CHAPTER 76 Patient Selection Criteria for Deep Brain Stimulation in Movement Disorders
Successful deep brain stimulation (DBS) therapy for movement disorders depends on a series of interrelated procedures that include precise lead placement and proficient electrode programming. However, the first and most important step toward consistent DBS outcomes remains careful patient selection because more than 30% of DBS failures can generally be ascribed to an incorrect initial diagnosis or inappropriate indication for surgery.1
General Selection Process
Neurological Evaluation
Preoperative evaluation for DBS normally begins with assessment by a neurologist with specific expertise in the management of movement disorders. The neurological evaluation, possibly performed by a movement disorders specialist, should be focused on establishing that one of the diagnoses amenable to DBS treatment has been made properly. The diagnoses currently approved in the United States and widely accepted for DBS therapy throughout the world are essential tremor (ET), Parkinson’s disease (PD), and dystonia. Other tremors (i.e., midbrain, cerebellar, and orthostatic tremor), tics, and choreas (Huntington’s chorea and neuroacanthocytosis) have also been targeted with DBS in more experimental settings. Table 76-1 summarizes movement disorders in which DBS is currently indicated.
TABLE 76-1 Movement Disorders for Which Deep Brain Stimulation Is Currently Indicated
| FOOD AND DRUG ADMINISTRATION–APPROVED INDICATION FOR DBS |
| Idiopathic Parkinson’s disease |
| Essential tremor |
| Primary dystonia |
| Generalized |
| Segmental |
| Hemidystonia |
| Cervical |
| OTHER MOVEMENT DISORDERS POSSIBLY RESPONSIVE TO DBS |
| Tardive dystonia |
| Myoclonic dystonia |
| Pantothenate kinase-associated neurodegeneration (PKAN) |
| Huntington’s chorea |
| Chorea acanthocytosis |
| Tics |
| Cerebellar tremor (multiple sclerosis) |
| Midbrain tremor |
| Orthostatic tremor |
| Lesch-Nyhan syndrome |
| MOVEMENT DISORDERS POORLY RESPONSIVE TO DBS |
| Multiple system atrophy |
| Progressive supranuclear palsy |
| Corticobasal degeneration |
| Vascular parkinsonism |
| Secondary dystonias |
The value of the initial neurological visit does not end with the selection process. It also establishes a clinical baseline for the best postoperative management and provides an opportunity to educate patients and caregivers on the proper risks and expectations with respect to outcome. The initial programming and subsequent setting and medication adjustments may represent quite a challenge when the patient is unknown to the treating physician. Patient expectations must be realistic and discussed early in the process. False expectations by patients or family members are common reasons for “DBS failures.”1–3 DBS management represents a significant commitment of time, and consequently the patient and family must be motivated to undergo the challenges associated with the procedure.3 The role of the initial neurological evaluation extends to the surgical date in DBS centers that have the team neurologist present in the operating room; this person is an important source of clinical information to the surgeon and may be a calming influence on the patient during the implantation procedure.
Neurosurgical Evaluation
A fundamental task for the neurosurgeon is to define whether the risk-to-benefit ratio of the surgical procedure is acceptable to the patient. The most fearsome risk associated with a DBS procedure is the occurrence of intracerebral hemorrhage, which may cause contralateral weakness or other neurological deficits, including death in the most severe cases.4 The risk for hemorrhage may vary from center to center, based on the experience of the functional surgeon, but it is never null. In addition, there are device-related risks of system failure and infection, which can occur in 20% to 25% of patients in the best centers.5,6 Patients are also reminded that battery replacement, requiring minor surgery, will be necessary after 2 to 5 years, depending on the current drain associated with therapeutic stimulation.
In addition, general contraindications to surgery should be explored. Patients with uncontrolled hypertension or diabetes, coronary artery disease, cardiac pacemakers, liver or kidney failure, seizure disorders, or coagulopathies may be poor candidates, although the risk-benefit ratio of DBS surgery should be assessed individually in every case.7 If the patient is a good surgical candidate and agrees to surgery, a tentative date for surgery is scheduled and the remainder of the preoperative evaluation is completed. If there is disagreement about the proper surgical target or treatment modality, the patient’s case should be reviewed at a multidisciplinary conference to arrive at a consensus.
Neurocognitive and Psychiatric Evaluation
A neuropsychologist and a psychiatrist are essential members of a good DBS program because proper cognitive assessment and psychiatric screening are fundamental steps in patient selection, in particular for subthalamic nucleus (STN) DBS for PD. Little or no data are available on patients with premorbid psychiatric or cognitive symptoms undergoing DBS of the globus pallidus (pars) interna (GPi) or ventral intermediate (VIM) nucleus of the thalamus.8
The prevalence of dementia is high in patients with PD,9 and preoperative dementia is a risk factor for permanent cognitive decline after DBS.10,11 Because of insufficient evidence on the predictive validity of any given neuropsychological assessment, interview, or cognitive test,8 several test batteries are used for the selection of surgical candidates, with the goal of excluding those with dementia or severe deficits in executive function.12 No consensus guidelines or “gold standards” are available, and detailed comparative data have not been published. In designing a neuropsychological battery for DBS candidates, it is important to cover the major neurocognitive domains for both patient selection and follow-up (Table 76-2); at the same time, the battery should not be excessively long because patients with PD fatigue easily. Moreover, many PD patients who are DBS candidates have severe medication-related “on-off fluctuations” and can sometimes experience significant cognitive disturbance during the “off” cycle and yet perform relatively normally during the “on period.”8,13,14 Unfortunately, neuropsychological testing is not universally performed before DBS, potentially leading to negative postsurgical outcomes.1
TABLE 76-2 Neuropsychological Evaluation of Patients with Parkinson’s Disease for Deep Brain Stimulation Surgery
| CRITERIA EVALUATED | EVALUATION TOOL |
|---|---|
| General |
A full psychiatric evaluation is essential for patients who pass cognitive screening but have signs of untreated depression or psychosis, including dopaminergic dysregulation syndrome, medication-induced hypomania/mania, and suicide risk.8
The need for systematic neuropsychological and neuropsychiatric evaluation is less established for other DBS indications, including ET and dystonia. These conditions are not usually characterized by progressive neurodegeneration and dementia. In addition, patients with dystonia who are DBS candidates are normally young and less prone to suffer cognitive abnormalities after surgery.15
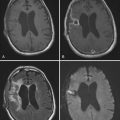
Neuroimaging
Preoperative imaging, preferably magnetic resonance imaging (MRI), is considered mandatory in patients being evaluated for DBS.8 In general, screening with MRI should rule out the presence of structural lesions or anatomic distortions16 that may either interfere with proper targeting (e.g., areas of encephalomalacia) or represent an increased risk for hemorrhage (e.g., abnormally enlarged lateral ventricles, severe brain atrophy). In addition, when the diagnosis of idiopathic PD is under scrutiny, MRI can show abnormalities typical of multiple system atrophy (MSA) or progressive supranuclear palsy (PSP),17 which would be a contraindication to DBS surgery (see Table 76-1).
Nuclear imaging studies (single-photon emission computed tomography/positron emission tomography) can occasionally be helpful in differentiating atypical parkinsonism from idiopathic PD.18 Although performed in the past to predict pallidotomy outcomes,19 the use of metabolic imaging modalities for screening patients undergoing DBS therapy is currently not part of routine DBS screening.
Specific Indications for Deep Brain Stimulation
Parkinson’s Disease
Selection Criteria
Among the many elements involved in successful DBS surgery for PD, patient selection has proved to be the most significant factor in determining postoperative benefit. Several good outcome predictors have been established, including a diagnosis of advanced idiopathic PD, response to levodopa, and absence of cognitive deterioration.8 The role of other variables, such as age and concurrent non–motor-associated symptoms, is less well defined (Table 76-3).
TABLE 76-3 Specific Deep Brain Stimulation Selection Criteria for Parkinson’s Disease
| SELECTION CRITERIA | COMMENTS |
|---|---|
| Diagnosis | A diagnosis of idiopathic PD should be carefully established according to available criteria because atypical parkinsonism (e.g., MSA, PSP, CBD) is generally poorly responsive to DBS |
| Disease severity |
The most important factors leading to performance of DBS are marked motor fluctuations in the response to dopaminergic therapy, including levodopa-induced dyskinesia and frequent and sudden wearing off with a prominent freezing responsive to levodopa
|
CBD, corticobasal degeneration; DBS, deep brain stimulation; MSA, multiple system atrophy; PD, Parkinson’s disease; PSP, progressive supranuclear palsy; UPDRS, Unified Parkinson’s Disease Rating Scale.
Diagnosis
DBS therapy should be considered only for patients with a confirmed diagnosis of advanced idiopathic PD, as defined by the presence of bradykinesia associated with at least one of the three following conditions: rigidity, resting tremor, and postural instability.21 It is important to differentiate idiopathic PD from the atypical parkinsonian disorders, which generally have an earlier onset and a more rapidly progressive course, including early dysautonomia, bulbar dysfunction, respiratory compromise, spasticity, ataxia, and apraxia.22 The most frequent atypical parkinsonian syndromes that can be misdiagnosed for idiopathic PD are PSP, MSA, Lewy body dementia (LBD), and corticobasal ganglionic degeneration (CBGD).21
Patients with atypical parkinsonian syndromes should not be selected for DBS therapy. Several case reports have demonstrated the ineffectiveness of DBS for MSA using either STN23–26 or GPi targets,27 even when the patient is responsive to levodopa. Although patients with levodopa-responsive bradykinesia, rigidity, or dystonia may show transient improvement,24 speech, swallowing, and gait usually deteriorate, motor fluctuations do not improve, and the levodopa dose remains unchanged.23,25 Clinical experience with DBS for other types of atypical parkinsonism, including CBGD and PSP, is extremely limited.28
Disease Severity and Duration
Although it is not considered a predictor of DBS outcome, the duration of PD should be taken into consideration when ruling out atypical parkinsonism.8,29 Typically, PD motor disability progresses slowly, so patients with advanced symptoms less than 5 years after onset should be evaluated further for atypical parkinsonism before being considered for DBS. At the same time, DBS should not be offered too late, when severe motor complications have resulted in marked loss of quality of life. Currently, DBS is performed after an average PD duration of 11 to 14 years. However, investigational studies offering DBS therapy at an early stage of the disease (7 years after initial motor symptoms) have yielded positive results, thus suggesting that DBS should be considered a therapeutic option earlier in the course of PD, when quality of life is still maintained.30 Indeed, there is little consensus on what defines advanced, medication-refractory PD and therefore candidacy for DBS. Severe PD disability generally coincides with Unified Parkinson’s Disease Rating Scale (UPDRS) motor scores of around 30 (out of a maximum of 108), and this would be a reasonable severity cutoff.7 Available experience with STN or GPi DBS has mostly been with levodopa-responsive patients having off-period UPDRS motor scores higher than 40 or 50.8 An ideal PD surgical candidate should be severely disabled when off levodopa while doing well, often with associated dyskinesias, on medications.
Response to Levodopa
A sustained preoperative response to levodopa not only provides support for the diagnosis of idiopathic PD but is also considered the best predictor of outcome after DBS.8,29 Levodopa responsiveness should ideally be assessed in each patient being considered for DBS8 with a dose sufficient to reproduce the patient’s best on response after a medication-free interval of 12 hours (usually overnight). It is particularly important to assess whether gait difficulties (in particular, freezing and imbalance) are sensitive to levodopa before offering DBS.
Levodopa response is normally defined as a 30% improvement in UPDRS motor scores (part III) over the off state,8,29 although there is no consensus on what constitutes an appropriate challenge dose of levodopa. A suprathreshold dose has been defined variably: use of the normal first dose of the day,31 a fixed 200-mg test dose,32 or even apomorphine33 has been proposed. In the experience of our group and others, however, patients with well-defined idiopathic PD can benefit from DBS even when their motor response is indeterminate because of intolerance to levodopa34 or when the most disabling symptom is a dopa-refractory tremor.2
Age
The role of age as an outcome predictor for DBS is somewhat controversial.28,35 Some authors consider advanced age (in particular, age older than 70 years) a poor outcome predictor if not a contraindication to DBS surgery20,29 because it has been correlated with negative outcomes such as cognitive decline11 and gait instability.35 Nonetheless, given that the average age at the onset of PD is 60 years and that the mean duration of illness is 10 to 15 years at the time of surgery, a large proportion of potential DBS candidates are 70 years or older. In reality, no specific age cutoff has been defined for DBS candidates with advanced PD.8 Decisions for or against DBS in the elderly population should be individualized by taking into account the grade of disability, risk factors for complications, general life expectancy, and the patient’s motivation. Unilateral procedures could be an option in some patients who are otherwise at too high a risk for a bilateral procedure. Alternative targets, such as thalamic and pallidal implants, may be considered in an older PD candidate when deteriorating cognition is an issue.36,37
Cognitive Status
Normal cognitive status should be established with an appropriate battery of neuropsychological testing.12 Preoperative dementia is considered a risk factor for permanent cognitive decline after DBS, independent of the target, even though the risk for cognitive decline after GPi DBS may be less than that after STN DBS.36,38 Older age and severe preoperative cognitive impairment might be associated with poorer neurobehavioral outcomes.39–44
Cognitive decline in PD is characterized by impaired executive function, visuospatial abnormalities, impaired memory, and language deficits.45 An appropriate scale that reliably incorporates executive function (e.g., frontal assessment battery and other practical tests of executive function) should be included in screening tests for PD dementia. However, in PD patients it may be difficult to assess impairment in domains other than memory.8 No studies have yet evaluated the sensitivity, specificity, and negative or positive predictive value of any disease, demographic, or test score variable in predicting which patients might experience such clinically meaningful cognitive declines.
Psychiatric Comorbid Conditions
A psychiatric evaluation should be performed to assess the presence of untreated depression, anxiety, apathy, dopaminergic dysregulation syndrome, medication-induced hypomania/mania, psychotic symptoms, and suicide risk because all have been related to some extent to STN DBS.8 Postoperative depression has been reported in 1% to 25% of patients,36,41,42,46–48 but preoperative assessment for depression is not always documented. Two studies focusing on whether preoperative depression was a risk factor for postoperative depression found conflicting results.42,47 In particular, neither study differentiated between postoperative depression and dopaminergic withdrawal symptoms.
The relationships among postoperative depression and preoperative depression, stimulation, medication changes, disease factors, and psychosocial factors has not been completely elucidated. A number of tools can be used, including the Beck Depression Inventory,49 Hamilton Depression Rating Scale,50 and Montgomery-Asberg Depression Rating Scale.51 Other scales, such as the Geriatric Depression Scale52 and Zung Self-Rating Depression Scale,53 have not been formally validated in patients with PD. Further research is required to determine the best (i.e., sensitive, specific, but also practical for clinicians to administer rapidly) depression screening tool for PD patients.
In a study focusing on behavioral symptoms, postoperative hypomania developed in one of two patients with preoperative hypomania.42 No associations between postoperative mania and preoperative mania have otherwise been reported; however, the adequacy of the preoperative assessment for behavioral disorders is not always known.
Psychosis in PD patients is characterized by visual hallucinations and delusions (often paranoid).54 Screening tools for psychosis should be sensitive to hallucinations, as well as other psychotic features such as delusions. Only one study evaluated the Parkinson Psychosis Rating Scale (PPRS), which may be appropriate for patients with PD.55 However, to determine its specificity, the PPRS needs to be evaluated in both nonpsychotic and psychotic PD patients. Criteria for psychosis from the fourth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV) have not been validated in PD. Likewise, there are insufficient data to draw conclusions about whether a preoperative history of medication-induced psychiatric symptoms or features of dopamine dysregulation syndrome worsen after surgery.
In uncontrolled series, suicide attempts and suicides have been documented in 0.5% to 2.9% of patients.42,56–58 A multicenter study of 450 STN DBS patients reported a postoperative suicide rate of 0.5%.57 In contrast, a study of 120 patients who underwent DBS (including patients with PD, dystonia, and ET) documented a postoperative suicide rate of 2.9% in PD patients who had undergone STN DBS.58 The authors suggested that young male patients with a history of multiple surgeries may be at greater risk for such outcomes. However, given the nature of the study as a small uncontrolled retrospective cohort from a single center, conclusions from this study are limited.
Target Selection
Ventral Intermediate Thalamus
The first reports of DBS for the treatment of PD used thalamic stimulation. In a series of 80 PD patients treated by either unilateral or bilateral VIM DBS, 88% achieved complete or nearly complete relief of tremor on the Fahn-Tolosa-Marín scale at 6 months to 8 years postoperatively.59 The effects of VIM DBS on other symptoms of PD, however, such as rigidity, bradykinesia, or drug-induced dyskinesias, were either short lasting or nonexistent. Currently, the role of VIM DBS for PD is limited to patients with tremor-predominant symptoms.
Globus Pallidus Interna
A number of studies have shown that bilateral GPi stimulation is safe and effective for the management of PD symptoms.60–62 Based on previous experience with pallidotomy,63 the ideal target for DBS is thought to be the most ventral-posterolateral area of the pallidum. In PD patients, GPi DBS improves tremor, rigidity, and bradykinesia in the off-medication state, as well as drug-induced dyskinesia, and results in overall improvement in UPDRS motor scores.64–66 The most pronounced and long-lasting effect is a reduction in on-medication dyskinesias,67 and PD patients suffering mainly from motor fluctuations and dyskinesias might be good candidates for GPi DBS. Unlike STN DBS, however, GPi DBS does not lead to a reduction in the patient’s levodopa requirement.68
Subthalamic Nucleus
The clinical efficacy of STN DBS in reducing PD symptoms has been reported by numerous investigators and validated in prospective, randomized trials.69–71 Long-term follow-up results show sustained improvement in tremor, rigidity, and akinesia in the off-medication state and a reduction in dopaminergic medication requirements 5 years after implantation.56,72–77 A reduction in levodopa dosage is usually achieved and leads indirectly to improvement in levodopa-induced dyskinesias.78,79 Initial improvements in gait, however, are not always sustained in the long term.56,69,80
Dystonia
Selection Criteria
Dystonia is a movement disorder characterized by sustained, involuntary muscle contractions generating twisting and repetitive movements or abnormal postures.81 Different muscle groups can be involved to a variable extent and severity can range from intermittent contractions limited to a single body region (focal dystonia) to generalized dystonia involving the axial and limb muscles. Dystonia may be classified by age at onset (early versus late), anatomic distribution (focal, segmental, multifocal, and generalized), and etiology. Etiologic classification of dystonia includes two broad categories: primary, or idiopathic, and secondary, or symptomatic.81 There is a bimodal distribution in the age at onset of primary dystonia, with modes at 9 years (early onset) and 45 years (late onset).82 The majority of early-onset cases begin with leg or arm dystonia that progresses to involve more than one limb, and in about 50% the dystonia eventually generalizes. Late-onset primary dystonia commonly affects the neck or cranial muscles and tends to remain localized as focal or segmental dystonia. With cloning of the DYT1 gene,83 it is now possible to diagnose a leading cause of generalized primary dystonia.
For the great majority of patients with dystonia, treatment is aimed at controlling symptoms rather than addressing the underlying cause. Pharmacologic therapies can be further subdivided into focal therapies such as intramuscular injections of botulinum toxin and systemic administration of medications that affect the central nervous system. Many medications have been reported to be of some benefit to selected dystonia patients, including anticholinergic, dopaminergic, and GABAergic (γ-aminobutyric acid agonists) agents, but no single therapy has been found to consistently produce improvement. Botulinum toxin is considered the treatment of choice for many focal dystonias.84
With the notable exception of DRD, pharmacologic treatment of primary generalized dystonia is mostly unsatisfactory. As a consequence, surgical attempts to relieve dystonic spasm have become progressively more relevant for the treatment of dystonia. Chronic stimulation of the GPi is currently considered a safe and effective treatment of advanced, disabling dystonia.85,86 Selection of appropriate patients for DBS is a prominent issue for neurologists and neurosurgeons who treat patients with movement disorders (Table 76-4). In determining an individual patient’s risk-benefit ratio, several variables need to be taken into consideration, including the patient’s motor, cognitive, overall medical, and psychological status.87 The best candidates are patients with primary generalized, segmental, or cervical dystonia or hemidystonia who have not responded to medications or botulinum toxin injections and have progressed to profound disability as a result of motor impairment or pain.87
TABLE 76-4 Specific Deep Brain Stimulation Selection Criteria for Dystonia
| SELECTION CRITERIA | COMMENT |
|---|---|
| Diagnosis |
A trial of levodopa therapy should always be performed to rule out patients with DRD. It is important to determine whether the target symptom or symptoms for surgery are the major source of disability and the likelihood that the symptom or symptoms will improve with DBS. Other sources of disability must be identified, and the patient’s individual risk of encountering complications should be considered. Ideally, surgery should be performed before secondary orthopedic complications (i.e., contractures) compromise the neurological rehabilitation.87
In general, patients with primary dystonia are better candidates for DBS than those with secondary dystonia.88 Short disease duration appears to be a positive outcome predictor.89 DYT1+ patients seem to respond better than others in some, but not all series, and their advantage may be attributable to their young age at onset and relatively quick progression warranting DBS surgery after a short duration of disease.85,89,90
DBS results in patients with secondary dystonia have generally been disappointing,88,91–93 with some notable exceptions, including those with tardive dystonia,94,95 myoclonic dystonia,96 and pantothenate kinase–associated neurodegeneration (PKAN).97–99
Target Selection
Although thalamic and subthalamic targets have occasionally been used as DBS targets, in particular for secondary dystonias, the vast majority of procedures for dystonia target the globus pallidum; indeed, DBS of the GPi proved to be a safe and effective treatment of advanced, disabling primary85,86 and some types of secondary dystonia.94,95,100,101
Thalamic DBS may be an option for some patients with secondary dystonia, including posttraumatic hemidystonia, postanoxic dystonia and bilateral basal ganglia necrosis, myoclonic dystonia, and dystonic paroxysmal nonkinesigenic dyskinesia.88 The thalamic structures targeted in these cases are the VIM nucleus,102–104 the ventro-oralis anterior (VOA) nucleus,105,106 and the ventroposterolateral nucleus.107 Combined implants of thalamic and pallidal targets in the same patients have also been successfully attempted.106,108
STN DBS is currently the procedure of choice for the treatment of medically refractory PD, for which it is effective in treating both “off”- and “on”-state dystonias.109 These results have prompted speculation on the potential of this target for the treatment of idiopathic torsion dystonia. Potential advantages of targeting the STN instead of the GPi include more rapid response to stimulation and the ability to achieve identical or enhanced clinical effects with less energy, thereby prolonging battery life. These ideas are supported by encouraging preliminary results.110,111
Essential Tremor
Selection Criteria
ET is a progressive neurological disease characterized by a postural or kinetic tremor affecting mainly the arms, but also the head, jaw, and voice, as well as other body regions.112 Tremor usually begins in the arms and then spreads to other regions in some patients. Essential head tremor is more likely to develop in women than in men.113 Other types of tremor may also occur, including occasionally rest tremor in the arms.114 In some patients, gait and balance difficulties, anxiety and depressive symptoms, and cognitive difficulty may also develop.115,116
ET is a common neurological disease, with a prevalence of approximately 4% in persons 40 years and older and considerably higher in the elderly population.114 ET is often mild and is occasionally defined as “benign essential tremor” or “familial tremor” because of the fact that approximately half the cases are transmitted with a pattern of inheritance most consistent with autosomal dominant transmission. However, no genes have as yet been identified.
Patients with severe tremor have difficulty performing many of their routine activities of daily living and require pharmacologic or surgical therapy.114,117 Before considering surgery, patients should undergo an adequate trial of first-line drugs alone and in combination, including propranolol (60 to 320 mg/day) and primidone (300 to 750 mg/day). If patients fail first-line therapy, trials of second-line (clonazepam, alprazolam, and topiramate) and third-line (clonidine, acetazolamide, flunarizine, and theophylline) drugs may be administered; however, these medications rarely result in marked improvement, and surgery should not be delayed unnecessarily.114 In general, oral medications tend to be more helpful for limb tremor than for head or voice tremor, which may benefit from botulinum toxin injections.
DBS is indicated for ET patients refractory to medications when tremor severity and distribution cause unacceptable impairment of activities of daily living.59,118–129 Table 76-5 summarizes current DBS selection criteria for ET. The most widely accepted scale for evaluating the severity of ET is the Fahn-Tolosa-Marín rating scale for tremor.130
TABLE 76-5 Specific Deep Brain Stimulation Selection Criteria for Essential Tremor
| SELECTION CRITERIA | COMMENT |
|---|---|
| Diagnosis | The symptom tremor is generally well responsive to thalamic DBS |
| Disease severity | Tremor must significantly interfere with the patient’s quality of life |
| Disease duration | No limitation |
| Age at surgery | Older age is not a specific exclusion criterion if the patient is cognitively intact and in good general health |
| Response to medications | Patients with ET must have medication-refractory symptoms, defined as having failed maximal titrations and preferably combinations of a beta blocker, primidone, and possibly a benzodiazepine |
| Cognitive status |
DBS, deep brain stimulation; ET, essential tremor; VIM, ventral intermediate nucleus of the thalamus.
Few reports have addressed cognitive function in patients with ET to document abnormalities that would suggest systematic neuropsychological testing before DBS surgery.131–136 However, no standardized cognitive screening has consistently been advocated to test ET patients before DBS implants. Quality of life can be investigated with the Quality of Life in Essential Tremor Questionnaire (QUEST); although still partially validated, this scale is the only one available to assess impairment of daily living activities in patients with ET.137
Target Selection
At present, the VIM nucleus of the thalamus is the most commonly targeted site for DBS in patients with ET.120,138–141 In addition, there is limited yet positive evidence that stimulation of the STN can also produce satisfactory tremor control in ET patents.142 Unilateral VIM stimulation results in marked short- and long-term improvement in contralateral action and postural tremor and in some cases may have a mild ipsilateral effect.122,141,143 There is, however, a decreasing effect over time, most noticeable with tremor of action.144
Because voice tremor is not reliably improved by unilateral VIM stimulation,125,145,146 it should not be a primary indication for DBS. Head tremor has also shown inconsistent or unpredictable improvement with unilateral and bilateral stimulation.3,122,125,139,147
Complex Tremor Syndromes
Selection Criteria
Cerebellar Tremor
Cerebellar tremor is characterized by a coarse action tremor, generally less than 5 Hz, and is occasionally associated with postural tremor. Typically, cerebellar tremor affects the upper extremities unilaterally or bilaterally, although head and trunk titubation is also common and may be the most disabling feature. A simple observation of the frequency and regularity of movements when performing typical activities (e.g., drinking from a cup) may give clues to the diagnosis.148 Cerebellar tremor is most commonly problematic in patients with MS, after head injury, following brainstem cerebrovascular events, and occasionally in those with spinocerebellar ataxia or the cerebellar subtype of MSA.
Disabling tremor that impairs a patient’s quality of life is seen in approximately 10% to 15% of MS clinic patients.149 Drug therapy with agents such as carbamazepine, clonazepam, l,5-hydroxytryptophan, and buspirone is rarely successful; occasional patients may have mild improvement with high-dose propranolol.149 Appropriate patients for stereotactic surgery should have tremor that significantly interferes with activities of daily living. Only two disease severity scales have been proposed, and both take into account tremor severity and distribution for evaluation of MS tremor.150,151 No validation studies are available.
MS patients have multiple other nervous system lesions that result in neurological deficits, and it is important to distinguish between tremor-related disability and disability caused by other deficits. In fact, studies of the effects of DBS on MS tremor consistently show some improvement in the majority of patients, but the improvement is often overshadowed by progression of the other symptoms of MS.141 Patients with marked sensory impairment in the target limb, excessive arm weakness, or marked truncal weakness resulting in a bed-bound state should not be offered surgery because significant functional improvement is unlikely to be achieved even if the tremor were eliminated.149
Holmes’ Tremor
Also known as “rubral tremor” or midbrain tremor, HT is an irregular, low-frequency rest and intention tremor that is enhanced by posture in most cases. The Movement Disorder Society has established three criteria for the diagnosis of HT, including (1) the presence of both resting and intentional tremor, (2) a slow frequency, usually less than 4.5 Hz, and (3) a variable delay (usually months) after occurrence of the lesion.152 HT has been reported in association with trauma, cerebrovascular events, neuroleptic agents, infections, MS, neoplasm, Wilson’s disease, cavernoma, and radiation toxicity.153 The pathogenesis of HT has been attributed to combined destruction of the pallidothalamic and cerebellothalamic pathways, with involvement of the rubro-olivo-cerebello-rubral loops and possibly the nigrostriatal system.154
Thalamic Tremor
TT is characterized by variable degrees of dystonia, athetosis, chorea, and action tremor and occasionally associated with myoclonic components after lateral posterior thalamic stroke, most frequently hemorrhagic in nature.155,156 Dystonia, athetosis, and chorea are usually associated with position sensory loss after thalamic lesions, whereas tremor and myoclonic movements are most frequently related to cerebellar ataxia.155 The pathogenesis of TT is unclear, but it has been related to defective motor-sensory integrative processes because of persistent failure of proprioceptive sensory and cerebellar input after recovery of motor dysfunction, with severe lateral-posterior thalamic strokes simultaneously damaging the lemniscal sensory pathway, the cerebellar-rubrothalamic tract, and, less severely, the pyramidal tract.155 TT generally starts gradually and progressively worsens for weeks or months before stabilizing. Involuntary movements usually remain persistent and only rarely show spontaneous improvement.155
Orthostatic Tremor
Described as a quivering tremor of the legs and trunk during standing accompanied by a sensation of unsteadiness, OT is usually relieved by walking or leaning against objects.157 It is characterized by distinctive 14- to 16-Hz lower extremity electromyographic activity that is evoked on standing but not while walking or supine. OT is believed to be a variant of ET despite lack of response to alcohol, beta blockers, and primidone and the absence of a family history.158,159 OT usually responds to clonazepam but shows a progressive reduction in the latency between standing and the onset of unsteadiness, with an increase in tremor severity that may result in an inability to stand still without support. Although patients may not fall, the sensation of unsteadiness can markedly interfere with their quality of life.160
Tremor severity, consequent disability, and lack of response to common antitremor medications are the criteria generally used to select patients with atypical tremor syndromes for DBS surgery. No specific neuropsychological selection criteria have been described in the literature, but it is probably good practice to test any DBS candidate older than 50 years. Physiologic assessment of patients with complex tremor and ataxia may help predict those who will most likely benefit from surgery. Thalamotomy has resulted in complete resolution of upper extremity postural tremor with frequencies greater than 3 Hz as assessed by an accelerometer, whereas tremor of less than 3 Hz did not improve postoperatively.149 Furthermore, frequency analysis during a wrist-tracking task may also be predictive of the response of action tremor to thalamotomy, with an 80% reduction in tremor in patients with just one frequency peak in the spectra and only a 30% reduction in those with multiple frequency peaks.161
MS patients who are being considered for thalamic DBS surgery to control intention tremor should undergo brain MRI within 3 months of surgery because their disease can progress without obvious clinical sequelae. We were surprised in one instance when the targeting MRI of an MS patient revealed a new plaque in the internal capsule that extended into the ventrolateral thalamus, the preferred target for tremor control. Stimulation within the ventrolateral thalamus in this patient yielded unwanted side effects at very low currents, most probably caused by aberrant conduction through this new plaque. Consequently, a DBS lead could not be implanted.16
Target Selection
DBS has been shown to be beneficial for several atypical tremor syndromes, although fewer cases have been reported and the benefit is less remarkable and less consistent than that reported for ET.141 Most studies of DBS for MS tremor targeted the thalamus and the VIM nucleus in particular.162,163 Other successful targets include the ventralis oralis posterior (VOP) nucleus of the thalamus and the zona incerta. Stimulation of these alternative targets produced a 64% improvement in postural tremor and a 36% improvement in intention tremor.164 Dual-electrode stimulation to simultaneously target the VIM/VOP border and the VOA/VOP border also provided significant reduction of tremor in one MS patient.165 Because DBS of the thalamic VIM nucleus produces often inconsistent and short-term benefits, further research is necessary to determine the most effective target for MS-associated tremor.
With the exception of one patient treated by GPi DBS,166 the thalamic VIM nucleus is also the most frequent target for successful DBS treatment of atypical tremors (mostly TT and HT) resulting from posttraumatic and vascular lesions.165,167–176 The youngest patient who underwent implantation, a 14-year-old girl, showed remarkable improvement (90%) with VIM DBS up to 2.5 years.153 Successful VIM DBS has also been reported in three patients suffering from OT.160,177
The caudal (motor) zona incerta has also been used as an alternative target for DBS treatment of atypical tremor, with reported improvement in all components of tremor affecting both the distal and proximal ends of limbs, as well as the axial musculature.178 Two patients with dystonic tremor and one with neuropathic-related tremor responded well to unilateral stimulation of the posterior subthalamic area.179 Subthalamic-thalamic stimulation achieved suppression of tremor related to spinocerebellar ataxia type 2.180
Multiple targets have also been used to improve HT symptoms. Simultaneous placement of two DBS electrodes at the VIM/VOP border and at the VOA/VOP border resulted in excellent reduction of symptoms in three patients.165 In one patient, combined STN-VIM stimulation but not stimulation of the STN or VIM nucleus alone produced global relief of tremor without adverse events.170
Tourette’s Syndrome
Selection Criteria
Tourette’s syndrome (TS) is a neuropsychiatric disorder characterized by multiple motor and vocal tics that wax and wane over time, often associated with behavioral disorders.181 The motor tics are stereotyped repetitive and involuntary movements that generally affect the face, head, and upper part of the body, whereas vocal tics are sounds usually represented by shouting, barking, sniffing, or grunting. Comorbid conditions include attention-deficit/hyperactivity disorder, obsessive-compulsive disorder, anxiety, and self-injurious behavior. Symptoms often disappear before or during early adulthood or may be controlled with medication.181 Some patients, however, may have medically resistant severe and disabling tics that persist or worsen in adulthood.
To be considered a surgical candidate, TS patients need to be refractory to medical treatment and be severely disabled by the condition.182 A multidisciplinary approach that includes neurological and psychiatric evaluation is strongly recommended. The main scale used to evaluate the severity of symptoms is the Yale Global Tic Severity Scale.183
The Dutch-Flemish Tourette Surgery Study Group has established guidelines for DBS in patients with TS,184 and the Movement Disorders Society has published the recommendations of the Tourette Syndrome Association.182 The proposed selection criteria include the following:
Target Selection
The choice of target in TS is still controversial inasmuch as good outcomes have been reported with both thalamic and GPi DBS. To date, five targets have been used for DBS in patients with TS: (1) the medial portion of the thalamus at the cross point of the centromedian nucleus/substantia periventricularis/VOA nucleus,187–190 (2) the medial portion of the thalamus at the centromedian nucleus and parafascicular nucleus,183 (3) the posteroventrolateral GPi,191 (4) the anteromedial GPi,183 and (5) the nucleus accumbens and anterior limb of the internal capsule.192,193
Huntington’s Disease and Other Choreas
Selection Criteria
Two types of chorea have been considered for treatment with DBS: Huntington’s disease (HD) and neuroacanthocytosis (NA). HD is a progressive hereditary neurodegenerative disease manifested by chorea and other hyperkinetic (dystonia, myoclonus, tics) and hypokinetic (parkinsonism) movement disorders. In addition, a variety of psychiatric and behavioral symptoms, along with cognitive decline, contribute significantly to the patient’s disability. No effective neuroprotective or disease-modifying therapy for HD is available.194 NA includes combined features of chorea, orofacial tics, dystonia, amyotrophy, and elevated serum creatine kinase levels, with a peculiar finding of spiked red blood cells (acanthocytosis) in the blood smear. NA has been described most commonly as an autosomal recessive hereditary gene defect located on chromosome 9, but it also occurs as an autosomal dominant disorder and as part of an X-linked disorder called McLeod’s syndrome.195 In most cases, the neurological disability caused by chorea is progressive.
Clinical assessment of patients with chorea can be standardized with the UHDRS196 or the Abnormal Involuntary Movement Scale.197 The functional status of HD patients is commonly assessed with the Total Functional Capacity Scale and the Independence Scale, both of which are incorporated into the UHDRS.
Medical therapy for chorea is fairly limited and restricted to symptomatic relief. Numerous medications have been used to improve chorea, including typical and atypical neuroleptics, dopamine depleters, antidepressants, antiglutamatergic drugs, GABA agonists, antiepileptic medications, acetylcholinesterase inhibitors, and botulinum toxin.196
Target Selection
Thalamic and pallidal targets have been used for DBS therapy in patients with chorea. Bilateral GPi DBS in HD was first used for the treatment of a 43-year-old patient who had genetically confirmed HD, rapidly progressive disabling chorea despite medical treatment (tetrabenazine, haloperidol, amantadine), and no psychiatric symptoms.198
Positive results of bilateral GPi DBS were reported in a second HD patient with debilitating choreoathetoid movements refractory to medical management (tetrabenazine, neuroleptics, minocycline) but no psychiatric comorbid conditions.199 The effects were maintained at 1 year, but progressive hypokinetic symptoms eventually developed. Combined thalamic (VOP) and pallidal (GPi) stimulation proved effective in controlling abnormal movements in one case of intractable senile chorea.200
A slightly larger experience is available for NA. Bilateral high-frequency stimulation (160 Hz) of the VOP nucleus of the thalamus improved trunk spasms in one patient with NA, with stable clinical benefit for 1 year, although no clear effect on dysarthria was observed.201 Interestingly, high-frequency stimulation of the GPi failed to improve202 or even worsened NA-related chorea,203 whereas the best results were obtained with low-frequency (40 Hz) bilateral pallidal DBS using monopolar stimulation on two adjacent contacts.203
Charles PD, Van Blercom N, Krack P, et al. Predictors of effective bilateral subthalamic nucleus stimulation for PD. Neurology. 2002;59:932-934.
Defer GL, Widner H, Marié RM, et al. Core Assessment Program for Surgical Interventional Therapies in Parkinson’s Disease (CAPSIT-PD). Mov Disord. 1999;14:572-584.
Deuschl G, Schade-Brittinger C, Krack P, et al. A randomized trial of deep-brain stimulation for Parkinson’s disease. N Engl J Med. 2006;355:896-908.
Guehl D, Cuny E, Tison F, Benazzouz A, et al. Deep brain pallidal stimulation for movement disorders in neuroacanthocytosis. Neurology. 2007;68:160-161.
Isaias IU, Alterman RL, Tagliati M. Outcome predictors of pallidal stimulation in patients with primary dystonia: the role of disease duration. Brain. 2008;131:1895-1902.
Kleiner-Fisman G, Herzog J, Fisman DN, et al. Subthalamic nucleus deep brain stimulation: summary and meta-analysis of outcomes. Mov Disord. 2006;21:290-304.
Krack P, Batir A, Van Blercom N, et al. Five-year follow-up of bilateral stimulation of the subthalamic nucleus in advanced Parkinson’s disease. N Engl J Med. 2003;349:1925-1934.
Kupsch A, Benecke R, Müller J, et al. Pallidal deep-brain stimulation in primary generalized or segmental dystonia. N Engl J Med. 2006;355:1978-1990.
Lang AE, Houeto JH, Krack P, et al. Deep brain stimulation: preoperative issues. Mov Disord. 2006;21:171-196.
Lyons KE, Pahwa R. Deep brain stimulation and tremor. Neurotherapeutics. 2008;5:331-338.
Malhado-Chang N, Alterman R, Tagliati M. Deep brain stimulation. In: Factor SA, Weiner WJ, editors. Parkinson’s Disease: Diagnosis and Clinical Management. 2nd ed. New York: Demos; 2007:663-688.
Mink JW, Walkup J, Frey KA, et al. Patient selection and assessment recommendations for deep brain stimulation in Tourette syndrome. Mov Disord. 2006;21:1831-1838.
Moro E, Lang AE, Strafella AP, et al. Bilateral globus pallidus stimulation for Huntington’s disease. Ann Neurol. 2004;56:290-294.
Okun M, Tagliati M, Pourfar M, et al. Management of referred DBS failures: A retrospective analysis from two movement disorders centers. Arch Neurol. 2005;62:1250-1255.
Okun MS, Fernandez HH, Pedraza O, et al. Development and initial validation of a screening tool for Parkinson disease surgical candidates. Neurology. 2004;63:161-163.
Pillon B. Neuropsychological assessment for management of patients with deep brain stimulation. Mov Disord. 2002;17:116-122.
Russmann H, Ghika J, Villemure JG, et al. Subthalamic nucleus deep brain stimulation in Parkinson disease patients over age 70 years. Neurology. 2004;63:1952-1954.
Schuurman PR, Bosch DA, Bossuyt PM, et al. A comparison of continuous thalamic stimulation and thalamotomy for suppression of severe tremor. N Engl J Med. 2000;342:461-468.
Vidailhet M, Vercueil L, Houeto JL. Bilateral deep-brain stimulation of the globus pallidus in primary generalized dystonia. N Engl J Med. 2005;352:459-467.
Volkmann J, Allert N, Voges J, et al. Long-term results of bilateral pallidal stimulation in Parkinson’s disease. Ann Neurol. 2004;55:871-875.
Voon V, Kubu C, Krack P, et al. Deep brain stimulation: neuropsychological and neuropsychiatric issues. Mov Disord. 2006;21:305-326.
Voon V, Moro E, Saint-Cyr J, et al. Psychiatric symptoms following surgery for Parkinson’s disease with an emphasis on subthalamic stimulation. Adv Neurol. 2005;96:130-147.
Weaver FM, Follett K, Stern M, et al. Bilateral deep brain stimulation vs best medical therapy for patients with advanced Parkinson disease: a randomized controlled trial. JAMA. 2009;301:63-73.
Welter ML, Houeto JL, Tezenas du Montcel S, et al. Clinical predictive factors of subthalamic stimulation in Parkinson’s disease. Brain. 2002;125:575-583.
Yap L, Kouyialis A, Varma TR. Stereotactic neurosurgery for disabling tremor in multiple sclerosis: thalamotomy or deep brain stimulation? Br J Neurosurg. 2007;21:349-354.
1 Okun M, Tagliati M, Pourfar M, et al. Management of referred DBS failures: a retrospective analysis from two movement disorders centers. Arch Neurol. 2005;62:1250-1255.
2 Okun MS, Fernandez HH, Pedraza O, et al. Development and initial validation of a screening tool for Parkinson disease surgical candidates. Neurology. 2004;63:161-163.
3 Rodriguez RL, Fernandez HH, Haq I, et al. Pearls in patient selection for deep brain stimulation. Neurologist. 2007;13:253-260.
4 Rezai AR, Kopell BH, Gross RE, et al. Deep brain stimulation for Parkinson’s disease: surgical issues. Mov Disord. 2006;21:197-218.
5 Oh MY, Abosch A, Kim SH, et al. Long-term hardware-related complications of deep brain stimulation. Neurosurgery. 2002;50:1268-1274.
6 Blomstedt P, Hariz MI. Hardware-related complications of deep brain stimulation: a ten year experience. Acta Neurochir. 2005;147:1061-1064.
7 Malhado-Chang N, Alterman R, et al. Deep brain stimulation. In: Factor SA, Weiner WJ, editors. Parkinson’s Disease: Diagnosis and Clinical Management. 2nd ed. New York: Demos; 2007:663-688.
8 Lang AE, Houeto JH, Krack P, et al. Deep brain stimulation: preoperative issues. Mov Disord. 2006;21:171-196.
9 Mayeux R, Denaro J, Hemenegildo N, et al. A population-based investigation of Parkinson’s disease with and without dementia. Relationship to age and gender. Arch Neurol. 1992;49:492-497.
10 Hariz MI, Johansson F, Shamsgovara P, et al. Bilateral subthalamic nucleus stimulation in a parkinsonian patient with preoperative deficits in speech and cognition: persistent improvement in mobility but increased dependency: a case study. Mov Disord. 2000;15:136-139.
11 Saint-Cyr JA, Trepanier LL, Kumar R, et al. Neuropsychological consequences of chronic bilateral stimulation of the subthalamic nucleus in Parkinson’s disease. Brain. 2000;123:2091-2108.
12 Pillon B. Neuropsychological assessment for management of patients with deep brain stimulation. Mov Disord. 2002;17:116-122.
13 Voon V, Kubu C, Krack P, et al. Deep brain stimulation: neuropsychological and neuropsychiatric issues. Mov Dis. 2006;21:305-326.
14 Parsons TD, Rogers SA, Braaten AJ, et al. Cognitive sequelae of subthalamic nucleus deep brain stimulation in Parkinson’s disease: a meta-analysis. Lancet Neurol. 2006;5:578-588.
15 Hälbig TD, Gruber D, Kopp UA, et al. Pallidal stimulation in dystonia: effects on cognition, mood, and quality of life. J Neurol Neurosurg Psychiatry. 2005;76:1713-1716.
16 Tagliati M, Alterman RL. Guidelines for patient selection for ablative and deep brain stimulation surgery. Semin Neurosurg. 2001;12:161-168.
17 Seppi K. MRI for the differential diagnosis of neurodegenerative parkinsonism in clinical practice. Parkinsonism Relat Disord. 2007;13:400-405.
18 Antonini A, Kazumata K, Feigin A, et al. Differential diagnosis of parkinsonism with [18F]fluorodeoxyglucose and PET. Mov Disord. 1998;13:268-274.
19 Alterman RL, Kelly P, Sterio D, et al. Selection criteria for unilateral posteroventral pallidotomy. Acta Neurochir Suppl. 1997;68:18-23.
20 Charles PD, Van Blercom N, Krack P, et al. Predictors of effective bilateral subthalamic nucleus stimulation for PD. Neurology. 2002;59:932-934.
21 Hughes AJ, Daniel SE, Kilford L, et al. Accuracy of clinical diagnosis of idiopathic Parkinson’s disease. A clinico-pathological study of 100 cases. J Neurol Neurosurg Psychiatry. 1992;55:181-184.
22 Jankovic J. Parkinson’s disease: clinical features and diagnosis. J Neurol Neurosurg Psychiatry. 2008;79:368-376.
23 Tarsy D, Apetauerova D, Ryan P, et al. Adverse effects of subthalamic nucleus DBS in a patient with multiple system atrophy. Neurology. 2003;61:247-249.
24 Visser-Vandewalle V, Temel Y, Colle H, et al. Bilateral high-frequency stimulation of the subthalamic nucleus in patients with multiple system atrophy-parkinsonism. Report of four cases. J Neurosurg. 2003;98:882-887.
25 Chou KL, Forman MS, Trojanowski JQ, et al. Subthalamic nucleus deep brain stimulation in a patient with levodopa-responsive multiple system atrophy. Case report. J Neurosurg. 2004;100:553-556.
26 Lezcano E, Gomez-Esteban JC, Zarranz JJ, et al. Parkinson’s disease–like presentation of multiple system atrophy with poor response to STN stimulation: a clinicopathological case report. Mov Disord. 2004;19:973-977.
27 Patrick S, Kristl V, Miet DL, et al. Deep brain stimulation of the internal pallidum in multiple system atrophy. Parkinsonism Relat Disord. 2006;12:181-183.
28 Bergmann KJ, Salak VL. Subthalamic stimulation improves levodopa responsive symptoms in a case of progressive supranuclear palsy. Parkinsonism Relat Disord. 2008;14:348-352.
29 Welter ML, Houeto JL, Tezenas du Montcel S, et al. Clinical predictive factors of subthalamic stimulation in Parkinson’s disease. Brain. 2002;125:575-583.
30 Schüpbach WM, Maltête D, Houeto JL, et al. Neurosurgery at an earlier stage of Parkinson’s disease: a randomized, controlled trial. Neurology. 2007;68:267-271.
31 Pahwa R, Wilkinson SB, Overman J, et al. Bilateral subthalamic stimulation in patients with Parkinson disease: long-term follow up. J Neurosurg. 2003;99:71-77.
32 Vingerhoets FJ, Villemure JG, Temperli P, et al. Subthalamic DBS replaces levodopa in Parkinson’s disease: two-year follow-up. Neurology. 2002;58:396-401.
33 Pinter MM, Alesch F, Murg M, et al. Apomorphine test: a predictor for motor responsiveness to deep brain stimulation of the subthalamic nucleus. J Neurol. 1999;246:907-913.
34 Katayama Y, Kasai M, Oshima H, et al. Subthalamic nucleus stimulation for Parkinson disease: benefits observed in levodopa-intolerant patients. J Neurosurg. 2001;95:213-221.
35 Russmann H, Ghika J, Villemure JG, et al. Subthalamic nucleus deep brain stimulation in Parkinson disease patients over age 70 years. Neurology. 2004;63:1952-1954.
36 Volkmann J, Allert N, Voges J, et al. Safety and efficacy of pallidal or subthalamic nucleus stimulation in advanced PD. Neurology. 2001;56:548-551.
37 Okun MS, Foote KD. Subthalamic nucleus vs globus pallidus interna deep brain stimulation, the rematch: will pallidal deep brain stimulation make a triumphant return? Arch Neurol. 2005;62:533-536.
38 Vingerhoets G, van der Linden C, Lannoo E, et al. Cognitive outcome after unilateral pallidal stimulation in Parkinson’s disease. J Neurol Neurosurg Psychiatry. 1999;66:297-304.
39 Defer GL, Widner H, Marié RM, et al. Core Assessment Program for Surgical Interventional Therapies in Parkinson’s Disease (CAPSIT-PD). Mov Disord. 1999;14:572-584.
40 Alegret M, Junque C, Valldeoriola F, et al. Effects of bilateral subthalamic stimulation on cognitive function in Parkinson disease. Arch Neurol. 2001;58:1223-1227.
41 Dujardin K, Defebvre L, Krystkowiak P, et al. Influence of chronic bilateral stimulation of the subthalamic nucleus on cognitive function in Parkinson’s disease. J Neurol. 2001;248:603-611.
42 Houeto JL, Mesnage V, Mallet L, et al. Behavioural disorders, Parkinson’s disease and subthalamic stimulation. J Neurol Neurosurg Psychiatry. 2002;72:701-707.
43 Trepanier LL, Kumar R, Lozano AM, et al. Neuropsychological outcome of GPi pallidotomy and GPi or STN deep brain stimulation in Parkinson’s disease. Brain Cogn. 2000;42:324-347.
44 Jarraya B, Bonnet AM, Duyckaerts C, et al. Parkinson’s disease, subthalamic stimulation, and selection of candidates: a pathological study. Mov Disord. 2003;18:1517-1520.
45 Aarsland D, Andersen K, Larsen JP, et al. Prevalence and characteristics of dementia in Parkinson disease: an 8-year prospective study. Arch Neurol. 2003;60:387-392.
46 Martinez-Martin P, Valldeoriola F, Tolosa E, et al. Bilateral subthalamic nucleus stimulation and quality of life in advanced Parkinson’s disease. Mov Disord. 2002;17:372-377.
47 Berney A, Vingerhoets F, Perrin A, et al. Effect on mood of subthalamic DBS for Parkinson’s disease: a consecutive series of 24 patients. Neurology. 2002;59:1427-1429.
48 Herzog J, Volkmann J, Krack P, et al. Two-year follow-up of subthalamic deep brain stimulation in Parkinson’s disease. Mov Disord. 2003;18:1332-1337.
49 Beck AT, Steer RA, Ball R, et al. Comparison of Beck Depression Inventories -IA and -II in psychiatric outpatients. J Pers Assess. 1996;67:588-597.
50 Hamilton M. A rating scale for depression. J Neurol Neurosurg Psychiatry. 1960;23:56-62.
51 Montgomery SA, Asberg M. A new depression scale designed to be sensitive to change. Br J Psychiatry. 1979;134:382-389.
52 Yesavage JA, Brink TL, Rose TL, et al. Development and validation of a geriatric depression screening scale: a preliminary report. J Psychiatr Res. 1983;17:37-49.
53 Zung WWK. A self-rating depression scale. Arch Gen Psychiatry. 1965;12:63-70.
54 Weintraub D, Stern MB. Psychiatric complications in Parkinson disease. Am J Geriatr Psychiatry. 2005;13:844-851.
55 Hobson P, Meara J. The detection of dementia and cognitive impairment in a community population of elderly people with Parkinson’s disease by use of the CAMCOG neuropsychological test. Age Ageing. 1999;28:39-43.
56 Krack P, Batir A, Van Blercom N, et al. Five-year follow-up of bilateral stimulation of the subthalamic nucleus in advanced Parkinson’s disease. N Engl J Med. 2003;349:1925-1934.
57 Voon V, Moro E, Saint-Cyr J, et al. Psychiatric symptoms following surgery for Parkinson’s disease with an emphasis on subthalamic stimulation. Adv Neurol. 2005;96:130-147.
58 Burkhard PR, Vingerhoets FJ, Berney A, et al. Suicide after successful deep brain stimulation for movement disorders. Neurology. 2004;63:2170-2172.
59 Benabid AL, Pollak P, Gao D, et al. Chronic electrical stimulation of the ventralis intermedius nucleus of the thalamus as a treatment of movement disorders. J Neurosurg. 1996;84:203-214.
60 Volkmann J, Sturm V, Weiss P, et al. Bilateral high-frequency stimulation of the internal globus pallidus in advanced Parkinson’s disease. Ann Neurol. 1998;44:953-961.
61 Ghika J, Villemure JG, Fankhauser H, et al. Efficiency and safety of bilateral contemporaneous pallidal stimulation (deep brain stimulation) in levodopa-responsive patients with Parkinson’s disease with severe motor fluctuations: a 2-year follow-up review. J Neurosurg. 1998;89:713-718.
62 Loher TJ, Burgunder JM, Pohle T, et al. Long-term pallidal deep brain stimulation in patients with advanced Parkinson disease: 1-year follow-up study. J Neurosurg. 2002;96:844-853.
63 Laitinen LV, Bergenheim AT, Hariz MI, et al. Ventroposterolateral pallidotomy can abolish all parkinsonian symptoms. Stereotact Funct Neurosurg. 1992;58:14-21.
64 Gross C, Rougier A, Guehl D, et al. High-frequency stimulation of the globus pallidus internalis in Parkinson’s disease: a study of seven cases. J Neurosurg. 1997;87:491-498.
65 Pahwa R, Wilkinson S, Smith D, et al. High-frequency stimulation of the globus pallidus for the treatment of Parkinson’s disease. Neurology. 1997;49:249-253.
66 Kumar R, Lang AE, Rodriguez-Oroz MC, et al. Deep brain stimulation of the globus pallidus pars interna in advanced Parkinson’s disease. Neurology. 2000;55:S34-S39.
67 Volkmann J, Allert N, Voges J, et al. Long-term results of bilateral pallidal stimulation in Parkinson’s disease. Ann Neurol. 2004;55:871-875.
68 Visser-Vandewalle V, van der Linden C, Temel Y, et al. Long-term motor effect of unilateral pallidal stimulation in 26 patients with advanced Parkinson disease. J Neurosurg. 2003;99:701-707.
69 DBS for Parkinson’s Disease Study Group. Deep-brain stimulation of the subthalamic nucleus or the pars interna of the globus pallidus in Parkinson’s disease. N Engl J Med. 2001;345:956-963.
70 Deuschl G, Schade-Brittinger C, Krack P, et al. A randomized trial of deep-brain stimulation for Parkinson’s disease. N Engl J Med. 2006;355:896-908.
71 Weaver FM, Follett K, Stern M, et al. Bilateral deep brain stimulation vs best medical therapy for patients with advanced Parkinson disease: a randomized controlled trial. JAMA. 2009;301:63-73.
72 Schüpbach WMM, Chastan N, Welter ML, et al. Stimulation of the subthalamic nucleus in Parkinson’s disease: a 5 year follow up. J Neurol Neurosurg Psychiatry. 2005;76:1640-1644.
73 Visser-Vandewalle V, van der Linden C, Temel Y, et al. Long-term effects of bilateral subthalamic nucleus stimulation in advanced Parkinson disease: a four year follow-up study. Parkinsonism Relat Disord. 2005;11:157-165.
74 Rodriguez-Oroz MC, Obeso JA, Lang AE, et al. Bilateral deep brain stimulation in Parkinson’s disease: a multicentre study with 4 years follow-up. Brain. 2005;128:2240-2249.
75 Østergaard K, Aa Sunde N. Evolution of Parkinson’s disease during 4 years of bilateral deep brain stimulation of the subthalamic nucleus. Mov Disord. 2006;21:624-631.
76 Liang GS, Chou KL, Baltuch GH, et al. Long-term outcomes of bilateral subthalamic nucleus stimulation in patients with advanced Parkinson’s disease. Stereotact Funct Neurosurg. 2006;84:221-227.
77 Piboolnurak P, Lang AE, Lozano AM, et al. Levodopa response in long-term bilateral subthalamic stimulation for Parkinson’s disease. Mov Disord. 2007;22:990-997.
78 Hamani C, Richter E, Schwalb JM, et al. Bilateral subthalamic nucleus stimulation for Parkinson’s disease: a systematic review of the clinical literature. Neurosurgery. 2005;56:1313-1321.
79 Kleiner-Fisman G, Herzog J, Fisman DN, et al. Subthalamic nucleus deep brain stimulation: summary and meta-analysis of outcomes. Mov Disord. 2006;21:290-304.
80 Tagliati M. Fine-tuning gait in Parkinson disease. Neurology. 2008;71:76-77.
81 Fahn S, Marsden CD, Calne DB. Classification and investigation in dystonia. In: Marsden CD, Fahn S, editors. Movement Disorders 2. London: Buttersworth; 1987:332-358.
82 Bressman SB, de Leon D, Brin MF, et al. Idiopathic torsion dystonia among Ashkenazi Jews: evidence for autosomal dominant inheritance. Ann Neurol. 1989;26:612-620.
83 Ozelius LJ, Hewett JW, Page C, et al. The early-onset torsion dystonia gene (DYT1) encodes an ATP-binding protein. Nat Genet. 1997;17:40-48.
84 Geyer HL, Tagliati M, Blatt K, Bressman S. Generalized torsion dystonia. In: Noseworthy J, editor. Neurological Therapeutics: Principles and Practice. 2nd ed. London: Taylor & Martin; 2006:2853-2863.
85 Vidailhet M, Vercueil L, Houeto JL. Bilateral deep-brain stimulation of the globus pallidus in primary generalized dystonia. N Engl J Med. 2005;352:459-467.
86 Kupsch A, Benecke R, Müller J, et al. Pallidal deep-brain stimulation in primary generalized or segmental dystonia. N Engl J Med. 2006;355:1978-1990.
87 Volkmann J, Benecke R. Deep brain stimulation for dystonia: patient selection and evaluation. Mov Disord. 2001;17:112-115.
88 Tagliati M, Shils JL, Sun C, Alterman RL. Deep brain stimulation for dystonia. Expert Rev Med Devices. 2004;1:33-41.
89 Isaias IU, Alterman RL, Tagliati M. Outcome predictors of pallidal stimulation in patients with primary dystonia: the role of disease duration. Brain. 2008;131:1895-1902.
90 Coubes P, Roubertie A, Vayssiere N, et al. Treatment of DYT1-generalised dystonia by stimulation of the internal globus pallidus. Lancet. 2000;355:2220-2221.
91 Tronnier V, Fogel W. Pallidal stimulation for generalized dystonia. Report of three cases. J Neurosurg. 2000;92:453-456.
92 Vercueil L, Pollak P, Fraix V, et al. Deep brain stimulation in the treatment of severe dystonia. J Neurol. 2001;248:695-700.
93 Ostrem JL, Starr PA. Treatment of dystonia with deep brain stimulation. Neurotherapeutics. 2008;5:320-330.
94 Trottenberg T, Volkmann J, Deuschl G, et al. Treatment of severe tardive dystonia with pallidal deep brain stimulation. Neurology. 2005;64:344-346.
95 Sako W, Goto S, Shimazu H, et al. Bilateral deep brain stimulation of the globus pallidus internus in tardive dystonia. Mov Disord. 2008;23:1929-1931.
96 Liu X, Griffin IC, Parkin SG, et al. Involvement of the medial pallidum in focal myoclonic dystonia: a clinical and neurophysiological case study. Mov Disord. 2002;17:346-353.
97 Castelnau P, Cif L, Valente EM, et al. Pallidal stimulation improves pantothenate kinase–associated neurodegeneration. Ann Neurol. 2005;57:738-741.
98 Krause M, Fogel W, Tronnier V, et al. Long-term benefit to pallidal deep brain stimulation in a case of dystonia secondary to pantothenate kinase–associated neurodegeneration. Mov Disord. 2006;21:2255-2257.
99 Mikati MA, Yehya A, Darwish H, et al. Deep brain stimulation as a mode of treatment of early onset pantothenate kinase–associated neurodegeneration. Eur J Paediatr Neurol. 2009;13:61-64.
100 Zhang J, Zhang K, Wang Z, Ge M, et al. Deep brain stimulation in the treatment of secondary dystonia. Chin Med J. 2006;119:2069-2074.
101 Pretto TE, D’Alvi A, Jung Kang U, et al. A prospective blinded evaluation of deep brain stimulation for the treatment of secondary dystonia and primary torticollis syndromes. J Neurosurg. 2008;109:405-409.
102 Trottenberg T, Meissner W, Kabus C, et al. Neurostimulation of the ventral intermediate thalamic nucleus in inherited myoclonus-dystonia syndrome. Mov Disord. 2001;16:769-771.
103 Loher TJ, Krauss JK, Burgunder JM, et al. Chronic stimulation of the ventrointermediate thalamus is effective for treatment of peripherally-induced dystonic paroxysmal nonkinesigenic dyskinesia. Neurology. 2001;56:268-270.
104 Kuncel AM, Turner DA, Ozelius LJ, et al. Myoclonus and tremor response to thalamic deep brain stimulation parameters in a patient with inherited myoclonus-dystonia syndrome. Clin Neurol Neurosurg. 2009;111:303-306.
105 Ghika J, Villemure JG, Miklossy J, et al. Postanoxic generalized dystonia improved by bilateral Voa thalamic deep brain stimulation. Neurology. 2002;58:311-313.
106 Fukaya C, Katayama Y, Kano T, et al. Thalamic deep brain stimulation for writer’s cramp. J Neurosurg. 2007;107:977-982.
107 Sellal F, Hirsch E, Barth P, et al. A case of symptomatic hemidystonia improved by ventrolateral thalamic stimulation. Mov Disord. 1993;8:515-518.
108 Schadt CR, Charles PD, Davis TL, et al. Thalamotomy, DBS-Vim, and DBS-GPi for generalized dystonia: a case report. Tenn Med. 2007;100:38-39.
109 Krack P, Pollak P, Limousin P, et al. From off-period dystonia to peak-dose chorea. The clinical spectrum of varying subthalamic nucleus activity. Brain. 1999;122:1133-1146.
110 Sun B, Chen S, Zhan S, et al. Subthalamic nucleus stimulation for primary dystonia and tardive dystonia. Acta Neurochir Suppl. 2007;97:207-214.
111 Kleiner-Fisman G, Linliang GS, Moberg PJ, et al. Subthalamic nucleus deep brain stimulation for severe idiopathic dystonia: impact on severity, neuropsychological status, and quality of life. J Neurosurg. 2007;107:29-36.
112 Benito-Leon J, Louis ED. Clinical update: diagnosis and treatment of essential tremor. Lancet. 2007;369:1152-1153.
113 Louis ED, Ford B, Frucht S. Factors associated with increased risk of head tremor in essential tremor: a community-based study in northern Manhattan. Mov Disord. 2003;18:432-436.
114 Louis ED, Barnes LF, Albert SM, et al. Correlates of functional disability in essential tremor. Mov Disord. 2001;16:914-920.
115 Stolze H, Petersen G, Raethjen J, et al. The gait disorder of advanced essential tremor. Brain. 2001;124:2278-2286.
116 Tan EK, Fook-Chong S, Lum SY, et al. Non-motor manifestations in essential tremor: use of a validated instrument to evaluate a wide spectrum of symptoms. Parkinsonism Relat Disord. 2005;11:375-380.
117 Rajput AH, Robinson CA, Rajput AH. Essential tremor course and disability: a clinicopathologic study of 20 cases. Neurology. 2004;62:932-936.
118 Blond S, Siegfried J. Thalamic stimulation for the treatment of tremor and other movement disorders. Acta Neurochir. 1991;52:109-111.
119 Alesch F, Pinter MM, Helscher RJ, et al. Stimulation of the ventral intermediate thalamic nucleus in tremor dominated Parkinson’s disease and essential tremor. Acta Neurochir. 1995;136:75-81.
120 Koller W, Pahwa R, Busenbark K, et al. High-frequency unilateral thalamic stimulation in the treatment of essential and parkinsonian tremor. Ann Neurol. 1997;42:292-299.
121 Hariz GM, Bergenheim AT, Hariz MI, et al. Assessment of ability/disability in patients treated with chronic thalamic stimulation for tremor. Mov Disord. 1998;13:78-83.
122 Ondo W, Jankovic J, Schwartz K, et al. Unilateral thalamic deep brain stimulation for refractory essential tremor and Parkinson’s disease tremor. Neurology. 1998;51:1063-1069.
123 Limousin P, Speelman JD, Gielen F, et al. Multicentre European study of thalamic stimulation in parkinsonian and essential tremor. J Neurol Neurosurg Psychiatry. 1999;66:289-296.
124 Kumar K, Kelly M, Toth C. Deep brain stimulation of the ventral intermediate nucleus of the thalamus for control of tremors in Parkinson’s disease and essential tremor. Stereotact Funct Neurosurg. 1999;72:47-61.
125 Sydow O, Thobois S, Alesch F, et al. Multicentre European study of thalamic stimulation in essential tremor: a six year follow up. J Neurol Neurosurg Psychiatry. 2003;74:1362-1363.
126 Koller WC, Lyons KE, Wilkinson SB, et al. Long-term safety and efficacy of unilateral deep brain stimulation of the thalamus in essential tremor. Mov Disord. 2001;16:464-468.
127 Rehncrona S, Johnels B, Widner H, et al. Long-term efficacy of thalamic deep brain stimulation for tremor: double-blind assessments. Mov Disord. 2003;18:163-170.
128 Putzke JD, Wharen REJr, Obwegeser AA, et al. Thalamic deep brain stimulation for essential tremor: recommendations for long-term outcome analysis. Can J Neurol Sci. 2004;31:333-342.
129 Pahwa R, Lyons KE, Wilkinson SB, et al. Long-term evaluation of deep brain stimulation of the thalamus. J Neurosurg. 2006;104:506-512.
130 Fahn S, Tolosa E, Marín C. Clinical rating scale for tremor. In: Jankovic J, Tolosa E, editors. Parkinson’s Disease and Movement Disorders. Baltimore: Urban & Schwartzenberg; 1988:225-234.
131 Gasparini M, Bonifati V, Fabrizio E, et al. Frontal lobe dysfunction in essential tremor: a preliminary study. J Neurol. 2001;248:399-402.
132 Lacritz LH, Dewey RBJr, Giller C, et al. Cognitive functioning in individuals with “benign” essential tremor. J Int Neuropsychol Soc. 2002;8:125-129.
133 Tröster AI, Woods SP, Fields JA, et al. Neuropsychological deficits in essential tremor: an expression of cerebello-thalamo-cortical pathophysiology? Eur J Neurol. 2002;9:143-151.
134 Lombardi WJ, Woolston DJ, Roberts JW, et al. Cognitive deficits in patients with essential tremor. Neurology. 2001;57:785-790.
135 Sahin HA, Terzi M, Ucak S, et al. Frontal functions in young patients with essential tremor: a case comparison study. J Neuropsychiatry Clin Neurosci. 2006;18:64-72.
136 Benito-Leon J, Louis ED. Essential tremor: emerging views of a common disorder. Nat Clin Pract Neurol. 2006;2:666-678.
137 Tröster AI, Pahwa R, Fields JA, et al. Quality of life in Essential Tremor Questionnaire (QUEST): development and initial validation. Parkinsonism Relat Disord. 2005;11:367-373.
138 Schuurman PR, Bosch DA, Bossuyt PM, et al. A comparison of continuous thalamic stimulation and thalamotomy for suppression of severe tremor. N Engl J Med. 2000;342:461-468.
139 Pahwa R, Lyons KE, Wilkinson SB, et al. Comparison of thalamotomy to deep brain stimulation of the thalamus in essential tremor. Mov Disord. 2001;16:140-143.
140 Vaillancourt DE, Sturman MM, Verhagen Metman L, et al. Deep brain stimulation of the Vim thalamic nucleus modifies several features of essential tremor. Neurology. 2003;61:919-925.
141 Lyons KE, Pahwa R. Deep brain stimulation and tremor. Neurotherapeutics. 2008;5:331-338.
142 Lind G, Schechtmann G, Lind C, et al. Subthalamic stimulation for essential tremor. Short- and long-term results and critical target area. Stereotact Funct Neurosurg. 2008;86:253-258.
143 Obwegeser AA, Uitti RJ, Witte RJ, et al. Quantitative and qualitative outcome measures after thalamic deep brain stimulation to treat disabling tremors. Neurosurgery. 2001;48:278-281.
144 Blomstedt P, Hariz GM, Hariz MI, et al. Thalamic deep brain stimulation in the treatment of essential tremor: a long-term follow-up. Br J Neurosurg. 2007;21:504-509.
145 Carpenter MA, Pahwa R, Miyawaki KL, et al. Reduction in voice tremor under thalamic stimulation. Neurology. 1998;50:796-798.
146 Obwegeser AA, Uitti RJ, Turk MF, et al. Thalamic stimulation for the treatment of midline tremors in essential tremor patients. Neurology. 2000;54:2342-2344.
147 Pahwa R, Lyons KL, Wilkinson SB, et al. Bilateral thalamic stimulation for the treatment of essential tremor. Neurology. 1999;53:1447-1450.
148 Deuschl G, Raethjen J, Lindemann M, et al. The pathophysiology of tremor. Muscle Nerve. 2001;24:716-735.
149 Alusi SH, Aziz TZ, Glickman S, et al. Stereotactic lesional surgery for the treatment of tremor in multiple sclerosis: a prospective case-controlled study. Brain. 2001;124:1576-1589.
150 Speelman JD, Van Manen J. Stereotactic thalamotomy for the relief of intention tremor of multiple sclerosis. J Neurol Neurosurg Psychiatry. 1984;47:596-599.
151 Bain PG, Findley LJ, Atchison P, et al. Human Movement and Balance Unit, Institute of Neurology, London, UK. Assessing tremor severity. J Neurol Neurosurg Psychiatry. 1993;56:868-873.
152 Deuschl G, Bain P, Brin M. Consensus statement of the Movement Disorder Society on tremor. Ad Hoc Scientific Committee. Mov Disord. 1998;13:2-23.
153 Peker S, Isik U, Akgun Y, et al. Deep brain stimulation for Holmes’ tremor related to a thalamic abscess. Childs Nerv Syst. 2008;24:1057-1062.
154 Deuschl G, Bergman H. Pathophysiology of nonparkinsonian tremors. Mov Disord. 2002;17:41-48.
155 Kim JS. Delayed onset mixed involuntary movements after thalamic stroke: clinical, radiological and pathophysiological findings. Brain. 2001;124:299-309.
156 Miwa H, Hatori K, Kondo T, et al. Thalamic tremor: case reports and implications of the tremor-generating mechanism. Neurology. 1996;46:75-79.
157 Heilman KM. Orthostatic tremor. Arch Neurol. 1984;41:880-881.
158 Papa SM, Gershink OS. Orthostatic tremor: an essential tremor variant? Mov Disord. 1988;3:97-108.
159 Fitzerald PM, Jankovic J. Orthostatic tremor: an association with essential tremor. Mov Disord. 1991;6:60-64.
160 Espay AJ, Duker AP, Chen R, et al. Deep brain stimulation of the ventral intermediate nucleus of the thalamus in medically refractory orthostatic tremor: preliminary observations. Mov Disord. 2008;23:2357-2362.
161 Liu X, Aziz TZ, Miall RC, et al. Frequency analysis of involuntary movements during wrist tracking: a way to identify MS patients with tremor who benefit from thalamotomy. Stereotact Funct Neurosurg. 2000;74:53-62.
162 Wishart HA, Roberts DW, Roth RM, et al. Chronic deep brain stimulation for the treatment of tremor in multiple sclerosis: review and case reports. J Neurol Neurosurg Psychiat. 2003;74:1392-1397.
163 Yap L, Kouyialis A, Varma TR. Stereotactic neurosurgery for disabling tremor in multiple sclerosis: thalamotomy or deep brain stimulation? Br J Neurosurg. 2007;21:349-354.
164 Nandi D, Aziz TZ. Deep brain stimulation in the management of neuropathic pain and multiple sclerosis tremor. J Clin Neurophysiol. 2004;21:31-39.
165 Foote KD, Seignourel P, Fernandez HH. Dual electrode thalamic deep brain stimulation for the treatment of posttraumatic and multiple sclerosis tremor. Neurosurgery. 2006;58:280-284.
166 Lim DA, Khandhar SM, Heath S, et al. Multiple target deep brain stimulation for multiple sclerosis related and poststroke Holmes’ tremor. Stereotact Funct Neurosurg. 2007;85:144-149.
167 Broggi G, Brock S, Franzini A, et al. A case of posttraumatic tremor treated by chronic stimulation of the thalamus. Mov Disord. 1993;8:206-208.
168 Shepherd GMG, Tauböll E, Bakke SJ, et al. Midbrain tremor and hypertrophic olivary degeneration after pontine hemorrhage. Mov Disord. 1997;12:432-437.
169 Kudo M, Goto S, Nishikawa S, et al. Bilateral thalamic stimulation for Holmes’ tremor caused by unilateral brainstem lesion. Mov Disord. 2001;16:170-174.
170 Romanelli P, Bronte-Stewart H, Courtney T, et al. Possible necessity for deep brain stimulation of both the ventralis intermedius and subthalamic nuclei to resolve Holmes tremor: case report. J Neurosurg. 2003;99:566-571.
171 Samadani U, Umemura A, Jaggi JL, et al. Thalamic deep brain stimulation for disabling tremor after excision of a midbrain cavernous angioma. J Neurosurg. 2003;98:888-890.
172 Goto S, Yamada K. Combination of thalamic Vim stimulation and Gpi pallidotomy synergistically abolishes Holmes’ tremor. J Neurol Neurosurg Psychiatry. 2004;75:1200-1207.
173 Nikkhah G, Prokop T, Hellwig B, et al. Deep brain stimulation of the nucleus ventralis intermedius for Holmes (rubral) tremor and associated dystonia caused by upper brainstem lesions: report of two cases. J Neurosurg. 2004;100:1079-1083.
174 Piette T, Mescola P, Henriet M, et al. A surgical approach to Holmes’ tremor associated with high-frequency synchronous bursts. Rev Neurol. 2004;160:707-711.
175 Umemura A, Samadani U, Jaggi JL, et al. Thalamic deep brain stimulation for posttraumatic action tremor. Clin Neurol Neurosurg. 2004;106:280-283.
176 Diederich NJ, Verhagen Metman L, Bakay RA, et al. Ventral intermediate thalamic stimulation in complex tremor syndromes. Stereotact Funct Neurosurg. 2008;86:167-172.
177 Guridi J, Rodriguez-Oroz MC, Arbizu J, et al. Successful thalamic deep brain stimulation for orthostatic tremor. Mov Disord. 2008;23:1808-1811.
178 Plaha P, Khan S, Gill SS. Bilateral stimulation of the caudal zona incerta nucleus for tremor control. J Neurol Neurosurg Psychiatry. 2008;79:504-513.
179 Blomstedt P, Fytagoridis A, Tisch S. Deep brain stimulation of the posterior subthalamic area in the treatment of tremor. Acta Neurochir. 2009;151:31-36.
180 Freund HJ, Barnikol UB, Nolte D, et al. Subthalamic-thalamic DBS in a case with spinocerebellar ataxia type 2 and severe tremor—an unusual clinical benefit. Mov Disord. 2007;22:732-735.
181 Leckman JF. Tourette’s syndrome. Lancet. 2002;360:1577-1586.
182 Mink JW, Walkup J, Frey KA, et al. Patient selection and assessment recommendations for deep brain stimulation in Tourette syndrome. Mov Disord. 2006;21:1831-1838.
183 Houeto JL, Karachi C, Mallet L, et al. Tourette’s syndrome and deep brain stimulation. J Neurol Neurosurg Psychiatry. 2005;76:992-995.
184 Maciunas RJ, Maddux BN, Riley DE, et al. Prospective randomized double-blind trial of bilateral thalamic deep brain stimulation in adults with Tourette syndrome. J Neurosurg. 2007;107:1004-1101.
185 American Psychiatric Association; Task Force on DSM-IV, Diagnostic and Statistical Manual of Mental Disorders. DSM-IV-TR, 4th ed. Washington, DC: American Psychiatric Association; 2000.
186 Robertson MM, Banerjee S, Kurlan R, et al. The Tourette Syndrome Diagnostic Confidence Index: development and clinical associations. Neurology. 1999;53:2108-2112.
187 Hassler R, Dieckmann G. Stereotaxic treatment of tics and inarticulate cries or coprolalia considered as motor obsessional phenomena in Gilles de la Tourette’s disease. Rev Neurol. 1970;123:89-100.
188 Vandewalle V, van der Linden C, Groenewegen HJ, et al. Stereotactic treatment of Gilles de la Tourette syndrome by high frequency stimulation of thalamus. Lancet. 1999;353:724.
189 Bajwa RJ, de Lotbinière AJ, King RA, et al. Deep brain stimulation in Tourette’s syndrome. Mov Disord. 2007;22:1346-1350.
190 Servello D, Porta M, Sassi M, et al. Deep brain stimulation in 18 patients with severe Gilles de la Tourette syndrome refractory to treatment: the surgery and stimulation. J Neurol Neurosurg Psychiatry. 2008;79:136-142.
191 Shahed J, Poysky J, Kenney C. GPi deep brain stimulation for Tourette syndrome improves tics and psychiatric comorbidities. Neurology. 2007;68:159-160.
192 Flaherty AW, Williams ZM, Amirnovin R, et al. Deep brain stimulation of the internal capsule for the treatment of Tourette syndrome: technical case report. Neurosurgery. 2005;57(4 Suppl):E403.
193 Kuhn J, Lenartz D, Mai JK, et al. Deep brain stimulation of the nucleus accumbens and the internal capsule in therapeutically refractory Tourette-syndrome. J Neurol. 2007;254:963-965.
194 Adam OR, Jankovic J. Symptomatic treatment of Huntington disease. Neurotherapeutics. 2008;5:181-197.
195 Walker RH, Danek A, Dobson-Stone C, et al. Developments in neuroacanthocytosis: expanding the spectrum of choreatic syndromes. Mov Disord. 2006;21:1794-1805.
196 Huntington Study Group. Unified Huntington’s Disease Rating Scale: reliability and consistency. Mov Disord. 1996;11:136-142.
197 Guy W. Abnormal Involuntary Movement Scale EDCEU Assessment Manual for Psychopharmacology. Washington, DC: U.S. Dept. of Health, Education and Welfare; 1976.
198 Moro E, Lang AE, Strafella AP, et al. Bilateral globus pallidus stimulation for Huntington’s disease. Ann Neurol. 2004;56:290-294.
199 Hebb MO, Garcia R, Gaudet P, et al. Bilateral stimulation of the globus pallidus internus to treat choreoathetosis in Huntington’s disease: technical case report. Neurosurgery. 2006;58:E383.
200 Yianni JJ, Nandi D, Bradley K, et al. Senile chorea treated by deep brain stimulation: a clinical, neurophysiological and functional imaging study. Mov Disord. 2004;19:597-602.
201 Burbaud P, Rougier A, Ferrer X, et al. Improvement of severe trunk spasms by bilateral high-frequency stimulation of the motor thalamus in a patient with chorea-acanthocytosis. Mov Disord. 2002;17:204-207.
202 Wihl G, Volkmann J, Allert N, et al. Deep brain stimulation of the internal pallidum did not improve chorea in a patient with neuro-acanthocytosis. Mov Disord. 2001;16:572-575.
203 Guehl D, Cuny E, Tison F, et al. Deep brain pallidal stimulation for movement disorders in neuroacanthocytosis. Neurology. 2007;68:160-161.