87
Other Vascular Disorders
This chapter covers a range of vascular disorders from livedo reticularis to common vascular ectasias such as venous lakes and telangiectasias. Additional disorders characterized by proliferation of blood vessels are covered in Chapters 85 (infantile hemangiomas and vascular malformations) and 94 (vascular neoplasms).
Livedo Reticularis
• Blue-violet netlike pattern that reflects an increase in deoxygenated blood within the venous plexus of the skin (Fig. 87.1); this increase can be due to a number of causes, including vasospasm of arterioles supplying the skin and sluggish flow due to hypercoagulability or luminal pathology.
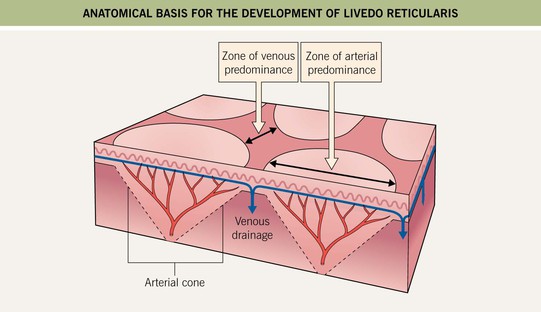
Fig. 87.1 Anatomic basis for the development of livedo reticularis. At the edges of arterial cones, the venous plexus is prominent. An increase in deoxygenated blood within this plexus (due to a decrease in blood flow into or through the skin or impeded drainage of blood) leads to livedo reticularis. If disease of the feeding arteriole is suspected, a wedge biopsy of the central cone can be performed.
• A common physiologic vasospastic response to cold that resolves with rewarming, as well as a sign of a number of systemic diseases, from severe atherosclerosis to systemic lupus erythematosus (Table 87.1; Fig. 87.2).
Table 87.1
Causes of livedo reticularis.
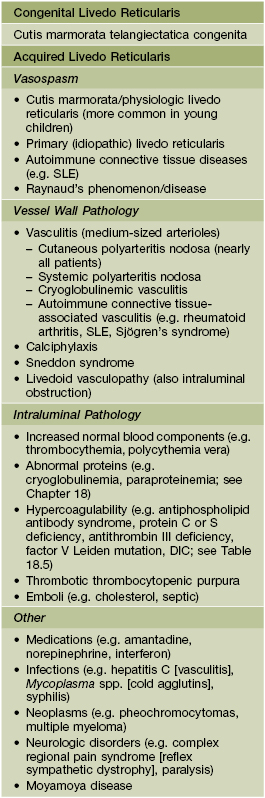
DIC, disseminated intravascular coagulation; SLE, systemic lupus erythematosus.



Fig. 87.2 Livedo reticularis. A An even, netlike pattern is seen on the thigh in physiologic livedo reticularis. B In primary (idiopathic) livedo reticularis, the pattern persists with rewarming. C Livedo reticularis in a patient with SLE. A, B, Courtesy, Christopher Baker, MD, and Robert Kelly, MD; C, Courtesy, Jeffrey Callen, MD.
• DDx: early phase of erythema ab igne; viral exanthems (e.g. erythema infectiosum), retiform purpura and necrosis due to more complete disruption of blood flow (Fig. 87.3; see Chapter 18); underlying etiologies are outlined in Table 87.1.
Flushing
• Common etiologies are menopause, other causes of estrogen deficiency (e.g. tamoxifen), rosacea, and medications (e.g. nicotinic acid, nitrates); uncommon causes are carcinoid syndrome, mastocytosis, and pheochromocytoma (Table 87.2).
Table 87.2
Causes of flushing.
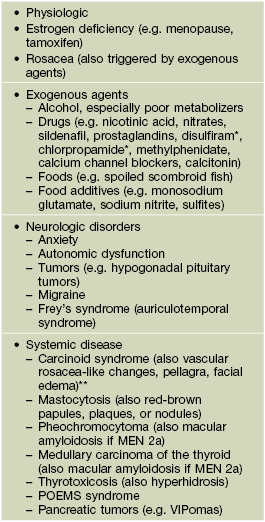
* With alcohol intake.
** Midgut tumors with liver metastases, type III gastric tumors, and bronchial tumors.
POEMS, polyneuropathy, organomegaly, endocrinopathy, M-protein (monoclonal gammopathy), skin changes; VIP, vasoactive intestinal polypeptide.
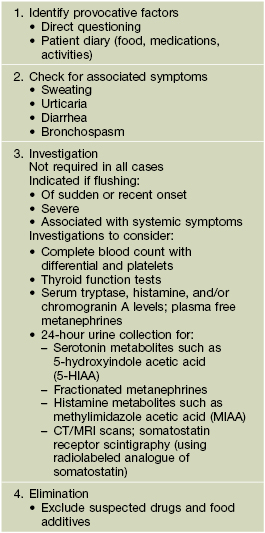
• Sites of involvement, primarily the face > ears, neck, and chest, are both visible and characterized by greater vasculature capacitance; an approach to the evaluation of a patient with flushing is outlined in Table 87.3.
Erythromelalgia
• Erythema, warmth, and painful burning sensation of the distal extremities (lower > upper) that is usually episodic but may be constant (Fig. 87.4); relieved by cooling and precipitated by warming, with attacks often beginning in the evening.
Telangiectasias
• Permanently dilated superficial cutaneous blood vessels; fine (diameter 0.1–1mm), red to blue-violet in color, and usually fade with pressure (Fig. 87.5).




Fig. 87.5 Telangiectasias. A Sun-induced telangiectasias on the cheek. B Prominent telangiectasias on the breast following radiation therapy. Note the overall rectangular configuration. C Fine blue-violet telangiectasias of the leg. D Venulectasias of the leg, which have a larger diameter (1–2 mm). The latter are a reflection of venous hypertension. A, B, Courtesy, Christopher Baker, MD, and Robert Kelly, MD. C, D, Courtesy, Jean L. Bolognia, MD.
• Although most commonly seen on the face and on the lower extremities in the settings of photodamage and venous hypertension, respectively, telangiectasias are associated with a number of conditions (Table 87.4) and have several variants (see later).
Table 87.4
Causes of telangiectasias.
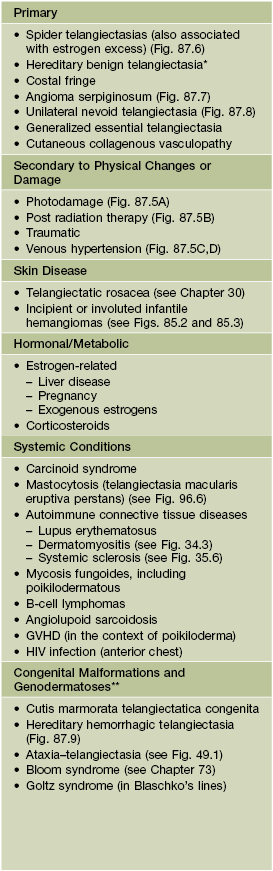
* Childhood onset of multiple punctate, linear, or arborizing telangiectasias favoring the sun-exposed areas of the face and upper extremities; the vermilion lips and palate are occasionally affected, but there is no visceral involvement.
** Not exhaustive list.
• Rx: fine wire diathermy, injection sclerotherapy (legs), laser or intense pulsed light therapy.
Spider Telangiectasia (Spider Angioma)
• Characterized by a red papule with multiple radiating fine vessels (‘legs’); the papular component is the site of the feeding arteriole; usually present as isolated lesions in children but are often multiple when associated with hyperestrogenemia, e.g. in the setting of pregnancy or hepatic cirrhosis in men.
• Usually develop in otherwise healthy women and children, with the most common locations being the face, neck, chest, and hands (Fig. 87.6).


Fig. 87.6 Spider telangiectasias. A Central red papule representing the feeding arteriole with radiating telangiectatic ‘legs’ on the cheek of a young child. B Multiple lesions in a jaundiced patient with liver disease. A, Courtesy, Phillip Bekhor, MD; B, Courtesy, Ronald Rapini, MD.

Fig. 87.7 Angioma serpiginosum. Clusters of dark red puncta on the arm in a serpiginous pattern. This disorder initially favors a single extremity, usually in a girl, and may be confused with a pigmented purpuric eruption.
Generalized Essential Telangiectasia
Hereditary Hemorrhagic Telangiectasia (Osler–Weber–Rendu Disease)
• The vascular lesions are actually arteriovenous malformations and are found in the skin, mucous membranes, GI tract, CNS, and other visceral organs (e.g. lung, liver); the disorder most often initially presents as recurrent epistaxis due to involvement of the nasal mucosa, with hemorrhage at other sites usually occurring later in life.
• The oral mucosal lesions (tongue, lips) usually appear during adolescence and predate the cutaneous ‘telangiectasias’ (face, hands); there is an increase in the overall number of lesions with time (Fig. 87.9).


Fig. 87.9 Hereditary hemorrhagic telangiectasia (Osler–Weber–Rendu disease). The majority of lesions are papular, but occasionally they resemble the mat telangiectasias observed in systemic sclerosis. Courtesy, Irwin Braverman, MD.
• Evaluation is outlined in Table 87.5.
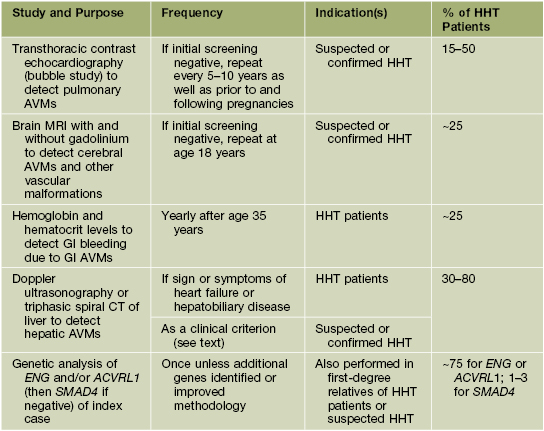
Table 87.5
Studies recommended to screen for systemic involvement and assist in the diagnosis of hereditary hemorrhagic telangiectasia (HHT).
Venous Lake
• A blue, soft papule that is compressible and, with pressure, both its color and elevation are diminished (Fig. 87.10); represents dilation of superficial blood vessels.

Fig. 87.10 Venous lake on the vermilion lip. This dark blue papule is soft and, with compression, can be emptied of most of its blood content. Courtesy, Ronald Rapini, MD.
Angiokeratomas
• Most commonly occur as multiple lesions on the scrotum or vulva (Fig. 87. 11) or as an isolated lesion on the lower extremity (Fig. 87.12).

Fig. 87.11 Angiokeratomas of the scrotum. These lesions typically arise along superficial vessels, and similar lesions are seen on the vulva in women. Courtesy, Christopher Baker, MD, and Robert Kelly, MD.

Fig. 87.12 Solitary angiokeratoma. Because of its dark color, this lesion may resemble cutaneous melanoma. Dermoscopy will readily distinguish between these two entities. Courtesy, Jean L. Bolognia, MD.
• Occasionally, angiokeratomas are grouped (circumscriptum and Mibelli forms) or rarely more widely distributed (diffusum form), especially within the girdle area; the latter form is a cutaneous manifestation of several lysosomal storage disorders (e.g. Fabry disease) (see Chapter 52).
Nevus anemicus
• Congenital circumscribed area of pale vasoconstriction, often 5–10 cm in diameter and occurs most commonly on the trunk (Fig. 87.13).
• The edges are irregular and disappear via diascopy (pressure), allowing distinction from nevus depigmentosus or vitiligo; application of heat or an ice cube accentuates the border as a result of hyperemia of surrounding uninvolved skin.
Angiospastic Macules (Bier Spots)
• Pale macules due to relative vasoconstriction within areas of subtle vascular mottling (Fig. 87.14); as with nevus anemicus, the border disappears with diascopy (pressure); dependency leads to accentuation of lesions due to venous congestion.

Fig. 87.14 Angiospastic macules (Bier spots). Multiple pale macules due to vasoconstriction within a background of erythema on the forearm.
• Most commonly observed in young healthy adults with lightly pigmented skin; no effective Rx.
For further information see Ch. 106. From Dermatology, Third Edition.