A., Landy H.J., Green B.A. Penetrating wounds of the spine. In: Wilkins R.H., Rengachary S.S., editors. Neurosurgery. New York: McGraw-Hill; 1996:3055-3061.
8. Wannamaker G.T. Spinal cord injuries: a review of the early treatment in 300 consecutive cases during the Korean conflict. J Neurosurg. 1954;11:517-524.
9. Bell R.S., Neal C.J., Tingo J., et al. Traumatic brain and spinal column injury: a 5-year study of the impact blast and other military grade weaponry on the central nervous system. J Trauma. 2009;66(4):S104-S111.
10. Heiden J.S., Weiss M.H., Rosenberg A.W., et al. Penetrating gunshot wounds of the cervical spine in civilians: review of 38 cases. J Neurosurg. 1975;42:575-579.
11. Kupcha P.C., An H.S., Cotler J.M. Gunshot wounds to the cervical spine. Spine. 1990;15:1058-1063.
12. Six E., Alexander E.Jr., Kelly D.L.Jr., et al. Gunshot wounds to the spinal cord. South Med J. 1979;72:699-702.
13. Stauffer E.S., Wood R.W., Kelly E.G. Gunshot wounds of the spine: the effects of laminectomy. J Bone Joint Surg [Am]. 1979;61:389-392.
14. Yashon D., Jane J.A., White R.J. Prognosis and management of spinal cord and cauda equina bullet injuries in sixty-five civilians. J Neurosurg. 1970;32:163-170.
15. Turgut M., Ozcan O.E., Gurcay O., Saglam S. Civilian penetrating spinal firearm injuries of the spine. Arch Orthop Trauma Surg. 1994;113:290-293.
16. Matson D.D. The treatment of acute compound injuries of the spinal cord due to missiles. Springfield, IL: Charles C. Thomas; 1948.
17. Benzel E.C., Hadden T.A., Coleman J.E. Civilian gunshot wounds to the spinal cord and cauda equina. Neurosurgery. 1987;20:281-285.
18. Cloeman J.E., Benzel E.C., Hadden T. Gunshot wounds to the spinal cord and cauda equina in civilians. Surg Forum. 1986;37:496-498.
19. Benzel E.C., Ball P.A. Controversies: penetrating injuries. In: Garfin S.R., Northrup B.E., editors. Surgery for spinal cord injuries. New York: Raven Press; 1993:269-278.
20. Grande C.M., Baron C.R., Stene J.K. Appropriate techniques for airway management of emergency patients with suspected spinal cord injury. Letter. Anesth Analg. 1988;67:714-715.
21. Jones R.E., Bucholz R.W., Schaefer S.D., et al. Cervical osteomyelitis complicating transpharyngeal gunshot wounds to the neck. J Trauma. 1979;19:630-634.
22. Jacobson S.A., Bor E. Spinal cord injury in Vietnamese combat. Paraplegia. 1970;7:263-281.
23. Antonelli M., Levy M., Andrews P.J., et al. Hemodynamic monitoring in shock and implications for management. International Consensus Conference, Paris, France, 27–28 April 2006. Intensive Care Med. 2007;33(4):575-590.
24. Tanguy A., Chabannes J., Debuelle A., et al. Intraspinal migration of a bullet with subsequent meningitis. J Bone Joint Surg [Am]. 1982;64:1244-1245.
25. May M., Chadaratana P., West J.W., et al. Penetrating neck wounds: selective exploration. Laryngoscope. 1975;85:57-75.
26. Meinke A.H., Bivins B.A., Sachatello C.R. Selective management of gunshot wounds to the neck: report of a series and review of the literature. Am J Surg. 1979;138:314-319.
27. Rao P.D., Bhatti F.K., Gaudindo J., et al. Penetrating injuries of the neck: criteria for exploration. J Trauma. 1983;23:47-49.
28. Schafer S.D., Bulcholz R.W., Jones R.E., et al. The management of transpharyngeal gunshot wounds to the cervical spine. Surg Gynecol Obstet. 1981;152:27-29.
29. Altman M.M., Joachims H.S. Osteomyelitis of the cervical spine after neck injuries. Arch Otolaryngol. 1972;96:72-75.
30. Venger B.H., Simpson R.K., Narayan R.K. Neurosurgical intervention in penetrating spinal trauma with associated visceral trauma. J Neurosurg. 1989;70:514-518.
31. Finitsis S.N., Falcone S., Green B.A. MR of the spine in the presence of metallic bullet fragments: is the benefit worth the risk? AJNR. 1999;20:354-356.
32. Bracken M.B., Shepard M.J., Collins W.F., et al. A randomized controlled trial of methylprednisolone or naloxone in the treatment of acute spinal-cord injury. N Engl J Med. 1990;332:1405-1411.
33. Prendergast M.R., Saxe J.M., Ledgerwood A.M., et al. Massive steroids do not reduce the zone of injury after penetrating spinal cord injury. J Trauma. 1994;37:576-580.
34. Simpson R.K., Venger B.H., Narayan R.K. Treatment of acute penetrating injuries of the spine. J Trauma. 1989;29:42-46.
35. Jacobs G.B., Berg R.A. The treatment of acute spinal cord injuries in a war zone. J Neurosurg. 1971;34:164-167.
36. Roffi R.P., Waters R.L., Adkins R.H. Gunshot wounds to the spine associated with a perforated viscus. Spine. 1989;14:808-811.
37. Waters R.L., Sie I.H. Spinal cord injuries from gunshot wounds to the spine. Clin Orthop Relat Res. 2003;408:120-125.
38. Kitchel S.H. Current treatment of gunshot wounds to the spine. Clin Orthop Relat Res. 2003;408:115-119.
39. Ott K., Tarlov E., Crowell R., et al. Retained intracranial metallic foreign bodies. Report of two cases. J Neurosurg. 1976;44:80-83.
40. Sherman I.J. Brass foreign body in the brain stem: a case report. J Neurosurg. 1960;17:483-485.
41. Waters R.L., Adkins R.H. The effects of removal of bullet fragments retained in the spinal canal: a collaborative study by the National Spinal Cord Injury Model Systems. Spine. 1991;16:934-939.
42. Beutel W.E., Roberts J.D., Langston H.T., et al. Subarachnoid-pleural fistula. J Thorac Cardiovasc Surg. 1980;80:21-24.
43. Djergaian R.S., Roberts J.D., Ditunno J.F., et al. Subarachnoid-pleural fistula in traumatic paraplegia. Arch Phys Med Rehabil. 1982;63:488-489.
44. Ward W.E., Maltby G.L. Associated complications in war wounds of the spine. JAMA. 1945;129:155-157.
45. Arasil E., Tascioglu A.O. Spontaneous migration of an intracranial bullet to the cervical spinal canal causing Lhermitte’s sign: case report. J Neurosurg. 1982;56:158-159.
46. Karim N.O., Nabors M.W., Golocovsky M., et al. Spontaneous migration of a bullet in the spinal subarachnoid space causing delayed radicular symptoms. Neurosurgery. 1986;18:97-100.
47. Milhorat T.H., Elowitz E.H., Johnson R.W., et al. Spontaneous movement of bullets in the brain. Neurosurgery. 1993;32:140-143.
48. Rengachary S.S., Carey M., Templer J. The sinking bullet. Neurosurgery. 1992;30:291-294.
49. Switz D.M., Elmorshidy M.E., Deyerle W.M. Bullets, joints, and lead intoxication. A remarkable and instructive case. Arch Intern Med. 1976;136:939-941.
50. Richards J.S. Pain secondary to gunshot wound during the initial rehabilitation process in spinal cord injury patients. J Rehabil Res Dev. 1988;25:75.
51. Richards J.S., Meredith R.L., Nepomuceno C., et al. Psycho-social aspects of chronic pain in spinal cord injury patients. Pain. 1980;8:355-366.