5
Pelvis and Perineum
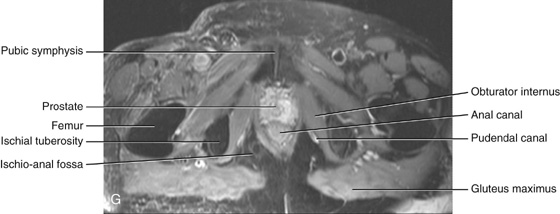
Ischio-anal fossae and their anterior recesses
ADDITIONAL LEARNING RESOURCES FOR CHAPTER 5, PELVIS AND PERINEUM, ON STUDENT CONSULT (www.studentconsult.com)
 Image Library—illustrations of pelvic and perineal anatomy, Chapter 5
Image Library—illustrations of pelvic and perineal anatomy, Chapter 5
 Self-Assessment (scored)—National Board style multiple-choice questions, Chapter 5
Self-Assessment (scored)—National Board style multiple-choice questions, Chapter 5
 Short Questions (not scored)—National Board style multiple-choice questions, Chapter 5
Short Questions (not scored)—National Board style multiple-choice questions, Chapter 5
 Interactive Surface Anatomy—interactive surface animations, Chapter 5
Interactive Surface Anatomy—interactive surface animations, Chapter 5
Regional anatomy
The pelvis and perineum are interrelated regions associated with the pelvic bones and the terminal parts of the vertebral column. The pelvis is divided into two regions (Fig. 5.1):
Fig. 5.1 Pelvis and perineum.
The bowl-shaped pelvic cavity (Fig. 5.1) enclosed by the true pelvis consists of the pelvic inlet, walls, and floor. This cavity is continuous superiorly with the abdominal cavity and contains and supports elements of the urinary, gastrointestinal, and reproductive systems.
The perineum (Fig. 5.1) is inferior to the floor of the pelvic cavity; its boundaries form the pelvic outlet. The perineum contains and supports the external genitalia and external openings of the genitourinary and gastrointestinal systems.
PELVIS
Bones
The bones of the pelvis consist of the right and left pelvic (hip) bones, the sacrum, and the coccyx. The sacrum articulates superiorly with vertebra LV at the lumbosacral joint. The pelvic bones articulate posteriorly with the sacrum at the sacro-iliac joints and with each other anteriorly at the pubic symphysis.
Pelvic bone
The pelvic bone is irregular in shape and has two major parts separated by an oblique line on the medial surface of the bone (Fig. 5.2A):
Fig. 5.2 Right pelvic bone. A. Medial view. B. Lateral view.
The linea terminalis is the lower two-thirds of this line and contributes to the margin of the pelvic inlet.
The lateral surface of the pelvic bone has a large articular socket, the acetabulum, which together with the head of the femur, forms the hip joint (Fig. 5.2B).
Inferior to the acetabulum is the large obturator foramen, most of which is closed by a flat connective tissue membrane, the obturator membrane. A small obturator canal remains open superiorly between the membrane and adjacent bone, providing a route of communication between the lower limb and the pelvic cavity.
The posterior margin of the bone is marked by two notches separated by the ischial spine (Fig. 5.2):
 the greater sciatic notch, and
the greater sciatic notch, and
The posterior margin terminates inferiorly as the large ischial tuberosity.
The irregular anterior margin of the pelvic bone is marked by the anterior superior iliac spine, the anterior inferior iliac spine, and the pubic tubercle.
Components of the pelvic bone
Each pelvic bone is formed by three elements: the ilium, pubis, and ischium. At birth, these bones are connected by cartilage in the area of the acetabulum; later, at between 16 and 18 years of age, they fuse into a single bone (Fig. 5.3).
Fig. 5.3 Ilium, ischium, and pubis.
Of the three components of the pelvic bone, the ilium is the most superior in position.
The ilium is separated into upper and lower parts by a ridge on the medial surface (Fig. 5.4A).
 Posteriorly, the ridge is sharp and lies immediately superior to the surface of the bone that articulates with the sacrum. This sacral surface has a large L-shaped facet for articulating with the sacrum and an expanded, posterior roughened area for the attachment of the strong ligaments that support the sacro-iliac joint (Fig. 5.4).
Posteriorly, the ridge is sharp and lies immediately superior to the surface of the bone that articulates with the sacrum. This sacral surface has a large L-shaped facet for articulating with the sacrum and an expanded, posterior roughened area for the attachment of the strong ligaments that support the sacro-iliac joint (Fig. 5.4).
 Anteriorly, the ridge separating the upper and lower parts of the ilium is rounded and termed the arcuate line (Fig. 5.4).
Anteriorly, the ridge separating the upper and lower parts of the ilium is rounded and termed the arcuate line (Fig. 5.4).
Fig. 5.4 Components of the pelvic bone. A. Medial surface. B. Lateral surface.
The arcuate line forms part of the linea terminalis and the pelvic brim.
The portion of the ilium lying inferiorly to the arcuate line is the pelvic part of the ilium and contributes to the wall of the lesser or true pelvis.
The upper part of the ilium expands to form a flat, fan-shaped “wing,” which provides bony support for the lower abdomen, or false pelvis (Fig. 5.4). This part of the ilium provides attachment for muscles functionally associated with the lower limb. The anteromedial surface of the wing is concave and forms the iliac fossa. The external (gluteal surface) of the wing is marked by lines and roughenings and is related to the gluteal region of the lower limb (Fig. 5.4B).
The entire superior margin of the ilium is thickened to form a prominent crest (the iliac crest), which is the site of attachment for muscles and fascia of the abdomen, back, and lower limb and terminates anteriorly as the anterior superior iliac spine and posteriorly as the posterior superior iliac spine (Fig. 5.4).
A prominent tubercle, tuberculum of iliac crest, projects laterally near the anterior end of the crest; the posterior end of the crest thickens to form the iliac tuberosity (Fig. 5.4).
Inferior to the anterior superior iliac spine of the crest, on the anterior margin of the ilium, is a rounded protuberance called the anterior inferior iliac spine (Fig 5.4). This structure serves as the point of attachment for the rectus femoris muscle of the anterior compartment of the thigh and the iliofemoral ligament associated with the hip joint. A less prominent posterior inferior iliac spine (Fig 5.4) occurs along the posterior border of the sacral surface of the ilium, where the bone angles forward to form the superior margin of the greater sciatic notch.
Clinical app
Bone marrow biopsy
In certain diseases (e.g., leukemia), a sample of bone marrow must be obtained to assess the stage and severity of the problem. The iliac crest is often used for such bone marrow biopsies. The iliac crest lies close to the surface, is palpable, and is easily accessed.
The anterior and inferior part of the pelvic bone is the pubis (Fig. 5.4). It has a body and two arms (rami).
 The inferior ramus projects laterally and inferiorly to join with the ramus of the ischium.
The inferior ramus projects laterally and inferiorly to join with the ramus of the ischium.
The ischium is the posterior and inferior part of the pelvic bone (Fig. 5.4). It has:
 a ramus that projects anteriorly to join with the inferior ramus of the pubis.
a ramus that projects anteriorly to join with the inferior ramus of the pubis.
The posterior margin of the bone is marked by a prominent ischial spine (Fig. 5.4) that separates the lesser sciatic notch, below, from the greater sciatic notch, above.
The most prominent feature of the ischium is a large tuberosity (the ischial tuberosity) on the posteroinferior aspect of the bone (Fig. 5.4). This tuberosity is an important site for the attachment of lower limb muscles and for supporting the body when sitting.
Sacrum
The sacrum, which has the appearance of an inverted triangle, is formed by the fusion of the five sacral vertebrae (Fig. 5.5). The base of the sacrum articulates with vertebra LV, and its apex articulates with the coccyx. Each of the lateral surfaces of the bone bears a large L-shaped facet for articulation with the ilium of the pelvic bone. Posterior to the facet is a large roughened area for the attachment of ligaments that support the sacro-iliac joint. The superior surface of the sacrum is characterized by the superior aspect of the body of vertebra SI and is flanked on each side by an expanded winglike transverse process termed the ala (Fig. 5.5A). The anterior edge of the vertebral body projects forward as the promontory. The anterior surface of the sacrum is concave; the posterior surface is convex. Because the transverse processes of adjacent sacral vertebrae fuse laterally to the position of the intervertebral foramina and laterally to the bifurcation of spinal nerves into posterior and anterior rami, the posterior and anterior rami of spinal nerves S1 to S4 emerge from the sacrum through separate foramina. There are four pairs of anterior sacral foramina on the anterior surface of the sacrum for anterior rami (Fig. 5.5A), and four pairs of posterior sacral foramina on the posterior surface for the posterior rami (Fig. 5.5B). The sacral canal is a continuation of the vertebral canal that terminates as the sacral hiatus.
Fig. 5.5 LV vertebra, sacrum, and coccyx. A. Anterior view. B. Posterior view. C. Lateral view.
Coccyx
The small terminal part of the vertebral column is the coccyx, which consists of four fused coccygeal vertebrae (Fig. 5.5A) and, like the sacrum, has the shape of an inverted triangle. The base of the coccyx is directed superiorly. The superior surface bears a facet for articulation with the sacrum and two horns, or cornua, one on each side, that project upward to articulate or fuse with similar downward-projecting cornua from the sacrum. These processes are modified superior and inferior articular processes that are present on other vertebrae. Each lateral surface of the coccyx has a small rudimentary transverse process, extending from the first coccygeal vertebra. Vertebral arches are absent from coccygeal vertebrae; therefore no bony vertebral canal is present in the coccyx.
Joints
Lumbosacral joints
The sacrum articulates superiorly with the lumbar part of the vertebral column. The lumbosacral joints are formed between vertebra LV and the sacrum and consist of (Fig. 5.6A):
 an intervertebral disc that joins the bodies of vertebrae LV and SI.
an intervertebral disc that joins the bodies of vertebrae LV and SI.
Fig. 5.6 Lumbosacral joints and associated ligaments. A. Lateral view. B. Anterior view.
These joints are similar to those between other vertebrae, with the exception that the sacrum is angled posteriorly on vertebra LV. As a result, the anterior part of the intervertebral disc between the two bones is thicker than the posterior part.
The lumbosacral joints are reinforced by strong iliolumbar and lumbosacral ligaments that extend from the expanded transverse processes of vertebra LV to the ilium and the sacrum, respectively (Fig. 5.6B).
Sacro-iliac joints
The sacro-iliac joints transmit forces from the lower limbs to the vertebral column. They are synovial joints between the L-shaped articular facets on the lateral surfaces of the sacrum and similar facets on the iliac parts of the pelvic bones (Figs. 5.6A, 5.7A). The joint surfaces have an irregular contour and interlock to resist movement. The joints often become fibrous with age and may become completely ossified.
Fig. 5.7 Sacro-iliac joints and associated ligaments. A. Lateral view. B. Anterior view. C. Posterior view.
Each sacro-iliac joint is stabilized by three ligaments:
 the anterior sacro-iliac ligament, which is a thickening of the fibrous membrane of the joint capsule and runs anteriorly and inferiorly to the joint (Figs. 5.6B, 5.7B);
the anterior sacro-iliac ligament, which is a thickening of the fibrous membrane of the joint capsule and runs anteriorly and inferiorly to the joint (Figs. 5.6B, 5.7B);
 the interosseus sacro-iliac ligament, which is the largest, strongest ligament of the three, is positioned immediately posterosuperior to the joint and attaches to adjacent expansive roughened areas on the ilium and sacrum, thereby filling the gap between the two bones (Fig. 5.7A and 5.7C); and
the interosseus sacro-iliac ligament, which is the largest, strongest ligament of the three, is positioned immediately posterosuperior to the joint and attaches to adjacent expansive roughened areas on the ilium and sacrum, thereby filling the gap between the two bones (Fig. 5.7A and 5.7C); and
 the posterior sacro-iliac ligament, which covers the interosseus sacro-iliac ligament (Fig. 5.7C).
the posterior sacro-iliac ligament, which covers the interosseus sacro-iliac ligament (Fig. 5.7C).
Clinical app
Common problems with the sacro-iliac joints
The sacro-iliac joints have both fibrous and synovial components, and as with many weight-bearing joints, degenerative changes may occur and cause pain and discomfort in the sacro-iliac region. In addition, disorders associated with the major histocompatibility complex antigen HLA B27, such as rheumatoid arthritis, psoriasis, and inflammatory bowel disease, can produce specific inflammatory changes within these joints.
Pubic symphysis joint
The pubic symphysis lies anteriorly between the adjacent surfaces of the pubic bones (Fig. 5.8). Each of the joint’s surfaces is covered by hyaline cartilage and is linked across the midline to adjacent surfaces by fibrocartilage. The joint is surrounded by interwoven layers of collagen fibers and the two major ligaments associated with it are (Fig. 5.8):
 the superior pubic ligament, located above the joint; and
the superior pubic ligament, located above the joint; and
 the inferior pubic ligament, located below it.
the inferior pubic ligament, located below it.
Fig. 5.8 Pubic symphysis and associated ligaments.
Orientation
In the anatomical position, the pelvis is oriented so that the front edge of the top of the pubic symphysis and the anterior superior iliac spines lie in the same vertical plane (Fig. 5.9). As a consequence, the pelvic inlet, which marks the entrance to the pelvic cavity, is tilted to face anteriorly, and the bodies of the pubic bones and the pubic arch are positioned in a nearly horizontal plane facing the ground.
Fig. 5.9 Orientation of the pelvis (anatomical position).
Gender differences
The pelvises of women and men differ in a number of ways, many of which have to do with the passing of a baby through a woman’s pelvic cavity during childbirth.
 The pelvic inlet in women is circular (Fig. 5.10A) compared with the more heart-shaped pelvic inlet (Fig. 5.10B) in men. The more circular shape is partly caused by the less distinct promontory and broader alae in women.
The pelvic inlet in women is circular (Fig. 5.10A) compared with the more heart-shaped pelvic inlet (Fig. 5.10B) in men. The more circular shape is partly caused by the less distinct promontory and broader alae in women.
 The angle formed by the two arms of the pubic arch is larger in women (80° to 85°) than it is in men (50° to 60°) (Fig. 5.10).
The angle formed by the two arms of the pubic arch is larger in women (80° to 85°) than it is in men (50° to 60°) (Fig. 5.10).
True pelvis
The true pelvis is cylindrical and has an inlet, a wall, and an outlet. The inlet is open, whereas the pelvic floor closes the outlet and separates the pelvic cavity, above, from the perineum, below.
Pelvic inlet
The pelvic inlet is the circular opening between the abdominal cavity and the pelvic cavity through which structures traverse between the abdomen and pelvic cavity. It is completely surrounded by bones and joints (Fig. 5.11). The promontory of the sacrum protrudes into the inlet, forming its posterior margin in the midline. On either side of the promontory, the margin is formed by the alae of the sacrum. The margin of the pelvic inlet then crosses the sacro-iliac joint and continues along the linea terminalis (i.e., the arcuate line, the pecten pubis, or pectineal line, and the pubic crest) to the pubic symphysis.
Fig. 5.11 Pelvic inlet.
Pelvic wall
The walls of the pelvic cavity consist of the sacrum, the coccyx, the pelvic bones inferior to the linea terminalis, two ligaments, and two muscles.
Clinical app
Pelvic fracture
The pelvis can be viewed as a series of anatomical rings. There are three bony rings and four fibro-osseous rings. The major bony pelvic ring consists of parts of the sacrum, ilium, and pubis, which forms the pelvic inlet. Two smaller subsidiary bony rings are the obturator foraminae. The greater and lesser sciatic foraminae, formed by the greater and lesser sciatic notches and the sacrospinous and sacrotuberous ligaments form the four fibro-osseous rings. It is not possible to break one side of a bony ring without breaking the other side of the ring, which in clinical terms means that if a fracture is demonstrated on one side, a second fracture should always be suspected.
Ligaments of the pelvic wall
The sacrospinous and sacrotuberous ligaments (Fig. 5.12A) are major components of the lateral pelvic walls that help define the apertures between the pelvic cavity and adjacent regions through which structures pass.
 The smaller of the two, the sacrospinous ligament, is triangular, with its apex attached to the ischial spine and its base attached to the related margins of the sacrum and the coccyx (Fig. 5.12A).
The smaller of the two, the sacrospinous ligament, is triangular, with its apex attached to the ischial spine and its base attached to the related margins of the sacrum and the coccyx (Fig. 5.12A).
 The sacrotuberous ligament is also triangular and is superficial to the sacrospinous ligament. Its base has a broad attachment that extends from the posterior superior iliac spine of the pelvic bone, along the dorsal aspect and the lateral margin of the sacrum, and onto the dorsolateral surface of the coccyx. Laterally, the apex of the ligament is attached to the medial margin of the ischial tuberosity (Fig. 5.12A).
The sacrotuberous ligament is also triangular and is superficial to the sacrospinous ligament. Its base has a broad attachment that extends from the posterior superior iliac spine of the pelvic bone, along the dorsal aspect and the lateral margin of the sacrum, and onto the dorsolateral surface of the coccyx. Laterally, the apex of the ligament is attached to the medial margin of the ischial tuberosity (Fig. 5.12A).
These ligaments stabilize the sacrum on the pelvic bones by resisting the upward tilting of the inferior aspect of the sacrum (Fig. 5.12B). They also convert the greater and lesser sciatic notches of the pelvic bone into foramina (Fig. 5.12A, B).
 The greater sciatic foramen lies superior to the sacrospinous ligament and the ischial spine.
The greater sciatic foramen lies superior to the sacrospinous ligament and the ischial spine.
Muscles of the pelvic wall
Two muscles, the obturator internus and the piriformis, contribute to the lateral walls of the pelvic cavity. These muscles originate in the pelvic cavity but attach peripherally to the femur (Table 5.1, Fig. 5.13).
Table 5.1 Muscles of the pelvic walls (spinal segments in bold are the major segments innervating the muscle)
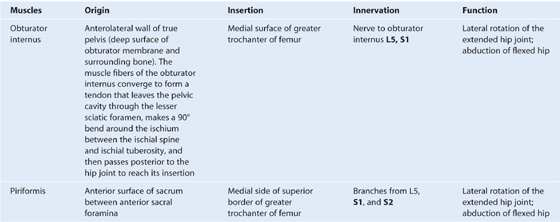
Fig. 5.13 Obturator internus and piriformis muscles (medial view of right side of pelvis).
Apertures in the pelvic wall
Each lateral pelvic wall has three major apertures through which structures pass between the pelvic cavity and other regions (Fig. 5.14):
 the greater sciatic foramen, and
the greater sciatic foramen, and
Fig. 5.14 Apertures in the pelvic wall.
At the top of the obturator foramen is the obturator canal, which is bordered by the obturator membrane, the associated obturator muscles, and the superior pubic ramus (Fig. 5.14). The obturator nerve and vessels pass from the pelvic cavity to the thigh through this canal.
The greater sciatic foramen is a major route of communication between the pelvic cavity and the lower limb (Fig. 5.14). It is formed by the greater sciatic notch in the pelvic bone, the sacrotuberous and the sacrospinous ligaments, and the spine of the ischium.
The piriformis muscle passes through the greater sciatic foramen, dividing it into two parts.
 The superior gluteal nerves and vessels pass through the foramen above the piriformis.
The superior gluteal nerves and vessels pass through the foramen above the piriformis.
The lesser sciatic foramen is formed by the lesser sciatic notch of the pelvic bone, the ischial spine, the sacrospinous ligament, and the sacrotuberous ligament (Fig. 5.14). The tendon of the obturator internus muscle passes through this foramen to enter the gluteal region of the lower limb.
Because the lesser sciatic foramen is positioned below the attachment of the pelvic floor, it acts as a route of communication between the perineum and the gluteal region. The pudendal nerve and internal pudendal vessels pass between the pelvic cavity (above the pelvic floor) and the perineum (below the pelvic floor), by first passing out of the pelvic cavity through the greater sciatic foramen, then looping around the ischial spine and sacrospinous ligament to pass through the lesser sciatic foramen to enter the perineum.
Pelvic outlet
The pelvic outlet is diamond shaped, with the anterior part of the diamond defined predominantly by bone and the posterior part mainly by ligaments (Fig. 5.15). In the midline anteriorly, the boundary of the pelvic outlet is the pubic symphysis.
Fig. 5.15 Pelvic outlet.
From the ischial tuberosities, the boundaries continue posteriorly and medially along the sacrotuberous ligament on both sides to the coccyx.
Terminal parts of the urinary and gastrointestinal tracts and the vagina pass through the pelvic outlet.
Clinical app
Pelvic measurements in obstetrics
Accurate measurements of a women’s pelvic inlet and outlet can help in predicting the likelihood of a successful vaginal delivery during childbirth. These measurements include:
 the sagittal inlet (between the promontory and the top of the pubic symphysis);
the sagittal inlet (between the promontory and the top of the pubic symphysis);
 the maximum transverse diameter of the inlet;
the maximum transverse diameter of the inlet;
 the bispinous outlet (the distance between ischial spines); and
the bispinous outlet (the distance between ischial spines); and
The area enclosed by the boundaries of the pelvic outlet and below the pelvic floor is the perineum.
Pelvic floor
The pelvic floor is formed by the pelvic diaphragm and, in the anterior midline, the perineal membrane and the muscles in the deep perineal pouch. The pelvic diaphragm is formed by the levator ani and the coccygeus muscles from both sides. The pelvic floor separates the pelvic cavity, above, from the perineum, below.
The pelvic diaphragm
The pelvic diaphragm is the muscular part of the pelvic floor. Shaped like a bowl or funnel and attached superiorly to the pelvic walls, it consists of the levator ani and the coccygeus muscles (Table 5.2, Fig. 5.16).
Table 5.2 Muscles of the pelvic diaphragm
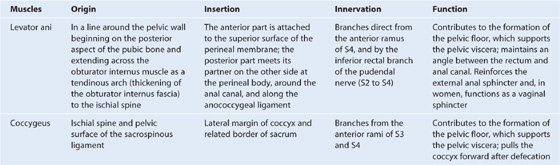
Fig. 5.16 Pelvic diaphragm.
The pelvic diaphragm’s circular line of attachment to the cylindrical pelvic wall passes, on each side, between the greater sciatic foramen and the lesser sciatic foramen. Thus:
The two levator ani muscles originate from each side of the pelvic wall, course medially and inferiorly, and join together in the midline. The attachment to the pelvic wall follows the circular contour of the wall and includes (Fig. 5.16):
 the posterior aspect of the body of the pubic bone,
the posterior aspect of the body of the pubic bone,
At the midline, the muscles blend together posterior to the vagina in women and around the anal aperture in both sexes. Posterior to the anal aperture, the muscles come together as a ligament or raphe called the anococcygeal ligament (anococcygeal body) and attaches to the coccyx (Fig. 5.16). Anteriorly, the muscles are separated by a U-shaped defect or gap termed the urogenital hiatus. The margins of this hiatus merge with the walls of the associated viscera and with muscles in the deep perineal pouch below. The hiatus allows the urethra (in both men and women), and the vagina (in women), to pass through the pelvic diaphragm (Fig. 5.16).
The levator ani muscles are divided into at least three collections of muscle fibers, based on site of origin and relationship to viscera in the midline: the pubococcygeus, the puborectalis, and the iliococcygeus muscles (Fig. 5.16).
The levator ani muscles help support the pelvic viscera and maintain closure of the rectum and vagina.
Clinical app
Defecation
At the beginning of defecation, closure of the larynx stabilizes the diaphragm and intra-abdominal pressure is increased by contraction of abdominal wall muscles. As defecation proceeds, the puborectalis muscle surrounding the anorectal junction relaxes, which straightens the anorectal angle. Both the internal and the external anal sphincters also relax to allow feces to move through the anal canal. Normally, the puborectal sling maintains an angle of about 90° between the rectum and the anal canal and acts as a “pinch valve” to prevent defecation. When the puborectalis muscle relaxes, the anorectal angle increases to about 130° to 140°.
The fatty tissue of the ischio-anal fossa allows for changes in the position and size of the anal canal and anus during defecation. During evacuation, the anorectal junction moves down and back and the pelvic floor usually descends slightly.
During defecation, the circular muscles of the rectal wall undergo a wave of contraction to push feces toward the anus. As feces emerge from the anus, the longitudinal muscles of the rectum and levator ani bring the anal canal back up, the feces are expelled, and the anus and rectum return to their normal positions.
The perineal membrane and deep perineal pouch
The perineal membrane is a thick fascial, triangular structure attached to the bony framework of the pubic arch (Fig. 5.17A). It is oriented in the horizontal plane and has a free posterior margin. Anteriorly, there is a small gap between the membrane and the inferior pubic ligament (a ligament associated with the pubic symphysis).
Fig. 5.17 Perineal membrane and deep perineal pouch. A. Inferior view. B. Superolateral view. C. Medial view.
The perineal membrane is related above to a thin space called the deep perineal pouch (deep perineal space) (Fig. 5.17B), which contains a layer of skeletal muscle and various neurovascular elements.
The deep perineal pouch is open above and is not separated from more superior structures by a distinct layer of fascia. The parts of perineal membrane and structures in the deep perineal pouch, enclosed by the urogenital hiatus above, therefore contribute to the pelvic floor and support elements of the urogenital system in the pelvic cavity, even though the perineal membrane and deep perineal pouch are usually considered parts of the perineum.
The perineal membrane and adjacent pubic arch provide attachment for the roots of the external genitalia and the muscles associated with them (Fig. 5.17C).
The urethra penetrates vertically through a circular hiatus in the perineal membrane as it passes from the pelvic cavity, above, to the perineum, below. In women, the vagina also passes through a hiatus in the perineal membrane just posterior to the urethral hiatus.
Within the deep perineal pouch, a sheet of skeletal muscle functions as a sphincter, mainly for the urethra, and as a stabilizer of the posterior edge of the perineal membrane (Table 5.3, Fig. 5.18).
Table 5.3 Muscles within the deep perineal pouch
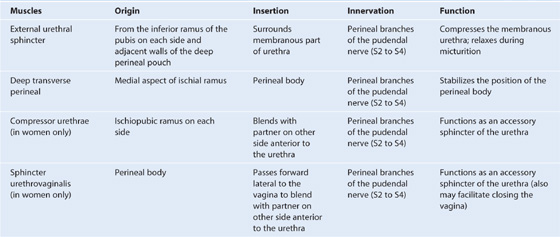
Fig. 5.18 Muscles in the deep perineal pouch. A. In women. B. In men.
 Anteriorly, a group of muscle fibers surround the urethra and collectively form the external urethral sphincter (Fig. 5.18).
Anteriorly, a group of muscle fibers surround the urethra and collectively form the external urethral sphincter (Fig. 5.18).
 Two additional groups of muscle fibers are associated with the urethra and vagina in women (Fig. 5.18A). One group forms the sphincter urethrovaginalis, which surrounds the urethra and vagina as a unit. The second group forms the compressor urethrae, on each side, which originate from the ischiopubic rami and meet anterior to the urethra. Together with the external urethral sphincter, the sphincter urethrovaginalis and compressor urethrae facilitate closing of the urethra.
Two additional groups of muscle fibers are associated with the urethra and vagina in women (Fig. 5.18A). One group forms the sphincter urethrovaginalis, which surrounds the urethra and vagina as a unit. The second group forms the compressor urethrae, on each side, which originate from the ischiopubic rami and meet anterior to the urethra. Together with the external urethral sphincter, the sphincter urethrovaginalis and compressor urethrae facilitate closing of the urethra.
Perineal body
The perineal body is an ill-defined but important connective tissue structure into which muscles of the pelvic floor and the perineum attach (Fig. 5.19). It is positioned in the midline along the posterior border of the perineal membrane, to which it attaches. The posterior end of the urogenital hiatus in the levator ani muscles is also connected to it.
Fig. 5.19 Perineal body.
The deep transverse perineal muscles intersect at the perineal body; in women, the sphincter urethrovaginalis also attaches to the perineal body. Other muscles that connect to the perineal body include the external anal sphincter, the superficial transverse perineal muscles, and the bulbospongiosus muscles of the perineum.
Clinical app
Episiotomy
During childbirth the perineal body may be stretched and torn. Traditionally it was felt that if a perineal tear is likely, the obstetrician may proceed with an episiotomy. This is a procedure in which an incision is made in the perineal body to allow the head of the fetus to pass through the vagina. There are two types of episiotomies: a median episiotomy cuts through the perineal body, while a mediolateral episiotomy is an incision 45° from the midline. The maternal benefits of this procedure have been thought to be less trauma to the perineum and decreased pelvic floor dysfunction. However, more recent evidence suggests that an episiotomy should not be performed routinely. Review of data has failed to show a decrease in pelvic floor damage with routine use of episiotomies.
Viscera
The pelvic viscera include parts of the gastrointestinal system, the urinary system, and the reproductive system. The viscera are arranged in the midline, from front to back; the neurovascular supply is through branches that pass medially from vessels and nerves associated with the pelvic walls.
Gastrointestinal system
Pelvic parts of the gastrointestinal system consist mainly of the rectum and the anal canal, although the terminal part of the sigmoid colon is also in the pelvic cavity (Fig. 5.20).
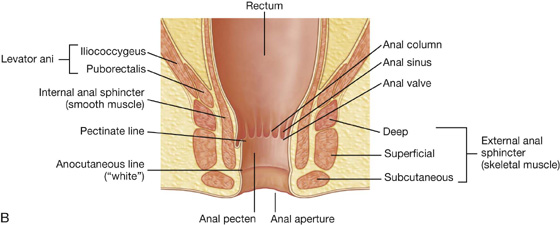
Fig. 5.20 Rectum and anal canal. A. Left pelvic bone removed. B. Longitudinal section.
Rectum
The rectum is continuous:
 above, with the sigmoid colon at about the level of vertebra SIII; and
above, with the sigmoid colon at about the level of vertebra SIII; and
The rectum, the most posterior element of the pelvic viscera, is immediately anterior to, and follows the concave contour of the sacrum (Fig. 5.20A).
The anorectal junction is pulled forward (perineal flexure) by the action of the puborectalis part of the levator ani muscle, so the anal canal moves in a posterior direction as it passes inferiorly through the pelvic floor.
In addition to conforming to the general curvature of the sacrum in the anteroposterior plane, the rectum has three lateral curvatures; the upper and lower curvatures to the right and the middle curvature to the left. The lower part of the rectum is expanded to form the rectal ampulla. Finally, unlike the colon, the rectum lacks distinct taeniae coli muscles, omental appendices, and sacculations (haustra of the colon).
Digital rectal examination
A digital rectal examination (DRE) is performed by placing the gloved and lubricated index finger into the rectum through the anus. The anal mucosa can be palpated for abnormal masses, and in women, the posterior wall of the vagina and the cervix can be palpated. In men, the prostate can be evaluated for any extraneous nodules or masses.
Anal canal
The anal canal begins at the terminal end of the rectal ampulla where it narrows at the pelvic floor (Fig. 5.20B). It terminates as the anus after passing through the perineum. As it passes through the pelvic floor, the anal canal is surrounded along its entire length by the internal and external anal sphincters, which normally keep it closed (Fig. 5.20B).
The lining of the anal canal bears a number of characteristic structural features that reflect the approximate position of the anococcygeal membrane in the fetus (which closes the terminal end of the developing gastrointestinal system in the fetus) and the transition from gastrointestinal mucosa to skin in the adult (Fig. 5.20B).
Clinical app
Carcinoma of the colon and rectum
Carcinoma of the colon and rectum (colorectum) is a common disease.
Given the position of the colon and rectum in the abdominopelvic cavity and its proximity to other organs, it is extremely important to accurately stage colorectal tumors: a tumor in the pelvis, for example, could invade the uterus or bladder.
Urinary system
The pelvic parts of the urinary system consist of the terminal parts of the ureters, the bladder, and the proximal part of the urethra (Fig. 5.21).
Fig. 5.21 Pelvic parts of the urinary system.
Ureters
The ureters enter the pelvic cavity from the abdomen by passing through the pelvic inlet (Fig. 5.21). On each side, the ureter crosses the pelvic inlet and enters the pelvic cavity in the area anterior to the bifurcation of the common iliac artery. From this point, it continues along the pelvic wall and floor to join the base of the bladder.
In the pelvis, the ureter is crossed by:
 the ductus deferens in men, and
the ductus deferens in men, and
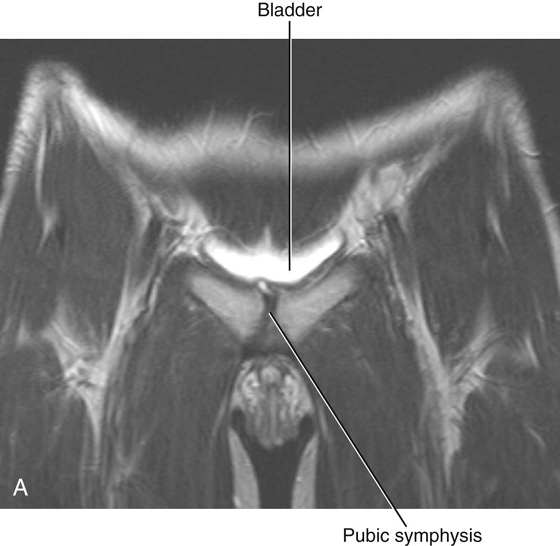
Bladder
The bladder is the most anterior element of the pelvic viscera. Although it is entirely situated in the pelvic cavity when empty, it expands superiorly into the abdominal cavity when full (see Fig. 5.21).
The empty bladder is shaped like a three-sided pyramid that has tipped over to lie on one of its margins (see Fig. 5.22A). It has an apex, a base, a superior surface, and two inferolateral surfaces (see Fig. 5.22A).
 The base of the bladder is shaped like an inverted triangle and faces posteroinferiorly. The two ureters enter the bladder at each of the upper corners of the base, and the urethra drains inferiorly from the lower corner of the base (Fig. 5.22A, B). Inside, the mucosal lining on the base of the bladder is smooth and firmly attached to the underlying smooth muscle coat of the wall—unlike elsewhere in the bladder where the mucosa is folded and loosely attached to the wall. The smooth triangular area between the openings of the ureters and urethra on the inside of the bladder is known as the trigone (Fig. 5.22B).
The base of the bladder is shaped like an inverted triangle and faces posteroinferiorly. The two ureters enter the bladder at each of the upper corners of the base, and the urethra drains inferiorly from the lower corner of the base (Fig. 5.22A, B). Inside, the mucosal lining on the base of the bladder is smooth and firmly attached to the underlying smooth muscle coat of the wall—unlike elsewhere in the bladder where the mucosa is folded and loosely attached to the wall. The smooth triangular area between the openings of the ureters and urethra on the inside of the bladder is known as the trigone (Fig. 5.22B).
The neck of the bladder surrounds the origin of the urethra at the point where the two inferolateral surfaces and the base intersect (see Fig. 5.21).
The neck is the most inferior part of the bladder and also the most “fixed” part. It is anchored into position by a pair of tough fibromuscular bands, which connect the neck and pelvic part of the urethra to the posteroinferior aspect of each pubic bone.
 In women, these fibromuscular bands are termed pubovesical ligaments (Fig. 5.23A). Together with the perineal membrane and associated muscles, the levator ani muscles, and the pubic bones, these ligaments help support the bladder.
In women, these fibromuscular bands are termed pubovesical ligaments (Fig. 5.23A). Together with the perineal membrane and associated muscles, the levator ani muscles, and the pubic bones, these ligaments help support the bladder.
 In men, the paired fibromuscular bands are known as puboprostatic ligaments because they blend with the fibrous capsule of the prostate, which surrounds the neck of the bladder and adjacent part of the urethra (Fig. 5.23B).
In men, the paired fibromuscular bands are known as puboprostatic ligaments because they blend with the fibrous capsule of the prostate, which surrounds the neck of the bladder and adjacent part of the urethra (Fig. 5.23B).
Although the bladder is considered to be pelvic in the adult, it has a higher position in children. At birth, the bladder is almost entirely abdominal; the urethra begins approximately at the upper margin of the pubic symphysis. With age, the bladder descends until after puberty when it assumes the adult position.
Clinical app
Bladder cancer
Bladder cancer is the most common tumor of the urinary tract and is usually a disease of the sixth and seventh decades, although there is an increasing trend for younger patients to develop this disease.
Bladder tumors may spread through the bladder wall and invade local structures, including the rectum, uterus (in women), and the lateral walls of the pelvic cavity. Prostatic involvement is not uncommon in male patients.
Large bladder tumors may produce complications, including invasion and obstruction of the ureters. Ureteric obstruction can then obstruct the kidneys and induce kidney failure.
Bladder stones
In some patients, small calculi (stones) form in the kidneys. These may pass down the ureter, causing ureteric obstruction, and into the bladder, where insoluble salts further precipitate on these small calculi to form larger calculi. Often, these patients develop (or may already have) problems with bladder emptying, which leaves residual urine in the bladder. This urine may become infected and alter the pH of the urine, permitting further precipitation of insoluble salts.
Clinical app
Suprapubic catheterization
In certain instances it is necessary to catheterize the bladder through the anterior abdominal wall. For example, when the prostate is markedly enlarged and it is impossible to pass a urethral catheter into the bladder. The bladder is a retroperitoneal structure and when full lies adjacent to the anterior abdominal wall.
The procedure of suprapubic catheterization is straightforward and involves the passage of a small catheter through the abdominal wall in the midline above the pubic symphysis. The catheter passes into the bladder without compromising other structures and allows drainage.
Urethra
The urethra begins at the base of the bladder and ends with an external opening in the perineum. The paths taken by the urethra differ significantly in women and men.
In women, the urethra is short, being about 4 cm long. It travels a slightly curved course as it passes inferiorly through the pelvic floor into the perineum, where it passes through the deep perineal pouch and perineal membrane before opening in the vestibule that lies between the labia minora (Fig. 5.24A).
Fig. 5.24 Urethra. A. In women. B. In men. C. Prostatic part of the urethra in men.
The urethral opening is anterior to the vaginal opening in the vestibule. The inferior aspect of the urethra is bound to the anterior surface of the vagina. Two small para-urethral mucous glands (Skene’s glands) are associated with the lower end of the urethra. Each drains via a duct that opens onto the lateral margin of the external urethral orifice.
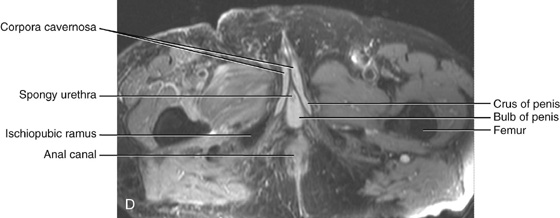
In men, the urethra is long, about 20 cm, and bends twice along its course (Fig. 5.24B). Beginning at the base of the bladder and passing inferiorly through the prostate, it passes through the deep perineal pouch and perineal membrane and immediately enters the root of the penis. As the urethra exits the deep perineal pouch, it bends forward to course anteriorly in the root of the penis. When the penis is flaccid, the urethra makes another bend, this time inferiorly, when passing from the root to the body of the penis. During erection, the bend between the root and body of the penis disappears.
The urethra in men is divided into preprostatic, prostatic, membranous, and spongy parts (see Fig. 5.24B).
Preprostatic part. The preprostatic part of the urethra is about 1 cm long, extends from the base of the bladder to the prostate, and is associated with a circular cuff of smooth muscle fibers (the internal urethral sphincter) (see Fig. 5.24B). Contraction of this sphincter prevents retrograde movement of semen into the bladder during ejaculation.
Prostatic part. The prostatic part of the urethra (see Fig. 5.24C) is 3 to 4 cm long and is surrounded by the prostate. In this region, the lumen of the urethra is marked by a longitudinal midline fold of mucosa (the urethral crest). The depression on each side of the crest is the prostatic sinus; the ducts of the prostate empty into these two sinuses.
Midway along its length, the urethral crest is enlarged to form a somewhat circular elevation (the seminal colliculus) (see Fig. 5.24C). In men, the seminal colliculus is used to determine the position of the prostate gland during transurethral transection of the prostate.
A small blind-ended pouch—the prostatic utricle (thought to be the homologue of the uterus in women)—opens onto the center of the seminal colliculus (see Fig. 5.24C). On each side of the prostatic utricle is the opening of the ejaculatory duct of the male reproductive system. Therefore the connection between the urinary and reproductive tracts in men occurs in the prostatic part of the urethra.
Membranous part. The membranous part of the urethra is narrow and passes through the deep perineal pouch (see Fig. 5.24B). During its transit through this pouch, the urethra, in both men and women, is surrounded by skeletal muscle of the external urethral sphincter.
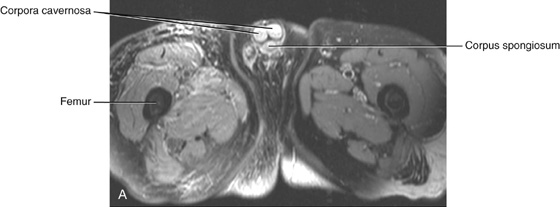
Spongy urethra. The spongy urethra is surrounded by erectile tissue (the corpus spongiosum) of the penis. It is enlarged to form a bulb at the base of the penis and again at the end of the penis to form the navicular fossa (see Fig. 5.24B). The two bulbourethral glands in the deep perineal pouch are part of the male reproductive system and open into the bulb of the spongy urethra. The external urethral orifice is the sagittal slit at the end of the penis.
Clinical app
Bladder infection
The relatively short length of the urethra in women makes them more susceptible than men to bladder infection. The primary symptom of urinary tract infection in women is usually inflammation of the bladder (cystitis). In children under 1 year of age, infection from the bladder may spread via the ureters to the kidneys, where it can produce renal damage and ultimately lead to renal failure. Early diagnosis and treatment are necessary.
Urethral catheterization
Urethral catheterization is often performed to drain urine from a patient’s bladder when the patient is unable to micturate. When inserting urinary catheters, it is important to appreciate the gender anatomy of the patient.
In men the spongy urethra angles superiorly to pass through the perineal membrane and into the pelvis. Just inferior to the perineal membrane, the wall of the urethral bulb is relatively thin and can be damaged when inserting catheters or doing cystoscopy. In women, these procedures are much simpler because the urethra is short and straight.
Reproductive system
In men
The reproductive system in men has components in the abdomen, pelvis, and perineum (Fig. 5.25A). The major components are a testis, epididymis, ductus deferens, and ejaculatory duct on each side, and the urethra and penis in the midline. In addition, three types of accessory glands are associated with the system:
Fig. 5.25 Reproductive system in men. A. Overview. B. Testis and surrounding structures.
 a pair of seminal vesicles, and
a pair of seminal vesicles, and
 a pair of bulbourethral glands.
a pair of bulbourethral glands.
The design of the reproductive system in men is basically a series of ducts and tubules. The arrangement of parts and linkage to the urinary tract reflects its embryological development.
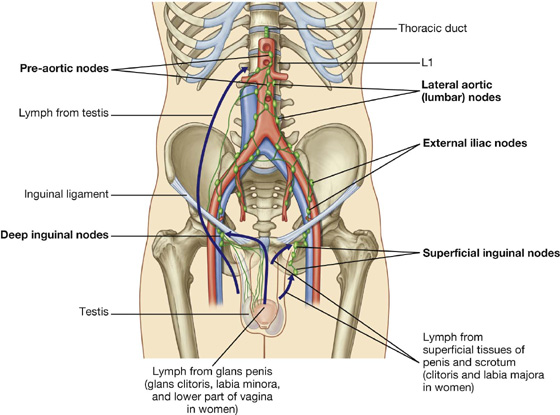
The testes originally develop high on the posterior abdominal wall and then descend, normally before birth, through the inguinal canal in the anterior abdominal wall and into the scrotum of the perineum. During descent, the testes carry their vessels, lymphatics, and nerves, as well as their principal drainage ducts, the ductus deferens (vas deferens) with them. The lymph drainage of the testes is therefore to the lateral aortic or lumbar nodes and pre-aortic nodes in the abdomen, and not to the inguinal or pelvic lymph nodes.
Each ellipsoid-shaped testis is enclosed within the end of an elongated musculofascial pouch, which is continuous with the anterior abdominal wall and projects into the scrotum. The spermatic cord is the tube-shaped connection between the pouch in the scrotum and the abdominal wall (Fig. 5.25A).
The sides and anterior aspect of the testis are covered by a closed sac of peritoneum (the tunica vaginalis), which originally connected to the abdominal cavity (Fig. 5.25B). Normally after testicular descent, the connection closes, leaving a fibrous remnant.
Each testis (Fig. 5.25B) is composed of seminiferous tubules and interstitial tissue surrounded by a thick connective tissue capsule (the tunica albuginea). Spermatozoa are produced by the seminiferous tubules. The 400 to 600 highly coiled seminiferous tubules are modified at each end to become straight tubules, which connect to a collecting chamber (the rete testis) in a thick, vertically oriented linear wedge of connective tissue (the mediastinum testis), projecting from the capsule into the posterior aspect of the gonad (Fig. 5.25B). Approximately 12 to 20 efferent ductules originate from the upper end of the rete testis, penetrate the capsule, and connect with the epididymis.
Clinical app
Undescended testes
Around the seventh month of gestation, the testes begin their descent from the posterior abdominal wall through the inguinal canal and into the scrotum. During the descent, the testes may arrest (undescended testes) or they may end up in an ectopic position. Undescended/ectopic testes are associated with infertility and increased risk of testicular tumors.
Clinical app
Hydrocele of the testis
A hydrocele of the testis is an accumulation of fluid within the cavity of the tunica vaginalis. Hydroceles are typically unilateral and in most cases their cause is unknown, although they may occur secondary to physical trauma, infection, or tumor.
Clinical app
Testicular tumors
Tumors of the testis account for a small percentage of malignancies in men. However, they generally occur in younger patients (between 20 and 40 years of age).
Early diagnosis of testicular tumor is extremely important. Abnormal lumps can be detected by palpation and diagnosis can be made using ultrasound.
Surgical removal of the malignant testis is often carried out using an inguinal approach. The testis is not usually removed through a scrotal incision because it is possible to spread tumor cells into the subcutaneous tissues of the scrotum, which has a different lymphatic drainage than the testis.
The epididymis is a single, long coiled duct that courses along the posterolateral side of the testis (Fig. 5.25B). It has two distinct components:
The ductus deferens is a long muscular duct that transports spermatozoa from the tail of the epididymis in the scrotum to the ejaculatory duct in the pelvic cavity (see Fig. 5.25A). It ascends in the scrotum as a component of the spermatic cord and passes through the inguinal canal in the anterior abdominal wall.
After passing through the deep inguinal ring, the ductus deferens bends medially around the lateral side of the inferior epigastric artery and crosses the external iliac artery and the external iliac vein at the pelvic inlet to enter the pelvic cavity (see Fig. 5.25A).
The duct descends medially on the pelvic wall, deep to the peritoneum, and crosses the ureter posterior to the bladder. It continues inferomedially along the base of the bladder, anterior to the rectum, almost to the midline, where it is joined by the duct of the seminal vesicle to form the ejaculatory duct (see Fig. 5.25A).
Between the ureter and ejaculatory duct, the ductus deferens expands to form the ampulla of the ductus deferens. The ejaculatory duct penetrates through the prostate gland to connect with the prostatic urethra.
Clinical app
Vasectomy
The ductus deferens transports spermatozoa from the tail of the epididymis in the scrotum to the ejaculatory duct in the pelvic cavity. Because it has a thick smooth muscle wall, it can be easily palpated in the spermatic cord between the testes and the superficial inguinal ring. Also, because it can be accessed through skin and superficial fascia, it is amenable to surgical dissection and surgical division. When this is carried out bilaterally (vasectomy), the patient is rendered sterile—this is a useful method for male contraception.
Each seminal vesicle is an accessory gland of the male reproductive system that develops as a blind-ended tubular outgrowth from the ductus deferens (see Fig. 5.25A). The tube is coiled with numerous pocket-like outgrowths and is encapsulated by connective tissue to form an elongate structure situated between the bladder and rectum. The gland is immediately lateral to and follows the course of the ductus deferens at the base of the bladder.
The duct of the seminal vesicle joins the ductus deferens to form the ejaculatory duct (see Fig. 5.25A). Secretions from the seminal vesicle contribute significantly to the volume of the ejaculate (semen).
The prostate is an unpaired accessory structure of the male reproductive system that surrounds the urethra in the pelvic cavity (see Fig. 5.25A). It lies immediately inferior to the bladder, posterior to the pubic symphysis, and anterior to the rectum.
The prostate is shaped like an inverted rounded cone with a larger base, which is continuous above with the neck of the bladder, and a narrower apex, which rests below on the pelvic floor. The inferolateral surfaces of the prostate are in contact with the levator ani muscles that together cradle the prostate between them.
The prostate develops as 30 to 40 individual complex glands, which grow from the urethral epithelium into the surrounding wall of the urethra. Collectively, these glands enlarge the wall of the urethra into what is known as the prostate; however, the individual glands retain their own ducts, which empty independently into the prostatic sinuses on the posterior aspect of the urethral lumen.
Secretions from the prostate, together with secretions from the seminal vesicles, contribute to the formation of semen during ejaculation.
The ejaculatory ducts pass almost vertically in an anteroinferior direction through the posterior aspect of the prostate to open into the prostatic urethra.
Clinical app
Prostate problems
Prostate cancer is one of the most commonly diagnosed malignancies in men, and often the disease is advanced at diagnosis. Prostate cancer typically occurs in the peripheral regions of the prostate and is relatively asymptomatic. In many cases, it is diagnosed by a digital rectal examination and by blood tests, which include serum acid phosphatase and serum prostate-specific antigen (PSA). In rectal examinations, the tumorous prostate feels “rock” hard. The diagnosis is usually made by obtaining a number of biopsies of the prostate.
Benign prostatic hypertrophy is a disease of the prostate that occurs with increasing age in most men (Fig. 5.26). It generally involves the more central regions of the prostate, which gradually enlarge. The prostate feels “bulky” on digital rectal examination. Owing to the more central hypertrophic change of the prostate, the urethra is compressed, and a urinary outflow obstruction develops in a number of patients. With time, the bladder may become hypertrophied in response to the urinary outflow obstruction. In some male patients, the obstruction becomes so severe that urine cannot be passed and transurethral or suprapubic catheterization is necessary. Despite being a benign disease, benign prostatic hypertrophy can therefore have a marked effect on the daily lives of many patients.
Fig. 5.26 Axial T2-weighted magnetic resonance image of benign prostatic hypertrophy.
The bulbourethral glands (see Fig. 5.25A), one on each side, are small, pea-shaped mucous glands situated within the deep perineal pouch. They are lateral to the membranous part of the urethra. The duct from each gland passes inferomedially through the perineal membrane to open into the bulb of the spongy urethra at the root of the penis.
Together with small glands positioned along the length of the spongy urethra, the bulbourethral glands contribute to lubrication of the urethra and the pre-ejaculatory emission from the penis.
In women
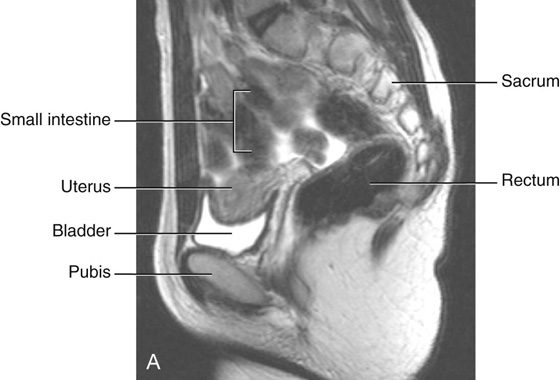
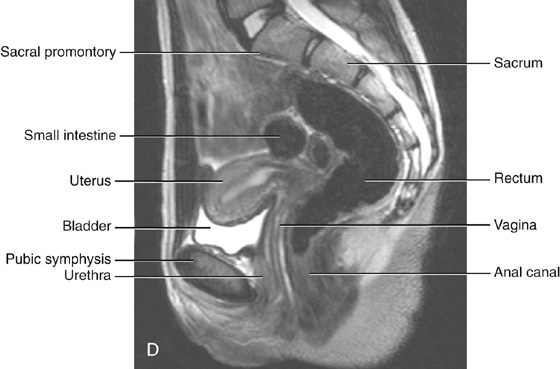
The reproductive tract in women is contained mainly in the pelvic cavity and perineum, although during pregnancy, the uterus expands into the abdomen cavity. Major components of the system consist of (Fig. 5.27):
Fig. 5.27 Reproductive system in women.
 a uterus, vagina, and clitoris in the midline.
a uterus, vagina, and clitoris in the midline.
In addition, a pair of accessory glands (the greater vestibular glands) are associated with the tract.
Like the testes in men, the ovaries develop high on the posterior abdominal wall and then descend before birth, bringing with them their vessels, lymphatics, and nerves. Unlike the testes, the ovaries do not migrate through the inguinal canal into the perineum, but stop short and assume a position on the lateral wall of the pelvic cavity (Fig. 5.28).
Fig. 5.28 Ovaries and broad ligament.
The ovaries lie adjacent to the lateral pelvic wall just inferior to the pelvic inlet. Each of the two almond-shaped ovaries is about 3 cm long and is suspended by a mesentery (the mesovarium) that is a posterior extension of the broad ligament.
Clinical app
Ovarian cancer
Ovarian cancer remains one of the major challenges in oncology. The ovaries contain numerous cell types, all of which can undergo malignant change and require different imaging and treatment protocols and ultimately have different prognoses. Ovarian cancer may occur at any age, but more typically it occurs in older women.
Many factors have been linked with the development of ovarian tumors, including a strong family history.
Cancer of the ovaries may spread via the blood and lymphatics, and frequently metastasizes directly into the peritoneal cavity. Such direct peritoneal cavity spread allows the passage of tumor cells along the paracolic gutters and over the liver from where this disease may disseminate easily. Unfortunately, many patients already have metastatic and diffuse disease at the time of diagnosis.
The uterus is a thick-walled muscular organ in the midline between the bladder and rectum (see Fig. 5.28). It consists of a body and a cervix, and inferiorly it joins the vagina (Fig. 5.29). Superiorly, uterine tubes project laterally from the uterus and open into the peritoneal cavity immediately adjacent to the ovaries (Fig. 5.29).
Fig. 5.29 Uterus. Anterior view. The anterior half of the uterus and vagina have been cut away.
The body of the uterus is flattened anteroposteriorly and, above the level of origin of the uterine tubes (Fig. 5.29), has a rounded superior end (fundus of uterus). The cavity of the body of the uterus is a narrow slit when viewed laterally, and is shaped like an inverted triangle when viewed anteriorly. Each of the superior corners of the cavity is continuous with the lumen of a uterine tube and the inferior corner is continuous with the central canal of the cervix.
Implantation of the blastocyst normally occurs in the body of the uterus. During pregnancy, the uterus dramatically expands superiorly into the abdominal cavity.
Clinical app
Hysterectomy
A hysterectomy is the surgical removal of the uterus. This is usually a complete excision of the body, fundus, and cervix of the uterus, though occasionally the cervix may be left in situ. In some instances the uterine (fallopian) tubes and the ovaries also are removed. This procedure is called a total abdominal hysterectomy and bilateral salpingo-oophorectomy.
Hysterectomy, oophorectomy, and salpingo-oophorectomy may be performed in patients who have reproductive malignancy, such as uterine, cervical, and ovarian cancers. Other indications include strong family history of reproductive disorders, endometriosis, and excessive bleeding. Occasionally the uterus may need to be removed postpartum because of excessive postpartum bleeding.
A hysterectomy is performed through a transverse suprapubic incision (Pfannenstiel’s incision). During the procedure, tremendous care is taken to identify the distal ureters and to ligate the nearby uterine arteries without damage to the ureters.
The uterine tubes extend from each side of the superior end of the body of the uterus to the lateral pelvic wall and are enclosed within the upper margins of the mesosalpinx portions of the broad ligaments. Because the ovaries are suspended from the posterior aspect of the broad ligaments, the uterine tubes pass superiorly over, and terminate laterally to, the ovaries.
Each uterine tube has an expanded trumpet-shaped end (the infundibulum), which curves around the superolateral pole of the related ovary (Fig. 5.30). The margin of the infundibulum is rimmed with small finger-like projections termed fimbriae. The lumen of the uterine tube opens into the peritoneal cavity at the narrowed end of the infundibulum. Medial to the infundibulum, the tube expands to form the ampulla and then narrows to form the isthmus, before joining with the body of the uterus (Fig. 5.30).
Fig. 5.30 Uterine tubes.
The fimbriated infundibulum facilitates the collection of ovulated eggs from the ovary. Fertilization normally occurs in the ampulla.
Clinical app
Tubal ligation
A simple and effective method of birth control is to surgically ligate (clip) the uterine tubes, preventing spermatozoa from reaching the ampulla.
The cervix forms the inferior part of the uterus and is shaped like a short, broad cylinder with a narrow central channel. The body of the uterus normally arches forward (anteflexed on the cervix) over the superior surface of the emptied bladder (Fig. 5.31A). In addition, the cervix is angled forward (anteverted) on the vagina so that the inferior end of the cervix projects into the upper anterior aspect of the vagina (Figs. 5.31A, 5.32). Because the end of the cervix is dome shaped, it bulges into the vagina, and a gutter, or fornix, is formed around the margin of the cervix where it joins the vaginal wall (Fig. 5.31B). The tubular central canal of the cervix opens, below, as the external os, into the vaginal cavity and, above, as the internal os, into the uterine cavity (Fig. 5.31B).
Clinical app
Carcinoma of the cervix and uterus
Carcinoma of the cervix and uterus is a common disease in women. Diagnosis is by inspection, cytology (examination of the cervical cells), imaging, biopsy, and dilatation and curettage (D&C) of the uterus.
Carcinoma of the cervix and uterus may be treated by local resection, removal of the uterus (hysterectomy), and adjuvant chemotherapy. The tumor spreads via lymphatics to the internal and common iliac lymph nodes.
The vagina is the copulatory organ in women. It is a distensible fibromuscular tube that extends from the perineum through the pelvic floor and into the pelvic cavity (see Fig. 5.32A). The internal end of the canal is enlarged to form a region called the vaginal vault.
The anterior wall of the vagina is related to the base of the bladder and to the urethra; in fact, the urethra is embedded in, or fused to, the anterior vaginal wall (see Fig. 5.32A).
Posteriorly, the vagina is related principally to the rectum.
Inferiorly, the vagina opens into the vestibule of the perineum immediately posterior to the external opening of the urethra. From its external opening (the introitus), the vagina courses posterosuperiorly through the perineal membrane and into the pelvic cavity, where it is attached by its anterior wall to the circular margin of the cervix.
The vaginal fornix is the recess formed between the margin of the cervix and the vaginal wall. Based on position, the fornix is subdivided into a posterior fornix, an anterior fornix, and two lateral fornices (see Figs. 5.31B, 5.32B).
The vaginal canal is normally collapsed so that the anterior wall is in contact with the posterior wall. By using a speculum to open the vaginal canal, a physician can see the domed inferior end of the cervix, the vaginal fornices, and the external os of the cervical canal in a patient (see Fig. 5.31B).
During intercourse, semen is deposited in the vaginal vault. Spermatozoa make their way into the external os of the cervical canal, pass through the cervical canal into the uterine cavity, and then continue through the uterine cavity into the uterine tubes.
Fascia
Fascia in the pelvic cavity lines the pelvic walls, surrounds the bases of the pelvic viscera, and forms sheaths around blood vessels and nerves that course medially from the pelvic walls to reach the viscera in the midline. This pelvic fascia is a continuation of the extraperitoneal connective tissue layer found in the abdomen.
In women
In women, a rectovaginal septum separates the posterior surface of the vagina from the rectum (Fig. 5.33A). Condensations of fascia form ligaments that extend from the cervix to the anterior (pubocervical ligament), lateral (transverse cervical or cardinal ligament), and posterior (uterosacral ligament) pelvic walls. These ligaments, together with the perineal membrane, the levator ani muscles, and the perineal body, are thought to stabilize the uterus in the pelvic cavity. The most important of these ligaments are the transverse cervical or cardinal ligaments, which extend laterally from each side of the cervix and vaginal vault to the related pelvic wall.
Fig. 5.33 Pelvic fascia. A. In women. B. In men.
In men
In men, a condensation of fascia around the anterior and lateral region of the prostate (prostatic fascia) contains and surrounds the prostatic plexus of veins and is continuous posteriorly with the rectovesical septum, which separates the posterior surface of the prostate and base of the bladder from the rectum (Fig. 5.33B).
Peritoneum
The peritoneum of the pelvis is continuous at the pelvic inlet with the peritoneum of the abdomen. In the pelvis, the peritoneum drapes over the pelvic viscera in the midline, forming:
 pouches between adjacent viscera, and
pouches between adjacent viscera, and
 folds and ligaments between viscera and pelvic walls.
folds and ligaments between viscera and pelvic walls.
Anteriorly, median and medial umbilical folds of peritoneum cover the embryological remnants of the urachus and umbilical arteries, respectively (Fig. 5.34). These folds ascend out of the pelvis and onto the anterior abdominal wall. Posteriorly, peritoneum drapes over the anterior and lateral aspects of the upper third of the rectum, but only the anterior surface of the middle third of the rectum is covered by peritoneum; the lower third of the rectum is not covered at all.
Fig. 5.34 Peritoneum in the pelvis. A. In women. B. In men.
In women
In women, the uterus lies between the bladder and rectum, and the uterine tubes extend from the superior aspect of the uterus to the lateral pelvic walls (Fig. 5.34A). As a consequence, a shallow vesico-uterine pouch occurs anteriorly, between the bladder and uterus, and a deep recto-uterine pouch (pouch of Douglas) occurs posteriorly, between the uterus and rectum. In addition, a large fold of peritoneum (the broad ligament), with a uterine tube enclosed in its superior margin and an ovary attached posteriorly, is located on each side of the uterus and extends to the lateral pelvic walls.
In the midline, the peritoneum descends over the posterior surface of the uterus and cervix and onto the vaginal wall adjacent to the posterior vaginal fornix. It then reflects onto the anterior and lateral walls of the rectum. The deep pouch of peritoneum formed between the anterior surface of the rectum and posterior surfaces of the uterus, cervix, and vagina is the recto-uterine pouch. A sharp sickle-shaped ridge of peritoneum (recto-uterine fold) occurs on each side near the base of the recto-uterine pouch. The recto-uterine folds overlie the uterosacral ligaments, which are condensations of pelvic fascia that extend from the cervix to the posterolateral pelvic walls.
Broad ligament
The broad ligament is a sheetlike fold of peritoneum, oriented in the coronal plane that runs from the lateral pelvic wall to the uterus, and encloses the uterine tube in its superior margin and suspends the ovary from its posterior aspect (see Fig. 5.34). The uterine arteries cross the ureters at the base of the broad ligaments, and the ligament of the ovary and round ligament of the uterus are enclosed within the parts of the broad ligament related to the ovary and uterus, respectively. The broad ligament has three parts (see Fig. 5.34A):
 the mesovarium, a posterior extension of the broad ligament, which attaches to the ovary.
the mesovarium, a posterior extension of the broad ligament, which attaches to the ovary.
The peritoneum of the mesovarium becomes firmly attached to the ovary as the surface epithelium of the ovary. The ovaries are positioned with their long axis in the vertical plane. The ovarian vessels, nerves, and lymphatics enter the superior pole of the ovary from a lateral position and are covered by another raised fold of peritoneum, which with the structures it contains forms the suspensory ligament of ovary (infundibulopelvic ligament) (see Fig. 5.34A).
The inferior pole of the ovary is attached to a fibromuscular band of tissue (the ligament of ovary), which courses medially in the margin of the mesovarium to the uterus and then continues anterolaterally as the round ligament of uterus (see Fig. 5.34). The round ligament of uterus passes over the pelvic inlet to reach the deep inguinal ring and then courses through the inguinal canal to end in connective tissue related to the labium majus in the perineum. Both the ligament of ovary and the round ligament of uterus are remnants of the gubernaculum, which attaches the gonad to the labioscrotal swellings in the embryo.
In men
In men, the visceral peritoneum drapes over the top of the bladder onto the superior poles of the seminal vesicles and then reflects onto the anterior and lateral surfaces of the rectum (see Fig. 5.34B). A rectovesical pouch occurs between the bladder and rectum.
Clinical app
The recto-uterine pouch
The recto-uterine pouch (pouch of Douglas) is an extremely important clinical region situated between the rectum and uterus. When the patient is in the supine position, the recto-uterine pouch is the lowest portion of the abdominopelvic cavity and is a site where infection and fluids typically collect. It is impossible to palpate this region transabdominally, but it can be examined by transvaginal and transrectal digital palpation. If an abscess is suspected, it may be drained by a needle placed through to the posterior fornix of the vagina or the anterior wall of the rectum.
Nerves
Somatic plexuses
Sacral and coccygeal plexuses
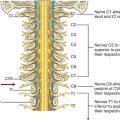
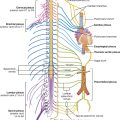
The sacral and coccygeal plexuses are situated on the posterolateral wall of the pelvic cavity and generally occur in the plane between the muscles and blood vessels. They are formed by the ventral rami of S1 to Co, with a significant contribution from L4 and L5, which enter the pelvis from the lumbar plexus (Figs. 5.35, 5.36). Nerves from these mainly somatic plexuses contribute to the innervation of the lower limb and muscles of the pelvis and perineum. Cutaneous branches supply skin over the medial side of the foot, the posterior aspect of the lower limb, and most of the perineum.
Fig. 5.35 Sacral and coccygeal plexuses.
Fig. 5.36 Components and branches of the sacral and coccygeal plexuses.
The sacral plexus on each side is formed by the anterior rami of S1 to S4, and the lumbosacral trunk (L4 and L5) (Fig. 5.36). The plexus is formed in relation to the anterior surface of the piriformis muscle, which is part of the posterolateral pelvic wall. Sacral contributions to the plexus pass out of the anterior sacral foramina and course laterally and inferiorly on the pelvic wall. The lumbosacral trunk, consisting of part of the anterior ramus of L4 and all of the anterior ramus of L5, courses vertically into the pelvic cavity from the abdomen by passing immediately anterior to the sacro-iliac joint.
Gray rami communicantes from ganglia of the sympathetic trunk connect with each of the anterior rami and carry postganglionic sympathetic fibers destined for the periphery to the somatic nerves (Fig. 5.37). In addition, special visceral nerves (pelvic splanchnic nerves) originating from S2 to S4 deliver preganglionic parasympathetic fibers to the pelvic part of the prevertebral plexus (Fig. 5.38, p. 237).
Fig. 5.37 Sympathetic trunks in the pelvis.
Fig. 5.38 Pelvic extensions of the prevertebral plexus. A. Anterior view.
Fig. 5.38 Pelvic extensions of the prevertebral plexus. B. Anteromedial view of right side of plexus.
Each anterior ramus has ventral and dorsal divisions that combine with similar divisions from other levels to form terminal nerves (Fig. 5.36). The anterior ramus of S4 has only a ventral division.
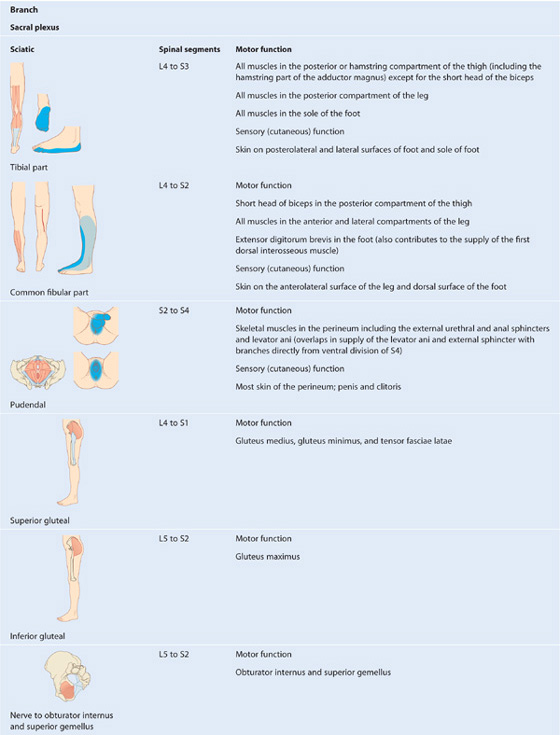
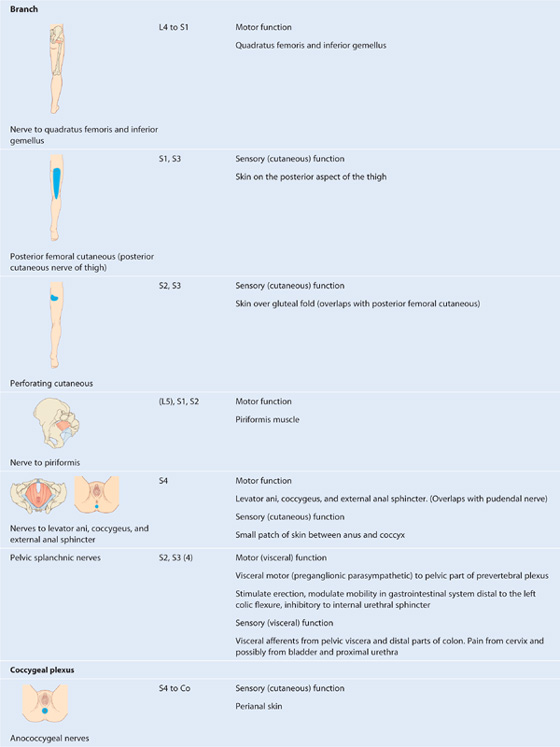
Branches of the sacral plexus include the sciatic nerve and gluteal nerves, which are major nerves of the lower limb, and the pudendal nerve, which is the nerve of the perineum (Table 5.4). Numerous smaller branches supply the pelvic wall, floor, and lower limb.
Table 5.4 Branches of the sacral and coccygeal plexuses (spinal segments in parentheses do not consistently participate)
Most nerves originating from the sacral plexus leave the pelvic cavity by passing through the greater sciatic foramen inferior to piriformis muscle, and enter the gluteal region of the lower limb. Other nerves leave the pelvic cavity using different routes; a few nerves do not leave the pelvic cavity and course directly into the muscles in the pelvic cavity. Finally, two nerves that leave the pelvic cavity through the greater sciatic foramen loop around the ischial spine and sacrospinous ligament and pass medially through the lesser sciatic foramen to supply structures in the perineum and lateral pelvic wall.
Sciatic nerve. The sciatic nerve is the largest nerve of the body and carries contributions from L4 to S3 (Table 5.4, Figs. 5.35, 5.36). It:
 innervates muscles in the posterior compartment of the thigh and muscles in the leg and foot; and
innervates muscles in the posterior compartment of the thigh and muscles in the leg and foot; and
 carries sensory fibers from the skin of the foot and lateral leg.
carries sensory fibers from the skin of the foot and lateral leg.
Pudendal nerve. The pudendal nerve forms anteriorly to the lower part of piriformis muscle from ventral divisions of S2 to S4 (Table 5.5; also see Figs. 5.35, 5.36). It:
Table 5.5 Muscles of the anal triangle

 is accompanied throughout its course by the internal pudendal vessels; and
is accompanied throughout its course by the internal pudendal vessels; and
Clinical app
Pudendal block
Pudendal block anesthesia is performed to relieve the pain associated with childbirth. Although the use of this procedure is less common since the widespread adoption of edipural anesthesia, it provides an excellent option for women who have a contraindication to neuraxial anesthesia (e.g., spinal anatomy, low platelets, too close to delivery). Pudendal blocks are also used for certain types of chronic pelvic pain. The injection is usually given where the pudendal nerve crosses the lateral aspect of the sacrospinous ligament near its attachment to the ischial spine. During childbirth, a finger inserted into the vagina can palpate the ischial spine. The needle is passed transcutaneously to the medial aspect of the ischial spine and around the sacrospinous ligament. Infiltration is performed and the perineum is anesthetized.
Other branches of the sacral plexus (see Table 5.4). Other branches of the sacral plexus include:
 sensory nerves to skin over the inferior gluteal region and posterior aspects of the thigh and upper leg (perforating cutaneous nerve and posterior cutaneous nerve of the thigh) (see Figs. 5.35, 5.36).
sensory nerves to skin over the inferior gluteal region and posterior aspects of the thigh and upper leg (perforating cutaneous nerve and posterior cutaneous nerve of the thigh) (see Figs. 5.35, 5.36).
The superior gluteal nerve leaves the pelvic cavity through the greater sciatic foramen superior to the piriformis muscle and supplies muscles in the gluteal region.
The inferior gluteal nerve leaves the pelvic cavity through the greater sciatic foramen inferior to the piriformis muscle and supplies the gluteus maximus.
The nerve to the obturator internus and the associated superior gemellus muscle leaves the pelvic cavity through the greater sciatic foramen inferior to the piriformis muscle. Like the pudendal nerve, it passes around the ischial spine and through the lesser sciatic foramen to enter the perineum and supply the obturator internus muscle from the medial side of the muscle, inferior to the attachment of the levator ani muscle.
The nerve to the quadratus femoris muscle and the inferior gemellus muscle, and the posterior cutaneous nerve of the thigh (posterior femoral cutaneous nerve) also leave the pelvic cavity through the greater sciatic foramen inferior to the piriformis muscle and course to muscles and skin, respectively, in the lower limb.
Unlike most of the other nerves originating from the sacral plexus, which leave the pelvic cavity through the greater sciatic foramen either above or below the piriformis muscle, the perforating cutaneous nerve leaves the pelvic cavity by penetrating directly through the sacrotuberous ligament and then courses to skin over the inferior aspect of the buttocks.
The nerve to the piriformis and a number of small nerves to the levator ani and coccygeus muscles originate from the sacral plexus and pass directly into their target muscles without leaving the pelvic cavity.
The small coccygeal plexus has a minor contribution from S4 and is formed mainly by the anterior rami of S5 and Co, which originate inferiorly to the pelvic floor. They penetrate the coccygeus muscle to enter the pelvic cavity and join with the anterior ramus of S4 to form a single trunk, from which small anococcygeal nerves originate (see Table 5.4). These nerves penetrate the muscle and the overlying sacrospinous and sacrotuberous ligaments and pass superficially to innervate skin in the anal triangle of the perineum.
Visceral plexuses
Paravertebral sympathetic chain
The paravertebral part of the visceral nervous system is represented in the pelvis by the inferior ends of the sympathetic trunks (Fig. 5.38A). Each trunk enters the pelvic cavity from the abdomen by passing over the ala of the sacrum medially to the lumbosacral trunks and posteriorly to the iliac vessels. The trunks course inferiorly along the anterior surface of the sacrum, where they are positioned medially to the anterior sacral foramina. Four ganglia occur along each trunk. Anteriorly to the coccyx, the two trunks join to form a single small terminal ganglion (the ganglion impar).
The principal function of the sympathetic trunks in the pelvis is to deliver postganglionic sympathetic fibers to the anterior rami of sacral nerves for distribution to the periphery, mainly to parts of the lower limb and perineum. This is accomplished by gray rami communicantes, which connect the trunks to the sacral anterior rami.
In addition to gray rami communicantes, other branches (the sacral splanchnic nerves) join and contribute to the pelvic part of the prevertebral plexus associated with innervating pelvic viscera.
Pelvic extensions of the prevertebral plexus
The pelvic parts of the prevertebral plexus carry sympathetic, parasympathetic, and visceral afferent fibers (see Fig. 5.38A). Pelvic parts of the plexus are associated with innervating pelvic viscera and erectile tissues of the perineum.
The prevertebral plexus enters the pelvis as two hypogastric nerves, one on each side, that cross the pelvic inlet medially to the internal iliac vessels. The hypogastric nerves are formed by the separation of the fibers in the superior hypogastric plexus into right and left bundles. The superior hypogastric plexus is situated anterior to vertebra LV between the promontory of the sacrum and the bifurcation of the aorta.
When the hypogastric nerves are joined by pelvic splanchnic nerves carrying preganglionic parasympathetic fibers from S2 to S4, the pelvic plexuses (inferior hypogastric plexuses) are formed (Fig. 5.38). The inferior hypogastric plexuses, one on each side, course in an inferior direction around the pelvic walls, medially to major vessels and somatic nerves. They give origin to the following subsidiary plexuses, which innervate the pelvic viscera:
Terminal branches of the inferior hypogastric plexuses penetrate and pass through the deep perineal pouch and innervate erectile tissues of the penis and the clitoris in the perineum (Fig. 5.38B). In men, these nerves, called cavernous nerves, are extensions of the prostatic plexus. The pattern of distribution of similar nerves in women is not entirely clear, but they are likely extensions of the uterovaginal plexus.
Sympathetic fibers enter the inferior hypogastric plexuses from the hypogastric nerves and from branches (sacral splanchnic nerves) of the upper sacral parts of the sympathetic trunks (see Fig. 5.38A). Ultimately, these nerves are derived from preganglionic fibers that leave the spinal cord in the anterior roots, mainly of T10 to L2. These fibers:
Parasympathetic fibers enter the pelvic plexus in pelvic splanchnic nerves that originate from spinal cord levels S2 to S4 (Fig. 5.38). They:
 stimulate bladder contraction,
stimulate bladder contraction,
Visceral afferent fibers follow the course of the sympathetic and parasympathetic fibers to the spinal cord. Afferent fibers that enter the cord in lower thoracic levels and lumbar levels with sympathetic fibers generally carry pain; however, pain fibers from the cervix and some pain fibers from the bladder and urethra may accompany parasympathetic nerves to sacral levels of the spinal cord.
Clinical app
Prostatectomy and impotence
It may be necessary to perform radical surgery to cure cancer of the prostate. To do this, the prostate and its attachments around the base of the bladder, including the seminal vesicles, must be removed en masse. Parts of the inferior hypogastric plexus in this region give rise to nerves that innervate the erectile tissues of the penis. Impotence may occur if these nerves cannot or are not preserved during removal of the prostate.
For the same reasons, women may experience sexual dysfunction if similar nerves are damaged during pelvic surgery, for example, during a total hysterectomy.
Blood vessels
Arteries
The major artery of the pelvis and perineum is the internal iliac artery on each side (Figs. 5.39, 5.40). In addition to providing a blood supply to most of the pelvic viscera, pelvic walls and floor, and structures in the perineum, including erectile tissues of the clitoris and the penis, this artery gives rise to branches that follow nerves into the gluteal region of the lower limb. Other vessels that originate in the abdomen and contribute to the supply of pelvic structures include the median sacral artery and, in women, the ovarian arteries.
Fig. 5.39 Branches of the posterior trunk of the internal iliac artery.
Fig. 5.40 Branches of the anterior trunk of the internal iliac artery. A. Male. B. Female.
Internal iliac artery
The internal iliac artery originates from the common iliac artery on each side, approximately at the level of the intervertebral disc between LV and SI and lies anteromedial to the sacro-iliac joint (Fig. 5.39). The vessel courses inferiorly over the pelvic inlet, then divides into anterior and posterior trunks at the level of the superior border of the greater sciatic foramen. Branches from the posterior trunk contribute to the supply of the lower posterior abdominal wall, the posterior pelvic wall, and the gluteal region. Branches from the anterior trunk supply the pelvic viscera, the perineum, the gluteal region, the adductor region of the thigh, and, in the fetus, the placenta.
Branches of the posterior trunk include the following (Fig. 5.39):
Branches of the anterior trunk of the internal iliac artery include the following (Fig. 5.40):
 The first branch of the anterior trunk is the umbilical artery, which gives origin to the superior vesical artery, then travels forward just inferior to the margin of the pelvic inlet. Anteriorly, the vessel leaves the pelvic cavity and ascends on the internal aspect of the anterior abdominal wall to reach the umbilicus. In the fetus, the umbilical artery is large and carries blood from the fetus to the placenta. After birth, the vessel closes distally to the origin of the superior vesical artery and eventually becomes a solid fibrous cord. On the anterior abdominal wall, the cord raises a fold of peritoneum termed the medial umbilical fold. The fibrous remnant of the umbilical artery itself is the medial umbilical ligament.
The first branch of the anterior trunk is the umbilical artery, which gives origin to the superior vesical artery, then travels forward just inferior to the margin of the pelvic inlet. Anteriorly, the vessel leaves the pelvic cavity and ascends on the internal aspect of the anterior abdominal wall to reach the umbilicus. In the fetus, the umbilical artery is large and carries blood from the fetus to the placenta. After birth, the vessel closes distally to the origin of the superior vesical artery and eventually becomes a solid fibrous cord. On the anterior abdominal wall, the cord raises a fold of peritoneum termed the medial umbilical fold. The fibrous remnant of the umbilical artery itself is the medial umbilical ligament.
 The uterine artery in women courses medially and anteriorly in the base of the broad ligament to reach the cervix (Figs. 5.40B, 5.41). Along its course, the vessel crosses the ureter and passes superiorly to the lateral vaginal fornix. Once the vessel reaches the cervix, it ascends along the lateral margin of the uterus to reach the uterine tube, where it curves laterally and anastomoses with the ovarian artery. The uterine artery is the major blood supply to the uterus and enlarges significantly during pregnancy. Through anastomoses with other arteries, the vessel contributes to the blood supply of the ovaries and vagina as well.
The uterine artery in women courses medially and anteriorly in the base of the broad ligament to reach the cervix (Figs. 5.40B, 5.41). Along its course, the vessel crosses the ureter and passes superiorly to the lateral vaginal fornix. Once the vessel reaches the cervix, it ascends along the lateral margin of the uterus to reach the uterine tube, where it curves laterally and anastomoses with the ovarian artery. The uterine artery is the major blood supply to the uterus and enlarges significantly during pregnancy. Through anastomoses with other arteries, the vessel contributes to the blood supply of the ovaries and vagina as well.
Fig. 5.41 Uterine and vaginal arteries.
Ovarian arteries
In women, the gonadal (ovarian) vessels originate from the abdominal aorta and then descend to cross the pelvic inlet and supply the ovaries (see Fig. 5.41). They anastomose with terminal parts of the uterine arteries. On each side, the vessels travel in the suspensory ligament of ovary (the infundibulopelvic ligament) as they cross the pelvic inlet to the ovary. Branches pass through the mesovarium to reach the ovary and through the mesometrium of the broad ligament to anastomose with the uterine artery. The ovarian arteries enlarge significantly during pregnancy to augment uterine blood supply.
Median sacral artery
The median sacral artery (see Figs. 5.40A and 5.41) originates from the posterior surface of the aorta just superior to the aortic bifurcation at vertebral level LIV in the abdomen. It descends in the midline, crosses the pelvic inlet, and then courses along the anterior surface of the sacrum and coccyx. It gives rise to the last pair of lumbar arteries and to branches that anastomose with the iliolumbar and lateral sacral arteries.
Veins
Pelvic veins follow the course of all branches of the internal iliac artery except for the umbilical artery and the iliolumbar artery (Fig. 5.42A). On each side, the veins drain into internal iliac veins, which leave the pelvic cavity to join common iliac veins situated just superior and lateral to the pelvic inlet.
Within the pelvic cavity, extensive interconnected venous plexuses are associated with the surfaces of the viscera (bladder, rectum, prostate, uterus, and vagina). Together, these plexuses form the pelvic plexus of veins. The part of the venous plexus surrounding the rectum and anal canal drains via superior rectal veins (tributaries of inferior mesenteric veins) into the hepatic portal system, and via middle and inferior rectal veins into the caval system. This pelvic plexus is an important portacaval shunt when the hepatic portal system is blocked (Fig. 5.42B).
The inferior part of the rectal venous plexus around the anal canal has two parts, an internal and an external. The internal rectal venous plexus is in connective tissue between the internal anal sphincter and the epithelium lining the canal. This plexus connects superiorly with longitudinally arranged branches of the superior rectal vein that lie one in each anal column. The external rectal venous plexus circles the external anal sphincter and is subcutaneous.
The single deep dorsal vein that drains erectile tissues of the clitoris and the penis passes directly into the pelvic cavity through a gap formed between the arcuate pubic ligament and the anterior margin of the perineal membrane. The vein joins the prostatic plexus of veins in men and the vesical (bladder) plexus of veins in women. Superficial veins that drain the skin of the penis and corresponding regions of the clitoris drain into the external pudendal veins, which are tributaries of the great saphenous vein in the thigh.
In addition to tributaries of the internal iliac vein, median sacral veins and ovarian veins parallel the courses of the median sacral artery and ovarian artery, respectively, and leave the pelvic cavity to join veins in the abdomen:
Lymphatics
Lymphatics from most pelvic viscera drain mainly into lymph nodes distributed along the internal iliac and external iliac arteries and their associated branches (Fig. 5.43), which drain into nodes associated with the common iliac arteries and then into the lateral aortic or lumbar nodes associated with the lateral surfaces of the abdominal aorta. In turn, these lateral aortic or lumbar nodes drain into the lumbar trunks, which continue to the origin of the thoracic duct at approximately vertebral level TXII.
Fig. 5.43 Pelvic lymphatics.
Lymphatics from the ovaries and related parts of the uterus and uterine tubes leave the pelvic cavity superiorly and drain, via vessels that accompany the ovarian arteries, directly into lateral aortic or lumbar nodes and, in some cases, into the pre-aortic nodes on the anterior surface of the aorta.
In addition to draining pelvic viscera, nodes along the internal iliac artery also receive drainage from the gluteal region of the lower limb and from deep areas of the perineum.
Hemorrhoids
A hemorrhoid is an engorgement of veins related to the anal sphincter. Hemorrhoids have a slight genetic predisposition; however, straining during bowel movements, obesity, and sedentary life style can also produce hemorrhoids, as can portal hypertension. The symptoms include irritation, pain, and swelling. Internal hemorrhoids originate from the internal rectal venous plexus that occurs inside the rectum and have a tendency to bleed. Prolapsed hemorrhoids are internal hemorrhoids that pass outside the anal canal and form lumps, which may undergo thrombosis and become painful. External hemorrhoids originate from the external rectal plexus and occur at the distal boundary of the anal canal.
PERINEUM
The perineum is a diamond-shaped region positioned inferiorly to the pelvic floor between the thighs. Its peripheral boundary is the pelvic outlet; its ceiling is the pelvic diaphragm (the levator ani and coccygeus muscles); and its narrow lateral walls are formed by the walls of the pelvic cavity below the attachment of the levator ani muscle (Fig. 5.44A).
Fig. 5.44 Borders and ceiling of the perineum. A. Boundaries of the perineum. B. Perineal membrane.
The perineum is divided into an anterior urogenital triangle and a posterior anal triangle.
 The anal triangle contains the anus and the external anal sphincter.
The anal triangle contains the anus and the external anal sphincter.
The pudendal nerve (S2 to S4) and the internal pudendal artery are the major nerve and artery of the region.
Borders and ceiling
The margin of the perineum is marked by the inferior border of the pubic symphysis at its anterior point, the tip of the coccyx at its posterior point, and the ischial tuberosities at each of the lateral points (Fig. 5.44A). The lateral margins are formed by the ischiopubic rami anteriorly and by the sacrotuberous ligaments posteriorly.
The perineum is divided into two triangles by an imaginary line between the two ischial tuberosities (Fig. 5.44A). Anterior to the line is the urogenital triangle and posterior to the line is the anal triangle. Significantly, the two triangles are not in the same plane. In the anatomical position, the urogenital triangle is oriented in the horizontal plane, whereas the anal triangle is tilted upward at the transtubercular line so that it faces more posteriorly.
The roof of the perineum is formed mainly by the levator ani muscles that separate the pelvic cavity, above, from the perineum, below. These muscles, one on each side, form a cone- or funnel-shaped pelvic diaphragm, with the anal aperture at its inferior apex in the anal triangle.
Surface anatomy
Defining the margins of the perineum
The pubic symphysis, ischial tuberosities, and tip of the sacrum are palpable on patients and can be used to define the boundaries of the perineum. This is best done with patients lying on their backs with their thighs flexed and abducted in the lithotomy position (Fig. 5.45).
Imaginary lines that join the ischial tuberosities with the pubic symphysis in front, and with the tip of the coccyx behind, outline the diamond-shaped perineum. An additional line between the ischial tuberosities divides the perineum into two triangles, the urogenital triangle anteriorly and anal triangle posteriorly. This line also approximates the position of the posterior margin of the perineal membrane. The midpoint of this line marks the location of the perineal body or central tendon of the perineum.
Perineal membrane and deep perineal pouch
The perineal membrane (see p. 218) is a thick fibrous sheet that fills the urogenital triangle (Fig. 5.44B). It has a free posterior border, which is anchored in the midline to the perineal body and is attached laterally to the pubic arch. Immediately superior to the perineal membrane is a thin region termed the deep perineal pouch, containing a layer of skeletal muscle and neurovascular tissues. Among the skeletal muscles in the pouch (see p. 218, Fig. 5.18) is the external urethral sphincter.
The perineal membrane and deep perineal pouch provide support for the external genitalia, which are attached to its inferior surface. Also, the parts of the perineal membrane and deep perineal pouch inferior to the urogenital hiatus in the levator ani provide support for pelvic viscera, above.
The urethra leaves the pelvic cavity and enters the perineum by passing through the deep perineal pouch and perineal membrane. In women, the vagina also passes through these structures posterior to the urethra.
Ischio-anal fossae and their anterior recesses
Because the levator ani muscles course medially from their origin on the lateral pelvic walls, above, to the anal aperture and urogenital hiatus, below, inverted wedge-shaped gutters occur between the levator ani muscles and adjacent pelvic walls as the two structures diverge inferiorly (Fig. 5.46). In the anal triangle, these gutters, one on each side of the anal aperture, are termed ischio-anal fossae. The lateral wall of each fossa is formed mainly by the ischium, obturator internus muscle, and the sacrotuberous ligament. The medial wall is the levator ani muscle. The medial and lateral walls converge superiorly where the levator ani muscle attaches to the fascia overlying the obturator internus muscle. The ischio-anal fossae allow movement of the pelvic diaphragm and expansion of the anal canal during defecation.
The ischio-anal fossae of the anal triangle are continuous anteriorly with recesses that project into the urogenital triangle superior to the deep perineal pouch. The ischio-anal fossae and their anterior recesses are normally filled with fat.
Clinical app
Abscesses in the ischio-anal fossae
The anal mucosa is particularly vulnerable to injury and may be easily torn by hard feces. Occasionally, patients develop inflammation and infection of the anal canal (sinuses or crypts), which can spread laterally into the ischio-anal fossae or superiorly into the pelvic cavity.
Anal triangle
The anal triangle of the perineum faces posteroinferiorly and is defined laterally by the medial margins of the sacrotuberous ligaments, anteriorly by a horizontal line between the two ischial tuberosities, and posteriorly by the coccyx. The ceiling of the anal triangle is the pelvic diaphragm, which is formed by the levator ani and coccygeus muscles. The anal aperture occurs centrally in the anal triangle and is related on either side to an ischio-anal fossa. The major muscle in the anal triangle is the external anal sphincter.
The external anal sphincter, which surrounds the anal canal, is formed by skeletal muscle and consists of three parts—deep, superficial, and subcutaneous—arranged sequentially along the canal from superior to inferior (Table 5.5, see Fig. 5.44B). The external anal sphincter is innervated by inferior rectal branches of the pudendal nerve and by branches directly from the anterior ramus of S4.
Urogenital triangle
The urogenital triangle of the perineum is the anterior half of the perineum and is oriented in the horizontal plane. It contains the roots of the external genitalia (Fig. 5.47) and the openings of the urogenital system.
Fig. 5.47 Erectile tissues of clitoris and penis. A. Clitoris. B. Penis.
The urogenital triangle is defined (see Fig. 5.44A):
 laterally by the ischiopubic rami,
laterally by the ischiopubic rami,
 posteriorly by an imaginary line between the ischial tuberosities, and
posteriorly by an imaginary line between the ischial tuberosities, and
 anteriorly by the inferior margin of the pubic symphysis.
anteriorly by the inferior margin of the pubic symphysis.
As with the anal triangle, the roof or ceiling of the urogenital triangle is the levator ani muscle.
Unlike the anal triangle, the urogenital triangle contains a strong fibromuscular support platform, the perineal membrane, and deep perineal pouch (see p. 218), which is attached to the pubic arch.
Anterior extensions of the ischio-anal fossae occur between the deep perineal pouch and the levator ani muscle on each side.
Between the perineal membrane and the membranous layer of superficial fascia is the superficial perineal pouch. The principal structures in this pouch are the erectile tissues of the penis and clitoris and associated skeletal muscles.
Structures in the superficial perineal pouch
The superficial perineal pouch contains (Figs. 5.47, 5.48):
Fig. 5.48 Muscles in the superficial perineal pouch. A. In women. B. In men.
 erectile structures that join together to form the penis in men and the clitoris in women; and
erectile structures that join together to form the penis in men and the clitoris in women; and
Each erectile structure consists of a central core of expandable vascular tissue and its surrounding connective tissue capsule.
Erectile tissues
Two sets of erectile structures join to form the penis and the clitoris.
A pair of cylindrically shaped corpora cavernosa, one on each side of the urogenital triangle, are anchored by their proximal ends to the pubic arch (Fig. 5.47). These attached parts are often termed the crura (from the Latin for “legs”) of the clitoris or the penis. The distal ends of the corpora, which are not attached to bone, form the body of the clitoris in women and the dorsal parts of the body of the penis in men.
The second set of erectile tissues surrounds the openings of the urogenital system.
 In women, a pair of erectile structures, termed the bulbs of vestibule, are situated one on each side at the vaginal opening and are firmly anchored to the perineal membrane (Fig. 5.47A). Small bands of erectile tissues connect the anterior ends of these bulbs to a single, small, pea-shaped erectile mass, the glans clitoris, which is positioned in the midline at the end of the body of the clitoris and anterior to the opening of the urethra.
In women, a pair of erectile structures, termed the bulbs of vestibule, are situated one on each side at the vaginal opening and are firmly anchored to the perineal membrane (Fig. 5.47A). Small bands of erectile tissues connect the anterior ends of these bulbs to a single, small, pea-shaped erectile mass, the glans clitoris, which is positioned in the midline at the end of the body of the clitoris and anterior to the opening of the urethra.
 In men, a single large erectile mass, the corpus spongiosum, is the structural equivalent to the bulbs of the vestibule, the glans clitoris, and the interconnecting bands of erectile tissues in women (Fig. 5.47B). The corpus spongiosum is anchored at its base (bulb of penis) to the perineal membrane. Its proximal end, which is not attached, forms the ventral part of the body of the penis and expands over the end of the body of the penis to form the glans penis. In men, the urethra is enclosed by the corpus spongiosum and opens at the end of the penis. This is unlike the situation in women where the urethra is not enclosed by erectile tissue of the clitoris and opens directly into the vestibule of the perineum.
In men, a single large erectile mass, the corpus spongiosum, is the structural equivalent to the bulbs of the vestibule, the glans clitoris, and the interconnecting bands of erectile tissues in women (Fig. 5.47B). The corpus spongiosum is anchored at its base (bulb of penis) to the perineal membrane. Its proximal end, which is not attached, forms the ventral part of the body of the penis and expands over the end of the body of the penis to form the glans penis. In men, the urethra is enclosed by the corpus spongiosum and opens at the end of the penis. This is unlike the situation in women where the urethra is not enclosed by erectile tissue of the clitoris and opens directly into the vestibule of the perineum.
The clitoris is composed of two corpora cavernosa and the glans clitoris (Fig. 5.47A). As in the penis, it has an attached part (root) and a free part (body).
The body of clitoris is supported by a suspensory ligament that attaches superiorly to the pubic symphysis (Fig. 5.48A). The glans clitoris is attached to the distal end of the body and is connected to the bulbs of the vestibule by small bands of erectile tissue. The glans clitoris is exposed in the perineum and the body of the clitoris can be palpated through skin.
The penis is composed mainly of the two corpora cavernosa and the single corpus spongiosum, which contains the urethra (Fig. 5.47B) As in the clitoris, it has an attached part (root) and a free part (body):
The base of the body of penis is supported by two ligaments: the suspensory ligament of penis (attached superiorly to the pubic symphysis), and the more superficially positioned fundiform ligament of penis (attached above to the linea alba of the anterior abdominal wall and splits below into two bands that pass on each side of the penis and unite inferiorly) (Fig. 5.48B).
Because the anatomical position of the penis is erect, the paired corpora are defined as dorsal in the body of the penis and the single corpus spongiosum as ventral, even though the positions are reversed in the nonerect (flaccid) penis.
The corpus spongiosum expands to form the head of penis (glans penis) over the distal ends of the corpora cavernosa (Fig. 5.47B).
Erection
Erection of the penis and clitoris is a vascular event generated by parasympathetic fibers carried in pelvic splanchnic nerves from the anterior rami of S2 to S4, which enter the inferior hypogastric part of the prevertebral plexus and ultimately pass through the deep perineal pouch and perineal membrane to innervate the erectile tissues. Stimulation of these nerves causes specific arteries in the erectile tissues to relax. This allows blood to fill the tissues, causing the penis and clitoris to become erect.
Greater vestibular glands
The greater vestibular glands (Bartholin’s glands) are seen in women. They are small, pea-shaped mucous glands that lie posterior to the bulbs of the vestibule on each side of the vaginal opening and are the female homologues of the bulbourethral glands in men (see Fig. 5.47). However, the bulbourethral glands are located within the deep perineal pouch, whereas the greater vestibular glands are in the superficial perineal pouch.
The duct of each greater vestibular gland opens into the vestibule of the perineum along the posterolateral margin of the vaginal opening.
Like the bulbourethral glands in men, the greater vestibular glands produce secretion during sexual arousal.
Muscles
The superficial perineal pouch contains three pairs of muscles: the ischiocavernosus, bulbospongiosus, and superficial transverse perineal muscles (Table 5.6, Fig. 5.48). Two of these three pairs of muscles are associated with the roots of the penis and clitoris; the other pair is associated with the perineal body.
Table 5.6 Muscles of the superficial perineal pouch

Surface anatomy
Superficial features of the external genitalia in women
In women, the clitoris and vestibular apparatus, together with a number of skin and tissue folds, form the vulva (Fig. 5.49A). On either side of the midline are two thin folds of skin termed the labia minora. The region enclosed between them, and into which the urethra and vagina open, is the vestibule. Anteriorly, the labia minora each bifurcate, forming a medial and a lateral fold. The medial folds unite to form the frenulum of clitoris, that joins the glans clitoris (Fig. 5.49B). The lateral folds unite ventrally over the glans clitoris and the body of clitoris to form the prepuce of clitoris (hood) (Fig. 5.49B). The body of the clitoris extends anteriorly from the glans clitoris and is palpable deep to the prepuce and related skin. Posterior to the vestibule, the labia minora unite, forming a small transverse fold, the frenulum of labia minora (the fourchette) Fig. 5.49C).
Fig. 5.49 Structures in the urogenital triangle of a woman. A. Inferior view of the urogenital triangle of a woman with major features indicated. B. Inferior view of the vestibule. The labia minora have been pulled apart to open the vestibule. Also indicated are the glans clitoris, the clitoral hood, and the frenulum of the clitoris. C. Inferior view of the vestibule showing the urethral and vaginal orifices and the hymen. The labia minora have been pulled further apart than in Figure 5.49B. D. Inferior view of the vestibule with the left labium minus pulled to the side to show the regions of the vestibule into which the greater vestibular and para-urethral glands open. E. View through the vaginal canal of the cervix. F. Inferior view of the urogenital triangle of a woman with the erectile tissues of the clitoris and vestibule and the greater vestibular glands indicated with overlays.
Within the vestibule, the vaginal orifice is surrounded to varying degrees by a ringlike fold of membrane, the hymen, which may have a small central perforation or may completely close the vaginal opening. Following rupture of the hymen (resulting from first sexual intercourse or injury), irregular remnants of the hymen fringe the vaginal opening (Fig. 5.49C).
The orifices of the urethra and the vagina are associated with the openings of glands. The ducts of the para-urethral glands (Skene’s glands) open into the vestibule, one on each side of the lateral margin of the urethra (Fig. 5.49D). The ducts of the greater vestibular glands (Bartholin’s glands) open adjacent to the posterolateral margin of the vaginal opening in the crease between the vaginal orifice and remnants of the hymen (Fig. 5.49D).
Lateral to the labia minora are two broad folds, the labia majora, which unite anteriorly to form the mons pubis (Fig. 5.49A). The mons pubis overlies the inferior aspect of the pubic symphysis and is anterior to the vestibule and the clitoris. Posteriorly, the labia majora do not unite and are separated by a depression termed the posterior commissure, which overlies the position of the perineal body (Fig. 5.49A).
The cervix is visible when the vaginal canal is opened with a speculum (Fig. 5.49E). The external cervical os opens onto the surface of the dome-shaped cervix. A recess or gutter, termed the fornix, occurs between the cervix and the vaginal wall and is further subdivided, based on location, into anterior, posterior, and lateral fornices.
The roots of the clitoris occur deep to surface features of the perineum and are attached to the ischiopubic rami and the perineal membrane.
The bulbs of the vestibule (Fig. 5.49F), composed of erectile tissues, lie deep to the labia minora on either side of the vestibule. These erectile masses are continuous, via thin bands of erectile tissues, with the glans clitoris, which is visible under the clitoral hood. The greater vestibular glands occur posterior to the bulbs of the vestibule on either side of the vaginal orifice.
The crura of clitoris are attached, one on each side, to the ischiopubic rami. Each crus is formed by the attached part of the corpus cavernosum. Anteriorly, these erectile corpora detach from bone, curve posteroinferiorly, and unite to form the body of the clitoris.
The body of clitoris underlies the ridge of skin immediately anterior to the clitoral hood (prepuce). The glans clitoris is positioned at the end of the body of clitoris.
Superficial features of the external genitalia in men
Superficial components of the genital organs in men consist of the scrotum and the penis (Fig. 5.50A). The urogenital triangle itself contains the root of the penis; however, the testes and associated structures, although they migrate into the scrotum from the abdomen, are generally evaluated with the penis during a physical examination.
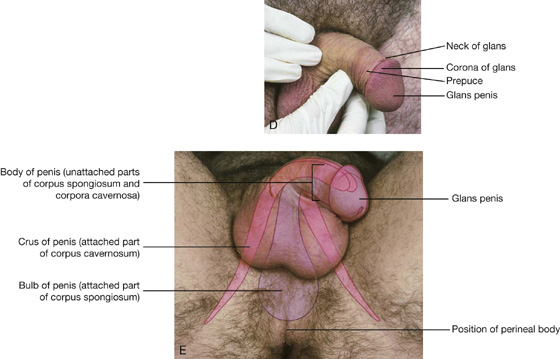
The scrotum in men is homologous to the labia majora in women. Each oval testis is readily palpable through the skin of the scrotum (Fig. 5.50A). Posterolateral to the testis is an elongated mass of tissue, often visible as a raised ridge that contains lymphatics and blood vessels of the testis, and the epididymis and ductus deferens. A midline raphe (Fig. 5.50B) is visible on the skin separating left and right sides of the scrotum. In some individuals, this raphe is prominent and extends from the anal aperture, over the scrotum and along the ventral surface of the body of the penis, to the frenulum of the glans.
The external urethral orifice is a sagittal slit, normally positioned at the tip of the glans (Fig. 5.50C). The inferior margin of the urethral orifice is continuous with a midline raphe of penis, which represents a line of fusion formed in the glans as the urethra develops in the fetus. The base of this raphe is continuous with the frenulum of the glans, which is a median fold of skin that attaches the glans to more loosely attached skin proximal to the glans. The base of the glans is expanded to form a raised circular margin (the corona of glans) (Fig. 5.50D); the two lateral ends of the corona join inferiorly at the midline raphe of the glans. The depression posterior to the corona is the neck of the glans. Normally, a fold of skin at the neck of the glans is continuous anteriorly with thin skin that tightly adheres to the glans and posteriorly with thicker skin loosely attached to the body. This fold, known as the prepuce, extends forward to cover the glans. The prepuce is removed during male circumcision, leaving the glans exposed.
The root of the penis is formed by the attached parts of the corpus spongiosum and the corpora cavernosa. The corpus spongiosum is attached to the perineal membrane and can be easily palpated as a large mass anterior to the perineal body. This mass, which is covered by the bulbospongiosus muscles, is the bulb of penis (Fig. 5.50E).
The corpus spongiosum detaches from the perineal membrane anteriorly, becomes the ventral part of the body of penis (shaft of penis), and eventually terminates as the expanded glans penis.
The crura of the penis, one crus on each side, are the attached parts of the corpora cavernosa and are anchored to the ischiopubic rami (Fig. 5.50E). The corpora cavernosa are unattached anteriorly and become the paired erectile masses that form the dorsal part of the body of the penis. The glans penis caps the anterior ends of the corpora cavernosa.
Superficial fascia of the urogenital triangle
The superficial fascia of the urogenital triangle is continuous with similar fascia on the anterior abdominal wall (Fig. 5.51).
Fig. 5.51 Superficial fascia. A. Lateral view. B. Anterior view.
As with the superficial fascia of the abdominal wall, the perineal fascia has a membranous layer on its deep surface. This membranous layer (Colles’ fascia) (Fig. 5.51), is attached:
 posteriorly to the perineal membrane and therefore does not extend into the anal triangle; and
posteriorly to the perineal membrane and therefore does not extend into the anal triangle; and
It defines the external limits of the superficial perineal pouch, lines the scrotum or labia, and extends around the body of the penis and clitoris (Fig. 5.51A).
Anteriorly, the membranous layer of fascia is continuous over the pubic symphysis and pubic bones with the membranous layer of fascia on the anterior abdominal wall. In the lower lateral abdominal wall, the membranous layer of abdominal fascia is attached to the deep fascia of the thigh just inferior to the inguinal ligament (Fig. 5.51).
Because the membranous layer of fascia encloses the superficial perineal pouch and continues up the anterior abdominal wall, fluids or infectious material that accumulate in the pouch can track out of the perineum and onto the lower abdominal wall. This material will not track into the anal triangle or the thigh because the fascia fuses with deep tissues at the borders of these regions.
Urethral rupture
Urethral rupture may occur at a series of well-defined anatomical points.
The most common injury is a rupture of the proximal spongy urethra below the perineal membrane. The urethra is usually torn when structures of the perineum are caught between a hard object (e.g., a steel beam or cross bar of a bicycle) and the inferior pubic arch. Urine escapes through the rupture into the superficial perineal pouch and descends into the scrotum and onto the anterior abdominal wall deep to the superficial fascia.
In association with severe pelvic fractures, urethral rupture may occur at the prostatomembranous junction above the deep perineal pouch. The urine will extravasate into the true pelvis.
The worst and most serious urethral rupture is related to serious pelvic injuries where there is complete disruption of the puboprostatic ligaments. The prostate is dislocated superiorly not only by the ligamentous disruption but also by the extensive hematoma formed within the true pelvis. The diagnosis can be made by palpating the elevated prostate during a digital rectal examination.
Somatic nerves
Pudendal nerve
The major somatic nerve of the perineum is the pudendal nerve (see p. 236 and Fig. 5.52A). As it enters and courses through the perineum, it travels along the lateral wall of the ischio-anal fossa in the pudendal canal, which is a tubular compartment formed in the fascia that covers the obturator internus muscle. This pudendal canal also contains the internal pudendal artery and accompanying veins (Fig. 5.52A).
Fig. 5.52 Pudendal nerve. A. In men. B. In women.
The pudendal nerve has three major terminal branches—the inferior rectal, perineal nerves, and the dorsal nerve of penis or clitoris—which are accompanied by branches of the internal pudendal artery (Fig. 5.52B).
 The dorsal nerve of penis and clitoris enters the deep perineal pouch (Fig. 5.52). It passes along the lateral margin of the pouch and then exits by passing inferiorly through the perineal membrane in a position just inferior to the pubic symphysis where it meets the body of the clitoris or the penis. It courses along the dorsal surface of the body to reach the glans. The dorsal nerve is sensory to the penis and clitoris, particularly to the glans.
The dorsal nerve of penis and clitoris enters the deep perineal pouch (Fig. 5.52). It passes along the lateral margin of the pouch and then exits by passing inferiorly through the perineal membrane in a position just inferior to the pubic symphysis where it meets the body of the clitoris or the penis. It courses along the dorsal surface of the body to reach the glans. The dorsal nerve is sensory to the penis and clitoris, particularly to the glans.
Other somatic nerves
Other somatic nerves that enter the perineum are mainly sensory and include branches of the ilio-inguinal, genitofemoral, posterior femoral cutaneous, and anococcygeal nerves.
Visceral nerves
Visceral nerves enter the perineum by two routes:
 Those to the skin, which consist mainly of postganglionic sympathetics, are delivered into the region along the pudendal nerve (see Fig. 5.37). These fibers join the pudendal nerve from gray rami communicantes that connect pelvic parts of the sympathetic trunks to the anterior rami of the sacral spinal nerves.
Those to the skin, which consist mainly of postganglionic sympathetics, are delivered into the region along the pudendal nerve (see Fig. 5.37). These fibers join the pudendal nerve from gray rami communicantes that connect pelvic parts of the sympathetic trunks to the anterior rami of the sacral spinal nerves.
 Those to erectile tissues enter the region mainly by passing through the deep perineal pouch from the inferior hypogastric plexus in the pelvic cavity (see Fig. 5.38). The fibers that stimulate erection are parasympathetic fibers, which enter the inferior hypogastric plexus via pelvic splanchnic nerves from spinal cord levels of S2 to S4.
Those to erectile tissues enter the region mainly by passing through the deep perineal pouch from the inferior hypogastric plexus in the pelvic cavity (see Fig. 5.38). The fibers that stimulate erection are parasympathetic fibers, which enter the inferior hypogastric plexus via pelvic splanchnic nerves from spinal cord levels of S2 to S4.
Blood vessels
Arteries
The most significant artery of the perineum is the internal pudendal artery (Fig. 5.53). Other arteries entering the area include the external pudendal, the testicular, and the cremasteric arteries.
Fig. 5.53 Arteries in the perineum.
Internal pudendal artery
The internal pudendal artery originates as a branch of the anterior trunk of the internal iliac artery in the pelvis (Fig. 5.53) and accompanies the pudendal nerve in the pudendal canal on the lateral wall of the ischio-anal fossa.
The branches of the internal pudendal artery are similar to those of the pudendal nerve in the perineum and include the inferior rectal and perineal arteries, and branches to the erectile tissues of the penis and clitoris (Fig. 5.53).
One or more inferior rectal arteries originate from the internal pudendal artery in the anal triangle and cross the ischio-anal fossa medially to branch and supply muscle and related skin (Fig. 5.53). They anastomose with middle and superior rectal arteries from the internal iliac artery and the inferior mesenteric artery, respectively, to form a network of vessels that supply the rectum and anal canal.
The perineal artery originates near the anterior end of the pudendal canal and gives off a transverse perineal branch, and a posterior scrotal or labial artery to surrounding tissues and skin (see Fig. 5.53).
Terminal part of the internal pudendal artery
The terminal part of the internal pudendal artery accompanies the dorsal nerve of the penis or clitoris into the deep perineal pouch and supplies branches to the tissues in the deep perineal pouch and erectile tissues.
Branches that supply the erectile tissues in men include the artery to the bulb of the penis, the urethral artery, the deep artery of the penis, and the dorsal artery of the penis (see Fig. 5.53).
Branches that supply the erectile tissues in women are similar to those in men.
 Arteries of the bulb of vestibule supply the bulb of the vestibule and related vagina.
Arteries of the bulb of vestibule supply the bulb of the vestibule and related vagina.
 Deep arteries of the clitoris supply the crura and corpus cavernosum of the body.
Deep arteries of the clitoris supply the crura and corpus cavernosum of the body.
 Dorsal arteries of the clitoris supply surrounding tissues and the glans.
Dorsal arteries of the clitoris supply surrounding tissues and the glans.
External pudendal arteries
The external pudendal arteries consist of a superficial vessel and a deep vessel, which originate from the femoral artery in the thigh. They course medially to enter the perineum anteriorly and supply related skin of the penis and scrotum or the clitoris and labia majora.
Testicular and cremasteric arteries
In men, the testicular arteries originate from the abdominal aorta and descend into the scrotum through the inguinal canal to supply the testes. Also, cremasteric arteries, which originate from the inferior epigastric branch of the external iliac artery, accompany the spermatic cord into the scrotum.
In women, small cremasteric arteries follow the round ligament of the uterus through the inguinal canal.
Veins
Veins in the perineum generally accompany the arteries and join the internal pudendal veins that connect with the internal iliac vein in the pelvis (Fig. 5.54). The exception is the deep dorsal vein of penis or clitoris that drains mainly the glans and the corpora cavernosa. The deep dorsal vein courses along the midline between the dorsal arteries on each side of the body of penis or clitoris, passes though the gap between the inferior pubic ligament and the deep perineal pouch, and connects with the plexus of veins surrounding the prostate in men or bladder in women.
Fig. 5.54 Perineal veins.
External pudendal veins, which drain anterior parts of the labia majora or the scrotum and overlap with the area of drainage of the internal pudendal veins, connect with the femoral vein in the thigh. Superficial dorsal veins of the penis or clitoris that drain skin are tributaries of the external pudendal veins.
Lymphatics
Lymphatic vessels from deep parts of the perineum accompany the internal pudendal blood vessels and drain mainly into internal iliac nodes in the pelvis.
Lymphatic channels from superficial tissues of the penis or the clitoris accompany the superficial external pudendal blood vessels and drain mainly into superficial inguinal nodes, as do lymphatic channels from the scrotum or labia majora (Fig. 5.55). The glans penis, the glans clitoris, labia minora, and the terminal inferior end of the vagina drain into deep inguinal nodes and external iliac nodes.
Fig. 5.55 Lymphatic drainage of the perineum.
Lymphatics from the testes drain via channels that ascend in the spermatic cord, pass through the inguinal canal, and course up the posterior abdominal wall to connect directly with lateral aortic or lumbar nodes and pre-aortic nodes around the aorta, at approximately vertebral levels LI and LII. Therefore, disease from the testes tracks superiorly to nodes high in the posterior abdominal wall and not to inguinal or iliac nodes.
Visualizing the male pelvic cavity and perineum in the axial plane
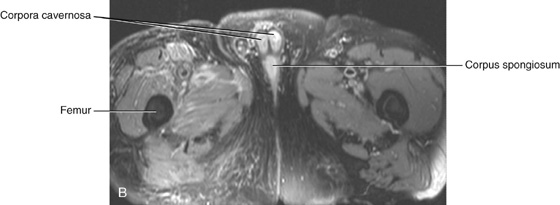
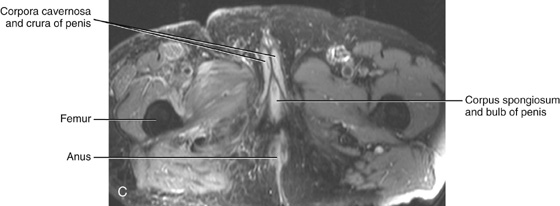
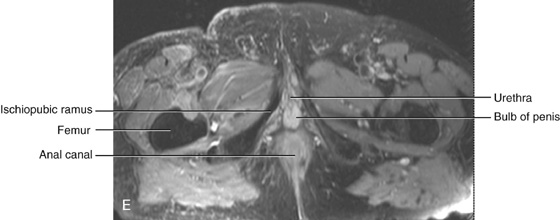
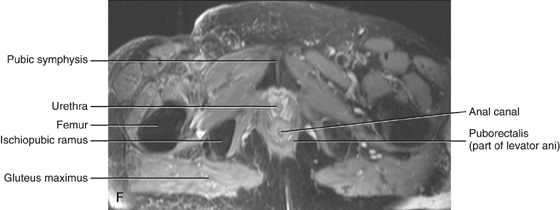
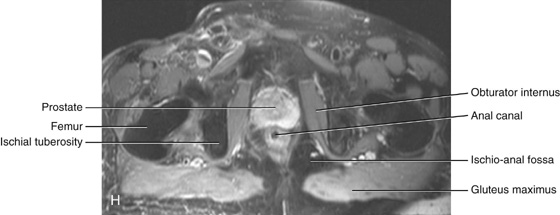
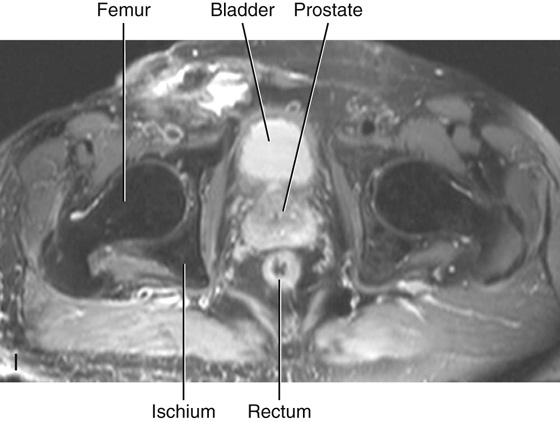
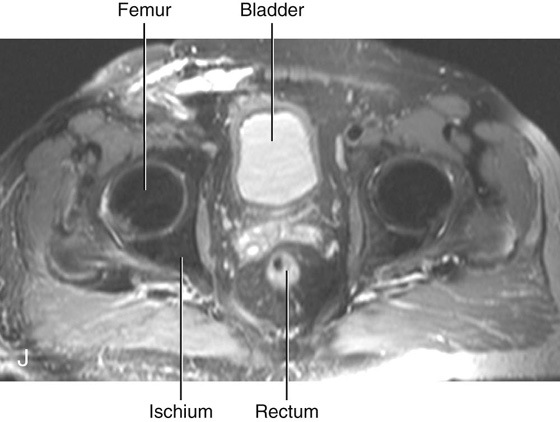
Fig. 5.56 A to J. Series of axial images that pass through the pelvic cavity and perineum from inferior to superior showing the various structures and their relationships to each other (T2-weighted MR images in axial plane.)
Visualizing the female pelvic cavity and perineum in the sagittal plane
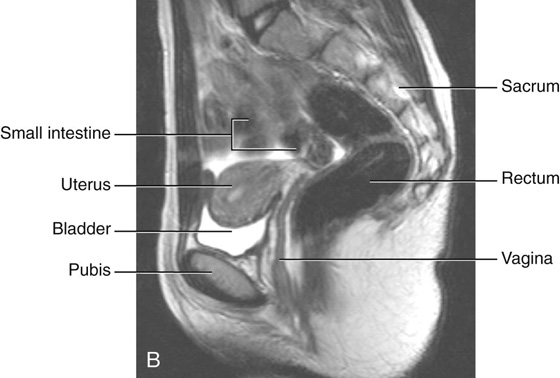
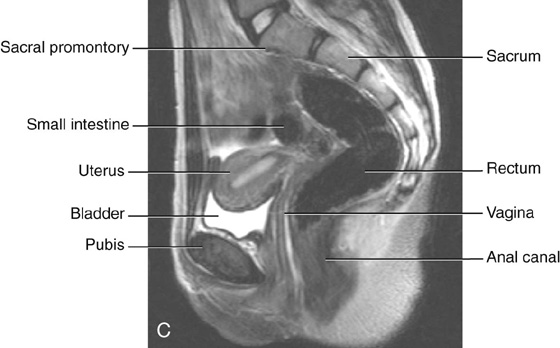
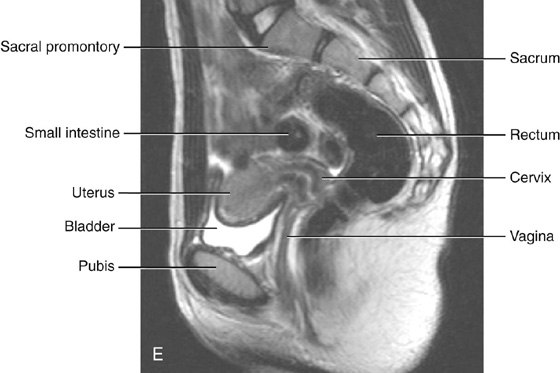
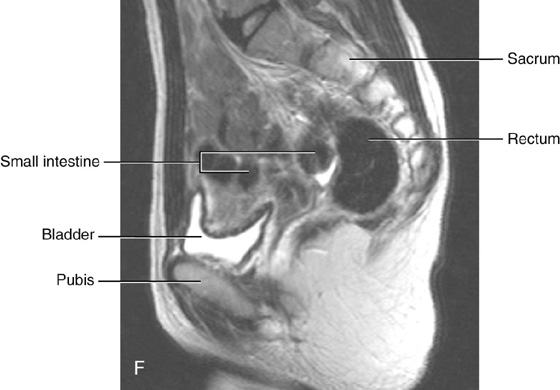
Fig. 5.57 A to F. Series of sagittal images that pass through the female pelvic cavity and perineum showing the various structures and their relationships to each other (T2-weighted MR images in sagittal plane.)
Visualizing the female pelvic cavity and perineum in the coronal plane
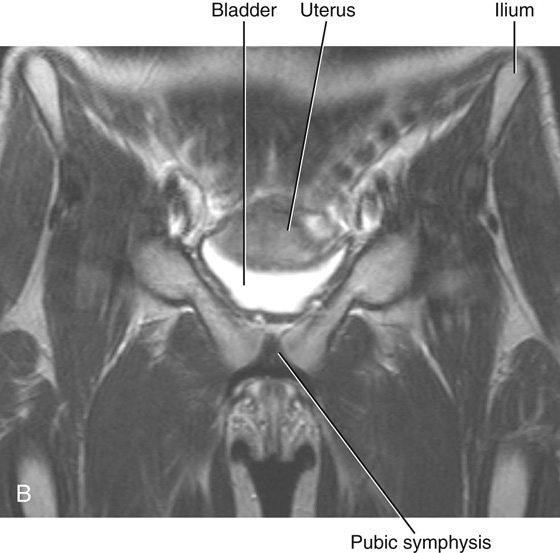
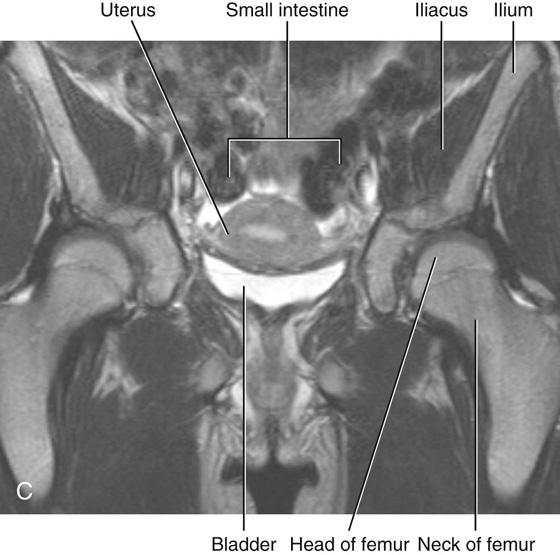
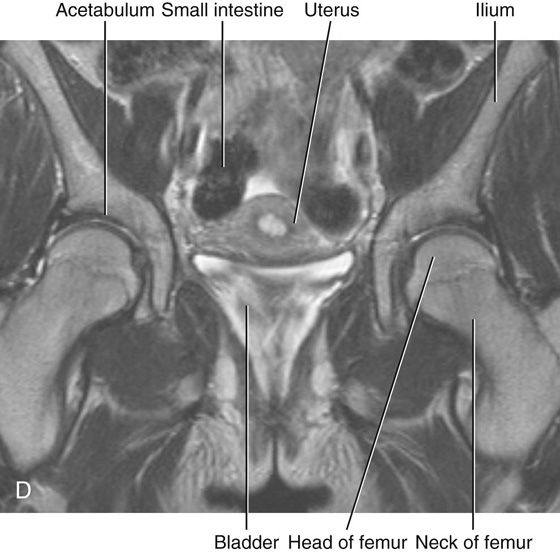
Fig. 5.58 A to D. Series of coronal images that pass through the pelvic cavity and perineum from anterior to posterior showing the various structures and their relationships to each other (T2-weighted MR images in coronal plane.)

 Medical Clinical Case Studies
Medical Clinical Case Studies Clinical Cases
Clinical Cases The superior region related to upper parts of the pelvic bones and lower lumbar vertebrae is the false pelvis (greater pelvis) and is generally considered part of the abdomen.
The superior region related to upper parts of the pelvic bones and lower lumbar vertebrae is the false pelvis (greater pelvis) and is generally considered part of the abdomen. The true pelvis (lesser pelvis) is related to the inferior parts of the pelvic bones, sacrum, and coccyx, and has an inlet and an outlet.
The true pelvis (lesser pelvis) is related to the inferior parts of the pelvic bones, sacrum, and coccyx, and has an inlet and an outlet.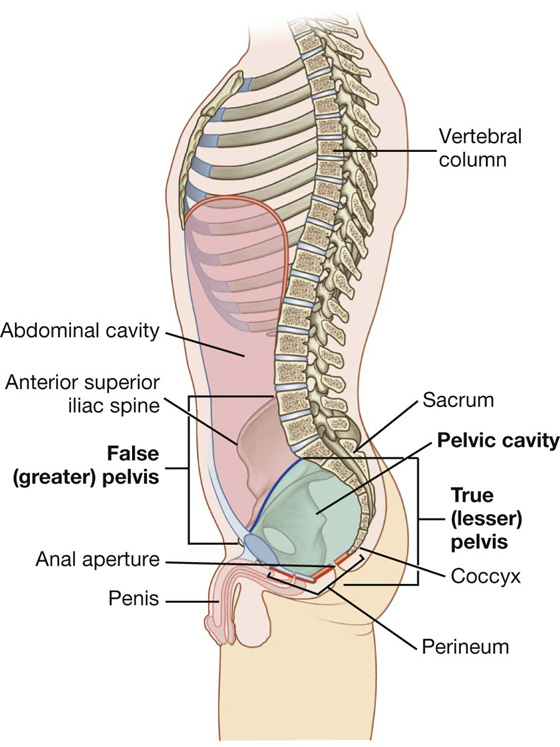
 The pelvic bone above this line represents the lateral wall of the false pelvis, which is part of the abdominal cavity.
The pelvic bone above this line represents the lateral wall of the false pelvis, which is part of the abdominal cavity. The pelvic bone below this line represents the lateral wall of the true pelvis, which contains the pelvic cavity.
The pelvic bone below this line represents the lateral wall of the true pelvis, which contains the pelvic cavity.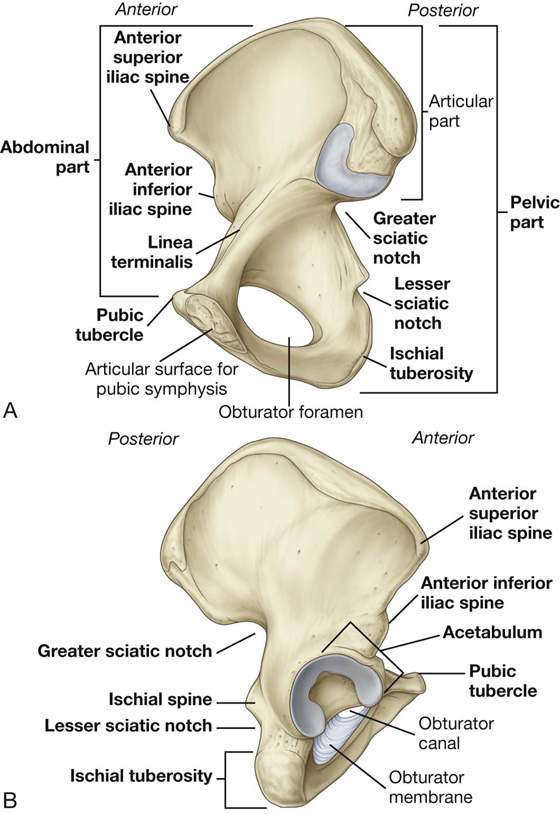
 the lesser sciatic notch.
the lesser sciatic notch.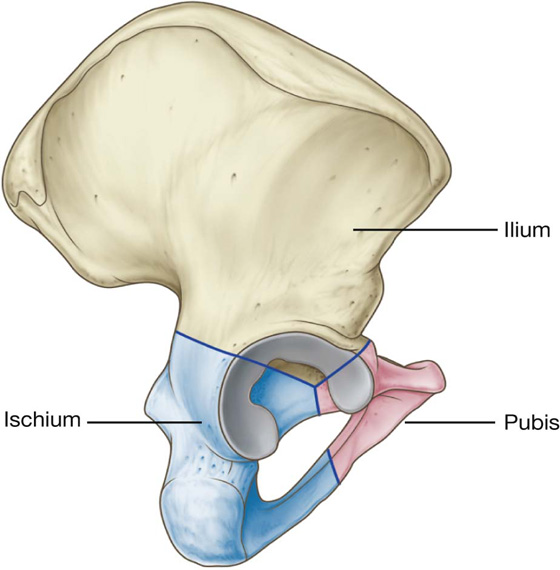
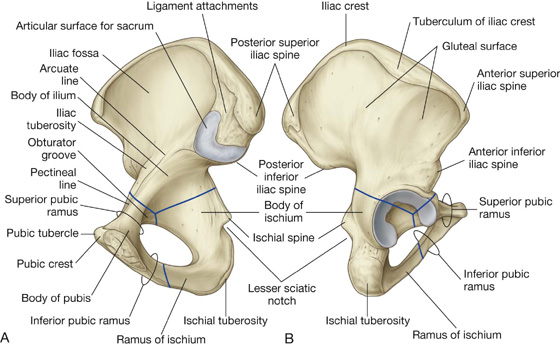
 The body is flattened dorsoventrally and articulates with the body of the pubic bone on the other side at the pubic symphysis. The body has a rounded pubic crest on its superior surface that ends laterally as the prominent pubic tubercle.
The body is flattened dorsoventrally and articulates with the body of the pubic bone on the other side at the pubic symphysis. The body has a rounded pubic crest on its superior surface that ends laterally as the prominent pubic tubercle. The superior pubic ramus projects posterolaterally from the body and joins with the ilium and ischium at its base, which is positioned toward the acetabulum. The sharp superior margin of this triangular surface is termed the pecten pubis (pectineal line), which forms part of the linea terminalis of the pelvic bone and the pelvic inlet. Anteriorly, this line is continuous with the pubic crest, which also is part of the linea terminalis and pelvic inlet. The superior pubic ramus is marked on its inferior surface by the obturator groove, which forms the upper margin of the obturator canal.
The superior pubic ramus projects posterolaterally from the body and joins with the ilium and ischium at its base, which is positioned toward the acetabulum. The sharp superior margin of this triangular surface is termed the pecten pubis (pectineal line), which forms part of the linea terminalis of the pelvic bone and the pelvic inlet. Anteriorly, this line is continuous with the pubic crest, which also is part of the linea terminalis and pelvic inlet. The superior pubic ramus is marked on its inferior surface by the obturator groove, which forms the upper margin of the obturator canal. a large body that projects superiorly to join with the ilium and the superior ramus of the pubis; and
a large body that projects superiorly to join with the ilium and the superior ramus of the pubis; and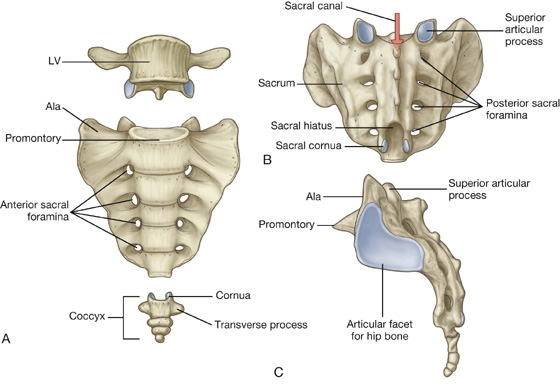
 the two zygapophyseal joints, which occur between adjacent inferior and superior articular processes; and
the two zygapophyseal joints, which occur between adjacent inferior and superior articular processes; and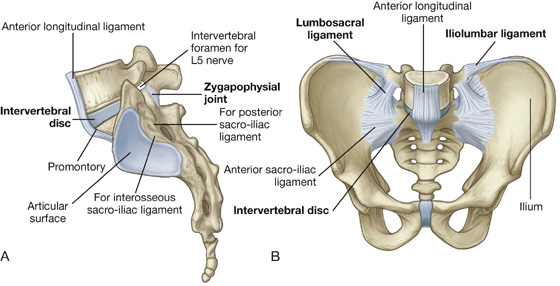
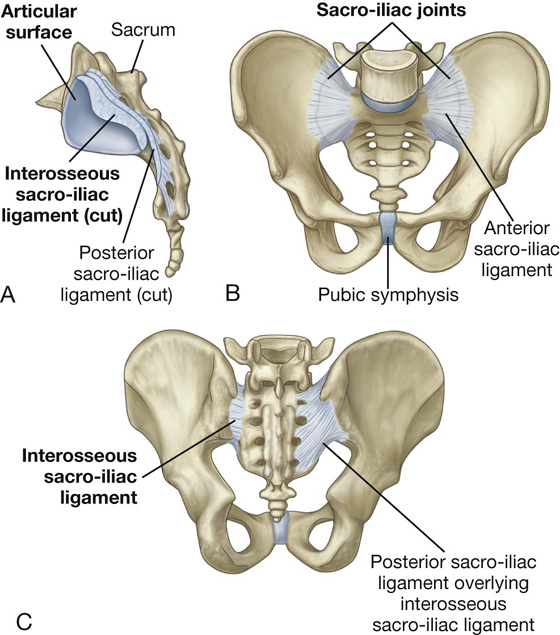
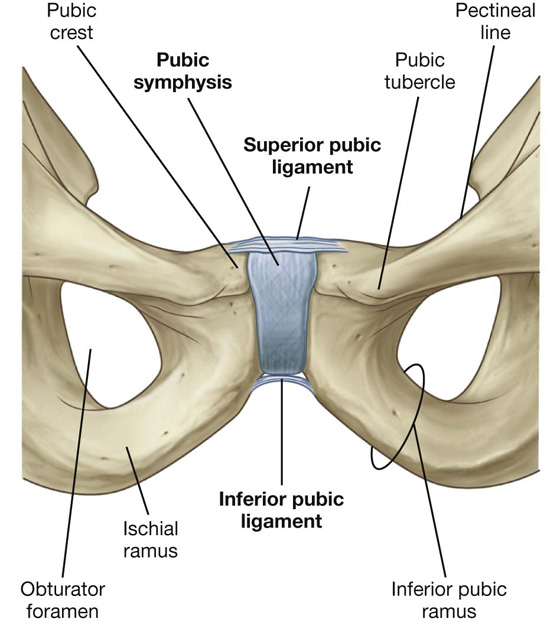
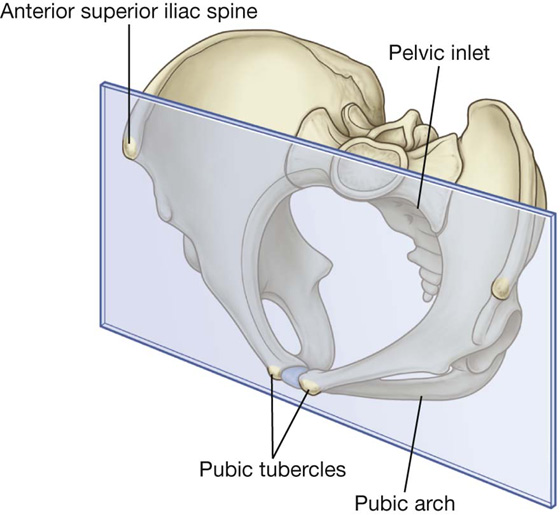
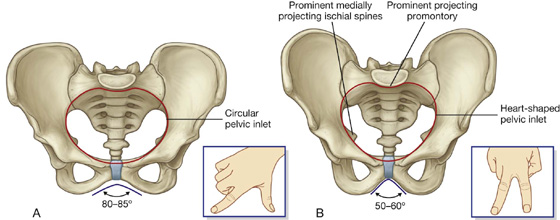
 The ischial spines generally do not project as far medially into the pelvic cavity in women as they do in men.
The ischial spines generally do not project as far medially into the pelvic cavity in women as they do in men.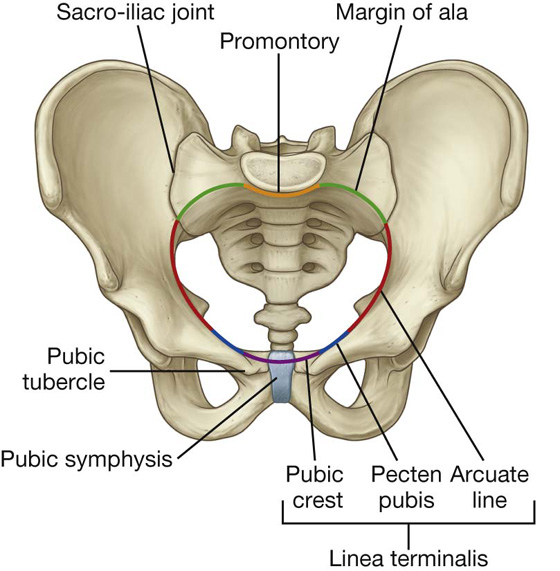
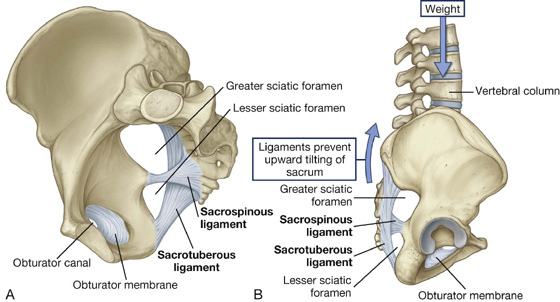
 The lesser sciatic foramen lies inferior to the ischial spine and sacrospinous ligament between the sacrospinous and sacrotuberous ligaments.
The lesser sciatic foramen lies inferior to the ischial spine and sacrospinous ligament between the sacrospinous and sacrotuberous ligaments.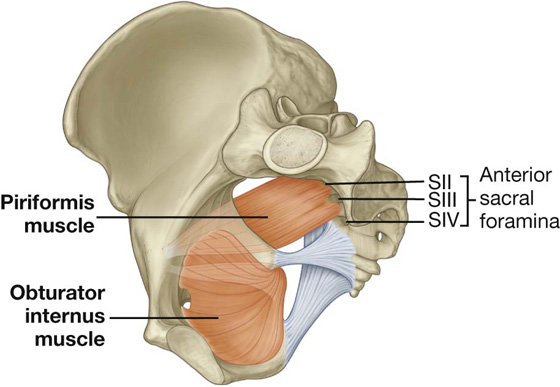
 the obturator canal,
the obturator canal, the lesser sciatic foramen.
the lesser sciatic foramen.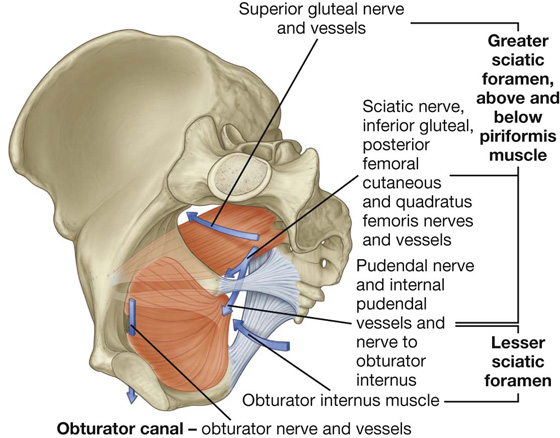
 Passing through the foramen below the piriformis are the inferior gluteal nerves and vessels, the sciatic nerve, the pudendal nerve, the internal pudendal vessels, the posterior femoral cutaneous nerves, and the nerves to the obturator internus and quadratus femoris muscles.
Passing through the foramen below the piriformis are the inferior gluteal nerves and vessels, the sciatic nerve, the pudendal nerve, the internal pudendal vessels, the posterior femoral cutaneous nerves, and the nerves to the obturator internus and quadratus femoris muscles.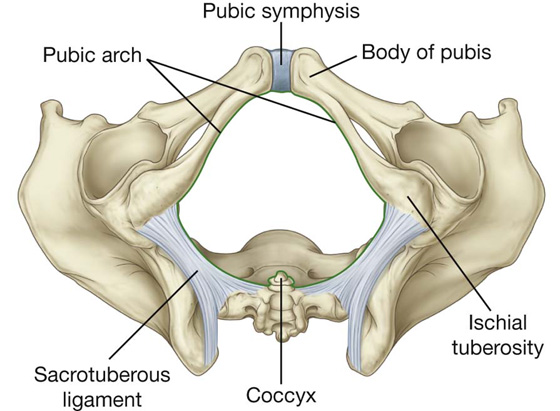
 the sagittal outlet (the distance between the tip of the coccyx and the inferior margin of the pubic symphysis).
the sagittal outlet (the distance between the tip of the coccyx and the inferior margin of the pubic symphysis).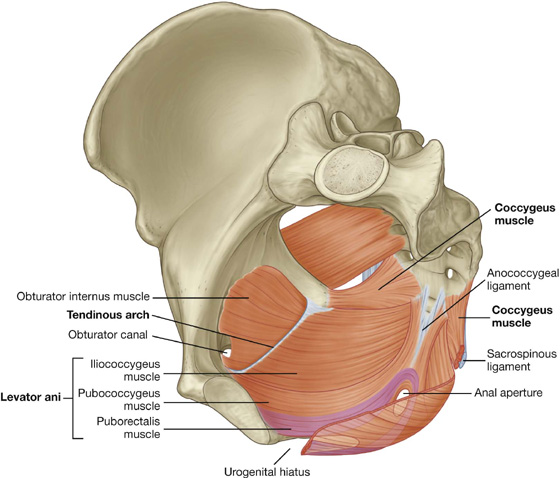
 the greater sciatic foramen is situated above the level of the pelvic floor and is a route of communication between the pelvic cavity and the gluteal region of the lower limb; and
the greater sciatic foramen is situated above the level of the pelvic floor and is a route of communication between the pelvic cavity and the gluteal region of the lower limb; and the lesser sciatic foramen is situated below the pelvic floor, providing a route of communication between the gluteal region of the lower limb and the perineum.
the lesser sciatic foramen is situated below the pelvic floor, providing a route of communication between the gluteal region of the lower limb and the perineum. a linear thickening called the tendinous arch in the fascia covering the obturator internus muscle, and
a linear thickening called the tendinous arch in the fascia covering the obturator internus muscle, and the spine of the ischium.
the spine of the ischium. The pubococcygeus originates from the body of the pubis and courses posteriorly to attach along the midline as far back as the coccyx. This part of the muscle is further subdivided on the basis of association with structures in the midline into the puboprostaticus (levator prostatae), the pubovaginalis, and the puboanalis muscles.
The pubococcygeus originates from the body of the pubis and courses posteriorly to attach along the midline as far back as the coccyx. This part of the muscle is further subdivided on the basis of association with structures in the midline into the puboprostaticus (levator prostatae), the pubovaginalis, and the puboanalis muscles. A second major collection of muscle fibers, the puborectalis portion of the levator ani muscles, originates, in association with the pubococcygeus muscle, from the pubis and passes inferiorly on each side to form a sling around the terminal part of the gastrointestinal tract. This muscular sling maintains an angle or flexure, called the perineal flexure, at the anorectal junction. This angle functions as part of the mechanism that keeps the end of the gastrointestinal system closed.
A second major collection of muscle fibers, the puborectalis portion of the levator ani muscles, originates, in association with the pubococcygeus muscle, from the pubis and passes inferiorly on each side to form a sling around the terminal part of the gastrointestinal tract. This muscular sling maintains an angle or flexure, called the perineal flexure, at the anorectal junction. This angle functions as part of the mechanism that keeps the end of the gastrointestinal system closed. The final part of the levator ani muscle is the iliococcygeus. This part of the muscle originates from the fascia that covers the obturator internus muscle. It joins the same muscle on the other side in the midline to form a ligament or raphe that extends from the anal aperture to the coccyx.
The final part of the levator ani muscle is the iliococcygeus. This part of the muscle originates from the fascia that covers the obturator internus muscle. It joins the same muscle on the other side in the midline to form a ligament or raphe that extends from the anal aperture to the coccyx.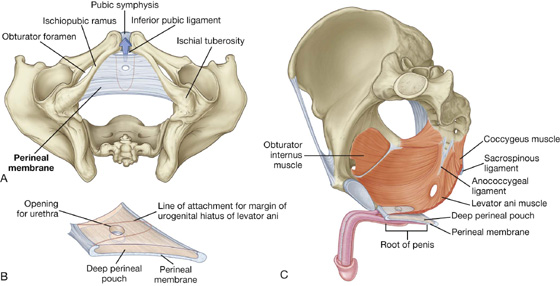
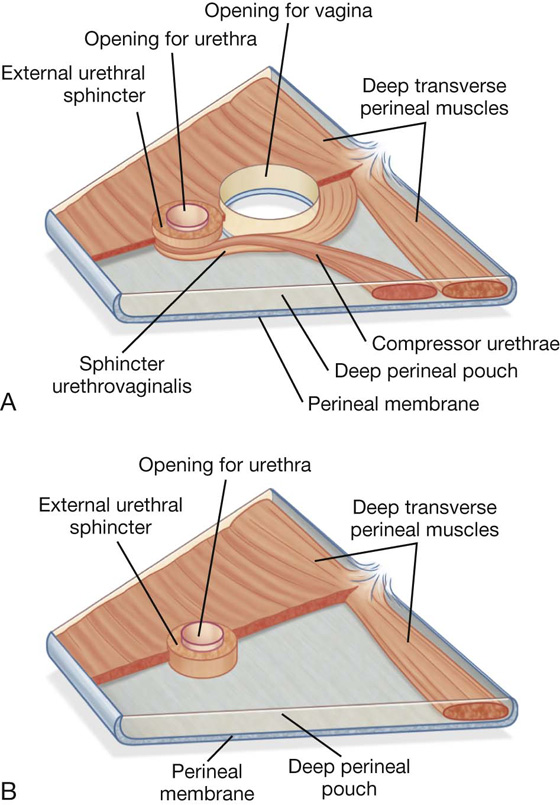
 In both men and women, a deep transverse perineal muscle on each side parallels the free margin of the perineal membrane and joins with its partner at the midline. These muscles are thought to stabilize the position of the perineal body, which is a midline structure along the posterior edge of the perineal membrane.
In both men and women, a deep transverse perineal muscle on each side parallels the free margin of the perineal membrane and joins with its partner at the midline. These muscles are thought to stabilize the position of the perineal body, which is a midline structure along the posterior edge of the perineal membrane.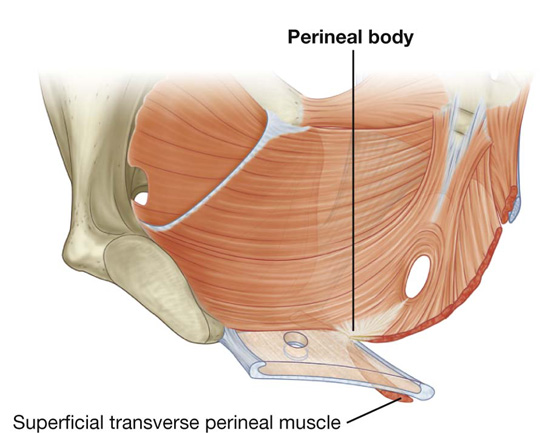
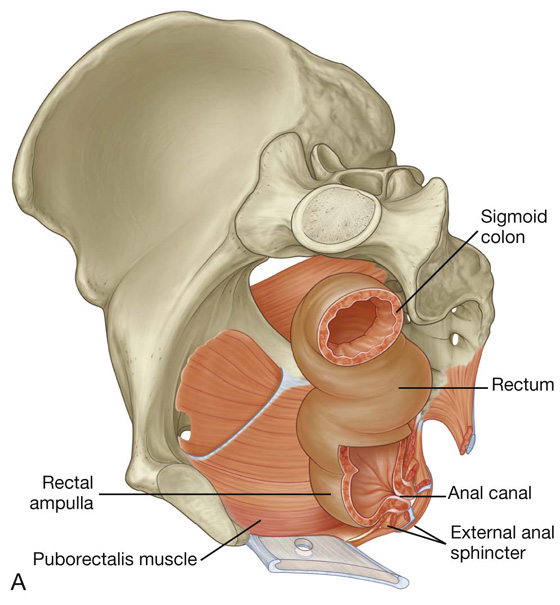
 below, with the anal canal as this structure penetrates the pelvic floor and passes through the perineum to end as the anus.
below, with the anal canal as this structure penetrates the pelvic floor and passes through the perineum to end as the anus. The upper part of the anal canal is lined by mucosa similar to that lining the rectum and is distinguished by a number of longitudinally oriented folds known as anal columns, which are united inferiorly by crescentic folds termed anal valves. Superior to each valve is a depression termed an anal sinus. The anal valves together form a circle around the anal canal at a location known as the pectinate line, which marks the approximate position of the anal membrane in the fetus.
The upper part of the anal canal is lined by mucosa similar to that lining the rectum and is distinguished by a number of longitudinally oriented folds known as anal columns, which are united inferiorly by crescentic folds termed anal valves. Superior to each valve is a depression termed an anal sinus. The anal valves together form a circle around the anal canal at a location known as the pectinate line, which marks the approximate position of the anal membrane in the fetus. Inferior to the pectinate line is a transition zone known as the anal pecten, which is lined by nonkeratinized stratified squamous epithelium. The anal pecten ends inferiorly at the anocutaneous line (“white line”), or where the lining of the anal canal becomes true skin.
Inferior to the pectinate line is a transition zone known as the anal pecten, which is lined by nonkeratinized stratified squamous epithelium. The anal pecten ends inferiorly at the anocutaneous line (“white line”), or where the lining of the anal canal becomes true skin.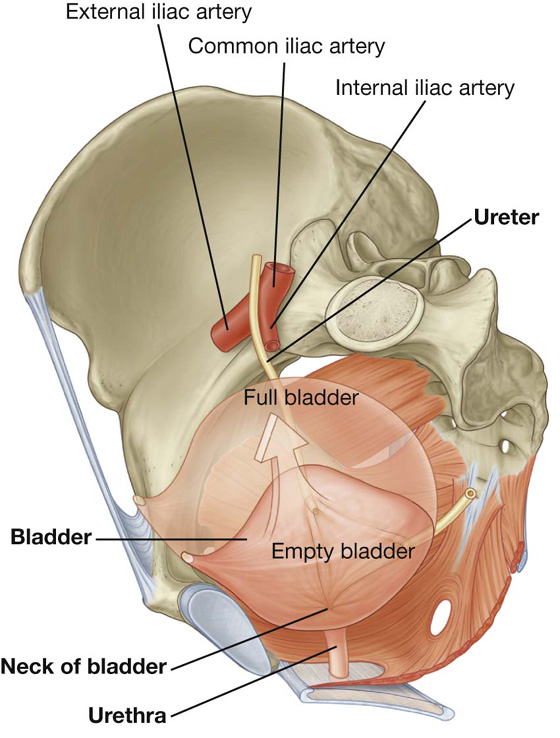
 the uterine artery in women.
the uterine artery in women. The apex of the bladder is directed toward the top of the pubic symphysis; a structure known as the median umbilical ligament (a remnant of the embryological urachus that contributes to the formation of the bladder) continues from it superiorly up the anterior abdominal wall to the umbilicus.
The apex of the bladder is directed toward the top of the pubic symphysis; a structure known as the median umbilical ligament (a remnant of the embryological urachus that contributes to the formation of the bladder) continues from it superiorly up the anterior abdominal wall to the umbilicus. The inferolateral surfaces of the bladder are cradled between the levator ani muscles of the pelvic diaphragm and the adjacent obturator internus muscles above the attachment of the pelvic diaphragm. The superior surface is slightly domed when the bladder is empty; it balloons upward as the bladder fills.
The inferolateral surfaces of the bladder are cradled between the levator ani muscles of the pelvic diaphragm and the adjacent obturator internus muscles above the attachment of the pelvic diaphragm. The superior surface is slightly domed when the bladder is empty; it balloons upward as the bladder fills.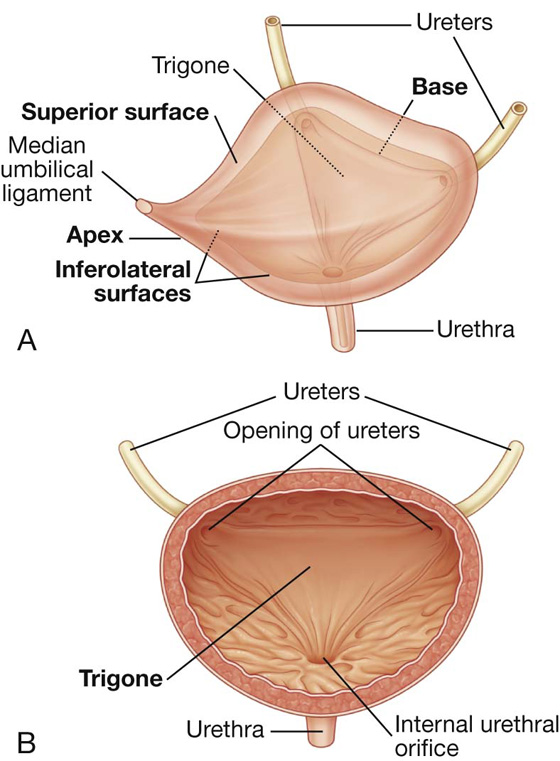
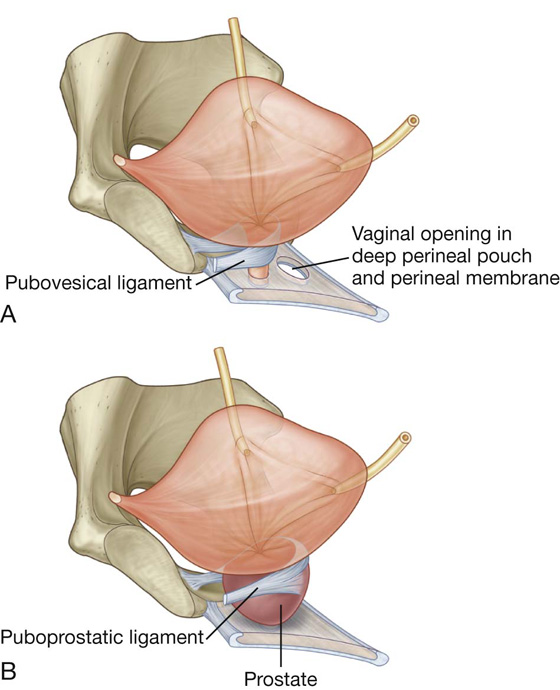
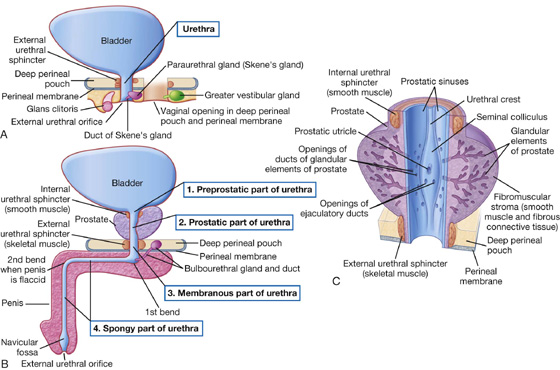
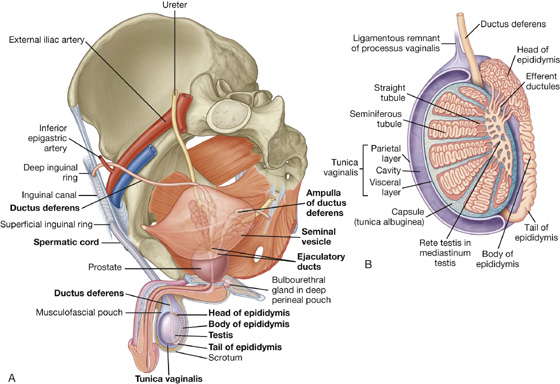
 a single prostate,
a single prostate, the efferent ductules, which form an enlarged coiled mass that sits on the posterior superior pole of the testis and forms the head of the epididymis; and
the efferent ductules, which form an enlarged coiled mass that sits on the posterior superior pole of the testis and forms the head of the epididymis; and the true epididymis, which is a single, long coiled duct into which the efferent ductules all drain, and which continues inferiorly along the posterolateral margin of the testis as the body of epididymis and enlarges to form the tail of epididymis at the inferior pole of the testis.
the true epididymis, which is a single, long coiled duct into which the efferent ductules all drain, and which continues inferiorly along the posterolateral margin of the testis as the body of epididymis and enlarges to form the tail of epididymis at the inferior pole of the testis.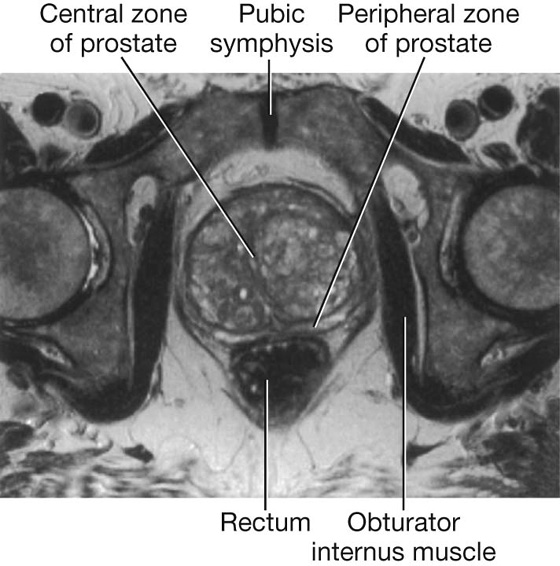
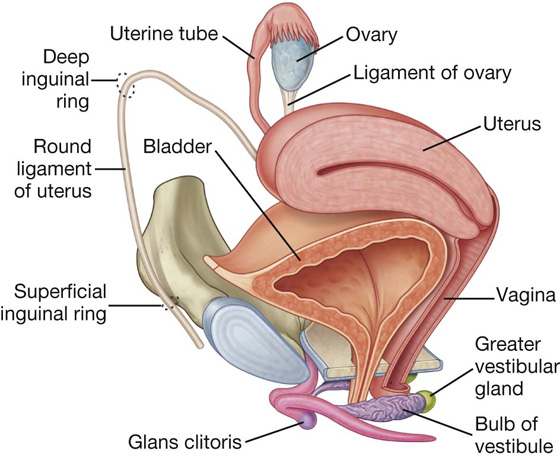
 an ovary on each side, and
an ovary on each side, and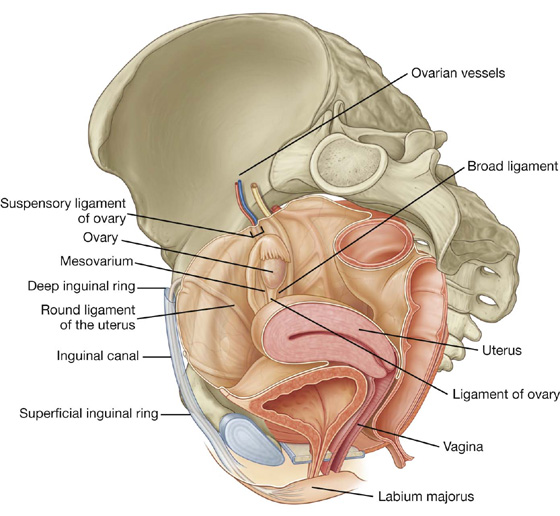
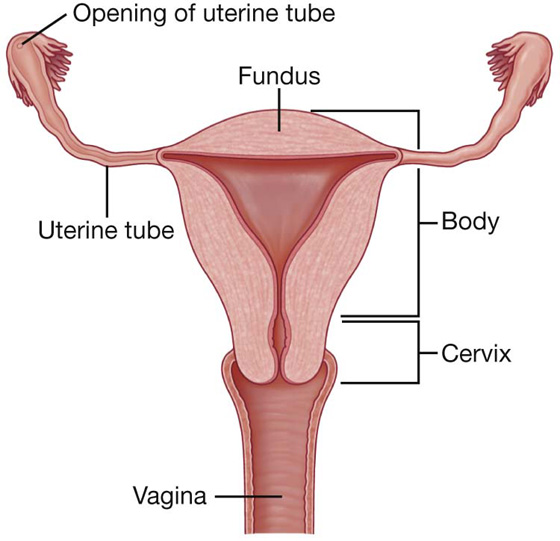
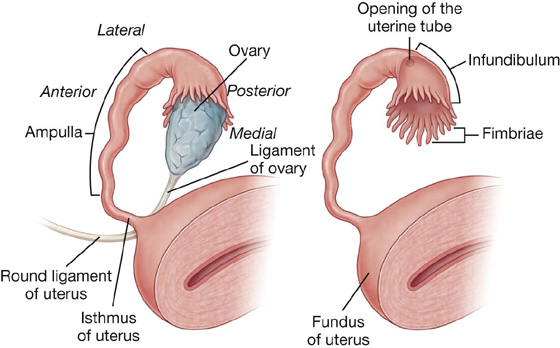
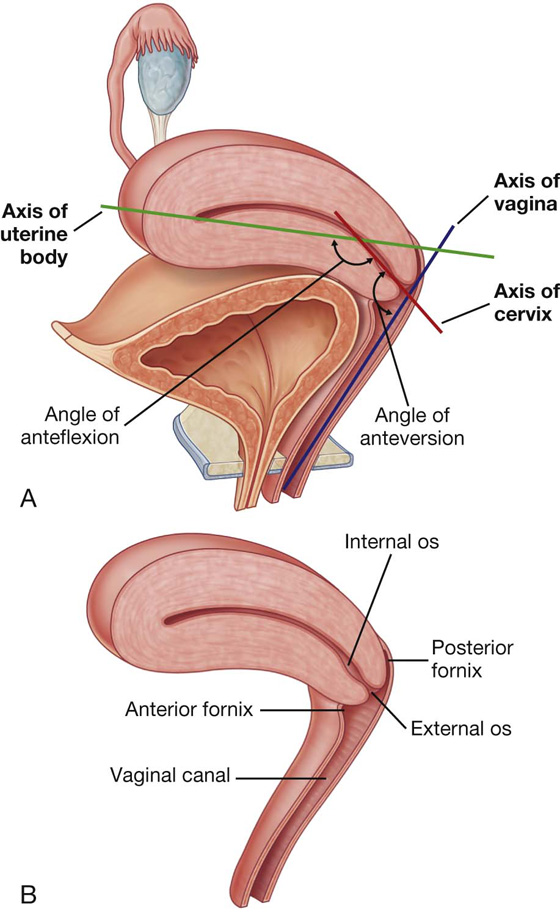
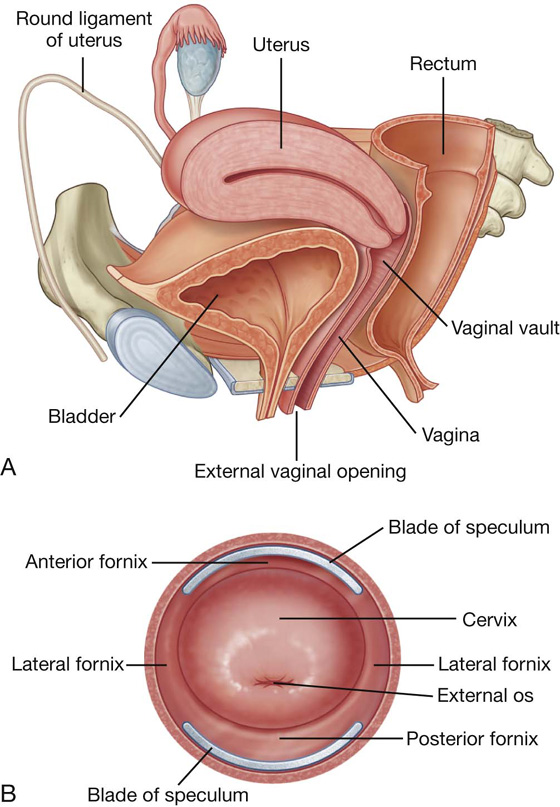
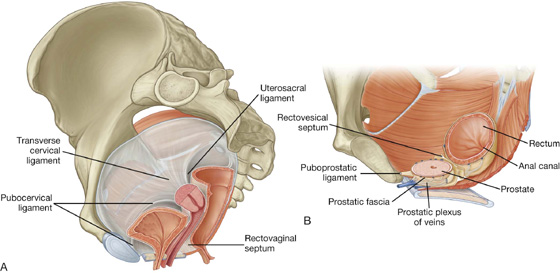
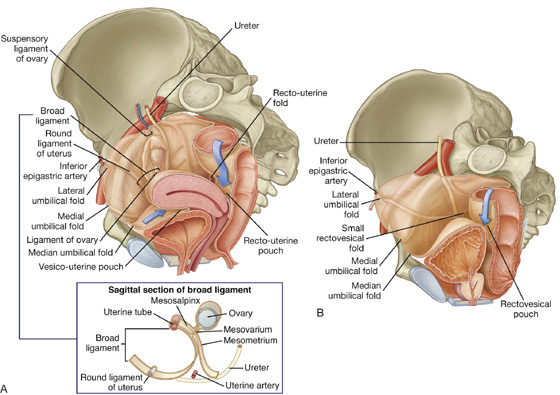
 the mesometrium, the largest part of the broad ligament, which extends from the lateral pelvic walls to the body of the uterus;
the mesometrium, the largest part of the broad ligament, which extends from the lateral pelvic walls to the body of the uterus; the mesosalpinx, the most superior part of the broad ligament, which suspends the uterine tube in the pelvic cavity; and
the mesosalpinx, the most superior part of the broad ligament, which suspends the uterine tube in the pelvic cavity; and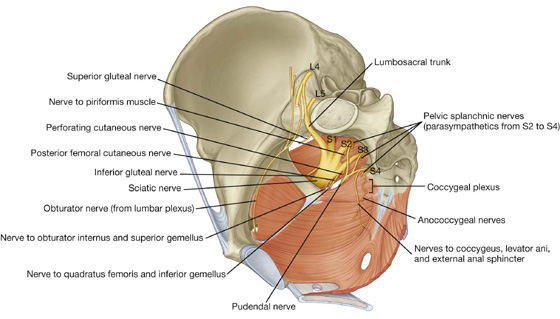
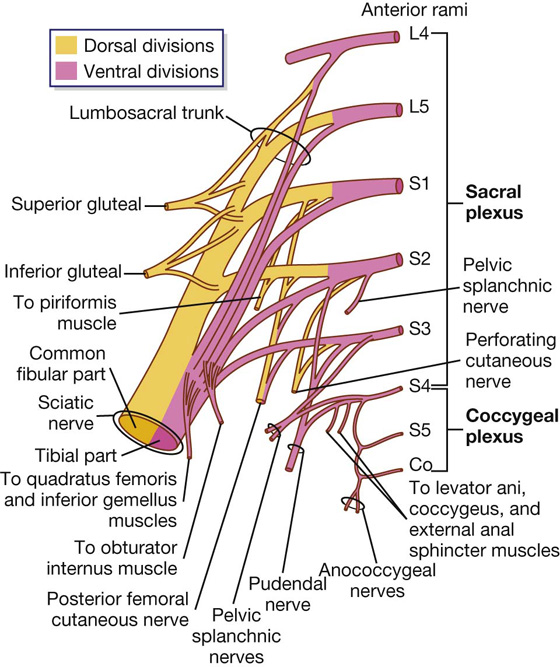
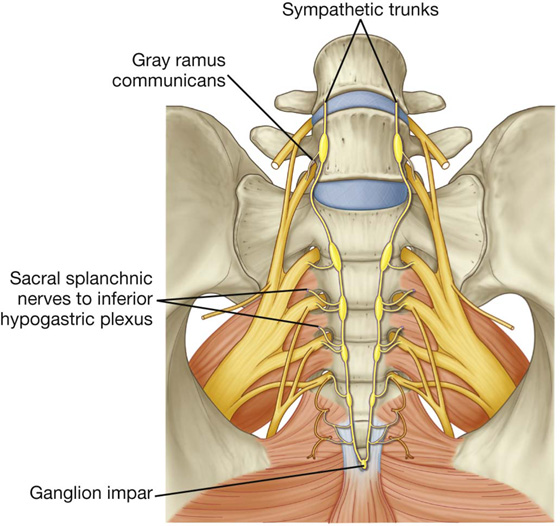
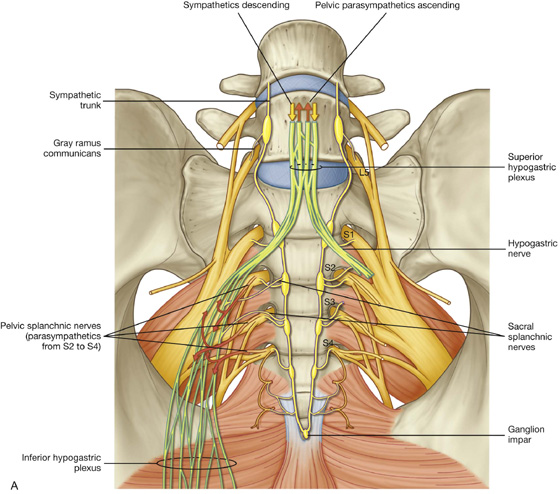
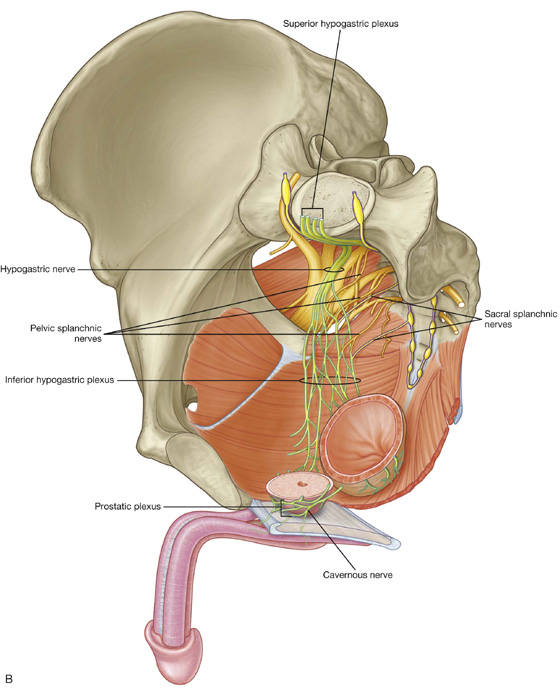
 forms on the anterior surface of the piriformis muscle and leaves the pelvic cavity through the greater sciatic foramen inferior to piriformis;
forms on the anterior surface of the piriformis muscle and leaves the pelvic cavity through the greater sciatic foramen inferior to piriformis; passes through the gluteal region into the thigh, where it divides into its two major branches, the common fibular nerve (common peroneal nerve) and the tibial nerve—dorsal divisions of L4, L5, S1, and S2 are carried in the common fibular part of the nerve and the ventral divisions of L4, L5, S1, S2, and S3 are carried in the tibial part;
passes through the gluteal region into the thigh, where it divides into its two major branches, the common fibular nerve (common peroneal nerve) and the tibial nerve—dorsal divisions of L4, L5, S1, and S2 are carried in the common fibular part of the nerve and the ventral divisions of L4, L5, S1, S2, and S3 are carried in the tibial part; leaves the pelvic cavity through the greater sciatic foramen, inferior to the piriformis muscle, and enters the gluteal region;
leaves the pelvic cavity through the greater sciatic foramen, inferior to the piriformis muscle, and enters the gluteal region; courses into the perineum by immediately passing around the sacrospinous ligament, where the ligament joins the ischial spine, and through the lesser sciatic foramen (this course takes the nerve out of the pelvic cavity, around the peripheral attachment of the pelvic floor, and into the perineum);
courses into the perineum by immediately passing around the sacrospinous ligament, where the ligament joins the ischial spine, and through the lesser sciatic foramen (this course takes the nerve out of the pelvic cavity, around the peripheral attachment of the pelvic floor, and into the perineum); innervates skin and skeletal muscles of the perineum, including the external anal and external urethral sphincters.
innervates skin and skeletal muscles of the perineum, including the external anal and external urethral sphincters. motor branches to muscles of the gluteal region, pelvic wall, and pelvic floor (superior and inferior gluteal nerves, nerve to obturator internus and superior gemellus, nerve to quadratus femoris and inferior gemellus, nerve to piriformis, nerves to levator ani); and
motor branches to muscles of the gluteal region, pelvic wall, and pelvic floor (superior and inferior gluteal nerves, nerve to obturator internus and superior gemellus, nerve to quadratus femoris and inferior gemellus, nerve to piriformis, nerves to levator ani); and the rectal plexus,
the rectal plexus, the uterovaginal plexus,
the uterovaginal plexus, the prostatic plexus, and
the prostatic plexus, and the vesical plexus.
the vesical plexus. innervate blood vessels,
innervate blood vessels, cause contraction of smooth muscle in the internal urethral sphincter in men and the internal anal sphincters in both men and women,
cause contraction of smooth muscle in the internal urethral sphincter in men and the internal anal sphincters in both men and women, cause smooth muscle contraction associated with the reproductive tract and with the accessory glands of the reproductive system, and
cause smooth muscle contraction associated with the reproductive tract and with the accessory glands of the reproductive system, and are important in moving secretions from the epididymis and associated glands into the urethra to form semen during ejaculation.
are important in moving secretions from the epididymis and associated glands into the urethra to form semen during ejaculation. are generally vasodilatory,
are generally vasodilatory, stimulate erection, and
stimulate erection, and modulate activity of the enteric nervous system of the colon distal to the left colic flexure (in addition to pelvic viscera, some of the fibers from the pelvic plexus course superiorly in the prevertebral plexus, or as separate nerves, and pass into the inferior mesenteric plexus of the abdomen).
modulate activity of the enteric nervous system of the colon distal to the left colic flexure (in addition to pelvic viscera, some of the fibers from the pelvic plexus course superiorly in the prevertebral plexus, or as separate nerves, and pass into the inferior mesenteric plexus of the abdomen).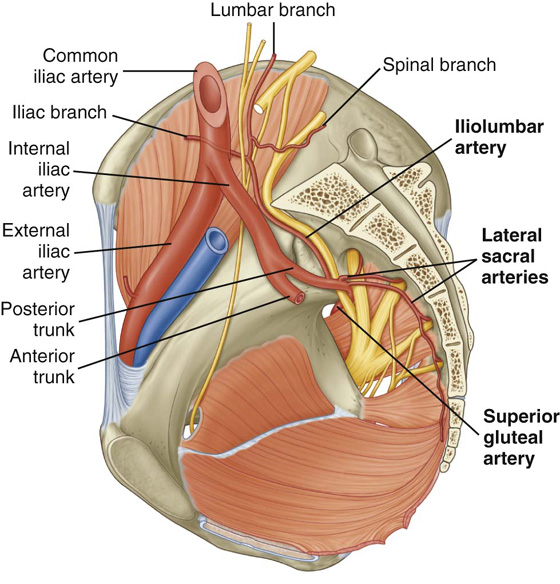
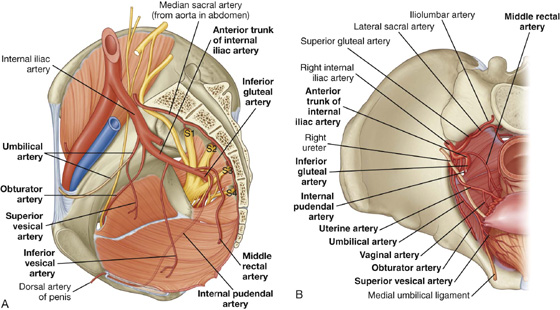
 The iliolumbar artery ascends laterally back out of the pelvic inlet and divides into a lumbar branch and an iliac branch. The lumbar branch contributes to the supply of the posterior abdominal wall, psoas, quadratus lumborum muscles, and cauda equina, via a small spinal branch that passes through the intervertebral foramen between LV and SI. The iliac branch passes laterally into the iliac fossa to supply muscle and bone.
The iliolumbar artery ascends laterally back out of the pelvic inlet and divides into a lumbar branch and an iliac branch. The lumbar branch contributes to the supply of the posterior abdominal wall, psoas, quadratus lumborum muscles, and cauda equina, via a small spinal branch that passes through the intervertebral foramen between LV and SI. The iliac branch passes laterally into the iliac fossa to supply muscle and bone. The lateral sacral arteries, usually two, originate from the posterior division of the internal iliac artery and course medially and inferiorly along the posterior pelvic wall. They give rise to branches that pass into the anterior sacral foramina to supply related bone and soft tissues, structures in the vertebral (sacral) canal, and skin and muscle posterior to the sacrum.
The lateral sacral arteries, usually two, originate from the posterior division of the internal iliac artery and course medially and inferiorly along the posterior pelvic wall. They give rise to branches that pass into the anterior sacral foramina to supply related bone and soft tissues, structures in the vertebral (sacral) canal, and skin and muscle posterior to the sacrum. The superior gluteal artery is the largest branch of the internal iliac artery. It courses posteriorly, usually passing between the lumbosacral trunk and anterior ramus of S1, to leave the pelvic cavity through the greater sciatic foramen above the piriformis muscle and enter the gluteal region of the lower limb. This vessel makes a substantial contribution to the blood supply of muscles and skin in the gluteal region and also supplies branches to adjacent muscles and bones of the pelvic walls.
The superior gluteal artery is the largest branch of the internal iliac artery. It courses posteriorly, usually passing between the lumbosacral trunk and anterior ramus of S1, to leave the pelvic cavity through the greater sciatic foramen above the piriformis muscle and enter the gluteal region of the lower limb. This vessel makes a substantial contribution to the blood supply of muscles and skin in the gluteal region and also supplies branches to adjacent muscles and bones of the pelvic walls. The superior vesical artery normally originates from the root of the umbilical artery and courses medially and inferiorly to supply the superior aspect of the bladder and distal parts of the ureter. In men, it also may give rise to an artery that supplies the ductus deferens.
The superior vesical artery normally originates from the root of the umbilical artery and courses medially and inferiorly to supply the superior aspect of the bladder and distal parts of the ureter. In men, it also may give rise to an artery that supplies the ductus deferens. The inferior vesical artery occurs in men and supplies branches to the bladder, ureter, seminal vesicle, and prostate. The vaginal artery in women is the equivalent of the inferior vesical artery in men and, descending to the vagina, supplies branches to the vagina and to adjacent parts of the bladder and rectum.
The inferior vesical artery occurs in men and supplies branches to the bladder, ureter, seminal vesicle, and prostate. The vaginal artery in women is the equivalent of the inferior vesical artery in men and, descending to the vagina, supplies branches to the vagina and to adjacent parts of the bladder and rectum. The middle rectal artery courses medially to supply the rectum. The vessel anastomoses with the superior rectal artery, which originates from the inferior mesenteric artery in the abdomen, and the inferior rectal artery, which originates from the internal pudendal artery in the perineum.
The middle rectal artery courses medially to supply the rectum. The vessel anastomoses with the superior rectal artery, which originates from the inferior mesenteric artery in the abdomen, and the inferior rectal artery, which originates from the internal pudendal artery in the perineum. The obturator artery courses anteriorly along the pelvic wall and leaves the pelvic cavity via the obturator canal. Together with the obturator nerve, above, and obturator vein, below, it enters and supplies the adductor region of the thigh.
The obturator artery courses anteriorly along the pelvic wall and leaves the pelvic cavity via the obturator canal. Together with the obturator nerve, above, and obturator vein, below, it enters and supplies the adductor region of the thigh. The internal pudendal artery courses inferiorly from its origin in the anterior trunk and leaves the pelvic cavity through the greater sciatic foramen inferior to the piriformis muscle. In association with the pudendal nerve on its medial side, the vessel passes laterally to the ischial spine and then through the lesser sciatic foramen to enter the perineum. The internal pudendal artery is the main artery of the perineum. Among the structures it supplies are the erectile tissues of the clitoris and the penis.
The internal pudendal artery courses inferiorly from its origin in the anterior trunk and leaves the pelvic cavity through the greater sciatic foramen inferior to the piriformis muscle. In association with the pudendal nerve on its medial side, the vessel passes laterally to the ischial spine and then through the lesser sciatic foramen to enter the perineum. The internal pudendal artery is the main artery of the perineum. Among the structures it supplies are the erectile tissues of the clitoris and the penis. The inferior gluteal artery is a large terminal branch of the anterior trunk of the internal iliac artery. It passes between the anterior rami S1 and S2 or S2 and S3 of the sacral plexus and leaves the pelvic cavity through the greater sciatic foramen inferior to the piriformis muscle. It enters and contributes to the blood supply of the gluteal region and anastomoses with a network of vessels around the hip joint.
The inferior gluteal artery is a large terminal branch of the anterior trunk of the internal iliac artery. It passes between the anterior rami S1 and S2 or S2 and S3 of the sacral plexus and leaves the pelvic cavity through the greater sciatic foramen inferior to the piriformis muscle. It enters and contributes to the blood supply of the gluteal region and anastomoses with a network of vessels around the hip joint.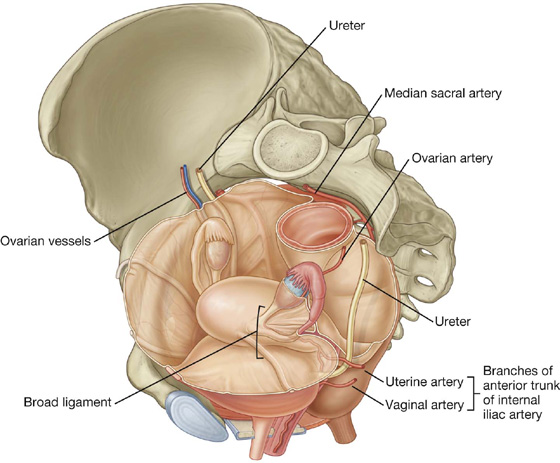
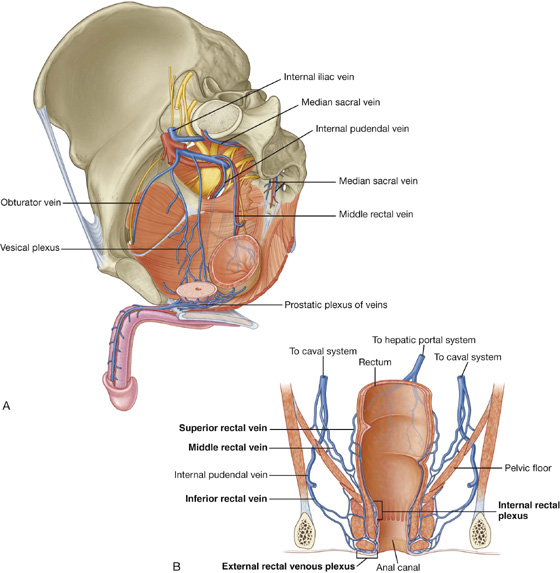
 The median sacral veins coalesce to form a single vein that joins either the left common iliac vein or the junction of the two common iliac veins to form the inferior vena cava.
The median sacral veins coalesce to form a single vein that joins either the left common iliac vein or the junction of the two common iliac veins to form the inferior vena cava. The ovarian veins follow the course of the corresponding arteries; on the left, they join the left renal vein and, on the right, they join the inferior vena cava in the abdomen.
The ovarian veins follow the course of the corresponding arteries; on the left, they join the left renal vein and, on the right, they join the inferior vena cava in the abdomen.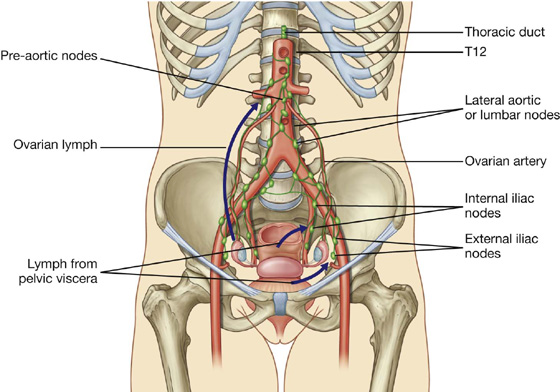
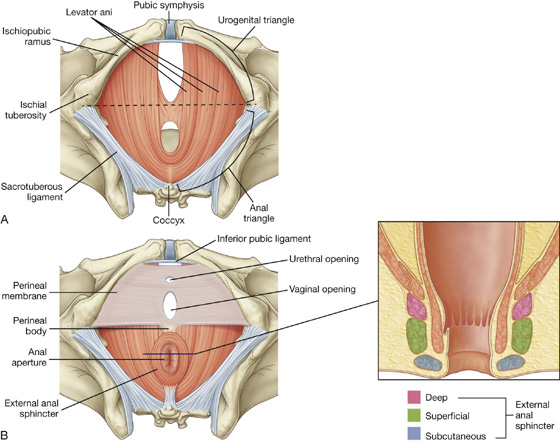
 The urogenital triangle is associated with the openings of the urinary systems and the reproductive systems and functions to anchor the external genitalia.
The urogenital triangle is associated with the openings of the urinary systems and the reproductive systems and functions to anchor the external genitalia. The ischial tuberosities are palpable on each side as large bony masses near the crease of skin (gluteal fold) between the thigh and gluteal region. They mark the lateral corners of the diamond-shaped perineum.
The ischial tuberosities are palpable on each side as large bony masses near the crease of skin (gluteal fold) between the thigh and gluteal region. They mark the lateral corners of the diamond-shaped perineum. The tip of the coccyx is palpable in the midline posterior to the anal aperture and marks the most posterior limit of the perineum.
The tip of the coccyx is palpable in the midline posterior to the anal aperture and marks the most posterior limit of the perineum. The anterior limit of the perineum is the pubic symphysis. In women, this is palpable in the midline deep to the mons pubis. In men, the pubic symphysis is palpable immediately superior to where the body of the penis joins the lower abdominal wall.
The anterior limit of the perineum is the pubic symphysis. In women, this is palpable in the midline deep to the mons pubis. In men, the pubic symphysis is palpable immediately superior to where the body of the penis joins the lower abdominal wall.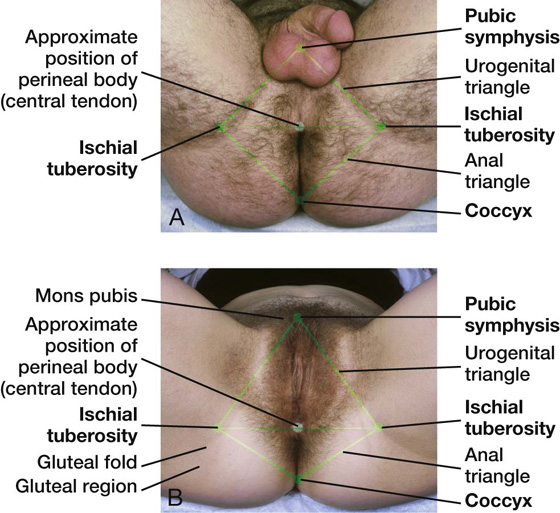
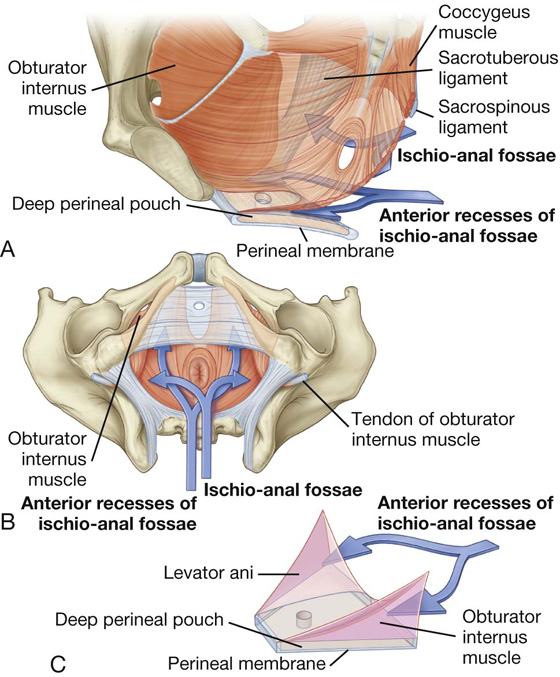
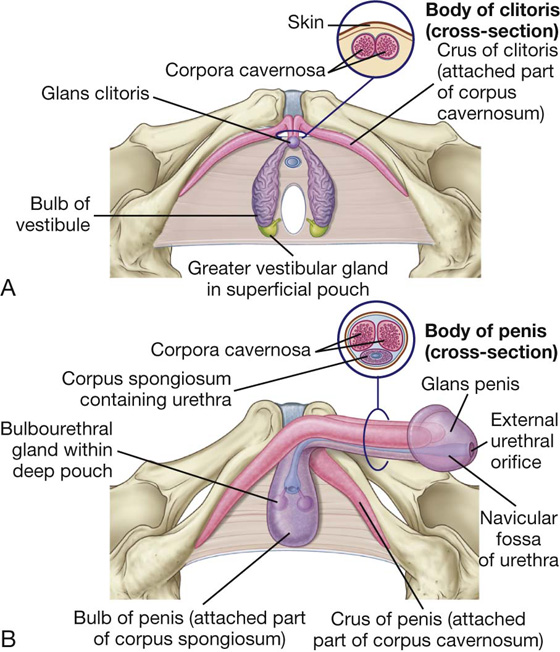
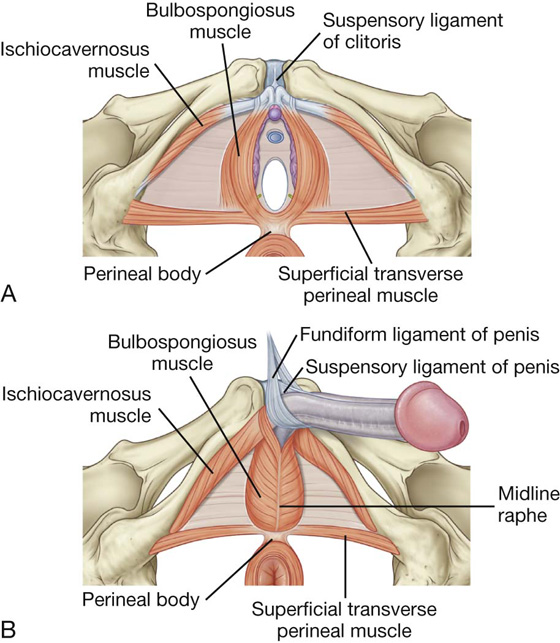
 skeletal muscles that are associated mainly with parts of the erectile structures attached to the perineal membrane and adjacent bone.
skeletal muscles that are associated mainly with parts of the erectile structures attached to the perineal membrane and adjacent bone. Unlike the root of penis, the root of clitoris technically consists only of the two crura. (Although the bulbs of the vestibule are attached to the glans clitoris by thin bands of erectile tissue, they are not included in the attached part of the clitoris.)
Unlike the root of penis, the root of clitoris technically consists only of the two crura. (Although the bulbs of the vestibule are attached to the glans clitoris by thin bands of erectile tissue, they are not included in the attached part of the clitoris.) The body of clitoris, which is formed only by the unattached parts of the two corpora cavernosa, angles posteriorly and is embedded in the connective tissues of the perineum.
The body of clitoris, which is formed only by the unattached parts of the two corpora cavernosa, angles posteriorly and is embedded in the connective tissues of the perineum. The root of penis consists of the two crura, which are proximal parts of the corpora cavernosa attached to the pubic arch, and the bulb of penis, which is the proximal part of the corpus spongiosum anchored to the perineal membrane.
The root of penis consists of the two crura, which are proximal parts of the corpora cavernosa attached to the pubic arch, and the bulb of penis, which is the proximal part of the corpus spongiosum anchored to the perineal membrane. The body of penis, which is covered entirely by skin, is formed by the tethering of the two proximal free parts of the corpora cavernosa and the related free part of the corpus spongiosum.
The body of penis, which is covered entirely by skin, is formed by the tethering of the two proximal free parts of the corpora cavernosa and the related free part of the corpus spongiosum.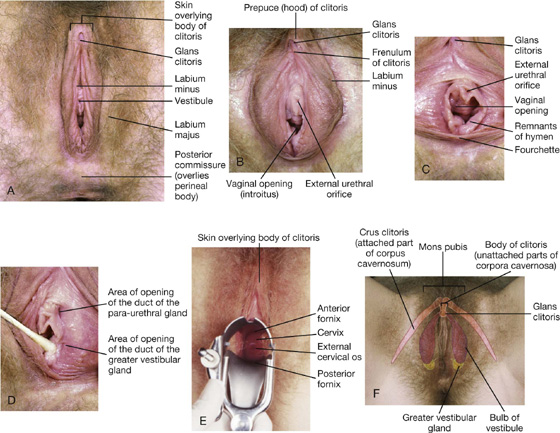
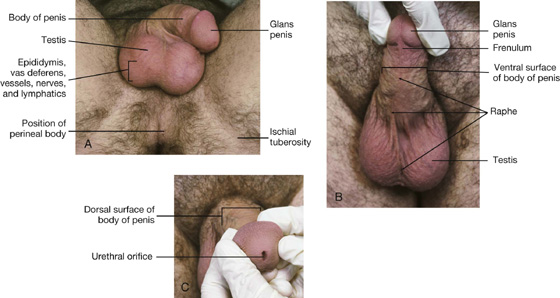
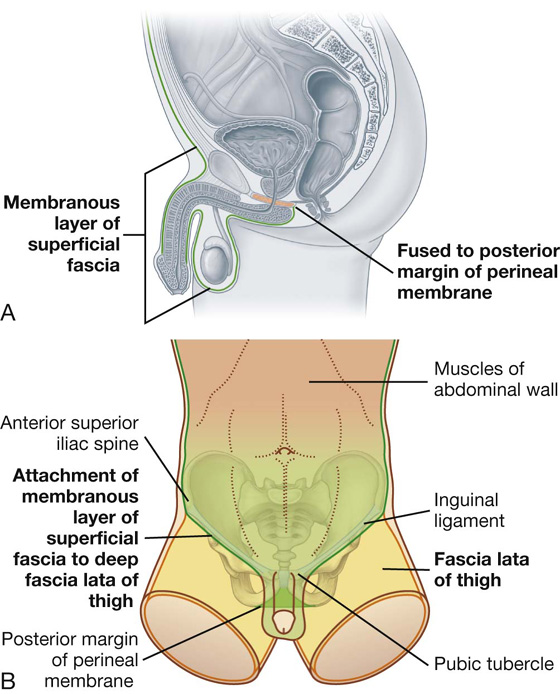
 to the ischiopubic rami that form the lateral borders of the urogenital triangle and therefore does not extend into the thigh.
to the ischiopubic rami that form the lateral borders of the urogenital triangle and therefore does not extend into the thigh.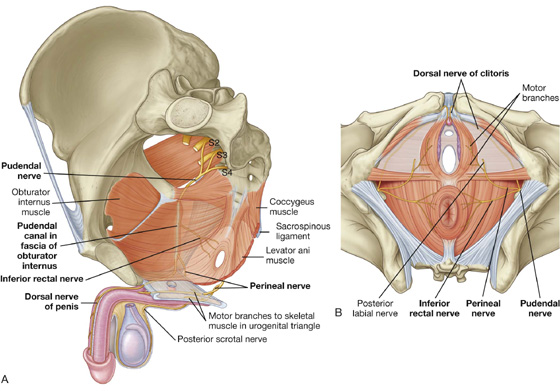
 The inferior rectal nerve is often multiple, penetrates through the fascia of the pudendal canal, and courses medially across the ischio-anal fossa to innervate the external anal sphincter and related regions of the levator ani muscles. The nerve is also general sensory for the skin of the anal triangle.
The inferior rectal nerve is often multiple, penetrates through the fascia of the pudendal canal, and courses medially across the ischio-anal fossa to innervate the external anal sphincter and related regions of the levator ani muscles. The nerve is also general sensory for the skin of the anal triangle. The perineal nerve passes into the urogenital triangle and gives rise to motor and cutaneous branches. The motor branches supply skeletal muscles in the superficial and deep perineal pouches. The largest of the sensory branches is the posterior scrotal nerve in men and the posterior labial nerve in women.
The perineal nerve passes into the urogenital triangle and gives rise to motor and cutaneous branches. The motor branches supply skeletal muscles in the superficial and deep perineal pouches. The largest of the sensory branches is the posterior scrotal nerve in men and the posterior labial nerve in women.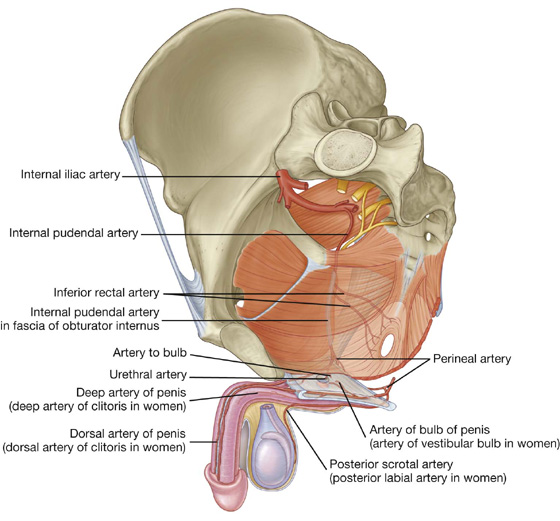
 The artery of bulb of penis has a branch that supplies the bulbourethral gland and then penetrates the perineal membrane to supply the corpus spongiosum.
The artery of bulb of penis has a branch that supplies the bulbourethral gland and then penetrates the perineal membrane to supply the corpus spongiosum. A urethral artery also penetrates the perineal membrane and supplies the penile urethra and surrounding erectile tissue to the glans.
A urethral artery also penetrates the perineal membrane and supplies the penile urethra and surrounding erectile tissue to the glans. Near the anterior margin of the deep perineal pouch, the internal pudendal artery bifurcates into two terminal branches. A deep artery of penis penetrates the perineal membrane to enter the crus and supply the crus and corpus cavernosum of the body. The dorsal artery of penis penetrates the anterior margin of the perineal membrane to meet the dorsal surface of the body of the penis. The vessel courses along the dorsal surface of the penis, medial to the dorsal nerve, and supplies the glans penis and superficial tissues of the penis; it also anastomoses with branches of the deep artery of penis and the urethral artery.
Near the anterior margin of the deep perineal pouch, the internal pudendal artery bifurcates into two terminal branches. A deep artery of penis penetrates the perineal membrane to enter the crus and supply the crus and corpus cavernosum of the body. The dorsal artery of penis penetrates the anterior margin of the perineal membrane to meet the dorsal surface of the body of the penis. The vessel courses along the dorsal surface of the penis, medial to the dorsal nerve, and supplies the glans penis and superficial tissues of the penis; it also anastomoses with branches of the deep artery of penis and the urethral artery.