Chapter 67 Pars plana lensectomy for retained intravitreal lens material
Introduction
The most common indication for pars plana lensectomy is crystaline lens or lens fragment dislocation into the vitreous cavity as a complication of cataract extraction1–3. 97% of cataract surgeons in the United States utilize phacoemulsification in cataract surgery, and 74% do not perform planned extracapsular cataract extraction4; thus, complications sustained during phacoemulsification account for the vast majority of retained lens material cases referred to retina surgeons2,5. A comprehensive multicenter study of capsule complications conducted in Sweden demonstrated that previous trauma, white or brunescent cataract, and phacodonesis were significant preoperative risk factors for capsule complications and that loose zonules, use of trypan blue, miosis, and inexperienced surgeons were intraoperative risk factors6. The Swedish used the term capsule complication to include zonular dehiscence, capsule rupture, vitreous loss, and lens remnants lost into the vitreous6. Whereas capsule complications occur in 1–6.1% of all cataract surgeries7,8, retained lens material has been reported to complicate between 0.3% and 1.1% of cataract extractions and occurs more commonly with inexperienced surgeons3,9–13. Other indications for pars plana lensectomy include traumatic cataract, crystalline lens dislocation associated with traumatic injury14, and lens subluxation caused by a variety of systemic conditions including Marfan syndrome, homocystinuria, and PXF syndrome15–17.
Preoperative evaluation
Initial diagnostic examination
The cataract incision should be identified and evaluated for leakage. The intraocular pressure should be assessed, because secondary glaucoma is present in about 50% of patients. Corneal edema may be present as early as the first postoperative day and may result in difficulty visualizing posterior pathology. The application of topical glycerin ophthalmic solution and the reduction of an elevated intraocular pressure may be effective in temporarily reducing corneal edema and facilitating anterior segment and fundus examinations. Anterior chamber inflammation can range from mild cell and flare to a severe fibrinous reaction simulating infectious endophthalmitis18. Slit-lamp biomicroscopy and gonioscopy may identify small lens fragments in the anterior chamber angle19.
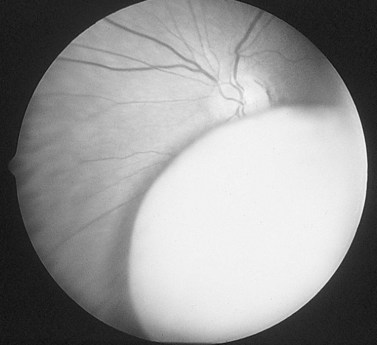
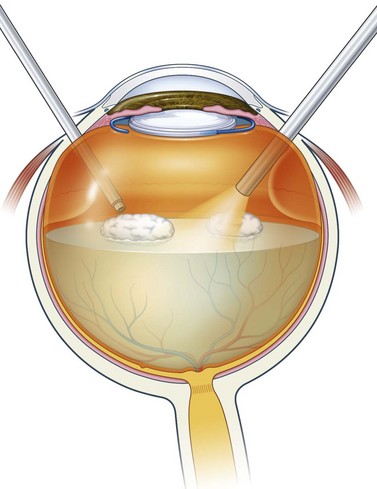
Visualization of the crystaline lens or lens fragments within the vitreous cavity by indirect ophthalmoscopy confirms the diagnosis. Cortical material appears white and fluffy (Fig. 67.1), and nuclear material appears yellowish-brown and has sharper borders, unless it is surrounded by cortex (Fig. 67.2). The examination should include indirect ophthalmoscopic examination of the peripheral retina, specifically looking for retinal tears, retinal detachment, and serous or hemorrhagic choroidal effusions. These complications are more likely to occur if the cataract surgeon has attempted to extract posterior lens fragments by irrigation or insertion of instruments into the posterior vitreous20,21.
Preoperative complications
Corneal edema
Approximately 50% of eyes with retained lens fragments present with corneal edema or corneal decompensation2,5,22–27. This probably results from a combination of surgical trauma, prolonged phacoemulsification times related to the complicated cataract removal, intraocular inflammation, and increased intraocular pressure. Fortunately, the corneal edema is usually transient and resolves with conservative treatment in the majority of affected eyes. Less commonly, retained nuclear fragments sequestered in the anterior chamber may traumatize the corneal endothelium and cause substantial corneal edema and reduced visual acuity, which is reversible following surgical removal of the fragments19. Approximately 3–10% of eyes with retained lens material will develop chronic corneal decompensation and bullous keratopathy that requires penetrating keratoplasty2,12,23.
Uveitis
An inflammatory response to retained lens fragments occurs in 56–87% of eyes with retained lens material2,22,23. Initially, the affected eye may appear quiet, with severe inflammation not developing until weeks later18. Treatment with topical cycloplegic agents and corticosteroids should be instituted preoperatively. Rarely, the uveitis may be so severe that it is clinically confused with infectious endophthalmitis18.
Glaucoma
Secondary glaucoma occurs in approximately 40–50% of eyes with retained lens material2,22–24,26,27. The elevation in intraocular pressure may result from lens fragments, heavy molecular weight soluble lens proteins, and macrophages which obstruct the trabecular meshwork28–30. A steroid-induced elevation in intraocular pressure may be the responsible mechanism in some eyes, creating a confusing clinical picture. Removal of the lens particles usually results in resolution of the secondary glaucoma31. However, as many as one-third of eyes with retained lens fragments treated by vitrectomy and lensectomy demonstrate a persistence of mildly elevated intraocular pressure that requires chronic treatment5.
Retinal detachment
Cataract surgery complicated by vitreous loss is associated with a 5% incidence of retinal detachment at 4 years, which is four to five times greater than the risk following uncomplicated cataract surgery32. In eyes with retained lens fragments, the incidence of retinal detachment is even greater, affecting from 3.8% to 23% of eyes2,12,23,26,33–35. About one-half of the retinal detachments are recognized prior to, or during, vitrectomy and one-half develop postoperatively2,33,34. The development of proliferative vitreoretinopathy may be more common in eyes with retained lens material, requiring the use of silicone oil for repair and limiting the final visual acuity2. Although retinal detachment occurs in the minority of eyes with retained lens material, it is the most common identifiable cause of reduced postoperative visual acuity in several studies22,25,33.
Endophthalmitis
Endophthalmitis may occur concomitantly with retained lens fragments after phacoemulsification23,36. B-scan ultrasonography has proven useful in demonstrating the size and type of retained lens material in eyes with endophthalmitis and opaque media36. Eyes with retained lens fragments and suspected endophthalmitis should be managed with immediate injection of intravitreal antibiotics in conjunction with pars plana vitrectomy and lensectomy or vitreous tap36. The decision of whether or not to perform pars plana lensectomy should be based on the indications for eyes with retained lens material without endophthalmitis. Although 50% of patients with retained lens fragments have been reported to have positive vitreous cultures, routine vitreous cultures are not recommended because they do not identify eyes at risk for endophthalmitis or influence the clinical management37.
Preoperative management
The preoperative management of eyes with retained lens material begins once the surgeon performing the cataract surgery recognizes this complication. After the determination is made that the crystaline lens or lens fragments are posteriorly dislocated into the vitreous cavity, no further attempts should be made to retrieve them. Nuclear fragments remaining in the capsular bag should be phacoemulsified, and residual lens cortex and viscoelastic material should be removed by careful irrigation and aspiration. Anterior vitrectomy may be performed if vitreous has entered the anterior chamber. Attempts to inject fluids or manipulate instruments in the posterior vitreous cavity38 should be avoided because of the risk of inducing retinal tears or detachments and exacerbating the uveitis20,24,39. The preservation of peripheral anterior or posterior lens capsule will allow insertion of a posterior chamber IOL, either at the time of the cataract surgery or at a later date. Placement of a posterior chamber intraocular lens has been shown in multivariate analysis to be associated with better final visual outcomes26. If adequate capsular support is not present, insertion of an anterior chamber intraocular lens may be considered. The cataract wound should be closed with 10-0 nylon sutures even if the wound was constructed to be ‘self-sealing’. Postoperative treatment with frequent topical corticosteroid and cycloplegic drops should be initiated and the patient should be evaluated for retained lens material.
Timing of pars plana lensectomy
Controversy exists regarding the optimal timing for the performance of pars plana lensectomy. Two small series suggested that eyes treated within 3 weeks of lens dislocation had a lower incidence of postoperative glaucoma1,5. However, larger and more recent series did not find a statistically significant difference in visual outcomes between eyes treated with early and with late pars plana lensectomy2,22,23,26,33,40. Because pars plana lensectomy has been shown to result in resolution of secondary ocular hypertension and uveitis, it should not be delayed in eyes that have adequate corneal clarity and fulfill the criteria for early pars plana lensectomy31. In some cases, corneal edema will prevent surgery because of its deleterious effects on visualization. In these cases, aggressive treatment of elevated intraocular pressure and uveitis will usually allow the edema to resolve sufficiently to permit safe vitreoretinal surgery.
Operative technique
Pars plana lensectomy
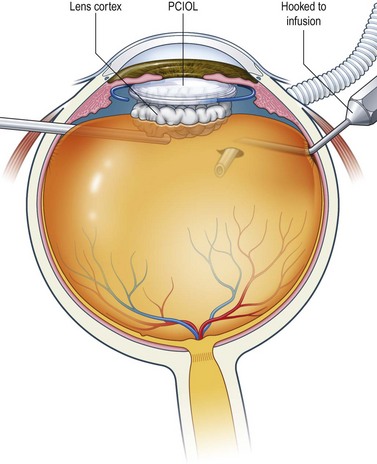
If lens material in the pupillary axis prevents visualization of the infusion cannula, a bent 21-gauge needle attached to an infusion bottle can be introduced through one of the superior sclerotomy sites and the vitreous cutter through the other site (Fig. 67.3). The infusion may be opened only after the lens material has been cleared from the visual axis, and the infusion cannula is directly visualized within the vitreous cavity.
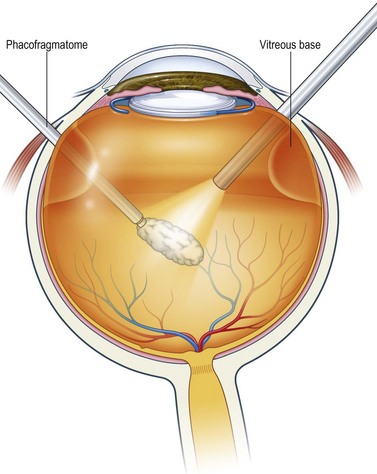
Next, vitreous debris and cortical lens material are cleared from the vitreous cavity with a standard vitrectomy cutter (Fig. 67.4). The vitreous base is trimmed peripherally and the retained lens material is freed from all vitreous attachments. Smaller or softer pieces of nucleus may be removed using the vitreous cutter alone, or by using the light pipe to crush the lens material into smaller pieces and force them into the cutting port.
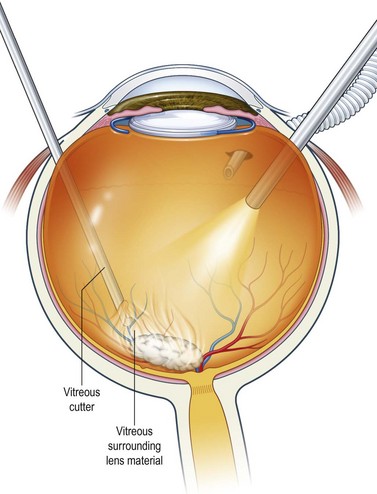
Fig. 67.4 The retained lens material is freed of all vitreous adhesions using the vitrectomy cutter.
Larger or harder pieces of nucleus require the use of a phacofragmatome, a 20-gauge ultrasound needle capable of phacoemulsifying the lens material. After the phacofragmatome is introduced into the vitreous cavity, aspiration is used to engage the lens material and to elevate it into the mid-vitreous cavity; only then is phacoemulsification power applied (Fig. 67.5). Ultrasound fragmentation has been shown in one study to be associated with worse visual outcomes41, but larger and more recent studies have shown that fragmentation is not associated with worse outcomes1,23,26,40.
Occasionally, hard nuclei may be difficult to phacoemulsify using the phacofragmatome alone. If the lens particle is repeatedly ejected from the tip of the phacofragmatome, several techniques may be utilized. Lowering the ultrasound power to 5–10% of the maximum power, increasing the vacuum, or using the pulse mode option on the phacofragmatome settings, may aid in keeping the lens material engaged. A bimanual technique that utilizes the light pipe or lighted pick to stabilize the nucleus in the mid-vitreous cavity is also effective42. One potential complication with the use of a lighted pick is the possibility of retained metal shavings if the pick and phacofragmatome come into contact during lens removal42.
Adjunctive perfluorocarbon liquids
Perfluorocarbon liquids may facilitate the safe removal of retained lens material in four ways. First, they provide protection from contusion injuries of the macula caused by lens particles that fall posteriorly or are projected from the tip of the phacofragmatome during emulsification43,44. Second, the relative buoyancy of lens material compared with perfluorocarbon liquid causes the lens material to float on the surface, reducing the risk of retinal damage during manipulation and engagement of the particles45. Third, perfluorocarbon liquids form a protective layer over the posterior pole, which may reduce the risk of damage to the retinal pigment epithelium and neurosensory retina resulting from the ultrasonic stream of the phacofragmatome46. Lastly, perfluorocarbon liquids are useful when a retinal detachment occurs concomitantly with retained lens material43. The decreased mobility of the retina afforded by the perfluorocarbon liquid bubble reduces the risk of inadvertent retinal injury, floats the lens material above the retinal surface, and aids in repair of the retinal detachment. The use of perfluorocarbon liquids has not been shown to be associated with better or worse visual outcomes26,33.
Enough perfluorocarbon liquid should be instilled into the eye to extend just outside the arcades (Fig. 67.6). Overfill can complicate the removal of lens material because the meniscus of the bubble tends to cause displacement of the lens fragments toward the retinal periphery and vitreous base. Attempts to remove particles that have become trapped in the vitreous base may cause retinal tears or dialyses.
Alternative techniques
Other techniques have been described for use in the management of extremely hard nuclear lens fragments. They involve mobilizing the retained lens fragments, either into the anterior chamber with delivery through a limbal incision, or into the posterior chamber with delivery through a pars plana incision47,48. Both of these techniques require large incisions in either the limbus or pars plana, and the former technique risks corneal endothelial injury. With the development of increasingly better phacofragmentation instruments, the techniques of corneal limbal extraction and phacohydroexpulsion have been largely abandoned.
Intraocular lens management
If an IOL was inserted at the time of cataract surgery, it may require intraoperative repositioning49. If an anterior or posterior chamber lens was not inserted at the time of cataract surgery, consideration should be given to placement of an IOL at the time of pars plana lensectomy. Placement of an IOL at this time is beneficial because it negates the need for additional surgery and, because it is inserted following the pars plana lensectomy, it does not interfere with the removal of the retained lens material. However, if there is significant corneal edema, choroidal detachment or hemorrhage, or lack of capsular support with a contraindication to anterior chamber lens placement, then IOL placement should be deferred. If inadequate capsular support is present, and insertion of an anterior chamber intraocular lens is not desirable, a sutured posterior chamber intraocular lens may be considered50. There is evidence to suggest that posterior chamber lenses may result in a higher rate of 20/40 or better visual acuity than anterior chamber lenses22,23,50.
Additional measures
Some authors including Ho et al. recommend the routine use of subconjunctival steroid placement at the end of surgery26.
Intraoperative complications
A retinal detachment, tear, or dialysis discovered at the time of pars plana lensectomy should be repaired using the standard operative techniques discussed in Chapter 58. Intraocular gas tamponade, required for repair of select retinal detachments, may result in secondary dislocation of a recently inserted sulcus-fixated posterior chamber intraocular lens.
Postoperative complications
Corneal edema
Corneal decompensation may be worsened as a result of vitrectomy and lensectomy. This further surgical insult to an already traumatized eye can exacerbate corneal edema. Medical management and watchful waiting will usually result in resolution of the edema; however, corneal edema persists in 3–10% of eyes with retained lens material2,12,23.
Retinal detachment
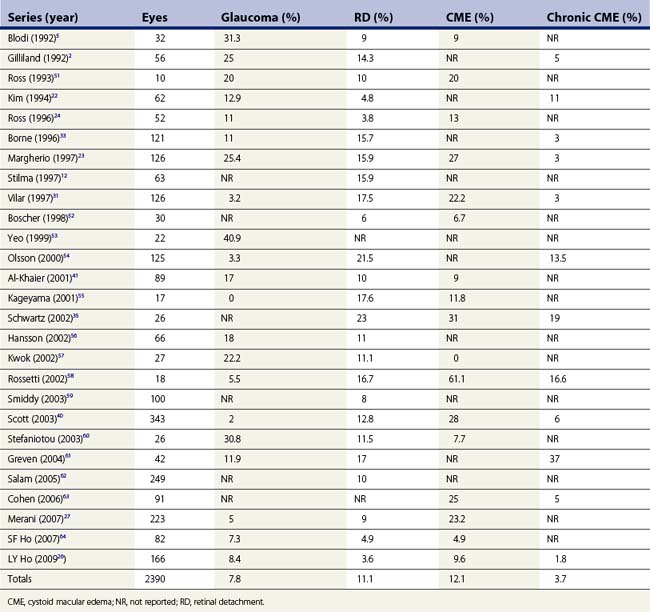
As discussed previously, retinal detachment occurs in 3.6% to 23% (Table 67.1) of eyes with retained lens fragments and 50% of the detachments occur after vitrectomy2,12,23,33,34,40. Proliferative vitreoretinopathy also develops more commonly with retinal detachments that occur in the postvitrectomy period1,2,5,65.
Cystoid macular edema
In the larger series that are published, postoperative cystoid macular edema (CME) occurs in 9.6–28% of eyes following vitrectomy and lensectomy26,33,40,66. However, it is difficult to determine if the CME is a consequence of the complicated cataract surgery, is related to the vitrectomy and lensectomy, or is due to perioperative complications such as retinal detachment or persistent uveitis. Vitrectomy is effective in reducing the inflammatory response and may secondarily reduce the incidence of postoperative CME in otherwise uncomplicated cases12,23. In eyes that require repair of a retinal detachment, CME may result in a further decrease in visual acuity2,33. Chronic CME has been reported in the larger series at a rate of 1.8–13.5%26,54 and, in the largest studied series of 343 eyes, Scott et al. reported that it was the most common cause of decreased final vision40.
Glaucoma
Secondary glaucoma usually resolves promptly following removal of the retained lens material31. If the intraocular pressure continues to rise following vitrectomy and lensectomy, the possibility of steroid-induced glaucoma should be considered. As many as one-third of eyes will develop a chronic elevation of intraocular pressure requiring medical treatment5.
Prognosis
Pars plana vitrectomy and lensectomy have proven to be effective in restoring vision for eyes with retained lens material. Between 44% and 72.3% of patients will obtain 20/40 or better acuity following pars plana lensectomy for retained lens fragments2,22,23,26,33,41. Improved surgical techniques, such as 23-gauge instrumentation, a lower threshold to intervene, and a heightened awareness by surgeons of potential complications and management options, have improved the safety and visual outcome of this procedure.
1 Fastenberg DM, Schwartz PL, Shakin JL, et al. Management of dislocated nuclear fragments after phacoemulsification. Am J Ophthalmol. 1991;112(5):535-539.
2 Gilliland GD, Hutton WL, Fuller DG. Retained intravitreal lens fragments after cataract surgery. Ophthalmology. 1992;99(8):1263-1267. discussion 8–9
3 Pande M, Dabbs TR. Incidence of lens matter dislocation during phacoemulsification. J Cataract Refract Surg. 1996;22(6):737-742.
4 Leaming DV. Practice styles and preferences of ASCRS members – 2003 survey. J Cataract Refract Surg. 2004;30(4):892-900.
5 Blodi BA, Flynn HWJr, Blodi CF, et al. Retained nuclei after cataract surgery [see comments]. Ophthalmology. 1992;99(1):41-44.
6 Artzén D, Lundstrôm M, Behndig A, et al. Capsule complication during cataract surgery: Case–control study of preoperative and intraoperative risk factors: Swedish Capsule Rupture Study Group report 2. J Cataract Refract Surg. 2009;35(10):1688-1693.
7 Narendran N. The Cataract National Dataset electronic multicentre audit of 55,567 operations: risk stratification for posterior capsule rupture and vitreous loss. Eye (London). 2009;23(1):31-37.
8 Norregaard JC, Bernth-Petersen P, Bellan L, et al. Intraoperative clinical practice and risk of early complications after cataract extraction in the United States, Canada, Denmark, and Spain. Ophthalmology. 1999;106(1):42-48.
9 Cotlier E, Rose M. Cataract extraction by the intracapsular methods and by phacoemulsification: the results of surgeons in training. Trans Am Acad Ophthalmol Otolaryngol. 1976;81(1):OP163-OP182.
10 Fung WE. Phacoemulsification. Ophthalmology. 1978;85(1):46-51.
11 Hurite FG. Symposium: Phacoemulsification. The contraindications to phacoemulsification and summary of personal experience. Trans Am Acad Ophthalmol Otolaryngol. 1974;78(1):OP14-OP17.
12 Stilma JS, van der Sluijs FA, van Meurs JC, et al. Occurrence of retained lens fragments after phacoemulsification in The Netherlands. J Cataract Refract Surg. 1997;23(8):1177-1182.
13 Leaming DV. Practice styles and preferences of ASCRS members –1994 survey. J Cataract Refract Surg. 1995;21(4):378-385.
14 Marcus DM, Topping TM, Frederick ARJr. Vitreoretinal management of traumatic dislocation of the crystalline lens. Internat Ophthalmol Clin. 1995;35(1):139-150.
15 Gerding H. Ocular complications and a new surgical approach to lens dislocation in homocystinuria due to cystathionine-beta-synthetase deficiency. Eur J Pediatr. 1998;157(Suppl 2):S94-101.
16 Hakin KN, Jacobs M, Rosen P, et al. Management of the subluxed crystalline lens. Ophthalmology. 1992;99(4):542-545.
17 Koenig SB, Mieler WF. Management of ectopia lentis in a family with Marfan syndrome [see comments]. Arch Ophthalmol. 1996;114(9):1058-1061.
18 Irvine WD, Flynn HWJr, Murray TG, et al. Retained lens fragments after phacoemulsification manifesting as marked intraocular inflammation with hypopyon. Am J Ophthalmol. 1992;114(5):610-614.
19 Bohigian GM, Wexler SA. Complications of retained nuclear fragments in the anterior chamber after phacoemulsification with posterior chamber lens implant. Am J Ophthalmol. 1997;123(4):546-547.
20 Aaberg TMJr, Rubsamen PE, Flynn HWJr, et al. Giant retinal tear as a complication of attempted removal of intravitreal lens fragments during cataract surgery. Am J Ophthalmol. 1997;124(2):222-226.
21 Terasaki H, Miyake Y, Miyake K. Visual outcome after management of a posteriorly dislocated lens nucleus during phacoemulsification. J Cataract Refract Surg. 1997;23(9):1399-1403.
22 Kim JE, Flynn HWJr, Smiddy WE, et al. Retained lens fragments after phacoemulsification [see comments]. Ophthalmology. 1994;101(11):1827-1832.
23 Margherio RR, Margherio AR, Pendergast SD, et al. Vitrectomy for retained lens fragments after phacoemulsification. Ophthalmology. 1997;104(9):1426-1432.
24 Ross WH. Management of dislocated lens fragments after phacoemulsification surgery. Can J Ophthalmol. 1996;31(5):234-240.
25 Tommila P, Immonen I. Dislocated nuclear fragments after cataract surgery. Eye. 1995;9(Pt 4):437-441.
26 Ho LY, Doft BH, Wang L, et al. Clinical predictors and outcomes of pars plana vitrectomy for retained lens material after cataract extraction. Am J Ophthalmol. 2009;147(4):587-594.e1.
27 Merani R, Hunyor AP, Playfair TJ, et al. Pars plana vitrectomy for the management of retained lens material after cataract surgery. Am J Ophthalmol. 2007;144(3):364-370.
28 Epstein DL. Diagnosis and management of lens-induced glaucoma. Ophthalmology. 1982;89(3):227-230.
29 Epstein DL, Jedziniak JA, Grant WM. Obstruction of aqueous outflow by lens particles and by heavy-molecular-weight soluble lens proteins. Invest Ophthalmol Visual Sci. 1978;17(3):272-277.
30 Filipe JC, Palmares J, Delgado L, et al. Phacolytic glaucoma and lens-induced uveitis. Internat Ophthalmol. 1993;17(5):289-293.
31 Vilar NF, Flynn HWJr, Smiddy WE, et al. Removal of retained lens fragments after phacoemulsification reverses secondary glaucoma and restores visual acuity. Ophthalmology. 1997;104(5):787-791. discussion 91–2
32 Javitt JC, Vitale S, Canner JK, et al. National outcomes of cataract extraction. I. Retinal detachment after inpatient surgery. Ophthalmology. 1991;98(6):895-902.
33 Borne MJ, Tasman W, Regillo C, et al. Outcomes of vitrectomy for retained lens fragments. Ophthalmology. 1996;103(6):971-976.
34 Smiddy WE, Flynn HWJr, Kim JE. Retinal detachment in patients with retained lens fragments or dislocated posterior chamber intraocular lenses. Ophthal Surg Lasers. 1996;27(10):856-861.
35 Schwartz SG. Retained lens fragments in resident-performed cataract extractions. The CLAO journal: official publication of the Contact Lens Association of Ophthalmologists Inc. 2002;28(1):44-47.
36 Kim JE, Flynn HWJr, Rubsamen PE, et al. Endophthalmitis in patients with retained lens fragments after phacoemulsification. Ophthalmology. 1996;103(4):575-578.
37 Joondeph BC, Myint S, Joondeph HC. Positive vitreous cultures in eyes with retained lens fragments. Retina. 1999;19(4):354-355.
38 Weinstein GW, Charlton JF, Esmer E. The ‘lost lens’: a new surgical technique using the Machemer lens. Ophthal Surg. 1995;26(2):156-159.
39 Monshizadeh R, Samiy N, Haimovici R. Management of retained intravitreal lens fragments after cataract surgery. Surv Ophthalmol. 1999;43(5):397-404.
40 Scott IU, Flynn HW, Smiddy WE, et al. Clinical features and outcomes of pars plana vitrectomy in patients with retained lens fragments. Ophthalmology. 2003;110(8):1567-1572.
41 Al-Khaier A, Wong D, Lois N, et al. Determinants of visual outcome after pars plana vitrectomy for posteriorly dislocated lens fragments in phacoemulsification. J Cataract Refract Surg. 2001;27(8):1199-1206.
42 You TT, Arroyo JG. Surgical approaches for the removal of posteriorly dislocated crystalline lenses. Internat Ophthalmol Clin. 1999;39(1):249-259.
43 Lewis H, Blumenkranz MS, Chang S. Treatment of dislocated crystalline lens and retinal detachment with perfluorocarbon liquids [see comments]. Retina. 1992;12(4):299-304.
44 Wallace RT, McNamara JA, Brown G, et al. The use of perfluorophenanthrene in the removal of intravitreal lens fragments. Am J Ophthalmol. 1993;116(2):196-200.
45 Greve MD, Peyman GA, Mehta NJ, et al. Use of perfluoroperhydrophenanthrene in the management of posteriorly dislocated crystalline and intraocular lenses. Ophthal Surg. 1993;24(9):593-597.
46 Movshovich A, Berrocal M, Chang S. The protective properties of liquid perfluorocarbons in phacofragmentation of dislocated lenses. Retina. 1994;14(5):457-462.
47 Shapiro MJ, Resnick KI, Kim SH, et al. Management of the dislocated crystalline lens with a perfluorocarbon liquid. Am J Ophthalmol. 1991;112(4):401-405.
48 Fuller D, Jost B. Phacohydroexpulsion: A new technique for removal of luxated sclerotic lens nuclei. Vitreoretinal Surg Tech. 1989;4:3. 6,8
49 Campo RV, Chung KD, Oyakawa RT. Pars plana vitrectomy in the management of dislocated posterior chamber lenses [see comments]. Am J Ophthalmol. 1989;108(5):529-534.
50 Omulecki W, Nawrocki J, Sempinska-Szewczyk J, et al. Transscleral suture fixation and anterior chamber intraocular lenses implanted after removal of posteriorly dislocated crystalline lenses. Eur J Ophthalmol. 1997;7(4):370-374.
51 Ross WH. Management of dislocated lens fragments following phacoemulsification surgery. Canadian journal of ophthalmology. J Can Ophtalmol. 1993;28(4):163-166.
52 Boscher C, Lebuisson DA, Lean JS, et al. Vitrectomy with endoscopy for management of retained lens fragments and/or posteriorly dislocated intraocular lens. Graefes Arch Clin Exp Ophthalmol. 1998;236(2):115-121.
53 Yeo LM, Charteris DG, Bunce C, et al. Retained intravitreal lens fragments after phacoemulsification: a clinicopathological correlation. Br J Ophthalmol. 1999;83(10):1135-1138.
54 Olsson RB, Ritland JS, Bjørnsson OM, et al. A retrospective study of patients with retained nuclear fragments after cataract extraction. Acta Ophthalmol Scand. 2000;78(6):677-679.
55 Kageyama T, Ayaki M, Ogasawara M, et al. Results of vitrectomy performed at the time of phacoemulsification complicated by intravitreal lens fragments. Br J Ophthalmol. 2001;85(9):1038-1040.
56 Hansson LJ, Larsson J. Vitrectomy for retained lens fragments in the vitreous after phacoemulsification. J Cataract Refract Surg. 2002;28(6):1007-1011.
57 Kwok AKH, Li KKW, Lai TYY, et al. Pars plana vitrectomy in the management of retained intravitreal lens fragments after cataract surgery. Clin Exp Ophthalmol. 2002;30(6):399-403.
58 Rossetti A, Doro D. Retained intravitreal lens fragments after phacoemulsification: complications and visual outcome in vitrectomized and nonvitrectomized eyes. J Cataract Refract Surg. 2002;28(2):310-315.
59 Smiddy WE, Guererro JL, Pinto R, et al. Retinal detachment rate after vitrectomy for retained lens material after phacoemulsification. Am J Ophthalmol. 2003;135(2):183-187.
60 Stefaniotou M, Aspiotis M, Pappa C, et al. Timing of dislocated nuclear fragment management after cataract surgery. J Cataract Refract Surg. 2003;29(10):1985-1988.
61 Greven CM, Piccione K. Delayed visual loss after pars plana vitrectomy for retained lens fragments. Retina (Philadelphia, Pa). 2004;24(3):363-367.
62 Salam GA, Greene JM, Deramo VA, et al. Retinal tears and retinal detachment as factors affecting visual outcome after cataract extraction complicated by posteriorly dislocated lens material. Retina (Philadelphia, Pa). 2005;25(5):570-575.
63 Cohen SM, Davis A, Cukrowski C. Cystoid macular edema after pars plana vitrectomy for retained lens fragments. J Cataract Refract Surg. 2006;32(9):1521-1526.
64 Ho SF, Zaman A. Clinical features and outcomes of pars plana vitrectomy in patients with retained lens fragments after phacoemulsification. J Cataract Refract Surg. 2007;33(12):2106-2110.
65 Hutton WL, Snyder WB, Vaiser A. Management of surgically dislocated intravitreal lens fragments by pars plana vitrectomy. Ophthalmology. 1978;85(2):176-189.
66 Kapusta MA, Chen JC, Lam WC. Outcomes of dropped nucleus during phacoemulsification. Ophthalmology. 1996;103(8):1184-1187.