83
Panniculitis
Introduction
• Panniculitis = inflammation of adipose tissue.
• There are various etiologies, and a clinical classification system is presented in Table 83.1.
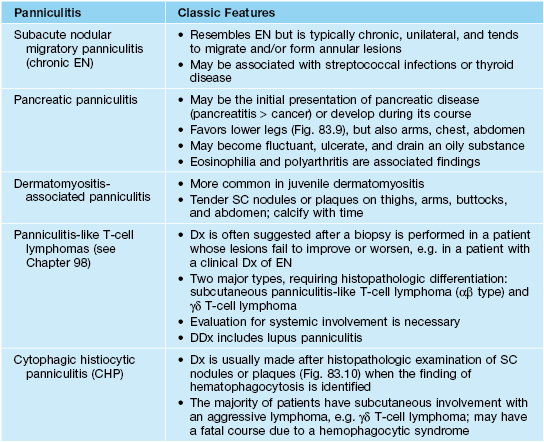
Table 83.1
Clinical classification of the panniculitides.
* The majority represent an underlying subcutaneous lymphoma.
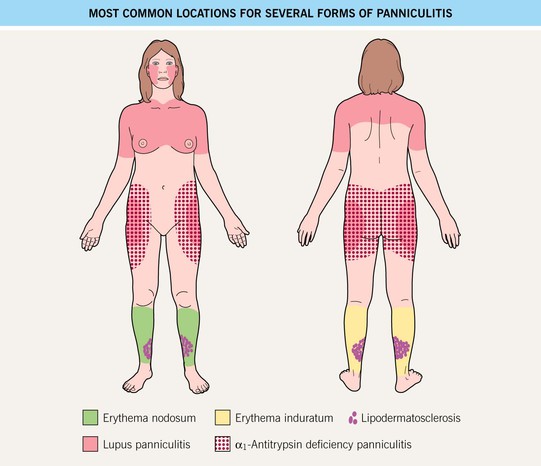
• Diagnosis is challenging and involves consideration of (1) patient characteristics such as age, immune status, underlying diseases; (2) location of the lesions (Fig. 83.1); (3) the presence or absence of ulceration and/or drainage; and (4) histopathological findings.
• Once the diagnosis of panniculitis is made, further evaluation for underlying etiology or associated conditions is necessary (Tables 83.2–83.4).
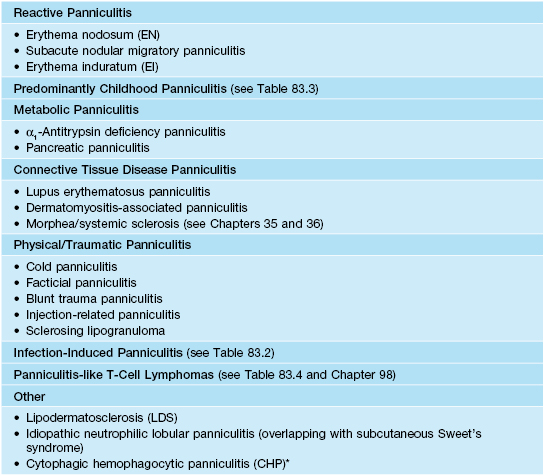
Table 83.2
The more common panniculitides.
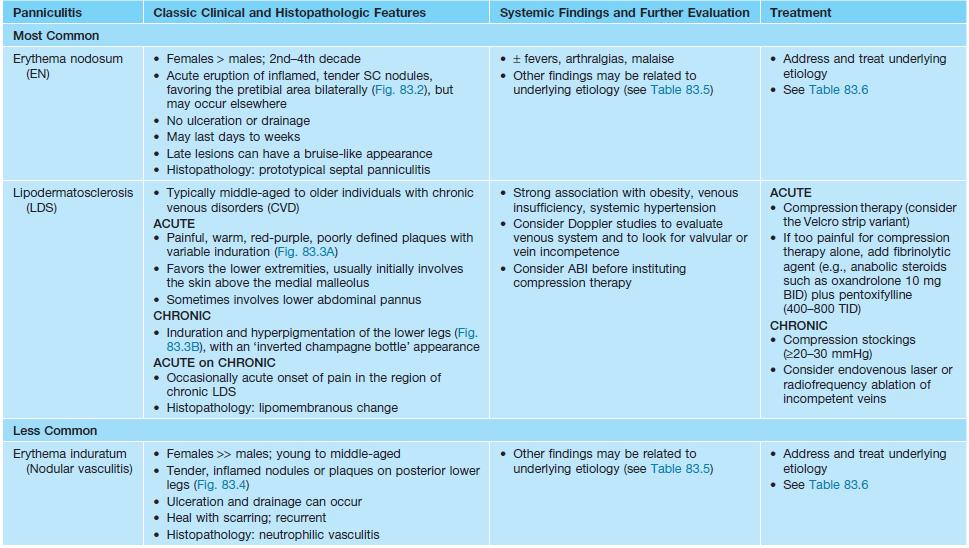
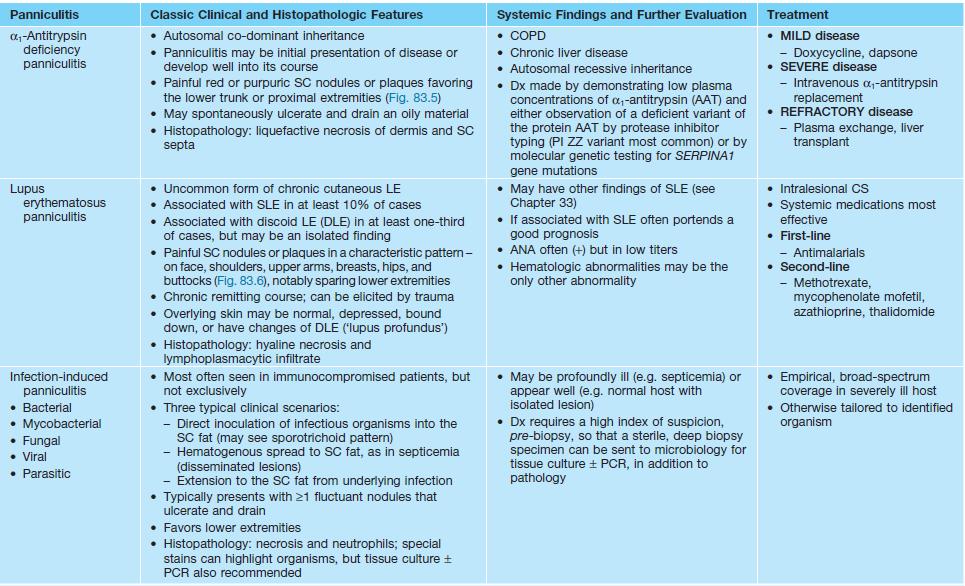
SC, subcutaneous; ABI, ankle brachial index; COPD, chronic obstructive pulmonary disease; ANA, antinuclear antibody; BID, twice daily; TID, three times a day.
Table 83.3
Predominantly childhood panniculitides.
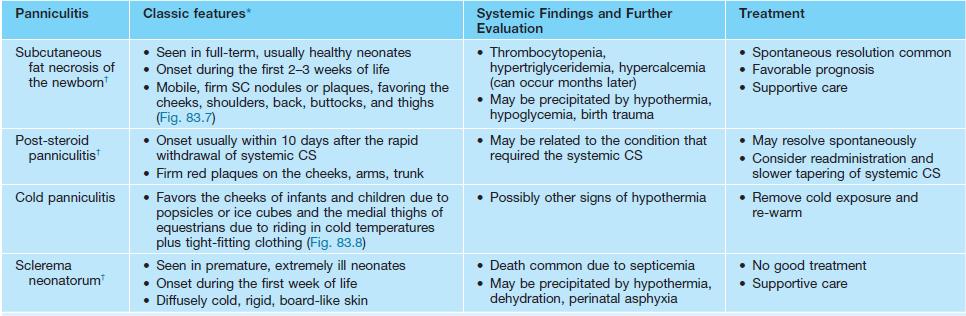
* All entities, except for cold panniculitis, will demonstrate needle-shaped clefts on histopathology.
† Seen exclusively in infants or children.
SC, subcutaneous.
Table 83.5
Causes of erythema nodosum and erythema induratum and suggested evaluations.
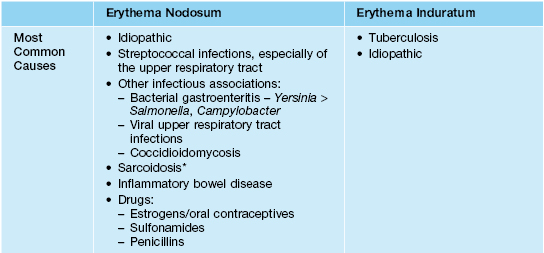
* Lofgren’s syndrome is an acute, spontaneously resolving form of sarcoidosis characterized by erythema nodosum, fever, hilar lymphadenopathy, polyarthritis, and uveitis.
† Erythema nodosum secondary to hepatitis B vaccine has also been reported.
** Basic workup in patients with erythema nodosum and erythema induratum with no obvious etiology.
WBC, white blood cell count; GI, gastrointestinal; RA, rheumatoid arthritis; TSH, thyroid-stimulating hormone; CBC, complete blood count; ESR, erythrocyte sedimentation rate; IGRA, interferon-γ release assay.
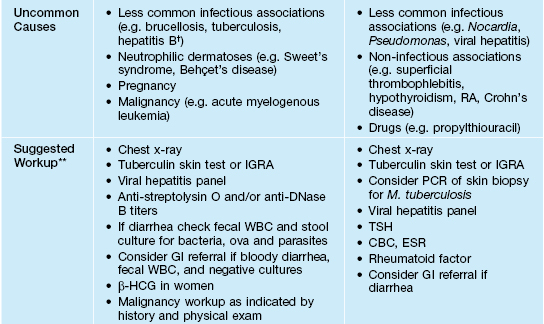
Table 83.6
Treatment recommendations for erythema nodosum and erythema induratum.
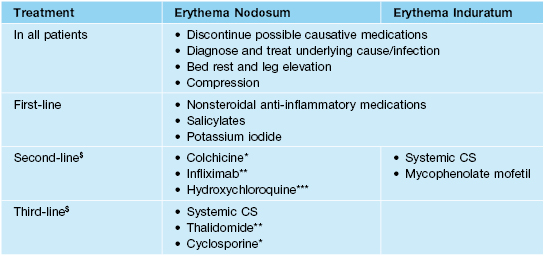
* Helpful for erythema nodosum occurring in the setting of Behçet’s disease.
** Helpful for erythema nodosum occurring in the setting of inflammatory bowel disease.
*** Helpful for chronic erythema nodosum.
$ Immunosuppressives to be used only if underlying infection has been excluded and/or treated.

Fig. 83.2 Erythema nodosum. Erythematous, tender nodules located bilaterally on the shins. Courtesy, Kenneth E. Greer, MD.


Fig. 83.3 Lipodermatosclerosis. A Acute phase with tender erythematous plaques on both lower extremities. This condition is often misdiagnosed as ‘bilateral recurrent cellulitis.’ B Chronic phase with sclerotic red-brown plaque on the lower medial leg. A, Courtesy, James Patterson, MD; B, Courtesy, Kenneth E. Greer, MD.

Fig. 83.4 Erythema induratum. Nodular lesions on the lower leg, with evidence of ulceration. Courtesy, Kenneth E. Greer, MD.

Fig. 83.5 α1-Antitrypsin deficiency panniculitis. Purpuric nodules on the ankles. Courtesy, Kenneth E. Greer, MD.


Fig. 83.6 Lupus panniculitis. A Erythematous plaque involving the orbital area. B Red-brown plaques on the upper outer arm. Note the significant subcutaneous atrophy and overlying lesions of discoid lupus erythematosus. A, Courtesy, James Patterson, MD; B, Courtesy, Kenneth E. Greer, MD.

Fig. 83.8 Cold panniculitis. Erythematous to violaceous plaques on the thighs of a young woman with equestrian cold panniculitis. Courtesy, Kenneth E. Greer, MD.

Fig. 83.10 Cytophagic histiocytic panniculitis. Subcutaneous nodules with purpura. The majority of these patients have an underlying subcutaneous lymphoma. Courtesy, Kenneth E. Greer, MD.
• Rx: involves specific treatment of the panniculitis and often treatment of an underlying disorder (see Tables 83.2–83.4).
For further information see Ch. 100. From Dermatology, Third Edition.