Pediatric breathing circuits
Mapleson circuits
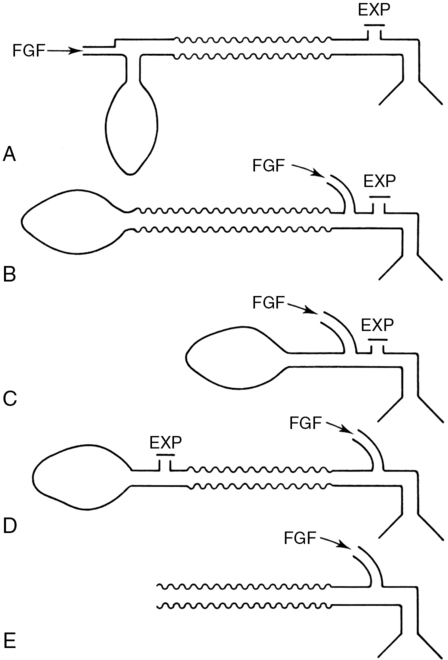
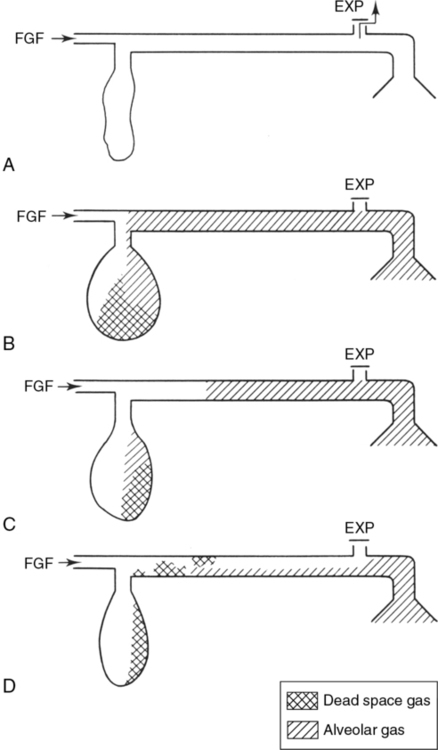
By the 1950s, several types of semiclosed circuits were used to deliver anesthetic gases. Semiclosed circuits under optimal conditions prevent rebreathing of alveolar gases. In 1954, the physicist William W. Mapleson analyzed five of these circuits and proposed optimal conditions that would prevent rebreathing. The efficiency of a nonrebreather is determined by the amount of fresh-gas flow, as well as by the positions of the inflow of fresh gas, the expiratory valve, and the reservoir bag. Mapleson labeled these circuits A, B, C, D, and E (Figure 193-1); subsequently, these circuits have been referred to as the Mapleson circuits, and Mapleson’s theoretical analyses have been verified empirically by others.
Mapleson A circuit
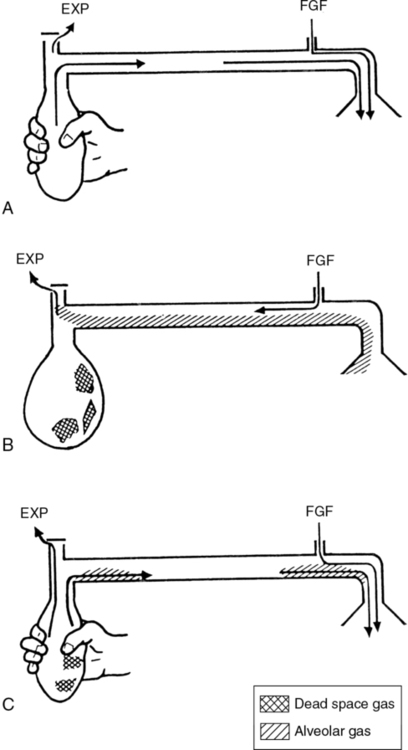
Immediately before the inspiratory phase of spontaneous ventilation occurs, continuous fresh gas flows into the reservoir bag and the circuit (Figure 193-2). As the patient inhales, the reservoir bag begins to empty. The lower the fresh-gas flow, or the higher the tidal volume, the emptier the reservoir bag becomes. During the expiratory phase, the reservoir bag completely fills with fresh gas, and, when the fresh-gas flow exceeds 70% of minute ventilation, enough pressure develops to vent alveolar and fresh gas through the APL valve. At the last stage of the expiratory phase, a pause occurs before the initiation of the next cycle. During the expiratory pause, fresh-gas flow further drives alveolar gas through the APL valve and virtually eliminates rebreathing.
In contrast with spontaneous ventilation, controlled ventilation (hand ventilation) of the Mapleson A circuit empties the reservoir bag at the end of the inspiratory phase (Figure 193-3). The reservoir bag refills with a mixture of alveolar gases, fresh gas, and dead-space gases during the expiratory phase. During controlled ventilation, the expiratory pause is minimal, which increases the likelihood of alveolar gas retention in the reservoir tubing and increases the amount of alveolar gases present with the initiation of the next inspiratory phase. Among the Mapleson circuits, the Mapleson A circuit under controlled ventilation is considered to be the least efficient at preventing rebreathing; rebreathing is overcome by increasing fresh-gas flow far exceeding minute ventilation.
Mapleson D circuit
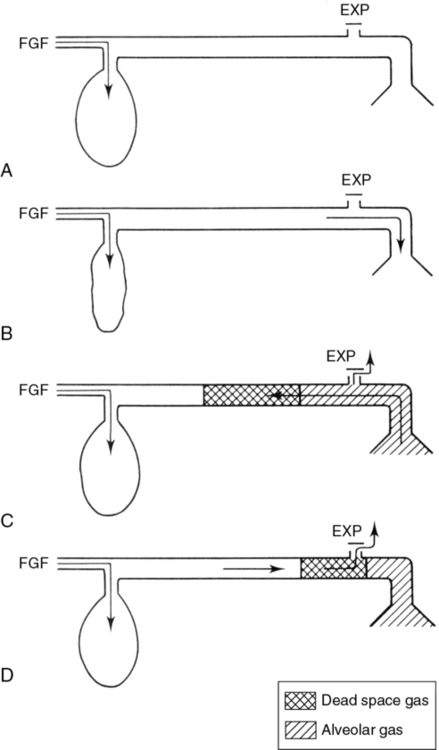
During spontaneous ventilation with the Mapleson D circuit (Figure 193-4), the alveolar gases are immediately mixed with fresh-gas flow as the gases pass down the reservoir tubing and fill the reservoir bag. When the reservoir bag is filled with a mixture of alveolar and fresh gases, the mixed gas is vented out the APL valve. The first gas to exit through the APL is the dead-space gas, followed by the mixture of alveolar and fresh gases. During the expiratory pause, fresh-gas flow expels most of the alveolar mixed gas if the minute ventilation is adequate. Therefore, to prevent rebreathing, the fresh-gas flow has to be twice the minute ventilation, and the expiratory pause has to be sufficiently long to allow all of the alveolar mixed gases to be expelled.
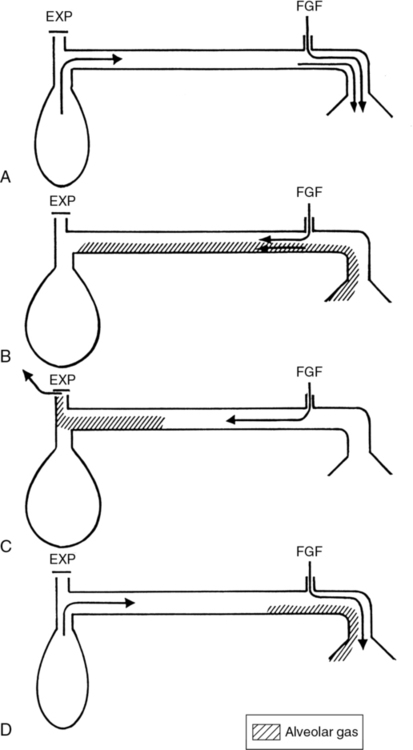
During the expiratory phase of controlled ventilation with the Mapleson D circuit (Figure 193-5), the fresh-gas flow drives the mixed alveolar gases and dead-space gases out of the APL valve. Furthermore, during the inhalation phase, the mixed alveolar gases are pushed and expelled not only by the continuous fresh-gas flow, but also by the positive pressure of controlled ventilation. The amount of fresh-gas flow necessary to minimize rebreathing is greater than the patient’s minute ventilation.